Abstract
Background
Heart failure is the third most fatal disease in Germany and generates considerable treatment costs. The multimodal program of inpatient rehabilitation can improve the symptoms and prognosis of these patients. At the present time, however, only few data are available on the effectiveness of rehabilitation for heart failure patients.
Methods
After receiving study approval from the ethics committee of the Saxony–Anhalt Medical Association, 200 patients with a primary or secondary diagnosis of heart failure were prospectively included in the study at Paracelsus-Harz-Clinic Bad Suderode, Quedlinburg, Germany. Baseline parameters such as age, gender, and BMI were documented. Outcome variables included NYHA classifications, quality of life, and mortality. For follow-up, the patients were contacted again by mail or phone after three and 12 months and, data on symptoms and serious events were recorded.
Results
The proportion of patients with a highly reduced ejection fraction (HFrEF) was 13.5%, with a midrange reduced ejection fraction (HFmrEF) 33%, and with preserved ejection fraction (HFpEF) 53.5%. The mean age was 64 ± 11.9 years, the proportion of women 24.1%. The effects of rehabilitation were documented by low overall mortality (no patient died during the stay, only 4% of the patients died in the 12-month follow-up) and an improvement in NYHA classification during and after the inpatient rehabilitation.
Conclusion
This monocentric study showed effects both for symptoms (improvement in NYHA classifications) and prognosis (overall mortality) after rehabilitation. These data reflect the effectiveness of multimodal rehabilitation and underscore the need for rehabilitation in patients diagnosed with heart failure after an acute event and hospital stay or who present with chronic deterioration.
Keywords: heart failure, cardiac rehabilitation, inpatient rehabilitation
Introduction
Heart failure (HF) is a chronic and progressive disease that affects millions of people worldwide. In these patients, performance is reduced owing to an insufficient supply of oxygen-saturated blood to the body. HF represents a serious clinical syndrome, which can become manifest in dyspnea, cyanosis, edema and reduced performance.1 Mortality is high2 and HF is associated with expensive medical care.3 In Germany, chronic HF is the third most common cause of death among men and the fourth most common among women. The current prevalence of HF in this country is 2–3.9%, with an annual increase of 400,000 patients. The older the patients are, the higher the risk of illness becomes.1 Owing to the increasing aging of the population and the increased chances of survival for people with coronary heart disease, cardiomyopathy, or secondary myocardial diseases, the rate of chronic HF can also be expected to rise in the next decades, too.4 Disease progression is often accompanied by acute life-threatening decompensations and hospitalization in the course of the illness. This, in turn, results in damage to the heart muscle and promotes the progression of the disease.5
The multimodal program of inpatient rehabilitation can improve symptoms and prognosis in these patients, and also help prevent decompensations.3 Optimization of the pharmacotherapy initiated during a hospital stay after an acute event, implementation of standardized training courses, individualized endurance and coordination training, and psychological support with help for professional reintegration constitute core components of the rehabilitation program for HF patients.6 At the present time, however, only few data are available on the effectiveness of rehabilitation for these individuals. Hardly any studies at all have addressed the issue of inpatient rehabilitation with heart failure at all.7
The goal of this work is to evaluate the treatment of patients with HF during and after inpatient rehabilitation.
Patients and Methods
After receiving approval from the ethics committee of the Saxony–Anhalt Medical Association, 200 consecutive patients with a main or secondary diagnosis of HF were prospectively included in this study conducted at Paracelsus Harz Clinic, Bad Suderode, Quedlinburg, Germany, after giving written informed consent. Patients were recruited from September 2016 to July 2017. Our study complies with the Declaration of Helsinki.
General parameters such as age, gender, body mass index (BMI), social status, and left ventricular ejection fraction (LVEF) were collected. Outcome variables included NYHA class, re-hospitalization, and mortality before and after discharge. Furthermore, quality of life (SF12- questionnaire), depression, and anxiety questionnaires (HADS-D- questionnaires) were evaluated.
