Abstract
Introduction
Myhre syndrome (MS) is an ultra‐rare disorder due to pathogenic variants in the SMAD4 gene that encodes a protein regulating the TGF‐β pathway and extra‐cellular matrix (ECM) homeostasis. Main clinical features of MS include thickening of skin and joint stiffness. Previous studies showed that losartan improved ECM deposition in MS fibroblasts.
Materials and methods
Four molecularly confirmed MS subjects (mean age 23.8 ± 17 years) were evaluated for: (a) skin thickness by Rodnan score, (b) joint range of motion (ROM) by goniometry, and (c) speckle‐tracking echocardiogram. Following baseline evaluations, three MS individuals received losartan for 12 months and pre‐defined endpoints were monitored after 6 and 12 months of treatment.
Results
At baseline, Rodnan scores were increased, joint ROM was reduced, and speckle‐tracking echocardiogram revealed reduced myocardial strain. In three MS subjects, improvements in skin thickness, joint ROM and to a lesser extent of myocardial strain, were observed after 6 and 12 months of losartan treatment.
Conclusions
Although further long‐term controlled clinical trials with a larger number of affected individuals are needed, the present study suggests that losartan might improve skin, joint and heart abnormalities of MS.
Keywords: losartan, Myhre syndrome, SMAD4, systemic sclerosis, TGF‐beta
1. INTRODUCTION
Myhre syndrome (MS; MIM 139210) is an autosomal dominant disorder presenting with short stature, short hands and feet, facial dysmorphisms, deafness, compact build, nonspecific skeletal anomalies, and a broad spectrum of scleroderma‐like manifestations, such as thickening of skin and joint stiffness due to progressive fibrosis (le Goff, Michot, & Cormier‐Daire, 2014; Lin et al., 2016). In MS abnormal fibrosis occurs spontaneously or following trauma or surgery, it is progressive, and it might lead to severe life‐threatening complications (e.g., laryngotracheal stenosis and pulmonary insufficiency, cardiomyopathy, and constrictive pericarditis) (Lin et al., 2016). MS is caused by recurrent pathogenic gain‐of‐function variants in the SMAD4 gene that encodes a protein involved in the bone morphogenetic pathway (BMP) and the transforming growth factor (TGF)‐β signaling pathway (Le Goff et al., 2012). SMAD4 pathogenic variants result in derangements of extra‐cellular matrix (ECM) homeostasis (le Goff et al., 2012; Piccolo et al., 2014). MS is part of TGF‐β‐pathies, a group of disorders that includes both genetic and nongenetic conditions, such as acromicric dysplasia (Banka et al., 2015), geleophysic dysplasia (Banka et al., 2015), Weill–Marchesani syndrome (Banka et al., 2015), Leri pleonosteosis (Banka et al., 2015), stiff skin syndrome (Banka et al., 2015), and systemic scleroderma (SSc). TGF‐β‐pathies share ECM abnormalities resulting in progressive fibrosis (Jensen et al., 2020). Rodnan score, joint range of motion (ROM) by goniometry and speckle‐tracking echocardiography have been used for monitoring skin, joint and heart fibrosis in SSc, the most common TGF‐β‐pathy (Khanna et al., 2017; Shima et al., 2015; Spethmann et al., 2014).
Losartan is an antihypertensive drug that blocks the type 1 receptor of angiotensin II. Besides its antihypertensive effect, losartan attenuates TGF‐β‐mediated fibrosis by lowering expression of TGF‐β activators and reducing both total and active TGF‐β and TGF‐β receptors (Habashi, 2006). Moreover, losartan can improve connective tissue abnormalities in SSc (Hughes et al., 2015). In MS fibroblasts, losartan restored balance in gene expression of metalloproteinases and their inhibitors and corrected fibrillin‐1 and COL1A1 deposition, suggesting an improvement of the ECM defect (Piccolo et al., 2014). Anecdotally, one MS individual with restrictive pulmonary disease treated with losartan in association with other anti‐inflammatory therapies showed some clinical improvement (Alape et al., 2020).
Clinical endpoints for monitoring MS progression and investigating new treatments are lacking and to overcome this gap, we took advantage of endpoints already established in SSc, including scores for skin thickness, joint ROM, and speckle‐tracking echocardiography (Khanna et al., 2017; Shima et al., 2015; Spethmann et al., 2014), that we evaluated in four MS individuals. Moreover, we investigated in three MS individuals the safety and efficacy of losartan.
