Abstract
BACKGROUND
With the aging world population, the incidence of falls has intensified and fall-related hospitalization costs are increasing. Falls are one type of event studied in the health economics of patient safety, and many developed countries have conducted such research on fall-related hospitalization costs. However, China, a developing country, still lacks large-scale studies in this area.
AIM
To investigate the factors related to the hospitalization costs of fall-related injuries in elderly inpatients and establish factor-based, cost-related groupings.
METHODS
A retrospective study was conducted. Patient information and cost data for elderly inpatients (age ≥ 60 years, n = 3362) who were hospitalized between 2016 and 2019 due to falls was collected from the medical record systems of two grade-A tertiary hospitals in China. Quantile regression (QR) analysis was used to identify the factors related to fall-related hospitalization costs. A decision tree model based on the chi-squared automatic interaction detector algorithm for hospitalization cost grouping was built by setting the factors in the regression results as separation nodes.
RESULTS
The total hospitalization cost of fall-related injuries in the included elderly patients was 180479203.03 RMB, and the reimbursement rate of medical benefit funds was 51.0% (92039709.52 RMB/180479203.03 RMB). The medical material costs were the highest component of the total hospitalization cost, followed (in order) by drug costs, test costs, treatment costs, integrated medical service costs and blood transfusion costs The QR results showed that patient age, gender, length of hospital stay, payment method, wound position, wound type, operation times and operation type significantly influenced the inpatient cost (P < 0.05). The cost grouping model was established based on the QR results, and age, length of stay, operation type, wound position and wound type were the most important influencing factors in the model. Furthermore, the cost of each combination varied significantly.
CONCLUSION
Our grouping model of hospitalization costs clearly reflected the key factors affecting hospitalization costs and can be used to strengthen the reasonable control of these costs.
Keywords: Falls, Elderly, Hospitalization costs, Quantile regression model, Decision tree model, Prevention
Core Tip: This retrospective study investigated the composition and factors of the hospitalization costs of fall-related injuries in elderly inpatients and established a factor-based, cost-related group. The total hospitalization costs were 180479203.03 RMB. The quantile regression (QR) results showed that patient age, gender, length of hospital stay, payment method, wound position, wound type, operation times and operation type significantly influenced the inpatient cost (P < 0.05). The cost grouping model was established based on the QR results, and the cost of each combination varied significantly. Our grouping model of hospitalization costs clearly reflects the key factors affecting hospitalization costs.
INTRODUCTION
Falls are defined as “events which result in a person coming to rest inadvertently on the ground or floor or other lower level”[1]. Due to aging of the world population, the incidence of falls has intensified, and the incidence rate in developing countries is greater than that in developed countries[2]. China has been characterized as an aging society since 1999 and is one of the fastest-aging countries in the world[3]. From 2006-2016, the death rate due to falls in China remained relatively high and rose slightly[4]. Falls are also a leading cause of death in developed countries, with one-third of adults aged over 65 falling each year[5]. Regarding the global ranking of causes of death, the World Health Organization has predicted that the ranking of falls will rise from 21st in 2012 to 17th by 2030 if preventive measures are not taken[6]. Falls are the leading cause of accidental injury and death among adults aged over 65 and are the main cause of disability, dysfunction and death in the elderly population[7,8].
The high incidence of injuries after falls results in high medical costs, placing a heavy burden on families and society. According to data from the United States Centers for Disease Control, in 2001 the economic burden caused by falls was US $20 million[9]. Falls among elderly individuals cost the US health care system US $30 billion in direct medical expenses alone in 2011; this amount would be much higher if long-term care costs were considered[10].
The second Global Ministerial Summit on Patient Safety, held in Bonn, Germany in 2017, released the report "The economics of patient safety: Strengthening a value-based approach to reducing patient harm at national level"[11], highlighting the need for health economics research from the patient safety perspective. Partly constituting research on the health economics of patient safety, studies on the economic burden and influencing factors of falls can help in focusing attention on fall prevention.
Studies have been conducted on the cost of falls[12-14], but few have investigated the waste of medical benefit funds or conducted a factor analysis of costs at different levels. To fill this gap, we identified the factors affecting hospitalization costs through quantile regression (QR) analysis. The chi-squared automatic interaction detector (CHAID) decision tree model was used to construct the grouping model of hospital costs for inpatients with fall injuries to further identify the important influencing factors. This research is meaningful for recognizing the importance of fall prevention and providing reasonable suggestions to control hospitalization costs based on health economics theory from the patient safety perspective.
MATERIALS AND METHODS
We conducted a retrospective study by searching and selecting the medical records of elderly inpatients due to falls from 2016-2019 in the electronic medical record system (EMRS) of two hospitals in China.