We divided the patients into three groups based on the left ventricular ejection fraction (LVEF), according to the AHA guideline from 2016. Patients with a current LVEF of less than 40% were assigned to the HFrEF group (Heart Failure with reduced Ejection Fraction). Patients with a LVEF above or equal to 50% represented the HFpEF group (Heart Failure with preserved ejection fraction). Those patients whose LVEF was between 40% and 49% were assigned to the HFmrEF group (Heart Failure with midrange Ejection Fraction).8
For the follow-up, the patients were contacted again by mail or phone after 3 and 12 months. Data on symptoms, serious events, and current medication were collected, and, again, questionnaires for monitoring quality of life, depression, and anxiety were completed.
In the SF-12 test, in order to record quality of life, for example, the patients were asked whether they were still able to take care of their everyday affairs or make social contacts, as they were in the past. They could grade their answers between 0, nothing is possible, and 3, having no restrictions.9 In the HADS-D test, there were two times seven questions, each to record the current level of anxiety and depression in the patient. For example, patients were asked whether they suddenly became anxious because of their illness or whether they were already worried upon waking up. They could answer yes or no.10 When classifying the NYHA classification, the patients had to state subjectively whether they have no dyspnea (NYHA I), dyspnea during heavy activity (NYHA II), dyspnea during light activity (NYHA III) or rest dyspnea (NYHA IV).11
Standard rehabilitation for patients with HF in the Paracelsus–Harz Clinic consists of medical history, laboratory tests, and electrocardiogram (ECG) at admission and cycle ergometry and echocardiography the day after admission. Depending on physical fitness, severity of primary disease, comorbidities, and other confounders, the exercise and rehabilitation program is set up the day after admission. Patients in good clinical condition participate 6 days a week in heart rate-monitored, 30-minute cycle ergometry training. Moreover, these patients participated in Nordic Walking, medical training therapy, intensive gymnastic/exercises, and other activities. Patients who are less physically fit participate in group exercises, chair exercises, and personal training sessions. All patients, independent of their physical fitness, attend seminars and lectures as part of the three-week rehabilitation program. Accordingly after classification of our study patients, all collected parameters were compared among these three HF groups.
The aim of these tests was to determine whether there are any correlations between the different HF groups with regard to the parameters surveyed, as well as the advantages and disadvantages of treatment.
Statistical Methods
Continuous variables are reported as mean ± standard deviation (SD) and categorical variables as percentage. Chi-squared test and one-factor ANOVA test were used to compare continuous, skewed, and categorical variables, respectively. A p-value <0.05 was considered statistically significant. All computations were carried out with SPSS software (version 25; IBM Corporation, Armonk, NY, USA).
Results
The mean patient age was 64.7 ± 11.9 years, 75.9% were male, and mean BMI was 29.0 ± 5.2 kg/m2. Mean length of inpatient rehabilitation was 27.7 ± 3.5 days. Furthermore, 1.5% had no educational qualifications and 11.8% had a university degree. Among the study participants, 33.8% were still in gainful employment and 56.8% had already retired. German pension insurance covered costs for 18.2% and health insurance for 51.8% of the patients. Arterial hypertension was reported in 79.9% of all patients at admission. Other cardiovascular risk factors included active smoking in 29.1% and diabetes in 41.7%. Further comorbidities are presented in Table 1. The proportion of patients with a highly reduced ejection fraction (HFrEF) was 13.5%, with a midrange reduced ejection fraction (HFmrEF) 33%, and with preserved ejection fraction (HFpEF) 53.3%. Follow-up information was obtained from 90.5% of the patients after 12 months.
Table 1.
