Abstract
Background
Since the emergence of COVID-19 pandemic, several cases of cerebral venous sinus thrombosis (CVST) have been reported in SARS-CoV-2 infected individuals.
Methods
Consecutive patients with documented SARS-CoV-2 infection, as well as clinical and radiological characteristics of CVST, were reported from three teaching hospitals in the South West, North West, and the center of Iran between June and July 2020. We also searched the abstract archives until the end of August 2020 and gathered 28 reported cases. The diagnostic criteria for SARS-CoV-2 infection were determined according to SARS-CoV-2 detection in oropharyngeal or nasopharyngeal samples in clinically suspected patients. Demographics, prominent COVID-19 symptoms, confirmatory tests for SARS-CoV-2 infection diagnosis, the interval between the diagnosis of SARS-CoV-2 infection and CVST, clinical and radiological features of CVST, therapeutic strategies, CVST outcomes, rate of hemorrhagic transformation, and mortality rate were investigated.
Results
Six patients (31–62 years-old) with confirmed CVST and SARS-CoV-2 infection were admitted to our centers. Four patients had no respiratory symptoms of SARS-CoV-2 infection. Five patients developed the clinical manifestations of CVST and SARS-CoV-2 infection simultaneously. Three patients had known predisposing factors for CVST. Despite receiving CVST and SARS-CoV-2 infection treatments, four patients died. SARS-COV-2 associated CVST patients were older (49.26 vs. 37.77 years-old), had lower female/male ratio (1.42 vs. 2.19), and higher mortality rate (35.29% vs. 6.07%) than CVST not associated with COVID-19.
Conclusions
The role of SARS-CoV-2 as a “cause” versus an “additive contributor” remains to be elucidated. Practitioners should be aware of the possibility of CVST in SARS-CoV-2 infection.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00415-021-10450-8.
Keywords: SARS-CoV-2, COVID-19, Coronavirus, Sinus thrombosis, Intracranial, Stroke
Introduction
Cerebral venous sinus thrombosis (CVST) is far less common than arterial stroke [1]; however, it occupies a prominent place in the field of cerebrovascular medicine due to the involvement of young adults and women of reproductive age [2, 3]. Furthermore, acute-phase survival and favorable long-term prognosis depend strongly on receiving prompt and adequate treatment. This makes early diagnosis of CVST tremendously important [4].
Since the emergence of the Coronavirus Disease 2019 (COVID-19) pandemic, non-respiratory manifestations of the disease like neurological manifestations [5] and thrombotic events have been progressively appreciated. Although there are some case reports and one case series [6–18] showing the association of the CVST and Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection, the data about diagnosis and prognosis in this association are still limited. We investigated the demographic, clinical, radiological, and prognostic characteristics of this association to improve the diagnosis and treatment of patients with CVST and COVID-19.
Methods
Consecutive patients with documented SARS-CoV-2 infection, as well as clinical and radiological characteristics of CVST, were recruited from three teaching hospitals in the Southwest, Northwest, and the center of Iran between June and July 2020. Only patients with either simultaneous CVST and COVID-19 presentation or CVST within two weeks of the typical presentations of COVID-19 were included. Patients who were admitted to the hospital with a diagnosis of CVST and developed COVID-19 as a nosocomial infection were excluded.
The diagnostic criteria for COVID-19 were determined according to SARS-CoV-2 detection in oropharyngeal or nasopharyngeal samples in clinically suspected patients [19]. CVST diagnosis was performed according to the American Heart Association/American Stroke Association statement [20]. Criteria for the diagnosis of CVST were the presence of relevant neurological syndromes (headache, intracranial hypertension, focal neurologic deficits, and/or encephalopathic states), and radiological confirmation (computed tomography (CT), CT venography, brain magnetic resonance imaging (MRI), and/or MR venography). Patients, whose manifestations could be better explained by any other neurological diseases were excluded.
We collected a wide range of variables including, sociodemographic and vascular risk factors. We also assessed COVID-19 symptoms, confirmatory tests for SARS-CoV-2 infection diagnosis, the interval between the clinical suspicion of SARS-CoV-2 infection and CVST onset. Clinical and radiological characteristics of CVST, including areas of involvement, therapeutic strategies, and outcomes were collected for all cases.
The possible predisposing factors for CVST were categorized into hormone-related causes (pregnancy, post-partum and oral contraceptive use), dehydration (including religious fasting), obesity, mechanical and traumatic causes, infections rather than SARS-CoV-2, hereditary thrombophilia (particularly proteins C and S deficiency, factor V Leiden, antithrombin III deficiency, hyperhomocysteinemia), malignancies, hematologic disorders (particularly sickle cell disease and paroxysmal nocturnal hemoglobinuria), inflammatory disorders (collagen vascular diseases, Behcet disease, vasculitis, inflammatory bowel disease), drug-induced, multifactorial, and idiopathic.
We also searched the abstract archives including PubMed, Web of Science, Scopus, and Google Scholar published until the end of August 2020. Searches were conducted using the following MeSH terms: “SARS-CoV-2”, “COVID-19”, “Coronavirus”, “Sinus Thrombosis”, and “Intracranial” and relevant full texts were found. At the end, we compared the cumulative data, which refer to data of SARS-COV-2 associated CVST cases, with previous non-COVID-19 CVST studies.
