Abstract
Background
With ageing population and higher prevalence of nonalcoholic steatohepatitis (NASH) and hepatocellular carcinoma (HCC) in older patients, more and more living donor liver transplants (LDLTs) are being considered in this group of patients as eligibility for deceased donor liver transplant is restricted to those aged 65 years and younger. However, the short- and long-term outcomes of this group have not been reported from India, which does not have a robust national health scheme. The aim of this study was to provide guidelines for transplant in this group.
Methods
All patients aged 60 years and older (group 1) who underwent LDLT in our centre between January 2006 and December 2017 were studied. A propensity score–matched group in 1:2 ratio was created with comparable sex and Model for End-Stage Liver Disease score (group 2). The 2 groups were compared for duration of hospital stay, surgical complications, hospital mortality and 1-, 3- and 5-year survival.
Results
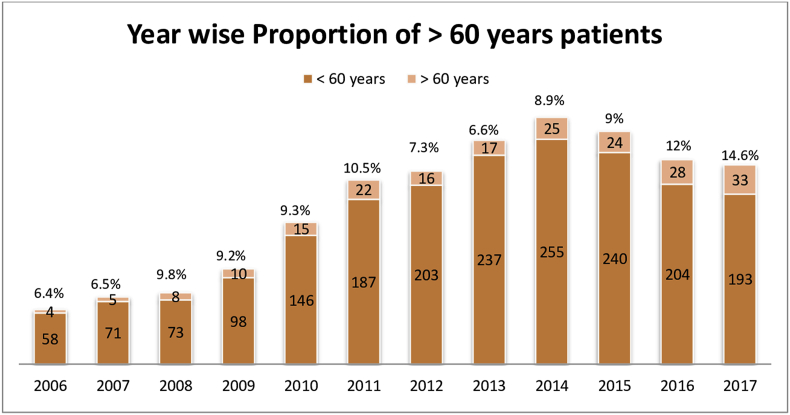
Group 1 consisted of 207 patients, and group 2 had 414 patients. The number of patients in group 1 gradually increased with time from 4 in 2006 to 33 in 2017 accounting for 15% of total cases. Group 1 had more patients with viral hepatitis, NASH and HCC, and they had a higher 30-day mortality due to cardiorespiratory complications. Although 1- and 3-year survival was similar, the 5-year survival was significantly lower in group 1.
Conclusion
Five-year survival was lower in the elderly group due to cardiorespiratory complications and recurrence of HCC. Outcomes in the elderly group can be improved with better patient selection and preventing HCC recurrence.
Keywords: elderly liver recipients, liver transplant in old patients, liver transplant outcomes, living donor liver transplantation, liver transplant in India
Abbreviations: BMI, Body Mass Index; CIT, Cold Ischaemia Time; CLD, Chronic Liver Disease; GRWR, Graft Recipient Weight Ratio; HAT, Hepatic Artery Thrombosis; HCC, Hepatocellular Carcinoma; LDLT, Living Donor Liver Transplant; MELD, Model of End-Stage Liver Disease; NASH, Nonalcoholic Steatohepatitis; PVT, Portal Vein Thrombosis; WIT, Warm Ischaemia Time
With increasing life expectancy and improving outcomes, more number of patients, as well as older patients, are coming forward for transplant in India. As more than 80% of transplants in India are living donor liver transplants (LDLTs), it raises an important ethical question, as most donors are much younger family members.1 Although the proportion of older patients may be lower than that of Western countries, overall it is still a huge number just by the sheer size of our total population. This increased demand is also from changing indications for transplant such as nonalcoholic steatohepatitis (NASH) and hepatocellular carcinoma (HCC).
Few deceased donor liver transplant (DDLT) centres from the USA and Europe have analysed the outcomes of elderly recipients and have shown conflicting results.2, 3, 4, 5, 6 The literature on outcomes after LDLT in the elderly patients is even more limited.7 This study will be the first from a resource-constrained country without a robust national health service. As transplant outcomes are better in countries where there is an organised system of follow-up and recall of patients, the results of this study will be important for transplant programs in resource-constrained countries.
