Abstract
Given links between stress and obesity, it is likely that individuals gained weight during the COVID-19 lockdown. Research suggests that religiosity facilitates coping, which may have lessened the relationship between stress and weight gain during the COVID-19 lockdown. We examined this relationship among Orthodox Jews (n = 731). Results indicated that stress was marginally associated with weight gain, and that this was moderated by intrinsic religiosity (IR). For those with low IR, stress correlated with weight gain, while for those with mean or higher IR, stress and weight change were unrelated. Results suggest that for some, religiosity may moderate links between stress and weight gain during times of crisis.
Keywords: Stress, Obesity, Religion, Pandemic
Introduction
Research consistently links stress and obesity (Moore and Cunningham 2012) including prospective studies suggesting that stress can cause obesity over time (Wardle et al. 2011). Various explanations for this link have been offered, and a recent integrative review by Tomiyama (2019) suggests three primary pathways. First, stress interferes with the self-regulatory processes associated with eating and physical activity (Liston et al. 2009; Pechtel and Pizzagalli 2011). Second, as corroborated by experimental research in humans and animals, stress leads to increased eating (Pecoraro et al. 2004), reduced physical activity (Mouchacca et al. 2013), and less sleep (Åkerstedt et al. 2007), all three of which are tied to weight gain (Patel and Hu 2008). Third, stress reliably activates several physiological systems strongly related to food consumption and weight regulation (Tomiyama 2019). Given the direct and indirect stressors associated with the COVID-19 pandemic (Taylor et al. 2020), it is likely that for many, stress and weight increased during this period.
On the other hand, it is well established that for many individuals, religion, which has been defined as the search for significance occurring within established contexts designed to facilitate spirituality (Pargament 1997), can provide comfort, support, and hope in times of distress through a variety of cognitive, emotional, and behavioral mechanisms (Rosmarin and Koenig 2020). In fact, the link between intrinsic religiosity (IR) and psychological wellbeing is one of the most robustly supported findings regarding religion and mental health (Hill and Pargament 2003; Koenig et al. 2012; Smith et al. 2003). IR involves a deep internal value of religion and refers to the degree to which religiosity provides an overall framework and a primary motivation in life, and measures of IR are strongly correlated with a variety of positive psychological outcomes. While the mediating processes for these effects are likely multifaceted and have yet to be fully explored, previous research suggests that some strong possibilities such as by providing a source for positive reappraisals (e.g., “Everything God does is for the good”), activating and meaningful activities such as prayer and religious study, and emotional support through a connection with a loving God (Rosmarin and Leidl 2020). These effects may be most apparent at times of stress, since IR provides latent adaptive resources that can be drawn on to buffer connections between stress and negative outcomes (Smith et al. 2003). Consistent with this idea, a large body of previous research suggests that religion and spirituality relate to better outcomes in the context of disaster (Aten et al. 2019). These effects may be particularly evident among the highly religious such as Orthodox Jews.
Orthodox Judaism is a broad categorization that includes numerous diverse religious cultures all of which subscribe to the Divine origins of the Torah and Talmudic interpretations of it (Encyclopedia Britannica 2014). Although there is a range in culture and practice among subgroups, all Orthodox Jews largely adhere to religious laws and customs, which fill everyday life with a sense of purpose and meaning. COVID-19 and the public health directives issued had a significant impact on regular aspects of Jewish religious practice (e.g., ritual baths, communal prayer, marriage ceremonies, and circumcision). Furthermore, stay-at-home restrictions may have been particularly stressful for Orthodox Jews since their culture is collective, communal, and familial (Heilman 2000). In addition, more traditional Hasidic or Haredi communities tend to be composed of large families (Pirutinsky et al. 2015) of low socioeconomic status (Pearson and Geronimus 2011). The community’s resistance to smartphones and Internet access has posed unique challenges during the pandemic due to the widespread reliance on such technologies in the face of social distancing conditions. Finally, conspiracy theories concerning COVID-19 have targeted Jews, echoing old libels related to past pandemics (e.g., Cohen and Hill 2007), and anti-Semitic incidents have increased 18% since the outbreak (Heller 2020) leading to another potential source of stress. Despite these unique stressors, our research has identified that religious factors can be beneficial within this religious-cultural group, particularly during times of high stress (Pirutinsky et al. 2020).
Accordingly, this research examined the relationship between perceived stress and weight change during the COVID-19 pandemic among Orthodox Jews. Following the ideas presented above, we hypothesized that (1) overall perceived COVID-19 related stress would correlate with weight gain and (2) IR would buffer against these effects.