This study was approved by the ethics committee and institutional review board of Shiraz University of Medical Sciences (IR.sums.rec.1399–235).
Results
Eight patients were initially recruited. In two patients, a diagnosis of SARS-CoV-2 infection was suspected due to the presence of pathognomonic findings in chest high-resolution computerized tomography or the presence of SARS-CoV-2-specific IgM antibody. For the sake of the highest specificity, these patients were excluded. Six patients with CVST and SARS-CoV-2 infection were presented. Demographics, main COVID-19 symptoms, confirmatory tests for COVID-19 diagnosis, the interval between the clinical suspicion to COVID-19 and the diagnosis of CVST, clinical and radiological characteristics of CVST, therapeutic strategies, and outcomes of patients with CVST associated with SARS-CoV-2 infection were investigated and presented in Table 1. Four out of six patients had no respiratory symptoms of SARS-CoV-2 infection. Five out of six patients had the clinical manifestations of CVST and SARS-CoV-2 infection, simultaneously. Three patients had known predisposing factors for CVST including pregnancy, protein C deficiency, and Hepatitis C. One patient had a previous history of CVST following an oral contraceptive usage. One patient was not a known case of systemic lupus erythematosus (SLE) or antiphospholipid antibody syndrome (APLS) but showed positive lupus anticoagulant during SARS-CoV-2 infection. Despite receiving CVST and COVID-19 treatments, four out of six patients died (between the day of admission until 21 days after admission). In two patients, death was primarily due to neurological deterioration and in two patients, death was primarily due to COVID-19. Endovascular intervention was performed for one of our patients; this proved to be futile despite initial recanalization. Case no.1, as an illustrative case, is presented in detail. The clinical vignettes of the other patients (case no. 2–6) were provided in the supplementary file.
Table 1.
Clinical features and outcomes of six patients with CVST correlated to COVID-19
| Case no | Age (years)/Sex/location (region) | Time of COVID-19 presentation (month of 2020) | COVID-19 clinical symptoms* | Confirmatory COVID-19 results | CVST clinical syndrome** | Baseline parenchymal lesions (Hemorrhagic or infarct) | CVST tempo*** | Interval between COVID-19 and CVST (days) | CVST radiological features | CVST predisposing factors | Other thrombotic events | Significant thrombophilia laboratories | Treatment Strategy for | Prognosis | Most probable cause of moratlity | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nasopharyngeal Swap PCR | Chest HRCT | COVID-19 | CVST | ||||||||||||||
| 1 | 62/Female/south west of Iran | June | Non-respiratory | + | Suspicious due to subpleural bands | A | Yes (Hemorrhagic) | Subacute | 0 | Multiple sinuses, cortical veins | Lupus anticoagulant |
DVT, suspicious MAT |
Lymphopenia, Thrombocytopenia, Elevated CRP, Elevated D-dimer, Elevated LDH, Elevated Lupus Anticoagulant, Elevated Antiphospholipid Antibody |
Antiviral Medications, Corticosteroid |
Unfractionated Heparin, Thrombectomy, Neurosurgical Intervention (craniotomy, ventriculostomy) |
Dead on 10th day | CVST |
| 2 | 68/Female/Center of Iran | July | Non-respiratory | + | − | B | No | Subacute | 0 | Multiple sinuses | Protein C deficiency | PTE | Thrombocytopenia, Elevated CRP, Elevated LDH |
Antiviral Medications, Hydroxychloroquine |
Unfractionated Heparin | Dead on 21th day | COVID-19 |
| 3 | 40/Male/south west of Iran | July | Non-respiratory | + | + | A | Yes (Infarct) | Subacute | 0 | Multiple sinuses, cortical veins | Chronic hepatitis C | DVT | Elevated LDH | Conservative Treatment | Unfractionated Heparin | Dead on 1st day | COVID-19 |
| 4 | 46/Male/north west of Iran | July | Respiratory, Non-respiratory | + | + | A | Yes (Hemorrhagic) | Acute | 15 | Cortical vein | Idiopathic | - | Thrombocytopenia, Elevated CRP, Elevated D-dimer, Elevated LDH |
Antiviral Medications, Corticosteroid |
Low Molecular Weight Heparin | Dead on 15th day | CVST |
| 5 | 32/Female/South West of Iran | August | Non-respiratory | + | ND | A | Yes (Hemorrhagic) | Subacute | 0 | Deep veins | Pregnancy | - | Elevated CRP, Elevated D-dimer | Conservative Treatment | Unfractionated Heparin |
Alive after 2 months |
NA |
| 6 | 31/Female/West of Iran | August | Respiratory, non-respiratory | + | + | A | Yes (Hemorrhagic) | Subacute | 0 | Sphenoparietal sinus, and superficial middle cerebral vein | Previous CVST | - | Lymphopenia, Elevated CRP, Elevated D-dimer |
Antiviral Medications, Corticosteroid |
Low Molecular Weight Heparin |
Alive after 2 months |
NA |
CVST cerebral venous sinus thrombosis, COVID-19 Coronavirus Disease 2019, PCR polymerase chain reaction, HRCT high-resolution computed tomography, ND not determined to be checked, DVT Deep venous thrombosis of lower extremities, MAT Mesenteric artery thrombosis, PTE pulmonary thromboembolism
*Non-respiratory: (headache, malaise, neurological symptoms, decrease level of consciousness, gastrointestinal symptom)
**CVST clinical syndrome: A—stroke-like: Brain Infarct with or without hemorrhagic transformation and focal neurologic deficit; B—encephalopathy syndrome with no brain infarct or raised intracranial pressure syndrome (RICP)
***CVST Tempo: acute (< 48 h); subacute (48 h to 30 days)
A cumulative data were defined as an amalgam of the current series and the previously reported CVST associated with COVID-19 cases [6–18]. A comparison between this cumulative data and some large-volume CVST studies performed before the COVID-19 pandemic [1, 3, 4, 21, 22], has been made (Table 3).
