Abstract
Background:
Resilience is the ability to adapt positively to stress and adversity. It is a potential therapeutic target as it is reduced in irritable bowel syndrome (IBS) compared to healthy controls and associated with worse symptom severity and poorer quality of life. The aim of this study was to examine if these findings are generalizable by comparing resilience between IBS versus the general population and other chronic gastrointestinal (GI) conditions.
Methods:
Participants in the general population completed an online survey containing questionnaires measuring demographics, diagnosis of IBS and other GI conditions, symptom severity, psychological symptoms, resilience, and early adverse life events (EALs). IBS was defined as having a physician diagnosis of IBS and/or meeting Rome criteria without co-morbid GI disease. All others were included in the general population group. The chronic GI conditions group included those with inflammatory bowel disease, celiac disease and/or microscopic colitis.
Results:
Resilience was lower in IBS (n=820) than the general population (n=1026; p≤0.001) and associated with worse IBS symptom severity (p<0.05). Global mental health affected resilience differently in IBS compared to the general population (all p’s<0.05). EALs were associated with decreased ability to bounce back from adversity in both IBS and the general population(p<0.001). Resilience scores were similar in IBS and other chronic GI conditions that present with similar symptoms.
Conclusion:
Resilience is lower compared to the general U.S. population but does not appear to be specific to IBS as it is comparable to other chronic GI conditions. Low resilience negatively affects symptom severity and mental health and thus, may serve as a novel therapeutic target.
Keywords: irritable bowel syndrome, resilience, inflammatory bowel disease, celiac disease
Introduction
Resilience is the ability of an individual to recover from, maintain social and physical function, and thrive in response to adversity and stress.1–3 This has become a growing area of interest in relation to stress-sensitive disorders such as post-traumatic stress disorder1, fibromyalgia4, depression/anxiety5 and, more recently, irritable bowel syndrome (IBS)6. Patients with these disorders who possess greater resilience have lower symptom burden and psychological distress.1, 4, 5, 7
Resilience is a complex concept that is comprised of various psychological constructs including hardiness, adaptability, self-efficacy, positive emotions, social support, coping style, perseverance and presence of a structured environment.8, 9 Maltby et. al. proposed a model of resilience consisting of three major concepts: 1) engineering resilience or the ability to return to equilibrium after a disturbance; 2) ecological resilience or the ability to resist a disturbance and maintain a stable state; and 3) adaptive resilience or the ability to accommodate and thrive in the presence of change.10 Several validated measures have been developed in an attempt to measure these various aspects of resilience. Maltby et. al. performed a factor analysis of five measures of resilience to determine how well these tools measured these three concepts.10 It was found that the Brief Resilience Scale (BRS)3; which was developed to specifically measure the ability to ‘bounce back’, represented a measure of engineering resilience. Questions from the Connor-Davidson Resilience Scale (CD-RISC)1; which was designed to measure multiple components of the resilience construct listed above, measured both adaptive and ecological resilience.
IBS is a disorder of gut-brain interaction characterized by abdominal pain associated with changes in stool frequency and/or form.11 A study by our group demonstrated that resilience, as measured by CD-RISC and BRS was significantly lower in patients with IBS compared to healthy controls.6 In addition, lower resilience was associated with worse IBS symptom severity and IBS-related quality of life. Our previous study also showed that early adverse life events (EALs), which have been associated with the development12 and severity13 of IBS, correlated with lower resilience in both IBS and healthy controls. The IBS patients and healthy controls in our previous study were recruited from the Los Angeles metropolitan area, thus it is not known if these results are applicable to the general U.S. population.
It is also not well known if resilience is decreased in chronic gastrointestinal (GI) disorders that present with similar symptoms as IBS. Though resilience has been studied to a limited extent in inflammatory bowel disease (IBD), studies of resilience in other conditions such as celiac disease and microscopic colitis have not been performed. One study demonstrated that higher CD-RISC resilience scores were associated with a higher level of readiness to transition from pediatric to adult care of IBD. However, when disease severity was controlled for, this effect was no longer seen.14 In a cohort of Swedish men born between 1952–1956 who participated in compulsory military service, those with low stress resilience in adolescence had an increased risk of developing IBD in adulthood.15 However, this study only looked at stress resilience and not the other components of resilience. Finally, a study compared CD-RISC and BRS scores as measures of resilience in healthy controls, IBS patients and IBD patients. Patients with IBS, specifically, demonstrated reduced resilience compared to healthy controls.16 This was a small study conducted in a similar population to the resilience in IBS study described above6 and, thus, the generalizability of these findings to the general population is unclear.