Methods
Participants and Procedure
Using email lists and web sites of Jewish organizations, social media, and snowball approaches, we recruited for a “Research Study on Jewish Community Responses to COVID-19.” The study was approved by the Institutional Review Board for Human Subject Research at Touro College, New York. Prospective participants were directed toward an anonymous online survey that included the study questionnaire, which assessed for demographics, COVID-19 risk factors, attitudes and behaviors, various facets of religion and spirituality, and several indices of mental health and wellbeing. The current study focused specifically on weight change, stress, and intrinsic religiosity. Data collection took place during the initial peak of the epidemic in the USA from March 30, 2020, until May 14, 2020. By March 30, there had been approximately 162,707 confirmed cases and 4381 deaths in the USA, counts which rose to 1,423,727 confirmed cases and 87,008 deaths by May 14, 2020 (Johns Hopkins University and Medicine 2020).
Of the 1779 participants who had completed the survey, 983 met criteria for the current study as they identified with an Orthodox Jewish religious affiliation and reported living in the USA. Of these, we excluded 252 participants reporting recent infection with COVID-19, since physical illness was likely to affect weight. Participants in the resulting sample (n = 731) were mostly female (66%), ranged in age from 18 to 89 (M = 40.59, SD = 16.79), and most were married (73%) or single/never-married (22%). Reported ethnicity was largely white (93%), and most were college educated (91%). Specific Orthodox affiliations included Hassidic (5%), Chabad/Lubavitch (2%), Yeshiva Orthodox (46%), Modern Orthodox (37%), and Sephardic-Religious (2%). Of these, 64% reported residing in the NY/NJ region, which is home to a large Orthodox Jewish population (Pew Research Center 2013, 2017). Notably, these regions were hit particularly hard during the initial wave of COVID-19 (Centers for Disease Control 2020). Finally, missing data were handled via pairwise deletion yielding slightly differing sample sizes for particular analyses.
Measures
All variables were measured using self-report questionnaires. Weight change was measured using a single item presented within a larger health related questionnaire. It read: “Approximately how much weight have you gained/lost in pounds since the start of the COVID-19 crisis?” Stress was measured using the short form of the Perceived Stress Scale (Warttig et al. 2013), which consists of four items such as “how often have you felt that you were unable to control the important things in your life?” and “how often have you felt difficulties were piling up so high that you could not overcome them?” and is scored on a five-point scale. Internal reliability in the sample was adequate (a = .70). Intrinsic religiosity (IR) was measured using the three-item subscale from the Duke Religion Index (Koenig et al. 1997). These items read: ‘‘my religious beliefs are what really lie behind my whole approach to life,” ‘‘in my life, I experience the presence of the Divine (i.e., God),” and ‘‘I try hard to carry my religion over into all other dealings in life.’’ These were rated on a five-point scale ranging from ‘‘definitely not true’’ to ‘‘definitely true,’’ and internal reliability in the sample was high (a = .86).
Results
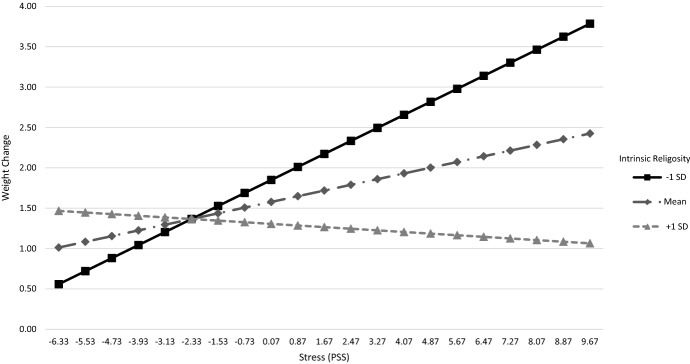
Correlations between study variables indicated that self-reported weight change correlated with perceived stress (r(658) = .08, p = .05) and with IR (r(690) = − .07, p = .06), whereas IR significantly correlated with lower self-reported stress (r(687) = − .13, p = .003). As described above, we hypothesized that those reporting higher stress during the study period would report more weight gain, and that this would be moderated by IR. We tested this using linear regression, all variables were mean centered prior to being entered, and analysis was conducted using SPSS 25. Model 1 included main effects of both stress and IR, and results indicated that they jointly predicted a small but significant proportion of the variance in weight change (∆r2 = .01, f(2, 653) = 3.37, p = .035). However, controlling for each other, both stress (b = .10, se = .06, t = 1.76, p = .08, 95%CI [− .01, .21]) and IR (b = − .10, se = .06, t = 1.70, p = .09, 95%CI [− .23, .02]) were each only marginally related to weight change. Model 2 added an interaction term between stress and IR, and results indicated that this explained a small but significant additional portion of variance (∆r2 = .01, f(1, 652) = 5.21, p = .02). These results were then graphed (Fig. 1) and probed using the Indirect macro (Preacher and Hayes 2004), which calculated conditional effects for the relationship between stress and weight gain at 3 levels of IR. Results indicated that for those with IR at 1 SD below the mean, stress was significantly correlated with increased weight gain (b = .20, se = .07, t = 2.81, p = .005, 95%CI [.06, .34]), while for those with mean levels of IR (b = .09, se = .06, t =.11, p = .20, 95%CI [− .02, .20]) and IR at 1 SD above the mean (b = − .03, se = .08, t = .32, p = .75, 95%CI [− .18, .13]) stress was unrelated to weight gain.
