Abstract
Background and Aims
Lower-cost biosimilar infliximab may address affordability concerns in the treatment of adults with Crohn’s disease (CD), however, evidence regarding the cost-effectiveness of switching from reference to biosimilar is warranted. The aim of this research was to assess the incremental cost of switching from treatment with reference infliximab to biosimilar compared with maintaining reference infliximab in adults with CD per quality-adjusted life year (QALY) gained.
Methods
A probabilistic cohort Markov model with 8-week cycle lengths was constructed to estimate the incremental costs and effects of switching over a 5-year time horizon from a public payer perspective. Base-case clinical inputs were obtained from NOR-SWITCH subgroup analyses and other published trials. Costs were obtained from Canadian sources. A total of 10,000 simulations were run. Sensitivity analysis was used to test the robustness of the results to variations in uncertain parameters.
Results
Switching to biosimilar infliximab was less costly but also less effective with incremental savings of $46,194 (95% confidence interval [CI]: $42,420, $50,455) and a loss in QALYs of −0.13 (95% CI: −0.16, −0.07). Eighty-three per cent of the simulations demonstrated incremental cost savings and an incremental loss of effectiveness. The model was sensitive to differences in rates of disease worsening between reference and biosimilar infliximab.
Conclusions
While biosimilar infliximab is associated with incremental savings for patients on maintenance therapy who are switched from reference infliximab, funding decision makers must decide whether a small loss of effectiveness is justified. Further evidence will help to inform reimbursement policy.
Keywords: Cost-utility analysis, Crohn’s disease, Infliximab
Introduction
While biologics are an important treatment option for many patients with complex diseases such as cancer, or inflammatory conditions, they require complex manufacturing, resulting in high costs (1,2). Studies have shown that expenditures on biologics in public and private drug plans has grown dramatically over time, creating sustainability concerns (3–6).
The anti-tumour necrosis factor (TNF) alpha biologic infliximab offers immense value in treating Crohn’s disease (CD), a fluctuating chronic illness which greatly affects quality of life (7). Treatment with infliximab has been shown to induce and maintain remission, reduce symptom flares and slow progression in some cases (8,9). The introduction of biosimilar infliximab represents another treatment option at a lower cost. A biosimilar is highly similar, but not identical to a reference biologic, and enters the market at a lower price than the reference (10). While biosimilars offer an opportunity to derive cost savings, their entrance has raised questions among stakeholders.
For example, because the manufacturing of biosimilars is more complicated than that of a small molecule drug, there may be variability between the biosimilar and the reference product (11). These variations can affect both the efficacy and immunogenicity of the drug (12). Immunogenicity is an important safety concern for treating physicians, particularly in considering switching, as anti-drug antibodies can neutralize the activity of the biologic, reduce efficacy or cause serious immune reactions (1). To date, the pivotal trials and observational evidence suggest that there are no clinically meaningful differences in safety and effectiveness between reference and biosimilar infliximab, however, stakeholders have maintained concerns regarding their use (13–16).
The NOR-SWITCH study was a randomized controlled trial that compared reference infliximab to biosimilar infliximab in CD, ulcerative colitis, spondylarthritis, rheumatoid arthritis, psoriatic arthritis and chronic plaque psoriasis. Disease worsening was the primary outcome and occurred in 26% of the group maintained on reference infliximab and 30% of the group switched from reference to biosimilar. The adjusted risk difference of −4.4% (95% confidence interval [CI]: −12.7% to 3.9%) in disease worsening was within the pre-specified margin implying biosimilar infliximab was not inferior to reference infliximab across all diseases. In the CD subgroup, disease worsening occurred in 21.2% of the reference group and 36.5% of the biosimilar infliximab group resulting in a risk difference of −14.3% (−29.3% to 0.7%) which was within the 15% clinical margin specified by the authors (11).
The objective of this economic evaluation was to utilize NOR-SWITCH to assess the incremental cost of switching from reference to biosimilar infliximab compared with maintaining reference infliximab in adult patients with moderate-to-severe CD per quality-adjusted life year (QALY) gained from a public health care system payer perspective over a 5-year time horizon.
Materials and Methods
Study Design
A cost-utility analysis was conducted from the perspective of the Canadian publicly funded health care payer. A cohort state transition (Markov) model was constructed and populated with parameters derived from the literature. It was assumed that the reference patient was 38 years old with a previous diagnosis of moderate-to-severe CD, weighed 75 kg and did not have any major comorbidities in accordance with the NOR-SWITCH population (11–13). It was assumed that the patient had been maintained on stable treatment with reference infliximab for a minimum of 6 months and could be taking concomitant immunosuppressives or prednisone (11).
Model Structure
The model evaluated a one-time switch from reference to biosimilar infliximab with identical dosing and administration. The comparator was maintenance treatment on reference infliximab. The model was built utilizing a health-state transition (Markov) framework in Treeage Pro 2018 (14). A Markov model is suitable for chronic conditions with ongoing risk, such as CD, where the patient may transition between a number of health states over the course of the time horizon of the analysis (18).
The model simulated disease progression and assessed costs and effects over a 5-year time horizon with 8-week cycle lengths in keeping with the dosing of infliximab (15,16). A total of 10,000 simulations were run and results were reported as mean total costs per patient per group, mean QALYs per patient per group, mean incremental costs, and mean QALYs with 95% CIs.
