Abstract
Background:
Cannabis and other drug use is associated with adverse health events, but little is known about the association of routine clinical screening for cannabis or other drug use and acute care utilization. This study evaluated whether self-reported frequency of cannabis or other drug use was associated with subsequent acute care.
Method:
This retrospective cohort study used EHR and claims data from 8 sites in Washington State that implemented annual substance use screening. Eligible adult primary care patients (N=47,447) completed screens for cannabis (N=45,647) and/or other drug use, including illegal drug use and prescription medication misuse, (N=45,255) from 3/3/15–10/1/2016. Separate single-item screens assessed frequency of past-year cannabis and other drug use: never, less than monthly, monthly, weekly, daily/almost daily. An indicator of acute care utilization measured any urgent care, emergency department visits, or hospitalizations ≤19 months after screening. Adjusted Cox proportional hazards models estimated risk of acute care.
Results:
Patients were predominantly non-Hispanic White. Those reporting cannabis use less than monthly (Hazard Ratio [HR]=1.12, 95% CI=1.03–1.21) or daily (HR=1.24; 1.10–1.39) had greater risk of acute care during follow-up than those reporting no use. Patients reporting other drug use less than monthly (HR=1.34; 1.13–1.59), weekly (HR=2.21; 1.46–3.35), or daily (HR=2.53; 1.86–3.45) had greater risk of acute care than those reporting no other drug use.
Conclusion:
Population-based screening for cannabis and other drug use in primary care may have utility for understanding risk of subsequent acute care. It is unclear whether findings will generalize to U.S. states with broader racial/ethnic diversity.
Keywords: marijuana, substance use, primary care, screening, acute care, emergency visits
1. INTRODUCTION
More than 30.5 million Americans use cannabis or other illegal drugs, or 11.2% of the U.S. population (Substance Abuse and Mental Health Services Administration, 2019). The number of people using cannabis and other drugs is increasing, driven primarily by cannabis use (Substance Abuse and Mental Health Services Administration, 2019) and its increasing availability in legal markets (Goodman et al., 2020). The prevalence of past-year cannabis or other drug use among primary care patients ranges from 4–21% and 2–26%, respectively (Lapham et al., 2017; McNeely et al., 2015a; McNeely et al., 2015b; McNeely et al., 2016; Pilowsky and Wu, 2012; Tiet et al., 2015). Together, cannabis and other drugs account for more than 5% of disability-adjusted life years through risk of adverse health outcomes, including injuries, mental health and substance use disorders (Murray and Lopez, 2013; U. S. Burden of Disease Collaborators et al., 2018). Studies suggest a strong association between cannabis or other drug use disorder and acute care, which includes urgent care, emergency department visits and hospitalizations (Bahorik et al., 2018; Campbell et al., 2017; Doupe et al., 2012; Gubatan et al., 2016; Wu et al., 2018; Zatzick et al., 2017).
While results from substance use screenings in primary care are intended to identify patients in need of further assessment and treatment, they may also be useful in identifying patients at risk for poor health outcomes and acute care utilization (Bradley et al., 2016; Chavez et al., 2016; Pilowsky and Wu, 2012; Rubinsky et al., 2019; Williams et al., 2012). Several brief screening instruments are available to detect cannabis and other drug use in primary care, with sensitivity and specificity for detecting use of “any drug” ranging from 0.71–0.94 and 0.87–0.97, respectively (Krist et al., 2020). The U.S. Preventive Services Task Force (USPSTF) now recommends screening for unhealthy drug use in primary care, and therefore adoption and implementation of screening may increase (Krist et al., 2020). Health systems may wish to adopt brief and valid screens, and they may be interested in knowing whether screens can identify patients at risk for adverse outcomes such as acute care (Krist et al., 2020; Pilowsky and Wu, 2012; Tai and Volkow, 2013). Although a previous secondary analysis of data from a drug use intervention trial found that cannabis use frequency among primary care patients was not associated with emergency department visits or hospitalizations (Fuster et al., 2014; Saitz et al., 2014), all patients in that study recently used other drugs. Information about the association between results from cannabis or other drug use screening and acute care utilization in primary care samples could potentially inform understanding of associated health risks.
The current study sought to examine the association between frequency of cannabis or other drug use and subsequent utilization of acute care, among patients visiting primary care clinics. Specifically, this study hypothesized that frequency of past-year cannabis and other drug use self-reported by primary care patients on separate single-item screens would be associated with increased risk of subsequent acute care. Because the association between substance use and health varies by other risk factors (Agrawal and Lynskey, 2007; Bradley et al., 2004; Cherpitel et al., 2012; Rubinsky et al., 2013; Volkow et al., 2014), this study explored whether sex, age, and having a substance use disorder diagnosis modified the association between screening scores and acute care utilization.
2. METHODS
2.1. Setting, data source, and sample
Data were from Kaiser Permanente Washington (KPWA), an integrated health system providing health insurance and health care in a state with legal medical cannabis use since 1998 and adult (≥21 years) recreational use since 2012. Data were derived from two sources: EHR data on substance use screening and other health services received inside the health care delivery system; and insurance claims data for health care services received elsewhere that were reimbursed by insurance.
Implementation of routine annual screening for past-year cannabis and other drug use began in March 2015 and rolled out across clinics over a three-year period as part of a larger effort to integrate behavioral health into primary care (Bobb et al., 2017; Glass et al., 2018; Richards et al., 2019). Patients eligible for the current study had a primary care visit between 3/3/2015 and 10/31/2016 at one of the first 8 clinics that implemented screening, were insured by KPWA, were ≥18 years old at the time of the visit, and were screened in primary care for cannabis and/or other drug use (75.5% of primary care patients). If patients were screened multiple times, data from the first screen was used. The single-item questions for cannabis and other drug use were administered on the same screening form, and approximately 95.2% of patients who completed one question completed both questions. Separate screening questions for cannabis and other drug use reflect the legal landscape of cannabis in Washington State. Because we used insurance claims data from the year prior to patients’ substance use screening to construct the study covariates, we excluded patients with ≥3-month gap in insurance coverage during the year prior to the visit (Strom and Bjornson, 2006) to help ensure that these variables could be adequately measured; 20% of otherwise eligible patients were excluded. Follow-up data were observed through 10/31/2016. The KPWA Institutional Review Board approved this study.
2.2. Measures
2.2.1. Primary Predictors
Primary care patients completed a 7-item self-report paper-based behavioral health screen that included questions about substance use. An electronic reminder prompted primary care staff to conduct annual screening and enter screening results into the EHR.