The primary aim of this study was to determine if resilience is lower in IBS compared to the general U.S. population. We hypothesize that resilience will be lower in IBS compared to the general population. The secondary aims of this study were to test the following hypotheses: 1) in those with IBS, lower resilience is associated with worse IBS symptom severity; 2) demographic factors and general physical and mental health measures will predict resilience and will be associated with resilience in different ways; 3) EALs are associated with lower resilience in both IBS and the general population but have a greater negative effect in those with IBS; and 4) resilience is lower in IBS compared to those with other chronic GI conditions that present with similar symptoms including IBD, celiac disease and microscopic colitis.
Materials and Methods
Subject Selection and Recruitment
Subjects were recruited between December 14 and 22, 2017 by the market research firm Cint USA, Inc. (Los Angeles, California). This firm was also used for the validation of the National Institutes of Health (NIH) Patient-Reported Outcomes Measurement Information System (PROMIS) for GI symptoms.17 The online study survey was sent to a nationwide sample of the general U.S. population with representation from all 50 states and to individuals across the U.S. who previously self-reported having a diagnosis of IBS. All subjects were English speaking and at least 18 years of age. All potential subjects completed an online consent form prior to completing the study survey. This study was approved by the Institutional Research Board of the University of California, Los Angeles.
Study Survey
The online study survey was designed using SurveyMonkey™. Demographic information collected included age, sex, ethnicity, race, education, income, marital status, employment status and military service. Participants were asked if they were diagnosed by a doctor with a number of medical conditions, including IBS, celiac disease, Crohn’s disease, ulcerative colitis, previous GI surgery, GI malignancy, anxiety, depression and substance abuse. All participants completed the Rome IV criteria questionnaire for IBS.11 Several additional validated questionnaires were collected including BRS3, CD-RISC1, PROMIS global physical and mental health18, Adverse Childhood Experience survey (ACE)19 and the IBS-Severity Scoring System (IBS-SSS)20. (See Supplementary Methods for details).
Subject Exclusion and Categorization
Three repeated survey questions were used to eliminate inconsistent responders from the data analysis. Participants who did not provide answers for the Rome IV or both resilience measures were excluded. Responders who indicated the presence of all listed comorbidities were also excluded due to concerns about the accuracy of their answers to the survey questions.
The IBS group was defined as those who indicated having a physician made diagnosis of IBS and/or met Rome III21 (i.e., presence of abdominal pain at least 3 days per month) or IV11 criteria without indicating co-morbid GI disease. For the comparisons between IBS and the general population, the general population group included all respondents not included in the IBS group.
For comparisons between participants with IBS and other chronic GI conditions with similar symptoms, the latter group was defined as respondents with a self-reported physician made diagnosis of Crohn’s disease, ulcerative colitis, celiac disease and/or microscopic colitis. These respondants did not have a concurrent diagnosis of IBS. These conditions were combined into one group and a separate exploratory analysis was performed due to the low number of individuals who reported having one of these diagnoses. A matched group of IBS participants from the larger IBS group was generated based on age and sex.
Statistical Analysis
Clinical characteristics were summarized and stratified by IBS status as count (%) and mean (standard deviation [SD]). Categorical variables were compared with IBS status using the χ2 or Fisher’s Exact test and continuous variables using the t-test or Wilcoxon rank sum test. Multivariable logistic regression was performed to determine the association between resilience and IBS status. Multivariable linear regression was performed to determine the association between resilience and IBS symptom severity. Covariates including age, income and education were modeled as continuous variables while sex, employment, marital status, active military service, ethnicity and race were modeled as categorical variables. Linear regression was used to determine the association between demographic, physical health status, mental health status and the presence of EALs with resilience and whether these factors moderate the effect of IBS status on resilience. Linear regression was used to determine whether IBS subjects have higher resilience compared to matched subjects with chronic GI comorbidities. A p-value of <0.05 was considered statistically significant.
Results
Subject Characteristics
There were 2,185 participants who responded to the survey. Of these, 339 (15.5%) were excluded based on incomplete or inconsistent survey answers (Supplementary Figure 1). There were 1846 participants who were included in the final analysis with 820 (44.4%) in the IBS group and 1026 (55.6%) in the general population group. The majority of our sample was from major metropolitan areas (73%) and all 50 states were represented. Compared to the general population group, the IBS group was older, had a higher proportion of women, higher proportion of Caucasians, a lower proportion of Hispanics, lower income, lower level of education, were more likely to be unemployed, were less likely to be single and less likely to be in active military service (all p’s<0.006 (Table 1)). Participants had similar numbers of EALs in both groups. In those with IBS, the average IBS-SSS score was 239±94.27 indicating moderate IBS symptom severity.