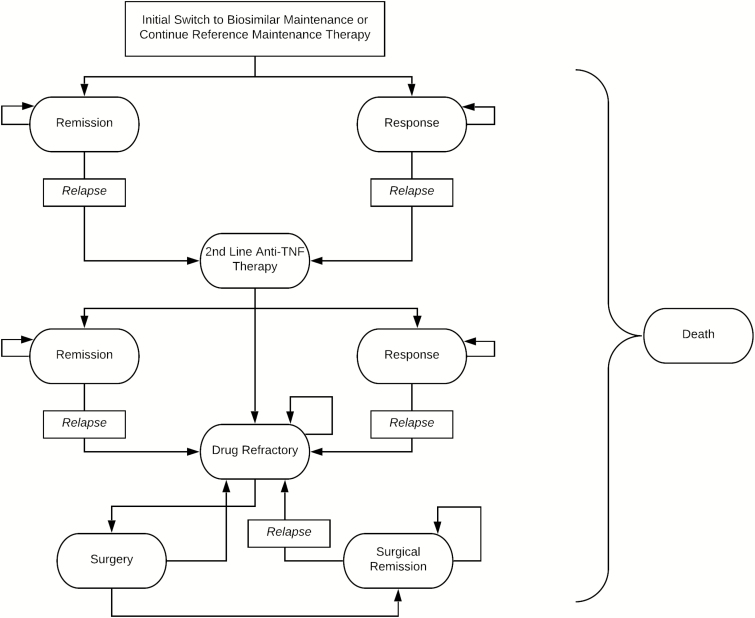
The structure of the model is summarized in Figure 1. The structure was designed in accordance with published economic evaluations of infliximab in CD and reviewed by a clinical expert for face validity (18). After entering the model, patients were distributed into clinical remission or clinical response health states. In subsequent cycles, it was assumed that a patient either maintained clinical remission or response, or relapsed. If a patient relapsed while on infliximab, they were switched to second-line treatment with adalimumab, which is recommended in the event of failure by Canadian guidelines (12,17). Subsequently, if they failed on adalimumab, then they entered a drug refractory state. A portion of the patients in the drug refractory state received a surgical intervention to treat their active disease, where they could then transition to surgical remission or if unsuccessful, a drug refractory state where they remained for the duration of the model. Similarly, if a patient relapsed from surgical remission, they remained in a drug refractory state. Finally, a patient could enter the absorbing death state from any health state. Patients were also subject to infusion-related adverse events during the infliximab treatment phase of the model.
Figure 1.
Model structure. The structure of the model is summarized in Figure 1. It is assumed that the patient enters the model and the treatment decision either requires the patient to continue maintenance therapy with reference infliximab or switch to treatment with biosimilar infliximab with identical dosing and administration. Patients then enter the Markov model and were distributed into one of two states: clinical remission or clinical response and move through the model as shown.
Future costs and outcomes were discounted to a present value at a rate of 1.5% in keeping with current Canadian Agency for Drugs and Technologies in Health (CADTH) guidelines (18).
Model Parameters
Since the analysis was probabilistic, a distribution was assigned to each input parameter, including transition probabilities, costs and utilities. Distributions were determined based on the mean values and standard deviations where available in published sources. Beta distributions were applied to utilities and to health state transition probabilities as they are bound by 0 and 1. Normal distributions for drug prices and physician fees were applied, and a gamma distribution was applied to surgical costs.
Transition Probabilities
The clinical inputs of the model were primarily informed by the CD subgroup of NOR-SWITCH (11). The trial showed that 41 patients in the reference group and 43 in the biosimilar group were in clinical remission as defined by the Harvey Bradshaw Index (HBI) (≤ 4 points) at the baseline of the trial (11). The analysis employed this proportion of patients in remission as the initial distribution of patients in the clinical remission state (all other patients were assumed to be in a clinical response state).
The rate of disease worsening, defined in the NOR-SWITCH study as a consensus between investigator and patient leading to major change in treatment or a change from baseline in HBI of 4 points or more and a score of 7 points or greater, was applied as the probability of relapse for patients on infliximab (11).
The transition probabilities for second-line treatment and surgical intervention were based on the methodology described in Blackhouse et al. (2012) and the referenced adalimumab clinical trials (12,19,20). The probability of achieving surgical remission was derived from a Markov cohort model in CD (21). Finally, the results of a study of postoperative recurrence of CD were used to derive a relapse rate from surgical remission (22).
For all states other than surgery, the probability of death was determined using annual probabilities of death from the Statistics Canada Life Table and a standardized mortality ratio of 1.45 (23,24). Mortality in the surgical state was derived from a meta-analysis of postoperative mortality patients with CD (25).
Utilities
The utilities from a study by Greenberg et al. (2015) were employed in this model (26). As informed by the available evidence, it was assumed that there was no difference in utilities between the reference and biosimilar (11). Table 1 presents a summary of the transition probabilities and utilities.
Table 1.
Parameters and distributions
| Parameter | Distribution | Mean value Reference | Mean value Biosimilar | Source |
|---|---|---|---|---|
| Initial | ||||
| Clinical Remission | Beta | 0.62 (α = 41, β = 25) | 0.68 (α = 43, β = 20) | Jorgensen et al. (2017) |
| Clinical Response | Beta | 0.38 (α = 25, β = 41) | 0.32 (α = 20, β = 43) | |
| Relapse | ||||
| Relapse from Response/Remission with IFX | Beta | 0.212 (α = 14, β = 52) | 0.365 (α = 23, β = 40) | Jorgensen et al. (2017) |
| Probability of moving from Drug Refractory to Surgery | Beta | 0.038 (α = 10, β = 251) | 0.038 (α = 10, β = 251) | Feagan et al. (2008) |
| Relapse from Surgical Remission | Beta | Year 1: 0.05 (α = 2, β = 38) Year 2: 0.211 (α = 8, β = 30) Year 3: 0.143 (α = 3, β = 21) | Year 1: 0.05 (α = 2, β = 38) Year 2: 0.211 (α = 8, β = 30) Year 3: 0.143 (α = 3, β = 21) | Onali et al. (2016) |
| Year 4: 0.111 (α = 2, β = 18) Year 5: 0.06 (α = 1, β = 15) | Year 4: 0.111 (α = 2, β = 18) Year 5: 0.06 (α = 1, β = 15) | |||
| Remission/Response | ||||
| ADA Response to Initial Therapy | Beta | 0.38 (α = 61, β = 98) | 0.38 (α = 61, β = 98) | Sandborn et al. (2007) |
| ADA Clinical Remission (After Initial Response) | Beta | 0.21 (α = 34, β = 27) | 0.21 (α = 34, β = 27) | |
| Probability of maintaining remission with ADA | Beta | 0.36 (α = 62, β = 110) | 0.36 (α = 62, β = 110) | Colombel et al. (2007) |
| Probability of maintaining response with ADA | Beta | 0.413 (α = 71, β = 101) | 0.413 (α = 71, β = 101) | |
| Probability of successful surgery | Beta | 0.52022 (α = 52.022, β = 47.978) | 0.52022 (α = 52.022, β = 47.978) | Silverstein et al. (1999) |
| Adverse Events in IFX States | ||||
| Probability of adverse events | Beta | 0.04 (α = 10, β = 231) | 0.02 (α = 4, β = 236) | Jorgensen et al. (2017) |
| Utilities | ||||
| Remission (IFX, ADA & Surgical) | Beta | 0.75 (SD: 0.12) | 0.75 (SD: 0.12) | Greenberg et al. (2015) |
| Response (IFX, ADA) | Beta | 0.63 (SD: 0.1) | 0.63 (SD: 0.1) | |
| Drug Refractory, Surgery and ADA Initiation | Beta | 0.51 (SD: 0.12) | 0.51 (SD: 0.12) |
ADA, Adalimumab; IFX, Infliximab; SD, Standard deviation.
