Abstract
OBJECTIVES:
Effective communication is critical for safely discharging hospitalized children, including those with limited English proficiency (LEP), who are at high risk of reuse. Our objective was to describe and compare the safety and family centeredness of nurse communication at hospital discharge for English-proficient (EP) and LEP families.
METHODS:
In this single-center, cross-sectional study, we used direct observation of hospital discharges for EP and LEP children. Observers recorded quantitative and qualitative details of nurse-family communication, focusing on 3 domains: safe discharge, family centeredness, and family engagement. Patient characteristics and percentages of encounters in which all components were discussed within each domain were compared between EP and LEP encounters by using Fisher’s exact tests. We used field notes to supplement quantitative findings.
RESULTS:
We observed 140 discharge encounters; 49% were with LEP families. Nurses discussed all safe discharge components in 31% of all encounters, most frequently omitting emergency department return precautions. Nurses used all family-centered communication components in 11% and family-engagement components in 89% of all encounters. Nurses were more likely to discuss all components of safe discharge in EP encounters when compared with LEP encounters (53% vs 9%; P < .001; odds ratio: 11.5 [95% confidence interval 4.4–30.1]). There were no differences in family centeredness or family engagement between LEP and EP encounters.
CONCLUSIONS:
Discharge encounters of LEP patients were less likely to include all safe discharge communication components, compared with EP encounters. Opportunities to improve nurse-family discharge communication include providing written discharge instructions in families’ primary language, ensuring discussion of return precautions, and using teach-back to optimize family engagement and understanding.
For hospitalized children and their families, the discharge process is inherently complex. Hospital discharge involves an extensive exchange of information between providers and families and offers an opportunity to bolster caregiver understanding of and confidence in executing postdischarge care plans.1–3 Ideally, all information critical to a patient’s safe discharge is accurately and thoroughly reviewed, including the discharge diagnosis, home instructions, follow-up appointments, return precautions, and discharge medications.2,3 Information should be reinforced via written discharge documentation in the family’s preferred language that is readable and understandable.3,4 Finally, communication should be family centered to optimize understanding, engagement, and collaboration, which are crucial for an effective discharge.3,5,6
Discharge communication challenges are likely amplified for families with limited English proficiency (LEP) because language barriers put them at increased risk for communication failures. In fact, LEP patients experience more frequent emergency department (ED) revisits7 and medication dosing errors.8 Despite multiple regional and federal efforts focused on improving access to interpreters,9–12 providers’ use of interpreters and communication with LEP families remain suboptimal, and up to 57% of pediatricians rely on English-speaking family members to communicate with LEP families.9 Furthermore, LEP parents report being less knowledgeable about care plans and perceive that medical staff spend less time with them than with their English-proficient (EP) counterparts.13
Despite known health care disparities for hospitalized LEP families, little is known about provider behavior and communication practices at the time of discharge. Characterizing communication practices at discharge is an important first step toward promoting a safer and more family-centered discharge process for LEP families. Thus, we aimed to describe and compare the safety and family centeredness of nurse communication and the level of family engagement during the discharge process for EP and LEP families.
Methods
Study Design
We conducted a cross-sectional study using direct structured observation of discharge encounters to characterize and compare nurse communication to a purposive sample of hospitalized EP and LEP pediatric patients and their parents at the time of discharge. This study design allowed us to (1) directly assess behavior in real time without relying on individual patient or nurse recollection, which may be subject to bias, and (2) examine the use of interpreters without having to assume quality interpretation or rely on an interpreter to gain that information.
Setting
This study was conducted at both the main and satellite campuses of a large children’s hospital in the Midwest with >600 registered beds. Approximately 7000 pediatric patients are discharged with common pediatric diagnoses each year; of those, ∼5% have LEP. Three interpretation modalities (in-person, video, and phone) are available, and written discharge instructions can be translated to an LEP family’s primary language by request. At the time of discharge, bedside nurses review written discharge instructions and the after-visit summary (AVS), prepared by the primary medical team, with patients and parents and address the family’s questions and concerns.
Study Population
We included EP and LEP discharge encounters for patients between the ages of 0 and 18 years hospitalized with common pediatric diagnoses (eg, asthma, dehydration, and appendicitis). Although the discharge process involves multiple stakeholders (ie, physicians, nurse practitioners, bedside nurses, interpreters, and language access services), for the purposes of our study, a discharge encounter was defined as the discrete period of time when the nurse reviews the discharge instructions and AVS with the family. The family was defined as the patient and/or the patient’s parents, whereas parents included family members or other individuals with an active role in the patient’s care after discharge. LEP families were defined as families who required use of an interpreter for medical communication at any point during the hospitalization. If a patient had both EP and LEP parents present at the time of discharge, the encounter was categorized as LEP. All languages and interpretation modalities were included to capture language and/or modality-specific communication challenges. Patients with complex chronic conditions and technology dependence (eg, chronic ventilator support or gastrostomy tube) were excluded because these discharges are prohibitively complicated to adequately capture with our observation method, given the involvement of multiple subspecialists, extensive care coordination, and patient education that is often segmented and dispersed throughout hospitalization (eg, tracheostomy teaching).14 This study was approved by the hospital’s institutional review board.