Patient Characteristics
| Variables | N=200 |
|---|---|
| Sociodemographic data | |
| Age (years) | 64.7 ± 11.9 |
| Female sex (%) | 24.1 |
| Male sex (%) | 75.9 |
| Weight (kg) | 86.2 ± 17.1 |
| BMI (kg/m2) | 29 ± 5.2 |
| Length of inpatient rehabilitation (days) | 21.7 ± 3.5 |
| Patient history/comorbidities | |
| Active smoking (%) | 29.1 |
| Hypertension (%) | 79.9 |
| Diabetes (%) | 41.7 |
| COPD (%) | 8 |
| Dyslipoproteinemia (%) | 69.8 |
| Renal insufficiency (%) | 16.1 |
| Atrial fibrillation (%) | 23.1 |
| Coronary heart disease (%) | 45.7 |
| Acute myocardial infarction (%) | 66.3 |
| Pulmonary embolism (%) | 4.5 |
| Heart Failure groups | |
| HFrEF (%) | 13.5 |
| HFmrEF (%) | 33 |
| HFpEF (%) | 53.5 |
| Cost bearer | |
| German pension insurance (%) | 48.2 |
| Health insurance (%) | 51.8 |
| Graduation | |
| No graduation (%) | 1.5 |
| Apprenticeship (%) | 86.7 |
| Graduate (%) | 11.8 |
| Employment | |
| Employed (%) | 33.8 |
| Unemployed (%) | 9 |
| Retired (%) | 56.8 |
Note: Categorial variables are presented in percent; continuous normally distributed variables as mean ± standard deviation at admission.
Abbreviations: HFrEF, highly reduced ejection fraction; HFmrEF, midrange reduced ejection fraction; HFpEF, preserved ejection fraction.
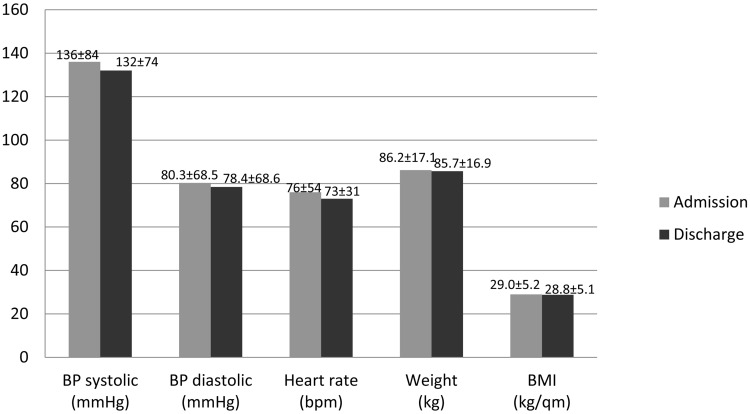
Figure 1 compares the vital parameters of the patients between inpatient admission and discharge. Systolic blood pressure dropped from an average of 136 mmHg to 132 mmHg and diastolic blood pressure fell from 80 mmHg to 78 mmHg. The heart rate decreased from 76 to 73 bpm during the inpatient stay. The patients lost an average of 0.7 kg in weight, which resulted in a drop in the BMI from 29.0 to 28.8 kg/m2.
Figure 1.
Development of vital parameters between admission and discharge.
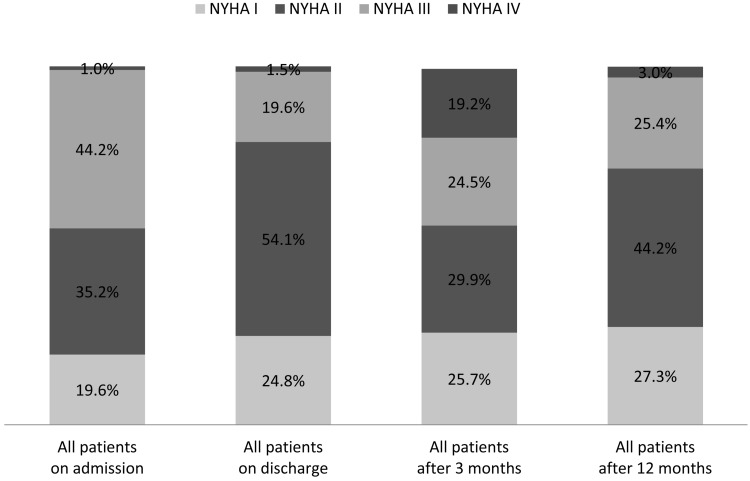
The effects of the rehabilitation were documented by an improvement in the NYHA classification during and partly after the inpatient rehabilitation (Figure 2). The share of patients with NYHA I class rose from 19.6% at admission to 24.8% at discharge and was even 27.3% after 1 year. NYHA class II rose from 35.2% at admission to 54.1% at discharge and was 44.2% after 1 year. NYHA class III fell from 44.2% at admission to 19.6% at discharge and was still 25.4% after 1 year. NYHA class IV was 1% at admission, 1.5% at discharge, and 3% after 1 year.