Table 3.
Comparison of the cumulative data (current cases and previous reported cases with CVST associated COVID-19) with previously published large-volume studies on CVST without COVID-19
| Cumulative data* | Borhani-Haghighi, et al. [4] | Ferro, et al. [21] | Wasay, et al. [1] | Shakibajahromi, et al. [22] | Borhani-Haghighi, et al. [3] | |
|---|---|---|---|---|---|---|
| Date | 2020 | 1993–2010 | 1998–2001 | 2009–2012 | 2012–2016 | 2000–2007 |
| Number of patients | 34 | 465 | 624 | 812 | 174 | 568 |
| Ethnicity | Mostly Iranian | Iranian | Mostly European abd American | Asian | Iranian | American |
| Mean age (years) | 49.26 | 29.5–43.8 | 39.1 | 31 | 37.8 | 46.9 |
| Female/male ratio | 1.42 | 2.8 | 2.92 | 1.43 | 2.8 | 1.8 |
| Most common predisposing factors | Idiopathic | gender-related causes (mainly OCP) | Thrombophilia; gender-related causes (mainly OCP) | gender-related causes (pregnancy/puerperium) | gender-related causes (mainly OCP) | Systemic malignancy |
| Hemorrhagic transformation | 55% | 11–58% | 39.3% | 26.7%(MRI), 9.6%(CT) | 40.1% | NM |
| Mortality | 35.29% | 11.4% | 8.3% | 3.3% (in hospital) | 5.2% | 3.5% |
CVST cerebral venous sinus thrombosis, COVID-19 coronavirus Disease 2019, OCP oral contraceptive pill, MRI magnetic resonance imaging, CT computed tomography, NM not mentioned
*Cumulative data (cases with CVST and COVID-19) were obtained from Iran, Singapore, United States, Belgium, Italy, UK, France, Netherlands, and Japan
Illustrative patient
A 62-year-old Iranian woman was admitted to the Emergency Department of Namazi Hospital, Shiraz, in the southern part of Iran in June 2020. She reported a 5-day history of a gradual and progressive throbbing right-sided occipital headache associated with nausea and vomiting. She developed blurred vision and left side weakness three days after the onset of headache.
Except for episodes of migraine headache, which were manageable with first-line analgesics, her medical or family history was unremarkable. Her family history did not indicate any potential prothrombotic conditions.
On arrival at the hospital, she was awake and oriented with a Glasgow Coma Scale (GCS) of 15 out of 15. Her vital signs and oxygen saturation were within normal limits. A neurological examination demonstrated bilateral papilledema, left-sided hemianopia, and left-sided hemiparesis. The plantar reflex was extensor on the left side.
Initial blood studies showed the following: white cell (8 × 103/μl, with lymphocyte count 7.7%, normal:4–10 × 103/μl), hemoglobin (14.9 gm/dl, normal:12–16 gm/dl), platelet (140 × 103 /mm3, normal:150–450 × 103./mm3), C-reactive protein (CRP) (40 mg/l, normal: 0–6 mg/l), erythrocyte sedimentation rate (ESR) (12 mm/hr, normal:0–30 mm/hr), lactate dehydrogenase (LDH) (751 u/l, normal: < 480 u/l), ferritin level (144 ng/ml, normal: 4–204 ng/ml), D-dimer (> 10,000 ng/ml FEU, normal: up to 500 ng/ml FEU), and normal liver function test (LFT). Viral markers including human immunodeficiency virus (HIV), the hepatitis C virus (HCV) antibody and the hepatitis B surface antigen (HBs Ag) were negative.
Due to the COVID-19 pandemic and elevated CRP, real-time reverse-transcriptase polymerase chain reaction (RT-PCR) for SARS-CoV-2 using oropharyngeal/nasopharyngeal swabs and lung high-resolution computed tomography (HRCT) was performed. RT-PCR was positive and lung HRCT revealed bilateral lower lobes subpleural bands.