Measures
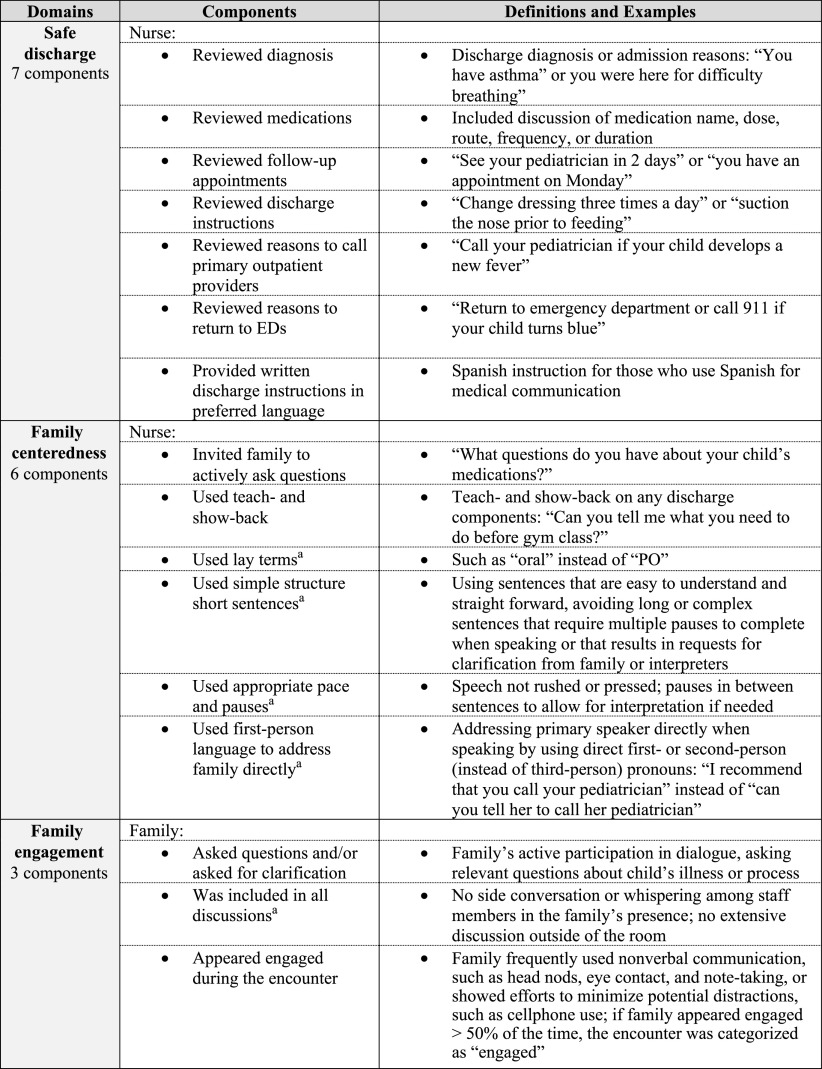
Patient demographics and clinical characteristics (age, sex, primary language, length of stay, insurance type, and discharge diagnosis) were extracted from the electronic health record (EHR). Quantitative measures of discharge communication were developed a priori from a review of the literature,2,3,5,15 local needs assessment,16 and local physician and nursing peer review to establish face validity. These measures included 3 domains: safe discharge, family centeredness, and family engagement. Definitions and examples of these measures are included in Fig 1. Qualitative data, including details about each encounter (eg, relevant clinical context, details about parents, and medical providers present) were collected as field notes to supplement quantitative findings. For LEP encounters, the observer recorded the presence of the interpreter, modality of the interpreter, language, and detail on interpreter-provider interactions, when appropriate. Questions from the observation checklist are included in Supplemental Fig 2.
FIGURE 1.
Measures of quality discharge communication: definitions and examples. a Initial data were recorded on a 4-point Likert scale: never, occasionally or sometimes, majority or most of the time, or all the time. PO, by mouth.
