Abstract
Objectives:
The purpose of this study was to select a health warning message location on a waterpipe (WP) that both attracted visual attention and conveyed the risks associated with WP smoking.
Methods:
During June through November 2019, we conducted a within-subjects randomized experiment (N = 74) using eye tracking equipment to examine visual attention to 3 placements of a health warning on the WP (stem, water bowl, hose). We asked young adult ever WP users 3 questions about WP harm perceptions. We used generalized linear mixed models to examine the amount of fixation time spent on the placement locations; we used repeated measures ANOVA to model changes in harm perceptions.
Results:
There were statistically significant differences across all 3 placement locations; regardless of place, all HWLs attracted a comparable amount of visual attention. Absolute WP harm perceptions significantly increased following the experiment and remained significantly higher at the one-week follow-up, compared to baseline.
Conclusions:
Warnings on WPs attracted visual attention and increased harm perceptions, and those harm perceptions remained high one week after the experiment. Findings indicate the value of including a warning on the WP device, and underscore the necessity and effectiveness of those health warnings to combat WP harm misperceptions.
Keywords: addiction, health communications, health policy, smoking and health, tobacco control, waterpipes
Waterpipe (WP) tobacco usage has become a global epidemic; in the United States (US); evidence demonstrates that WP use is widespread, especially among young adults with 44% of US young adults reporting ever use, and 11% reporting daily use.1 This tobacco product is demonstrated to be harmful, addictive, and may serve as a gateway to cigarette smoking,2 and a barrier to tobacco cessation.3 Although WP use is more often intermittent than daily, relative to a cigarette smoking, WP tobacco smoking yields similar or higher nicotine exposure and 56-fold greater inhaled smoke volume;4 in the short term, WP use can impair lung function, and serious long-term health risks include bronchitis, emphysema, coronary artery disease, and cancers.5
Health warning labels (HWLs) on tobacco products perform several key functions to inform users about health risks of use; they increase awareness of health risks, support cessation, and deter initiation of use.6,7 Pictorial images with text messages further increase smokers’ intentions to quit.8,9 Under current regulation by the US Food and Drug Administration (FDA) all packages of waterpipe (WP) tobacco sold in the US must include the following text-only warning message: “WARNING: This product contains nicotine. Nicotine is an addictive chemical.”10 The FDA warning on nicotine may increase knowledge, as young adult WP users perceive WP smoking is less addictive and contains less nicotine than cigarettes.11 Yet, misperceptions extend beyond nicotine; both WP users and non-users erroneously believe that WP use is less harmful than cigarettes, and this misperception is associated with current use.12,13
HWLs are an opportunity to correct known misperceptions of WP use as a low-risk behavior that is safer than cigarette use.14,15 However, a HWL can only perform this function if the messages are visible to users and potential users. As the current regulations only require a HWL on the WP tobacco package, and most WP users in the US smoke in a café environment where the WP tobacco is unwrapped and prepared before it is brought to them, café users never see this warning.14,16 The Tobacco Control Act does allow for the requirement that devices used to smoke tobacco include health warnings. Despite this, research into the potential placement of HWLs on WP devices has been limited. Using an Internet-based survey with drawings of a WP, a convenience sample of college students that recently used WP rated the water bowl, mouthpiece, and stem as equally noticeable locations on the device.11 Similarly, after viewing images of WPs affixed with HWLs, the water bowl, hose, and mouthpiece locations were favored by Egyptian adult WP users during qualitative interviews.17 Other work has identified that the mouthpiece/hose of a WP is an especially visible location for a HWL, followed closely by the stem or base.18
As outlined in work by Brewer et al,19 attention to the warning message is necessary for a consumer to react to and think about the HWL information that will inform subsequent risk perceptions and other beliefs; without these steps, an HWL cannot influence quit intentions nor quit attempts. Their Tobacco Warnings Model proposes that “warnings increase noticing and attention to the message,” which results in increased affective response (including fear) and talking with others about the information in the messages. Eye tracking, a technique which uses a near-infrared camera to precisely capture visual attention, has been used to examine tobacco warnings on advertisements and product packages,20,21 but to date none have examined WP devices.