Frequency of past-year cannabis use was assessed by scaled-response to the item, “How often in the past year have you used marijuana?” (Lapham et al., 2017). Marijuana use was undefined for the patient and could include recreational and medical use. Frequency of past-year other drug use which came after the cannabis question on the 7-item screen, was assessed with a validated single-item screening question adapted to a scaled response: “How often in the past year have you used an illegal drug or used a prescription medication for non-medical reasons?”(Smith et al., 2010) For both items, response options were never, less than monthly, monthly, weekly, and daily/almost daily from the third item of the Alcohol Use Disorder Identification Test (Babor et al., 2001). These single-item screens are very brief, a key consideration for routine use in primary care (Krist et al., 2020; National Council for Behavioral Health, 2018).
2.2.2. Outcome
Acute care was defined as any urgent care, emergency department visit, and/or hospital admission from screen to study-end date. The outcome was assessed as the number of days between screen date and first date of acute care.
2.2.3. Covariates
Demographic characteristics included sex (male/female), age (18–29, 30–49, 50–64, ≥65 years), race (American Indian/Alaskan Native, Asian, Black, Hawaiian or Pacific Islander, multiracial, White, other, unknown), and ethnicity (Hispanic or Latino, not Hispanic or Latino, unknown) at the time of screening.
International Classification of Diseases (ICD) 9 and 10 codes were used to create indicators of clinical characteristics, including past-year mental health (major depression, anxiety, serious mental illness) and substance use disorder (SUD) diagnoses (tobacco, alcohol, cannabis, opioid, and other drug use disorders). SUD diagnoses are often under-recognized in clinical settings (Bobb et al., 2020); patients with a documented SUD diagnosis may be unique from patients who use substances but do not have a diagnosis, and their acute care utilization may vary. Morbidity level was measured with a case-mix system that defines Resource Utilization Band (RUB) scores validated for forecasting health care utilization in primary care patients (Fredriksson et al., 2015; Lind et al., 2013; Starfield and Kinder, 2011; Zielinski et al., 2009). RUB scores range 0–5 with higher scores indicating higher morbidity.
2.3. Analyses
Demographic and clinical characteristics were described overall and by frequency of past-year cannabis and other drug use.
In time-to-event analyses, each of the two primary predictors were examined in separate models as a categorical variable, with no past-year use as the reference. Follow-up time was censored at date of disenrollment from insurance, death, or end of the study period. Cox proportional hazards models (Cox, 1972) estimated relative hazards of acute care associated with past-year frequency of use. We assessed for overall variation in the hazard of acute care across frequency of use categories using a joint Wald’s test before examining category-level associations. Violations to the proportional hazards assumption were assessed graphically and by interacting the natural log of time to acute care with the primary predictor to examine whether the association changed over time (Cleves et al., 2002). We found no evidence for violation of the proportional hazard’s assumption.
We fit 3 different models: unadjusted, adjusted for demographic characteristics, and adjusted for demographic and clinical characteristics. Adjusted models allowed for a non-linear association between age and acute care via restricted cubic splines (Harrell, 2001). In all models, the baseline hazard was stratified by clinic, and clustering of patients by providers was accounted for using robust variance estimates (Lin and Wei, 1989; Williams, 2000). A priori, we selected the model adjusted for demographic factors to be primary, whereas the model adjusted for clinical characteristics was specified to examine whether frequency of use is associated with risk of acute care or whether frequency of use co-varies with other factors known to be associated with acute care utilization. We did not control for other drug use in cannabis analyses or cannabis use in other drug use analyses because not all health systems will adopt both cannabis and other drug screening, and we wanted to provide estimates of acute care risk that do not depend on knowing the frequency at which patients use other, potentially unassessed, substances. Effect modification by sex (Agrawal and Lynskey, 2007; Rubinsky et al., 2013), age (Cherpitel et al., 2012; Rubinsky et al., 2013; Volkow et al., 2014), or past-year SUD (Bradley et al., 2004; Volkow et al., 2014) was assessed using a Wald’s test of the interaction term in models adjusted for demographic characteristics. Hazard ratio estimates were reported within subgroups. Analyses were conducted using Stata 15 (StataCorp, 2017).
3. RESULTS
3.1. Demographic and clinical characteristics
A total of 47,447 primary care patients were eligible for this study. Of those, 45,647 completed the cannabis screen and 45,255 completed the other drug use screen (95% of all participants completed both). Approximately 60% of patients were female, 46% were ≥65 years old, 5% had Hispanic ethnicity, and 81% were White (Table 1). For both cannabis and other drug use, patients reporting no use were more likely to be female and tended to be older. There tended to be a higher prevalence of any SUD and mental health diagnoses for patients reporting daily/almost daily use compared to those reporting less frequent use.
