Abstract
Background
A systemic coagulation dysfunction has been associated with COVID-19. In this case report, we describe a COVID-19-positive patient with multisite arterial thrombosis, presenting with acute limb ischaemia and concomitant ST-elevation myocardial infarction and oligo-symptomatic lung disease.
Case summary
An 83-year-old lady with history of hypertension and chronic kidney disease presented to the Emergency Department with acute-onset left leg pain, pulselessness, and partial loss of motor function. Acute limb ischaemia was diagnosed. At the same time, a routine ECG showed ST-segment elevation, diagnostic for inferior myocardial infarction. On admission, a nasopharyngeal swab was performed to assess the presence of SARS-CoV-2, as per hospital protocol during the current COVID-19 pandemic. A total-body CT angiography was performed to investigate the cause of acute limb ischaemia and to rule out aortic dissection; the examination showed a total occlusion of the left common iliac artery and a non-obstructive thrombosis of a subsegmental pulmonary artery branch in the right basal lobe. Lung CT scan confirmed a typical pattern of interstitial COVID-19 pneumonia. Coronary angiography showed a thrombotic occlusion of the proximal segment of the right coronary artery. Percutaneous coronary intervention was performed, with manual thrombectomy, followed by deployment of two stents. The patient was subsequently transferred to the operating room, where a Fogarty thrombectomy was performed. The patient was then admitted to the COVID area of our hospital. Seven hours later, the swab returned positive for COVID-19.
Discussion
COVID-19 can have an atypical presentation with thrombosis at multiple sites.
Keywords: COVID-19, Multisite thrombosis, Myocardial infarction, Case report
Learning points
COVID-19 infection can include multiorgan involvement with different clinical expressions.
Alteration of the coagulation cascade in COVID-19 has been already described and may be responsible for some of the manifestations of the disease.
Primary Specialties involved other than cardiology
Vascular surgery, Internal Medicine, Radiology
Introduction
Coronavirus disease 2019 (COVID-19) has emerged as a dramatic health emergency all over the world. Even though the most frequent expression is pulmonary infection, evidence of the involvement of other organs has been described.1,2
Recently, numerous case reports and studies also detailed concomitant coagulation disorders during COVID-19 infection. Different theories have been considered to explain this manifestation, such as the increase in the vasoconstrictor angiotensin II, the decrease in the vasodilator angiotensin, and the sepsis-induced release of cytokines.3
We report the case of a patient with COVID-19 infection with a multisite involvement due to multiple thromboses.
Timeline
| Time | Event |
|---|---|
| Emergency Room admission | Patient complained of lower limb pain, and acute left lower limb ischaemia was diagnosed. A nasopharyngeal swab for COVID-19 was performed, as per hospital protocol. Routine ECG showed inferior ST-segment elevation myocardial infarction. |
| 30 min after admission | A total-body angioCT scan was performed, showing thrombotic occlusion of the left common iliac artery, thrombosis of a branch of the pulmonary artery, and interstitial pneumonia. |
| 60 min after admission | The patient was transferred to the Cath Lab to perform primary PCI of the right coronary artery |
| 2 h after admission | The patient was transferred to the vascular surgery operating theatre to perform left iliac artery thrombectomy. |
| 4 h after admission | The patient was transferred to the COVID area of the hospital. Aspirin, clopidogrel, and enoxaparin were prescribed. The patient did not complain of dyspnoea. |
| 2 days after admission | The patient developed acute right lower limb ischaemia, with diagnosis of thrombotic occlusion of the right common iliac artery. |
| 3 days after admission | The patient died of multiorgan failure. |
Case presentation
An 83-year-old woman with a history of arterial hypertension and chronic kidney disease presented to the Emergency Room with an acute (<2 h) onset of left leg pain and numbness, and partial loss of motor function. The leg also showed pallor, pulselessness, and poikilothermia. The patient did not complain of chest pain.
A diagnosis of acute limb ischaemia was made, class IIb of the Rutherford classification. At the same time, a routine ECG showed ST-segment elevation in the inferior leads, leading to a diagnosis of inferior ST-segment elevation myocardial infarction (STEMI) (Figure 1A). Blood pressure and SpO2 were normal (130/75 mmHg, SpO2 98%). Fast echocardiography showed akinesia of the inferior and infero-lateral walls with a mild reduction of the ejection fraction (40%). A dose loading of aspirin (250 mg i.v.) was administered. The patient reported a cough over the last 2 days, but she had no fever on admission. A nasopharyngeal swab was performed to assess the presence of SARS-CoV-2, as per hospital protocol during the COVID-19 pandemic. A total-body CT angiography was performed to investigate the cause of acute limb ischaemia and rule out aortic dissection. A lung CT scan was also performed to assess potential COVID-19 pneumonia.