Data Collection
Between June 21, 2018, and May 25, 2019, we prospectively identified potentially eligible patients ready for discharge using the anticipated discharge date and discharge criteria entered at each patient’s admission into our EHR,17 followed by confirmation with the charge nurse, primary physician team, and bedside nurse. We used purposive sampling with a targeted approach to capture the variety of age ranges and diagnoses that were matched between EP and LEP patients. On the basis of preliminary observations revealing 80% of EP encounters discussed all safe discharge components, we aimed to observe 62 encounters per group to provide the power of 80% to detect a 25% between-group difference for this component. A subset of observations had duplicate observations to test interobserver reliability (κ ≥ 0.7; Supplemental Table 3). Trained observers (A.Y.C., E.A., V.W., M.D., and D.M., consisting of 1 physician, 1 medical student, and 3 trained research assistants) collected observation data using a structured form in a secure Web-based Research Electronic Data Capture database.18 To supplement structured observation findings, observers recorded detailed field notes and prompted nurses to provide clarifying comments or reflections after each encounter. Of note, the nurse and family were aware that the observer was evaluating the discharge process but were unaware of the specific objectives or data collected.
Analysis
Demographic data, patient characteristics, and discharge communication components were assessed by using descriptive statistics. Diagnoses were categorized by using the Clinical Classifications Software.19 Comparison of EP and LEP encounters were conducted by using Fisher’s exact test for categorical variables and Wilcoxon rank test for continuous variables. Odds ratios were developed by using logistic regression, with each of the component outcome variables and EP and LEP group as the predictor variable (SAS version 9.4; SAS Institute, Inc, Cary, NC). The study team reviewed field notes to supplement and provide context for quantitative findings.
Results
Demographics and Clinical Characteristics
A total of 140 discharges were observed, which involved 87 nurses. A total of 72 discharge encounters were categorized as EP, and 68 were categorized as LEP. The median patient age was 3.5 years (interquartile range [IQR] 0.4–10.2), and most patients were boys (59%), non-Hispanic (64%), and publicly insured (65%; Table 1). The most common primary diagnoses involved the respiratory (31%) and digestive (12%) systems; diagnoses were similar between the EP and LEP groups. The median length of stay was 42 hours (IQR 29–68), and the median encounter duration was 9 minutes (IQR 7–13). Of the 68 LEP encounters, Spanish was as the primary language in 34%, and an interpreter was used in 63%. The LEP discharge encounters were significantly longer than the EP encounters (11 minutes [IQR 9–16] vs 8 minutes [IQR 5–1]; P <.01). LEP families, compared with EP families, were mostly Hispanic (71% vs 1%) and less likely to be insured privately (10% vs 42%). Additional demographic characteristics are summarized in Table 1.
TABLE 1.
Patient Demographics and Clinical Characteristics Within Observed Discharge Encounters
| Characteristic | Overall (n = 140) | EP (n = 72) | LEP (n = 68) | Pa |
|---|---|---|---|---|
| Patient demographics | ||||
| Male sex, n (%) | 83 (59) | 40 (56) | 43 (63) | .392 |
| Age, median (IQR), y | 3.5 (0.4–10.2) | 4.1 (0.3–12.6) | 2.6 (0.7–8.4) | .591 |
| Race, n (%) | <.001 | |||
| White | 65 (46) | 54 (75) | 11 (16) | — |
| Black or African American | 19 (14) | 15 (21) | 4 (6) | — |
| Otherb | 56 (40) | 3 (4) | 53 (78) | — |
| Ethnicity, n (%) | <.001 | |||
| Hispanic | 49 (35) | 1 (1) | 48 (71) | — |
| Non-Hispanic | 90 (64) | 70 (97) | 20 (29) | — |
| Unknown | 1 (1) | 1 (1) | 0 (0) | — |
| Primary insurance, n (%) | <.001 | |||
| Public | 91 (65) | 36 (56) | 30 (75) | — |
| Private | 36 (30) | 27 (42) | 4 (10) | — |
| International | 1 (1) | 0 (0) | 1 (2) | — |
| Other or unknown | 12 (9) | 2 (3) | 10 (15) | — |
| Patient clinical characteristics, n (%) | ||||
| Primary diagnosis type | .084 | |||
| Infectious and parasitic | 5 (4) | 3 (4) | 2 (3) | — |
| Endocrine and immunity | 9 (6) | 6 (8) | 3 (4) | — |
| Blood | 1 (1) | 1 (1) | 0 (0) | — |
| Mental | 1 (1) | 1 (1) | 0 (0) | — |
| Nervous system | 8 (6) | 3 (4) | 5 (7) | — |
| Circulatory | 1 (1) | 1 (1) | 0 (0) | — |
| Respiratory | 43 (31) | 21 (29) | 22 (32) | — |
| Digestive | 17 (12) | 4 (6) | 13 (19) | — |
| Genitourinary | 9 (6) | 4 (6) | 5 (7) | — |
| Skin and subcutaneous | 11 (8) | 9 (13) | 2 (3) | — |
| Musculoskeletal and connective | 6 (4) | 4 (6) | 2 (3) | — |