Table 1.
Characteristics of adult primary care patients who completed a screen about past-year cannabis or other drug use, by frequency of use
| Screened for cannabis use |
Screened for other drug use |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | By frequency of past-year use |
p | Overall | By frequency of past-year use |
p | |||||||||
| (N=45,647) | Never (N=39,827) | Less than Monthly (N=2,902) | Monthly (N=886) | Weekly (N=901) | Daily or almost daily (N=1,131) | (N=45,255) | Never (N=44,726) | Less than Monthly (N=381) | Monthly (N=49) | Weekly (N=35) | Daily or almost daily (N=69) | |||
| Column % | Column % | |||||||||||||
| Female | 59.6 | 60.9 | 55.8 | 48.4 | 42.4 | 46.6 | <0.001 | 59.6 | 59.7 | 50.9 | 36.7 | 48.6 | 43.8 | <0.001 |
| Age | ||||||||||||||
| 18–29 years | 7.6 | 5.6 | 19.5 | 21.7 | 22.5 | 24.5 | <0.001 | 7.5 | 7.2 | 36.0 | 34.7 | 37.1 | 50.0 | <0.001 |
| 30–49 years | 19.4 | 18.4 | 27.3 | 26.4 | 19.3 | 26.9 | 19.4 | 19.3 | 23.9 | 16.3 | 14.3 | 10.9 | ||
| 50–64 years | 27.2 | 26.9 | 29.4 | 30.5 | 32.0 | 27.7 | 27.3 | 27.3 | 18.6 | 18.4 | 14.3 | 20.3 | ||
| ≥65 years | 45.9 | 49.2 | 23.8 | 21.4 | 26.2 | 21.0 | 45.9 | 46.1 | 21.5 | 30.6 | 34.3 | 18.8 | ||
| Race | ||||||||||||||
| American Indian or Alaska Native | 0.7 | 0.7 | 0.9 | 0.5 | 1.2 | 0.8 | <0.001† | 0.7 | 0.7 | 1.1 | 0.0 | 0.0 | 1.6 | 0.004† |
| Asian | 7.6 | 8.4 | 3.1 | 2.0 | 1.7 | 1.7 | 7.6 | 7.7 | 5.0 | 0.0 | 0.0 | 4.7 | ||
| Black | 2.7 | 2.7 | 3.4 | 3.4 | 2.4 | 3.7 | 2.7 | 2.7 | 5.0 | 0.0 | 0.0 | 0.0 | ||
| Hawaiian or Pacific Islander | 0.6 | 0.6 | 0.5 | 0.7 | 0.6 | 0.7 | 0.6 | 0.6 | 0.5 | 0.0 | 2.9 | 1.6 | ||
| Multiracial | 2.6 | 2.3 | 4.0 | 4.1 | 5.3 | 4.6 | 2.6 | 2.6 | 4.5 | 8.2 | 5.7 | 4.7 | ||
| Other | 2.3 | 2.4 | 2.0 | 2.3 | 1.4 | 2.2 | 2.3 | 2.3 | 3.4 | 0.0 | 0.0 | 1.6 | ||
| White | 80.9 | 80.5 | 83.6 | 84.0 | 84.6 | 82.7 | 80.9 | 80.9 | 76.9 | 89.8 | 91.4 | 85.9 | ||
| Unknown | 2.6 | 2.5 | 2.5 | 3.2 | 2.8 | 3.6 | 2.6 | 2.6 | 3.7 | 2.0 | 0.0 | 0.0 | ||
| Hispanic or Latino Ethnicity | 4.7 | 4.7 | 4.9 | 4.4 | 3.8 | 4.8 | 0.432 | 4.7 | 4.7 | 5.5 | 4.1 | 0.0 | 1.6 | 0.384† |
| Diagnoses in prior year | ||||||||||||||
| Tobacco use disorder | 3.6 | 3.2 | 4.8 | 6.4 | 7.7 | 8.0 | <0.001 | 3.6 | 3.5 | 5.0 | 4.1 | 17.1 | 14.1 | <0.001† |
| Alcohol use disorder | 1.6 | 1.4 | 2.2 | 3.1 | 3.6 | 4.2 | <0.001 | 1.6 | 1.5 | 3.2 | 2.0 | 5.7 | 9.4 | <0.001† |
| Cannabis use disorder | 0.4 | 0.3 | 0.7 | 0.5 | 0.8 | 1.5 | <0.001 | 0.4 | 0.3 | 0.8 | 8.2 | 8.6 | 25.0 | <0.001† |
| Opioid use disorder | 0.5 | 0.4 | 0.9 | 0.8 | 1.0 | 1.7 | <0.001 | 0.5 | 0.4 | 1.1 | 8.2 | 8.6 | 25.0 | <0.001† |
| Other drug use disorder | 0.1 | 0.1 | 0.1 | 0.0 | 0.3 | 0.4 | 0.013† | 0.1 | 0.1 | 1.1 | 2.0 | 5.7 | 1.6 | <0.001†` |
| Major depression | 15.2 | 14.5 | 19.0 | 20.9 | 18.9 | 23.6 | <0.001 | 15.2 | 15.1 | 18.1 | 26.5 | 37.1 | 28.1 | <0.001 |
| Anxiety | 10.2 | 9.5 | 14.0 | 16.6 | 15.8 | 17.2 | <0.001 | 10.2 | 10.2 | 14.4 | 16.3 | 14.3 | 17.2 | 0.009 |
| Serious mental illness | 0.1 | 0.1 | 0.1 | 0.2 | 0.0 | 0.2 | 0.135† | 0.1 | 0.01 | 0.5 | 0.0 | 0.0 | 0.0 | 0.118† |
| Resource Utilization Band (5 categories) | ||||||||||||||
| ≤ 1 | 4.1 | 3.8 | 7.0 | 5.9 | 5.6 | 4.8 | <0.001 | 4.1 | 4.1 | 6.3 | 6.5 | 0.0 | 3.3 | <0.001† |
| 2 | 10.6 | 10.2 | 14.6 | 13.6 | 13.3 | 11.2 | 10.6 | 10.6 | 15.8 | 10.9 | 2.9 | 4.9 | ||
| 3 | 56.7 | 56.4 | 58.2 | 60.6 | 57.9 | 59.4 | 56.7 | 56.7 | 59.0 | 54.4 | 64.7 | 52.5 | ||
| 4 | 19.0 | 19.6 | 14.4 | 14.7 | 15.8 | 16.9 | 19.1 | 19.1 | 12.8 | 26.1 | 14.7 | 32.8 | ||
| 5 | 9.5 | 10.0 | 5.9 | 5.3 | 7.4 | 7.7 | 9.5 | 9.5 | 6.3 | 2.2 | 17.7 | 6.6 | ||
Fisher’s exact used to calculate p-values due to small numbers; all other p-values are calculated with chi-squared test of independence
Censoring occurred for 1,354 patients who disenrolled from insurance and 34 who died. At 6 and 12 months, respectively, 18,739 and 7,314 patients contributed follow-up time. Days of follow-up ranged up to 609 days (median=144), and 12,891 (27% of total sample) patients experienced an acute care event during the study period.
3.2. Cannabis use frequency and subsequent acute care utilization
In the unadjusted Cox proportional hazard model, there was no evidence of an association between frequency of past-year cannabis use and subsequent acute care utilization (Table 2). In the primary model adjusted for demographic characteristics, frequency of cannabis use was significantly associated with subsequent acute care utilization (p=0.002). Patients reporting less than monthly (Hazard Ratio [HR]=1.12, 95% CI=1.03–1.21, p=0.006) or daily/almost daily use (HR=1.24, 95% CI=1.10–1.39, p<0.001) had greater hazard of acute care than those reporting no use. There was no evidence of greater hazard of acute care for patients reporting monthly or weekly use. In the model adjusted for demographic and clinical characteristics, there was no evidence of an association between frequency of cannabis use and acute care utilization per the joint Wald’s test despite category-level associations.
Table 2.