The gap in current research knowledge on HWLs for WP tobacco has been recognized as research need.22 A more rigorous examination of HWL placement locations on a WP device is needed to inform the optimal placement for such a warning to be noticed by WP users. The primary aim of our study was to go beyond self-reported data to apply an objective approach to select a HWL message location that attracted visual attention on a WP device. A secondary aim was to assess the impact of viewing WP warning labels on risk perceptions.
METHODS
Participants
Recruitment occurred on our university’s campus and in the surrounding community. We recruited participants through social media advertisements, flyers, and word-of-mouth. Interested individuals called or emailed to inquire about the study. A phone screening protocol was used to determine eligibility. Eligible participants were young adults (age 18–29 years) who had smoked WP at least once. Additionally, they had to be free of eye conditions that are contraindications to eye tracking (glaucoma, macular degeneration, cataracts, eye implants, permanently dilated pupils, inability to see out of both eyes). Individuals who were interested and eligible after the phone screening were scheduled for a single, in-person session.
Procedures
Prior to beginning the eye tracking protocol, a research assistant explained the study and obtained signed informed consent. After that, participants completed a short survey that included questions about demographics, WP smoking, tobacco use, and risk perceptions of tobacco use, including WP.
Participants were seated in a chair within a typical viewing distance (24 to 32 inches) from a computer monitor equipped with a near-infrared camera with their chin placed in a chin rest. Images were displayed on a portable computer monitor, and data were captured with eye tracking equipment (SensoMotoric Instruments, 120 Hz REDm System). Study stimuli consisted of high-quality photos of 4 WPs (3 commercial WPs and a research-grade WP) in one of 3 conditions: no warning, text only, and text + graphic warning labels, with the labels placed in 3 locations: hose, stem, and water bowl. In previous research, our team developed and tested the warning label that included the message “WARNING: Hookah smoke contains poisons that cause mouth and lung cancers” paired with either an image of diseased lungs or a diseased mouth. Development of these WP-specific HWLs is described elsewhere.23
Prior to viewing study stimuli, calibration procedures were conducted up to 3 times to assure data quality. Participants were told they would view images of tobacco products and advertisements; the study stimuli was displayed at a fixed interval of 5 seconds, based on previous eye tracking studies with similar HWL stimuli.24,25 The stimuli consisted of 80 images viewed in a randomized order. We used the following factorial design: 4 pipes × 3 label conditions (text, 2 text + graphic labels) × 3 locations on the WP (stem, water bowl, hose) × 2 views (full or cropped image). As a control, we included one image of each pipe without any warning (both full and cropped, for 8 additional images), which is the current regulatory standard. Although we considered additional control conditions with different message content (eg, neutral, non-warning language), this was not included due to concerns for participant burden and because our focus was label placement. A mouthpiece placement location was excluded based on qualitative interviews where users expressed concerns that the plastic warning label would interfere with puffing behavior (data not shown).
The views were selected to provide readability of the HWL message (cropped image) and an approximation of café environment (full image). Figure 1 displays sample stimuli of a select WP with all 4 label conditions for all placement locations. To make the viewing activity less redundant, we included 16 other tobacco-related images (eg, e-cigarette, combustible cigarette, and smokeless tobacco advertisements) interspersed in the stimulus set. Participants viewed each image for a fixed interval of 5 seconds to standardize total viewing time across each image. In addition, after every 8–10 images, participants were asked questions to maintain attention. Questions were related to the activity (eg, “What color was the hookah pipe in the last picture?”) or focused on knowledge or opinions (eg, “How much do you agree or disagree with the following statement? The water in the bowl filters out all the toxins from hookah smoking”). The total experiment viewing time was 8.5 minutes.
Figure 1.
