Abstract
Purpose
The main objectives of the study are firstly to measure the COVID–19 preventive health behaviors related among health care providers (HCPs), then to identify the determinants of such behavior using the protection motivation theory (PMT).
Patients and Methods
An online cross-sectional survey, containing closed-ended questions, was distributed among healthcare professionals including physicians, pharmacists, technicians, and nurses. It consisted of questions assessing socio-demographic and occupational characteristics, in addition to questions from the modified PMT that has been tailored for the COVID-19 pandemic through five sub-constructs: perceived severity and perceived vulnerability, response efficacy, self-efficacy, response costs, and behavioral intention.
Results
A total of 385 HCPs have participated in the study with a mean age of 40.08±8.2 years; the majority was Saudi, married, and having children. There was a significant association between intention to comply with COVID-19 preventive behavior and being females, nurses, having training in Infection prevention and control (IPC) measures, and availability of personal protective equipment (PPE) during work time (p≤0.01). Other demographic variables, working experience, the status of being in the workforce during the pandemic COVID-19 in Saudi Arabia did not have a significant effect on the intention of HCPs to comply with COVID-19 preventive behavior. The vast majority 85.7% of HCPs answered “always” regarding the behavioral intention of HCPs to comply with COVID-19 preventive behavior. There was a significant positive correlation between COVID-19 behavioral intention and other constructs of PMT model, including perceived severity (r=0.272) perceived vulnerability (r= 0.248), self-efficacy (r=0.218), response-efficacy (r=0.167), and response-cost (r=0.13). Gender, availability of PPE, and self-efficacy had a significant prediction of COVID-19 behavioral intentions (P <0.05) with a predicted increase of 0.56, 0.37, and 0.12, respectively, in the mean of the intention score. Self-efficacy was the highest significant predictor of the behavior (p=0.008).
Conclusion
Females’ gender, nurses, having training in IPC measures, and availability of PPE during work time have a significant association with intention to comply with COVID-19 preventive behavior. The present study coping appraisal particularly self-efficacy predicted the COVID-19 pandemic protection motivation and preventive behavior more than threat appraisal. Therefore, future training programs must consider the level of self-efficacy of HCPS, and increase their knowledge regarding the effectiveness of recommendation strategies to perform protective measures against the COVID-19.
Keywords: COVID-19, behavioral intention, preventive health practice, threat appraisal, coping appraisal, protection motivation theory
Introduction
Novel coronavirus disease 2019 (COVID-19) is the most recent highly contagious human respiratory infectious disease is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and has recently gained global attention after being officially announced as a causative agent of COVID −19 by the Chinese Centre for Disease Control and Prevention.1,2 The emergence of highly communicable COVID-19 globally with an exponential rate of increase creating ever-increasing morbidity and mortality coupled with its novelty and unknown nature of the virus creating global attention and has caused an outburst of health systems generating alarming death rates in many countries worldwide.3
High transmissibility and rapid dissemination of COVID-19 have created an unprecedented state of emergency worldwide in response to this, The World Health Organization (WHO) affirmed the Covid-19 as a public health emergency of international concern on the 30th of January 2020, and called for collaborative efforts of all countries to prevent the rapid spread of COVID-19.4 Then, on the 11th of March 2020, WHO has formally declared that COVID-19 is a global pandemic in response to its continued spread at an alarming rate and overcome geographical barriers achieving a remarkable proliferation and swept more than 210 countries and territories, accounting for 4,038,747 laboratory-confirmed cases and 279,468 deaths had been reported globally and attributed to COVID-19 until May 10, 2020.5
The Kingdom of Saudi Arabia (KSA) reported its COVID-19 first case on March 2, 2020. Since then, it has exponentially spread day by day.6 Then faces a sudden hike in the number of positive cases the largest number of infections reported in a single Arab country on March 29, the kingdom of Saudi Arabia had recorded 39,048 cases of the COVID-19, with a several confirmed cases are continuing to increase up till now.7 A rapidly escalating pandemic of the COVID-19 has created a massive threat to humanity that could potentially have profound and long-term impacts on public health and could have detrimental effects on psychological health, economic, social, and religious life. In response to this, governments worldwide recognize the effectiveness of applying precautionary measures to restrain the disease. It is worth mentioning that antiviral therapy is still under trial and developments and no vaccine has been approved yet.8 Therefore, non-pharmaceutical interventions and preventive measures are considered as the mainstay and are highly recommended to halt the spread of COVID-19. Consequently, countries started to implement strict control measures at different levels.