Table 1:
Subject Characteristics
| General Population (n=1026) | IBS (n=820) | p-value | |
|---|---|---|---|
| Age | 40.43 (13.84) | 45.11 (15.07) | <0.001 |
| Female (%) | 692 (67%) | 692 (85%) | <0.001 |
| Ethnicity – Hispanic | 101 (11%) | 31 (4%) | <0.001 |
| Race | <0.001 | ||
| Caucasian | 831 (81%) | 743 (90%) | |
| African American | 84 (8%) | 29 (4%) | |
| American Indian/Asian/Hawaiian/Other | 86 (8%) | 18 (2%) | |
| Multiracial | 25 (3%) | 30 (4%) | |
| Marital Status (%) | 0.006 | ||
| Single | 271 (26.62%) | 176 (21.52%) | |
| Married or equivalent relationship | 635 (62.38%) | 514 (62.84%) | |
| Divorced | 83 (8.15%) | 94 (11.49%) | |
| Widowed | 29 (2.85%) | 34 (4.16%) | |
| Income (%) | 0.003 | ||
| Less than $10,000 | 73 (7.48%) | 55 (6.96%) | |
| $10,000-$19,999 | 100 (10.25%) | 87 (11.01%) | |
| $20,000-$29,999 | 99 (10.14%) | 111 (14.05%) | |
| $30,000-$39,999 | 106 (10.86%) | 91 (11.52%) | |
| $40,000-$49,999 | 76 (7.79%) | 81 (10.25%) | |
| $50,000-$59,999 | 89 (9.12%) | 77 (9.75%) | |
| $60,000-$69,999 | 65 (6.66%) | 65 (8.23%) | |
| $70,000-$79,999 | 121 (12.4%) | 66 (8.35%) | |
| Greater than $80,000 | 247 (25.31%) | 157 (19.87%) | |
| Education (%) | <0.001 | ||
| 8th grade or less | 2 (0.2%) | 1 (0.12%) | |
| Some high school | 38 (3.71%) | 24 (2.93%) | |
| High school graduate | 220 (21.48%) | 167 (20.37%) | |
| Some college | 252 (24.61%) | 291 (35.49%) | |
| College graduate | 294 (28.71%) | 238 (29.02%) | |
| Post-graduate education | 218 (21.29%) | 99 (12.07%) | |
| Employment (%) | <0.001 | ||
| Employed | 592 (58.85%) | 401 (49.94%) | |
| Unemployed | 200 (19.88%) | 202 (25.16%) | |
| Retired | 148 (14.71%) | 177 (22.04%) | |
| Student | 66 (6.56%) | 23 (2.86%) | |
| Military Status (%) | <0.001 | ||
| Not in military | 871 (88.16%) | 769 (95.06%) | |
| Actively in the military | 42 (4.25%) | 2 (0.25%) | |
| Military Veteran | 75 (7.59%) | 38 (4.7%) | |
| BRS Score (0–5) | 3.23 (0.83) | 2.98 (0.91) | <0.001 |
| CD-RISC (0–100) | 70.09 (17.64) | 65.2 (17.5) | <0.001 |
| ACE Score (0–8) | 2.7 (2.39) | 2.5 (2.12) | 0.329 |
| PROMIS global Health Physical (2–10) | 7.3 (2) | 6.52 (1.9) | <0.001 |
| PROMIS global Health Mental (2–10) | 6.88 (2.22) | 6.02 (2.15) | <0.001 |
| IBS-SSS (0–500) | 239 (94.27) | ||
| IBS Subtype (%) | |||
| Constipation | 225 (27.44%) | ||
| Diarrhea | 231 (28.17%) | ||
| Mixed | 312 (38.05%) | ||
| Unspecified | 44 (5.37%) | ||
| Declined to answer | 8 (0.98%) |
Abbreviations: IBS- irritable bowel syndrome; BRS-Brief Resilience Score; CD-RISC- Connor Davidson Resilience Scale, ACE-adverse childhood experiences survey; PROMIS- patient reported outcomes measurement information system; IBS-SSS- IBS-Severity Scoring System