Patients and methods
This study includes all patients who underwent LDLT from January 2006 to December 2017 in Centre for Liver and Biliary Sciences, New Delhi, India. This study is a retrospective analysis of our prospectively maintained database. Patients were divided into two groups; group 1 were older patients (>60 yrs) and group 2 consisted of younger recipients (18-60 yrs). Group 2 consisted of sex and Model for End-Stage Liver Disease (MELD) score matched cohort with 1:2 ratio. The two groups were compared for demographic data, 30-day hospital mortality, average length of hospital stay, postoperative complications and 1-, 3- and 5-year survival. Our follow-up protocol is to examine the patient every week for first one month after discharge. In the follow-up clinic, the coordinator teaches the recipient what tests to do and how frequently they should be carried out. They are tutored to fill an Excel sheet where not only all the test results are entered but also the doses of the immunosuppressive medication are entered. Advice is given regarding the doses electronically after the coordinator consults the doctors. Patients are contacted by mail or telephone if they have defaulted twice. Patients are encouraged to visit the centre twice a year.
Inclusion criteria
All adult patients from the Indian subcontinent who underwent elective LDLT were included.
Exclusion criteria
Paediatric patients and patients with LDLT for acute liver failure, ABO incompatible LDLT, retransplantation and DDLT were excluded from the study.
Statistical analysis
Pretransplant and intraoperative variables, donor and graft characteristics and postoperative outcomes of groups 1 and 2 were compared using the Chi-square test (noncontinuous variables), Student's t-test (continuous variables with normal distribution) and Mann–Whitney U-test (continuous variables with nonparametric distribution). The Kaplan–Meier method was used to estimate the 1-, 3- and 5-year survival. Statistical analysis was performed using SPSS, version 22, software. All P values presented are two sided, and P value < 0.05 was considered statistically significant.
Results
A total of 2542 patients from the Indian subcontinent underwent LDLT at our centre between 2006 and 2017. After applying inclusion and exclusion criteria, 2172 patients were included for analysis, provided a minimum one-year follow-up was available. These patients were classified into two groups according to their age. Group 1 consisted of liver transplant recipients aged 60 years and older, and group 2 was the younger cohort of patients aged 18–60 years. A total of 207 patients were included in group 1, and 1965 patients were younger than 60 years. For direct comparison, a case-matched analysis was performed using matched cohorts created from propensity scores. The 1:2 matching algorithm identified two matched cohorts (n = 207 in group 1 and n = 414 in group 2) in which both the cohorts were comparable in terms of sex and MELD score. This allowed for the direct comparison of preoperative variables, intraoperative variables and postoperative outcomes between group 1 and 2. Between 2006 and 2017, the number of patients aged older than 60 years gradually increased from 4 in 2006 to 33 in 2017 accounting for 15% of total cases performed in 2017. The year wise trend in the number of elderly patients undergoing LDLT was analysed, and it is represented in Figure 1. Preoperative variables in the groups were similar for sex and MELD score as group 2 was created using sex and MELD score match in the ratio 1:2. The number of patients with viral hepatitis–related cirrhosis, NASH and HCC was higher in group 1, and the number of patients with alcoholic liver disease was higher in group 2. Group 1 had a higher proportion of patients with hypertension, coronary artery disease, diabetes and respiratory conditions, as shown in Table 1. However, there were no significant differences in donor age, body mass index (BMI) and intraoperative variables such as graft type, graft weight, warm ischaemic time and cold ischaemic time (Table 2). This study shows longer hospital stay, higher cardiac and respiratory complications and higher mortality in the group 1 cohort. Postoperative complications in both the groups have been tabulated and compared in Table 3. Technical complications such as hepatic artery thrombosis, portal vein thrombosis and hepatic vein stenosis and bile leaks were similar in both the groups. The neurological complications were similar in both groups.
Figure 1.
Year wise trend in elderly patients undergoing LDLT compared with total patients. LDLT, living donor liver transplant.
Table 1.