Protection of HCPs and prevention of intra-hospital transmission of infection is a priority and important aspect in pandemic response.9 COVID-19 has posed a serious occupational health risk to the Healthcare professionals (HCPs) owing to their frequent exposure to a highly transmittable pathogen in infected individuals.10
To raise preparedness regarding prevention and control of COVID-19 among HCPs, WHO has issued several guidelines and recommendations in response to the COVID-19 pandemic.11,12 It is noteworthy mentioning that even though these guidelines reduce the occupational spread of infection among HCPs; the adherence to these regulations is problematic. Adherence to such guidelines is influenced by an individual’s perceptions. In this regard, understanding the behaviors of HCPs, including the wearing of appropriate personal protective equipment (PPE), is essential in COVID-19 prevention achieving the successful implementation of such measures.
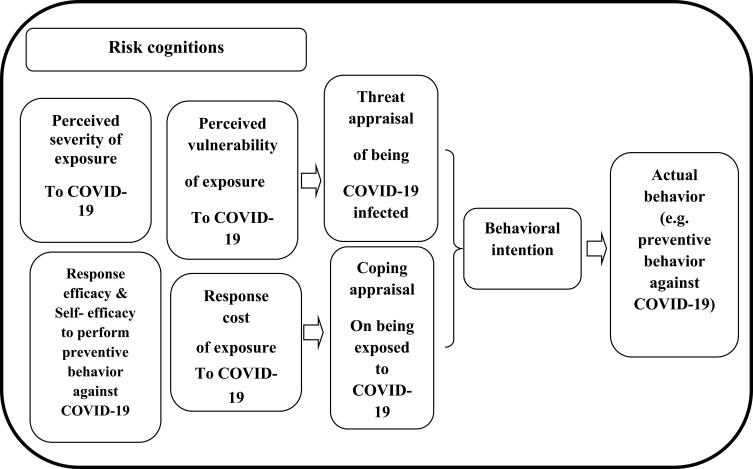
Amongst the most important health behavior theories for changing the behavior is the protection motivation theory (PMT) addresses people’s risk perception and assesses the intention to adopt protective measures which are significantly influenced by high levels of perceived risk. The theory posits that public perception of the severity and vulnerability to a certain health threat determines their risk perception about a disease. PMT was designed and modified by Rogers13,14 has been widely used in recent years as a framework for the explanation of the intention of individuals to adopt protective behaviors at the time of feeling threatened with health risk.15–17 PMT is composed of five sub-constructs, organized as two pathways as illustrated in Figure 1; threat appraisal pathway includes two sub-constructs namely perceived severity and perceived vulnerability, and the coping appraisal pathway consists of three sub-constructs: response efficacy, self-efficacy, and response costs.18 A previous Iranian study was conducted for predicting preventive behaviours of HCW towards Covid-19 and they reported that a desirable level of the COVID-19 preventive behaviours. Moreover, they found that threat, coping appraisal and the intentions significantly predict protection motivation to conduct COVID-19 preventive behaviour based on the PMT.18
Figure 1.
Conceptual framework of PMT and its five constructs.
Based on this, the current study is designed to measure the COVID–19 preventive health behaviors related to then to identify the determinants of such behavior using PMT among sampled HCPs.
Materials and Methods
Study design and setting: A cross-sectional study was conducted among healthcare providers in Saudi Arabia after the lockdown period of pandemic COVID-19 during 2 months period from May to June 2020.
Sample Size and Sampling Technique
To achieve maximal participation, convenience sampling and snowball sampling technique were used in finding the respondents, whereas participants were asked to kindly share the survey with their professional networks. The optimal sample size (385 participants) was estimated by using an online sample size calculator.19 Due to the unavailability of the proportion of the preventive behaviors towards COVID-19 pandemic among healthcare providers, we used a proportion of 50%, with a 95% confidence interval (CI), and 5% margin of error. The Inclusion criteria were HCPs (physicians, pharmacists, specialists, technicians, and nurses) currently working in the frontline and the emergency departments and agreed to participate in the study.
Research Tools
The data were collected using an online electronic questionnaire designed on Google forms and circulated via social applications on social media such as Facebook, Twitter, and WhatsApp groups. The questionnaire took approximately 7 minutes to be completed.
The questionnaire consisted of two parts:
•The first part covers socio-demographic and occupational characteristics: including age, gender, marital status, having children, residence, occupation (medical/paramedical personnel), and work experience.