Resilience in IBS versus the general population
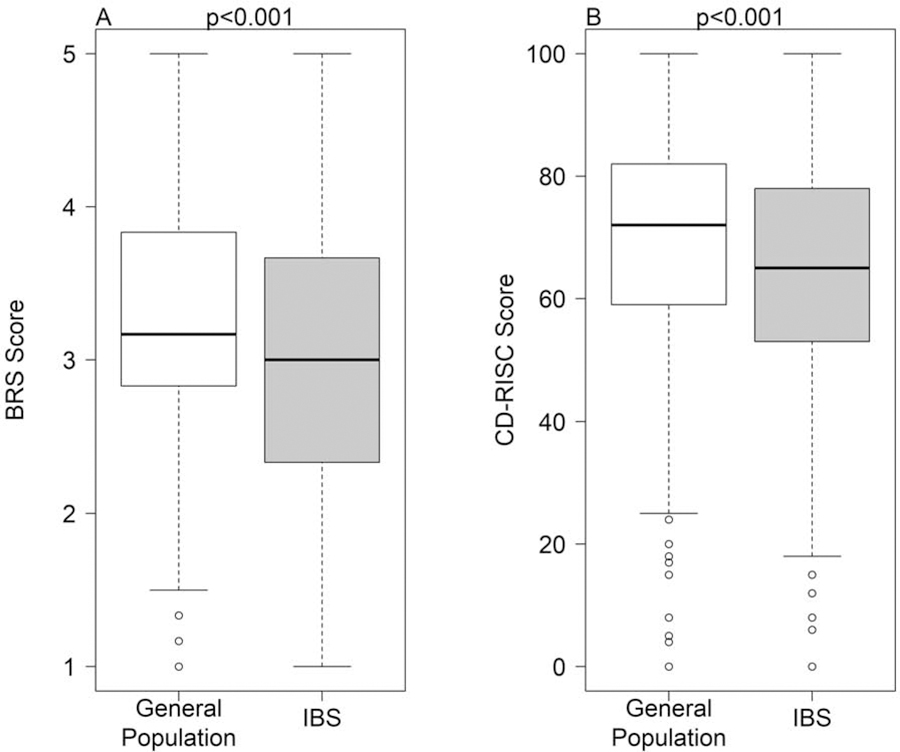
After controlling for age, sex, income, employment status, education, military status, marital status, ethnicity and race, respondents with IBS had significantly lower mean resilience scores compared to the general population group as measured by BRS (β=−0.23, 95% CI[−0.32,−0.15], p<0.001) and CD-RISC (β=−3.84, 95% CI [−5.52,−2,76], p<0.001) (Figure 1).
Figure 1:
Resilience in IBS (n=820) is lower vs. general population (n=1026) subjects as measured by A) BRS and B) CD-RISC.
Resilience and IBS symptom severity
Decreased resilience as measured by BRS (β=−0.002, 95% CI [−0.002, −0.0008], p<0.001) and CD-RISC (β=−0.015, 95% CI [−0.03,−0.001], p=0.032) was associated with worse IBS symptom severity as measured by the IBS-SSS.
Demographic determinants of resilience overall
Overall, demographic factors were associated with the different components of resilience (Tables 2 and 3). Unemployment, female gender, and being retired or widowed were associated with lower resilience as measured by at least one of the resilience questionnaires (all p<0.05). Older age, African American race, active military service, higher income, and higher level of education were associated with higher resilience scores (all p<0.05). This did not differ between IBS and the general population.
Table 2:
Demographic Determinants of Resilience as Measured by BRS Regression Table
| Outcome: BRS Score | Coefficient | SE | p-value |
|---|---|---|---|
| Intercept | 2.793 | 0.135 | <0.001 |
| IBS vs General Population | −0.234 | 0.043 | <0.001 |
| Military Status | |||
| Active vs Not Active | −0.275 | 0.139 | 0.049 |
| Veteran vs Not Active | 0.087 | 0.089 | 0.325 |
| Employment Status | |||
| Unemployed vs Employed | −0.260 | 0.057 | <0.001 |
| Retired vs Employed | −0.210 | 0.070 | 0.003 |
| Student vs Employed | −0.052 | 0.113 | 0.642 |
| Marital Status | |||
| Married vs Single | −0.093 | 0.056 | 0.098 |
| Divorced vs Single | −0.077 | 0.084 | 0.357 |
| Widowed vs Single | −0.316 | 0.127 | 0.013 |
| Race/Ethnicity | |||
| African American vs Caucasian | 0.261 | 0.091 | 0.004 |
| Other Ethnicity vs Caucasian | −0.099 | 0.096 | 0.300 |
| Multiracial vs Caucasian | −0.044 | 0.124 | 0.726 |
| Income | 0.023 | 0.010 | 0.018 |
| Education | 0.033 | 0.022 | 0.141 |
| Age | 0.010 | 0.002 | <0.001 |
| Female vs Male | −0.121 | 0.053 | 0.021 |
Table 3:
Demographic Determinants of Resilience as Measured by CD-RISC Regression Table