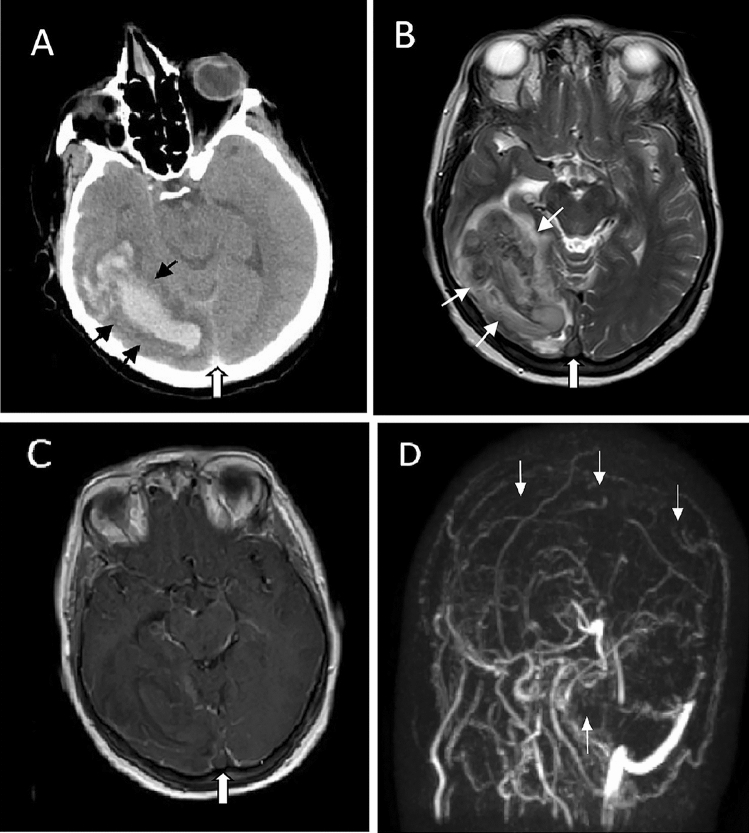
Spiral brain CT demonstrated a hemorrhagic venous infarct in the right parieto-occipital area associated with dense clot sign in the posterior part of the superior sagittal sinus (Fig. 1a). Brain MRI and MRV confirmed the diagnosis of CVST with displaying widespread thromboses in cortical veins, superior sagittal, transverse, and sigmoid sinuses (Fig. 1b–d). Consequently, the patient was promptly treated with unfractionated heparin 1000 units/hr as a continuous IV infusion, acetazolamide 250 mg P.O. twice daily, furosemide 20 mg P.O. twice daily, hypertonic saline (NaCl 5%) 1 vial IV q8h, lopinavir/ritonavir 400/100 mg P.O. twice daily, and dexamethasone 8 mg IV once daily.
Fig. 1.
a Axial non-enhanced spiral brain computed tomography (CT) scan shows a large hematoma with surrounding edema in the right parieto-occipital lobe (black thin arrows); Note the dense clot sign in the posterior part of the superior sagittal sinus, characteristic of thrombosis (white thick arrow). b Axial T2-weighted magnetic resonance (MR) image shows a large heterogeneous lesion with surrounding edema in the right parieto-occipital lobe (white thin arrows) associated with loss of signal void in the posterior region of the superior sagittal sinus (white thick arrow) suggestive of the venous sinus thrombosis with hemorrhagic venous infarction. c Axial contrast-enhanced T1-weighted MR image shows a filling defect in the posterior part of the superior sagittal sinus suggestive of thrombosis (white thick arrow). d Brain MR venography shows extensive thrombosis in the superior sagittal, right transverse, and sigmoid sinuses as well as the right internal jugular vein (white thin arrows)
On the 4th day of admission, despite receiving a therapeutic dose of anticoagulant, she was still suffering from a severe headache and developed an altered mental status. The subsequent brain CT showed slight hematoma expansion and aggravation of the brain edema. Intrasinus thrombolysis and mechanical thrombectomy were considered for her. Recombinant tissue plasminogen activator (rTPA) 20 mg was infused slowly into the superior sagittal sinus followed by manual thrombosuction with a satisfactory result. However, despite the initial recanalization, her clinical condition deteriorated within the next two days. She developed a decreased level of consciousness (GCS 8 out of 15) and gasping respiration. Afterward, she developed sustained metabolic acidosis. Mesenteric artery thrombosis could be one of the differential diagnoses; however, mesenteric artery CT angiography could not be performed owing to her poor condition.
On the 7th day of admission, she became febrile (T: 38.5 °C) and blood culture was positive for enterobacter species. Ampisulbactam 3 gr IV q8h and vancomycin 1 gr IV q12h were administered. Due to the right-sided leg swelling and significant size difference between right and left calves’ circumference, a color doppler ultrasound of both lower extremities was performed which revealed partial thrombosis of the right saphenofemoral vein.
Hypercoagulable workup was substantial for elevated lupus anticoagulant (> 120 s, normal: 28–45 s), positive anti-phospholipid IgM antibody (1.3, normal: < 1.2), antinuclear antibody (1.5, normal: < 1.2), and anti-double-stranded DNA (27 IU/ml, normal: < 18 IU/ml). The other vasculitis and hypercoagulable markers were normal.
The brain CT on the 8th day demonstrated evidence of a midline shift to the left side about 10 mm. She underwent a decompressive craniectomy. On the ninth day of admission, she became hypotensive and had coffee-ground nasogastric tube drainage. Blood investigation showed leukocytosis (13.8 × 103/ul), significant hemoglobin drop (from 14.9 to 10.3 gm/dl), thrombocytopenia (65 × 103/mm3), elevated partial thromboplastin time (159 s, normal:25–36 s), and prothrombin time (22.8, normal:10–13 s) as well as low fibrinogen level (102 mg/dl, normal: 200-400 mg/dl). The putative differential diagnosis was septic shock and disseminated intravascular coagulation (DIC). She died on the 10th day of admission.