•The second part includes questions from the modified protection motivation theory (PMT) that has been tailored for the COVID-19 pandemic,18 which assesses threat appraisal pathway through two sub-constructs: perceived severity (five items), perceived vulnerability (three items), and Coping appraisal pathway consists of three sub-constructs: response efficacy (seven items), self-efficacy (five items), and response costs (one item). The items were rated on a 5-point Likert scale ranging from strongly disagree= 1 to strongly agree= 5. The threat appraisal score is calculated by summing up the perceived vulnerability and severity scores with total score ranges from (8–40), while the coping appraisal score is calculated by summing up the self-efficacy and response efficacy scores then subtracting the response cost score with a total score ranges from (12–60). Finally, the Preventive behavior (behavioral intention) was assessed by four-item using a 4-point scale (1, never; 2, sometimes (2–3 times a day); 3, oftentimes (5 times a day); 4, always) with Total score ranges from (4–16).
Development, Validity, and Reliability of the Questionnaire
First; the researchers of the study collaborated to review all the related literature and generate the constructs of the PMT matching with COVID-19 pandemic preventive behaviors. Second; the draft was circulated twice among the team members of the research, and a panel of three epidemiologist experts. Third; a pilot version of the instrument was produced after making the required rewording and corrections according to the received feedback and then pre-tested on 10 HCPs to check the data collection tool’s impending problems. Finally, the reliability of the questionnaire was tested through Cronbach’s alpha test and was >0.70 for all questions.
Data Management and Analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 20.0 (SPSS, Chicago, IL, USA). Dependent variables: COVID-19 behavioral intentions and Independent variables: socio-demographic, work-related characteristics, and constructs of protection motivation theory. The assessment of the normality of data distribution was confirmed by the Kolomogroph test. Descriptive analysis was performed by mean, standard deviations for quantitative data and frequencies, percentages for qualitative data as applicable. Pearson’s correlation was used between PMT components.
Binary logistic regression analysis was done to determine the factors influencing practicing protective behaviors and the results were described by adjusted odds ratios (aOR) with 95% confidence intervals (CI). Logistic regression analysis was performed to predict potentially significant determinants of behavior. A P-value of ≤ 0.05 is considered statistically significant.
Ethical Considerations
Before collecting data, ethical approval was taken from the Institutional Review Board in Princess Nourah Bint Abdulrahman University (No #20-0238#). Consent from the participant after being informed about the purpose of the study, the confidentiality of the shared information, and anonymity of the participants. It clearly stated that their participation was voluntary, the questionnaires were strictly confidential and anonymous and each questionnaire was numerically coded. All procedures of the research were conducted according to the Declaration of Helsinki on ethical principles for medical research involving human subjects.20
Results
A total of 385 HCPs have participated in the study with a mean age of 40.08±8.2 years; 60.8% were females. The majority were Saudi, married, and having children (77.1%, 81.6%, and 77.1%, respectively). The health-care providers were 166 (43.1%) nurses, 113 (29.4%) physicians, 63 (16.4%) technicians, and 43 (11.2%) pharmacists. Seventy-nine percent of HCPs were in the workforce during the COVID-19 pandemic in KSA. More than half (61.8%) of HCPs were working in primary health-care center followed by (11.9%) working in the surveillance team, and 179 (46.5%) have working experience from (11–20) years.
There was a significant association between intention to comply with COVID-19 preventive behavior and being females, nurses, having training in IPC measures, and availability of PPEs during work time (p≤0.01). Other demographic variables, working experience, the status of being in the workforce during the pandemic COVID-19 in KSA have not significant effect on the intention of HCPs to comply with COVID-19 preventive behavior as shown in Table 1.
Table 1.