Pretransplant Variables of the Recipients in Both the Groups.
| Group 1 > 60yrs (n = 207) | Group 2 < 60yrs (n = 414) | P value | |
|---|---|---|---|
| Age | 63.93 ± 2.98 years | 42.58 ± 14.61 years | |
| Sex | |||
| Males | 156 (75.4%) | 313 (75.6%) | |
| Females | 51 (24.6%) | 101 (24.4%) | |
| BMI | 24.33 ± 5.92 | 25.02 ± 6.31 | 0.092 |
| MELD score | 17.95 ± 6.9 | 18.06 ± 7.1 | |
| Child-Pugh score | |||
| A | 18 (8.7%) | 21 (5.07%) | |
| B | 96 (46.4%) | 178 (42.9%) | |
| C | 93 (44.9%) | 215 (51.9%) | |
| Aetiology | |||
| Viral | 111 (53.6) | 185 (44.7) | 0.03 |
| HBV | 20 (9.7%) | 44 (10.6%) | |
| HCV | 85 (41.1%) | 137 (33.1%) | |
| HBV + HCV | 6 (2.9%) | 4 (1%) | |
| Alcohol | 23 (11.1%) | 88 (21.3%) | 0.02 |
| NASH | 35 (16.9%) | 46 (11.1%) | 0.02 |
| Cryptogenic | 33 (15.9%) | 72 (17.4%) | 0.75 |
| Others | 5 (2.4%) | 23 (5.6) | 0.075 |
| Autoimmune | 4 (1.9%) | 5 (1.2%) | |
| PSC | 1 (0.04%) | 5 (1.2%) | |
| PBC | 0 (0%) | 3 (0.7%) | |
| SBC | 0 (0%) | 1 (0.2%) | |
| BCS | 0 (0%) | 8 (1.9%) | |
| Wilson | 0 (0%) | 1 (0.2%) | |
| Comorbidities | |||
| Hypertension | 26 (12.6%) | 32 (7.7%) | 0.05 |
| Coronary artery disease | 4 (1.9%) | 1 (0.2%) | 0.02 |
| Diabetes | 78 (37.7%) | 84 (20.3%) | 0.003 |
| Respiratory diseases | 14 (6.8%) | 5 (1.2%) | 0.001 |
| HCC | 82 (39.6%) | 86 (20.8%) | 0.001 |
| Renal dysfunction | |||
| AKI | 26 (12.6%) | 56 (13.5%) | 0.73 |
AKI, acute kidney injury; BCS, budd chiari syndrome; BMI, body mass index; HBV, hepatitis B virus; HCC, hepatocellular carcinoma; HCV, hepatitis C virus; MELD, Model for End-Stage Liver Disease; NASH, nonalcoholic steatohepatitis; PBC, primary biliary cirrhosis; PSC, primary sclerosing cholangitis; SBC, secondary biliary cirrhosis.
Table 2.
Intraoperative Variables.
| Group 1 – more than 60 yrs (n = 207) | Group 2 – less than 60 yrs (n = 414) | |
|---|---|---|
| Liver graft type | ||
| Modified right lobe graft | 180 (87%) | 355 (85.7%) |
| Standard right lobe graft | 5 (2.4%) | 9 (2.1%) |
| Extended right lobe graft | 11 (5.3%) | 24 (5.8%) |
| Left lobe graft | 9 (4.3%) | 21 (5.1%) |
| Right posterior sector graft | 2 (1%) | 5 (1.2%) |
| Graft recipient weight ratio (GRWR) | 1.06 | 1.07 |
| Cold ischaemia time (CIT) | 105.84 ± 57.12 | 110.94 ± 69.94 |
| Warm ischaemia Time (WIT) | 37.42 ± 11.36 | 38.41 ± 18.19 |
Table 3.
Postoperative Complications.
| Group 1 (>60 yrs) n = 207 | Group 2 (<60 yrs) n = 414 | P value | |
|---|---|---|---|
| Hospital stay (days) | 25.68 ± 11.40 | 22.89 ± 15.93 | 0.02 |
| In-hospital mortality | 35 (16.9%) | 45 (10.9%) | 0.03 |
| Postoperative complications | |||
| Sepsis | 18 (8.6%) | 32 (7.7%) | 0.6 |
| Bile leak | 15 (7.2%) | 26 (6.28%) | 0.6 |
| Vascular complications | |||
| HAT | 2 (1%) | 4 (1%) | 1 |
| PVT | 3 (1.4%) | 5 (1.2%) | 0.8 |
| HV obstruction | 3 (1.4%) | 2 (0.5%) | 0.2 |
| Neurological events | 12 (5.8%) | 16 (3.9%) | 0.27 |
| Cardiovascular events | 8 (3.9%) | 2 (0.5) | 0.01 |
| Respiratory events | 11 (5.3) | 7 (1.6) | 0.01 |
| Bleeding | 3 (1.4%) | 5 (1.2%) | 0.8 |
HAT, hepatic artery thrombosis; HV, hepatic vein; PVT, portal vein thrombosis.