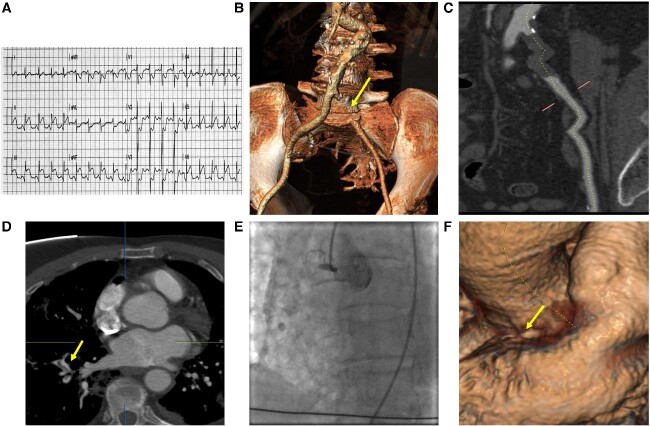
Figure 1.
Electrocardiography, CT and angiographic findings. (A) Electrocardiography showing sinus rhythm with ST-segment elevation in DII, DIII, aVL and V6 and ST-segment depression in V1-V3. (B and C) CT reconstruction of complete left common iliac occlusion. (D and E) evidence at pulmonary CT of thrombus in segmentary arteryE-F: angiographic and CT images of total thrombotic occlusion of right coronary artery.
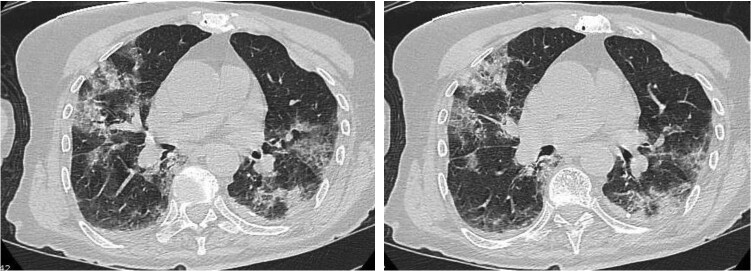
Figure 2.
CT lung findings suggestive of COVID-19 infection
A total occlusion of the left common iliac artery was diagnosed (Figure 1B and C) together with subsegmental thrombosis of a right lobe pulmonary artery branch (Figure 1D). The lung CT scan showed a typical COVID pneumonia, with multiple bilateral, mainly subpleural, ground-glass opacities (figure 2). At 2 h after admission, the patient was transferred to the Cath Lab for emergency coronary angiography. A total occlusion of the proximal right coronary artery was diagnosed (Video 1), as also shown by CT angiography, together with a critical stenosis of the mid left anterior descending artery and of the first obtuse marginal branch (Figure 1E and F; Video 2).
Percutaneous coronary intervention (PCI) was performed with i.v. cangrelor administration, manual thrombectomy, and subsequent deployment of two drug-eluting stents. The final angiography showed no reflow in the distal segment of the right coronary artery (Video3). No reflow was treated with intracoronary adenosine, without success. At the end of the procedure, the patient had good haemodynamic parameters (blood pressure was 130/80 mmHg). The patient was then transferred from the Cath Lab to the operating room to undergo Fogarty thrombectomy of the left common iliac artery. At the end of cangrelor infusion, clopidogrel 600 mg was administered and the patient was admitted to the COVID area of our hospital.
Seven hours later, the results of the nasopharyngeal swab revealed the presence of SARS-CoV-2. Low molecular weight heparin was administered according to body weight, in combination with dual antiplatelet therapy, in order to treat multiple thromboses. In the following 48 h, the clinical condition of the patient worsened, with onset of right common iliac thrombosis and impairment of cardiac function. Blood sample results of the patient during hospitalization are reported in Table 1. The patient died for multiorgan failure during the third day after admission.
Table 1.
