This editorial refers to ‘Outdoor light at night and risk of coronary heart disease among older adults: a prospective cohort study’†, by S. Sun et al., on page 822.
Environmental triggers of the global burden of disease and deaths
The aim of exposome research is to characterize the impact of all environmental exposures during our entire life span on the biochemical systems in our body and their associated (mostly adverse) health effects.1 The need for exposome research is emphasized by health side effects caused by ambient chemical pollution (from soil, water, and air) leading to up to 13 million premature deaths worldwide, with a major part representing non-communicable diseases.2 However, these numbers do not take into account the impact of additional environmental stressors contributing significantly to the global burden of disease such as light exposure, mental stress, and the temperature.3 The leading role of air pollution [e.g. fine particulate matter, particles with a diameter <2.5 µm (PM2.5)] as an environmental health risk factor is well established, especially for causing cardiovascular disease including ischaemic heart disease and stroke, and by increasing mortality.4 , 5 There is also a growing body of evidence showing that noise, in particular transportation noise, represents an important environmental health risk factor, mainly by increasing the risk of cardiovascular, metabolic, and neuropsychological disease and thereby causing ∼1.6 million disability-adjusted life years in the Western European region.6 The adverse health effects of nocturnal light pollution are not very well characterized so far, highlighting the novelty of the work by Sun et al. published in this issue of the European Heart Journal.7 Within the next sections we will provide a short overview of the importance of light exposure at night as a potential health risk factor and try to elucidate its major mechanism of action. We will also critically evaluate the major messages of the current work by Sun et al. and discuss their societal impact.
Nocturnal light exposure causes sleep disturbances and stress responses
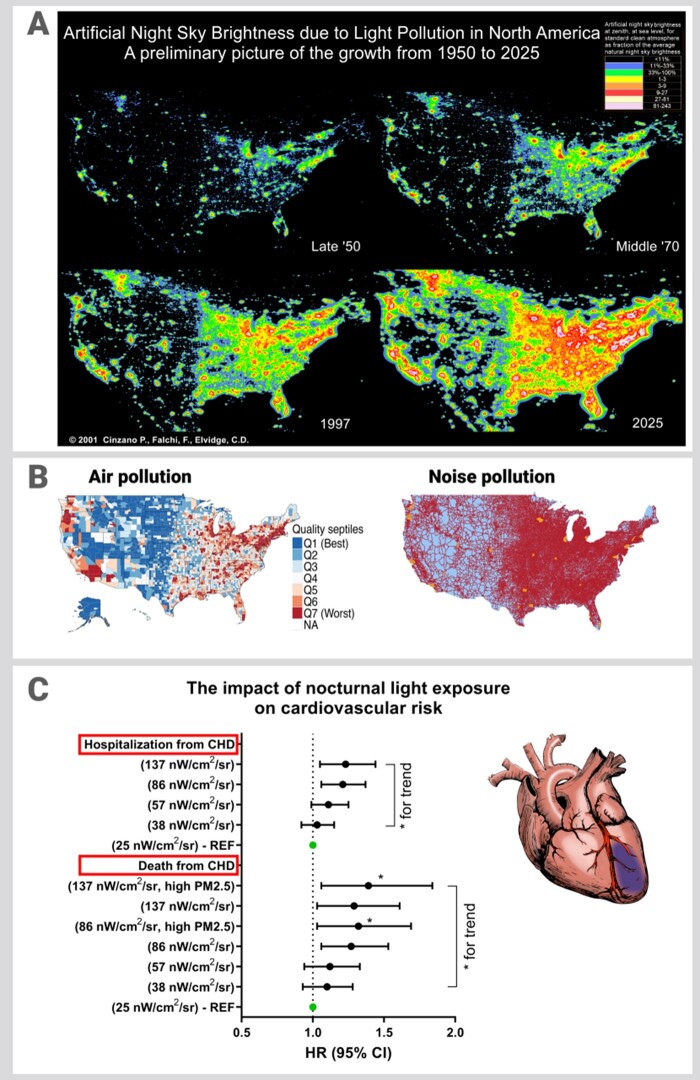
In his review article ‘Missing the dark – health effects of light pollution’ in 2009, Chepesiuk gives a historic overview on electrified illumination at night supplemented by worrisome satellite images of light pollution evolvement in the USA starting in the 1950s and ending with a projection for the year 2025 (Figure 1).8 The author explains in detail not only how light pollution evolves but also how it irritates animals (e.g. causing billions of deaths of birds due to collisions), disturbs our sleep, impairs our circadian rhythm, and thereby causes severe health effects such as cancer and cardiovascular disease, which are the subject of chronobiological studies. Bedrosian and Nelson reviewed in detail the impact of light exposure timing on brain function and mood.9 They conclude that disruption of circadian rhythm by night-time light dysregulates essential processes such as hormone secretion, cellular function, and gene expression, which is associated with higher risk of acquiring certain cancers, metabolic dysfunction, and mood disorders. A detailed perspective of nocturnal light pollution was also provided for the global level.10
Figure 1.