Estimated relative hazards of acute care utilization according to patient-reported frequency of past-year cannabis and other drug use
| UNADJUSTED1 | ADJUSTED FOR DEMOGRAPHIC CHARACTERISTICS (Primary model) 2 | ADJUSTED FOR DEMOGRAPHIC AND CLINIICAL CHARACTERISTICS3 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | (95% CI) | p | Joint p | HR | (95% CI) | p | Joint p | HR | (95% CI) | p | Joint p | |
| Frequency of Past-Year Cannabis Use | ||||||||||||
| Never | REF | REF | REF | |||||||||
| Less than Monthly | 1.00 | (0.93–1.08) | 0.950 | 0.197 | 1.12 | (1.03, 1.21) | 0.006* | 0.002* | 1.09 | (1.01, 1.18) | 0.024* | 0.102 |
| Monthly | 0.89 | (0.78–1.01) | 0.076 | 1.01 | (0.88, 1.15) | 0.916 | 0.94 | (0.82, 1.09) | 0.410 | |||
| Weekly | 0.99 | (0.86–1.14) | 0.895 | 1.12 | (0.98, 1.29) | 0.106 | 1.08 | (0.94, 1.24) | 0.277 | |||
| Daily/almost daily | 1.08 | (0.96–1.22) | 0.181 | 1.24 | (1.10, 1.39) | 0.001* | 1.11 | (0.99, 1.25) | 0.082 | |||
| Frequency of Past-Year Other Drug Use | ||||||||||||
| Never | REF | REF | REF | |||||||||
| Less than Monthly | 1.23 | (1.03, 1.46) | 0.019* | < 0.001* | 1.34 | (1.13, 1.59) | 0.001* | < 0.001* | 1.29 | (1.09, 1.54) | 0.004* | < 0.001* |
| Monthly | 0.76 | (0.41, 1.42) | 0.388 | 0.85 | (0.45, 1.60) | 0.606 | 0.71 | (0.34, 1.47) | 0.355 | |||
| Weekly | 2.13 | (1.41, 3.22) | <0.001* | 2.21 | (1.46, 3.35) | <0.001* | 1.57 | (0.96, 2.58) | 0.071 | |||
| Daily/almost daily | 2.37 | (1.76, 3.21) | <0.001* | 2.53 | (1.86, 3.45) | <0.001* | 1.82 | (1.29, 2.57) | 0.001* | |||
Abbreviations: HR, hazard ratio; CI, confidence interval; REF, reference category
Joint P considers overall variation across primary predictor categories using a Wald’s test with 4 degrees of freedom.
Indicates estimate is statistically significant at alpha level of 0.05
Unadjusted model stratified by site
Adjusted for demographic characteristics of gender, age, race/ethnicity and stratified by site
Adjusted for demographic characteristics and clinical characteristics including mental health diagnoses (depression, anxiety, serious mental illness) and substance use disorders (alcohol, tobacco, cannabis, opioid, and other drug use disorders), and resource utilization band score, and stratified by site
3.3. Other drug use frequency and acute care utilization
In all models, frequency of other drug use was significantly associated with acute care utilization (joint p’s<0.001; Table 2). Specifically, in the unadjusted model, patients reporting less than monthly (HR=1.23, 95% CI=1.03–1.46, p=0.019), weekly (HR=2.13, 95% CI: 1.41–3.22, p<0.001), and daily/almost daily drug use (HR=2.37, 95% CI: 1.76–3.21, p<0.001) had greater hazard of acute care compared to patients reporting no use. In the primary model adjusted for demographic characteristics, patients reporting drug use less than monthly (HR=1.34, 95% CI: 1.13–1.59, p=0.001), weekly (HR=2.21, 95% CI: 1.46–3.35, p<0.001) and daily/almost daily (HR=2.53, 95% CI: 1.86–3.45, p<0.001) had a greater hazard of acute care compared to patients reporting no use. In the model adjusted for demographic and clinical characteristics, only patients reporting less than monthly (HR= 1.29, 95% CI: 1.09–1.54, p=0.004) and daily/almost daily drug use (HR=1.82, 95% CI: 1.29–2.57, p=0.001) had a greater hazard of acute care compared to patients reporting no use.
3.4. Effect modification by sex, age or prior substance use disorders diagnosis
3.4.1. Cannabis use frequency and acute care utilization.
There was a significant interaction between frequency of cannabis use and sex (p=0.003). In analyses of sex-specific subgroups, females reporting less than monthly (HR=1.16, 95% CI=1.06–1.27, p=0.001), weekly (HR=1.28, 95% CI=1.07–1.54, p=0.008), and daily/almost daily cannabis use (HR=1.39, 95% CI=1.19–1.63, p<0.001) had a greater hazard of acute care compared to females reporting no past-year cannabis use. In contrast, there was no evidence that hazard of acute care varied for men across frequency of cannabis use (Table S1, Figure 1).
Figure 1. Estimated relative hazards of acute care utilization according to patient-reported frequency of past-year cannabis and other drug use, overall and by subgroup.
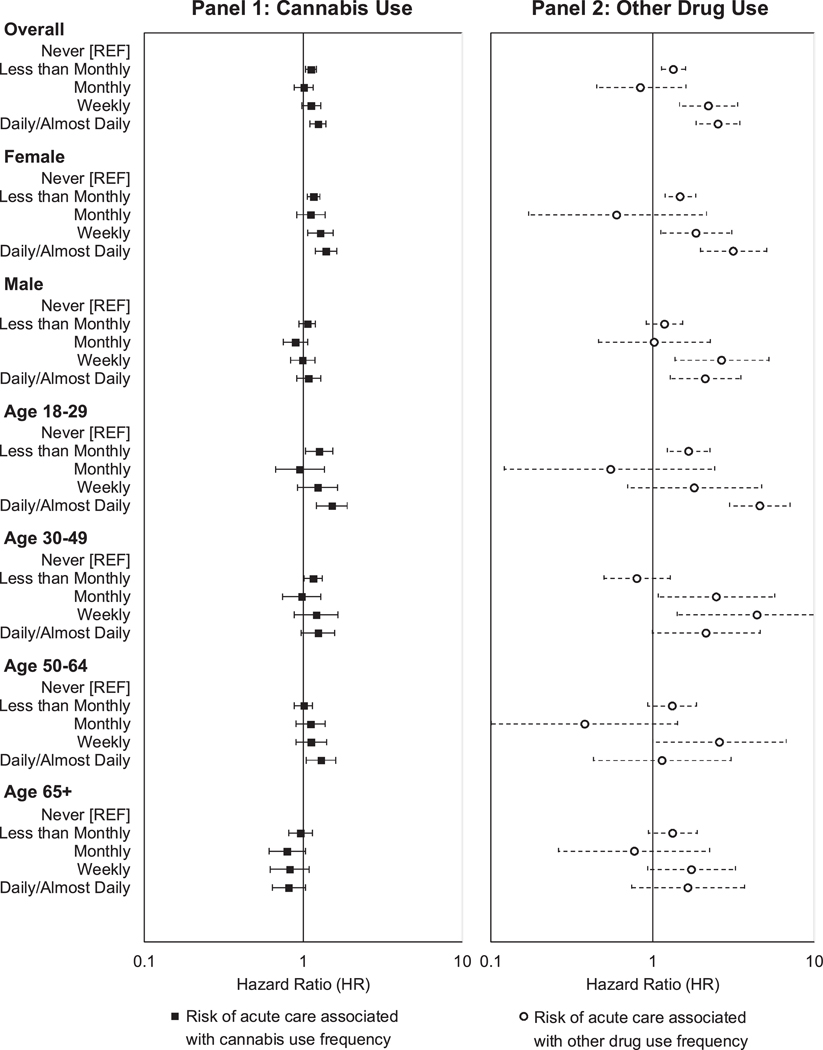
Overall and stratified hazard ratios for frequency of past-year cannabis use (panel 1) and other drug use (panel 2) estimated using Cox proportional hazards models with robust standard errors, adjusted for demographic characteristics and stratified by clinic. Estimates are relative to no past-year use and are presented on the log-scale with 95% confidence intervals.