Costs
Direct health care costs in the model included costs for infliximab, adalimumab, concomitant immunosuppressives and steroids, physician services and surgery. When applicable, all costs were inflated to 2017 Canadian dollars using the Consumer Price Index for Health and Personal Care in Canada (27).
Normal distributions for drug costs were established based on real-world Canadian prices. Average prices for reference infliximab, adalimumab and concomitant therapies were established based on Canadian formularies with a publicly available price (28–34). A standard deviation (SD) was derived based on this range of prices (Supplementary Appendix).
For biosimilar infliximab, the Ontario price was employed and the same standard deviation as reference infliximab was applied. Ontario dispensing fees and infusion costs for infliximab were also applied. These distributions for drug costs were reflective of Canadian public list prices as of 2017 and do not account for changes in price over time or any confidential price rebates which may exist.
In cases when a patient required a fraction of an infliximab vial to meet the required dose, it was assumed that there was vial wastage and usage was rounded to the next whole vial. Administration costs of CAD $139.80, consisting of nursing supervision time and infusion costs, and adverse event treatment costs of CAD$13.95, consisting of nursing supervision time and treatment medications, were also included for infliximab.
Drugs used in the drug refractory state or as concomitant therapy included prednisone, 6-mercaptorurine, methotrexate and azathioprine. The dosage regimens and proportions of patients utilizing these therapies were based on NOR-SWITCH, expert opinion and on the methods employed by Blackhouse et al. (2012) (11,12,31). A summary of the drug costs is presented in Table 2.
Table 2.
Drug costs
| Drug | Price (SD) | Dose | Total drug cost per cycle | Total dispensing fee per cycle |
|---|---|---|---|---|
| Reference Infliximab | $994.75 (44.94) per 100 mg/10 mL | 5 mg/kg Patient Weight: 75 kg | $3,979.00 | $8.83 |
| Biosimilar Infliximab | $525.00 (44.94) per 100 mg/vial | 5 mg/kg Patient Weight: 75 kg | $2,100.00 | $8.83 |
| Adalimumab (Initiation Cycle) | $916.86 (334.06) per 40 mg/0.8 mL | Week 0: 160 mg Week 2: 80 mg Week 4,6, 8: 40 mg | $8,251.74 | $35.32 |
| Adalimumab (Maintenance Cycle) | $916.86 (334.06) per 40 mg/0.8 mL | Week 2, 4, 6, 8: 40 mg | $3,667.44 | $35.32 |
| Prednisone | $0.0480 (0.0269) per tablet | 20 mg per day (4 tabs) | $15.17 | $8.83 (per 100-day supply) |
| Azathioprine | $0.2140 (0.0836) per tablet | 150 mg per day (3 tabs) | $40.37 | $8.83 (per 100-day supply) |
| 6 Mercaptopurine | $2.9378 (0.1202) per tablet | 75 mg per day (1.5 days) | $251.19 | $8.83 (per 100-day supply) |
| Methotrexate | $0.6474 (0.0255) per tablet | 25 mg per day (10 tabs) | $366.96 | $8.83 (per 100-day supply) |
All costs in 2017 Canadian dollars.
SD, Standard deviation.
It was assumed that an ileocolic surgical resection was conducted during the surgical state and the costs for surgery were derived from the Ontario Case Costing Initiative (OCCI). A weighted average (by number of cases) of two Case Mix Group (CMG) codes for resection was derived to represent the cost for a resection for patients with a CD diagnosis aged 18 to 69 years in Ontario, resulting in a surgical cost of CAD$12,138 (SD: $5,729) (41). Presurgery consults, the surgical procedure, and postsurgery assessments were based upon expert opinion and prices were obtained from the Ontario Schedule of Benefits (35,36).
The number of physician visits was estimated based on a profile of resource utilization for CD patients developed by an expert panel of clinical gastroenterologists (35). Assessment fees for physician visits for Canadian provinces were used to derive a mean and standard deviation which were applied with a normal distribution (36–45).
Societal Perspective
Employing the model described above, an alternative societal perspective was also tested. Lost time was accrued in the event of an in-patient hospital stay, a physician visit and an infusion visit (Supplementary Appendix) (46). An average hourly wage for an adult working age population was employed (47).
Uncertainty Analyses
One-way probabilistic analyses were run to determine the incremental costs and incremental effects for alternative values for patient weight, infliximab drug cost, health state utilities and the relapse rate from clinical remission or from response states after being switched to biosimilar infliximab. One-way probabilistic analysis was conducted by altering the point estimate and distribution, where applicable, for the variable of interest and running the analysis with 10,000 simulations. Structural uncertainty was evaluated through varying the discount rate (0% to 5%) and the time horizon of the model (1 year and 10-year time horizon).
Finally, a threshold analysis was conducted on the probability of relapse in the biosimilar group to determine the per cycle transition probability where the average QALYs associated with the biosimilar infliximab treatment group surpassed that of the reference infliximab group. Table 3 includes a summary of all one-way sensitivity analyses and their corresponding distributions.
Table 3.
Sensitivity analyses
| Sensitivity analysis parameter | Distribution | Mean value Reference | Mean value Biosimilar |
|---|---|---|---|
| Reference Infliximab Drug Cost | |||
| 20% Price Discount | Beta | $795.95 (SD: 44.936) | N/A |
| Biosimilar Infliximab Drug Cost | |||
| 72% Price Discount | Beta | N/A | $279.07 (SD: 44.936) |
| Utilities | |||
| Remission (IFX, ADA, Surgical) | Beta | 0.82 (α = 82, β = 18) | 0.82 (α = 82, β = 18) |
| Response (IFX, ADA) | Beta | 0.73 (α = 73, β = 27) | 0.73 (α = 73, β = 27) |
| ADA Initiation, Drug Refractory, Surgery | Beta | 0.51 (α = 54, β = 46) | 0.51 (α = 54, β = 46) |
| Patient Weight | Fixed | 40 kg | 40 kg |
| 50 kg | 50 kg | ||
| 60 kg | 60 kg | ||
| 70 kg | 70 kg | ||
| 80 kg | 80 kg | ||
| 90 kg | 90 kg | ||
| Relapse Rates | |||
| Relapse Rate from IFX Clinical Remission | Beta | 0.08 (SD: 0.08) | |
| Relapse Rate from IFX Clinical Response | Beta | 0.25 (SD: 0.3) |
All costs in 2017 Canadian dollars.