| Congenital anomalies | 2 (1) | 0 (0) | 2 (3) | — |
| Perinatal | 12 (9) | 9 (13) | 3 (4) | — |
| Injury and poisoning | 9 (6) | 3 (4) | 6 (9) | — |
| Others | 6 (4) | 3 (4) | 3 (4) | — |
| Length of stay, median (IQR), h | 42 (29–68) | 42 (32–57) | 4 7(28–78) | .381 |
| Discharge encounter characteristics, n (%) | ||||
| Family members presentc | .217 | |||
| Primary female parent only | 55 (39) | 32 (44) | 23 (34) | — |
| Primary male parent only | 15 (11) | 9 (13) | 6 (9) | — |
| No caregiver present | 1 (1) | 1 (2) | 0 (0) | — |
| Multiple people present | 69 (49) | 30 (42) | 39 (57) | — |
| Encounter languages (patient and family) | <.001 | |||
| English onlyd | 72 (51) | 70 (97) | 2 (3) | — |
| Spanish | 48 (34) | 0 (0) | 48 (71) | — |
| Other languagese | 20 (14) | 2 (3) | 18 (27) | — |
| Campus | .028 | |||
| Main | 107 (76) | 61 (85) | 46 (68) | — |
| Satellitef | 33 (24) | 11 (15) | 22 (32) | — |
| Encounter duration, median (IQR), min | 9 (7–13) | 8 (5–11) | 11 (9–16) | <.001 |
—, not applicable.
P values are from χ2 or Fisher’s exact test for categorical variables and Wilcoxon rank test for continuous variables.
Included Middle Eastern, Asian American, Hispanic, and unknown as denoted in the EHR.
The primary female parent includes biological mom, grandmother, or other primary female legal guardians or caregivers; the primary male parent includes biological dad, grandfather, or other primary male legal guardians or caregivers.
In 2 LEP encounters, only English was used despite the presence of an LEP family member or existing nursing concern about limited comprehension due to language barrier.
Included Chinese, Korean, Japanese, Arabic, Russian, French, Nepali, Burmese and/or Hakha Chin, and German; 2 EP families were fluent in multiple languages as hence categorized under “other languages.”
Most physicians work at both the main and satellite campuses; the nurses typically work only at 1 campus. None of the nurses observed in either campuses were certified bilingual providers (certified by language access services to communicate with families without the use of a professional interpreter).
Safe Discharge
In the safe discharge domain, nurses discussed all 7 components in 31% of encounters, most often omitting discussion of ED return precautions (missing in 56%; Table 2). Nurses discussed all 7 components of safe discharge in 53% of EP encounters versus 9% of LEP encounters (P < .001; odds ratio [OR]: 11.5; 95% confidence interval [CI] 4.4–30.1). Nurses discussed return precaution to the ED less frequently in LEP encounters compared with EP encounters (43% of LEP encounters versus 68% of EP encounters; P = .004). Although written discharge instructions were provided in all encounters, only 27% of LEP patients, compared with 99% of EP patients, received discharge instructions in their primary language (P < .001). Field notes revealed that nurses relied heavily on written instructions for the order and content of the safe discharge components discussed with families.
TABLE 2.
Quality Discharge Communication Measures: Domains and Components
| Characteristics | Overall (n = 140), n (%) | EP (n = 72), n (%) | LEP (n = 68), n (%) | Pa | OR (95% CI) |
|---|---|---|---|---|---|
| Safe discharge | |||||
| All componentsb | 44 (31) | 38 (53) | 6 (9) | <.001 | 11.5 (4.4–30.1) |
| Diagnosis | 99 (71) | 52 (72) | 47 (69) | .714 | NA |
| Medicationc | 123 (98) | 59 (98) | 64 (97) | 1.000 | NA |
| Home instructions | 129 (92) | 67 (93) | 62 (92) | .760 | NA |
| Follow-up appointments | 136 (97) | 71 (99) | 65 (96) | .356 | NA |
| Reasons to call primary outpatient providers | 122 (87) | 66 (92) | 56 (82) | .131 | NA |
| Reasons to return to ED | 78 (56) | 49 (68) | 29 (43) | .004 | NA |
| Written instructions in primary language | 89 (64) | 71 (99) | 18 (27) | <.001 | NA |
| Family centeredness | |||||
| All components | 15 (11) | 7 (10) | 8 (12) | .788 | 0.8 (0.3–2.4) |
| Active invitation to family for questions | 134 (96) | 70 (97) | 64 (94) | .432 | NA |
| Teach- and show-back | 15 (11) | 7 (10) | 8 (12) | .788 | NA |
| First-person languaged | 138 (99) | 72 (100) | 66 (97) | .234 | NA |
| Lay termsd | 140 (100) | 72 (100) | 68 (100) | NA | NA |
| Simple structure, short sentenced | 140 (100) | 72 (100) | 68 (100) | NA | NA |
| Appropriate pace and pausesd | 140 (100) | 72 (100) | 68 (100) | NA | NA |
| Family engagement | |||||
| All components | 124 (89) | 62 (86) | 62 (91) | .430 | 0.6 (0.2–1.8) |
| Asked questions or provided clarification | 125 (89) | 62 (86) | 63 (93) | .277 | NA |
| Family was included in all discussiond | 139 (99) | 72 (100) | 67 (99) | .486 | NA |
| Appear engaged during the encounter | 140 (100) | 72 (100) | 68 (100) | NA | NA |
NA, not applicable; —, not applicable.