Blood sample results
| Measure | Reference range | Admission | Day 1 | Day 2 |
|---|---|---|---|---|
| Red blood cell count, ×106/μL | 4.2–5.4 | 3.61 | 3.13 | 2.85 |
| Haemoglobin, g/dL | 11.5–16.0 | 10.6 | 9.3 | 8.5 |
| Haematocrit, % | 37–47 | 32.4 | 26.9 | 25 |
| White blood cell count, per μL | 4.0–11.0 | 15.84 | 23.36 | 26.61 |
| Lymphocyte count | ||||
| Relative, % | 20–50 | 9.2 | 5.3 | 3.0 |
| Absolute, 103/μL | 0.9–4.5 | 1.45 | 1.23 | 0.79 |
| Platelet count, 103/μL | 140–450 | 453 | 425 | 468 |
| Sodium, mEq/L | 135–145 | 143 | 141 | 140 |
| Potassium, mEq/L | 3.5–5.1 | 5.22 | 5.92 | 6.16 |
| Chloride, mEq/L | 95–110 | 104 | NA | NA |
| Calcium, mg/dL | 8.6–10.2 | 10 | NA | NA |
| Creatinine, mg/dL | 0.5–1.1 | 2.70 | 2.75 | 3.62 |
| LDH, U/L | 135–214 | NA | 1390 | 1470 |
| Myoglobin, μg/L | 25–58 | NA | 4686 | 7009 |
| C-reactive protein, mg/dL | <0.5 | 6.42 | 8.80 | 9.91 |
| Procalcitonin (PCT), ng/mL | <0.5 | 0.28 | 3.63 | NA |
| High-sensitivity troponin T, ng/mL | <14 | 109 | >10 000 | >10 000 |
| BNP, pg/mL | <100 | NA | 893 | NA |
| D-dimer, mg/L | <0.3 | NA | 1.8 | NA |
Discussion
The clinical evolution of COVID-19 is generally characterized by respiratory symptoms, including fever, cough, pharyngodynia, fatigue, and complications related to pneumonia and acute respiratory distress syndrome, as recently reported.4 However, some authors have reported atypical clinical presentations, such as cardiac or neurological involvement.1,2 Moreover, a procoagulant systemic response has been described.5 The pathogenesis of this response is probably multifactorial, and actually not well known. It is probable that the infection leads to endothelial dysfunction, with excess thrombin production and a shutdown of fibrinolysis, resulting in a hypercoagulable state.6 In addition, COVID-19 pneumonia can lead to severe hypoxia, enhancing thrombosis through increased blood viscosity and through a hypoxia-inducible transcription factor (HIF)-dependent signalling pathway.7 Recently, pathological examinations have revealed oedema, a proteinaceous exudate, focal reactive hyperplasia of pneumocytes with patchy inflammatory cellular infiltration, and multinucleated giant cells, with occlusion and microthrombosis in pulmonary small vessels of critically ill patients.8 Our patient showed a simultaneous acute arterial thrombosis at three different sites, resulting in STEMI, acute limb ischaemia, and pulmonary artery thrombosis. Although the patient had no respiratory symptoms at admission, a lung CT revealed typical COVID-19 pneumonia. The lack of referred chest pain in the presence of inferior STEMI might depend on the simultaneous presence of intense acute pain in the left leg, due to acute limb ischaemia, diverting attention from chest pain. A systemic inflammation and hypercoagulant state due to SARS-CoV-2 infection with bilateral pneumonia probably underlies the multisite artery thrombosis which occurred in our patient, even in the absence of typical respiratory symptoms. It is also probable that the onset of limb ischaemia as the first thrombotic event amplified the coagulation cascade leading to thrombosis.
Conclusion
Although COVID-19 usually involves the lungs with a respiratory distress syndrome, a systemic procoagulant state may develop, leading to atypical presentations including multisite arterial thrombosis. Prophylactic anticoagulation with low molecular weight heparin has been proposed in some countries, including Italy, but evidence of the safety and efficacy of such treatment is still lacking.
Supplementary material
Supplementary material are available at European Heart Journal Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: Patient's consent to pubblication is included in the form consens for surgical procedure that patient signed when she was admitted.
Conflict of interest: none declared.
Funding: none declared.
Lead author biography
Marco Angelillis is a Cardiology PhD specialized in interventional cardiologist. He is a resident physician in Italy. His competences are coronary and structural heart interventions and advanced imaging techniques, especially cardiac computed tomography. He also carries out clinician activities in the ICU and consultation activities.

References
- 1. Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M.. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:819–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baig AM, Khaleeq A, Ali U, Syeda H.. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host–virus interaction, and proposed neurotropic mechanisms. ACS Chem Neurosci 2020;11:995–998. [DOI] [PubMed] [Google Scholar]
- 3. Mezalek ZT, Khibri H, Ammouri W, Bouaouad M, Haidour S, Harmouche H, Maamar M, Adnaoui M.. COVID-19 associated coagulopathy and thrombotic complications. Clin Appl Thromb Hemost 2020;26:1076029620948137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, Xia J, Yu T, Zhang X, Zhang L.. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tang N, Li D, Wang X, Sun Z.. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020;18:844–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Levi M, van der Poll T.. Coagulation and sepsis. Thromb Res 2017;149:38–44. [DOI] [PubMed] [Google Scholar]
- 7. Gupta N, Zhao YY, Evans CE.. The stimulation of thrombosis by hypoxia. Thromb Res 2019;181:77–83. [DOI] [PubMed] [Google Scholar]
- 8. Tian S, Hu W, Niu L, Liu H, Xu H, Xiao SY.. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol 2020;15:700–704. [DOI] [PMC free article] [PubMed] [Google Scholar]