ADA, Adalimumab; IFX, Infliximab; SD, Standard deviation.
Results
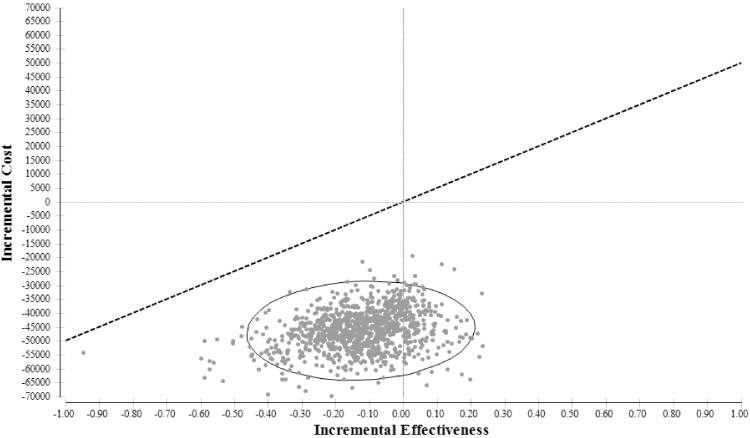
For clarity, the results of the base case are presented as separate incremental effects and incremental costs rather than an incremental cost-effectiveness ratio (ICER) given that the results primarily lie in the south-west quadrant of the ICER plane (less effective and less costly).
The average total costs per person were CAD$96,385 (SD: $6,834) and CAD$50,191 (SD: $4,771) for the reference infliximab and biosimilar strategies, respectively. Total incremental costs were −$46,194 (95% CI: −$42,420 to −$50,455) over the 5-year time horizon. With regards to effectiveness, maintenance treatment with reference infliximab was associated with 3.19 QALYs (SD: 0.35) and the biosimilar strategy was associated with 3.06 QALYs (SD: 0.38) resulting in an incremental loss of 0.13 QALYs (95% CI: −0.16 to −0.07) (or 6.5 quality-adjusted weeks) over the 5-year time horizon (See Table 4.).
Table 4.
Probabilistic base case results
| Cost | (95% confidence interval) | Incremental cost (95% confidence interval) | |
|---|---|---|---|
| Maintain Treatment with Reference Infliximab | $96,385 | ($83,213 to $109,976) | −$46,194 (−$42,420 to −$50,455) |
| Switch to Maintenance Treatment with Biosimilar Infliximab | $50,191 | ($40,792 to $59,521) | |
| Effectiveness per patient | (95% confidence interval) | Incremental effect (95% confidence interval) | |
| Maintain Treatment with Reference Infliximab | 3.19 | (2.47 to 3.83) | −0.13 (−0.16 to −0.07) |
| Switch to Maintenance Treatment with Biosimilar Infliximab | 3.06 | (2.31 to 3.76) |
All costs in 2017 Canadian dollars.
The results of the base case probabilistic analysis indicated that switching to biosimilar infliximab was associated with incremental savings, but a small incremental reduction in QALYs over a 5-year time horizon. As shown in Figure 2, 83.67% of the iterations were less costly and less effective while 16.33% were less costly and more effective.
Figure 2.
Cost-effectiveness of biosimilar infliximab results. As shown in the figure, 83.67% of the iterations lie in the south-west quadrant (less costly and less effective) and 16.33% lie in the south-east quadrant (less costly and more effective). Those simulations that lie in the south-east quadrant imply that switching to biosimilar infliximab is a dominant strategy as it results in incremental cost-savings and an incremental gain in QALYs. The dashed line shows a decision-maker willingness to pay threshold of $50,000 which represents a maximum the decision maker may be willing to pay for one additional QALY.
Societal Perspective
Compared to the base case, costs in both groups increased and cost savings moderately decreased. When the societal perspective is taken, costs in the maintain treatment on reference infliximab group were CAD $105,063 (95% CI: $83,213 to $109,976) and the switch group costs were CAD $59, 998 (95% CI: $40,792 to $59,521) for incremental costs over the 5 years of CAD −$45,066 (95% CI: −$41,520 to −$49,046) (Supplementary Appendix).
Uncertainty Analyses
The one-way sensitivity analyses indicated that the results were sensitive to variation in variables which influenced infliximab drug cost, such as patient weight and infliximab price. When biosimilar drug price was reduced to $279.09 per 100 mg vial (72% discount from the Canadian reference price), the incremental savings increased to CAD $61,245 (95% CI: $56,624 to $66,335). In comparison when the reference infliximab price was lowered to $795.95 per 100 mg vial (20% discount from the current public Canadian list price) the cost savings were reduced to CAD $30,011 (95% CI: $27,639 to 32,653).
On the effectiveness side of the analysis, when alternative utility weights were employed that reflected a Canadian CD population, the results showed the reference infliximab group was associated with an increased 3.51 (95% CI: 1.5 to 4.95) QALYs (48). The biosimilar group was also associated with an increased 3.33 (95% CI: 1.04 to 4.95) QALYs. However, this also increased the incremental decrement in QALYs.
Finally, when alternative relapse rates that reflected the results of a meta-analysis conducted by Komaki et al. (2017) were tested, both costs and outcomes of the model differed (11,49). Costs associated with the biosimilar increased to CAD $67,502 (95% CI: $50,158 to $83,679) which reduced the incremental costs to CAD −$28,924 (95% CI: −$26,280 to −$33,213). Importantly, with this lower relapse rate, the outcomes for the biosimilar group increased to 3.40 QALYs (95% CI: 2.53 to 4.13). When the relapse rates derived by Komaki et al. (2017) were employed biosimilar infliximab was a dominant strategy associated with incremental savings and an incremental gain in effectiveness.