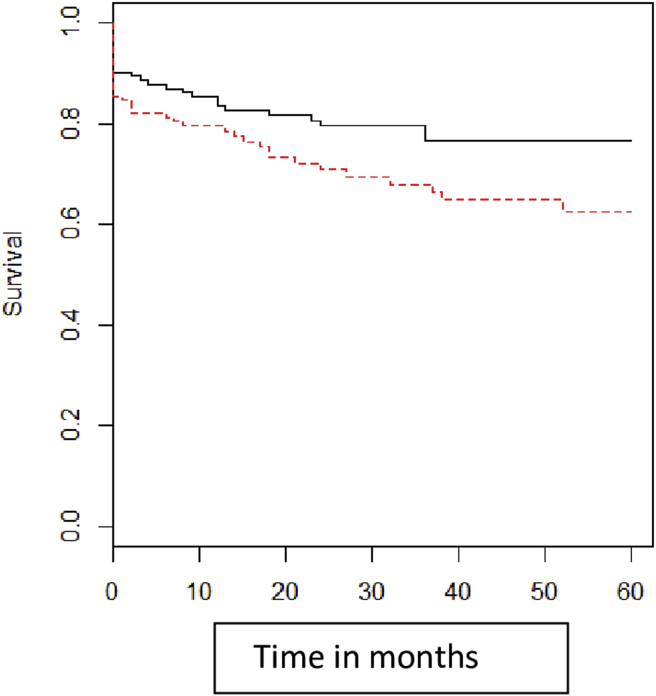
Kaplan-Meir survival was plotted for the two groups to study 1-, 3- and 5-year survival, and it is shown in Figure 2. Although there was lower survival in the elderly group at 1 and 3 years, it was not statistically significant, but at 5 years, it became statistically significant. Cardiovascular complications and HCC recurrence contributed for the difference.
Figure 2.
Kaplan-Meier curve for 1-, 3- and 5-year survival of group 1 and group 2.
Analysis of survival
Overall patient survival at 30 days was 91% in the younger group and 85% in elderly patients (p = 0.04) The 1-yr survival for these groups was 85% and 80%, respectively (p = 0.18). The 3-yr survival for these groups was 78% and 69%, respectively (p = 0.12 not significant). The 5-yr survival was 75% and 61%, respectively, and it was statistically significantly lower in the elderly group (p = 0.01).
Discussion
In India, average life expectancy in men and women is 67 years and 70 years, respectively,8 and most people until recently would not come forward for LDLT. However, with improving outcomes and higher prevalence of NASH and HCC, many patients are now being transplanted.
This study intended to analyse the outcome data of LDLT in elderly patients and to look at the impact of comorbid conditions on postoperative outcomes.
The year wise trend in elderly patients undergoing LDLT shows that the number is gradually increasing year by year as shown in graph 1. In 2006, only 4 of 58 patients were more than 60 years old, whereas in 2017, 33 elderly patients underwent LDLT comprising 15% of the total number. There are many reasons for this increase in the trend of liver transplant in elderly patients such as increase in the population of elderly people, higher prevalence of HCC in the elderly, improved outcome of medical therapy of chronic viral hepatitis and higher prevalence of NASH.9 It is also possible that older patients are more likely to be financially capable to go through transplant. At the same time, as the experience of surgeons and anaesthetists is increasing, they are becoming more liberal in accepting elderly patients as candidates for LDLT.