Setting
The study was conducted in two participating hospitals: The First Affiliated Hospital of Chongqing Medical University and Jinshan Branch of the First Affiliated Hospital of Chongqing Medical University. The First Affiliated Hospital of Chongqing Medical University is a large-scale comprehensive teaching hospital that integrates medical treatment, teaching, scientific research, prevention, and health care and involves a foreign element; it has a 3200-bed tertiary referral center. Jinshan Branch of the First Affiliated Hospital of Chongqing Medical University is also a tertiary referral center. It has 1000 beds and is the only large public hospital in the new north zone. This facility integrates medical treatment, rehabilitation, prevention, and health care and involves a foreign element. The two hospitals have the same EMRS, hospital information system (HIS) and medical insurance management information system.
Participants
Patient records were selected if they met the following criteria: (1) According to the electronic medical record, patients were diagnosed with fall-related injuries upon admission; alternatively, the chief complaint recorded and history of present illness included the keywords "falling”, “falls”, “slip”, “stumble”, “trip”, or “tumble”; (2) Patients were discharged between January 1, 2016, and December 31, 2019; and (3) Patients were ≥ 60 years old. A total of 4059 cases were included. Figure 1 presents a diagram of the inclusion and exclusion process. A total of 3362 valid data points were collected after exclusion.
Figure 1.
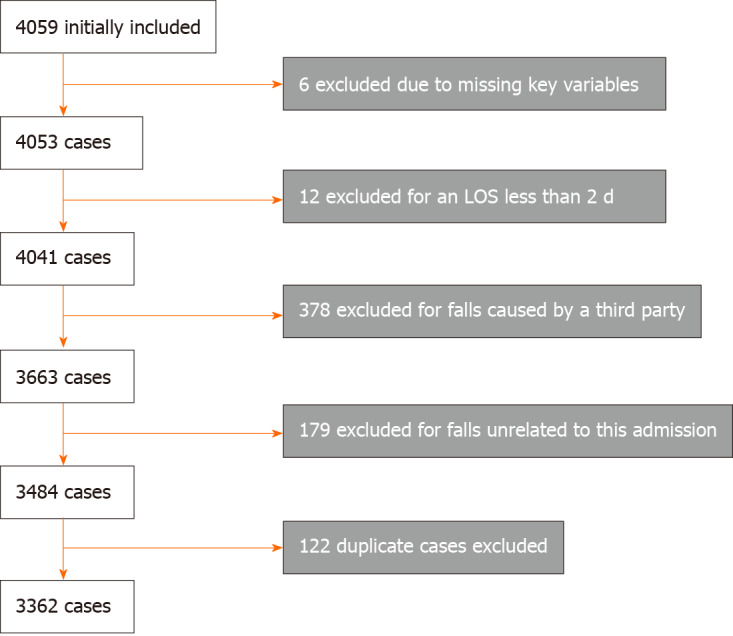
Flow diagram of included and excluded cases. LOS: Length of stay.
Data collection
Based on the results of previous studies and data availability, we imported the patient ID numbers from the EMRS into the HIS to select their gender, age, marital status, length of stay (LOS), operation times, payment method, employment status, community type, pattern of admission, wound position, wound type, operation type and hospitalization costs for analysis. Medicare reimbursement information was obtained from the medical insurance management information system.
Statistical analysis
Before the study, we discussed and built scientific investigation projects with experts in related fields and conducted training for two graduate students participating in this work to explain the research purpose and data retrieval process. During this study, relevant data were collected and numbered based on each hospital’s conditions. Double entry and validation were conducted during data collection and entry to ensure data accuracy.
The consumer price index (CPI) from 2016-2019 published by the National Bureau of Statistics of the People's Republic of China was used to revise amounts to eliminate the impact of inflation and to make the comparison of costs more scientific. The CPI in 2016, 2017, 2018 and 2019 was 101.8%, 101%, 102% and 104.7%, respectively[15].
Excel 2010 was used to establish the database. SPSS 23.0 and STATA 15.1 were used for analysis. The medical costs for the enrolled subjects presented a skewed distribution, which was described by M (P25, P75). Univariate analysis was performed using the rank-sum test and Spearman correlation analysis, and a test level of 0.05 was set. The items with statistically significant differences in the univariate analysis results were taken as independent variables. Costs were log-transformed and included as dependent variables in the QR to analyze the influencing factors, and the 10%, 50%, and 90% quantiles of hospitalization costs were selected for QR analysis. The results were imported into the CHAID decision tree model to establish the grouping model of hospitalization costs.
RESULTS
General information
Of the 3362 inpatients with complete data, 1218 (36.2%) were male and 2144 (63.8%) were female. The average age was 74 ± 9 years, and the average LOS was 14 d. There were 2644 (78.6%) urban residents and 718 (21.4%) rural residents. A total of 1388 (41.3%) cases were admitted from the emergency department, 1714 (51.0%) cases were admitted from the outpatient department, 256 (7.6%) cases were transferred to the hospital, and 4 (0.1%) cases were admitted to the hospital by other means.