2. SUBJECTS AND METHODS
2.1. Ethics statement
Losartan was given as off‐label treatment that received institutional review board approval and either parents or adult subjects were provided written informed consent at the beginning the study.
2.2. Clinical evaluations
Four Caucasians subjects (S1‐S4) included in this study had a MS diagnosis confirmed by SMAD4 pathogenic variants. Modified Rodnan score (mRSS; Khanna et al., 2017), joint ROM, and speckle tracking echocardiography were evaluated in all four individuals. Three subjects (S1‐S3) were re‐evaluated after 6 and 12 months of losartan treatment. The mRSS evaluates skin thickness by clinical palpation using a 0–3 scale for each of 17 surface anatomic areas of the body: face, anterior chest, abdomen, fingers (right and left separately), forearms, upper arms, tights, lower legs, dorsum of hands, and feet (Khanna et al., 2017). ROM was evaluated by goniometer (Shima et al., 2015) at elbow, wrist, knee, and ankle. ROM and mRSS were both evaluated in independent age‐, gender‐, and ethnicity‐matched controls (n = 5) from an outpatient general pediatric clinic. Skin thickness and joint ROM were evaluated by two examiners (G.C. for S1, S2, and S3 and G.M. for S4) three times per visit in each individual. Speckle‐tracking echocardiography using GE Healthcare VividE9 was used for quantitative assessment of motion of myocardial tissue. The software divided cardiac walls in several segments based on 17‐segment model, and we tracked points on a frame‐by‐frame basis to include the entire myocardium. Strain as percentage change in length of a myocardial segment and automatic function imaging was applied to analyze global longitudinal systolic peak strain (GLPS) of three apical views, including GLPS of apical four chamber view (GLPS‐A4C), GLPS of apical two chamber view (GLPS‐A2C), GLPS of apical long axis view (GLPS‐LAX) that generated an average GLPS (GLPS‐Avg; Menting et al., 2016). For S4, only GLPS‐Avg was available. Normal values have been reported to be 20.2 ± 1.6 for adults (Menting et al., 2016) and 20.2 ± 0.7 for pediatric patients (Levy et al., 2016).
2.3. Losartan treatment
Oral losartan for 12 months was given to three MS subjects (one child and two adults—S1, S2, S3). Following baseline evaluations, losartan was titrated to maintain baseline blood pressure levels (Table 1). Adverse events were recorded along with pre‐defined endpoints including: skin fibrosis and thickness by mRSS [performed by one examiner (G.C.) three times per visit], ROM of elbow, wrist, knee, ankle joints by goniometer [performed by one examiner (G.C.) three times per visit]; myocardial strain by two‐dimensional speckle tracking echocardiography [performed by the same operator (G.L.)].
TABLE 1.
Demographics and baseline clinical features
| Subject 1a | Subject 2b | Subject 3b,c | Subject 4 | |
|---|---|---|---|---|
| Current age (years) | 3.8 | 41.3 | 34 | 16 |
| Gender | Female | Female | Male | Female |
| Weight kg (SDS) | 11.5 (−2.2) | 56.5 (0) | 61 (0) | 34.5 (−3) |
| Height cm (SDS) | 83.8 (−3.9) | 140 (−3.8) | 140.5 (−4.4) | 126 (−5.7) |
| Head circumference cm (SDS) | 45.5 (−2.2) | 52.4 (−2.2) | 55.5 (−0.7) | 55 |
| Intellectual disability |
+ Mild |
+ Mild |
+ Severe |
+ Mild‐to‐moderate |
| Autism spectrum disorder | − | − | + | + |