Structural Uncertainty Analyses
A 1-year time horizon was tested, as this was the length of time of the NOR-SWITCH study. The results demonstrated that the increment in costs was reduced to CAD −$13,106 (95% CI: −$13,481 to −$12,778), however, the difference in incremental effect was also smaller at −0.01 (95% CI: −0.01 to −0.01). A longer time horizon of 10 years was also tested, however, certain assumptions had to be extended for the 10-year period which increased uncertainty. The increment in costs increased to CAD −$67,212 (95% CI: −$55,688 to −$81,392) as did the incremental loss in QALYs to −0.23 (95% CI: −0.37 to −0.04). The discount rate did not substantially impact the results and was not presented. A summary of all sensitivity analyses can be found in Table 5.
Table 5.
Sensitivity analyses results
| Parameter sensitivity analysis | Treatment group | Cost | Incremental cost (95% confidence interval) | Effectiveness (95% confidence interval) | Incremental effect (95% confidence interval) |
|---|---|---|---|---|---|
| Base Case | |||||
| Maintain | $96,385 ($83,213 to $109,976) | −$46,194 (−$42,420 to −$50,455) | 3.19 (2.47 to 3.83) | −0.13 (−0.16 to −0.07) | |
| Switch | $50,191 ($40,792 to $59,521) | 3.0607 (2.31 to 3.76) | |||
| Reference Infliximab Price | |||||
| 20% Price Reduction in Reference Infliximab Price | Maintain | $80,203 ($68,432 to $92,173) | −$30,011 (−$27,639 to −$32,653) | 3.19 (2.47 to 3.83) | −0.13 (−0.16 to −0.07) |
| Switch | $50,191 ($40,792 to $59,521) | 3.06 (2.31 to 3.76) | |||
| Biosimilar Price | |||||
| Biosimilar Price set at 72% Discount from Reference Infliximab Price | Maintain | $96,385 ($83,213 to $109,976) | −$61,245 (−$56,624 to −$66,335) | 3.19 (2.47 to 3.83) | −0.13 (−0.1604 to −0.0729) |
| Switch | $35,140 ($26,588 to $43,641) | 3.06 (2.31 to 3.76) | |||
| Utility | |||||
| Gregor et al. (1997) Utilities | Maintain | $96,385 ($83,213 to $109,976) | −$46,194 (−$42,420 to −$50,455) | 3.50 (1.49 to 4.95) | −0.16 (−0.24 −0.01) |
| Switch | $50,191 ($40,792 to $59,521) | 3.34 (1.25 to 5.00) | |||
| Biosimilar Relapse Rate | |||||
| Komaki et al. (2017) Relapse Rates | Maintain | $96,426 ($83,370 to $109,959) | −$28,924 (−$26,280 to −$33,213) | 3.19 (2.47 to 3.83) | 0.21 (0.06 to 0.30) |
| Switch | $67,502 ($50,158 to $83,679) | 3.40 (2.53 to 4.13) | |||
| Time Horizon | |||||
| 1 Year | Maintain | $32,334 ($29,403 to $35,264) | −$13,106 (−$13,481 to −$12,778) | 0.84 (0.64 to 1.00) | −0.13 (−0.16 to −0.07) |
| Switch | $19,228 ($15,922 to $22,486) | 0.83 (0.63 to 0.99) | |||
| Time Horizon | |||||
| 10 Years | Maintain | $132,420 ($107,873 to $159,986) | −$67,212 (−$55,688 to −$81,392) | 5.72 (4.27–7.07) | −0.23 (−0.37 to −0.04) |
| Switch | $65,207 ($52,185 to $78,594) | 5.49 (3.91–7.04) |
Threshold Analysis
The results of the analysis showed that if the probability of relapsing from a clinical remission state after being switched to biosimilar infliximab is less than 0.0327 per 8-week cycle then the expected QALYs for the biosimilar treatment group will be greater than that of the reference infliximab group. In the base case, the rate of relapse is 0.05461; therefore, a 40% reduction in relapse rate per 8-week cycle would be required.
Discussion
Biosimilars are a relatively new therapeutic option in CD for stakeholders in Canada and they have identified a need for further evidence—particularly with regards to switching from a reference biologic to a biosimilar product (50,51). CADTH emphasized this in their report and identified that existing evidence does not adequately address concerns regarding the cost-effectiveness of switching (50).
Results of the analysis indicated that approximately 84% of the time, biosimilars were less costly and less effective. Biosimilar infliximab was associated with incremental savings over a 5-year time horizon. This is an important finding with regards to sustainability, as patients with CD require lifetime treatment. However, decision makers must also account for an incremental loss of effectiveness. The analysis indicated that the average incremental loss over the 5-year time horizon was approximately 6.5 quality-adjusted life-weeks. The results of the uncertainty analyses suggested that the conclusions of the model were sensitive to: time horizon, relapse rate from the switch group and prices of infliximab, however, the results are likely robust in demonstrating that the intervention is cost-effective.
It is ultimately dependent on the willingness of decision makers to fund interventions in the south-west quadrant—which requires weighing a loss in effectiveness against cost savings. Increasingly, as health care systems seek to rationalize services in the face of growing budget constraints, the budget allocation decision before decision makers is what loss of effectiveness is acceptable, rather than what increased cost.
Payers and decision makers that move forward with funding switching to a biosimilar have several policy options available to them. Less aggressive strategies include mandating the development of switching evidence in order to support switching designations or an incentive-based scheme (52). Green Shield Canada for example, implemented a successful incentive-based biosimilar transition pilot for arthritis indications and have extended the program (53). More aggressive strategies could include tendering for a molecule where the winning bidder supplies the product for a given time period, such as in Norway (54). Another policy option is to mandate switching whereby all patients on the reference are switched to treatment with the biosimilar, save for exceptional cases. The public drug plan in British Columbia implemented a mandated switch with their Biosimilar Initiative in 2019, which involves switching patients from reference infliximab to biosimilar infliximab and this includes patients with gastrointestinal indications such as CD (55).
If drug plan decision makers are willing to accept a minimal reduction in benefit and move forward with policies which drive switching, substantial savings could be generated for Canadian public drug plans as suggested by this analysis. If the savings are reinvested and result in more QALYs gained than if those same funds were utilized to fund less effective interventions, then there may be additional value in switching for society as whole.
The findings of this analysis were similar to those derived by a study conducted by Husereau et al. (2018), which found 10-year costs associated with reference infliximab and biosimilar infliximab were CDN $168,210 and $120,753, respectively (52). Husereau et al. (2018) found that reference infliximab was associated with 6.02 QALYs while biosimilar infliximab was associated with 5.76 QALYs, an incremental loss of 0.27 (52). The major differences between the present analysis and that study are threefold: Husereau et al. utilized a 10-year time horizon, accounted for dose escalation, and relapse rates after year 1 of the evaluation were based on a network meta-analysis and calibration exercise. Despite these differences, Husereau et al. similarly found that switching to biosimilar infliximab was associated with an incremental reduction in costs and with an incremental loss in benefits.