Amongst the preoperative variables, the two groups were different only in terms of age as the second group was chosen with sex and MELD score matching. The BMI of both the groups was also not different statistically. In both the groups, chronic viral infection–related cirrhosis was the most common indication for LDLT. However, the proportion of patients with chronic viral hepatitis was higher in the older group, and this was statistically significant (53.6% versus44.7%). In the viral aetiology category, hepatitis C was the leading cause in both the groups. In contrast to our findings, many studies have shown that incidence of viral infection is higher in the younger group of patients undergoing LDLT.10, 11, 12, 13, 14 Our study is one of the few studies that have shown a higher incidence in elderly patients.15,16
Alcoholic liver disease was more common in the younger group than in the elderly group (21.3% vs. 11.1%). Many studies have observed similar findings of alcohol-related chronic liver disease (CLD) being more common in the younger group.10,11,17,18
NASH is a rapidly growing aetiology of CLD requiring liver transplantation in many parts of the world.19,20 In our study, NASH-related CLD is the second most common cause for LDLT in the elderly group with 16.9% incidence, whereas it was seen in 11.1% of the younger group. This is similar to many other series from the Western World which reported a higher incidence of NASH-related CLD in elderly patients.7,18,21
Comorbidities such as diabetes mellitus, hypertension, cardiac and respiratory diseases were significantly higher in the elderly group, as shown in Table 1, in keeping with similar finding in other studies.11,22 Many studies have also shown that preoperative comorbidities are associated with higher morbidity and mortality.23, 24, 25, 26
Presence of HCC is an important prognostic factor in liver transplantation. In our study, the occurrence of HCC was significantly higher in elderly patients than in the younger group as shown in Table 1 and may have contributed to their lower 5-year survival.
In both the groups, the donor characteristics and intraoperative variables were no different. This is in contrast to what has been reported in DDLT series where reperfusion injury and cardiovascular events are more common. LDLT has a unique advantage of optimizing patient condition, choosing the best donor and keeping minimal warm and cold ischaemic times.
In both the groups, the most common complication was sepsis. The incidence of vascular complications such as hepatic artery thrombosis, portal vein thrombosis and hepatic vein outflow obstruction was comparable in both the elderly and younger groups in line with findings from other studies.15,22,27,28 Biliary complications were similar in both the groups, and major bile leaks progressed to form stricture in both the groups.29 Postoperative haemorrhage was also similar in the two groups, and nearly 40% of early reexploration was due to bleeding. Complications such as cardiac and respiratory complications were significantly higher in the elderly group, particularly if they had preexisting impairment and led to prolonged hospital stay. Surprisingly, neurological events were similar in both the groups and may have been from our detailed neurological workup.
Overall, in-hospital mortality was 16.9% vs. 10.9% in group 1 and 2, respectively. It was significantly higher in the elderly group. In the elderly group, the most common cause of death was sepsis and respiratory failure (Table 4). In the younger group, the most common cause was sepsis followed by graft dysfunction. The higher mortality in the elderly group was contributed significantly by cardiac and respiratory complications. In the elderly group, patients with multiple comorbidities had significantly higher mortality compared with patients with single comorbidity (p = 0.04).
Table 4.
Post Operative Causes of Death.
| Cause | Group 1 (>60 yrs) n = 207 | Group 2 (<60 yrs) n = 414 | P value |
|---|---|---|---|
| Sepsis | 8 | 17 | 0.5 |
| Graft dysfunction | 4 | 9 | 0.3 |
| Cardiovascular | 4 | 1 | 0.05 |
| Respiratory failure | 8 | 3 | 0.04 |
| Renal failure | 2 | 3 | 0.8 |
| Bile leak | 1 | 1 | 0.8 |
| HAT | 1 | 1 | 0.8 |
| PVT | 1 | 2 | 0.7 |
| Outflow obstruction | 1 | 0 | |
| Intracranial bleed | 1 | 0 | |
| Others | 4 | 8 |
HAT, hepatic artery thrombosis; PVT, portal vein thrombosis.
The one-year survival was 80% in the elderly group and 85% in the younger group. There was no statistical difference. In elderly group, most deaths in first year after discharge from hospital were again related to underlying cardiac and respiratory morbidity, along with infection complications which might be secondary to immunosuppression, whereas infection was the predominant cause of death in the younger group. Three-year survival among both groups was 69% vs. 78% which was again statistically not significant. However, the five-year survival was significantly better in the younger group, 61% vs 75%. The increased deaths in the elderly group beyond three years were again contributed significantly by cardiovascular and recurrence of HCC-related deaths. The presence of HCC at the time of transplant contributed significantly to recurrence and deaths after 3 years of LDLT.