Figure 2.
NYHA-classes during study course.
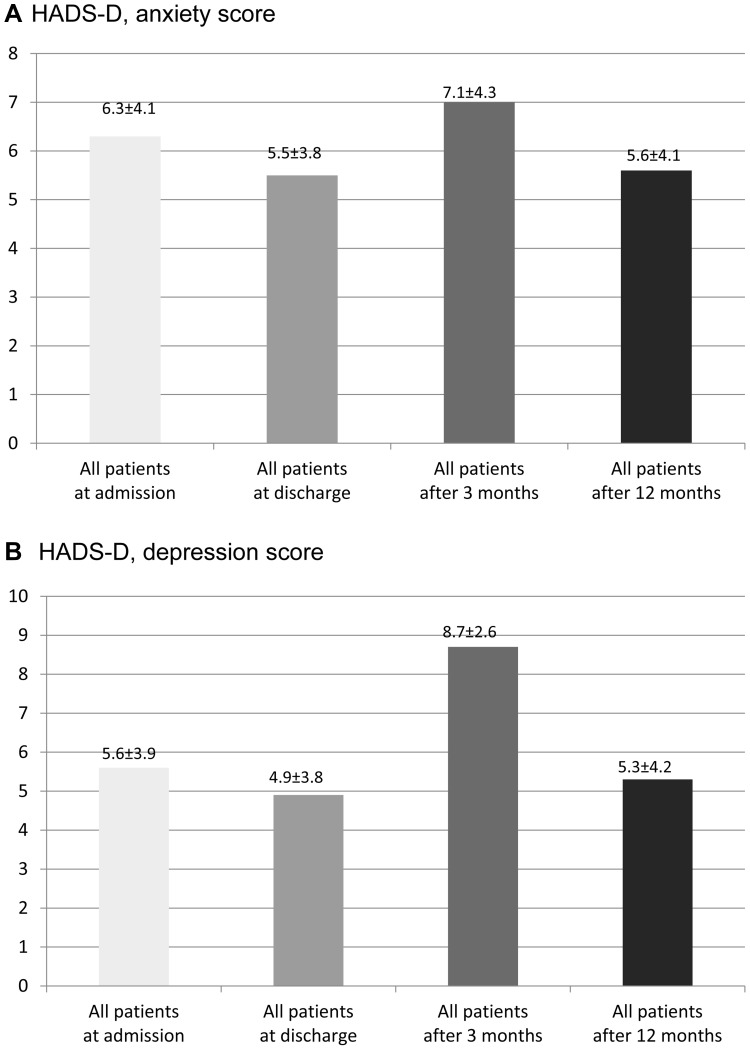
Neither HADS-D anxiety nor HADS-D depression scores had changed significantly between the time of admission and discharge as compared to the types of HF. The overall value of the anxiety symptoms was slightly below the middle of the range (score 8–11) both at admission and upon released from the hospital. This trend and the lack of statistical significance were also observed in the follow-up surveys (Figure 3A and B).
Figure 3.
(A) HDS-D, anxiety score. (B) HADS-D, depression score.
The questionnaires on the quality of life of the patients (SF-12) also did not differ significantly between the groups and during the course of the study. The values of the physical summation scale as a whole are below the average total value of 50 per summation scale. The psychological summation scale shows an increase by approximately three points, which indicates a slight improvement in the psychological state. An analogous dynamic can be found in the evaluation of the SF-12 values after 3 and 12 months (Figure 4A and B).
Figure 4.
(A) SF-12: Physical summation scale. (B) SF-12: Psychologic summation scale.