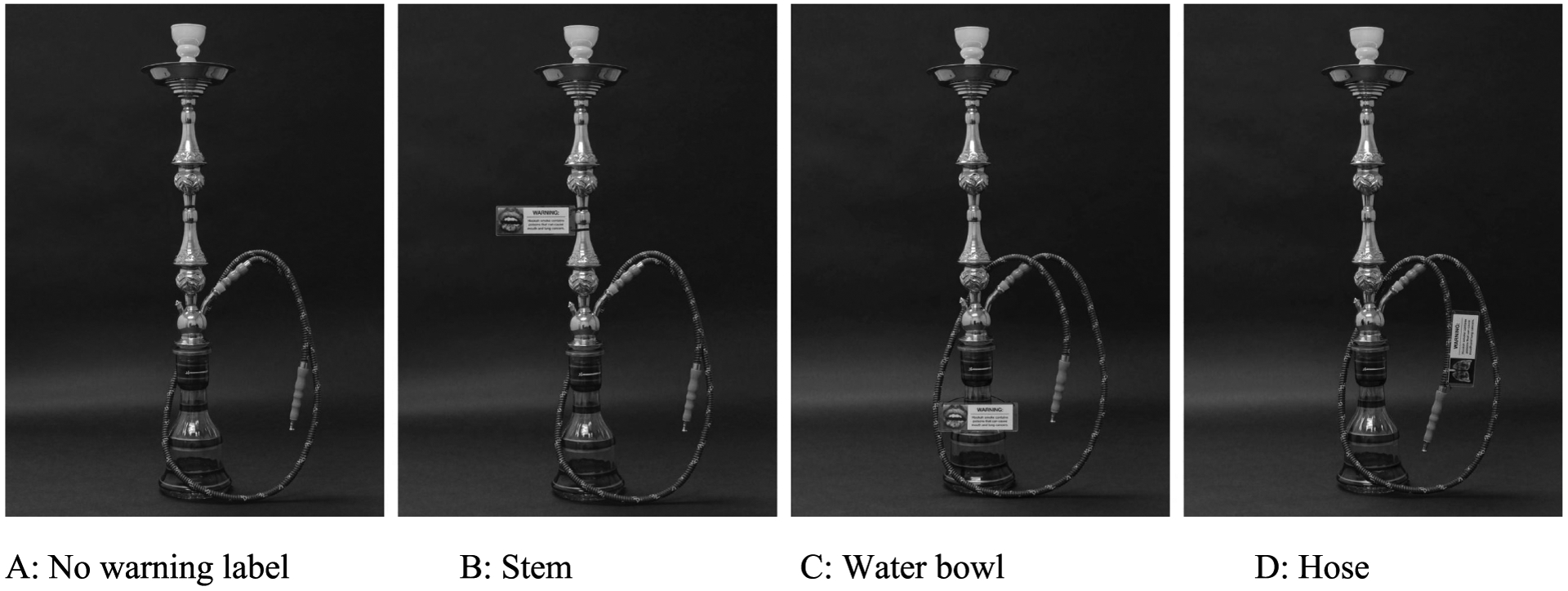
Example Waterpipe Imagery for 3 Health Warning Label Types and 4 Placement Locations
After the experiment, participants completed a survey that asked about their intentions to continue, reduce, or quit smoking WP, and questions that assessed their risk perceptions associated with WP smoking. Participants received $30 in cash in appreciation of their time. One week after the experiment all participants were contacted by phone and asked questions (unaided) to recall placement and content of the message. Additionally, they were asked about their intentions to smoke WP and questions about their risk perceptions. Participants received a $10 gift card for their time.
Measures
For the eye tracking measures, 3 areas of interest (AOIs) were defined a priori for stimuli based on the 3 warning placement locations: water bowl, stem, and hose. The duration of dwell time in milliseconds was assessed for each AOI.
Risk perceptions were measured as an absolute and relative risk, where the absolute risk (“How much do you think people harm themselves when they smoke hookah?”) was rated from no harm to extreme harm (0–10), and relative risk perceptions were measured for both e-cigarettes and combustible cigarettes (“Is smoking hookah less harmful, about the same or more harmful”). Responses were dichotomized into relative risk perception of more harmful (when rated as “more harmful”) or less harmful (when rated as “about the same” or “less harmful”); responses of “don’t know” were excluded from the analysis. In the follow-up survey, participants were asked: “To what extent did the warnings make you think about the risk of smoking hookah?” to assess how much they thought about the warnings since the experiment rated on a 9-point scale from not at all to extremely.