P values are from χ2 or Fisher’s exact test.
Not all encounters had medications. For encounters with no medications, if the other 6 components were discussed, the encounter was considered to have all components of safe discharge domain.
Fourteen patients did not have discharge medications (N = 126; EP: n = 60; LEP: n = 66).
Initial data were recorded on a 4-point Likert scale that was then dichotomized with the component considered to be present for all the time and majority or most of the time and absent for occasionally or sometime and never.
Family Centeredness
In the family-centeredness domain, nurses used all 6 components in only 11% of encounters, primarily because of the infrequent use of teach-back. There was no significant difference between EP and LEP encounters for the use of all components (10% vs 12%; P = .788; OR: 0.8; 95% CI 0.3–2.4; Table 2). Teach-back was used in 11% of encounters. Nurses were observed to use lay terms, appropriate pace, and pauses in all EP and LEP encounters. First-person language, defined as addressing the primary speaker directly, whether it be patients or parents, and active invitation of family members to ask questions and participate were used in the vast majority of encounters. Field notes, however, revealed that nurses’ use of first-person language was dependent on the audience and content; nurses spoke to parents when discussing reasons to return to ED and spoke to patients when discussing activity restrictions. Nurses were also observed highlighting, circling, and writing in additional information (eg, time of next dose) on the AVS to enhance family understanding.
Family Engagement
In the family-engagement domain, all 3 components were present in 89% of encounters, with no significant difference between EP and LEP encounters (86% vs 91%; P = .430; OR: 0.6; 95% CI 0.2–1.8; Table 2). Families’ active participation (proactively asking questions and providing clarification) was present in 89% of encounters. Families were observed to appear engaged (exhibiting nonverbal cues, including nodding and eye-contact) in all EP and LEP encounters. Field notes revealed that families asked questions about follow-up appointments and return to school and, additionally, provided unprompted clarification about home pharmacy and home equipment. Some clarifying questions from the family required further action by the nurse (eg, asking the medical team to answer the family’s question). Field notes also revealed that when parents of differing English proficiency were in the room, nurses spoke almost exclusively to the English-speaking parent and exhibited limited engagement with the LEP parent. English-speaking parents were used as ad hoc interpreters in these encounters.
Discussion
Through observation of nurse-family discharge communication, we identified opportunities to improve communication with hospitalized pediatric patients and their parents for nurses who review the discharge instructions and, also, for the primary medical team who prepares those written instructions. Our assessment of safe discharge communication revealed that nurses often omit discussion of ED return precautions and medical providers often failed to provide written discharge instructions in a family’s primary language. These failures were more pronounced with LEP families than with EP families. Additionally, although use of communication practices that promote family centeredness and family engagement were frequently observed, teach-back was underused regardless of the family’s English proficiency. These findings add a detailed and novel understanding of discharge communication between medical providers and pediatric patients and families based on their English proficiency.
For a successful transition home, an accurate and thorough discussion of discharge instructions is critical. This should include a discussion of follow-up appointments, return precautions, and discharge medications.2,3 Particularly, understanding when to return to the ED after a hospital discharge and how to recognize potentially significant clinical changes in a timely manner are crucial for all patients and caregivers.20,21 However, in previous ED-based literature, it is suggested that information exchanged at discharge is often incomplete and return precautions are, often, not discussed.22 In our findings, it is suggested that discussion of return precautions may also be lacking from inpatient discharges, which may have negative implications for recently hospitalized children who often have not yet returned to a baseline state of health at the time of discharge. Moreover, return precautions were discussed less frequently in LEP encounters. This is concerning because LEP patients and families not only face challenges in communicating with health professionals and navigating the health system because of language and cultural barriers but, also, experience more frequent adverse events and reuse compared with EP patients.23,24
Ideally, all of the information components critical to a patient’s safe discharge should be reinforced with written discharge documentation that is not only accurate and complete but, also, readable, understandable, and written in the patient’s primary language.3,4 Written discharge instructions improve information recall for ED patients but are likely to play an even greater role after a hospitalization2,3 because families are overwhelmed with information and emotional stress during inpatient stays6 and may feel inadequately prepared to continue self-care at home.4,25 In our observations, 73% of LEP families were discharged with written instructions in English only. This is problematic, given LEP patients and families more often have limited health literacy,23 face language and cultural barriers that prevent them from navigating the health system effectively,26,27 and are at an increased risk for worse health outcomes.24,28 In our study, we found a frequent lack of written instructions in the family’s primary language, coupled with a significantly lower number of LEP families being instructed on reasons to return to the ED, which leaves families with critical knowledge gaps regarding postdischarge care plans. Targeted efforts that ensure providers prioritize verbal and written review of return precautions is essential.