Discussion
This study represents a case series of CVST associated with SARS-CoV-2 infection, diagnosed and treated at multiple institutions throughout Iran. We provided a brief overview of all previously reported cases in Table 2 as well [6–18].
Table 2.
A brief overview of clinical features and outcomes of the published cases diagnosed with CVST and COVID-19
| Case Number/Country | Age & Sex | COVID-19 Clinical Symptoms* | Confirmatory COVID-19 Results | CVST Clinical Syndrome** | Baseline Parenchymal Lesions (Hemorrhagic or infarct) | CVST Tempo*** | Interval Between COVID-19 and CVST (days) | CVST Radiological Features | CVST Predisposing Factors # | Other Thrombotic Events | Significant Thrombophilia Laboratories | Treatment for | Mortality | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nasopharyngeal Swab PCR | Chest HRCT | Positive Serum Antibody | COVID-19 | CVST | ||||||||||||
| Baudar, et al. [6] Belgium | 33 Y/O, F | Respiratory | + | − | + | C | Yes (Infarct) | Subacute | 21 | Cortical Veins | Female Gender Related Causes, Obesity | NM | Elevated D-dimer, Elevated fibrinogen | NM | Dabigatran | - |
| Klein, et al. [7] United States | 29 Y/O, F | Respiratory | + | + | NM | A | Yes (Hemorrhagic) | Subacute | 7 | Multiple Sinuses | Hematologic Diseases | NM | Lymphopenia, Elevated CRP, Elevated D-dimer, Elevated LDH, Elevated Antiphospholipid Antibody | NM | Unfractionated Heparin, LMWH | - |
| Garaci, et al. [8] Italy | 44 Y/O, F | Respiratory | + | + | + | A | NM | Subacute | 14 | Multiple Sinuses | Idiopathic | Disseminated Intravascular Coagulation, Superior Vena Cava & Right Pulmonary Artery Thrombosis | Lymphopenia, Thrombocytopenia, Elevated D-dimer | Hydroxychloroquine, Azithromycin, Tocilizumab | LMWH | NM |
| Hughes, et al. [9] UK | 59 Y/O, M | Non-respiratory | + | NM | NM | A | NM | Subacute | 0 | Multiple Sinuses | Idiopathic | NM | Elevated CRP, Elevated fibrinogen | NM | LMWH | - |
| Cavalcanti, et al. [10] United States | 38 Y/O, M | Non-respiratory | + | + | NM | B | No | Subacute | 3 | Multiple Sinuses | Dehydration | NM | Lymphopenia, Thrombocytopenia, Elevated D-dimer | Lopinavir-Ritonavir | LMWH, Endovascular Intervention (Thrombectomy) + tPA | + |
| Cavalcanti, et al. [10] United States | 41 Y/O, F | NM | NM | + | NM | A | Yes (Hemorrhagic) | Acute | NM | Multiple Sinuses | Female Gender Related Causes | NM | Lymphopenia, Elevated D-dimer | Hydroxychloroquine, Azithromycin | Unfractionated Heparin, Neurosurgical Intervention (Craniectomy, Ventriculostomy) | + |
| Cavalcanti, et al. [10] United States | 23 Y/O, M | Respiratory | + | NM | NM | D | Yes (Hemorrhagic) | Subacute | 7 | Multiple Sinuses | Dehydration | NM | Thrombocytopenia, Elevated D-dimer | Hydroxychloroquine, Azithromycin | NM | + |
| Hemasian and Ansari [11] Iran | 65 Y/O, M | Non-respiratory | + | + | NM | A | Yes (Hemorrhagic) | Acute | 0 | Multiple Sinuses | Idiopathic | NM | Lymphopenia, Elevated LDH | Hydroxychloroquine, Co-amoxiclave | Anticoagulant Therapy (NM) | - |
| Poillon, et al. [12] France | 62 Y/O, F | Respiratory | + | + | NM | A | Yes (Hemorrhagic) | Acute | 15 | Multiple Sinuses | Obesity | NM | Elevated D-dimer | NM | NM | NM |
| Poillon, et al. [12] France | 54 Y/O, F | Respiratory | NM | + | NM | A | Yes (Hemorrhagic) | Acute | 14 | Single Sinus | Malignancies | NM | Elevated CRP, Elevated D-dimer | NM | NM | NM |
| Malentacchi, et al. [13] Italy | 81 Y/O, M | Respiratory | + | NM | NM | D | Yes (Infarct) | Subacute | Few Days | Single Sinus | Malignancies, Drug-induced | Arterial Stroke | Elevated CRP, Elevated D-dimer, Elevated LDH, Elevated fibrinogen | Darunavir/Ritonavir, Hydroxychloroquine, Steroid | Anticoagulant Therapy (NM) | + |
| Bolaji, et al. [14] UK | 63 Y/O, M | Respiratory | + | NM | NM | A | Yes (Hemorrhagic) | Acute | 7 | Multiple Sinuses | Idiopathic | NM | Lymphopenia, Elevated CRP, Elevated D-dimer, Elevated Ferritin, Elevated Lupus Anticoagulant, Elevated fibrinogen | Clarithromycin | LMWH, Edoxaban | - |
| Roy-Gash, et al. [15] France | 63 Y/O, F | Respiratory | − | + | + | A | Yes (Hemorrhagic) | Acute | 12 | Multiple Sinuses | Idiopathic | NM | Elevated Ferritin, Elevated fibrinogen | NM | Unfractionated Heparin, Neurosurgical Intervention (Craniectomy, Ventriculostomy) | + |
| Aghayari Sheikh Neshin, et al. [16] Iran | 43 Y/O, F | Non-respiratory | + | + | NM | A | Yes (Infarct) | Acute | 0 | Multiple Sinuses | Idiopathic | NM | Elevated CRP, Elevated LDH | Hydroxychloroquine, Oseltamivir,Ceftriaxone | LMWH | - |