| Heart disease |
+ Tetralogy of Fallot |
+ Aortic stenosis, arrhythmia |
− |
+ Aortic stenosis |
| Life‐threating complications | Pericarditis | − | − | 3‐min cardiac arrest |
| Hearing loss | − | + | N.A. | + |
| Eye |
+ Ectopia lentis |
− | − |
+ Myopia, astigmatism, cataract |
| Lung | − |
+ Restrictive pulmonary disease |
N.A. |
+ Restrictive pulmonary disease |
| Gastrointestinal system | − |
+ Recurrent abdominal pain |
+ Hyperamylasemia |
+ Duodenal and pyloric stenosis |
| Puberty/reproductive system | − |
+ Secondary amenorrhea |
− | N.A. |
| Recurrent infections | − | + | − |
+ Pneumonia |
| Surgery |
+ Tetralogy of Fallot correction |
+ Correction of aortic valve disease, endometrial curettage for menorrhagia |
+ Arthroscopy left elbow with secondary ankylosis |
+ Cardiac surgeries and pyloric/duodenal stenosis |
| Others | − | Recurrent abdominal pain, persistent neutrophilic leukocytosis, polycythemia, anxiety | − | Hepatomegaly, anxiety |
| Systolic blood pressure range mmHg | 92–75 | 130–100 | 110–85 | 110 |
| Diastolic blood pressure range mmHg | 50–70 | 86–76 | 72–58 | 64 |
| Drugs | Furosemide, Esomeprazol, aspirin | Aldactone, furosemide, omeprazole, aspirin | − | Aldactone, Esomeprazol |
2.4. Statistical analyses
Statistical analyses were performed using nonparametric tests (Kruskal–Wallis) and parametric tests (ANOVA, Student‐test). Statistical significance of differences among groups was evaluated using Kruskal–Wallis rank sum test (a nonparametric test which was used when ANOVA assumptions are not verified). Shapiro–Wilk test on the ANOVA residuals and Levene's test were used to test whether data are normally distributed and the variance across species are homogeneous. As the statistical test is significant, a post‐hoc analysis based on a Dunnet multiple pairwise‐comparisons was applied to determine significance difference between specific pairs of species. Analysis was carried out in R software environment and in GraphPadPrism8. p values below .05 were considered as statistically significant.
3. RESULTS
3.1. Baseline assessment
Three female and one male individuals with MS were evaluated [(average age: 23.8 ± 17 years (range 3.8–41.3 years)] (Table 1). S1, S2, and S3 were previously reported (Alagia et al., 2018; Caputo et al., 2012; Titomanlio et al., 2001). All subjects carried the same recurrent pathogenic SMAD4 sequence variant (NM_005359.5: c.1498A>G, p.Ile500Val) and presented with typical facial dysmorphisms, cardiac abnormalities, and intellectual disability (Table 1). Cardiac abnormalities included tetralogy of Fallot, progressive aortic valve disease, cardiac rhythm abnormalities, and pericarditis (Table 1). In SSc, mRSS is increased with an average score of 15 ± 12 (Khanna, 2006; Reveille et al., 2001). In four MS subjects, mRSS total score ranged from 10 to 25, with an average of 15.8 ± 1.5 that overlapped with the scores of SSc, and was different compared to the scores of 1.6 ± 1.2 (range: 0–4) detected in age‐ and gender‐matched controls (n = 5; p < .001; Figure 1a,b). Joint ROM of elbow flexion, wrist dorsal and palmar flexion, knee flexion, ankle plantar, and dorsal flexion measured by goniometer (Luttgens & Hamilton, 1997) in MS subjects were globally reduced compared to controls (p < .001; Figure 1c,d).
FIGURE 1.