There was a significant interaction between frequency of cannabis use and age (p=0.006). In age-specific subgroups, younger adults age 18–29 reporting less than monthly (HR=1.26, 95% CI=1.03–1.53, p=0.024) and daily/almost daily cannabis use (HR=1.52, 95% CI=1.21–1.90, p<0.001) had a greater hazard of acute care compared to those of the same age reporting no use. For patients age 30–49, only those reporting less than monthly cannabis use (HR=1.15, 95% CI=1.01–1.32, p=0.039) had a greater hazard of acute care compared to those of the same age reporting no use. For patients age 50–64, only those reporting daily/almost daily use (HR=1.29, 95% CI=1.04–1.60, p=0.022) had a greater hazard of acute care compared to those of the same age reporting no use. For patients age 65 and over, there was no evidence that those reporting any cannabis use had a greater hazard of acute care compared to those of the same age group reporting no cannabis use (Table S1, Figure 1).
There was no evidence of a significant interaction between frequency of cannabis use and documentation of a past-year SUD.
3.4.2. Other drug use frequency and acute care utilization.
There was no evidence of a significant interaction between frequency of other drug use and sex, or documentation of a past-year SUD.
There was a significant interaction between frequency of other drug use and age group (p=0.002). In analyses of age-specific subgroups, younger adults age 18–29 reporting less than monthly (HR=1.67, 95% CI=1.23–2.26, p=0.001) or daily/almost daily drug use (HR=4.59, 95% CI=2.98–7.07, p<0.001) had a greater hazard of acute care compared to those of the same age reporting no use. For patients age 30–49, those reporting monthly (HR=2.47, 95% CI: 1.08–5.67, p=0.032) or weekly drug use (HR=4.42, 95% CI=1.41–13.85, p=0.011) had a greater hazard of acute care compared to those of the same age reporting no use. For patients age 50–64 and patients 65 and over, there was no evidence that the hazard of acute care varied by frequency of other drug use (Table S1, Figure 1).
4. DISCUSSION
In a health system that conducts annual population-based screening for substance use in primary care, patient self-report of frequency of past-year cannabis and other drug use predicted risk of subsequent acute care. Specifically, patients reporting less than monthly and daily/almost daily cannabis use had higher risk of using acute care services than patients reporting no cannabis use. Patients reporting less than monthly, weekly, and daily/almost daily use of other drugs had a higher risk of using acute care services than patients reporting no use. Moreover, sex and age group modified several associations. To our knowledge, this is the first study to evaluate whether substance use screens administered as part of routine primary care predicted risk of subsequent acute care.
While frequency of cannabis use was associated with subsequent acute care, the pattern of associations did not provide evidence for a linear dose-response relationship. Patients with the most frequent cannabis use (daily/almost daily) or rare use (less than monthly) had an elevated risk of acute care, but there was no evidence of increased risk for patients reporting monthly or weekly use. It was not surprising that daily/almost daily use increased risk, as daily use is associated with increased risk of cannabis use disorders and prior studies have found an association between cannabis use disorder and acute care (Campbell et al., 2017; Gubatan et al., 2016). However, the lack of a dose-response relationship could suggest that another factor may affect this association. It could also be that a unique mechanism contributes to risk of acute care among patients with rare use. For instance, injuries or illnesses requiring acute care could potentially be more common among people who use infrequently because they may have less experience with highly potent methods of cannabis administration and products (Loflin and Earleywine, 2014), be more susceptible to psychoactive effects (Kim et al., 2016; Ramaekers et al., 2009), or experience unanticipated acute medical effects (Hall and Degenhardt, 2009; Vitale and van de Mheen, 2006; Volkow et al., 2014). Although beyond the scope of this study, future studies may wish to explore the admission diagnoses recorded in acute care settings for patients with cannabis use. A laboratory-based study found that cannabis use was associated with adverse effects for people who used cannabis infrequently (Spindle et al., 2018). If future studies find similar patterns, it may be important to educate patients who rarely use cannabis about potential harms. These findings run contrary to a previous study that found no association between cannabis use and acute care. However, the prior study was cross sectional, and participants were eligible by virtue of a positive screen for drug use and enrolled in a randomized controlled trial (Fuster et al., 2014). We also note that while our primary models indicated that patients with daily/almost daily cannabis use had an increased risk of acute care, the effect size was modest and the association was attenuated when adjusted for clinical characteristics, unlike in prior studies focusing on risk associated with cannabis use disorders (Campbell et al., 2017; Gubatan et al., 2016). More work is needed to evaluate whether the frequency of use per se is independently associated with increased risk of acute care.
There was indication of a dose-response relationship between frequency of other drug use and subsequent acute care-except for the category of monthly use, which was not associated with acute care. The association for less than monthly and daily/almost daily drug use was also independent of other clinical characteristics such as mental health and SUDs. Several prior drug-specific studies have evaluated whether various frequencies of drug use were associated with acute care utilization in other populations (Frank et al., 2015; Marshall et al., 2012). Specifically, one study found that risk of having an emergency department visit was elevated for people who used methamphetamines daily, but not less than daily, when compared to no use (Marshall et al., 2012). In contrast, a cross-sectional study found any frequency of non-medical use of prescription pain medication was associated with emergency department visits (Frank et al., 2015). It is unclear why, in the current study, monthly drug use was not associated with acute care utilization. Analyses may have been underpowered due to the small number of patients reporting drug use, or differences in findings may reflect differences in how studies asked about frequency and timing of drug use. One other study found neither an association between occasional crack cocaine use relative to no use, nor daily crack cocaine use relative to occasional use and emergency department visits (Siegal et al., 2006). However, all participants in that study had previously used cocaine (Siegal et al., 2006).
Risk of acute care varied across frequency of cannabis use by sex and age but not past-year SUD. Specifically, an increased risk of acute care was observed for females, but not males, in sex-stratified models. Reasons for these differences are unknown, but it is known that women experience more adverse outcomes when they use cannabis (Cooper and Haney, 2014). Risks also varied by age, such that younger, but not older adults, who reported cannabis use experienced an elevated risk of acute care. Risk of acute care also varied across other drug screening score by age but not sex or past-year SUD. Risk was highest among the younger persons, echoing results from a study reporting younger age as a correlate of frequent emergency department use among a cohort of people who inject drugs (Nambiar et al., 2018). Effect modification findings need replication in other samples.
