Abstract
Background
Containment, involving separation and restriction of movement of people due to the COVID-19 pandemic, and mitigation, also referred to as lockdown, involving closure of schools, universities and public venues, has had a profound impact on people's lives globally. The study focuses on the effects of containment and mitigation measures, on the behavior of children and youth (CaY) with Autism Spectrum Disorders (ASD). The study primary aim was to examine the impact of these urgent measures on the behaviors, communication, sleep, and nutritional status of the CaY. A secondary aim was to explore risk and protective factors on behavior change including sociodemographic variables, living conditions, ASD symptom severity and continuity of interventions.
Methods
The study sample consisted of 239 ASD subjects, 2–21 years of age, enrolled in the ELENA cohort in France at Stage 3 confinement and mitigation measures announced on March 16, 2020. A parent informant completed the COVID-19 questionnaire.
Results
Of the domains examined, challenging behaviors, communicative skills and sleep had the greatest impact; in terms of risk and protective factors, subject age, ASD severity, single parenthood, daily living skills, and intervention continuity were most likely to impact behaviors; living conditions were not linked to behavior change.
Conclusions
The findings highlight the topography of behavioral change in CaY with ASD following institution of containment and mitigation measures during the COVID-19 pandemic and help identify risk and protective factors to help better address needs and tailor interventions in the future.
Keywords: COVID-19, Containment, Autism spectrum disorders, Children behaviors, France
Abbreviations: Autism Spectrum Disorders (ASD), Children and Youth (CaY)
1. Introduction
The coronavirus disease 2019 (COVID-19), first identified in December 2019 in Wuhan, China, spread rapidly across the globe, and was declared a pandemic by the World Health Organization on March 11, 2020 (World Health Organization, 2020). On March 16, 2020, population measures were implemented across France to control the community transmission of COVID-19 including containment, involving social distancing with restriction of movements, and mitigation, also known referred to as lockdown, involving the closure of nurseries, school, universities, and cancellation of public venues such as sports and concerts, introduction of restricted work hours and teleworking, use of face coverings when distancing was not possible, and implementation of hygiene measures. As the number of reported cases and deaths from COVID-19 increased in ensuing weeks, the French population was subjected to several months of social isolation, and allowed to leave only for essential sustenance and medical needs (Casagrande et al., 2020). In this paper we use the terms containment and mitigation that represented an extended period of restriction to prevent widespread community transmission, instead of the term quarantine that refers to a period of isolation of persons potentially exposed to COVID-19.
These restrictive measures have had a profound impact on people's lives (Brondino et al., 2020; Colizzi et al., 2020; Pisano et al., 2020). For some children, adolescents and adults alike, the sudden disruption of daily routines and family lives represented a distressing event. In fact, some authors (Pfefferbaum and North, 2020; Rubin and Wessely, 2020) have suggested that, in addition to the stress associated with the fear of contracting the illness, containment and mitigation themselves have presented additional psychological burden for the population (Casagrande et al., 2020; Qiao et al., 2020; Yan and Huang, 2020).
Regarding children and youth, the effects of quarantine in Italy involved parental stress and psychological problems in families facing the COVID-19 (Spinelli et al., 2020) with children and youth staying at home without the opportunity to engage in familiar activities that helped enrich their daily lives (Spinelli et al., 2020). In an Indian study (Saurabh and Ranjan, 2020), most confined children and adolescents during the COVID-19 pandemic were reported to exhibit psychological distress much higher than the non-confined group. In China, Jiao et al. (2020) reported the presence of psychological difficulties in children during the COVID-19 pandemic, with fear, inattention and irritability being the most severe symptoms in children. A further study of confinement in Italy and Spain (2020), showed that 85.7% of the parents perceived changes in their children's emotional state and behavior, the most frequent symptoms being difficulty concentrating, boredom, irritability, restlessness, loneliness, and worries. Similarly, a qualitative study of emotional and behavioral correlates of confinement of 4–10 years children in Italy (Pisano et al., 2020), also showed marked effects, with half the children exhibiting greater irritability, intolerance of rules and excessive demands. Concerning the sleep patterns of children, a study by Orgilés et al. (2020) noted more hours of sleep during confinement, whereas a study by Pisano et al. (2020) showed that one in five children present sleep problems including difficulty falling sleep as well as frequent waking up. Finally, a mixed-methods study showed that disease-containment measures during the pandemic leads to post-traumatic stress disorder (PTSD) with 30% of isolated children meeting PTSD criteria based on parent report, and 25% met PTSD criteria based on self-reports (Sprang and Silman, 2013).