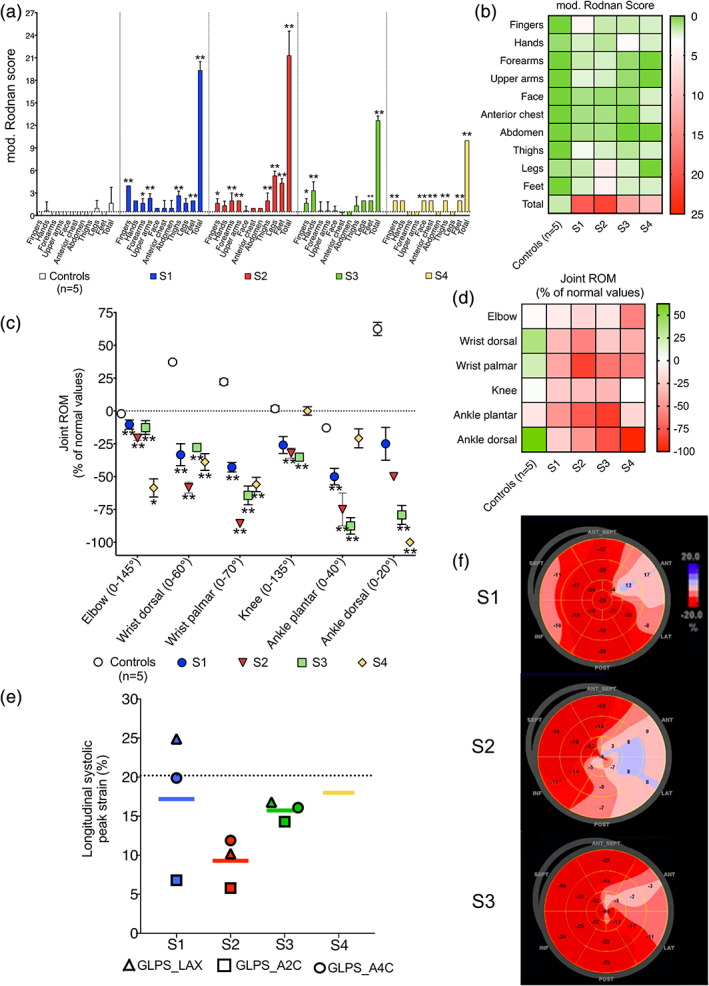
(a) Rodnan score at each skin site in subjects S1, S2, S3, S4 and controls (n = 5). (b) Heatmap for Rodnan score at each skin site and total score in each individual and controls. (c) Joint range of motion (ROM) at the elbow, wrist, knee and ankle in S1, S2, S3, S4 and controls (n = 5). Normal range from Luttgen and Hamilton (Luttgens & Hamilton, 1997) are reported in parenthesis. (d) Heatmap of joint ROM for each patient and controls at different sites. (e) Average global longitudinal systolic peak strain (GLPS). Dashed line indicates average value in controls, that in children corresponds to 20.2 ± 0.7% and in adults to 20.2 ± 1.6%. (f) Heart walls divided into 17 segments and segmental strain measurements were plotted in a bull's eye and left ventricular global longitudinal strain based on all three apical views was calculated. For S4, only average GLPS was available. GLPS, global longitudinal systolic peak strain; GLPS_LAX, long axis view; GLPS_A2C, apical 2 chambers view; GLPS_A4C, apical four chambers view [Color figure can be viewed at wileyonlinelibrary.com]
MS subjects were evaluated by speckle‐tracking echocardiography and average GLPS in four MS subjects was 15.3 ± 2% (Figure 1e,f) that is below the normal values of 20.2 ± 1.6% and 20.2 ± 0.7% reported in adults (Menting et al., 2016) and children (Levy et al., 2016), respectively. Lower GLPS values are detected in conditions impairing myocardial motion, such as myocardial fibrosis (Menting et al., 2016).
3.2. Losartan treatment
S4 discontinued losartan shortly after the time it was started because of dizziness, whereas the remaining three MS subjects (S1, S2, and S3) were treated with losartan for 12 months and evaluated after 6 and 12 months of treatment for mRSS, joint ROM, and speckle‐tracking echocardiography. S1 tolerated 0.7 mg/kg per day of losartan while subjects S2 and S3 who were both adults, were administered 100 mg and 50 mg per day, respectively (Figure 2a). S3 had orthostatic hypotension with 100 mg per day, and thus he continued with the lower dose of 50 mg/day (Figure 2a). S2 had aortic stenosis, a condition that might result in hypotension under losartan treatment. Nevertheless, this subject did not experience drops in blood pressure with losartan treatment.
FIGURE 2.