This study has several limitations. The sample was representative of predominantly non-Hispanic White patients enrolled in a single health plan in Washington State, where medical and recreational cannabis use is legal. It is unclear whether findings are generalizable to health systems in U.S. states with broader racial/ethnic diversity, or states where cannabis use is illegal. Analyses excluded patients who missed their annual behavioral health screening. However, prior analyses have found few differences between patients who did and did not complete screening (Lapham et al., 2017; Sayre et al., 2020). Another limitation was that the screens for cannabis and other drug use have not been validated against diagnostic interviews. However, these screens were adapted from well-validated measures (Babor et al., 2001; Smith et al., 2010; WHO ASSIST Working Group, 2002), have face validity, and demonstrate associations with other risk indicators such as behavioral health conditions (Lapham et al., 2018; Sayre et al., 2020). Patients may have under-reported their substance use due to stigma (McNeely et al., 2018) or due to how the questions were worded. For example, it is possible that a patient might not know to report the use of a substance if they did not know it was illegal or if they did not know they were using it not as prescribed. Also, the other drug use measure does not assess specific drug exposure and does not ask about polydrug use. This is a common problem with screening instruments. For instance, the AUDIT-C alcohol screening instrument markedly under-estimates average consumption but is still an excellent marker risk of AUD and other adverse events (Chavez et al., 2012; Rubinsky et al., 2013). Data validation and quality concerns have also been described for ICD diagnoses, which were used in this study for covariate adjustment, however these diagnoses may accurately represent what is known about patients in a clinical context (Cowie et al., 2017). Analyses were likely limited by the small number of patients who indicated monthly to daily/almost daily other drug use and were underpowered to detect effect modification by race/ethnicity. This study looked at incident acute care: there may be associations between cannabis or other drug use and volume of acute care utilization. Nevertheless, this is a unique study with population-based screening results on 47,447 patients who had frequency of past-year cannabis and/or other drug responses and acute care utilization documented in their EHRs, allowing us to examine the performance of screening in a real world sample as opposed to a sample that has consented to participating in research interviews or interventions.
5. CONCLUSION
In a sample of predominantly non-Hispanic White primary care patients, frequency of past-year use derived from patient responses to routine population-based screening for cannabis and other drug use in primary care was associated with acute care utilization. Further research is needed to replicate these findings in racially diverse populations, understand conditions that lead to acute care, and evaluate whether changes in screening results are associated with changes in risk of acute care. If replicated, they may have implications for counseling patients about risks associated with cannabis and other drug use.
Supplementary Material
Supplemental File 1. Estimated relative hazards of acute care utilization for subgroups according to frequency of past-year cannabis and other drug use
Highlights.
Frequency of past-year cannabis and other drug use predicted risk of acute care
Rare and frequent cannabis use was associated with increased risk of acute care
Increasing use of other drugs was associated with increased risk of acute care
Associations were modified by gender and age.
Acknowledgements
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Agency for Healthcare Research and Quality.
Role of funding source
Research reported in this publication was supported by the National Institute on Drug Abuse and the National Institute on Alcohol Abuse and Alcoholism of the National Institutes of Health under Award Numbers UG1DA040314, K01AA023859 and K24AA022128, as well as the Agency for Healthcare Research and Quality under award number R18HS023173.
Footnotes
Author Disclosures
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
None.
References
- Agrawal A, Lynskey MT, 2007. Does gender contribute to heterogeneity in criteria for cannabis abuse and dependence? Results from the national epidemiological survey on alcohol and related conditions. Drug Alcohol Depend 88(2–3), 300–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG, 2001. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care, 2nd Edition. http://www.dass.stir.ac.uk/DRUGS/pdf/audit.pdf. (Accessed Feb 1 2012).
- Bahorik AL, Satre DD, Kline-Simon AH, Weisner CM, Young-Wolff KC, Campbell CI, 2018. Alcohol, marijuana, and opioid use disorders: 5-Year patterns and characteristics of emergency department encounters. Substance abuse 39(1), 59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobb JF, Lee AK, Lapham GT, Oliver M, Ludman E, Achtmeyer C, Parrish R, Caldeiro RM, Lozano P, Richards JE, Bradley KA, 2017. Evaluation of a Pilot Implementation to Integrate Alcohol-Related Care within Primary Care. Int J Environ Res Public Health 14(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobb JF, Qiu H, Matthews AG, McCormack J, Bradley KA, 2020. Addressing identification bias in the design and analysis of cluster-randomized pragmatic trials: a case study. Trials 21(1), 289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley KA, Kivlahan DR, Zhou XH, Sporleder JL, Epler AJ, McCormick KA, Merrill JO, McDonell MB, Fihn SD, 2004. Using alcohol screening results and treatment history to assess the severity of at-risk drinking in Veterans Affairs primary care patients. Alcohol Clin Exp Res 28(3), 448–455. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Rubinsky AD, Lapham GT, Berger D, Bryson C, Achtmeyer C, Hawkins EJ, Chavez LJ, Williams EC, Kivlahan DR, 2016. Predictive validity of clinical AUDIT-C alcohol screening scores and changes in scores for three objective alcohol-related outcomes in a Veterans Affairs population. Addiction 111(11), 1975–1984. [DOI] [PubMed] [Google Scholar]
- Campbell CI, Bahorik AL, Kline-Simon AH, Satre DD, 2017. The role of marijuana use disorder in predicting emergency department and inpatient encounters: A retrospective cohort study. Drug Alcohol Depend 178, 170–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavez LJ, Liu C-F, Tefft N, Hebert PL, Clark BJ, Rubinsky AD, Lapham GT, Bradley KA, 2016. Unhealthy alcohol use in older adults: Association with readmissions and emergency department use in the 30 days after hospital discharge(). Drug and alcohol dependence 158, 94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavez LJ, Williams EC, Lapham G, Bradley KA, 2012. Association between alcohol screening scores and alcohol-related risks among female veterans affairs patients. J Stud Alcohol Drugs 73(3), 391–400. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ, Ye Y, Watters K, Brubacher JR, Stenstrom R, 2012. Risk of injury from alcohol and drug use in the emergency department: a case-crossover study. Drug Alcohol Rev 31(4), 431–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleves MA, Gould WW, Gutierrez RG, 2002. An Introduction to Survival Analysis Using Stata. Stata Press. [Google Scholar]