Composition of inpatient hospitalization costs
The total hospitalization cost for these patients (n = 3362) was 180479203.03 RMB, and the cost for each patient was 117.00-634774.25 [M = 44788.30 (P25 = 18870.67, P75 = 65783.72)] RMB. Medical material costs were the highest component of the total hospitalization cost, followed (in order) by drug costs, test costs, treatment costs, integrated medical service costs and blood transfusion costs (Table 1). A total of 92039709.52 RMB was reimbursed by medical benefit funds, accounting for 51.0% of the total costs. The reimbursement amount per case ranged from 0.000-621697.62 [M = 15264.22 (P25 = 4308.38, P75 = 36228.40)] RMB.
Table 1.
Cost structure of elderly inpatients due to falls (RMB)
|
Component
|
Frequency (n)
|
Estimated cost (RMB)
|
Percentage of total cost (%)
|
| Medical material | 3158 | 75206147.24 | 41.7 |
| Medicine | 3315 | 29348327.34 | 16.3 |
| Tests | 3354 | 29158384.41 | 16.1 |
| Treatment | 3123 | 24439465.13 | 13.5 |
| Integrated medical services | 3362 | 19654703.83 | 10.9 |
| Blood transfusion | 922 | 2672175.08 | 1.5 |
All costs are expressed in 2019 RMB.
Single-factor analysis
The univariate analysis results in Table 2 show that gender, age, operation times, LOS, payment method, wound position, wound type and operation type had a significant impact on total hospitalization cost (P < 0.05).
Table 2.
Univariate analysis of the hospitalization costs for elderly inpatients due to falls (RMB)
|
Variable
|
Frequency (n)
|
Percentage of total cases (%)
|
Estimated cost [M (P25, P75)]
|
R value
|
P
value
|
| Gender | 0.037 | 0.032a | |||
| Male | 1218 | 36.2 | 41317.97 (14486.61, 66018.59) | ||
| Female | 2144 | 63.8 | 45469.65 (23487.13, 65686.64) | ||
| Age (yr) | 0.060 | 0.000a | |||
| 60-69 | 1221 | 36.3 | 42378.54 (21803.38, 62729.14) | ||
| 70-79 | 1052 | 31.3 | 42991.27 (19400.01, 63875.40) | ||
| ≥ 80 | 1089 | 32.4 | 51642.56 (16687.27, 69590.67) | ||
| Operation times | 0.533 | 0.000a | |||
| 0 (h) | 672 | 20.0 | 10026.07 (5212.80, 21657.76) | ||
| 1-2 | 2456 | 73.0 | 50940.59 (32230.26, 67879.28) | ||
| 3-5 | 234 | 7.0 | 76253.72 (44619.24, 110755.35) | ||
| LOS (d) | 0.520 | 0.000a | |||
| 0-14 | 2410 | 71.7 | 36806.75 (11381.93, 53622.53) | ||
| 15-30 | 721 | 21.4 | 66957.46 (50485.18, 83432.30) | ||
| 31-90 | 198 | 5.9 | 106569.47 (75836.07, 144853.33) | ||
| ≥ 91 | 33 | 1.0 | 137591.53 (69378.56, 223584.67) | ||
| Payment method | -0.051 | 0.003a | |||
| Worker medical insurance | 2022 | 60.1 | 44952.14 (21700.61, 66985.45) | ||
| Resident medical insurance | 1050 | 31.4 | 44962.41 (16506.52, 64478.55) | ||
| Commercial medical insurance | 1 | 0.0 | 1562060.23 | ||
| Individual medical care | 4 | 0.1 | 35922.53 (28653.18, 113184.59) | ||
| Public medical care | 280 | 8.3 | 41233.85 (9716.64, 63933.44) | ||
| Other | 5 | 0.1 | 56320.25 (35953.57, 157804.79) | ||
| Wound position | 0.267 | 0.000a | |||
| None | 2 | 0.0 | 11198.42 (5451.68, 0.00) | ||
| Trunk | 135 | 4.0 | 26295.28 (8463.58, 65953.88) | ||
| Upper limbs | 394 | 11.7 | 39361.70 (8891.22, 54170.21) | ||
| Head and neck | 434 | 12.9 | 20706.67 (9742.51, 42939.47) | ||
| Prosthesis | 7 | 0.2 | 43500.02 (11673.20, 115267.90) | ||
| Organ | 42 | 1.3 | 28087.94 (12783.60, 67501.29) | ||
| Spinal cord | 736 | 21.9 | 41242.70 (26249.93, 52136.72) | ||
| Lower limbs | 1612 | 48.0 | 29935.61 (57052.51, 72001.03) | ||
| Wound type | 0.264 | 0.000a | |||
| Dislocation | 39 | 1.2 | 10786.93 (6307.10, 39300.03) | ||
| Contusion | 216 | 6.4 | 13295.61 (7904.67, 25306.53) | ||
| Soft tissue injury | 63 | 1.9 | 21142.78 (8768.91, 40579.88) | ||
| Joint injury | 143 | 4.2 | 18130.31 (10022.10, 53393.29) | ||
| Visceral rupture | 40 | 1.2 | 36412.73 (12834.19, 57043.39) | ||
| Fracture | 2831 | 84.2 | 48665.48 (26412.69, 68.344) | ||
| Other | 30 | 0.9 | 12262.80 (5962.26, 46411.80) | ||
| Operation type | 0.642 | 0.000a | |||
| None | 673 | 20.0 | 5223.96 (10030.03, 21687.66) | ||
| Fixation | 271 | 8.0 | 5603.54 (9215.08, 16469.74) | ||
| Debridement and suturing | 194 | 5.8 | 16671.87 (52139.40, 90254.74) | ||
| Surgical exploration | 117 | 3.5 | 19388.44 (29844.72, 52741.55) | ||
| Open reduction | 1296 | 38.5 | 37836.56 (46549.68, 62950.43) | ||
| Replacement | 682 | 20.3 | 57135.64 (67049.09, 79342.16) | ||
| Decompression | 56 | 1.7 | 63967.42 (85712.16, 108458.43) | ||
| Other | 73 | 2.2 | 11879.72 (36707.28, 93072.05) |
All costs are expressed in 2019 RMB.