The specific vulnerabilities of risk groups have been highlighted during the COVID-19 outbreak, including the elderly, persons with pre-existing medical comorbidities, pregnant women, as well as the homeless (Courtenay and Perera, 2020; Kirby, 2020; Qiao et al., 2020; World Health Organization, 2020). Less attention has been paid to people with neurodevelopmental disorders, although it is increasingly recognized that people with pre-existing mental conditions need extra support during confinement (Brooks et al., 2020) and have more risk of psychological distress following disaster-related traumas (Alvarez and Hunt, 2005; Cavallera et al., 2020; Cukor et al., 2011).
In persons with neurodevelopmental disorders, including those with Autism Spectrum Disorder (ASD), already with compromised deficits in social communication and interactions and restricted patterns of behavior (American Psychiatric Association, 2013), vulnerability to COVID-19 has been considerable (Frankova, 2020). Especially since persons with ASD follow routines and need to be prepared for changes and transitions, unexpected events lead to behavioral challenges (Courtenay and Perera, 2020; Frankova, 2020) and suffering (Narzisi, 2020). Moreover, given that repetitive thoughts and anxiety are common among persons with ASD (Meier et al., 2015), they are likely to be overwhelmed by negative information related to COVID-19 in the media. Persons with ASD also represent a highly heterogeneous group that may have sensory aversion to tolerate protective covering or comply with requests for screening. These factors therefore heighten their vulnerabilities, fears and guarded thinking (Courtenay and Perera, 2020), increase their stereotypies and may even lead to emergence of extreme challenging behaviors such as self-injury (Narzisi, 2020). Since children and youth with ASD are expected to undergo interventions for several hours a week with special therapists at home or in dedicated centers or in clinics and institutes (Narzisi, 2020), the ensuing interruption or modification of level of interventions due to containment measures compounds their well-being. As noted by Courtenay and Perera (2020), the impact of confinement on children and youth with ASD has been especially heightened where the usual support of residential schools, day services, or respite care centers have been withdrawn due to the pandemic.
In the general population, Brooks et al. (2020) highlighted as main stressors the duration of isolation, fear of infection, frustration, boredom, not having adequate information or clear guidelines from authorities, financial problems and stigma related to exposure or illness. Other factors include the configuration of the home environment in terms of indoor space (room per person ratio) or access to outdoor safe play areas. According to Orgilés et al. (2020), psychological effects were noted to be more prominent among children in Spain compared to those in Italy, due to greater availability of home gardens and more relaxed confinement rules in the latter setting. The sensory calming effect of peaceful indoor spaces, as well as access to outdoors, with opportunity for exercise and participatory activities was salient. In addition, the interruption of interventions in the familiar setting was likely to be disproportionately disruptive for children and youth with ASD. Other risk factors could be linked to age, severity of ASD symptoms as well as co-occurrence of other mental disorder and specifiers including intellectual disorders.
1.1. Aims of the study
The main aim of the current study was to examine the behavioral effects of containment and mitigation during the COVID-19 pandemic on a sample of children and youth with ASD. Specifically, the current study examined changes in sleep, nutrition, communication, challenging behaviors and stereotyped behaviors. A secondary aim was to explore the risk and protective factors related to changes in behaviors related to age, ASD symptom severity, sociodemographic factors, living conditions and interventions continuity.
2. Materials and method
2.1. Study design
The present study is a cross-sectional descriptive and analytical survey carried out between 27 April and May 13, 2020, during the Stage 3 maximum containment and mitigation level measures in France (President of the French Republic, 2020). The source population for this sub study was all participants of the ELENA Cohort, for whom parents have answered to the specific COVID-19 questionnaire. The ELENA cohort is a French prospective and multi-center study of ASD subjects ascertained between ages 2–16 years in which patients are followed for a period of 6 years. By collecting clinical, social, environmental, and genetic data, as well as data relating to the parental quality of life, the main objectives of the ELENA cohort are (i) to identify patterns in outcome trajectories for a large sample of children and adolescents with ASD, (ii) to examine determinants of these outcome trajectories at different follow-up stages, and (iii) to constitute an open French database on ASD that promotes collaboration in translational studies (Baghdadli et al., 2019; Rattaz et al., 2020). Complete details of the protocol have been published in detail elsewhere (Baghdadli et al., 2019). The current study was approved by the Internal Review Board of University Hospital of Montpellier.