Fig. 1.
Moderation effect of IR on the relationship between stress and weight change
Discussion
In this study, we hypothesized that perceived stress in the context of COVID-19 would correlate with weight gain, and that IR would moderate or “buffer” this effect. Results indicated that overall in the sample, stress marginally correlated with weight gain and furthermore, as hypothesized, this was significantly moderated by IR. For those low in IR, higher stress correlated with more weight gain, while for those with mean or higher IR, stress and weight change were unrelated. These results have several incremental implications. First, they support the connection between stress and weight gain in a naturalistic religious-cultural community sample during a pandemic. Second, they provide additional evidence to the extant literature, suggesting that religious coping can moderate the impact of stress on behavioral health outcomes. Third, they extend findings regarding religion and mental health to Orthodox Jews who are underrepresented in such research (Rosmarin et al. 2017). Finally, they more broadly suggest that religiosity may promote better health in the face of overwhelming crises, such as COVID-19.
So why might IR buffer against stress effects on weight gain? Previous research and theory suggests several possibilities. First, as discussed above, stress reduces self-regulation, which in turn reduces the ability to monitor and inhibit eating. Previous research links religiosity to increased self-control (McCullough and Willoughby 2009) including prospective (Pirutinsky 2014) and experimental studies (Rounding et al. 2012). Accordingly, IR may buffer the effects of stress by increasing self-control and improving the regulation of consumption. Second, for those with high IR, religion is a “master motive” providing a highly salient meaning system, which previous research suggests lessens the impact of stress, trauma, and even physical pain (Dezutter et al. 2010). Finally, many methods of religious coping involve turning one’s attention away from emotional responses and focusing instead on S/R (Pargament 1997). Thus, IR may provide a source of internal and external stimuli that shift attention from eating cues to values-based thoughts and activities (Pirutinsky 2020).
On the other hand, this study had several limitations. It relied exclusively on self-report measures, although self-reported weight generally accords with weight measured objectively in adults (Spencer et al. 2002). In addition, the question regarding weight gain asked about gain since the start of the pandemic and that period of time may have varied slightly between subjects. Furthermore, this study exclusively focused on Orthodox Jews, who according to Pew Research Center (2017) account for about 10% of American Jewry, which limits the generalizability of the results to other religious cultures (Cohen and Hill 2007; Cohen 2009), as research suggests that the relationship between religion and health is stronger within religious cultures (Saroglou and Cohen 2013) and Orthodox Jewish culture is highly religious in terms of beliefs, behaviors, and the social environment (Pirutinsky 2009). Finally, it did not measure the various possible mediating factors that explain the connection between IR and reduced weight gain among those highly stressed. Despite these limitations, our findings further substantiate the link between stress and weight gain and highlight potentially salubrious religious factors for coping and health behaviors.