P < 0.05.
QR analysis
Based on the univariate analysis results, gender, age, LOS, payment method, wound position, wound type, operation times, and operation type were selected as independent variables for inclusion in the model.
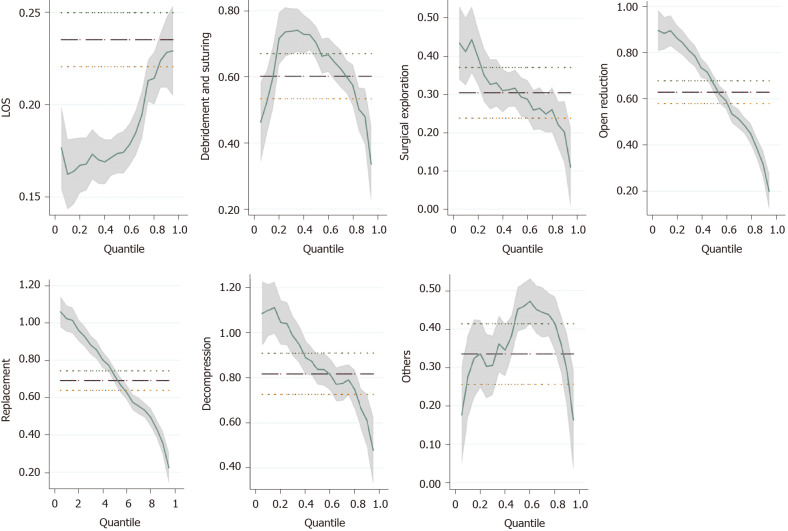
As shown in Table 3, the pseudo R2 of the three quantiles decreased from 0.5467 to 0.3848, indicating that the fitting results of the model were optimal at the 10% quantile. The coefficient changes in factors with a significant influence at the 10%, 50% and 90% quantiles of hospitalization cost are shown in Figure 2.
Table 3.
Quantile regression analysis of hospitalization costs
|
Variable
|
Hospitalization costs
|
||
|
Q10
|
Q50
|
Q90
|
|
| Operations times | 0.038 | 0.067b | 0.133b |
| LOS | 0.162b | 0.174b | 0.228b |
| Age | 0.038b | 0.018b | 0.003 |
| Gender (Contrast = Male) | |||
| Female | 0.01 | 0.018 | 0.026a |
| Payment methods (Contrast = Worker medical insurance) | |||
| Resident medical insurance | 0.005 | 0.007 | -0.008 |
| Commercial medical insurance | -0.35 | -0.751b | -1.185b |
| Individual medical care | 0.176 | 0.034 | -0.017 |
| Public medical care | -0.184b | -0.019 | 0.006 |
| Other | -0.057 | 0.054 | -0.107 |
| Wound position (Contrast = None) | |||
| Trunk | -0.277 | 0.063 | 0.646b |
| Upper limbs | -0.393 | -0.066 | 0.502a |
| Head and neck | -0.117 | 0.317 | 0.763b |
| Prosthesis | -0.227 | 0.049 | 0.500 |
| Organ | -0.314 | 0.2 | 0.760b |
| Spinal cord | -0.342 | -0.037 | 0.497a |
| Lower limbs | -0.305 | 0.022 | 0.584a |
| Wound type (Contrast = Dislocation) | |||
| Contusion | 0.890b | -0.153a | -0.187a |
| Soft tissue injury | 0.942b | -0.052 | -0.08 |
| Joint injury | 0.757b | -0.06 | -0.112 |
| Visceral rupture | 0.851b | 0.015 | 0.047 |
| Fracture | 0.900b | 0.068 | -0.006 |
| Other | 0.735b | -0.162a | -0.025 |
| Operation type (Contrast = None) | |||
| Fixation | -0.024 | -0.071a | -0.209b |
| Debridement and suturing | 0.523b | 0.704b | 0.480b |
| Surgical exploration | 0.413b | 0.317b | 0.202b |
| Open reduction | 0.883b | 0.666b | 0.319b |
| Replacement | 1.023b | 0.717b | 0.355b |
| Decompression | 1.100b | 0.837b | 0.608b |
| Other | 0.276b | 0.452b | 0.286b |
| Pseudo R2 | 0.5467 | 0.4767 | 0.3848 |
P < 0.05.