| Outcome: CD-RISC | Coefficient | SE | p-value |
|---|---|---|---|
| Intercept | 57.39 | 2.71 | <0.001 |
| IBS vs General Population | −3.84 | 0.86 | <0.001 |
| Military Status | |||
| Active vs Not Active | 12.11 | 2.88 | <0.001 |
| Veteran vs Not Active | 1.40 | 1.77 | 0.429 |
| Employment Status | |||
| Unemployed vs Employed | −6.89 | 1.15 | <0.001 |
| Retired vs Employed | −1.50 | 1.40 | 0.284 |
| Student vs Employed | −0.96 | 2.22 | 0.664 |
| Marital Status | |||
| Married vs Single | 1.25 | 1.12 | 0.267 |
| Divorced vs Single | −1.11 | 1.68 | 0.510 |
| Widowed vs Single | −4.41 | 2.47 | 0.074 |
| Race/Ethnicity | |||
| African American vs Caucasian | 7.41 | 1.81 | <0.001 |
| Other Ethnicity vs Caucasian | −5.42 | 1.93 | 0.005 |
| Multiracial vs Caucasian | −0.93 | 2.55 | 0.715 |
| Income | 0.56 | 0.19 | 0.004 |
| Education | 1.49 | 0.44 | 0.001 |
| Age | 0.10 | 0.04 | 0.012 |
| Female vs Male | −0.59 | 1.05 | 0.576 |
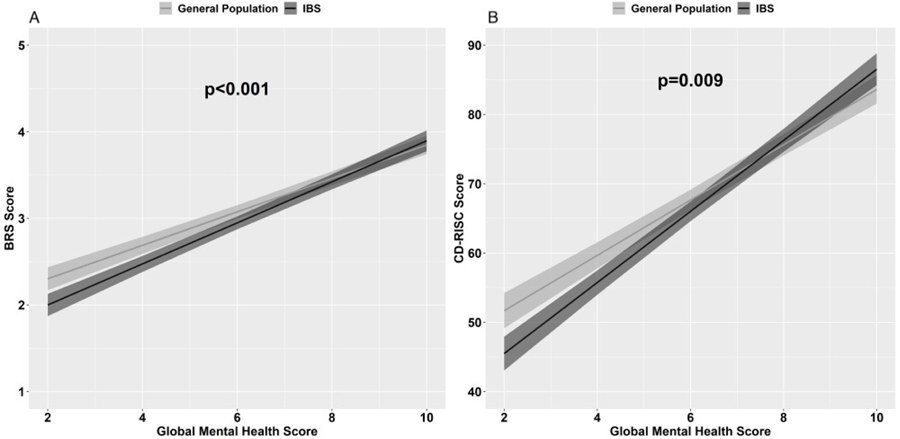
Association of global physical and mental health with resilience
Overall, higher global mental and physical health were associated with increased resilience as measured by the two resilience measures (p<0.001). Global mental health scores moderated the effect of IBS status on CD-RISC (p<0.001) and BRS (p=0.009) scores. Among those with a lower global mental health score, the IBS group had lower resilience compared to the general population group (Figure 2). Global physical health scores did not moderate the effect of IBS status on the resilience measures.
Figure 2:
Effect of global mental health on resilience as measured by A) BRS and B) CD-RISC. Among those with low global mental health scores, subjects in the general population had higher resilience compared to IBS subjects.
Association of early life adversity with resilience in IBS and the general population
Overall, a history of EALs was associated with decreased BRS scores (β=−0.060, 95% CI [−0.080, −0.040], p<0.001) but not CD-RISC scores. The presence of EALs did not moderate the effect of IBS status on either BRS or CD-RISC scores.
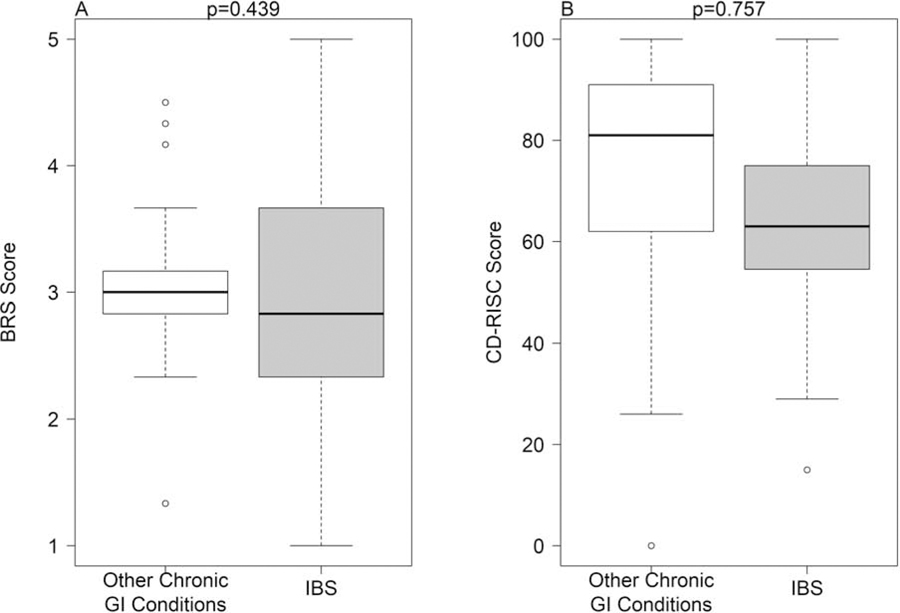
Resilience in IBS vs. those with other chronic GI conditions
Ninety-five participants had a self-reported diagnosis of a non-IBS chronic GI condition (21 ulcerative colitis, 15 Crohn’s disease, 17 celiac, 13 microscopic colitis and 29 with overlap of at least two of these conditions) and were matched for age and sex to 95 IBS participants. IBS did not have significantly different resilience compared to those with other chronic GI conditions as measured by BRS and CD-RISC (Figure 3).