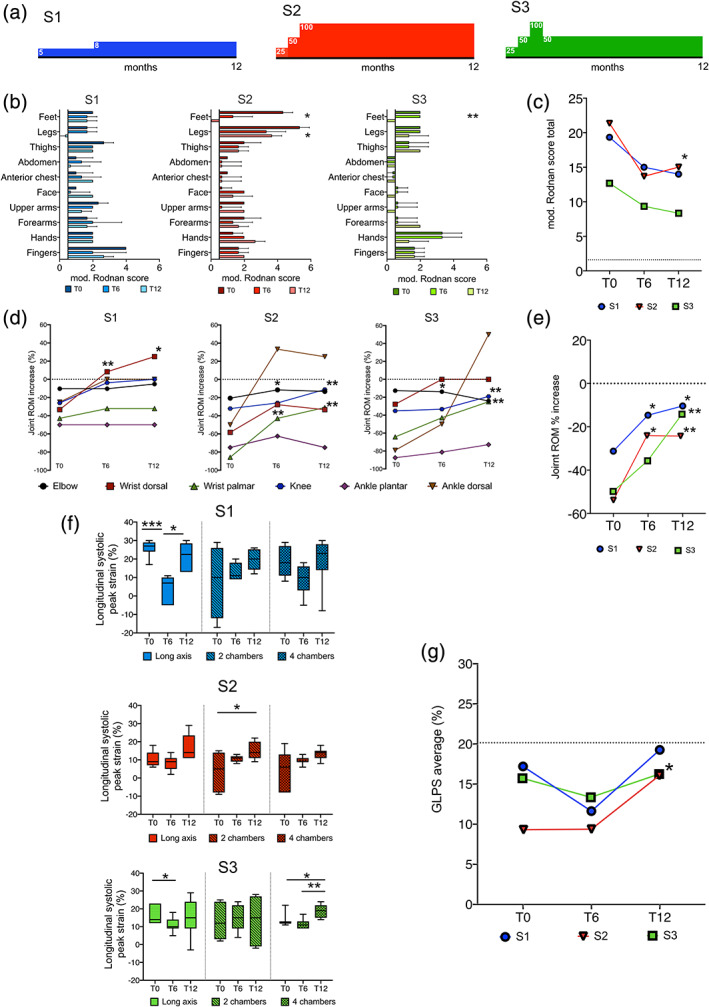
(a) Subjects S1 (blue), S2 (red), S3 (green) were treated with losartan for 12 months and the dose was titrated according to blood pressure levels (numbers in boxes indicate mg per day). (b,c) Modified Rodnan scores evaluated at baseline (T0) and after 6 (T6) and 12 (T12) months of treatment with losartan in subjects S1, S2, and S3. Single sites (b) andglobal (c) scores are shown. Dashed lines (c) indicate average total score detected in controls (n =5). (D,E) Joint ROM in three MS subjects at baseline (T0) and after 6 (T6) and 12 (T12) months of treatment. Single sites (d) and average scores (e) are shown. The dashed line (d, e) indicates average value in controls. (f, g) Apical views (long axis, two chambers, four chambers; f) and average global longitudinal systolic peak strain (GLPS; g) in three subjects after 6 and 12 months of treatment with losartan. The dashed line indicates the average value in controls: GLPS average normal values in children is 20.2 ± 0.7% and in adults is 20.2 ± 1.6%. ANOVA and Kruskal–Wallis rank sum test have been used for significance calculation, *p < .05, **p < .01 [Color figure can be viewed at wileyonlinelibrary.com]
During treatment, S2 self‐reported an improvement in climbing stairs and parents reported improvement in swimming skills in S3. Following 12 months of losartan, mRSS decreased in all subjects compared to baseline evaluations (Figure 2b,c) and joint ROM improved in all subjects (Figure 2d,e). Although a statistical significance was only obtained for S2, a trend towards improved GLPS was observed in the other two subjects treated with losartan. The improved area varied among subjects, and myocardial segments belonging to 2‐ and 4‐chamber views showed statistical differences at T6 and T12 in S2 and S3, respectively (Figure 2f,g and Figure S1).
4. DISCUSSION
Early diagnosis of MS by high‐throughput targeted, exome or genome sequencing is becoming increasingly more common (Alagia et al., 2018), thus offering the opportunity for surveillance of long‐term and life‐threatening disease complications. Moreover, there is a strong need to gain knowledge on the natural history of MS and to identify endpoints that can be evaluated to establish the efficacy of novel therapies. In the present study, we aimed at identifying such endpoints. In addition, we investigated the efficacy of losartan treatment in a pilot preliminary study on MS subjects.