P < 0.01. LOS: Length of stay.
Figure 2.
Coefficient curves in the quantile regression analysis. The factors with significant influence at 10%, 50% and 90% quantiles of hospitalization expenses were selected for plotting. LOS: Length of stay.
Patient LOS and operation type had a significant impact on the three quantiles of total hospitalization cost (P < 0.05), and the influence of patient LOS and operation times at the highest quantile was greater than that at the lowest quantile. Regarding operation type, the hospitalization costs for surgical exploration, open reduction, replacement and decompression were significantly higher at the 10% quantile than for patients without surgery. The costs for patients with debridement and suturing and other types of surgery were significantly higher at the 50% quantile (P < 0.05). The hospitalization costs for patients with fixation were significantly lower at the 90% quantile (P < 0.05). The influence of age at the low quantile of cost was greater than that at the middle quantile. The hospitalization costs for female patients were significantly higher than those for male patients at the 90% quantile (P < 0.05). Patients who chose to use commercial medical insurance and public medical care for reimbursement paid lower hospitalization costs than those who chose to use worker medical insurance at the 90% and 10% quantiles, respectively. Regarding wound position, the costs for patients with trunk, upper limb, head and neck, organ, spinal cord and lower limb injuries were significantly higher at the 90% quantile than for those without injuries (P < 0.05). The wound type had a significant positive effect at the 10% quantile of costs (P < 0.05).
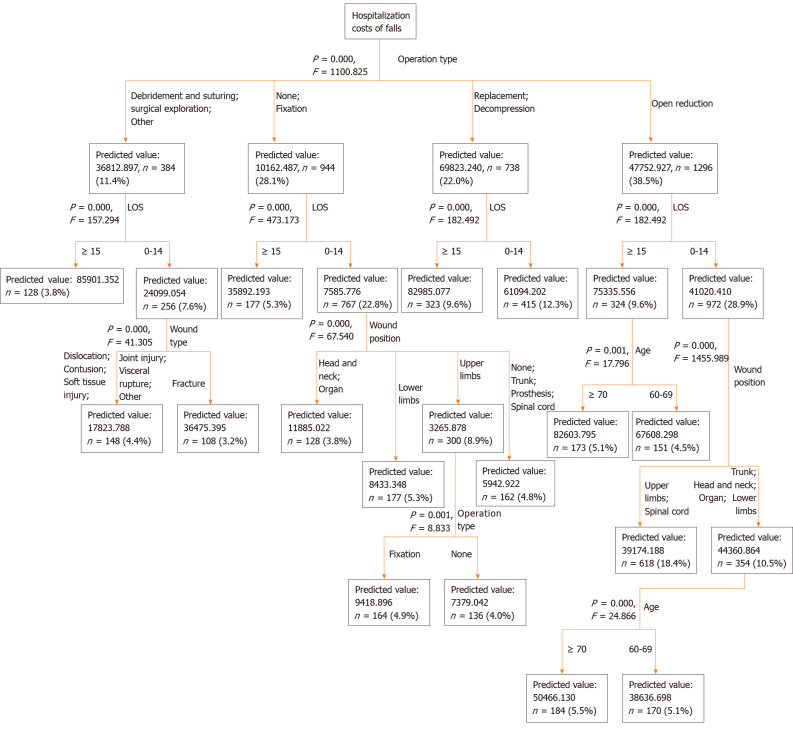
Hospitalization cost grouping
We constructed and conducted branch reduction on the decision tree model using the CHAID algorithm[16]. Inpatient hospitalization costs were taken as the dependent variable, and age, gender, operation times, LOS, payment method, wound position, wound type and operation type were used as classification nodes. The parameters used in this study were as follows: The maximum depth of the decision tree was 5; the minimum sample number of the parent node was 200; the minimum sample number of the child node was 100; and the significance level of the splitting node was α = 0.05[17]. The grouping results are shown in Figure 3.
Figure 3.
Grouping results based on the decision tree model. LOS: Length of stay.
Based on the decision tree analysis, 5 variables, including age, LOS, operation type, wound position and wound type, were finally determined. Patients who had debridement and suturing, surgical exploration or other operations and who stayed in the hospital for more than 15 d had the highest hospitalization costs, while the costs for those who had fixation or no operation, stayed in the hospital for less than 14 d, and had trunk, prosthesis, spinal cord or no injuries were the lowest. The between-group hypothesis test (P < 0.05) indicated that the cost difference between the groups was relatively large and the within-group variation in hospitalization costs was relatively small, demonstrating that the grouping of the model was reasonable.