Figure 3:
Resilience is similar in IBS (n=95) vs. other chronic GI conditions (n=95) as measured by A) BRS and B) CD-RISC.
Discussion
This study examines various components and determinants of resilience in a large population of IBS subjects compared to the general U.S. population and, in an exploratory analysis, to patients with other chronic GI conditions. The major findings of this study include: 1) overall resilience is lower in IBS subjects compared to the general population; 2) lower resilience was associated with worse IBS symptom severity; 3) different demographic factors affect resilience in similar ways in IBS and the general population; 4) decreased resilience was associated with lower global mental health to a greater degree in IBS vs the general population; 5) a history of more EALs was associated with decreased ability to bounce back in both IBS and the general population; and 6) IBS subjects have similar resilience as those with other chronic GI conditions that present with similar symptoms.
Our previous finding of lower resilience in a community sample of IBS and healthy subjects6 was confirmed in this larger study conducted in a general U.S. population sample. The use of two different resilience measures allowed for a deeper understanding of how certain demographic factors and clinical traits can affect the components of resilience differently. As an example, the ability to adapt, return to equilibrium, having a sense of control and self-efficacy are components of resilience that were associated with global mental health scores in this study. Whereas, those with higher numbers of EALs had a decreased ability to bounce back from adversity specifically. Thus, if one were to develop a therapeutic intervention that targets resilience in IBS, there should be a focus on improving the ability to bounce back in those with EALs. On the other hand, in those with lower mental health scores in the absence of EALs, an intervention that has more of a focus on self-efficacy and adaptability may be more beneficial. In addition, we need to recognize that there are demographic factors that can affect the resilience of an individual in general and may ultimately impact response to potential therapeutic interventions designed to target resilience.
EALs have been associated with altered resilience22 and chronic diseases including IBS13. In a study of the general population in Germany, those who reported more EALs and had low resilience demonstrated more somatic symptoms and higher levels of distress. Thus, the presence of higher levels of resilience served as a protective factor against somatic symptoms and distress even in those with EALs.22 These data are mirrored in the results from the current study where a history of EALs decreased the ability to bounce back from adversity regardless of IBS status. Based on this, altered resilience may offer an explanation as to why some individuals who experience early life adversity develop chronic medical conditions and negative health behaviors, while others do not. It is conceivable that the presence of higher levels of resilience may be protective against the development of stress-sensitive disorders, such as IBS, in individuals exposed to early life adversity. Biologic correlates of both EALs and decreased resilience include a dysregulated hypothalamic-pituitary-adrenal (HPA) axis stress response and compromised corticolimbic inhibition enhancing stress and emotional responses, which are thought to play pathophysiologic roles in IBS.13, 23, 24, 25
In the current study, the general population does not represent a completely ‘healthy’ control group. Despite this, IBS respondents demonstrated lower resilience compared to this group which could include those with other chronic medical conditions like cardiovascular disease, metabolic disorders, other chronic pain conditions, etc. This suggests that decreased resilience maybe a characteristic of IBS specifically. However, in our exploratory analysis comparing IBS with other chronic GI conditions that present with similar symptoms there was no difference in overall resilience. This suggests that the presence of chronic GI symptoms may relate to lower resilience scores. It remains unclear whether the presence of chronic GI symptoms contribute to lower levels of resilience or whether having low resilience causes pervasive and more severe symptoms in chronic GI conditions. To our knowledge, this is the first study to measure resilience in both IBS and chronic GI disease patients in a large U.S. population sample. However, caution should be taken in interpreting these results due to the relatively small sample size of participants with chronic GI conditons in our study. Larger, well-characterized patient populations are needed to confirm these findings. Future studies could determine if resilience is altered in patients with persistent GI symptoms despite adequate control of their underlying disease (e.g., in patients with IBD-IBS overlap).