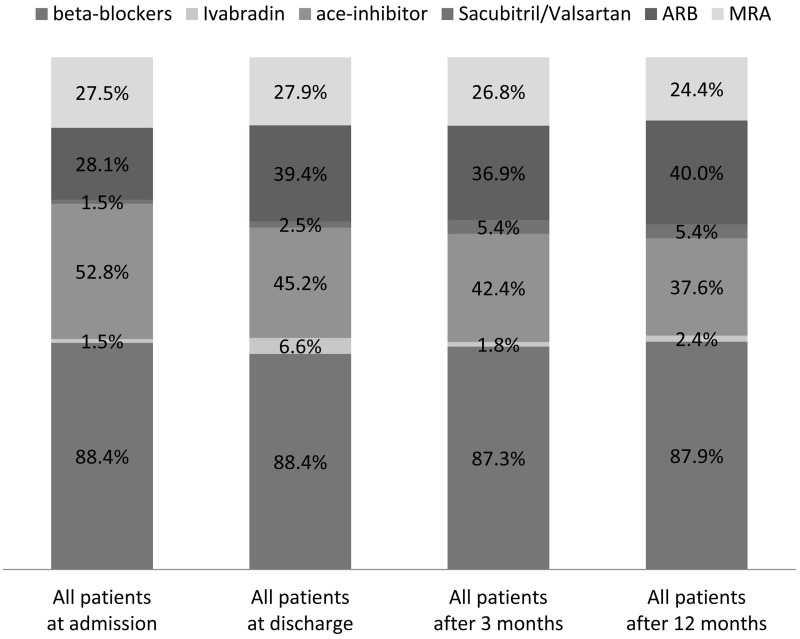
Drug Treatment
Drug treatment is outlined in Table 2. The drugs typically used for HF patients3 are beta-blockers, ACE inhibitors, angiotensin-receptor blockers (ARB), mineralocorticoid receptor antagonists (MRA), Ivabradine, and sacubitril/valsartan. Their use during and after inpatient rehabilitation is shown in Figure 5. At admission, 52.8% of the patients were using ACE inhibitors. Here, a change was observed during the course of the study, with 45.2% taking ACE inhibitors at discharge and 37.6% after 12 months. The use of beta-blockers was stable at 88.4% at admission and discharge and decreased to 87.9% after 1 year. At admission, 28.1% of the patients were taking ARBs. ARB use rose at discharge to 39.4% and to 40% after 1 year. The use of MRAs was nearly stable: 27.5% at admission and 27.9% at discharge. This rate changed during the study follow-up period to 24.4% after 12 months. The use of Ivabradine rose from 1.5% at admission to 6.6% at discharge and fell to 2.4% after 1 year. Medication with sacubitril/valsartan rose continuously from 1.5% at admission to 2.5% at discharge and to 5.5% after 1 year.
Table 2.
Drug Treatment During Study Course
| Drug, % | Admission | Discharge | After 3 Months | After 12 Months |
|---|---|---|---|---|
| Ca-antagonists | 24.1 | 33.8 | 28.8 | 29.7 |
| Beta-blockers | 88.4 | 88.4 | 87.3 | 87.9 |
| Ivabradine | 1.5 | 6.6 | 1.8 | 2.4 |
| Amiodaron | 4.5 | 2.5 | 3.0 | 3.0 |
| ACE inhibitors | 52.8 | 45.2 | 42.4 | 37.6 |
| ARBs | 28.1 | 39.4 | 36.9 | 40.0 |
| Sacubitril/valsartan | 1.5 | 2.5 | 5.4 | 5.5 |
| MRA | 27.5 | 27.9 | 26.8 | 24.4 |
| Statins | 75.4 | 83.3 | 79.4 | 76.4 |
| Aspirin | 71.9 | 67.7 | 66.1 | 63.6 |
| P2Y12 inhibitors | 56.3 | 56.6 | 50.0 | 21.2 |
| OACs | 31.2 | 34.3 | 31.5 | 30.9 |
| Insulin | 2.5 | 14.1 | 13.3 | 10.9 |
| OADs | 21.1 | 24.7 | 23.0 | 23.6 |
Abbreviations: ACE, angiotensin-converting enzyme; ARB, angiotensin-receptor blocker; OAK, oral anticoagulation; OAD, oral antidiabetics; MRA, mineralocorticoid receptor antagonist.