2.2. Data collection
A letter was sent to the parents in the ELENA cohort via the database electronic system inviting them to participate to the present study by filling out an online questionnaire. Only one questionnaire was completed per child by one parent or both parents serving as joint informant. The COVID-19 parent structured questionnaire comprised of 4 parts: (i) Family environment: house size, number of rooms, household number and composition, and outdoor accessibility; (ii) Parent professional status: loss or reduction of work and teleworking; (iii); Level of information on COVID-19; and (iv) Child status: health, special education interventions, medical care and any need for care (related or unrelated to COVID-19). The parents were also asked to describe their children's behavior during the pandemic on a 3-point Likert scale (unchanged, improved, worse) for 5 domains: nutrition, sleep, challenging behaviors, communicative abilities, and stereotyped behaviors. The clinical characteristics were collected before confinement by licensed psychologists using standardized tools during assessments scheduled in the context of the ELENA protocol. Child and youth adaptive skills were assessed through the Vineland Adaptive Behavior Scales, Second Edition (VABS-II) (Sparrow et al., 2005). Symptom severity was measured using the calibrated severity score (CSS) of the Autism Diagnostic Observation Schedule-2 (ADOS-2) (Gotham et al., 2008; Lord et al., 2012). A best estimate intellectual functioning was calculated using standardized and validated instruments (Brunet-Lézine R (Brunet et al., 1997); BECS (Adrien, 2008); PEP-3 (Lansing et al., 2010); WPPSI-IV (Wechsler, 2014b); WISC-V (Wechsler, 2014a); WAIS-IV (Wechsler, 2008); K-ABC (Kaufman and Kaufman, 1983)) selected in function of child's age and level, according to the approach of Howlin et al. (2014). The tools and measures are thoroughly described in the cohort study profile (Baghdadli et al., 2019).
2.3. Statistical analysis
According to the normality of the continuous variables, mean with standard deviation (SD) or median with interquartile range (IQR) were reported. Categorical variables were described with frequency and percentage. To determine first the factors linked to each child or youth behavior change domain during confinement (i.e., communicative abilities, sleep, nutrition, challenging and stereotyped behaviors), we used Pearson chi-square tests for categorical variables and Anova regressions or Kruskal-Wallis tests for continuous variables. Multivariate polytomic regressions were then used to determine factors significantly associated for each child or youth behavior change domain during confinement. Variables with P value < 0.20 in univariate analysis were included in the multivariate model and we presented OR with 95% confidence intervals. Backward selection was used. Multivariate regressions were adjusted with the child's best estimate IQ. Following factors were considered in the analysis: child and youth age during confinement, last ELENA follow-up ADOS-2 comparison score (CSS), last VABS-II standard scores in communication, socialization and daily living skills, number of children living in home, outing during confinement, continuation of care during confinement, adequation between rooms number and inhabitants, access to an outdoor, single parent family, questionnaire responder and child’ gender. P-values below 0.05 were considered statistically significant. Analyses were performed using SAS software v9.3.
3. Results
3.1. Study sample
Among the 892 participants included in ELENA cohort, there were 240 children and youth (CaY), 2–21 years of age, whose parents completed the COVID-19 questionnaire. One child was excluded because he didn't live with his parents at the time of the confinement. The 239 CaY who were involved in the analyses had higher scores regarding best estimate IQ (p = 0.01), VABS daily living skills (p = 0.03) and communication (p = 0.003) scores than the others participants from the ELENA cohort, but no difference regarding ASD severity at the ADOS were found (Supplementary Table S1, available as supplementary data). The questionnaire was filled for 188 children by the mothers (78.7%), for 18 by the fathers (7.5%), for 32 by both parents together (13.4%) and for 1 child by another adult in the child's entourage who lived with him or her (0.4%). Among the 239 children and adolescents, 190 were males (79.5%; 4–1 male to female ratio). Children's mean age was 9.1 years (SD = 4.0). More details about participants' characteristics are in Table 1 .
Table 1.
ASD children and youth characteristics.
| All children N = 239 | |
|---|---|
| Sex | |
| Male | 190 (79.50%) |
| Female | 49 (20.50%) |
| Age during quarantine (years) | 9.11 (±4.0) |
| Intellectual level | |
| Best estimate t IQ | |
| <70 | 82 (35.65%)* |
| ≥70 | 148 (64.35%) |
| ADOS | |
| Comparison score | 7.242 (±1.818)** |
| Vineland Adaptive Behavior Scales (VABS II) | |
| Communication SS | 72.13 (±16.16)° |
| Daily living skills SS | 72.20 (±14.07)° |
| Socialization SS | 68.96 (±13.19)° |
Data are given in mean (SD), median (IQR), or n (%).