Socio-Demographic, Work-Related Characteristics of the Sampled HCPs and Their Intention to Comply with COVID-19 Preventive Behavior (n=385)
| Characteristics | Responses | Total No (%) |
Intension of HCPs to Comply with COVID-19 Preventive Behavior | X2 Test | P value | |
|---|---|---|---|---|---|---|
| Do not Intend No (%) |
Intend No (%) |
|||||
| Age groups(y) | ≤ 35 | 112(29.1) | 45(31.5) | 67(27.7) | 0.63 | 0.73 |
| 35–44 | 146(37.9) | 52(36.4) | 94(38.8) | |||
| ≥45 | 127(33.0) | 46(32.2) | 81(33.5) | |||
| X ±SD | 40.08±8.2 | |||||
| Gender | Male | 151(39.2) | 68(47.6) | 83(34.3) | 6.63 | 0.01* |
| Female | 234(60.8) | 75(52.4) | 159(65.7) | |||
| Marital state | Not Married | 71(18.4) | 30(21.0) | 41(16.9) | 0.97 | 0.32 |
| Married | 314(81.6) | 113(79.0) | 201(83.1) | |||
| Having children | No | 88(22.9) | 37(25.9) | 51(21.1) | 1.17 | 0.28 |
| Yes | 297(77.1) | 106(74.1) | 191(78.9) | |||
| Nationality | Non-Saudi | 88(22.9) | 34(23.8) | 54(22.3) | 0.11 | 0.77 |
| Saudi | 297(77.1) | 109(76.2) | 188(77.7) | |||
| Profession | Physician | 113(29.4) | 48(33.6) | 65(26.9) | 19.23 | <0.0001* |
| Pharmacist | 43(11.2) | 23(16.1) | 20(8.3) | |||
| Nurse | 166(43.1) | 42(29.4) | 124(51.2) | |||
| Technician | 63(16.4) | 30(21.0) | 33(13.6) | |||
| Being on workforce during the pandemic COVID-19 in KSA | No | 81(21.0) | 24(16.8) | 57(23.6) | 2.48 | 0.12 |
| Yes | 304(79.0) | 119(83.2) | 185(76.4) | |||
| Work sector | Primary healthcare center | 238(61.8) | 89(62.2) | 149(61.6) | 6.99 | 0.14 |
| General public hospitals | 39(10.1) | 15(10.5) | 24(9.9) | |||
| Private hospital/center | 33(8.6) | 6(4.2) | 27(11.2) | |||
| Health Quarantine | 29(7.5) | 14(9.8) | 15(6.2) | |||
| Surveillance team | 46(11.9) | 19(13.3) | 27(11.2) | |||
| Working hours/day | ≤ 8 | 286(74.3) | 99(69.2) | 187(77.3) | 3.04 | 0.08 |
| > 8 | 99(25.7) | 44(30.8) | 55(22.7) | |||
| Working experience(y) | ≤10 | 95(24.7) | 35(24.5) | 60(24.8) | 0.35 | 0.84 |
| 11–20 | 179(46.5) | 69(48.3) | 110(45.5) | |||
| > 20 | 111(28.8) | 39(27.3) | 72(29.8) | |||
| Level of training in IPC measures | Basic | 187(48.6) | 82(57.3) | 105(43.4) | 7.59 | 0.02* |
| Intermediate | 109(28.3) | 31(21.7) | 78(32.2) | |||
| Advanced | 89(23.1) | 30(21.0) | 59(24.4) | |||
| PPEs are available during work time | Sometimes | 96(24.9) | 38(26.6) | 58(24.0) | 13.6 | 0.001* |
| Often | 135(35.1) | 64(44.8) | 71(29.3) | |||
| Always | 154(40.0) | 41(28.7) | 113(46.7) | |||
| COVID-19 Infected | No | 329(85.5) | 120(83.9) | 209(86.4) | 0.43 | 0.51 |
| Yes | 56(14.5) | 23(16.1) | 33(13.6) | |||
| Total | 385(100.0) | 143(37.1) | 242(62.9) | |||
Note: *P ≤ 0.05 is significance.
Abbreviations: IPC, infection prevention and control; PPE, personal protective equipment; HCPs, health care providers.
Results in Table 2 indicated that the modified PMT that has been tailored for the COVID-19 pandemic (perceived severity, perceived vulnerability, self-efficacy, response-efficacy, and behavioral intention) has a reliability coefficient test (Cronbach’s alpha) > 0.70 for all questions.
Table 2.
Descriptive Statistics and Cronbach Alpha for Protection Motivation Theory Subscales
| Items | Min - Max | X±SD | Cronbach Alpha | |
|---|---|---|---|---|
| Perceived severity | 5 | 5–25 | 18.62±3.6 | 0.78 |
| Perceived vulnerability | 3 | 3–15 | 12.12±2.35 | 0.76 |
| Self-efficacy | 5 | 5–25 | 19.5±3.2 | 0.72 |
| Response-efficacy | 7 | 7–35 | 30.1±4.6 | 0.73 |
| Behavioral intension | 4 | 4–16 | 14.4±2.2 | 0.75 |
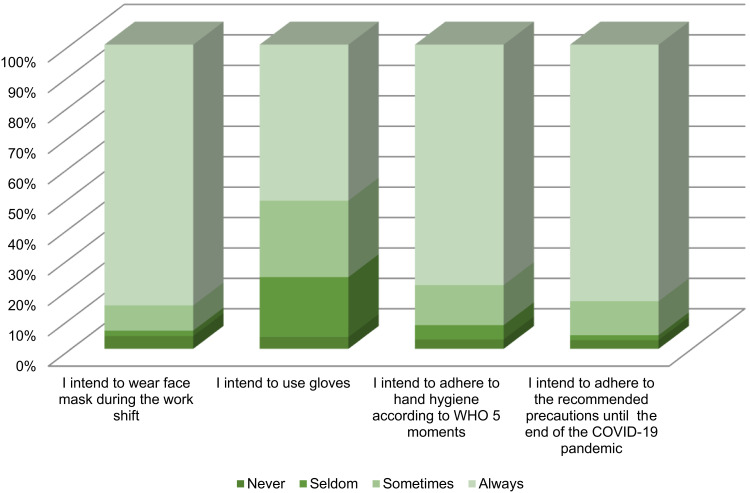
As regards, the behavioral intention of HCPs to comply with COVID-19 preventive behavior, Figure 2 shows that a vast majority (range from 51.2% to 85.7%) of HCPs answered “always” for all the behavioral intention questions.