Data Analysis
Our primary analyses focused on differences in total dwell time and number of visits to a warning label by label location (stem, hose, water bowl) and message (text only, text plus mouth graphic, text plus lung graphic) when presented a cropped image of the pipe. Generalized linear mixed models were used consisting of fixed effects of location, message, and a message-by-location interaction. The dwell time model assumed a normal distribution, identity link, and the following random effects: participant, pipe, and random 2-way and 3-way interactions between participant, pipe, location, and message. The model for number of visits to a label assumed a Poisson distribution, log link, and random participant and pipe effects (no random interactions were considered due to convergence problems). Tukey’s post hoc method was used to adjust for multiple comparisons when there was a significant main effect of location or message. In secondary analyses, we used generalized linear mixed models containing fixed effects of pipe, location, message, and their 2-way interactions to determine if the associations of our outcomes (dwell time and number of visits) with label location and message differ by pipe. The model for number of visits to a label contained a random main effect for participant while the dwell time model contained multiple random participant effects (main effects plus 2-way and 3-way interactions with pipe, location, and message). If there was a statistically significant interaction, we performed stepdown tests of the main effects at each level of pipe and used Holm’s method to control the overall type-I error rate.26 The eye tracking equipment recorded an average of 48,000 total observations per participant. Each observation was recorded on average every 9 milliseconds. Each observation contained vertical and horizontal eye coordinates for the image being viewed by the participant within the 5 seconds (5000 milliseconds) intervals. If a participant’s vertical and horizontal eye coordinates were zero for a given observation, we considered this to be missing eye tracking data. Six participants were excluded from the analysis due to a high proportion of missing eye tracking data (> 0.25) or a low number of total observations (< 46,000).
For the absolute risk perception measures, changes were analyzed using repeated measures ANOVA to identify whether there were differences between the 3 study time periods – baseline, immediately following the experiment, and one-week follow-up surveys; pairwise comparisons were made using paired t-tests. For each relative risk perception measure, Cochran’s Q test was used to compare the proportion of “more harmful” responses across the 3 study periods and pairwise comparisons of time periods were performed using McNemar’s test. For pairwise comparisons, we used a Bonferroni-corrected statistical significance threshold of .017.
RESULTS
Study participants were 51.3% male, 56.8% non-Hispanic white, and 56.8% between the ages of 21 and 23 years (N = 74). Most (74.3%) reported ever use of WP tobacco more than once, and 32.4% reported any past month use. Most reported first use of WP tobacco occurred at age 19 or younger (81.1%) and first use was in a café or restaurant (60.8%) or friend’s home (25.7%).
Complete eye tracking data were available for 66 participants. In Table 1, visual attention measures for both the full and cropped WP images across the 3 locations (water bowl, hose, and stem), type of HWL (lung, mouth, and text), and across all 4 WP devices are shown. For the full image, the stem attracted the greatest attention (1.1 seconds), followed by the water bowl (1.0 seconds) and hose (0.8 seconds), though visual attention was only significantly different between the stem and hose (p = .04). Significantly more attention was paid to the water bowl in cropped images (1.6 seconds compared to 1.2 seconds for hose and stem, p < .05 for each comparison). There were no statistically significant differences in either the full or cropped images for the HWL by type of content (p > .05), but the visual attention varied significantly between the WP devices, ranging from 0.9 seconds to 1.4 seconds (p < .01). Figure 2 displays a visualization of the aggregate visual attention to a single pipe showing the series of all 4 warning label placements; for this focus map visualization, the more fixations on an area lead to a clear view of the content, and darker areas indicate fewer fixations.
Table 1.
Differences in Dwell Time by Health Warning Label Placement Location, Type, and Waterpipe Device (N = 66 participants)
| Full Image | Cropped Image | ||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | P | Mean | SD | P | ||
| Location | Water bowl | 982.5 | 1094.3 | .050 | 1564.8 | 1346.7 | .019 |
| Hose | 793.5 | 925.3 | 1192.5 | 1146.3 | |||
| Stem | 1116.7 | 1135.5 | 1171.8 | 1121.2 | |||
| Type | Lung | 1004.1 | 1097.0 | .336 | 1306.2 | 1202.5 | .162 |
| Mouth | 944.0 | 1026.3 | 1366.0 | 1275.5 | |||
| Text | 944.6 | 1066.2 | 1256.9 | 1184.8 | |||
| Any warning | 964.2 | 1063.5 | <.001 | 1309.7 | 1221.9 | < .001 | |
| No warning | 92.3 | 285.5 | 86.8 | 273.4 | |||
| Pipe | 1 | 853.8 | 1058.5 | .004 | 1192.8 | 1181.2 | .001 |
| 2 | 989.3 | 1082.7 | 1304.8 | 1236.1 | |||
| 3 | 977.1 | 1040.7 | 1318.4 | 1193.6 | |||
| 4 | 1036.7 | 1065.7 | 1422.8 | 1267.0 | |||
Figure 2.