- Cooper ZD, Haney M, 2014. Investigation of sex-dependent effects of cannabis in daily cannabis smokers. Drug Alcohol Depend 136, 85–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowie MR, Blomster JI, Curtis LH, Duclaux S, Ford I, Fritz F, Goldman S, Janmohamed S, Kreuzer J, Leenay M, Michel A, Ong S, Pell JP, Southworth MR, Stough WG, Thoenes M, Zannad F, Zalewski A, 2017. Electronic health records to facilitate clinical research. Clin Res Cardiol 106(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox DR, 1972. Regression models and life‐tables. Journal of the Royal Statistical Society: Series B (Methodological) 34(2), 187–202. [Google Scholar]
- Doupe MB, Palatnick W, Day S, Chateau D, Soodeen RA, Burchill C, Derksen S, 2012. Frequent users of emergency departments: developing standard definitions and defining prominent risk factors. Annals of emergency medicine 60(1), 24–32. [DOI] [PubMed] [Google Scholar]
- Frank JW, Binswanger IA, Calcaterra SL, Brenner LA, Levy C, 2015. Non-medical use of prescription pain medications and increased emergency department utilization: Results of a national survey. Drug Alcohol Depend 157, 150–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksson M, Edenström M, Lundahl A, Björkman L, 2015. ACG model can predict large consumers of health care. Health care resources can be used more wisely, individuals at risk can receive better care. Lakartidningen 112. [PubMed] [Google Scholar]
- Fuster D, Cheng DM, Allensworth-Davies D, Palfai TP, Samet JH, Saitz R, 2014. No detectable association between frequency of marijuana use and health or healthcare utilization among primary care patients who screen positive for drug use. Journal of general internal medicine 29(1), 133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass JE, Bobb JF, Lee AK, Richards JE, Lapham GT, Ludman E, Achtmeyer C, Caldeiro RM, Parrish R, Williams EC, Lozano P, Bradley KA, 2018. Study protocol: a cluster-randomized trial implementing Sustained Patient-centered Alcohol-related Care (SPARC trial). Implement Sci 13(1), 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman S, Wadsworth E, Leos-Toro C, Hammond D, International Cannabis Policy Study, t., 2020. Prevalence and forms of cannabis use in legal vs. illegal recreational cannabis markets. Int J Drug Policy 76, 102658. [DOI] [PubMed] [Google Scholar]
- Gubatan J, Staller K, Barshop K, Kuo B, 2016. Cannabis Abuse Is Increasing and Associated with Increased Emergency Department Utilization in Gastroenterology Patients. Dig Dis Sci 61(7), 1844–1852. [DOI] [PubMed] [Google Scholar]
- Hall W, Degenhardt L, 2009. Adverse health effects of non-medical cannabis use. The Lancet 374(9698), 1383–1391. [DOI] [PubMed] [Google Scholar]
- Harrell FE, 2001. General Aspects of Fitting Regression Models, in: Harrell FE (Ed.) Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis. Springer; New York, New York, NY, pp. 11–40. [Google Scholar]
- Kim HS, Hall KE, Genco EK, Van Dyke M, Barker E, Monte AA, 2016. Marijuana Tourism and Emergency Department Visits in Colorado. N Engl J Med 374(8), 797–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, Caughey AB, Curry SJ, Donahue K, Doubeni CA, Epling JW Jr., Kubik M, Ogedegbe G, Pbert L, Silverstein M, Simon MA, Tseng CW, Wong JB, 2020. Screening for Unhealthy Drug Use: US Preventive Services Task Force Recommendation Statement. Jama 323(22), 2301–2309. [DOI] [PubMed] [Google Scholar]
- Lapham GT, Lee AK, Caldeiro RM, Glass JE, Carrell DS, Richards JE, Bradley KA, 2018. Prevalence of Behavioral Health Conditions Across Frequency of Cannabis Use Among Adult Primary Care Patients in Washington State. J Gen Intern Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapham GT, Lee AK, Caldeiro RM, McCarty D, Browne KC, Walker DD, Kivlahan DR, Bradley KA, 2017. Frequency of cannabis use among primary care patients in Washington State. Journal of the American Board of Family Medicine : JABFM 30(6), 795–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin DY, Wei LJ, 1989. The Robust Inference for the Cox Proportional Hazards Model. Journal of the American Statistical Association 84(408), 1074–1078. [Google Scholar]
- Lind BK, Gerkovich MM, Cherkin DC, Deyo RA, Sherman KJ, Lafferty WE, 2013. Effect of Risk Adjustment Method on Comparisons of Health Care Utilization Between Complementary and Alternative Medicine Users and Nonusers. Journal of Alternative and Complementary Medicine 19(3), 250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loflin M, Earleywine M, 2014. A new method of cannabis ingestion: the dangers of dabs? Addict Behav 39(10), 1430–1433. [DOI] [PubMed] [Google Scholar]
- Marshall BDL, Grafstein E, Buxton JA, Qi J, Wood E, Shoveller JA, Kerr T, 2012. Frequent methamphetamine injection predicts emergency department utilization among street-involved youth. Public health 126(1), 47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely J, Cleland CM, Strauss SM, Palamar JJ, Rotrosen J, Saitz R, 2015a. Validation of Self-Administered Single-Item Screening Questions (SISQs) for Unhealthy Alcohol and Drug Use in Primary Care Patients. J Gen Intern Med 30(12), 1757–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely J, Kumar PC, Rieckmann T, Sedlander E, Farkas S, Chollak C, Kannry JL, Vega A, Waite EA, Peccoralo LA, Rosenthal RN, McCarty D, Rotrosen J, 2018. Barriers and facilitators affecting the implementation of substance use screening in primary care clinics: a qualitative study of patients, providers, and staff. Addict Sci Clin Pract 13(1), 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely J, Strauss SM, Saitz R, Cleland CM, Palamar JJ, Rotrosen J, Gourevitch MN, 2015b. A Brief Patient Self-administered Substance Use Screening Tool for Primary Care: Two-site Validation Study of the Substance Use Brief Screen (SUBS). Am J Med 128(7), 784 e789–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeely J, Wu LT, Subramaniam G, Sharma G, Cathers LA, Svikis D, Sleiter L, Russell L, Nordeck C, Sharma A, O’Grady KE, Bouk LB, Cushing C, King J, Wahle A, Schwartz RP, 2016. Performance of the Tobacco, Alcohol, Prescription Medication, and other Substance use (TAPS) tool for substance use screening in primary care patients. Ann Intern Med 165(10), 690–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD, 2013. Measuring the global burden of disease. N Engl J Med 369(5), 448–457. [DOI] [PubMed] [Google Scholar]
- Nambiar D, Spelman T, Stoové M, Dietze P, 2018. Are People Who Inject Drugs Frequent Users of Emergency Department Services? A Cohort Study (2008–2013). Substance Use & Misuse 53(3), 457–465. [DOI] [PubMed] [Google Scholar]