Diffuse fibrosis of skin and internal organs with dermal thickening and collagen infiltration, are manifestation of MS (le Goff et al., 2014) resembling the skin involvement of SSc, a chronic multisystem autoimmune disorder due to excessive collagen deposition in skin and visceral organs. MS and SSc share the involvement of TGF‐β pathway as underlying disease mechanism (Banka et al., 2015). Based on these similarities, we applied in MS the measurements used to monitor SSc, including mRSS, goniometry, and speckle‐tracking echocardiography to evaluate skin, joint, and myocardial fibrosis, respectively. Total mRSS was increased in MS compared to controls and within the range typically observed in SSc (Khanna, 2006). Notably, in S1 who was 3‐year and 10‐month old at the time of the evaluation, mRSS was 19 which was higher than age‐matched controls, suggesting that fibrotic skin induration might be an early and progressive finding in MS. Compared to normal values (Luttgens & Hamilton, 1997) and our internal controls, MS individuals also showed reduced joint ROM with a pattern of joint involvement (wrists and ankles) similar to SSc (Shima et al., 2015). However, both mRSS and joint ROM evaluations were performed in a nonblinded manner and thus, potential bias cannot be excluded.
Consistent with high prevalence of cardiac problems in MS (Lin et al., 2016), all five MS cases showed cardiac involvement, including congenital heart disease (tetralogy of Fallot in two cases), progressive aortic valve disease, constrictive pericarditis, and arrhythmia. The presence of congenital heart defects, especially following surgical correction, is per se responsible for abnormal speckle tracking parameters (Takayasu et al., 2011). Nevertheless, cardiac involvement (i.e., morphological and electrical) was absent in S3, suggesting that reduced myocardial strain is an intrinsic abnormality of MS. Speckle tracking echocardiography can detect subclinical myocardial damage and areas of regional fibrosis and stiffness in scleroderma patients (Candan et al., 2017). Here, we showed that systolic strain rate was significantly reduced in MS cases, suggesting that GLPS might be a sensitive, noninvasive method to detect cardiac fibrosis in MS. However, further prospective studies are needed to establish the clinical relevance and prognosis of the cardiac fibrosis in MS.
Based on previous studies (Piccolo et al., 2014), we evaluated the efficacy of losartan in reducing fibrosis‐related symptoms in three MS subjects. Skin fibrosis and joint ROM were both significantly improved after 12 months of treatment with upper and lower arms showing the most substantial changes. Moreover, cardiac fibrosis showed a significant improvement in one subject (S2) and a trend for improvement in the remaining two cases. Taken together, reduced skin fibrosis and increased joint ROM and GLPS suggest an improvement of the underlying connective tissue defect in MS by losartan. The two adult subjects (S2 and S3) received different doses of losartan because of an adverse event of decreased blood pressure in one of them (S3). Although generally well tolerated, losartan can induce hypotension and this risk is especially higher in MS patients with aortic stenosis.
The lack of a control group and the small sample size are limitations of this pilot study and further clinical trials performed in a blinded and randomized fashion and involving a larger number of cases are needed to show whether losartan is an effective treatment for MS. This study does not allow firm conclusions on the efficacy of losartan to be drawn and thus, treatment with losartan in MS based on currently available data is not recommended. Nevertheless, the preliminary data from this pilot study are encouraging and support future development of clinical trials.
In conclusion, the present study identifies endpoints to monitor progression of MS on skin, joints and heart that might be useful also to evaluate treatment efficacy. Given its excellent safety profile, and its effects on skin, joint, and heart fibrosis, this study suggests that losartan might provide clinical benefit in MS.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
Gerarda Cappuccio and Nicola Brunetti‐Pierri conceptualized the paper, collected patients' information from collaborators, conducted and managed the trial. Martina Caiazza, Marta Rubino, and Giuseppe Limongelli performed cardiological evaluations. Alessandro Roca, Daniela Melis contributed to clinical case information. Antonella Iuliano performed statistical analysis. All the authors critically revised the manuscript and gave final approval.
Supporting information
FIGURE S1 Bull's eye 17‐segment model plot from speckle tracking echocardiography during losartan treatment. T0: baseline; T6: 6 months of losartan treatment; T12: 12 months of losartan treatment
ACKNOWLEDGMENTS
We are grateful to patients and their parents for participating to the study. This study was supported by Fondazione Telethon, Telethon Undiagnosed Diseases Program (TUDP, GSP15001). We acknowledge M. Aschwanden, B. Donner, B. Müller‐Schenker, J.‐P. Pfammatter, C. Seppi, and A. Wörner for clinical and instrumental evaluations of subject S4.