Figure 5.
Heart failure medication during study course.
In the 200 participating patients, HF medication was changed in 79 patients by the 3-month -follow-up, which corresponds to 39.5%. Up to the 12-month follow-up, medication was changed in a total of 97 patients, which corresponds to 48.5%. In the end, a physician had prescribed all changes in HF medication. In 19 cases a patient requested such a change, but this was discussed with the physician who continued to treat the patient. None of the patients reported that they had completely independently changed their therapy regimen.
Adverse Events
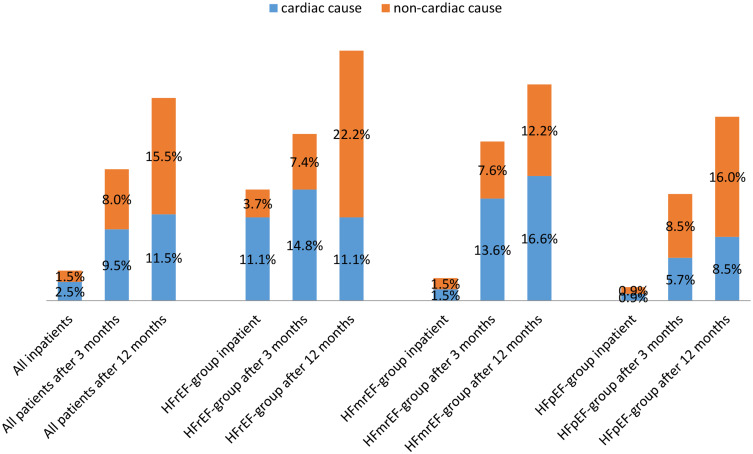
Adverse events are outlined in Figure 6, differentiated according to HF type. During the inpatient stay, a total of eight patients needed to be transferred owing to an acute event, which corresponds to 4%. Just under two-thirds of these were cardiac events and one-third non-cardiac. Among these patients, thoracic pain prompted the transfer in two cases. Due to thoracic pain, one woman needed to be transferred to another hospital, an acute myocardial infarction could be excluded; a tachycardic event presented in a patient with a known absolute arrhythmia; and, after an acute myocardial infarction, emergency transfer to the heart center in Leipzig was required for yet another patient. One man developed dyspnea, thoracic pain, and cyanosis. Shortly after the transfer, he died in the emergency room before receiving further diagnostic tests and therapy. Two other patients suffered from nosebleed, which could only be stopped in a special clinic.
Figure 6.
Hospitalizations.
After evaluating the twelve-month follow-up questionnaires, 64 patients had been rehospitalized: 33 cases were of cardiac and 31 cases of noncardiac origin. In six cases, cardiac hospitalizations specifically involved interventions due to the coronary heart disease; in 14 cases myocardial decompensation occurred; and in 10 patients, cardiac arrhythmia requiring intervention had developed. Three patients suffered a fatal myocardial infarction. When considering the outcome “death”; however, no patient died during the inpatient stay at the Harz Clinic in Bad Suderode. One patient died shortly after being transferred to another hospital with symptomatic dyspnea, thoracic pain, and cyanosis. Seven further patients died within a year. A total of five non-fatal myocardial infarctions occurred. The drop-out rate was 19 patients.
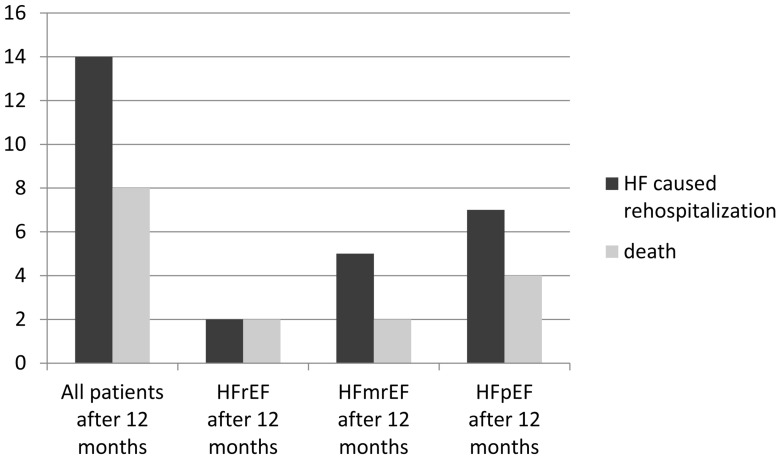
Figure 7 outlines rehospitalizations owing HF and death of any cause during the course of the study according to HF type.