- National Council for Behavioral Health, 2018. Implementing Care for Alcohol & Other Drug Use in Medical Setting: An Extension of SBIRT. National Council for Behavioral Health, Washington DC. [Google Scholar]
- Pilowsky DJ, Wu LT, 2012. Screening for alcohol and drug use disorders among adults in primary care: a review. Subst Abuse Rehabil 3(1), 25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramaekers JG, Kauert G, Theunissen EL, Toennes SW, Moeller MR, 2009. Neurocognitive performance during acute THC intoxication in heavy and occasional cannabis users. J Psychopharmacol 23(3), 266–277. [DOI] [PubMed] [Google Scholar]
- Richards JE, Bobb JF, Lee AK, Lapham GT, Williams EC, Glass JE, Ludman EJ, Achtmeyer C, Caldeiro RM, Oliver M, Bradley KA, 2019. Integration of screening, assessment, and treatment for cannabis and other drug use disorders in primary care: An evaluation in three pilot sites. Drug Alcohol Depend 201, 134–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubinsky AD, Chavez LJ, Berger D, Lapham GT, Hawkins EJ, Williams EC, Bradley KA, 2019. Utility of routine alcohol screening for monitoring changes in alcohol consumption. Drug Alcohol Depend 201, 155–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR, Bradley KA, 2013. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol Clin Exp Res 37(8), 1380–1390. [DOI] [PubMed] [Google Scholar]
- Saitz R, Palfai TP, Cheng DM, Alford DP, Bernstein JA, Lloyd-Travaglini CA, Meli SM, Chaisson CE, Samet JH, 2014. Screening and brief intervention for drug use in primary care: the ASPIRE randomized clinical trial. JAMA 312(5), 502–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayre M, Lapham GT, Lee AK, Oliver M, Bobb JF, Caldeiro RM, Bradley KA, 2020. Routine Assessment of Symptoms of Substance Use Disorders in Primary Care: Prevalence and Severity of Reported Symptoms. J Gen Intern Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegal HA, Falck RS, Wang J, Carlson RG, Massimino KP, 2006. Emergency department utilization by crack-cocaine smokers in Dayton, Ohio. The American journal of drug and alcohol abuse 32(1), 55–68. [DOI] [PubMed] [Google Scholar]
- Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R, 2010. A single-question screening test for drug use in primary care. Arch Intern Med 170(13), 1155–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spindle TR, Cone EJ, Schlienz NJ, Mitchell JM, Bigelow GE, Flegel R, Hayes E, Vandrey R, 2018. Acute Effects of Smoked and Vaporized Cannabis in Healthy Adults Who Infrequently Use Cannabis: A Crossover Trial. JAMA Netw Open 1(7), e184841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starfield B, Kinder K, 2011. Multimorbidity and its measurement. Health Policy 103(1), 3–8. [DOI] [PubMed] [Google Scholar]
- StataCorp, 2017. Stata Statistical Software: Release 15. StataCorp LLC, College Station, TX. [Google Scholar]
- Strom BL, Bjornson DC, 2006. Book Review: Pharmacoepidemiology, 4th Edition. Annals of Pharmacotherapy 40(5), 1000–1001. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2019. Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health, in: PEP19–5068, H.P.N. (Ed.) NSDUH Series H-54. Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Tai B, Volkow ND, 2013. Treatment for substance use disorder: opportunities and challenges under the affordable care act. Soc Work Public Health 28(3–4), 165–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiet QQ, Leyva YE, Moos RH, Frayne SM, Osterberg L, Smith B, 2015. Screen of Drug Use: Diagnostic Accuracy of a New Brief Tool for Primary Care. JAMA Intern Med 175(8), 1371–1377. [DOI] [PubMed] [Google Scholar]
- U. S. Burden of Disease Collaborators, Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E, Lee A, Khan AR, Ahmadi A, Ferrari AJ, Kasaeian A, Werdecker A, Carter A, Zipkin B, Sartorius B, Serdar B, Sykes BL, Troeger C, Fitzmaurice C, Rehm CD, Santomauro D, Kim D, Colombara D, Schwebel DC, Tsoi D, Kolte D, Nsoesie E, Nichols E, Oren E, Charlson FJ, Patton GC, Roth GA, Hosgood HD, Whiteford HA, Kyu H, Erskine HE, Huang H, Martopullo I, Singh JA, Nachega JB, Sanabria JR, Abbas K, Ong K, Tabb K, Krohn KJ, Cornaby L, Degenhardt L, Moses M, Farvid M, Griswold M, Criqui M, Bell M, Nguyen M, Wallin M, Mirarefin M, Qorbani M, Younis M, Fullman N, Liu P, Briant P, Gona P, Havmoller R, Leung R, Kimokoti R, Bazargan-Hejazi S, Hay SI, Yadgir S, Biryukov S, Vollset SE, Alam T, Frank T, Farid T, Miller T, Vos T, Barnighausen T, Gebrehiwot TT, Yano Y, Al-Aly Z, Mehari A, Handal A, Kandel A, Anderson B, Biroscak B, Mozaffarian D, Dorsey ER, Ding EL, Park EK, Wagner G, Hu G, Chen H, Sunshine JE, Khubchandani J, Leasher J, Leung J, Salomon J, Unutzer J, Cahill L, Cooper L, Horino M, Brauer M, Breitborde N, Hotez P, Topor-Madry R, Soneji S, Stranges S, James S, Amrock S, Jayaraman S, Patel T, Akinyemiju T, Skirbekk V, Kinfu Y, Bhutta Z, Jonas JB, Murray CJL, 2018. The State of US Health, 1990–2016: Burden of Diseases, Injuries, and Risk Factors Among US States. JAMA 319(14), 1444–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitale S, van de Mheen D, 2006. Illicit drug use and injuries: A review of emergency room studies. Drug Alcohol Depend 82(1), 1–9. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Baler RD, Compton WM, Weiss SR, 2014. Adverse health effects of marijuana use. N Engl J Med 370(23), 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO ASSIST Working Group, 2002. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction 97(9), 1183–1194. [DOI] [PubMed] [Google Scholar]
- Williams EC, Bryson CL, Sun H, Chew RB, Chew LD, Blough DK, Au DH, Bradley KA, 2012. Association between alcohol screening results and hospitalizations for trauma in Veterans Affairs outpatients. Am J Drug Alcohol Abuse 38(1), 73–80. [DOI] [PubMed] [Google Scholar]
- Williams RL, 2000. A note on robust variance estimation for cluster-correlated data. Biometrics 56(2), 645–646. [DOI] [PubMed] [Google Scholar]
- Wu LT, Zhu H, Ghitza UE, 2018. Multicomorbidity of chronic diseases and substance use disorders and their association with hospitalization: Results from electronic health records data. Drug and alcohol dependence 192, 316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick DF, Rowhani-Rahbar A, Wang J, Russo J, Darnell D, Ingraham L, Whiteside LK, Guiney R, Hedrick MK, Rivara FP, 2017. The Cumulative Burden of Mental, Substance Use, and General Medical Disorders and Rehospitalization and Mortality After an Injury. Psychiatric services (Washington, D.C.) 68(6), 596–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zielinski A, Kronogård M, Lenhoff H, Halling A, 2009. Validation of ACG Case-mix for equitable resource allocation in Swedish primary health care. BMC Public Health 9(1), 347. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental File 1. Estimated relative hazards of acute care utilization for subgroups according to frequency of past-year cannabis and other drug use