Figure 2.
Behavioral intention of respondent HCPs to comply with COVID-19 preventive behavior.
Table 3 shows that there was a strong significant intention (p≤0.001) of HCPs to comply with COVID-19 preventive behavior concerning coping appraisal scale; self-efficacy, and response-efficacy subscales of PMT compared to the threat appraisal; perceived severity, and perceived vulnerability.
Table 3.
Subscales of PMT Among HCPs and Their COVID-19 Behavioral Intentions (n=385)
| Characteristics | Intention of HCPs to Comply with COVID-19 Preventive Behavior | t-test | P value | |
|---|---|---|---|---|
| Do not Intend | Intend | |||
| Threat appraisal | 30.04±6.3 | 31.15±4.99 | −1.92 | 0.06 |
|
18.2±4.4 | 18.9±3.49 | −1.77 | 0.078 |
|
11.9±2.54 | 12.3±2.22 | −1.61 | 0.108 |
| Coping appraisal | 44.6±7.41 | 47.57±6.43 | −4.09 | <0.001* |
|
18.6±3.3 | 20.2±3.07 | −4.59 | <0.001* |
|
29.13±5.03 | 30.71±4.26 | −3.28 | 0.001* |
|
3.2±1.07 | 3.3±1.07 | −.75 | 0.46 |
Note: *P ≤ 0.05 is significance.
Abbreviation: HCPs, health care providers.
There was a significant positive correlation between COVID-19 behavioral intention and other constructs of PMT model, including: perceived severity (r=0.272) perceived vulnerability (r= 0.248), self-efficacy (r=0.218), response-efficacy (r=0.167), and response-cost (r=0.13) as demonstrated in Table 4.
Table 4.
Correlation Between COVID-19 Behavioral Intention, and Constructs of Protection Motivation Theory Among HCPs
| Correlation Variables | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| 1. Behavioral intension | 1 | |||||
| 2. Perceived severity | 0.272** | 1 | ||||
| 3. Perceived vulnerability | 0.248** | 0.556** | 1 | |||
| 4. Self-efficacy | 0.218** | 0.096 | 0.128* | 1 | ||
| 5. Response-efficacy | 0.167** | 0.153** | 0.234** | 0.593** | 1 | |
| 6. Response-cost | 0.13* | 0.388** | 0.270** | 0.091 | 0.111* | 1 |
Notes: **Correlation is significant at the 0.01 level (2-tailed); *Correlation is significant at the 0.05 level (2-tailed).
Regarding the logistic regression analysis for factors predicting COVID-19 behavioral intentions, Table 5 shows that the gender, availability of PPE, and self-efficacy had a significant prediction of COVID-19 behavioral intentions (P <0.05) with a predicted increase of 0.56, 0.37, and 0.12, respectively, in the mean of the intension score. Self-efficacy was the highest significant predictor of the behavior (p=0.008).
Table 5.
Logistic Regression Analysis for Factors Predicting COVID-19 Behavioral Intensions
| Predictors | B | Wald | P value | Exp(B) | 95% C.I. for EXP(B) | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Constant | −6.206 | 23.582 | 0.000 | 0.002 | ||
| Gender | 0.568 | 6.217 | 0.013* | 1.765 | 1.129 | 2.759 |
| Profession | 0.145 | 1.855 | 0.173 | 1.156 | 0.938 | 1.424 |
| Availability of PPE | 0.373 | 5.621 | 0.018* | 1.452 | 1.067 | 1.977 |
| IPC training | 0.214 | 2.264 | 0.132 | 1.239 | 0.937 | 1.638 |
| Perceived severity | 0.039 | 1.141 | 0.286 | 1.040 | 0.968 | 1.118 |
| Perceived vulnerability | 0.061 | 0.967 | 0.325 | 1.062 | 0.942 | 1.199 |
| Response efficacy | 0.019 | 0.309 | 0.578 | 1.019 | 0.954 | 1.088 |
| Self-efficacy | 0.122 | 7.020 | 0.008* | 1.130 | 1.032 | 1.237 |
| Response cost | −.025 | 0.046 | 0.831 | 0.975 | 0.777 | 1.225 |
Note: *P ≤ 0.05 is significance.