(A) Simulation of light pollution growth in the United States: 1950s, 1970s, 1990s, and projected to 2025. Calculated according to Cinzano in “Light Pollution: The Global View” (edited by H.E. Schwarz) and reused with permission by P. Cinzano, F. Falchi, C. D. Elvidge. © 2001 ISTIL- Light Pollution Science and Technology Institute, Italy. (B) Distribution of air pollution and road/aviation noise exposure levels shows a co-localization with light pollution in the USA. Air pollution map reused from Khan et al.15 © 2019 under the Creative Commons Attribution License. Noise pollution map was qualitatively approximated from United States Department of Transportation, Bureau of Transportation Statistics (https://maps.bts.dot.gov/arcgis/apps/webappviewer/index.html?id=a303ff5924c9474790464cc0e9d5c9fb). Red color = areas with higher noise exposure. Orange color = noise exposure hot spots. (C) Hazard ratio for light pollution-mediated coronary heart disease (hospitalization from CHD) and mortality (death from CHD). All conditions were adjusted by the most common confounders such as age, sex, and medication, but also social status and others. High particulate matter caused additive risk effects for CHD death but not CHD hospitalization. The graph was generated from tabular data from Sun et al.7 with permission.
It is very likely that the adverse health effects of nocturnal light pollution are mediated by similar pathomechanisms to those described for nocturnal traffic noise exposure.11 For example, sleep fragmentation and deprivation, followed by stress responses and dysregulation of circadian rhythm, may represent the major triggers of disease and mortality induced by nocturnal light pollution (Figure 1). In support of this assumption, a large cohort study in >265 000 participants revealed that outdoor light exposure at night increases the risk of depressive symptoms [odds ratio (OR) 1.29; 95% confidence interval (CI) 1.15–1.46] or suicidal behaviours (OR 1.27; 95% CI 1.16–1.39),12 thereby suggesting neurobiological changes caused by nocturnal light pollution. A small cohort study in 528 elderly Japanese participants observed an increase in systolic and diastolic blood pressure by 3.7% and 4.5% (4.3 and 3.0 mmHg), respectively, for a 5 lux [1 lux = 1 lumen/m2; 1 lumen is equivalent to ∼0.1 W (bulb) or 0.01 W (LED)] increase in outdoor light exposure at night.13 This systolic blood pressure increase of 4.3 mmHg may be translated to a 6.1% increase in total mortality (= 10 000 excess deaths per year) of Japanese people at higher age. In an animal study, constant illumination accelerated the onset of metabolic syndrome and spontaneous and chemically induced tumorigenesis, and shortened the life span in both male and female rats, all of which was prevented by administration of melatonin in the drinking water.14
Nocturnal outdoor light exposure increases the risk of coronary heart disease
The present study by Sun et al.7 analysed the association between outdoor light exposure at night and incident risk of coronary heart disease (CHD) and mortality in the elderly Hong Kong population (58 692 individuals). Over a follow-up time of 11 years, the authors enrolled 3772 CHD hospitalizations and 1695 CHD deaths. Outdoor illumination at night was obtained from satellite data with a precision of 1 km2. The authors revealed that after multivariable adjustment, light exposure at night [change of 60.0 nW/cm2/sr (units of radiance = watt per steradian per square metre] is associated with increased risk of these outcomes, with a hazard ratio of 1.11 (95% CI 1.03–1.18) for CHD hospitalizations and 1.10 (95% CI 1.00–1.22) for CHD deaths, with an overall monotonic exposure–response function. Moreover, sensitivity analyses indicated that these associations were stable. For high PM2.5 doses (yearly exposure to >7.3 μg/m3) there was an additive interaction effect on CHD mortality in the highest light pollution quintiles (86 and 137 nW/cm2/sr) with a hazard ratio of 1.32 and 1.39, respectively (Figure 1). Additionally, the authors assessed night-time road traffic noise levels (Lnight) at the residential address of each participant and were able to adjust for it throughout the analyses, confirming the robustness of the results. This is of special importance, since it was shown that participants in the highest light pollution quintiles (fourth quintile 72.0–106.5 nW/cm2/sr; fifth quintile, 106.5–233.1 nW/cm2/sr) were also exposed to the highest levels of PM2.5 and night-time traffic noise, indicating that these three environmental hazards may together be responsible for these adverse health effects.