There were strengths and limitations associated with the analysis. The model framework was built in consultation with Canadian experts in CD and in keeping with economic evaluations of infliximab (12,56). This framework accounted for differences between clinical remission and response states and also modeled subsequent treatment options post-relapse. However, as with any disease state, there are limitations to modelling a complex disease and treatment pathway. For example, guidelines recommend that the physician consider dose escalation as well as a switch to a second-line anti-TNF therapy (17). However, this analysis only modelled a switch to second-line treatment after relapsing on treatment with infliximab.
Therefore, this model does not account for the additional costs or benefits from re-establishing remission or response associated with patients who would otherwise receive dose escalation. A cost-effectiveness analysis conduction by Kaplan et al. comparing dose escalation and initiating adalimumab for loss of response in CD over a 1-year time horizon and found that infliximab dose escalation yielded more QALY (0.79) compared with the adalimumab strategy (0.76) but the cost was considerable (57). By not including the possibility of dose escalation on reference infliximab the cost-effectiveness of biosimilar infliximab may have been underestimated.
There were also strengths and limitations associated with the primary data sources that were utilized to inform the model. NOR-SWITCH was not powered to show noninferiority in individual diseases. Therefore, while CD-specific outcomes were utilized to inform the model, NOR-SWITCH was not powered to test whether there was non-inferiority between the reference and biosimilar infliximab treatment groups within individual immune-mediated diseases. The non-inferiority nature of the trial and the 15% margin, particularly as it relates to the CD group, has been criticized (58). In a non-inferiority study, the analysis attempts to prove that a new treatment is not clinically inferior to standard therapy, and therefore, the researcher must determine what is clinically meaningless in order to set the margin (58,59). Canadian gastroenterologists have expressed concern with the 15% margin, stating that a narrower margin of 7.5% would be preferred (58). Finally, the absence of other randomized controlled trials also meant that validation exercises through the use of calibration could not be conducted.
While the data had its weaknesses, mainly due to the lack of available literature, NOR-SWITCH remained the best available evidence to inform relapse rates for an economic model of switching to biosimilar infliximab. Furthermore, employing relapse rates for switching to biosimilar infliximab from the NOR-SWITCH trial was likely a conservative assumption. The sensitivity analysis that derived rates from a meta-analysis that demonstrated lower relapse rates after switching to biosimilar infliximab, suggested that biosimilar infliximab was a dominant strategy as the outcomes for the switch group improved (49).
In conclusion, biosimilars represent an important addition to the treatment options available to adult patients with CD. This chronic disease can have serious impacts on patients’ quality of life and expanding access to high-value treatments is integral to improve patient outcomes. This cost-utility analysis provides valuable information to decision makers regarding the cost-effectiveness of a switch to biosimilar infliximab and emphasizes that making reimbursement decisions is challenging, and therefore, further research will be important to develop policies which meet the needs of society.
Funding
This work was generously supported by the Hospital for Sick Children’s Research Training Competition (Restracomp) Award, the Ontario Graduate Scholarship Program, the Institute of Health Policy, Management and Evaluation and the CIHR Travel Award—Institute Community Support.
Supplementary Material
Acknowledgments
We would like to acknowledge Don Husereau who graciously provided information regarding the network meta-analysis employed in the article “Policy Options for Infliximab Biosimilars in Inflammatory Bowel Disease Given Emerging Evidence for Switching” as well as other resources regarding the clinical effectiveness of biologics.
Author Contributions: A.H. was responsible for (a) the conception and design of the study, acquisition of data, analysis and interpretation of data, (b) drafting the article and revising it critically for important intellectual content, and (c) final approval of the version submitted. J.M. was responsible for (a) the conception and design of the study, interpretation of data, (b) revising the article critically for important intellectual content, and (c) final approval of the version submitted. M.M. was responsible for (a) the conception and design of the study, interpretation of data, (b) revising the article critically for important intellectual content, and (c) final approval of the version submitted. W.U. was responsible for (a) the conception and design of the study, interpretation of data, (b) revising the article critically for important intellectual content, and (c) final approval of the version submitted.
Institution where the research was performed: Hospital for Sick Children Research Institute, Ontario, Canada
Conflict of Interest
The authors have no conflicts of interest to disclose at this time. No ethical approvals were required for this work.
References
- 1. Lybecker KM. The Biologics Revolution in the Production of Drugs. Fraser Institute, July 2016. <https://www.fraserinstitute.org/sites/default/files/biologics-revolution-in-the-production-of-drugs.pdf> (Accessed July 2017). [Google Scholar]
- 2. National Prescription Drug Utilization Information System. Potential Savings from Biosimilars in Canada. <http://www.pmprb-cepmb.gc.ca/view.asp?ccid=1304> (Accessed February 2018).
- 3. IMS Brogan. IMS Brogan Private Drug Plan Drug Cost Forecast Commissioned by Rx&D. November, 2013. <http://innovativemedicines.ca/wp-content/uploads/2015/05/20131125_Report_IMS_Brogan_PDP_Forecast_EN_Final.pdf> (Accessed July 2017). [Google Scholar]
- 4. Canadian Institute for Health Information. Prescribed Drug Spending in Canada, 2017, Ottawa, Ontario: A Focus on Public Drug Programs, 2017. <https://secure.cihi.ca/free_products/pdex2017-report-en.pdf> (Accessed July 2017). [Google Scholar]
- 5. IQVIA Institute for Human Data Science. Advancing Biosimilar Sustainability in Europe: A Multi-Stakeholder Assessment. Parsippany, NJ: IQVIA Institute for Human Data Science, September 4, 2018. [Google Scholar]
- 6. Mulcahy AW, Hlavka JP, Case SR. Biosimilar cost savings in the United States: Initial experience and future potential. Rand Health Q 2018;7(4):3. [PMC free article] [PubMed] [Google Scholar]
- 7. Crohn’s and Colitis Foundation of Canada. The impact of inflammatory bowel disease in Canada 2012 Final Report and Recommendations. 2012. <http://crohnsandcolitis.ca/Crohns_and_Colitis/documents/reports/ccfc-ibd-impact-report-2012.pdf> (Accessed June 2017).