Figure 7.
Heart failure caused rehospitalization and death during study course.
Discussion
HF is a life-threatening disease. After 1 year, 17% of inpatient patients die and 44% are rehospitalized because of HF.8
In the present study, mortality and numbers of patients rehospitalized because of HF was surprisingly low at 4% and 7%, respectively. Since all patients participated in cardiac rehabilitation (CR) as the main inclusion criterion of the study, we hypothesize that patient outcome during the 12-month follow-up is influenced by participating in CR.
Previous studies on the effectiveness of CR are very heterogeneous in terms of the number of patients enrolled, the type of randomization, the duration of the follow-up, and the type and duration of the intervention. A recent Cochrane analysis showed that CR is effective with regards to mortality, cardiac events, exercise capacity, and modification of risk factors.12
As part of the multimodal rehabilitation, which is typically performed in Germany, exercise has been shown to improve outcome in HF patients.
In 2004, Whellan et al found that physical training can significantly reduce morbidity and probably also mortality in patients with chronic HF.13
Finally, since 2009, data have been available from the multicenter, prospective, randomized, and controlled HF-ACTION study of 2331 patients with an EF <35% and receiving the best possible therapy and aggregate care. Initially, no significant decrease in mortality and hospitalization rates were observed – after an observation period lasting 30 months. In this study, the patients trained for the first 3 months according to the trainer’s instructions followed by continuing the training at home. The primary endpoint only showed a significant improvement after the data had been adjusted. A connection between the increase in the amount of training and the reduction in mortality and hospitalization was found. In summary, this study was able to show that physical training for HF patients poses no risk and also positively affects and improves physical, psychological, and social restrictions, symptoms, and quality of life.14
In general, seriously ill patients can also participate in moderate endurance training, which can also help improve their health and well-being.15 One major criticism of the available studies is that, often, no older patients were included, such that the informative value of these studies must be regarded as limited, especially for the group of patients over 65 years of age. The present study considered patients with an average age of 65.
The ESC guideline for the diagnosis and treatment of acute and chronic HF, which was published in 2016 and was developed with the approval of the Heart Failure Association (HFA) of the ESC, has given a class IA recommendation for physical training – for chronic HF. Nevertheless, prevention and rehabilitation of HF hardly play a role according to the current ESC guideline.16
No reliable data are available regarding the therapy and the intensity of physical training at HFmrEF. The present study explicitly compared the endpoints of the HFmrEF group with those of the HFrEF and HFpEF. Accordingly, it became apparent that the HFmrEF group is a separate disease entity with its own characteristics.
Another important effect of CR is improved compliance to drug therapy. During the current study, the use of beta-blockers was stable. However, the use of ARB, Ivabradine, and sacubitril/valsartan rose. Other recent trials in patients with HF show that as disease progresses, compliance with medication decreases.17
Multimodal rehabilitation also includes psychosocial care, which is effective in patients with HF (awareness, knowledge and social support).
In the current study, HADS-D and SF-12 showed no significant development of anxiety, depression, and quality of life in the patients.
Limitations
The study is limited by its monocentric design, which has the potential for under-reporting (e.g., acute myocardial decompensation, and emergency admission to the hospital). Due to missing or some old references, it is unfortunately not really possible to make comparisons with studies by other authors.
Conclusion
Although limited by its monocentric design, this prospective study showed effects both for symptoms (improvement in NYHA classification) and prognosis (overall mortality) after rehabilitation. These data underline the need for rehabilitation in patients diagnosed with HF after an acute event and hospital stay or who present with chronic deterioration.
In the future, it will be necessary to encourage more and possibly also interventional studies that can provide further data concerning inpatient cardiac rehabilitation.