Strengths and limitations of the study
Taken together, the present study by Sun et al. provides strong evidence that light at night may constitute a relevant contributor to increased risk of CHD. Importantly, this is the first study to prospectively examine the association between light at night and risk of CHD on the basis of a large, well-characterized cohort. The results were robust and remained significant even after adjustment for a wide range of individual and neighbourhood-level risk factors including air and noise pollution, with the latter described to exert adverse health effects by similar pathomechanisms to those proposed for light at night. Extensive sensitivity analyses were conducted to prove the stability of results from which emerged evidence that environmental hazards, i.e. light at night and air pollution, may act together to increase the risk of CHD mortality. However, some limitations and gaps should be considered. Since Hong Kong ranks among the most polluted areas in the world and the investigated sample represents an older Chinese population, the findings may have limited generalizability to other areas, ethnicities, and age groups. As disturbed sleep and dysregulated circadian rhythm are proposed to be among the key mechanisms by which light pollution increases risk of disease and mortality, a direct assessment of these variables (by, for example, sleep quality) would be highly beneficial. Exposure misclassification has most probably occurred since individuals with higher light exposure may be more likely to implement adaptive measures such as using light-blocking curtains; in this case a mismatch between outdoor and indoor light conditions would interfere with the results. In agreement with the analysis of the joint effects of light and air pollution, a more sophisticated approach in the case of noise exposure would allow a better differentiation of independent exposure effects and assessment of potential additive/interactive effects.
What are the societal consequences?
Environmental (cardiovascular) risk factors are on the rise and rarely come alone, especially in densely populated and highly urbanized areas. Although we have made significant medical and societal progress over the last years in combating and preventing traditional cardiovascular risk factors such as smoking, diabetes mellitus, hypercholesterolaemia, and obesity on an individual basis, there is a great need to take into account environmental cardiovascular risk factors in order to fight the global burden of cardiovascular disease successfully. Currently, the public interest and efforts in addressing the health burden of environmental stressors have increased significantly and our societies are becoming more and more aware of the impact of the environment on health and disease. We need more effective policies and prevention strategies that adequately strengthen these efforts in order to reduce the burden of disease imposed by environmental risk factors such as light, air, and noise pollution.
Acknowledgements
The present work was supported by a vascular biology research grant from the Boehringer Ingelheim Foundation for the collaborative research group ‘Novel and neglected cardiovascular risk factors: molecular mechanisms and therapeutic implications’ to study the effects of environmental risk factors on vascular function and oxidative stress (A.D. and T.M.). The authors also acknowledge the continuous support by the Heart Foundation of Mainz and the DZHK (German Center for Cardiovascular Research), Partner Site Rhine-Main, Mainz, Germany.
Conflict of interest: none declared.
Footnotes
† doi:10.1093/eurheartj/ehaa846.
Contributor Information
Thomas Münzel, Department of Cardiology, Cardiology I, University Medical Center Mainz, Mainz, Germany; German Center for Cardiovascular Research (DZHK), Partner Site Rhine-Main, Mainz, Germany.
Omar Hahad, Department of Cardiology, Cardiology I, University Medical Center Mainz, Mainz, Germany; German Center for Cardiovascular Research (DZHK), Partner Site Rhine-Main, Mainz, Germany.