In-hospital mortality after LDLT is higher in the elderly group, and it is secondary to preexisting cardiac and respiratory morbidities, and hence, optimization/screening before LDLT is recommended. One- and three-year survival is similar in both the groups. Five-year survival is lower in the elderly group and it is from increased cardiovascular diseases, and hence, a multidisciplinary follow-up of these patients is recommended. Recurrence of HCC is also an important cause for deaths after 3 years. As overall survival is satisfactory, age alone should not deter from transplant.
CRediT authorship contribution statement
Ravindra Nidoni: Writing - original draft, Investigation. Rajasekhar Kandagaddala: Methodology, Software, Validation, Formal analysis. Shaleen Agarwal: Writing - review & editing. Rajesh Dey: Writing - review & editing. Bhargava R. Chikkala: Data curation. Subhash Gupta: Conceptualization, Supervision.
Conflicts of interest
The authors have none to declare.
Funding
None.
References
- 1.Gupta S. Living donor liver transplant is a transparent activity in India. J Clin Exp Hepatol. 2013;3:61–65. doi: 10.1016/j.jceh.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kollmann D., Maschke S., Rasoul-Rockenschaub S. Outcome after liver transplantation in elderly recipients (>65 years) — a single-center retrospective analysis. Dig Liver Dis. 2018;50:1049–1055. doi: 10.1016/j.dld.2018.06.018. [DOI] [PubMed] [Google Scholar]
- 3.Egeli T., Unek T., Agalar C. Survival outcomes after liver transplantation in elderly patients: a single-center retrospective analysis. Transplant Proc. 2019;51:1143–1146. doi: 10.1016/j.transproceed.2019.01.090. [DOI] [PubMed] [Google Scholar]
- 4.Burra P., De Martin E., Gitto S., Villa E. Influence of age and genderbefore and after liver transplantation. Liver Transpl. 2013;19:122–134. doi: 10.1002/lt.23574. [DOI] [PubMed] [Google Scholar]
- 5.Sutherland A.I., Jzermans J.N.I., Forsythe J.L., Dor F.J. Kidney and liver transplantation in the elderly. Br J Surg. 2016;103:62–72. doi: 10.1002/bjs.10064. [DOI] [PubMed] [Google Scholar]
- 6.Lei Yu, Carithers Robert. Liver transplantation in the elderly: an evidence based review on patient outcome, selection and management strategies. J Biomed Sci Eng. 2014;7:651–661. [Google Scholar]
- 7.Chen H.-P., Tsai Y.-F., Lin J.-R., Liu F.-C., Yu H.P. Recipient age and mortality risk after liver transplantation: a population-based cohort study. PloS One. 2016;11(3) doi: 10.1371/journal.pone.0152324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.National Health Profile. 2019. https://www.cbhidghs.nic.in/showfile.php?lid=1147 14th issue. [Google Scholar]
- 9.Tajiri K., Shimizu Y. Liver physiology and liver diseases in the elderly. World J Gastroenterol. 2013;19:8459–8467. doi: 10.3748/wjg.v19.i46.8459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Su F., Yu L., Berry K. Aging of liver transplant registrants and recipients: trends and impact on waitlist outcomes, post-transplantation outcomes, and transplant-related survival benefit. Gastroenterology. 2016;150:441–453. doi: 10.1053/j.gastro.2015.10.043. [DOI] [PubMed] [Google Scholar]
- 11.Wilson G.C., Quillin R.C., 3rd, Wima K. Is liver transplantation safe and effective in elderly (>/=70 years) recipients? A case-controlled analysis. HPB. 2014;16:1088–1094. doi: 10.1111/hpb.12312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim J., Ko M.E., Nelson R.A. Increasing age and survival after orthotopic liver transplantation for patients with hepatocellular cancer. J Am Coll Surg. 2014;218:431–438. doi: 10.1016/j.jamcollsurg.2013.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Schwartz J.J., Pappas L., Thiesset H.F. Liver transplantation in septuagenarians receiving model for end-stage liver disease exception points for hepatocellular carcinoma: the national experience. Liver Transpl. 2012;18:423–433. doi: 10.1002/lt.23385. [DOI] [PubMed] [Google Scholar]