DISCUSSION
This study found that hospitalization costs resulting from falls totaled more than 100 million RMB, and the reimbursement rate of medical insurance funds exceeded 50%. The costs of falls among elderly Chinese patients were lower than those reported in high-income countries. A recent study in Texas reported that the cost of falls for people aged over 65 was greater than US $1.1 billion[18]. A study conducted in the United States showed that the average hospitalization cost for falls was US $29562[12], while in Canada the mean cost for hip fracture patients older than 50 was US $19743[19]. This lower amount may be due to differences in medical costs between the countries and differences in the quality of health care. The medical cost of falls is an avoidable expense because falls cause avoidable accidental injuries. Measures to support fall prevention are beneficial for reducing this unnecessary economic burden.
Among the hospitalization costs for elderly patients due to falls, medical material costs accounted for the highest proportion (41.7%), which might be related to the large number of patients in this study with fracture injuries. Surgery was the main method of treatment for fracture injuries, and internal fixation devices or joint prostheses were frequently used. These materials are expensive and thus inevitably drive up hospitalization costs. To reduce the economic burden of patients with fall injuries, it is necessary to strengthen the management of high-value medical materials and advocate choosing cost-effective materials without affecting patient safety.
Although many developed countries have conducted relevant studies on the hospitalization costs of falls[9,10,18,20-22], there are few statistical analyses of the influencing factors of such hospitalization costs. Understanding the influencing factors of these costs will help governments improve the cost management system.
In addition to investigating the economic burden caused by falls, QR analysis and grouping model construction for hospitalization costs were conducted to determine the influencing factors.
The QR results showed that operation times, LOS and gender had a significant positive effect in the group with higher expenses. In a prior analysis by Wiktorowicz et al[19], the cost varied depending on the context of a patient’s place of residence, age, and survival to 1 year. We found that more women than men were hospitalized due to falls. Studies have reported that the risk of falls differs by gender, and women are more likely to fall than men[23,24], which might be related to the more rapid loss of muscle strength in women.
The cost for patients with worker medical insurance was higher than that for patients with commercial or public medical insurance in the different quantiles, which might be associated with the high reimbursement rate of worker medical insurance in China. The high reimbursement rate indirectly increases the treatment demand.
Age had a greater impact on people with low costs. This could be because people with low costs may pay less attention to their health in daily life than people with high costs. The influence of age on medical costs was closely related to the patient’s health condition, and improving the health condition can obviously reduce the incidence of disease and medical consumption caused by age. Thus, it is necessary to strengthen disease prevention and treatment.
The position and type of wound had an impact on the different cost quantiles. Hall et al also showed that the type of injury was the most significant determinant of hospital costs. These findings indicate that fall prevention measures should consider how to reduce the extent of a patient’s injuries. For example, people may be able to reduce the severity of injury by wearing a protective device should a fall occur.
Our study revealed that all types of surgery, except fixation, had a significant positive effect on the total cost. Complex surgery not only increases the use of medical materials but also increases the LOS due to a complicated postoperative recovery. Therefore, promoting enhanced recovery after surgery would be very effective in reducing hospitalization costs at the high, medium and low quantiles[25,26].
Based on QR analysis, statistically significant variables were included in the CHAID decision tree analysis. The decision tree's predictive risk score was found to be 0.071. The cost grouping model could clearly and intuitively reflect the influencing factors of cost. These findings provide guidance for relevant departments to formulate targeted improvement measures that could help to reduce the economic burden of disease. They also provide a reference value for improving medical insurance payment standards.
Limitations of the study
In this study, the economic burden estimation followed the principle of robust estimation, measuring direct medical costs. However, some patients did not complete all of their treatment due to economic disadvantages, complicated diseases or other conditions during hospitalization; therefore, the actual costs are likely higher.
CONCLUSION
This study discusses the medical economic burden caused by falls. Although falls are avoidable, the medical costs due to falls are expensive, and the reimbursement rate of medical benefit funds is high. The economic benefits of prevention far outweigh those of treatment. The grouping model of fall hospitalization expenses constructed in this study provides a reference for identifying key points of cost management and control.
ARTICLE HIGHLIGHTS
Research background
With the aging world population the incidence of falls has intensified and hospitalization costs are increasing. Falls are one type of event studied in the health economics of patient safety.
Research motivation
Many developed countries have conducted research on fall-related hospitalization costs. However, China, a developing country, still lacks large-sample studies.
Research objectives
The aim of the study was to investigate the composition and factors related to the hospitalization costs of fall-related injuries in elderly inpatients and establish factor-based, cost-related groupings to provide a basis for the rational economic control of hospitalization costs.
Research methods
Quantile regression (QR) analysis was used to identify the factors related to fall-related hospitalization costs. A decision tree model based on the chi-squared automatic interaction detector algorithm for hospitalization cost grouping was built by setting the factors in the regression results as separation nodes.