| Sugiyama, et al. [17] Japan | 56 Y/O, M | Respiratory | + | + | NM | C | NM | Acute | 16 | Single Sinus | Idiopathic | Bilateral Pulmonary Embolism | Elevated CRP, Elevated D-dimer, Elevated Ferritin | Ciclesonide, Azithromycin, Favipiravir, Methylprednisolone | Unfractionated Heparin, Edoxaban | - |
| Mowla, et al., [18] Iran, Singapore, and the United States | 32–71 Y/O, 8 F & 5 M | 1, no Symptom 12, Respiratory | + for 12 | NM | NM | 6, A 7, B | 6 Yes (4, Hemorrhagic; 2, Infarct), 7, No | NM | Range: 1–14 Days | 4, Multiple Sinuses 9, Single Sinus | 3, Female Gender Related Causes 10, None Reported | None | D-dimer, 3/13 Avaiable and All Elevated CRP, 12/13 Avaibable and in 11 /12 Were Elevated Lymphopenia, 4/13 Thrombocytopenia, Data Available in 12/13, and 1/12 had Thrombocytopenia | NM | 12, Anticoagulant Therapy (NM) 1, Anticoagulant Therapy (NM) + Neurosurgical Intervention (Craniectomy, Ventriculostomy) | 3/13 Died |
CVST cerebral venous sinus thrombosis, COVID-19 Coronavirus Disease 2019, F Female, M Male, PCR polymerase chain reaction, HRCT high-resolution computed tomography, NM: not mentioned
*Non-respiratory: (headache, malaise, neurological symptoms, decrease level of consciousness, gastrointestinal symptom); **CVST clinical syndrome: A—stroke-like: Brain Infarct with or without hemorrhagic transformation and focal neurologic deficit; B—raised intracranial pressure syndrome (RICP); C—encephalopathy syndrome with no brain infarct or RICP; D—particular syndromes (cavernous sinus syndrome, inferior petrosal sinus syndrome,…)
***CVST Tempo: acute (< 48 h); subacute (48 h to 30 days)
#Female gender-related causes: (pregnancy, post-partum and oral contraceptive pill (OCP) use); LMWH: low-molecular weight heparin; tPA: tissue plasminogen activator
Several months after the spread of SARS-CoV-2, the association of the infection with thromboembolic events such as cerebrovascular disease seems to be stronger than considered incidental. SARS-CoV-2 infection can deplete angiotensin-converting enzyme 2 (ACE2) via receptor engulfment, make ACE1 unopposed with the production of angiotensin II, and induce thrombosis as a result [23]. Sepsis-induced coagulopathy (SIC) is associated with the SARS-CoV-2 infection. Both viral particles and damage-associated molecular patterns can trigger the coagulation pathway via an inflammatory cascade [24]. There are some reports on the possible role of antiphospholipid antibodies and lupus anticoagulants in arterial stroke associated with SARS-CoV-2 infection as well [25]. Hence, it seems that a hypercoagulable and hyperinflammatory state following SARS-CoV-2 infection might be associated with CVST; as reported in some cases with COVID-19 and ischemic stroke [26].
Whether SARS-CoV-2 infection “triggers” the coagulation cascade in patients with other underlying diseases or directly “causes” CVST remains to be elucidated [27]. Since 48% of the cumulative data (data of CVST associated with COVID-19) group had other predisposing factors for CVST, the role of SARS-CoV-2 as a principal contributor versus an additive factor is still unclear.
The mean age of the patients in the CVST associated with COVID-19 group is greater than the former reports of CVST without SARS-CoV-2 infection (49.26 vs. 37.77 years old). Since older patients seem to be more susceptible to SARS-CoV-2 infection [28], the mean age of CVST patients is expected to be higher in the setting of SARS-CoV-2 infection. Meanwhile, the proportion of women was much higher in the former reports of CVST without COVID-19 (2.19 vs. 1.42). Given that men are more vulnerable to the severe consequences of COVID-19 [29] and as mentioned before, the incidence of thrombotic events is greater in seriously affected patients with COVID-19 [30], a reduction in the dominance of women over men in the context of SARS-CoV-2 infection might be reasonable.
Besides, three patients of the current study and three of the previously reported cases developed other thrombotic events such as deep vein thrombosis, pulmonary thromboembolism, or arterial thrombosis, simultaneously with CVST or during hospitalization. It might be due to a higher load of thrombophilia caused by SARS-CoV-2 [27].
The mortality rate in CVST associated with SARS-CoV-2 infection is higher (35.29%) than the former reports of CVST (6.07%) (shown in Table 3). A higher burden of thrombosis, the involvement of several dural sinuses, and the wide range of COVID-19 complications [31] may contribute to the worse outcomes in these patients. These complications demand a high level of vigilance from physicians about CVST in COVID-19 patients.