- 8. Targan SR, Hanauer SB, van Deventer SJ, et al. . A short-term study of chimeric monoclonal antibody cA2 to tumor necrosis factor alpha for Crohn’s disease. Crohn’s Disease cA2 Study Group. N Engl J Med 1997;337(15):1029–35. [DOI] [PubMed] [Google Scholar]
- 9. Hanauer SB, Feagan BG, Lichtenstein GR, et al. ; ACCENT I Study Group Maintenance infliximab for Crohn’s disease: The ACCENT I randomised trial. Lancet 2002;359(9317):1541–9. [DOI] [PubMed] [Google Scholar]
- 10. Health Canada. Fact Sheet Subsequent Entry Biologics in Canada August 2017. <http://www.hc-sc.gc.ca/dhp-mps/brgtherap/activit/fs-fi/fs-fi_seb-pbu_07-2006-eng.php> (Accessed September 2017).
- 11. Jørgensen KK, Olsen IC, Goll GL, et al. ; NOR-SWITCH study group Switching from originator infliximab to biosimilar CT-P13 compared with maintained treatment with originator infliximab (NOR-SWITCH): A 52-week, randomised, double-blind, non-inferiority trial. Lancet 2017;389(10086):2304–16. [DOI] [PubMed] [Google Scholar]
- 12. Blackhouse G, Assasi N, Xie F, et al. . Canadian cost-utility analysis of initiation and maintenance treatment with anti-TNF-α drugs for refractory Crohn’s disease. J Crohns Colitis 2012;6(1):77–85. [DOI] [PubMed] [Google Scholar]
- 13. Leslie WD, Miller N, Rogala L, et al. . Body mass and composition affect bone density in recently diagnosed inflammatory bowel disease: The Manitoba IBD Cohort Study. Inflamm Bowel Dis 2009;15(1):39–46. [DOI] [PubMed] [Google Scholar]
- 14. TreeAge Pro 2018, R2. Williamstown, MA, 2018. <http://www.treeage.com>. [Google Scholar]
- 15. Janssen Inc. Product Monograph - REMICADE ® Powder for Solution, Sterile, Lyophilized, 100 mg/vial Biological Response Modifier. Toronto, Ontario, Canada: Janssen Inc., 2016. [Google Scholar]
- 16. Celltrion Healthcare Co Ltd. Product Monograph - INFLECTRA Powder for Solution, Sterile, Lyophilized, 100 mg/vial. Yeonsu-gu, Incheon, Republic of Korea: Celltrion Healthcare Co. Ltd., 2016. [Google Scholar]
- 17. Sadowski DC, Bernstein CN, Bitton A, et al. ; CAG Crohn’s Consensus Group Canadian Association of Gastroenterology Clinical Practice Guidelines: The use of tumour necrosis factor-alpha antagonist therapy in Crohn’s disease. Can J Gastroenterol 2009;23(3):185–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Canadian Agency for Drugs and Technologies in Health (CADTH). CADTH Methods and Guidelines - Guidelines for the Economic Evaluation of Health Technologies, Canada. 4th edn Ottawa, Ontario: Canadian Agency for Drugs and Technologies in Health, March, 2017. [Google Scholar]
- 19. Sandborn WJ, Rutgeerts P, Enns R, et al. . Adalimumab induction therapy for Crohn disease previously treated with infliximab: A randomized trial. Ann Intern Med 2007;146(12):829–38. [DOI] [PubMed] [Google Scholar]
- 20. Colombel JF, Sandborn WJ, Rutgeerts P, et al. . Adalimumab for maintenance of clinical response and remission in patients with Crohn’s disease: The CHARM trial. Gastroenterology 2007;132(1):52–65. [DOI] [PubMed] [Google Scholar]
- 21. Silverstein MD, Loftus EV, Sandborn WJ, et al. . Clinical course and costs of care for Crohn’s disease: Markov model analysis of a population-based cohort. Gastroenterology 1999;117(1):49–57. [DOI] [PubMed] [Google Scholar]
- 22. Onali S, Calabrese E, Petruzziello C, et al. . Post-operative recurrence of Crohn’s disease: A prospective study at 5 years. Dig Liver Dis 2016;48(5):489–94. [DOI] [PubMed] [Google Scholar]
- 23. Bitton A, Vutcovici M, Sewitch M, et al. . Mortality trends in Crohn’s disease and ulcerative colitis: A population-based study in Québec, Canada. Inflamm Bowel Dis 2016;22(2):416–23. [DOI] [PubMed] [Google Scholar]
- 24. Statistics Canada, Life tables, Canada, Provinces and Territories (2011 to 2013, no. 1). 2017. <https://www150.statcan.gc.ca/n1/en/catalogue/84-537-X> (Accessed September 2017). [Google Scholar]
- 25. Singh S, Al-Darmaki A, Frolkis AD, et al. . Postoperative mortality among patients with inflammatory bowel diseases: A systematic review and meta-analysis of population-based studies. Gastroenterology 2015;149(4):928–37. [DOI] [PubMed] [Google Scholar]
- 26. Greenberg D, Schwartz D, Vardi H, et al. ; Israeli IBD Research Nucleus [IIRN] Health-related utility weights in a cohort of real-world Crohn’s disease patients. J Crohns Colitis 2015;9(12):1138–45. [DOI] [PubMed] [Google Scholar]
- 27. Statistics Canada. Consumer Price Index, Health and Personal Care, by province (Canada). <http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/econ161a-eng.htm> (Accessed March 29, 2018).
- 28. British Columbia Ministry of Health. BC PharmaCare Formulary Search. <https://pharmacareformularysearch.gov.bc.ca/> (Accessed April 2018).
- 29. Alberta Health. Alberta Drug Benefit List; April 1, 2018. <https://www.ab.bluecross.ca/dbl/publications.html> (Accessed April 2018).
- 30. Government of Saskatchewan Drug Plan and Extended Benefits Branch. Saskatchewan Online Formulary Database. <http://formulary.drugplan.ehealthsask.ca/> (Accessed April 2018).
- 31. Ontario Ministry of Health and Long Term Care. Ontario Drug Benefit Formulary. <https://www.formulary.health.gov.on.ca/formulary/> (Accessed April 2018).
- 32. Regie de l’assurance maladie. Quebec List of Medications; April 18, 2018. <http://www.ramq.gouv.qc.ca/en/publications/citizens/legal-publications/Pages/list-medications.aspx> (Accessed April 2018).