Cappuccio G, Caiazza M, Roca A, et al. A pilot clinical trial with losartan in Myhre syndrome. Am J Med Genet Part A. 2021;185A:702–709. 10.1002/ajmg.a.62019
Funding information Fondazione Telethon, Grant/Award Number: GSP15001
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Alagia, M. , Cappuccio, G. , Pinelli, M. , Torella, A. , Brunetti‐Pierri, R. , Simonelli, F. , … Brunetti‐Pierri, N. (2018). A child with Myhre syndrome presenting with corectopia and tetralogy of Fallot. American Journal of Medical Genetics, Part A, 176(2), 426–430. 10.1002/ajmg.a.38560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alape, D. , Singh, R. , Folch, E. , Fernandez Bussy, S. , Agnew, A. , & Majid, A. (2020). Life‐threatening multilevel airway stenosis due to Myhre syndrome. American Journal of Respiratory and Critical Care Medicine, 201(6), 731–732. 10.1164/rccm.201905-0922IM [DOI] [PubMed] [Google Scholar]
- Banka, S. , Cain, S. A. , Carim, S. , Daly, S. B. , Urquhart, J. E. , Erdem, G. , … Newman, W. G. (2015). Leri's pleonosteosis, a congenital rheumatic disease, results from microduplication at 8q22.1 encompassing GDF6 and SDC2 and provides insight into systemic sclerosis pathogenesis. Annals of the Rheumatic Diseases, 74(6), 1249–1256. 10.1136/annrheumdis-2013-204309 [DOI] [PubMed] [Google Scholar]
- Candan, O. , Gecmen, C. , Bayam, E. , Guner, A. , Celik, M. , & Doğan, C. (2017). Mechanical dispersion and global longitudinal strain by speckle tracking echocardiography: Predictors of appropriate implantable cardioverter defibrillator therapy in hypertrophic cardiomyopathy. Echocardiography, 34(6), 835–842. 10.1111/echo.13547 [DOI] [PubMed] [Google Scholar]
- Caputo, V. , Cianetti, L. , Niceta, M. , Carta, C. , Ciolfi, A. , Bocchinfuso, G. , … Tartaglia, M. (2012). A restricted spectrum of mutations in the SMAD4 tumor‐suppressor gene underlies Myhre syndrome. The American Journal of Human Genetics, 90(1), 161–169. 10.1016/j.ajhg.2011.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habashi, J. P. (2006). Losartan, an AT1 antagonist, prevents aortic aneurysm in a mouse model of Marfan syndrome. Science, 312(5770), 117–121. 10.1126/science.1124287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, M. , Ong, V. H. , Anderson, M. E. , Hall, F. , Moinzadeh, P. , Griffiths, B. , … Herrick, A. L. (2015). Consensus best practice pathway of the UKscleroderma study group: Digital vasculopathy in systemic sclerosis. Rheumatology, 54(11), 2015–2024. 10.1093/rheumatology/kev201 [DOI] [PubMed] [Google Scholar]
- Jensen, B. , James, R. , Hong, Y. , Omoyinmi, E. , Pilkington, C. , Sebire, N. J. , … Eleftheriou, D. (2020). A case of Myhre syndrome mimicking juvenile scleroderma. Pediatric Rheumatology Online Journal, 18(1), 72 10.1186/s12969-020-00466-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna, D. (2006). Minimally important difference in diffuse systemic sclerosis: Results from the D‐penicillamine study. Annals of the Rheumatic Diseases, 65(10), 1325–1329. 10.1136/ard.2005.050187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna, D. , Furst, D. E. , Clements, P. J. , Allanore, Y. , Baron, M. , Czirjak, L. , … Denton, C. P. (2017). Standardization of the modified Rodnan skin score for use in clinical trials of systemic sclerosis. Journal of Scleroderma and Related Disorders, 2(1), 11–18. 10.5301/jsrd.5000231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- le Goff, C. , Michot, C. , & Cormier‐Daire, V. (2014). Myhre syndrome. Clinical Genetics, 85(6), 503–513. 10.1111/cge.12365 [DOI] [PubMed] [Google Scholar]
- le Goff, C. , Mahaut, C. , Abhyankar, A. , le Goff, W. , Serre, V. , Afenjar, A. , … Cormier‐Daire, V. (2012). Mutations at a single codon in Mad homology 2 domain of SMAD4 cause Myhre syndrome. Nature Genetics, 44(1), 85–88. 10.1038/ng.1016 [DOI] [PubMed] [Google Scholar]