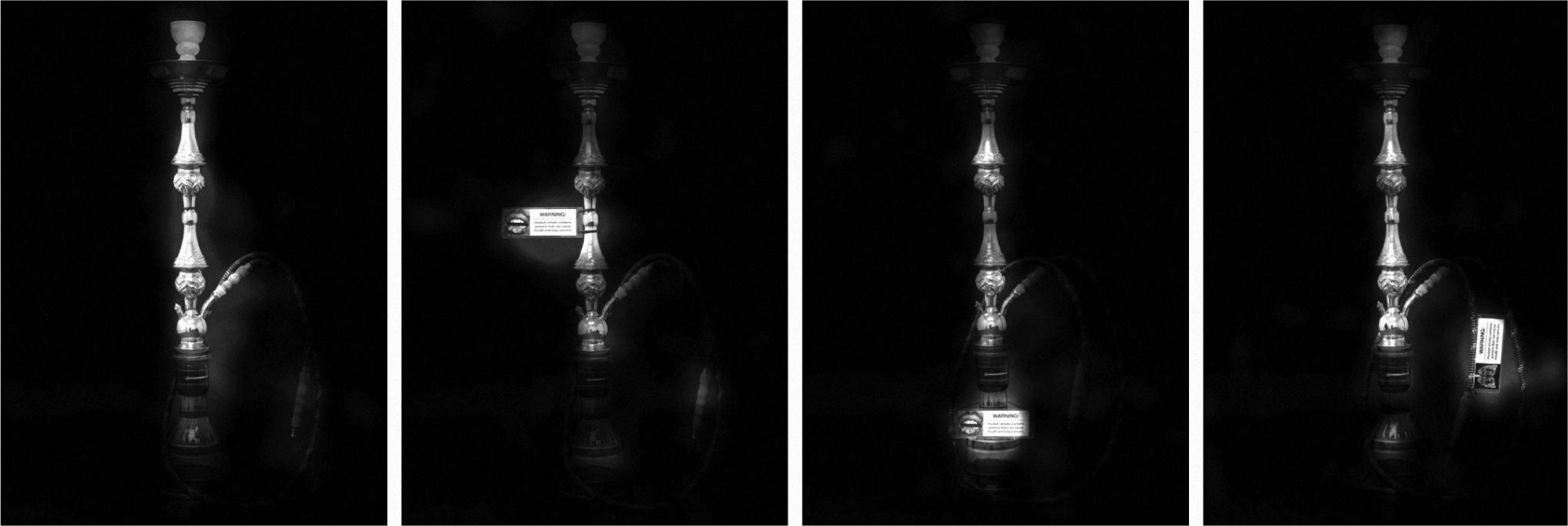
Focus Maps for Health Warning Label Placement Locations
All participants endorsed that the warning labels made them think about the risks of hookah in the previous week, and 23% rated as “extremely” for the extent the warnings made them think about the health risks of WP use. Table 2 shows the ratings for absolute and relative harm perceptions prior to study initiation (baseline), immediately following the experiment, and at a one-week follow-up contact. Absolute harm perception changed significantly over time (p < .001). Absolute WP harm perceptions significantly increased following the experiment (mean difference 1.24; SE 0.26; p < .001) and remained significantly higher at the one-week follow-up, compared to baseline (mean difference 1.69; SE 0.24; p < .001). Harm perceptions did not change relative to combustible cigarettes (p = .27) or e-cigarettes (p = .16).
Table 2.
Absolute and Relative Harm Perceptions of Waterpipe Use Over Time (N = 76)
| Harm Perception Ratings | Baseline | Posta | One-week follow-up |
|---|---|---|---|
| Mean rating of absolute harm perception on a scale of 0–10 (SD) | 5.2 (2.4) | 6.5 (2.6) | 6.8 (1.9) |
| Hookah is more harmful than cigarettes (%) | 41.7% | 35.3% | 37.7% |
| Hookah is more harmful than e-cigarettes (%) | 43.3% | 51.5% | 54.4% |
Note.