Andreas Daiber, Department of Cardiology, Cardiology I, University Medical Center Mainz, Mainz, Germany; German Center for Cardiovascular Research (DZHK), Partner Site Rhine-Main, Mainz, Germany.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
References
- 1. Wild CP. Complementing the genome with an ‘exposome’: the outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol Biomarkers Prev 2005;14:1847–1850. [DOI] [PubMed] [Google Scholar]
- 2. Landrigan PJ, Fuller R, Acosta NJR, Adeyi O, Arnold R, Basu NN, Balde AB, Bertollini R, Bose-O’Reilly S, Boufford JI, Breysse PN, Chiles T, Mahidol C, Coll-Seck AM, Cropper ML, Fobil J, Fuster V, Greenstone M, Haines A, Hanrahan D, Hunter D, Khare M, Krupnick A, Lanphear B, Lohani B, Martin K, Mathiasen KV, McTeer MA, Murray CJL, Ndahimananjara JD, Perera F, Potocnik J, Preker AS, Ramesh J, Rockstrom J, Salinas C, Samson LD, Sandilya K, Sly PD, Smith KR, Steiner A, Stewart RB, Suk WA, van Schayck OCP, Yadama GN, Yumkella K, Zhong M. The Lancet Commission on pollution and health. Lancet 2018;391:462–512. [DOI] [PubMed] [Google Scholar]
- 3. Sainani K. Taking on the exposome. Bringing bioinformatics tools to the environmental side of the health equation. Biomed Comp Rev 2016;Fall 2016:14–21. [Google Scholar]
- 4. Lelieveld J, Pozzer A, Poschl U, Fnais M, Haines A, Munzel T. Loss of life expectancy from air pollution compared to other risk factors: a worldwide perspective. Cardiovasc Res 2020;116:1910–1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burnett R, Chen H, Szyszkowicz M, Fann N, Hubbell B, Pope CA 3rd, Apte JS, Brauer M, Cohen A, Weichenthal S, Coggins J, Di Q, Brunekreef B, Frostad J, Lim SS, Kan H, Walker KD, Thurston GD, Hayes RB, Lim CC, Turner MC, Jerrett M, Krewski D, Gapstur SM, Diver WR, Ostro B, Goldberg D, Crouse DL, Martin RV, Peters P, Pinault L, Tjepkema M, van Donkelaar A, Villeneuve PJ, Miller AB, Yin P, Zhou M, Wang L, Janssen NAH, Marra M, Atkinson RW, Tsang H, Quoc Thach T, Cannon JB, Allen RT, Hart JE, Laden F, Cesaroni G, Forastiere F, Weinmayr G, Jaensch A, Nagel G, Concin H, Spadaro JV. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc Natl Acad Sci USA 2018;115:9592–9597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kempen EV, Casas M, Pershagen G, Foraster M. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cardiovascular and metabolic effects: a summary. Int J Environ Res Public Health 2018;15:379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sun S, Cao W, Ge Y, Ran J, Sun F, Zeng Q, Guo M, Huang J, RS-Y Lee, Tian L, Wellenius GA. Outdoor light at night and risk of coronary heart disease among older adults: a prospective cohort study. Eur Heart J 2021;42:822–830. [DOI] [PubMed] [Google Scholar]
- 8. Chepesiuk R. Missing the dark: health effects of light pollution. Environ Health Perspect 2009;117:A20–A27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bedrosian TA, Nelson RJ. Timing of light exposure affects mood and brain circuits. Transl Psychiatry 2017;7:e1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Falchi F, Cinzano P, Duriscoe D, Kyba CC, Elvidge CD, Baugh K, Portnov BA, Rybnikova NA, Furgoni R. The new world atlas of artificial night sky brightness. Sci Adv 2016;2:e1600377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Munzel T, Kroller-Schon S, Oelze M, Gori T, Schmidt FP, Steven S, Hahad O, Roosli M, Wunderli JM, Daiber A, Sorensen M. Adverse cardiovascular effects of traffic noise with a focus on nighttime noise and the new WHO noise guidelines. Annu Rev Public Health 2020;41:309–328. [DOI] [PubMed] [Google Scholar]
- 12. Min JY, Min KB. Outdoor light at night and the prevalence of depressive symptoms and suicidal behaviors: a cross-sectional study in a nationally representative sample of Korean adults. J Affect Disord 2018;227:199–205. [DOI] [PubMed] [Google Scholar]
- 13. Obayashi K, Saeki K, Iwamoto J, Ikada Y, Kurumatani N. Association between light exposure at night and nighttime blood pressure in the elderly independent of nocturnal urinary melatonin excretion. Chronobiol Int 2014;31:779–86. [DOI] [PubMed] [Google Scholar]
- 14. Anisimov VN, Vinogradova IA, Panchenko AV, Popovich IG, Zabezhinski MA. Light-at-night-induced circadian disruption, cancer and aging. Curr Aging Sci 2012;5:170–177. [DOI] [PubMed] [Google Scholar]
- 15. Khan A, Plana-Ripoll O, Antonsen S, Brandt J, Geels C, Landecker H, Sullivan PF, Pedersen CB, Rzhetsky A. Environmental pollution is associated with increased risk of psychiatric disorders in the US and Denmark. PLoS Biol 2019;17:e3000353. [DOI] [PMC free article] [PubMed] [Google Scholar]