Providing family-centered care that optimizes family understanding, engagement, and collaboration is crucial to boost understanding and confidence for families to execute postdischarge care plans.1–3,5 In studies, researchers addressing communication behavior during rounds have identified strategies to improve family centeredness, including the use of lay terms and simple sentence structure, active invitation for questions, and use of teach- and show-back.5,29,30 These strategies may be particularly relevant at the time of discharge because they empower families to share concerns with the opportunity for medical providers to address concerns in real time. The components of family-centered communication were present in the majority of encounters in our study, with the exception of teach-back. The use of teach- or show-back, an established evidence-based strategy,31–33 has been associated with improved family comprehension in the hospital during family-centered rounds for all patients.29 This strategy, considered helpful by medical providers and interpreters in their communication with families,16 has the potential to be particularly powerful in communicating with LEP families and could be a target for future endeavors to improve the discharge process for these families.
A perceived lack of engagement from LEP families16 and decreased participation of LEP families in patient care are often considered as potential drivers of differences in provider behavior.13,34 With our observations of LEP family engagement at discharge, we add a novel understanding to this topic. We found most families to be actively engaged in the discharge process, with no significant difference between LEP and EP families. Thus, family engagement was not the primary driver of differences seen in communication practices when caring for LEP and EP patients. Although the overall engagement of families remained high for all patients in our study, LEP parents were observed to be less engaged if they had an English-speaking spouse, and nurses were observed to speak almost exclusively to the parent who was fluent in English. This confirms previously reported findings that medical providers and interpreters perceive LEP parents to be less engaged if they have English-speaking spouses16 and raises concerns, given the use of family members to interpret in medical settings has, previously, been associated with increased communication errors.11 In light of this literature, with our findings, we highlight opportunities to better involve all caregivers in the child’s discharge communication, particularly when there is a mismatch in English proficiency status among family members.
Our study has several limitations. First, this study was conducted in a nonrandom sample of discharge encounters at a single institution with LEP prevalence below the national average, which limits the generalizability of our findings. However, in our observations, which included a large number of nurse participants, we identified several critical gaps in discharge communication that will be important to investigate further at other institutions nationally. Second, we used a novel observation tool that is not yet fully validated, which may have influenced our findings. To ensure identification of relevant domains and elements during tool development, we used an extensive literature search and peer review from nurses and physicians to establish face validity, and, during data collection, observers took extensive field notes to ensure the capture of additional relevant details that could be missed by this newly developed tool. Some of the observed differences could be due to variation in other nonobserved factors this tool is not designed to capture (eg, AVS preparation process or unconscious biases of medical team), which can be the topics of future study. Third, the observer’s presence may have influenced participants to behave in what they perceived to be a more socially desirable manner. To minimize this effect, although the nurse and family were aware that the observer was evaluating the discharge process, they were unaware of the specific objectives or data collected. Finally, despite an adequate sample size, there was variability across important factors and insufficient numbers of nonevents to conduct a multivariable analysis to control for potential confounding variables, and we were unable to link observations with patient outcomes (eg, revisits, medication errors after discharge, and family comprehension), which could be a topic of future study.
Conclusions
Our observations reveal gaps in the safety and family centeredness of discharge communication for hospitalized pediatric patients and their parents. Particularly, we identified opportunities to increase the use of teach-back for all patients as well as deficiencies in discussion of return criteria and the receipt of appropriately translated discharge instructions that disproportionally affected LEP patients. With our work, we highlight a need for focused efforts to improve the discharge process and medical provider communication for patients and families, particularly those with LEP.35 Future qualitative studies will be important to gain a deeper understanding of the challenges of the discharge process from the perspectives of LEP families. Additional efforts to determine the association of provider communication at discharge with patient outcomes, including reuse and medication errors, will be critical to fully understanding the implications of our findings.
Acknowledgments
We acknowledge nursing and language access services leadership at Cincinnati Children’s Hospital Medical Center, including Brenda Demeritt, BSN, RN, MHA, and Andy Schwieter, for partnership critical for recruitment of participants.