Immediately following the experiment
DISCUSSION
There was no single clear placement location that meaningfully attracted more visual attention, as all locations attracted visual attention when a HWL was present; the water bowl attracted more visual attention compared to the hose or stem in the cropped image, but we did not observe this relationship in the full WP image. Considering the relatively small differences between the dwell time on the various locations, any of the placement locations attracted a significant amount of attention. Our findings establish that placement of a waterpipe warning on the hose, water bowl, or stem attracted visual attention to health warnings on the WP device, thereby demonstrating an applicable regulatory strategy to inform WP users on health risk information. According to the Tobacco Warnings Model, paying attention to a HWL is a key first step needed for an individual to recall the health warning messages, comprehend it, and subsequently inform decisions to change behavior.19,27,28 Our findings align with this model, demonstrating attention to several viable placement locations for WP warning labels, and a statistically significant increase in health risk perceptions following the experiment.
Given the rising trends in waterpipe smoking among youth and young adults in the US,1,14,29 strong regulatory policies are needed prevent future WP-related morbidity and mortality. Despite global popularity and known health risks, it is surprising that there are only a handful of WP-specific laws enacted in 6 countries,30 and none of those warnings are in compliance with WHO FCTC recommendations.31 Our findings support the feasibility of placing a FCTC-compliant HWL on a waterpipe device across 3 prominent locations. In the US, the FDA Deeming rule allowed mandating a warning label on the WP itself32 which may be more effective, because as noted above, most WP smokers consume while in a café where they do not see the tobacco package.
When Mostafa et al17 conducted qualitative interviews with WP users and non-users, participants mentioned that if HWLs were placed on the device, current users might cut down or quit entirely. Whereas changes in WP smoking in response to HWLs on WP devices have yet to be examined, Islam et al11 found that HWLs on WP devices motivated cessation-related thinking and intentions among users. Furthermore, our findings aligned with the conclusions from a survey of 367 college students that stated preferences to HWL to be placed on a WP stem, water bowl, or hose/mouthpiece.11
The present study has limitations to consider. Within this laboratory-based study, the viewing experience of static imagery will not be identical to a café environment that includes other users that will naturally draw attention away from the WP. Participants viewed 80 waterpipe images during a brief (<10 minutes) time period, which approximated viewing one WP device per minute during a typical waterpipe café session.33 Despite previous studies examining the hose and mouthpiece as separate placement locations,11,17,18 the current study examined the hose only. Our research question concerned label placement and focused on the examination of HWLs relative to the current regulatory standard of no label; future studies using a blank (text-free) or a “fake” warnings could address questions regarding message content.34 All WPs were viewed at a table-top level, but a café environment can include low lighting and the WP device being on the floor; thus, a water bowl or stem HWL placement would not be as visible (unpublished data). Ever users of WP were the focus of the present research, but it is not known whether more frequent users could have different perceptions of risks. The within-subjects design does not allow examination of differences in risk perceptions by individual HWLs. Given the evidence that HWLs inform risk perceptions in experimental trials,6,8,35 future studies should focus on testing specific HWL messages to inform health risks.
Our findings provide strong, objective evidence that any WP placement would attract visual attention from users beyond the current café standard of no warning. Moreover, the WP-specific warning labels increased risk perceptions among young adult users known to underestimate the risks associated with WP use.15 Given the gaps in the current policy environment regarding HWLs on WP devices, our findings that all locations with a warning attracted attention provide additional evidence to suggest the viability of placement of HWLs on WP devices to attract attention and inform appropriate risk perceptions of WP use. There is a need for the development of WP-specific guidelines to consider the placement, size, and type of HWL that can be most effective in addressing misperceptions among consumers.
Acknowledgements
This work was funded by grant R01CA229306. Research reported here was supported by the National Cancer Institute and FDA Center for Tobacco Products (CTP). The research was also supported, in part, by The Ohio State University Comprehensive Cancer Center and the National Institutes of Health under grant number P30CAO16058. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Footnotes
Conflict of Interest Disclosure Statement
None of the authors has a conflict of interest to declare.