Given the association of lower resilience with worse IBS symptom severity seen in this study, one could hypothesize that this could be a therapeutic target in patients with IBS. Resilience as a treatment target to improve outcomes has been previously studied in various mental and physical health conditions. Previous studies have demonstrated that resiliency training programs can improve an individual’s resilience in various medical conditions, high stress occupations, and college students undergoing academic stress.26,27 Resilience training programs based on mindfulness-based stress reduction and/or cognitive behavioral therapy (CBT) have a moderately positive effect in improving resilience. Although these behavioral therapies have been shown to be efficacious in IBS28–31, studies examining a specific resilience intervention in IBS are currently lacking. A recent, relatively small study, showed that gut-directed hypnotherapy, a well-recognized efficacious treatment for IBS32, improved resilience scores, IBS symptom severity and quality of life vs untreated IBS patients.33 However, it remains unknown if targeting resilience can improve objective outcomes in patients with IBS.
Strengths of this study are the large general population and IBS samples, novelty of data, use of validated questionnaires measuring the various components of resilience, use of validated diagnostic criteria for IBS, and comparison of IBS to both the general population and other chronic GI disorders which present with similar symptoms. Limitations include that the diagnosis of IBS and other chronic GI diseases could not be verified by an experienced clinician with expertise in the field or diagnostic testing given the design of this study, but we did survey for physician diagnosed disease rather than a self-reported or assumed diagnosis. Interpretation of the data comparing IBS and other chronic GI conditions is limited due to lack of information regarding the severity of disease or medication use for these conditions. In addition, the general population group may contain patients with IBS-IBD overlap. This is a relatively small group given the large sample size in this study and thus is unlikely to affect the results. It was felt to be more important to remove potential symptomatic mimics from the IBS group for this analysis. There may be evidence of selection bias in the general population group. This is evident in the fact that there is a higher proportion of individuals with IBD and microscopic colitis than would be expected in the general population. This remains a relative small proportion of respondants and is thus unlikely to affect the results. In addition, as this was an online survey, this may have affected obtaining a truly nationally representative sample in that it was only accessible to those with computer access. Finally, although we utilized several well validated measures of resilience, our operational definition of resilience is limited to those obtained from patient’s self-report. This did not allow us to address resilience as defined by other biological (i.e., HPA axis stress response) or behavioral (i.e., health care seeking behaviors) measures.
In summary, this study demonstrates that resilience is lower in those with IBS compared to the general U.S. population. Though resilience is often considered a trait, many aspects of the resilience construct can be dynamic throughout a lifetime. Targeting resilience may be an important and clinically meaningful outcome in IBS treatment trials. Longitudinal studies are needed to address whether improving resilience in IBS patients ultimately improves other objective outcome measures such as frequency of IBS symptom flares and healthcare resource utilization.
Supplementary Material
Supplementary Figure 1: Participant flow diagram
What You Need to Know.
Background
Resilience is the ability to recover from and adapt to stress and adversity.
Resilience is decreased in select IBS patients compared to healthy controls and is associated with worse symptom severity and poorer quality of life but has not been studied in the general U.S. population.
Findings
Resilience is decreased in individuals with IBS compared to the general U.S. population.
Lower resilience is associated with worse IBS symptom severity.
IBS and patients with other chronic GI conditions that present with similar symptoms have similar levels of resilience.
Implications for Patient Care
Resilience may serve as a therapeutic target in the management of chronic GI conditions including IBS.
Acknowledgements:
The research staff of the G. Oppenheimer Center for Neurobiology of Stress and Resilience, University of California Los Angeles.
Financial Support
The study was in part supported by NIH grant P30 DK041301.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Potential Competing Interests
CHP- None; BDN- None; WS- None; APP- None; LK-None; AG-None; CL-None; LAK-None; JSS- None; RH-None; BES-None; LC- None
References
- 1.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 2003;18:76–82. [DOI] [PubMed] [Google Scholar]
- 2.Luthar SS, Cicchetti D, Becker B. The construct of resilience: A critical evaluation and guidelines for future work. Child Development 2000;71:543–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith BW, Dalen J, Wiggins K, et al. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med 2008;15:194–200. [DOI] [PubMed] [Google Scholar]
- 4.McAllister SJ, Vincent A, Hassett AL, et al. Psychological resilience, affective mechanisms, and symptom burden in a tertiary care sample of patients with fibromyalgia. Stress Health 2015;31:299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Min JA, Jung YE, Kim DJ, et al. Characteristics associated with low resilience in patients with depression and/or anxiety disorders. Qual Life Res 2013;22:231–41. [DOI] [PubMed] [Google Scholar]