- 33. Nova Scotia Pharmacare. Nova Scotia Formulary April 2018. <https://novascotia.ca/dhw/pharmacare/formulary.asp> (Accessed April 2018).
- 34. Government of Newfoundland and Labrador. Search the NLPDP Drug Product Database. <http://www.health.gov.nl.ca/health/prescription/newformulary.asp> (Accessed April 2018).
- 35. Marshall J, Blackhouse G, Goeree R, et al. . Infliximab for the Treatment of Crohn’s Disease: A Systematic Review and Cost-Utility Analysis. Ottawa: Canadian Coordinating Office for Health Technology Assessment; March 2002. [Google Scholar]
- 36. Ontario Ministry of Health and Long Term Care. Schedule of Benefits Physician Services Under the Health Insurance Act. <http://www.health.gov.on.ca/en/pro/programs/ohip/sob/physserv/sob_master20151221.pdf> (Accessed May 2018).
- 37. British Columbia Ministry of Health. Medical Services Commission Payment Schedule. December 31, 2017. <https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/msp/physicians/payment-schedules/msc-payment-schedule> (Accessed May 2018).
- 38. Government of Alberta. Medical Procedure List as of 01 April 2017 <https://open.alberta.ca/publications/somb-2017-04-01> (Accessed May 2018).
- 39. Government of Saskatchewan. Payment Schedule For Insured Services Provided by a Physician; April 1, 2018. <https://www.ehealthsask.ca/services/resources/Resources/physician-payment-schedule-apr-18.pdf> (Accessed May 2018).
- 40. Manitoba Ministry of Health. MANITOBA PHYSICIAN’S MANUAL April 1, 2018. <https://www.gov.mb.ca/health/documents/physmanual.pdf> (Accessed May 2018).
- 41. Nova Scotia Medical Services Insurance. Physician’s Manual 2014. <https://msi.medavie.bluecross.ca/physicians-manual/> (Accessed May 2018).
- 42. Government of New Brunswick. New Brunswick Physicians’ Manual; May 18, 2017. <https://www2.gnb.ca/content/dam/gnb/Departments/h s/pdf/en/Physicians/new_brunswick_physicians_manual.pdf> (Accessed May 2018).
- 43. Government of Prince Edward Island. Master Agreement between the Medical Society of Prince Edward Island and the Government of Prince Edward Island and Health PEI April 1, 2015 - March 31, 2019; 2015. <http://www.gov.pe.ca/photos/original/hpei_master_agr.pdf> (Accessed May 2018).
- 44. Newfoundland and Labrador Department of Health and Community Services. Medical Payment Schedule June 1, 2013; 2013. <https://www.health.gov.nl.ca/health/mcp/providers/Full_MCP_Payment_Schedule-03_13_14.pdf> (Accessed May 2018).
- 45. Régie de l’assurance de maladie de Québec. Manuel Des Pharmaciens; July 2017. <http://www.ramq.gouv.qc.ca/fr/professionnels/pharmaciens/manuels/Pages/manuel-pharmaciens.aspx> (Accessed May 2018).
- 46. Bashir N. The Economic Evaluation of Early Intervention with Anti-TNF-α Treatments in Pediatric Crohn’s Disease. University of Toronto, 2018. [Google Scholar]
- 47. Statistics Canada. Average hourly wages of employees by selected characteristics and occupation, unadjusted data, by province (monthly) <http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/labr69a-eng.htm> (Accessed May 2018).
- 48. Gregor JC, McDonald JW, Klar N, et al. . An evaluation of utility measurement in Crohn’s disease. Inflamm Bowel Dis 1997;3(4):265–76. [PubMed] [Google Scholar]
- 49. Komaki Y, Yamada A, Komaki F, et al. . Systematic review with meta-analysis: The efficacy and safety of CT-P13, a biosimilar of anti-tumour necrosis factor-α agent (infliximab), in inflammatory bowel diseases. Aliment Pharmacol Ther 2017;45(8):1043–57. [DOI] [PubMed] [Google Scholar]
- 50. Canadian Agency for Drugs and Technologies in Health. Rapid Response Report: Switching from Innovator to Biosimilar (Subsequent Entry) Infliximab: An Updated Review of the Clinical Effectiveness, Cost-Effectiveness and Guidelines; Ottawa, Ontario: Canadian Agency for Drugs and Technologies in Health, January 18, 2017. [PubMed] [Google Scholar]
- 51. Institute of Health Economics. Towards an Alberta approach for biosimilar reimbursement - Summary report of the IHE Biosimilars Forum; Edmonton, Alberta, Canada: Institute of Health Economics, October 6, 2016. [Google Scholar]
- 52. Husereau D, Feagan B, Selya-Hammer C. Policy options for infliximab biosimilars in inflammatory bowel disease given emerging evidence for switching. Appl Health Econ Health Policy 2018;16(3):279–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Green Shield Canada. GSC’s Biosimilar Transition Program Completes Successful Pilot <https://www.greenshield.ca/en-ca/news/post/gsc-s-biosimilar-transition-program-completes-a-successful-pilot> (Accessed December 2018).
- 54. Mack A. Norway, biosimilars in different funding systems. What works? Generics and Biosimilar Initiative J, 2015;4(2):90–92. [Google Scholar]
- 55. BC Pharmacare. BC Pharmacare Newsletter Edition 19-007 <https://www2.gov.bc.ca/assets/gov/health/health-drug-coverage/pharmacare/newsletters/news19-007.pdf> (Accessed September 2019).
- 56. Marshall JK, Blackhouse G, Goeree R, Brazier N, Irvine EJ, O’Brien BJ.. Clinical and Economic Assessment: Infliximab for the Treatment of Crohn’s Disease. Ottawa: Canadian Coordinating Office for Health Technology Assessment, 2002. [Google Scholar]
- 57. Kaplan GG, Hur C, Korzenik J, et al. . Infliximab dose escalation vs. initiation of adalimumab for loss of response in Crohn’s disease: A cost-effectiveness analysis. Aliment Pharmacol Ther 2007;26(11–12):1509–20. [DOI] [PubMed] [Google Scholar]
- 58. Community Academic Research Education (CARE). CARE perspectives: NOR-SWITCH trial a discussion between Dr. John Marshall and Dr. Brian Feagan 2017. [Google Scholar]
- 59. Hahn S Understanding noninferiority trials. Korean J Pediatr 2012;55(11):403–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.