Footnotes
Dr Choe conceptualized and designed the study, recruited participants, led data collection, analysis, and interpretation, and drafted the initial manuscript; Drs Unaka, Thomson, and Schondelmeyer supervised the conceptualization and design of the study and supervised data collection, analysis, and interpretation; Ms Mangeot contributed to the design of the study and conducted analysis and interpretation of data; Ms Wagner, Ms Durling, Ms Moeller, and Ms Ampomah contributed to the design of the study and development of the data collection tool and participated in data collection, analysis, and interpretation; and all authors critically reviewed and revised the manuscript and approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: Dr Thomson is supported by the Agency for Healthcare Research and Quality (grant K08 HS02513). Dr Schondelmeyer is supported by the Agency for Healthcare Research and Quality (grant K08 HS026763). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Funded by the Pediatric Hospital Medicine Fellows grant at Cincinnati Children’s Hospital Medical Center. This work was completed in partial fulfillment of the Master of Science degree in Clinical and Translational Research in the Division of Epidemiology, Department of Environmental and Public Health Sciences, College of Medicine, University of Cincinnati, which is supported by an institutional Clinical and Translational Science Award, National Institutes of Health National Center for Advancing Translational Sciences grant 1UL1TR001425. In this work, we used the Research Electronic Data Capture database, which was made available through the Center for Clinical and Translational Science and Training at the University of Cincinnati, supported by National Institutes of Health National Center for Advancing Translational Sciences grant UL1TR000077. Ms Wagner’s effort was funded by a research stipend through the Medical Student Scholars Program at the University of Cincinnati College of Medicine. Dr Thomson’s effort contributing to this article was, in part, funded by the Agency for Healthcare Research and Quality (grant K08 HS02513). Dr Schondelmeyer’s effort contributing to this article was, in part, funded by the Agency for Healthcare Research and Quality (grant K08 HS026763). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations. The funding organizations had no role in the design, preparation, review, or approval of this article. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Williams MV, Budnitz T, Coleman EA, et al. The Society of Hospital Medicine Project BOOST Implementation Guide to Improve Care Transitions. 2014. Available at: www.hospitalmedicine.org/Web/Quality_Innovation/Implementation_Toolkits/Project_BOOST/Web/Quality___Innovation/Implementation_Toolkit/Boost/First_Steps/Implementation_Guide.aspx
- 2.Soong C, Daub S, Lee J, et al. Development of a checklist of safe discharge practices for hospital patients. J Hosp Med. 2013;8(8):444–449 [DOI] [PubMed] [Google Scholar]
- 3.Berry JG, Blaine K, Rogers J, et al. A framework of pediatric hospital discharge care informed by legislation, research, and practice. JAMA Pediatr. 2014;168(10):955–962; quiz 965–956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Unaka NI, Statile A, Haney J, Beck AF, Brady PW, Jerardi KE. Assessment of readability, understandability, and completeness of pediatric hospital medicine discharge instructions. J Hosp Med. 2017;12(2):98–101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Subramony A, Hametz PA, Balmer D. Family-centered rounds in theory and practice: an ethnographic case study. Acad Pediatr. 2014;14(2):200–206 [DOI] [PubMed] [Google Scholar]
- 6.Solan LG, Beck AF, Brunswick SA, et al. ; H2O Study Group. The family perspective on hospital to home transitions: a qualitative study. Pediatrics. 2015;136(6). Available at: www.pediatrics.org/cgi/content/full/136/6/e1539 [DOI] [PubMed] [Google Scholar]
- 7.Gallagher RA, Porter S, Monuteaux MC, Stack AM. Unscheduled return visits to the emergency department: the impact of language. Pediatr Emerg Care. 2013;29(5):579–583 [DOI] [PubMed] [Google Scholar]
- 8.Harris LM, Dreyer BP, Mendelsohn AL, et al. Liquid medication dosing errors by Hispanic parents: role of health literacy and English proficiency. Acad Pediatr. 2017;17(4):403–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.DeCamp LR, Kuo DZ, Flores G, O’Connor K, Minkovitz CS. Changes in language services use by US pediatricians. Pediatrics. 2013;132(2). Available at: www.pediatrics.org/cgi/content/full/132/2/e396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255–299 [DOI] [PubMed] [Google Scholar]