Compliance with ethical standards
Conflict of interest
The authors declare that they complied this research complied with the Ethical Standards of the Journal of Religion and Health, that they had no conflicts of interest, and that they did not receive any external funding for this study. Financial support was received from McLean Hospital development fund #041537.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Aten JD, Smith WR, Davis EB, Van Tongeren DR, Hook JN, Davis DE, Shannonhouse L, DeBlaere C, Ranter J, O'Grady K, Hill PC. The psychological study of religion and spirituality in a disaster context: A systematic review. Psychological Trauma: Theory, Research, Practice, and Policy. 2019;11(6):597–613. doi: 10.1037/tra0000431. [DOI] [PubMed] [Google Scholar]
- Åkerstedt T, Kecklund G, Gillberg M. Sleep and sleepiness in relation to stress and displaced work hours. Physiology and Behavior. 2007;92(1–2):250–255. doi: 10.1016/j.physbeh.2007.05.044. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. (2020). Cases of coronavirus disease (COVID-19) in the U.S. Retrieved April 22, 2020 from https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
- Cohen AB. Many forms of culture. American Psychologist. 2009;64:194–204. doi: 10.1037/a0015308. [DOI] [PubMed] [Google Scholar]
- Cohen AB, Hill PC. Religion as culture: Religious individualism and collectivism among American Catholics, Jews, and Protestants. Journal of Personality. 2007;75:709–742. doi: 10.1111/j.1467-6494.2007.00454.x. [DOI] [PubMed] [Google Scholar]
- Dezutter J, Robertson LA, Luyckx K, Hutsebaut D. Life satisfaction in chronic pain patients: The stress-buffering role of the centrality of religion. Journal for the Scientific Study of Religion. 2010;49:507–516. doi: 10.1111/j.1468-5906.2010.01525.x. [DOI] [PubMed] [Google Scholar]
- Encyclopædia Britannica. (2014). Orthodox Judaism. Encyclopædia Britannica. Retrieved October 22, 2020 from https://www.britannica.com/topic/Orthodox-Judaism.
- Heilman SC. Defenders of the faith: Inside ultra-orthodox Jewry. Berkeley: University of California Press; 2000. [Google Scholar]
- Heller, J. (April 20, 2020). Coronavirus crisis stoking anti-Semitism worldwide: Report. Reuters. Retrieved October 22, 2020 from https://www.reuters.com/article/us-health-coronavirus-israel-antisemitis/coronavirus-crisis-stoking-anti-semitism-worldwide-report-idUSKBN22219C.
- Hill PC, Pargament KI. Advances in the conceptualization and measurement of religion and spirituality: Implications for physical and mental health research. American Psychologist. 2003;58(1):64–74. doi: 10.1037/0003-066X.58.1.64. [DOI] [PubMed] [Google Scholar]
- Johns Hopkins University and Medicine. (2020, April 29). Cumulative cases by date [Infographic]. Johns Hopkins University and Medicine Coronavirus Resource Center. Retrieved October 22, 2020 from https://coronavirus.jhu.edu/data/cumulative-cases.
- Koenig HG, King DE, Carson VB. Handbook of religion and health. 2. Oxford: Oxford University Press; 2012. [Google Scholar]
- Koenig H, Patterson G, Meador K. Religion Index for psychiatric research: A 5-item measure for use in health outcomes studies. American Journal of Psychiatry. 1997;154:885–866. doi: 10.1176/ajp.154.6.885b. [DOI] [PubMed] [Google Scholar]
- Liston C, McEwen BS, Casey BJ. Psychosocial stress reversibly disrupts prefrontal processing and attentional control. Proceedings of the National Academy of Sciences. 2009;106(3):912–917. doi: 10.1073/pnas.0807041106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore CJ, Cunningham SA. Social position, psychological stress, and obesity: A systematic review. Journal of the Academy of Nutrition and Dietetics. 2012;112(4):518–526. doi: 10.1016/j.jand.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Mouchacca J, Abbott GR, Ball K. Associations between psychological stress, eating, physical activity, sedentary behaviours and body weight among women: A longitudinal study. BMC Public Health. 2013;13(1):828. doi: 10.1186/1471-2458-13-828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pargament K. The psychology of religion and coping. New York: Guilford Press; 1997. [Google Scholar]
- Patel SR, Hu FB. Short sleep duration and weight gain: A systematic review. Obesity. 2008;16(3):643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearson JA, Geronimus AT. Race/ethnicity, socioeconomic characteristics, coethnic social ties, and health: Evidence from the national Jewish population survey. American Journal of Public Health. 2011;101(7):1314–1321. doi: 10.2105/AJPH.2009.190462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pechtel P, Pizzagalli DA. Effects of early life stress on cognitive and affective function: An integrated review of human literature. Psychopharmacology. 2011;214(1):55–70. doi: 10.1007/s00213-010-2009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pecoraro N, Reyes F, Gomez F, Bhargava A, Dallman MF. Chronic stress promotes palatable feeding, which reduces signs of stress: Feedforward and feedback effects of chronic stress. Endocrinology. 2004;145(8):3754–3762. doi: 10.1210/en.2004-0305. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. (2013). A portrait of Jewish Americans. Findings from a Pew Research Center survey of U.S. Jews. Washington, D.C. Retrieved October 22, 2020 from http://www.pewforum.org/2013/10/01/jewish-american-beliefs-attitudes-culture-survey.