The lack of respiratory symptoms of COVID-19 has been observed in four of our patients and four of the previously reported cases, indicating the absence of correlation between the presence of the respiratory symptoms and the risk of developing CVST. Besides, in five cases of the current series and three of the previously reported cases, there was no gap between the diagnosis of COVID-19 and CVST, suggesting that CVST might be the primary manifestation of COVID-19. Therefore, a high level of suspicion of SARS-CoV-2 infection is essential in all patients with CVST within the pandemic.
Endovascular intervention was performed for one of our patients (case no.1 in Table 1) and one of the patients reported by Cavalcanti et al. [10] with relative success and recanalization of the thrombosed sinuses; however, the patients’ outcomes were not changed and both patients died.
As limitations of the current study, some inflammatory or coagulation biomarkers of the patients were missing. This can be justified because of the dismal clinical condition of some of our patients. Meanwhile, we did not have more accurate diagnostic modalities than brain CT scan to diagnose CVST due to unanticipated death in two patients.
As a major drawback, it should be stressed that with the small sample size of the current study and with the non-matched control group of patients with CVST not associated with COVID-19 from previous studies, it is impossible to speculate about the causative effect of COVID-19 on CVST. Besides, three out of the six patients had known predisposing factors for CVST. It also may be against the causative speculation. In the same way, it cannot be concluded that COVID-19 has any detrimental effect on CVST natural history. Larger case-controlled studies about this “association” are highly recommended.
Nevertheless, based on the current small series, in the COVID-19 pandemic era, a high index of suspicion of CVST should be considered [32], particularly in patients with headache, focal neurological deficit, symptoms/signs of increased intracranial pressure, and encephalopathy; whether they present respiratory symptoms of SARS-CoV-2 infection or not.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by MAD, ME, AAB, ZB, FF, HM, ARJ, MP, NF, MB, MO, MSS, SSZ, FM, AS, SS, AM, MRA, and RZ. The first draft of the manuscript was written by ABH, EH, VRO, RF, MR, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
None.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This study was approved by the ethics committee and institutional review board of Shiraz University of Medical Sciences (IR.sums.rec.1399–235).
Informed consent
For this type of study, formal consent is not required.
Footnotes
Vahid Reza Ostovan, Razieh Foroughi, and Mahtab Rostami have contributed equally to this work and should be considered as co-first authors.
Contributor Information
Etrat Hooshmandi, Email: ehoshmandi@gmail.com.
Afshin Borhani-Haghighi, Email: neuro.ab@gmail.com.
References
- 1.Wasay M, Kaul S, Menon B, Dai AI, Saadatnia M, Malik A, et al (2019) Asian study of cerebral venous thrombosis. J Stroke Cerebrovasc Dis Off J Natil Stroke Assoc 28(10):104247 [DOI] [PubMed]
- 2.Ashjazadeh N, Borhani-Haghighi A, Poursadeghfard M, Azin H. Cerebral venous-sinus thrombosis: a case series analysis. Iran J Med Sci. 2011;36(3):178–182. [PMC free article] [PubMed] [Google Scholar]
- 3.Borhani-Haghighi A, Edgell RC, Cruz-Flores S, Feen E, Piriyawat P, Vora N, et al. Mortality of cerebral venous-sinus thrombosis in a large national sample. Stroke. 2012;43(1):262–264. doi: 10.1161/STROKEAHA.111.635664. [DOI] [PubMed] [Google Scholar]
- 4.Borhani-Haghighi A, Ashjazadeh N, Safari A, Cruz-Flores S. Cerebral venous sinus thrombosis in iran: cumulative data, shortcomings and future directions. Iran Red Crescent Med J. 2012;14(12):805–810. doi: 10.5812/ircmj.3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gklinos P. Neurological manifestations of COVID-19: a review of what we know so far. J Neurol. 2020;26:1–5. doi: 10.1007/s00415-020-09939-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baudar C, Duprez T, Kassab A, Miller N, Rutgers MP. COVID-19 as triggering co-factor for cortical cerebral venous thrombosis? J Neuroradiol. 2020;S0150–9861(20):30205–30214. doi: 10.1016/j.neurad.2020.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klein DE, Libman R, Kirsch C, Arora R (2020) Cerebral venous thrombosis: a typical presentation of COVID-19 in the young. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc 29(8):104989 [DOI] [PMC free article] [PubMed]