3 missing value, °4 missing values * 9 missing values, ** 24 missing values.
3.2. Family and sociodemographic characteristics
Participants’ familial and sociodemographic characteristics are described in Table 2 . About 24% of the children belonged to single-parent families. Majority of families had only one child with ASD or another neurodevelopmental disorder living in the house (81.6%, n = 195), whereas 17.2% of families had two (n = 41) and 1.3% had three children with ASD or another neurodevelopmental living in the house (n = 3). A decline in household income was reported by 99 respondents (n = 41.6%) who attributed it to total or partial unemployment due to COVID-19.
Table 2.
Family and sociodemographic characteristics.
| N = 239 | |
|---|---|
| Mother's age (years) | 41.64 (±6.79) |
| Father's age (years) | 44.80 (±7.85) |
| Single parent family | |
| No | 182 (76.15%) |
| Yes | 57 (23.85%) |
| Number of children in the house | |
| 1 | 73 (30.54%) |
| 2 | 102 (42.6%) |
| ≥3 | 64 (26.78%) |
| Number of ASD CaY in the house | |
| 1 | 195 (81.59%) |
| 2 | 41 (17.15%) |
| 3 | 3 (1.26%) |
| Father's educational level | |
| Elementary | 5 (2.43%)£ |
| High school | 95 (46.12%) |
| College/University | 106 (51.46%) |
| Mother's educational level | |
| Elementary | 2 (0.95%)££ |
| High school | 81 (38.57%) |
| College/University | 127 (60.48%) |
| Professional situation | |
| Responder's professional situation | |
| Working | 140 (58.82%)¤ |
| Continuity of activities | 40 (28.78%)¤ |
| Complete activity shutdown | 30 (21.58%) |
| Partial technical unemployment | 16 (11.51%) |
| Full technical unemployment | 10 (7.19%) |
| Telework | 43 (30.94%) |
| Student | 1 (0.42%) |
| Retired | 3 (1.26%) |
| Job search | 17 (7.14%) |
| At home | 77 (32.35%) |
| Spouse's professional situation | |
| Working | 159 (66.81%)¤ |
| Continuation of activities | 62 (38.99%) |
| Complete shutdown of activity | 23 (14.47%) |
| Partial technical unemployment | 19 (11.95%) |
| Full technical unemployment | 15 (9.43%) |
| Telework | 31 (19.50%) |
| Student | 9 (5.66%) |
| Retired | 4 (1.68%) |
| In search of employment | 10 (4.20%) |
| At home | 13 (5.46%) |
| Loss of income during confinement | |
| No | 139 (58.40%)¤ |
| Yes | 99 (41.60%) |
Data are given in mean (SD), or n (%).
1 missing value, 3 missing values, £ 33 missing values, ££ 29 missing values.
3.3. Living conditions
The average household size was 4 (SD = 1.2), with two children per household on average (SD = 1.0). On average there were 4.5 rooms per household (SD = 1.4). For 78.7% of respondents (n = 188), the number of rooms in the home was at least equal to the number of occupants. Most respondents in our sample had a garden (64.9%, n = 155). Around 25% of respondents (n = 60), reported that at least one parent teleworked. Overall, 67.0% of CaY went able to access outdoors regularly during confinement, while 33.0% were strictly confined at home (n = 78). Among the most frequent reasons for strict confinement were fear of contamination (n = 48), refusal by the child or youth (n = 12) and having access to a garden (n = 7). The majority of the respondents (83.9%, n = 198) stated that they were aware of the specific conditions of authorization of outings for people with disabilities.
3.4. Interventions received for ASD
Most of the CaY (86.0%, n = 203) were in school before confinement and mitigation measures; 61.4% (n = 145), were receiving special education or care services, 78.8% (n = 186) were in therapy with a professional (mostly speech or physical), and 5.5% (n = 13) were receiving no interventions at all. During the confinement, interventions were maintained for 75.8% (n = 169) and were interrupted for 24.2% (n = 54). For those whom interventions were maintained, these took the form of phone interviews with the parents (44.4%, n = 103), videoconferences with the child (18.1%, n = 42) or appointment with the child (8.6%, n = 20).