- Pew Research Center. (2017). A portrait of American Orthodox Jews: A further analysis of the 2013 survey of US Jews. Washington, D.C. Retrieved October 22, 2020 from https://www.pewforum.org/2015/08/26/a-portrait-of-american-orthodox-jews/.
- Pine DS, Goldstein RB, Wolk S, Weissman MM. The association between childhood depression and adulthood body mass index. Pediatrics. 2001;107(5):1049–1056. doi: 10.1542/peds.107.5.1049. [DOI] [PubMed] [Google Scholar]
- Pirutinsky S. The terror management function of Orthodox Jewish religiosity: A religious culture approach. Mental Health, Religion and Culture. 2009;12(3):247–256. doi: 10.1080/13674670802455756. [DOI] [Google Scholar]
- Pirutinsky S. Does religiousness increase self-control and reduce criminal behavior? A longitudinal analysis of adolescent offenders. Criminal Justice and Behavior. 2014;41:1290–1307. doi: 10.1177/0093854814531962. [DOI] [Google Scholar]
- Pirutinsky, S. (2020). Attentional biases and religious coping. Manuscript submitted for publication.
- Pirutinsky S, Cherniak AD, Rosmarin DH. COVID-19, mental health, and religious coping among American Orthodox Jews. Journal of Religion and Health. 2020;59:2288–2301. doi: 10.1007/s10943-020-01070-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirutinsky S, Schechter I, Kor A, Rosmarin D. Family size and psychological functioning in the Orthodox Jewish community. Mental Health, Religion and Culture. 2015;18(3):218–230. doi: 10.1080/13674676.2015.1042851. [DOI] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, and Computers. 2004;36:717–731. doi: 10.3758/BF03206553. [DOI] [PubMed] [Google Scholar]
- Rounding K, Lee A, Jacobson JA, Ji LJ. Religion replenishes self-control. Psychological Science. 2012;23:635–642. doi: 10.1177/0956797611431987. [DOI] [PubMed] [Google Scholar]
- Rosmarin DH, Koenig HG, editors. Handbook of religion and mental health. Amsterdam: Elsevier; 2020. [Google Scholar]
- Rosmarin DH, Leidl B. Spirituality, religion, and anxiety disorders. In: Rosmarin DH, Koenig HG, editors. Handbook of spirituality, religion, and mental health. Amsterdam: Elsevier; 2020. pp. 41–60. [Google Scholar]
- Rosmarin DH, Pirutinsky S, Carp S, Appel M, Kor A. Religious coping across a spectrum of religious involvement among Jews. Psychology of Religion and Spirituality. 2017;9(Suppl 1):S96–S104. doi: 10.1037/rel0000114. [DOI] [Google Scholar]
- Saroglou V, Cohen AB. Cultural and cross-cultural psychology of religion. In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. New York: Guilford Press; 2013. pp. 330–354. [Google Scholar]
- Smith TB, McCullough ME, Poll J. Religiousness and depression: evidence for a main effect and the moderating influence of stressful life events. Psychological Bulletin. 2003;129(4):614–636. doi: 10.1037/0033-2909.129.4.614. [DOI] [PubMed] [Google Scholar]
- Spencer EA, Appleby PN, Davey GK, Key TJ. Validity of self-reported height and weight in 4808 EPIC–Oxford participants. Public Health Nutrition. 2002;5(4):561–565. doi: 10.1079/PHN2001322. [DOI] [PubMed] [Google Scholar]
- Taylor S, Landry CA, Paluszek MM, Fergus TA, McKay D, Asmundson GJ. COVID stress syndrome: Concept, structure, and correlates. Depression and Anxiety. 2020;37(8):706–714. doi: 10.1002/da.23071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomiyama AJ. Stress and obesity. Annual Review of Psychology. 2019;70:703–718. doi: 10.1146/annurev-psych-010418-102936. [DOI] [PubMed] [Google Scholar]
- Wardle J, Chida Y, Gibson EL, Whitaker KL, Steptoe A. Stress and adiposity: A meta-analysis of longitudinal studies. Obesity. 2011;19(4):771–778. doi: 10.1038/oby.2010.241. [DOI] [PubMed] [Google Scholar]
- Warttig SL, Forshaw MJ, South J, White AK. New, normative, English-sample data for the short form perceived stress scale (PSS-4) Journal of Health Psychology. 2013;18:1617–1628. doi: 10.1177/1359105313508346. [DOI] [PubMed] [Google Scholar]