Abbreviations: IPC, infection prevention and control; PPE, personal protective equipments; HCPs, health care providers.
Discussion
Recently, one of the most common discussions worldwide is the preventive behavior toward the ongoing COVID-19 pandemic. In the current study, the determinants and predictors of preventive behaviors among HCPs were presented in the framework of the PMT model.
The present results revealed that there was a significant association between intention to comply with COVID-19 preventive behavior and female gender. Evidence from infectious disease outbreaks21 similar to COVID-19, besides other publications22 in terms of health beliefs and healthy behaviors, showed similar findings that women were more adopted and adherent to preventive behavior than men.
This gender difference might be attributed to the social and gender norms in most of the countries that women are foremost shouldering compound burdens and leading the health response for her family members especially, most of our participants were nurses who made her more fear of COVID-19 infection and so more willing to preventive behaviors than the men. From this perspective, certain plans to reinforce the preventive behaviors for COVID-19 are needed to cover the gender gaps.
The only way to control new life-threatening epidemics at the early stage is optimal IPC behaviors and maximal PPE protection.23 This study showed that having training in IPC measures were significantly associated with intention to comply with COVID-19 preventive behavior. In contrast, a previous study reported increasing numbers of COVID-19 cases among HCPs and suggests that IPC measures should be revisited in the guidelines.24 Furthermore, a study that was conducted by Lai et al, 202025 reported worse IPC behaviors among HCWs and attributed these results to the higher workload and insufficient supplies and resources among these HCWs.
Despite shortages of PPE are expected during pandemics due to high demand, as occurred in past epidemics,26 but on the other hand, the protective behaviors of HCPs against COVID-19 showed that a vast majority of the participant always intended to wear a face mask, use gloves, and adhere to hand hygiene and the recommended precautions until the end of COVID-19 pandemic.
PMT is originally developed to explain how to influence risky behavior and which components a persuasive message should include.14 The findings of our study showed that the coping appraisal of PMT (particularly self-efficacy and response-efficacy) was highly significantly associated with the intention to engage in COVID-19 protective behaviors compared to the threat appraisal. Similarly, the role of coping appraisal has been reported in previous studies conducted by Gong et al, 2009, and Chen et al, 2010.27,28 By contrast, protective behaviors against workplace illnesses were unfavorable among healthcare staff in other studies.29,30 The disparity of different studies may be related to factors such as awareness, the perceived threat of illnesses, and training provided in the workplace.
In the last years, PMT was successfully applied for predicting the prevention of infectious and chronic non-communicable diseases, such as HIV/AIDS,27,31 respiratory infectious disease,32 coronary artery disease,33 schistosomiasis,34 and cancer prevention behaviors.35 Yet, this theory has not been used to explore the protective behaviors of COVID-19 in Saudi Arabia.
Previous publications36,37 reported that those enjoying a higher level of self-efficacy perceive themselves capable of making achievements and show a tendency to preventive behaviors of the disease. In alignment with these findings, our results reported that self-efficacy was the highest significant predictor of the behavior. Thus, it is suggested to be targeted in COVID-19 health promotion programs for HCPs to increase their behavior intentions by providing positive coping messages to enhance their confidence in protective behaviors and increase motivation for preventing COVID-19.
On the other hand, threat appraisal appeared to be of relatively little importance for predicting COVID-19 health-protective behaviors. This could be explained by the fact that the majority of participants were less than 45 years old which may be a reason for the unprecedented effect of perceived severity and vulnerability in PMT and preventive behaviors.
The Limitations of the Study
This study has some limitations. Data were self-reported through a cross-sectional survey. So, it is hard to exclude information bias or verify the observed relationship between PMT sub-constructs and intention behavior. Moreover, the study sample was convenience sampling. Thus, we cannot generalize our findings to the general HCPs of KSA. Despite these limitations, findings from this study may contribute to the existing literature by exploring the determinants of preventive behaviors towards the COVID-19 pandemic and serve as an important resource supporting more effective COVID-19 prevention and control programs.