- 14.Cross T.J., Antoniades C.G., Muiesan P. Liver transplantation in patients over 60 and 65 years: an evaluation of long-term outcomes and survival. Liver Transpl. 2007;13:1382–1388. doi: 10.1002/lt.21181. [DOI] [PubMed] [Google Scholar]
- 15.Ikegami T., Bekki Y., Imai D. Clinical outcomes of living donor liver transplantation for patients 65 years old or older with preserved performance status. Liver Transpl. 2014;20:408–415. doi: 10.1002/lt.23825. [DOI] [PubMed] [Google Scholar]
- 16.Felga G., Silva Evangelista A., Rogerio de Oliveira Salvalaggio P., Bruno de Rezende M., Dias de Almeida M. Liver transplantation for unresectable hepatocellular carcinoma in elderly patients: what to expect. Transplant Proc. 2014;46:1764–1767. doi: 10.1016/j.transproceed.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Bilbao I., Dopazo C., Lazaro J.L. Our experience in liver transplantation in patients over 65 yr of age. Clin Transplant. 2008;22:82–88. doi: 10.1111/j.1399-0012.2007.00749.x. [DOI] [PubMed] [Google Scholar]
- 18.Malinis M.F., Chen S., Allore H.G., Quagliarello V.J. Outcomes among older adult liver transplantation recipients in the model of end stage liver disease (MELD) era. Ann Transplant. 2014;19:478–487. doi: 10.12659/AOT.890934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samji Naga S., Verma Rajanshu, Sanjaya K. SatapathyMagnitude of NonAlcoholic fatty liver disease: western perspective. J Clin Exp Hepatol. 2019;9:497–505. doi: 10.1016/j.jceh.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu B., Kwok D., Wong V.W.S. Magnitude of non-alcoholic fatty liver disease: eastern perspective. J Clin Exp Hepatol. 2019;9:491–496. doi: 10.1016/j.jceh.2019.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wilson G.C., Cutler Quillin R., III, Wima K. Is liver transplantation safe and effective in elderly (≥70 years) recipients? A case-controlled analysis. HPB. 2014;16:1088–1094. doi: 10.1111/hpb.12312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Audet M., Piardi T., Panaro F. Liver transplantation in recipients over 65 yr old: a single center experience. Clin Transplant. 2010;24:84–90. doi: 10.1111/j.1399-0012.2009.00972.x. [DOI] [PubMed] [Google Scholar]
- 23.Lentine K.L., Costa S.P., Weir M.R. Cardiac disease evaluation and management among kidney and liver transplantation candidates: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. J Am Coll Cardiol. 2012;60:434–480. doi: 10.1016/j.jacc.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 24.Donovan R.J., Choi C., Ali A. Perioperative cardiovascular evaluation for orthotopic liver transplantation. Dig Dis Sci. 2017;62:26–34. doi: 10.1007/s10620-016-4371-3. [DOI] [PubMed] [Google Scholar]
- 25.Plotkin J.S., Scott V.L., Pinna A., Dobsch B.P., De Wolf A.M., Kang Y. Morbidity and mortality in patients with coronary artery disease undergoing orthotopic liver transplantation. Liver Transpl Surg. 1996;2:426–430. doi: 10.1002/lt.500020604. [DOI] [PubMed] [Google Scholar]
- 26.Konerman M.A., Fritze D., Weinberg R.L., Sonnenday C.J., Sharma P. Incidence of and risk assessment for adverse cardiovascular outcomes after liver transplantation: a systematic review. Transplantation. 2017;101:1645–1657. doi: 10.1097/TP.0000000000001710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdelfattah M.R., Elsiesy H. Reappraisal of upper age limit for adult living-donor liver transplantation using right lobe grafts: an outcome analysis. Eur J Gastroenterol Hepatol. 2015;27:593–599. doi: 10.1097/MEG.0000000000000322. [DOI] [PubMed] [Google Scholar]
- 28.Montalti R., Rompianesi G., Di Benedetto F. Liver transplantation in patients aged 65 and over: a case-control study. Clin Transplant. 2010;24:188–193. doi: 10.1111/j.1399-0012.2010.01230.x. 2010. [DOI] [PubMed] [Google Scholar]
- 29.Wadhawan M., Kumar A., Gupta S. Post-transplant biliary complications: an analysis from a predominantly living donor liver transplant center. J Gastroenterol Hepatol. 2013;28:1056–1060. doi: 10.1111/jgh.12169. [DOI] [PubMed] [Google Scholar]