- 6.Park SH, Naliboff BD, Shih W, et al. Resilience is decreased in irritable bowel syndrome and associated with symptoms and cortisol response. Neurogastroenterol Motil 2018;30:e13155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fischer S, Lemmer G, Gollwitzer M, et al. Stress and resilience in functional somatic syndromes--a structural equation modeling approach. PLoS One 2014;9:e111214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health and Quality of Life Outcomes 2011;9:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pangallo A, Zibarras L, Lewis R, et al. Resilience through the lens of interactionism: a systematic review. Psychol Assess 2015;27:1–20. [DOI] [PubMed] [Google Scholar]
- 10.Maltby J, Day L, Hall S. Refining trait resilience: Identifying engineering, ecological, and adaptive facets from extant measures of resilience. PLoS One 2015;10:e0131826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterol 2016;150:1393–1407. [DOI] [PubMed] [Google Scholar]
- 12.Bradford K, Shih W, Videlock EJ, et al. Association between early adverse life events and irritable bowel syndrome. Clin Gastroenterol Hepatol 2012;10:385–90 e1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park SH, Videlock EJ, Shih W, et al. Adverse childhood experiences are associated with irritable bowel syndrome and gastrointestinal symptom severity. Neurogastroenterol Motil 2016;28:1252–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carlsen K, Haddad N, Gordon J, et al. Self-efficacy and resilience are useful predictors of transition readiness scores in adolescents with inflammatory bowel diseases. Inflamm Bowel Dis 2017;23:341–346. [DOI] [PubMed] [Google Scholar]
- 15.Melinder C, Hiyoshi A, Fall K, et al. Stress resilience and the risk of inflammatory bowel disease: a cohort study of men living in Sweden. BMJ Open 2017;7:e014315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kilpatrick LA, Gupta A, Love AD, et al. Neurobiology of psychological resilience in irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) patients. Gastroenterol 2015;148. [Google Scholar]
- 17.Spiegel B, Hays RD, Bolus R, et al. Development of the NIH Patient-Reported Outcomes Measurement Information System (PROMIS) gastrointestinal symptom scales. Am J Gastroenterol 2014;109:1804–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hays RD, Bjorner JB, Revicki DA, et al. Development of physical and mental health summary scores from the Patient-Reported Outcomes Measurement Information System (PROMIS) global items. Qual Life Res 2009;18:873–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. American Journal of Preventive Medicine;14:245–258. [DOI] [PubMed] [Google Scholar]
- 20.Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Alimentary Pharmacology and Therapeutics 1997;11:395–402. [DOI] [PubMed] [Google Scholar]
- 21.Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterol 2006;130:1480–91. [DOI] [PubMed] [Google Scholar]
- 22.Beutel ME, Tibubos AN, Klein EM, et al. Childhood adversities and distress - The role of resilience in a representative sample. PLoS One 2017;12:e0173826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Videlock EJ, Adeyemo M, Licudine A, et al. Childhood trauma is associated with hypothalamic-pituitary-adrenal axis responsiveness in irritable bowel syndrome. Gastroenterol 2009;137:1954–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta A, Mayer EA, Acosta JR, et al. Early adverse life events are associated with altered brain network architecture in a sex-dependent manner. Neurobiol Stress 2017;7:16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gupta A, Love A, Kilpatrick LA, et al. Morphological brain measures of cortico-limbic inhibition related to resilience. J Neurosci Res 2017;95:1760–1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Joyce S, Shand F, Tighe J, et al. Road to resilience: a systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open 2018;8:e017858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dolbier C, Steinhardt M. Evaluation of a resilience intervention to enhance coping strategies and protective factors and decrease symptomatology. J Am Coll Health 2008;56:445–453. [DOI] [PubMed] [Google Scholar]
- 28.Lackner JM, Jaccard J, Keefer L, et al. Improvement in gastrointestinal symptoms after cognitive behavior therapy for refractory irritable bowel syndrome. Gastroenterol 2018;155:47–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gaylord SA, Palsson OS, Garland EL, et al. Mindfulness training reduces the severity of irritable bowel syndrome in women: results of a randomized controlled trial. Am J Gastroenterol 2011;106:1678–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ford AC, Quigley EM, Lacy BE, et al. Effect of antidepressants and psychological therapies, including hypnotherapy, in irritable bowel syndrome: systematic review and meta-analysis. Am J Gastroenterol 2014;109:1350–1365. [DOI] [PubMed] [Google Scholar]
- 31.Keefer L, Palsson OS, Pandolfino JE. Best Practice Update: Incorporating Psychogastroenterology Into Management of Digestive Disorders. Gastroenterol 2018;154:1249–1257. [DOI] [PubMed] [Google Scholar]
- 32.Ford AC, Moayyedi P, Chey WD, et al. American College of Gastroenterology monograph on management of irritable bowel syndrome. Am J Gastroenterol 2018;113:1–18. [DOI] [PubMed] [Google Scholar]
- 33.Peter J, Tran US, Michalski M, et al. The structure of resilience in irritable bowel syndrome and its improvement through hypnotherapy: Cross-sectional and prosepctive longitudinal data. PLoS One 2018;13:e0202538. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1: Participant flow diagram