Conclusion
In conclusion, females’ gender, nurses, having training in IPC measures, and availability of PPEs during work time have a significant association with intention to comply with COVID-19 preventive behavior. The present study coping appraisal particularly, self-efficacy predicted COVID-19 pandemic protection motivation and preventive behavior more than threat appraisal. Therefore, future training programs must consider the level of self-efficacy of HCPS, and increase their knowledge regarding the effectiveness of recommendation strategies to perform protective measures against the COVID-19.
Acknowledgments
We would like to acknowledge all the HCPs who participated in and contributed samples to the study for their cooperation and help in facilitating data collection.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work. No funds were received for this study from any funding organization.
References
- 1.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gates B. Responding to Covid-19 - a once-in-a-century pandemic? N Engl J Med. 2020;382:1677–1679. doi: 10.1056/NEJMp2003762 [DOI] [PubMed] [Google Scholar]
- 4.Sohrabi C, Alsafi Z, O’Neill N, et al. World health organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eurosurveillance editorial team. Note from the editors: world health organization declares novel coronavirus (2019-nCoV) sixth public health emergency of international concern. Euro Surveill. 2020;25(5):pii=200131e. doi: 10.2807/1560-7917.ES.2020.25.5.200131e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Worldometers.info, Dover, Delaware, U.S.A. Available from: http://www.worldometers.info/coronavirus/#countries. Accessed May30, 2020.
- 7.Barry M, Al Amri M, Memish ZA. COVID-19 in the shadows of MERS-CoV in the Kingdom of Saudi Arabia. J Epidemiol Glob Health. 2020;10(1):1–3. doi: 10.2991/jegh.k.200218.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arabia MoHoS. Media center. 2020. Available from: https://www.moh.gov.sa/en/Ministry/MediaCenter/Pages/default.aspx. Accessed May30, 2020.
- 9.Nemati M, Ebrahimi B, Nemati F. Assessment of Iranian nurses’ knowledge and anxiety toward COVID-19 during the current outbreak in Iran. Arch Clin Infect Dis. 2020;15(COVID–19). doi: 10.5812/archcid.102848 [DOI] [Google Scholar]
- 10.Gan WH, Lim JW, Koh D. Preventing intra-hospital infection and transmission of COVID-19 in healthcare workers. Saf Health Work. 2020;11(2):241–243. doi: 10.1016/j.shaw.2020.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pakistan reports death of third doctor from coronavirus. n.d.. https://nation.com.pk/06-Apr-2020/pakistan-reports-death-of-3rd-doctor-from-coronavirus. Accessed May30, 2020.
- 12.Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. n.d.. Available from: https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125. Accessed May30, 2020.
- 13.Rogers RW. A protection motivation theory of fear appeals and attitude change. J Psychol. 1975;91(5):93–114. doi: 10.1080/00223980.1975.9915803 [DOI] [PubMed] [Google Scholar]
- 14.Rogers RW. Cognitive and physiological processes in fear-based attitude change: a revised theory of protection motivation In: Cacioppo J, Petty R, editors. Social Psychophysiology. New York, NY: Guilford; 1983:153–176. [Google Scholar]
- 15.Milne S, Sheeran P, Orbell S. Prediction and intervention in health-related behavior: a meta-analytic review of protection motivation theory. J Appl Soc Psychol. 2000;30(1):106–143. doi: 10.1111/j.1559-1816.2000.tb02308.x [DOI] [Google Scholar]
- 16.Yan YQ, Jacques-Tiura AJ, Chen XG, et al. Application of the protection motivation theory in predicting cigarette smoking among adolescents in China. Addict Behav. 2014;39(1):181–188. doi: 10.1016/j.addbeh.2013.09.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Webb TL, Sniehotta FF, Michie S. Using theories of behaviour change to inform interventions for addictive behaviours. Addiction. 2010;105(11):1879–1892. doi: 10.1111/j.1360-0443.2010.03028.x [DOI] [PubMed] [Google Scholar]
- 18.Bashirian S, Jenabi E, Khazaei S, et al. Factors associated with preventive behaviours of COVID-19 among hospital staff in Iran in 2020: an application of the protection motivation theory. J Hosp Infect. 2020;105(3):430–433. doi: 10.1016/j.jhin.2020.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sampsize. Sample size for a prevalence survey, with finite population correction. Available from: http://sampsize.sourceforge.net/iface/#prev. Accessed April7, 2018.