- 8.Garaci F, Di Giuliano F, Picchi E, Da Ros V, Floris R. Venous cerebral thrombosis in COVID-19 patient. J Neurol Sci. 2020;414:116871. doi: 10.1016/j.jns.2020.116871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hughes C, Nichols T, Pike M, Subbe C, Elghenzai S. Cerebral venous sinus thrombosis as a presentation of COVID-19. Eur J Case Rep Intern Med. 2020;7(5):001691. doi: 10.12890/2020_001691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cavalcanti DD, Raz E, Shapiro M, Dehkharghani S, Yaghi S, Lillemoe K, et al. Cerebral venous thrombosis associated with COVID-19. AJNR Am J Neuroradiol. 2020;41(8):1370–1376. doi: 10.3174/ajnr.A6644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hemasian H, Ansari B. First case of Covid-19 presented with cerebral venous thrombosis: a rare and dreaded case. Rev Neurol (Paris) 2020;176(6):521–523. doi: 10.1016/j.neurol.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Poillon G, Obadia M, Perrin M, Savatovsky J, Lecler A. Cerebral venous thrombosis associated with COVID-19 infection: causality or coincidence? J Neuroradiol. 2020 doi: 10.1016/j.neurad.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malentacchi M, Gned D, Angelino V, Demichelis S, Perboni A, Veltri A, et al. Concomitant brain arterial and venous thrombosis in a COVID-19 patient. Eur J Neurol. 2020 doi: 10.1111/ene.14380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bolaji P, Kukoyi B, Ahmad N, Wharton C. Extensive cerebral venous sinus thrombosis: a potential complication in a patient with COVID-19 disease. BMJ Case Rep. 2020;13(8):e236820. doi: 10.1136/bcr-2020-236820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roy-Gash F, De Mesmay M, Devys JM, Vespignani H, Blanc R, Engrand N. COVID-19-associated acute cerebral venous thrombosis: clinical, CT, MRI and EEG features. Crit Care. 2020;24(1):419. doi: 10.1186/s13054-020-03131-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aghayari Sheikh Neshin S, Basirjafari S, Saberi A, Shahhosseini B, Zarei M. Liver abnormality may develop cerebral vein thrombosis in COVID-19. J Neurol Sci. 2020;417:117076. doi: 10.1016/j.jns.2020.117076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sugiyama Y, Tsuchiya T, Tanaka R, Ouchi A, Motoyama A, Takamoto T, et al. Cerebral venous thrombosis in COVID-19-associated coagulopathy: a case report. J Clin Neurosci. 2020;79:30–32. doi: 10.1016/j.jocn.2020.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mowla A, Shakibajahromi B, Shahjouei S, Borhani-Haghighi A, Rahimian N, Baharvahdat H, et al (2020) Cerebral venous sinus thrombosis associated with SARS-CoV-2; a multinational case series. J Neurol Sci:117183 [DOI] [PMC free article] [PubMed]
- 19.Ellul MA, Benjamin L, Singh B, Lant S, Michael BD, Easton A, et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19(9):767–783. doi: 10.1016/S1474-4422(20)30221-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Saposnik G, Barinagarrementeria F, Brown RD, Jr, Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(4):1158–1192. doi: 10.1161/STR.0b013e31820a8364. [DOI] [PubMed] [Google Scholar]
- 21.Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT) Stroke. 2004;35(3):664–670. doi: 10.1161/01.STR.0000117571.76197.26. [DOI] [PubMed] [Google Scholar]
- 22.Shakibajahromi B, Borhani-Haghighi A, Salehi A, Vardanjani HM, Ghaedian M, Safari A, et al. Clinical and radiological characteristics and predictors of outcome of cerebral venous sinus thrombosis, a hospital-based study. Acta Neurol Belg. 2020;120(4):845–852. doi: 10.1007/s13760-018-1009-6. [DOI] [PubMed] [Google Scholar]
- 23.Kim JS. Coronavirus disease 2019 and stroke. J Stroke. 2020;22(2):157–158. doi: 10.5853/jos.2020.01760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iba T, Levy JH, Levi M, Thachil J. Coagulopathy in COVID-19. J Thromb Haemost. 2020;18(9):2103–2109. doi: 10.1111/jth.14975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rothstein A, Oldridge O, Schwennesen H, Do D, Cucchiara BL. Acute cerebrovascular events in hospitalized COVID-19 patients. Stroke. 2020;51(9):e219–e222. doi: 10.1161/STROKEAHA.120.030995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beyrouti R, Adams ME, Benjamin L, Cohen H, Farmer SF, Yen Goh Y, et al. Characteristics of ischaemic stroke associated with COVID-19. J Neurol Neurosurg Psychiatry. 2020;91(8):889–891. doi: 10.1136/jnnp-2020-323586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bhatia R, Srivastava MVP. COVID-19 and stroke: incidental, triggered or causative. Ann Indian Acad Neurol. 2020;23(3):318–324. doi: 10.4103/aian.AIAN_380_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang J, Wang X, Jia X, Li J, Hu K, Chen G, et al. Risk factors for disease severity, unimprovement, and mortality in COVID-19 patients in Wuhan. China Clin Microbiol Infect. 2020;26(6):767–772. doi: 10.1016/j.cmi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, et al. Clinical characteristics of covid-19 in New York City. N Engl J Med. 2020;382(24):2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Klok FA, Kruip M, van der Meer NJM, Arbous MS, Gommers D, Kant KM, et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: an updated analysis. Thromb Res. 2020;191:148–150. doi: 10.1016/j.thromres.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McIntosh K, Hirsch MS, Bloom A. Coronavirus disease 2019 (COVID-19): epidemiology, virology, clinical features, diagnosis, and prevention. Lancet Infect Dis. 2020;1:2019–2020. [Google Scholar]
- 32.Shakibajahromi B, Borhani-Haghighi A, Haseli S, Mowla A (2020) Cerebral venous sinus thrombosis might be under-diagnosed in the COVID-19 era. eNeurological Sci 20:100256. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.