- 11.Flores G, Abreu M, Barone CP, Bachur R, Lin H. Errors of medical interpretation and their potential clinical consequences: a comparison of professional versus ad hoc versus no interpreters. Ann Emerg Med. 2012;60(5):545–553 [DOI] [PubMed] [Google Scholar]
- 12.Cora-Bramble D; American Academy of Pediatrics. Culturally Effective Care Toolkit: Providing Culturally Effective Pediatric Care. Itasca, IL: American Academy of Pediatrics; 2018 [Google Scholar]
- 13.Zurca AD, Fisher KR, Flor RJ, et al. Communication with limited English-proficient families in the PICU. Hosp Pediatr. 2017;7(1):9–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Auger KA, Kenyon CC, Feudtner C, Davis MM. Pediatric hospital discharge interventions to reduce subsequent utilization: a systematic review. J Hosp Med. 2014;9(4):251–260 [DOI] [PubMed] [Google Scholar]
- 16.Choe AY, Unaka NI, Schondelmeyer AC, Bignall WJR, Vilvens HL, Thomson JE. Inpatient communication barriers and drivers when caring for limited English proficiency children. J Hosp Med. 2019;14(10):607–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.White CM, Statile AM, White DL, et al. Using quality improvement to optimise paediatric discharge efficiency. BMJ Qual Saf. 2014;23(5):428–436 [DOI] [PubMed] [Google Scholar]
- 18.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agency for Healthcare Research and Quality Health Care Utilization Project. Clinical Classifications Software (CCS) for ICD-10-PCS (beta version). Available at: https://www.hcup-us.ahrq.gov/toolssoftware/ccs10/ccs10.jsp. Accessed June 11, 2019
- 20.Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language barriers and resource utilization in a pediatric emergency department. Pediatrics. 1999;103(6, pt 1):1253–1256 [DOI] [PubMed] [Google Scholar]
- 21.Glick AF, Farkas JS, Nicholson J, et al. Parental management of discharge instructions: a systematic review. Pediatrics. 2017;140(2):e20164165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gutman CK, Cousins L, Gritton J, et al. Professional interpreter use and discharge communication in the pediatric emergency department. Acad Pediatr. 2018;18(8):935–943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sentell T, Braun KL. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J Health Commun. 2012;17(suppl 3):82–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khan A, Coffey M, Litterer KP, et al. Families as partners in hospital error and adverse event surveillance. JAMA Pediatr. 2017;171(4):372–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Unaka NI, Statile AM, Choe A, Shonna Yin H. Addressing health literacy in the inpatient setting. Curr Treat Options Pediatr. 2018;4(2):283–299 [Google Scholar]
- 26.Flores G. Language barriers to health care in the United States. N Engl J Med. 2006;355(3):229–231 [DOI] [PubMed] [Google Scholar]
- 27.Flores G, Tomany-Korman SC. The language spoken at home and disparities in medical and dental health, access to care, and use of services in US children. [published correction appears in Pediatrics. 2009;124(4):1265]. Pediatrics. 2008;121(6). Available at: www.pediatrics.org/cgi/content/full/121/6/e1703 [DOI] [PubMed] [Google Scholar]
- 28.Lion KC, Rafton SA, Shafii J, et al. Association between language, serious adverse events, and length of stay among hospitalized children. Hosp Pediatr. 2013;3(3):219–225 [DOI] [PubMed] [Google Scholar]
- 29.Lion KC, Mangione-Smith R, Martyn M, Hencz P, Fernandez J, Tamura G. Comprehension on family-centered rounds for limited English proficient families. Acad Pediatr. 2013;13(3):236–242 [DOI] [PubMed] [Google Scholar]
- 30.Pickel S, Shen MW, Hovinga C. Look who’s talking: comparing perceptions versus direct observations in family-centered rounds. Hosp Pediatr. 2016;6(7):387–393 [DOI] [PubMed] [Google Scholar]
- 31.Starmer AJ, Spector ND, Srivastava R, et al. ; I-PASS Study Group. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803–1812 [DOI] [PubMed] [Google Scholar]
- 32.Jager AJ, Wynia MK. Who gets a teach-back? Patient-reported incidence of experiencing a teach-back. J Health Commun. 2012;17(suppl 3):294–302 [DOI] [PubMed] [Google Scholar]
- 33.Kornburger C, Gibson C, Sadowski S, Maletta K, Klingbeil C. Using “teach-back” to promote a safe transition from hospital to home: an evidence-based approach to improving the discharge process. J Pediatr Nurs. 2013;28(3):282–291 [DOI] [PubMed] [Google Scholar]
- 34.Levin AB, Fisher KR, Cato KD, Zurca AD, October TW. An evaluation of family-centered rounds in the PICU: room for improvement suggested by families and providers. Pediatr Crit Care Med. 2015;16(9):801–807 [DOI] [PubMed] [Google Scholar]
- 35.Lion KC, Raphael JL. Partnering health disparities research with quality improvement science in pediatrics. Pediatrics. 2015;135(2):354–361 [DOI] [PMC free article] [PubMed] [Google Scholar]