Research results
The total hospitalization cost of fall-related injuries in the elderly patients investigated was 180479203.03 RMB. The cost grouping model was established based on the QR results, and patient age, length of stay, operation type, wound position and wound type were the most important influencing factors in the model.
Research conclusions
Our grouping model of hospitalization costs clearly reflects the key factors affecting hospitalization costs and is meaningful for strengthening the reasonable control of these costs.
Research perspectives
This was a retrospective study; hence, a prospective large-scale multicenter study is still required.
ACKNOWLEDGEMENTS
We are grateful to the medical insurance information center, the medical record management center and the hospital information center of The First Affiliated Hospital of Chongqing Medical University and the Jinshan Branch of the First Affiliated Hospital of Chongqing Medical University for their help.
Footnotes
Institutional review board statement: The study was approved by the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University (Approval No. 2019-288).
Informed consent statement: Informed written consent was obtained from the patients for publication of this report and any accompanying images.
Conflict-of-interest statement: The authors declare that they have no conflicts of interest.
Manuscript source: Unsolicited manuscript
Peer-review started: August 13, 2020
First decision: November 23, 2020
Article in press: December 16, 2020
Specialty type: Geriatrics and gerontology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Lukman AF S-Editor: Zhang H L-Editor: Webster JR P-Editor: Ma YJ
Contributor Information
Fei-Yue Su, Department of Urology, The First Affiliated Hospital of Chongqing Medical University, Chongqing 400016, China.
Mei-Ling Fu, Department of Medical Insurance, The First Affiliated Hospital of Chongqing Medical University, Chongqing 400016, China.
Qing-Hua Zhao, Department of Nursing, The First Affiliated Hospital of Chongqing Medical University, Chongqing 400016, China.
Huan-Huan Huang, Department of Nursing, The First Affiliated Hospital of Chongqing Medical University, Chongqing 400016, China.
Di Luo, Department of Urology, The First Affiliated Hospital of Chongqing Medical University, Chongqing 400016, China.
Ming-Zhao Xiao, Department of Urology, The First Affiliated Hospital of Chongqing Medical University, Chongqing 400016, China. xmz.2004@163.com.
Data sharing statement
The data underlying this article were provided by The First Affiliated Hospital of Chongqing Medical University and the Jinshan Branch of The First Affiliated Hospital of Chongqing Medical University under licence. Data will be shared on request to the corresponding author with permission of The First Affiliated Hospital of Chongqing Medical University and the Jinshan Branch of The First Affiliated Hospital of Chongqing Medical University.
References
- 1.Peng K, Tian M, Andersen M, Zhang J, Liu Y, Wang Q, Lindley R, Ivers R. Incidence, risk factors and economic burden of fall-related injuries in older Chinese people: a systematic review. Inj Prev. 2019;25:4–12. doi: 10.1136/injuryprev-2018-042982. [DOI] [PubMed] [Google Scholar]
- 2.Khow KSF, Visvanathan R. Falls in the Aging Population. Clin Geriatr Med. 2017;33:357–368. doi: 10.1016/j.cger.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 3.Hao X, Yang Y, Gao X, Dai T. Evaluating the Effectiveness of the Health Management Program for the Elderly on Health-Related Quality of Life among Elderly People in China: Findings from the China Health and Retirement Longitudinal Study. Int J Environ Res Public Health. 2019;16 doi: 10.3390/ijerph16010113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cheng P, Wang L, Ning P, Yin P, Schwebel DC, Liu J, Qi J, Hu G, Zhou M. Unintentional falls mortality in China, 2006-2016. J Glob Health. 2019;9:010603. doi: 10.7189/jogh.09.010603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carpenter CR, Cameron A, Ganz DA, Liu S. Older Adult Falls in Emergency Medicine: 2019 Update. Clin Geriatr Med. 2019;35:205–219. doi: 10.1016/j.cger.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization. Injuries and violence: the facts. 2014. Cited 1 August 2020 Available from: https://apps.who.int/iris/handle/10665/149798 .
- 7.Saftari LN, Kwon OS. Ageing vision and falls: a review. J Physiol Anthropol. 2018;37:11. doi: 10.1186/s40101-018-0170-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gilbert R, Todd C, May M, Yardley L, Ben-Shlomo Y. Socio-demographic factors predict the likelihood of not returning home after hospital admission following a fall. J Public Health (Oxf) 2010;32:117–124. doi: 10.1093/pubmed/fdp077. [DOI] [PubMed] [Google Scholar]
- 9.McMurdo ME. 'Guideline for the prevention of falls in older persons': essential reading. Age Ageing. 2002;31:13–14. doi: 10.1093/ageing/31.1.13. [DOI] [PubMed] [Google Scholar]
- 10.Mills KM, Sadler S, Peterson K, Pang L. An Economic Evaluation of Preventing Falls Using a New Exercise Program in Institutionalized Elderly. J Phys Act Health. 2018;15:397–402. doi: 10.1123/jpah.2017-0225. [DOI] [PubMed] [Google Scholar]
- 11.Slawomirski L , Auraaen A, Klazinga NS. The economics of patient safety: Strengthening a value-based approach to reducing patient harm at national level. 2017. Available from: OECD Health Working Papers: No. 96.