Acknowledgment
This study was supported by an unrestricted grant from Novartis®, Germany.
Disclosure
The authors report no conflict of interest in this work.
References
- 1.Stork S, Handrock R, Jacob J, et al. Epidemiology of heart failure in Germany: a retrospective database study. Clin Res Cardiol. 2017;106(11):913–922. doi: 10.1007/s00392-017-1137-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Christ M, Stork S, Dorr M, et al.; Heart failure epidemiology 2000-2013: insights from the German federal health monitoring system. Eur J Heart Fail. 2016;18(8):1009–1018. doi: 10.1002/ejhf.567 [DOI] [PubMed] [Google Scholar]
- 3.Cooperation between the German Medical Association and the National Association of Statutory Health Insurance Physicians at the Medical Center for Qualification in Medicine (ÄZQ). Berlin, Germany. [Google Scholar]
- 4.Freud T, Gerste B, Jencke E, Quality of post-inpatient drug supply for patients with heart failure. Hospital report 2016. (Stuttgart), 2016; 229–249
- 5.Murad K, Golf DCJ, Morgan TM, et al. Burden of comorbidities and functional and cognitive impairments in elderly patients at the initial diagnosis of heart failure and their impact on total mortality. The cardiovascular health study. JACC Heart Fail. 2015;3(7):542–550. doi: 10.1016/j.jchf.2015.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rademacher W, Glatz J, Laugner P, et al. Psychocardiologic rehabilitation-interdisciplinary treatment as a pilot project. J Cardiol. 2019;13:40–48. [Google Scholar]
- 7.Medline-research and clinical evidence research from 23rd of November. 2020.
- 8.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure of the European society of cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128 [DOI] [PubMed] [Google Scholar]
- 9.Petermann F. Hospital Anxiety and Depression Scale, German Version (HADS-D). J Psychiatry Psychol Psychother. 2011;59(3):251–253. [Google Scholar]
- 10.Wirtz MA, Morfeld M, Glaesmer H, Braehler E. Confirmatory test of the scale structure of the SF-12 version 2.0 in a sample representable of the German population. Diagnostica. 2018;64(2):84–96. doi: 10.1026/0012-1924/a000194 [DOI] [Google Scholar]
- 11.Hunt SA, Abraham WT, Chin MH, et al. Focused update incorporated into ACC/AHA 2005 guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2009;119:e391–e479. [DOI] [PubMed] [Google Scholar]
- 12.Schwaab B, Albus C, Waller C, Fritsche K, Gunold H, Haas M. Cochrane analysis in cardiac rehabilitation. Int J Cardiol 2018;97(02):117–126. [Google Scholar]
- 13.Whellan DJ, Slow LK, Best BK, Kraus WE, Califf RM, O Connor CM. Cardiac rehabilitation and survival in patients with left ventricular systolic dysfunction. Am Heart J. 2004;142:160–166. doi: 10.1067/mhj.2001.115785 [DOI] [PubMed] [Google Scholar]
- 14.O Connor CM, Whellan DJ, Lee KJ, et al.; HF-ACTION Investigations. Efficacy and safety of exercise training in patients with chronic heart failure. HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1439–1450. doi: 10.1001/jama.2009.454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tiller D, Russ M, Greiser KH, et al. Prevalence of symptomatic heart failure with reduced and with normal ejection fraction in an elderly general population-the CARLA study. PLoS One. 2013;8(3):e59225. doi: 10.1371/journal.pone.0059225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reibis RK, Schlitt A, Glatz J, et al. Rehabilitation in heart failure. Rehabilitation (Stuttg). 2016;55(2):115–27; quiz 128–9. doi: 10.1055/s-0042-103302 [DOI] [PubMed] [Google Scholar]
- 17.Holstiege J, Akmatov MK, Steffen A, Bätzing J, Prevalence of heart failure-nationwide trends, regional variations and frequent comorbidities. Central institute for stationary health care in Germany (Ci) supply atlas report- no. 18/19, Berlin. 2018. doi: 10.20364/UA-18.09 [DOI]