References
- 1.Salloum RG, Thrasher JF, Getz KR, et al. Patterns of waterpipe tobacco smoking among U.S. young adults, 2013–2014. Am J Prev Med. 2017;52(4):507–512. doi: 10.1016/j.amepre.2016.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maziak W. The waterpipe: a new way of hooking youth on tobacco. Am J Addict. 2014;23(2):103–107. doi: 10.1111/j.1521-0391.2013.12073.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maziak W, Taleb Z Ben, Bahelah R et al. The global epidemiology of waterpipe smoking. Tob Control. 2015;24(Suppl I):i3–il2. doi: 10.1136/tobaccocontrol-2014-051903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cobb CO, Shihadeh A, Weaver MF, Eissenberg T. Waterpipe tobacco smoking and cigarette smoking: a direct comparison of toxicant exposure and subjective effects. Nicotine Tob Res. 2011;13(2):78–87. doi: 10.1093/ntr/ntq212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.E1-Zaatari ZM, Chami HA, Zaatari GS, Zaatari G. Health effects associated with waterpipe smoking. Tob Control. 2015;24(Suppl 1):i13–i43. doi: 10.1136/tobaccocontrol-2014-051908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hammond D. Health warning messages on tobacco products: a review. Tob Control. 2011;20(5):327–337. doi: 10.1136/tc.2010.03763 [DOI] [PubMed] [Google Scholar]
- 7.Fong GT, Hammond D, Hitchman SC. The impact of pictures on the effectiveness of tobacco warnings. Bull World Health Organ. 2009;87(8):640–643. doi: 10.2471/blt.09.069575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hammond D, Fong GT, Borland R, et al. Communicating risk to smokers: the impact of health warnings on cigarette packages. Am J Prev Med. 2007;32(3):202–209. doi: 10.1016/j.amepre.2006.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammond D, Fong GT, McNeill A, et al. Effectiveness of cigarette warning labels in informing smokers about the risks of smoking: findings from the International Tobacco Control (ITC) 4 Country Survey. Tob Control. 2006;(15 Suppl 3):iii 19–iii25. doi: 10.1136/tc.2005.012294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deeming Tobacco Products To Be Subject to the Federal Food, Drug, and Cosmetic Act, as Amended by the Family Smoking Prevention and Tobacco Control Act; Restrictions on the Sale and Distribution of Tobacco Products and Required Warning Statements for Tobacco. US Food and Drug Administration. 2016:28973–29106. https://www.federalregister.gov/documents/2016/05/10/2016-10685/deeming-tobacco-products-to-be-subject-to-the-federal-food-drug-and-cosmetic-act-as-amended-by-the. Published May 10, 2016. AccessedDecember 11, 2020. [PubMed]
- 11.Islam F, Salloum RG, Nakkash R, et al. Effectiveness of health warnings for waterpipe tobacco smoking among college students. Int J Public Health. 2016;61(6):709–715. doi: 10.1007/s00038-016-0805-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cornacchione J, Wagoner KG, Wiseman KD, et al. Adolescent and young adult perceptions of hookah and little cigars/cigarillos: implications for risk messages. J Health Commun. 2016;21(7):818–825. doi: 10.1080/10810730.2016.1177141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Primack BA, Sidani J, Agarwal AA, et al. Prevalence of and associations with waterpipe tobacco smoking among U.S. university students. Ann Behav Med. 2008;36(1):81–86. doi: 10.1007/s12160-008-9047-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heinz AJ, Giedgowd GE, Crane NA, et al. A comprehensive examination of hookah smoking in college students: use patterns and contexts, social norms and attitudes, harm perception, psychological correlates and co-occurring substance use. Addict Behav. 2013;38(11):2751–2760. doi: 10.1016/j.addbeh.2013.07.009 [DOI] [PubMed] [Google Scholar]
- 15.Akl EA, Jawad M, Lam WY, et al. Motives, beliefs and attitudes towards waterpipe tobacco smoking: a systematic review. Harm Reduct J. 2013;10(12). doi: 10.1186/1477-7517-10-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asfar T, Ward KD, Eissenberg T, Maziak W. Comparison of patterns of use, beliefs, and attitudes related to waterpipe between beginning and established smokers. BMC Public Health. 2005;5(1):19. doi: 10.1186/l471-2458-5-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mostafa A, Mohammed HT, Hussein WM, et al. Would placing pictorial health warnings on waterpipe devices reduce waterpipe tobacco smoking? A qualitative exploration of Egyptian waterpipe smokers’ and non-smokers’ responses. Tob Control. 