- 12.Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. J Am Geriatr Soc. 2018;66:693–698. doi: 10.1111/jgs.15304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Burns ER, Stevens JA, Lee R. The direct costs of fatal and non-fatal falls among older adults - United States. J Safety Res. 2016;58:99–103. doi: 10.1016/j.jsr.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haddad YK, Bergen G, Florence CS. Estimating the Economic Burden Related to Older Adult Falls by State. J Public Health Manag Pract. 2019;25:E17–E24. doi: 10.1097/PHH.0000000000000816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Bureau of Statistics, PRC 2019, September 12. Cited 1 August 2020 Available from: http://data.stats.gov.cn .
- 16.Li H, Wu TT, Yang DL, Guo YS, Liu PC, Chen Y, Xiao LP. Decision tree model for predicting in-hospital cardiac arrest among patients admitted with acute coronary syndrome. Clin Cardiol. 2019;42:1087–1093. doi: 10.1002/clc.23255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu SW, Pan Q, Chen T. Research on diagnosis-related group grouping of inpatient medical expenditure in colorectal cancer patients based on a decision tree model. World J Clin Cases. 2020;8:2484–2493. doi: 10.12998/wjcc.v8.i12.2484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Towne SD, Smith ML, Li Y, Dowdy D, Ahn S, Lee S, Yoshikawa A, Jiang L. A Multi-Level Analyses of Charges and Cost of Fall-Related Hospitalizations Among Older Adults: Individual, Hospital, and Geospatial Variation. J Aging Soc Policy. 2020:1–22. doi: 10.1080/08959420.2020.1740639. [DOI] [PubMed] [Google Scholar]
- 19.Wiktorowicz ME, Goeree R, Papaioannou A, Adachi JD, Papadimitropoulos E. Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporos Int. 2001;12:271–278. doi: 10.1007/s001980170116. [DOI] [PubMed] [Google Scholar]
- 20.DeGrauw X, Annest JL, Stevens JA, Xu L, Coronado V. Unintentional injuries treated in hospital emergency departments among persons aged 65 years and older, United States, 2006-2011. J Safety Res. 2016;56:105–109. doi: 10.1016/j.jsr.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 21.Hartholt KA, Polinder S, Van der Cammen TJ, Panneman MJ, Van der Velde N, Van Lieshout EM, Patka P, Van Beeck EF. Costs of falls in an ageing population: a nationwide study from the Netherlands (2007-2009) Injury. 2012;43:1199–1203. doi: 10.1016/j.injury.2012.03.033. [DOI] [PubMed] [Google Scholar]
- 22.Heinrich S, Rapp K, Rissmann U, Becker C, König HH. Service use and costs of incident femoral fractures in nursing home residents in Germany: the Bavarian Fall and Fracture Prevention Project (BF2P2) J Am Med Dir Assoc. 2011;12:459–466. doi: 10.1016/j.jamda.2010.11.008. [DOI] [PubMed] [Google Scholar]
- 23.Hoang OT, Jullamate P, Piphatvanitcha N, Rosenberg E. Factors related to fear of falling among community-dwelling older adults. J Clin Nurs. 2017;26:68–76. doi: 10.1111/jocn.13337. [DOI] [PubMed] [Google Scholar]
- 24.Kwan MM, Close JC, Wong AK, Lord SR. Falls incidence, risk factors, and consequences in Chinese older people: a systematic review. J Am Geriatr Soc. 2011;59:536–543. doi: 10.1111/j.1532-5415.2010.03286.x. [DOI] [PubMed] [Google Scholar]
- 25.Quack V, Ippendorf AV, Betsch M, Schenker H, Nebelung S, Rath B, Tingart M, Lüring C. [Multidisciplinary Rehabilitation and Fast-track Rehabilitation after Knee Replacement: Faster, Better, Cheaper? Rehabilitation (Stuttg) 2015;54:245–251. doi: 10.1055/s-0035-1555887. [DOI] [PubMed] [Google Scholar]
- 26.Elsarrag M, Soldozy S, Patel P, Norat P, Sokolowski JD, Park MS, Tvrdik P, Kalani MYS. Enhanced recovery after spine surgery: a systematic review. Neurosurg Focus. 2019;46:E3. doi: 10.3171/2019.1.FOCUS18700. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article were provided by The First Affiliated Hospital of Chongqing Medical University and the Jinshan Branch of The First Affiliated Hospital of Chongqing Medical University under licence. Data will be shared on request to the corresponding author with permission of The First Affiliated Hospital of Chongqing Medical University and the Jinshan Branch of The First Affiliated Hospital of Chongqing Medical University.