- Levy, P. T. , Machefsky, A. , Sanchez, A. A. , Patel, M. D. , Rogal, S. , Fowler, S. , … Singh, G. K. (2016). Reference ranges of left ventricular strain measures by two‐dimensional speckle‐tracking echocardiography in children: A systematic review and meta‐analysis. Journal of the American Society of Echocardiography, 29(3), 209–225.e6. 10.1016/j.echo.2015.11.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, A. E. , Michot, C. , Cormier‐Daire, V. , L'Ecuyer, T. J. , Matherne, G. P. , Barnes, B. H. , … Lindsay, M. E. (2016). Gain‐of‐function mutations in SMAD4 cause a distinctive repertoire of cardiovascular phenotypes in patients with Myhre syndrome. American Journal of Medical Genetics. Part A, 170(10), 2617–2631. 10.1002/ajmg.a.37739 [DOI] [PubMed] [Google Scholar]
- Luttgens, K. , & Hamilton, N. (1997). Kinesiology: scientific and, basis of human motion (9th ed.). Madison, WI: Benchmark. [Google Scholar]
- Menting, M. E. , van Grootel, R. W. J. , van den Bosch, A. E. , Eindhoven, J. A. , McGhie, J. S. , Cuypers, J. A. A. E. , … Roos‐Hesselink, J. W. (2016). Quantitative assessment of systolic left ventricular function with speckle‐tracking echocardiography in adult patients with repaired aortic coarctation. The International Journal of Cardiovascular Imaging, 32(5), 777–787. 10.1007/s10554-016-0838-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccolo, P. , Mithbaokar, P. , Sabatino, V. , Tolmie, J. , Melis, D. , Schiaffino, M. C. , … Brunetti‐Pierri, N. (2014). SMAD4 mutations causing Myhre syndrome result in disorganization of extracellular matrix improved by losartan. European Journal of Human Genetics, 22(8), 988–994. 10.1038/ejhg.2013.283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reveille, J. D. , Fischbach, M. , McNearney, T. , Friedman, A. W. , Aguilar, M. B. , Lisse, J. , … GENISOS Study Group . (2001). Systemic sclerosis in 3 US ethnic groups: A comparison of clinical, sociodemographic, serologic, and immunogenetic determinants. Seminars in Arthritis and Rheumatism, 30(5), 332–346. 10.1053/sarh.2001.20268 [DOI] [PubMed] [Google Scholar]
- Shima, Y. , Hosen, N. , Hirano, T. , Arimitsu, J. , Nishida, S. , Hagihara, K. , … Kumanogoh, A. (2015). Expansion of range of joint motion following treatment of systemic sclerosis with tocilizumab. Modern Rheumatology, 25(1), 134–137. 10.3109/14397595.2013.874749 [DOI] [PubMed] [Google Scholar]
- Spethmann, S. , Rieper, K. , Riemekasten, G. , Borges, A. C. , Schattke, S. , Burmester, G.‐R. , … Knebel, F. (2014). Echocardiographic follow‐up of patients with systemic sclerosis by 2D speckle tracking echocardiography of the left ventricle. Cardiovascular Ultrasound, 12, 13 10.1186/1476-7120-12-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takayasu, H. , Takahashi, K. , Takigiku, K. , Yasukochi, S. , Furukawa, T. , Akimoto, K. , … Shimizu, T. (2011). Left ventricular torsion and strain in patients with repaired tetralogy of Fallot assessed by speckle tracking imaging. Echocardiography, 28(7), 720–729. 10.1111/j.1540-8175.2011.01417.x [DOI] [PubMed] [Google Scholar]
- Titomanlio, L. , Marzano, M. G. , Rossi, E. , D'Armiento, M. , de Brasi, D. , Vega, G. R. , … Sebastio, G. (2001). Case of Myhre syndrome with autism and peculiar skin histological findings. American Journal of Medical Genetics, 103(2), 163–165. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FIGURE S1 Bull's eye 17‐segment model plot from speckle tracking echocardiography during losartan treatment. T0: baseline; T6: 6 months of losartan treatment; T12: 12 months of losartan treatment
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