2019;28(4):475–478. doi: 10.1136/tobaccocontrol-2018-054494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mostafa A, Mohammed HT. Graphic health warnings and their best position on waterpipes: a cross-sectional survey of expert and public opinion. Tob Prev Cessat. 2017;3(116). doi: 10.18332/tpc/70873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brewer NT, Parada H, Hall MG, et al. Understanding why pictorial cigarette pack warnings increase quit attempts. Ann Behav Med. 2018;53(3):232–243. doi: 10.1093/abm/kay032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meernik C, Jarman K, Towner Wright S, et al. Eye tracking outcomes in tobacco control regulation and communication: a systematic review. Tob Regul Sci. 2016;2(4):377–403. doi: 10.1800l/TRS.2.4.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaufman AR, Klein EG, Koblitz A, Price S. A vision for eye-tracking research in tobacco regulatory science. Tob Regul Sci. 2018;4(6):3–7. doi: 10.18001/TRS.4.6.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thrasher JF, Brewer NT, Niederdeppe J, et al. Advancing tobacco product warning labels research methods and theory: a summary of a grantee meeting held by the US National Cancer Institute. Nicotine Tob Res. 2019;21(7):855–862. doi: 10.1093/ntr/nty017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mouman M, Brinkman M, Keller-Hamilton B, et al. Waterpipe tobacco warnings need to inform users of harm: evidence from studies with young adults. Tob Regul Sci. 2020;6(4):279–288. doi: 10.18001/TRS.6.4.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maynard OM, Attwod A, O’Brien L, et al. Avoidance of cigarette pack health warnings among regular cigarette smokers. Drug Alcohol Depend. 2014;136:170–174. doi: 10.1016/j.drugalcdep.2014.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klein EG, Shoben AB, Krygowski S, et al. Does size impact attention and recall of graphic health warnings? Tob Regul Sci. 2015;1(2): 175–185. doi: 10.18001/trs.1.2.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6:65–70. [Google Scholar]
- 27.Kees J, Burton S, Andrews JC, Kozup J. Understanding how graphic pictorial warnings work on cigarette packaging. J Public Policy Mark. 2010;29(2):265–276. doi: 10.1509/jppm.29.2.265 [DOI] [Google Scholar]
- 28.Rogers WA, Lamson N, Rousseau GK. Warning research: an integrative perspective. Hum Factors. 2000;42(1):102–139. doi: 10.1518/001872000779656624 [DOI] [PubMed] [Google Scholar]
- 29.Gilreath TD, Leventhal A, Barrington-Trimis JL, et al. Patterns of alternative tobacco product use: emergence of hookah and e-cigarettes as preferred products amongst youth. J Adolesc Health. 2016;58(2): 181–185. doi: 10.1016/j.jadohealth.2015.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jawad M, El Kadi L, Mugharbil S, Nakkash R. Waterpipe tobacco smoking legislation and policy enactment: a global analysis. Tob Control. 2015;24(Suppl 1):i60–i65. doi: 10.1136/tobaccocontrol-2014-051911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nakkash R, Khalil J. Health warning labelling practices on narghile (shisha, hookah) waterpipe tobacco products and related accessories. Tob Control. 2010; 19(3):235–239. doi: 10.1136/tc.2009.031773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.US Food and Drug Administration. Required nicotine addictiveness warning on packages and advertising. http://www.fda.gov/TobaccoProducts/Labeling/ProductsIngredientsComponents/ucm482575.htm#nicotine. PublishedJanuary 3, 2020. Accessed March 13, 2020.
- 33.Helen GS, Benowitz NL, Dains KM, et al. Nicotine and carcinogen exposure after water pipe smoking in hookah bars. Cancer Epidemiol Biomarkers Prev. 2014;23(6):1055–1066. doi: 10.1158/1055-9965.EPI-13-0939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Keller-Hamilton B, Roberts ME, Slater MD, et al. Adolescent males’ responses to blu’s fake warnings. Tob Control. 2019;28(e2):el51–el53. doi: 10.1136/tobaccocontrol-2018-054805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kimber C, Frings D, Cox S, et al. Communicating the relative health risks of e-cigarettes: an online experimental study exploring the effects of a comparative health message versus the EU nicotine addiction warnings on smokers’ and non-smokers’ risk perceptions and behavioural intentions. Addict Behav. 2020; 101:106177. doi: 10.1016/j.addbeh.2019.106177 [DOI] [PMC free article] [PubMed] [Google Scholar]