- 20.World Medical Association. World medical association declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Med Assoc. 2013;310:2191e 2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 21.Moran KR, Del Valle SY. A meta-analysis of the association between gender and protective behaviors in response to respiratory epidemics and pandemics. PLoS One. 2016;11(10):e0164541. doi: 10.1371/journal.pone.0164541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karimy M, Araban M, Zareban I, Taher M, Abedi A. Determinants of adherence to self-care behavior among women with type 2 diabetes: an explanation based on health belief model. Med J Islam Repub Iran. 2016;30:368. [PMC free article] [PubMed] [Google Scholar]
- 23.Wenzel RP, Bearman G, Edmond MB. Lessons from severe acute respiratory syndrome (SARS): implications for infection control. Arch Med Res. 2005;36(6):610–616. doi: 10.1016/j.arcmed.2005.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Islam MS, Rahman KM, Sun Y, Qureshi M, Abdi I, Chughtai A. Current knowledge of COVID-19 and infection prevention and control strategies in healthcare settings: a global analysis. Infect Control Hosp Epidemiol. 2020;41(10):1196–1206. doi: 10.1017/ice.2020.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lai X, Wang X, Yang Q, et al. Will healthcare workers improve infection prevention and control behaviors as COVID-19 risk emerges and increases, in China? Antimicrob Resist Infect Control. 2020;9(1):1–9. doi: 10.1186/s13756-020-00746-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chughtai AA, Seale H, Islam MS, Owais M, Macintyre CR. Policies on the use of respiratory protection for hospital health workers to protect from coronavirus disease (COVID-19). Int J Nurs Stud. 2020;105:103567. doi: 10.1016/j.ijnurstu.2020.103567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gong J, Stanton B, Lunn S, et al. Effects through 24 months of an HIV/AIDS prevention intervention program based on protection motivation theory among preadolescents in the Bahamas. Pediatrics. 2009;123:E917–E928. doi: 10.1542/peds.2008-2363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen X, Stanton B, Gomez P, et al. Effects on condom use of an HIV prevention programme 36 months postintervention: a cluster randomized controlled trial among Bahamian youth. Int J STD AIDS. 2010;21:622–630. doi: 10.1258/ijsa.2010.010039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fathi Y, Barati M, Zandiyeh M, Bashirian S. Prediction of preventive behaviors of the needlestick injuries during surgery among operating room personnel: application of the health belief model. Int J Occup Environ Med. 2017;8(4):232–240. doi: 10.15171/ijoem.2017.1051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nga TWY, Cowling BJ, ChiSo H, Ip DKM, Liao Q. Testing an integrative theory of health behavioural change for predicting seasonal influenza vaccination uptake among healthcare workers. Vaccine. 2020;38(3):690–698. doi: 10.1016/j.vaccine.2019.10.041 [DOI] [PubMed] [Google Scholar]
- 31.Zhang L, Li X, Zhou Y, et al. Predictors of consistent condom use among chinese female sex workers: an application of the protection motivation theory. Health Care Women Int. 2015;36(7):816–833. doi: 10.1080/07399332.2014.942902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams L, Rasmussen S, Kleczkowski A, et al. Protection motivation theory and social distancing behaviour in response to a simulated infectious disease epidemic. Psychol Health Med. 2015;20(7):832–837. doi: 10.1080/13548506.2015.1028946 [DOI] [PubMed] [Google Scholar]
- 33.Tulloch H, Reida R, D’angeloa MS, et al. Predicting short and long-term exercise intentions and behaviour in patients with coronary artery disease: a test of protection motivation theory. Psychol Health. 2009;24(3):255–269. doi: 10.1080/08870440701805390 [DOI] [PubMed] [Google Scholar]
- 34.Xiao H, Li S, Chen X, et al. Protection motivation theory in predicting intention to engage in protective behaviors against schistosomiasis among middle school students in rural China. PLoS Negl Trop Dis. 2014;8(10):e3246. doi: 10.1371/journal.pntd.0003246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Babazadeh T, Nadrian H, Banayejeddi M, et al. Determinants of skin cancer preventive behaviors among rural farmers in iran: an application of protection motivation theory. J Cancer Educ. 2016:1–9. doi: 10.1007/s13187-016-1004-7. [DOI] [PubMed] [Google Scholar]
- 36.Zare Sakhvidi MJ, Zare M, Mostaghaci M, Mehrparvar AH, Morowatisharifabad MA, Naghshineh E. Psychosocial predictors for cancer prevention behaviors in workplace using protection motivation theory. Adv Prev Med. 2015;467–498. doi: 10.1155/2015/467498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leigh L, Taylor C, Glassman T, Thompson A, Sheu JJ. A cross-sectional examination of the factors related to emergency nurses’ motivation to protect themselves against an Ebola infection. J Emerg Nurs. 2020;46(6):814–826. doi: 10.1016/j.jen.2020.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]