3.5. Sleep, communication, nutrition, stereotyped and challenging behaviors
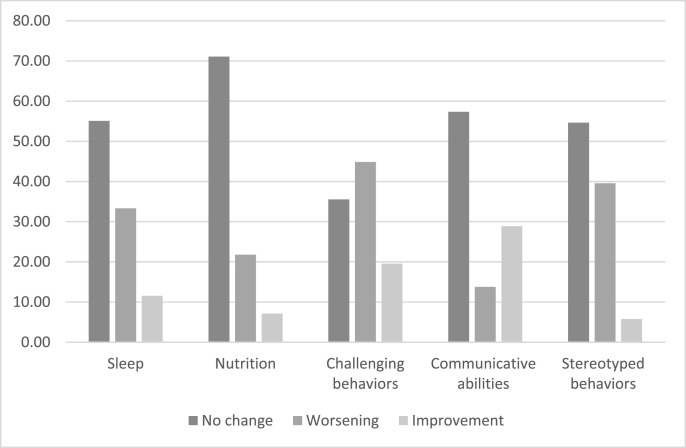
With regards sleep, communicative abilities and stereotyped behaviors, about half the parents (respectively 55.5% (n = 131), 57.2% (n = 135) and 54.7% (n = 129)) reported no changes during confinement. When a change was reported in these domains, the behavior was more often perceived as worsening than improving, except for communication in which more parents reported progress (28.8%, n = 68) than regression (14%, n = 33). Most parents (71.6%, n = 169) reported no change in nutrition behaviors, with only one fifth of them reported a worsening. Most parents (64.4%, n = 152) reported increase in challenging behaviors during confinement (see Fig. 1 ).
Fig. 1.
Parental perception of their children's behaviors during confinement (%).
3.6. Univariate analysis: links between reported behavior changes and clinical/environmental variables
For sleep, the univariate analysis first showed that subjects who were noted to have improved sleep were significantly younger (median = 7.0, IQR [4.5–10.0], n = 28) than those for whom no change in sleep was reported (median = 9.0, IQR [6–12]), n = 131, p = 0.01). CaY with reported improved sleep had a lower severity score (median 6.0, (IQR: [5.0–7.0], n = 23) than those who worsened their sleep (median 8.0, IQR: [6.0–9.0], n = 70, p = 0.003) or those for whom no change was reported by their parents (median 7.0, IQR: [6.0–9.0], n = 120, p = 0.01). Finally, there is more single parent families among CaY who improved or worsened their sleep (33.8%, n = 26 and 32.1%, n = 9 respectively) than among those for whom sleep didn't change during COVID-19 pandemic (16.8%, n = 22), p = 0.01.
Challenging behaviors were also significantly linked to the subject age. CaY whose parents reported decrease in challenging behaviors were younger (median = 7.0, IQR = [5.0–10.0], n = 46) than those whose parents reported no change (median = 9.0, IQR = [7.0–12.0], n = 84), p = 0.004.
Regarding changes in communicative abilities, subjects whose parents reported improvement in communicative abilities were younger (median = 6.0, IQR = [5.0–9.0], n = 68) than those with parent report of regression (median = 9.0, IQR = [6.0–14.0], n = 33) or no change in communicative abilities (median = 9.0, IQR = [7.0–12.0], n = 135), p < 0.01. Results showed that there were more subjects for whom interventions were maintained during COVID-19 among those who progressed in communication (86.8%, n = 59) than among those whose communicative abilities didn't change (65.9%, n = 89) or regressed (63.6%, n = 21). Finally, there were more single parent families among CaY whose communicative abilities regressed (30.3%, n = 10) or didn't change (28.1%, n = 38) than among those whose communicative abilities progressed (13.2%, n = 9), p = 0.04.
Adaptive level and living conditions were not significantly related to the changes in behaviors during COVID-19. Finally, changes in nutrition and stereotyped behaviors were not related to any of the variables above.
3.7. Multivariate analysis
In the multivariate analysis and after adjustment, higher ADOS score was associated with decreased probability of improvement of sleep [OR 0.70 (95%CI 0.53–0.91)] compared to the group without change in sleep. Belonging to a single parent family was a risk factor for the sleep worsening [OR 3.63 (95%CI 1.76–7.49)].
Then, an increase in VABS-II daily living skills score increased the risk to belong to the group with improvement in challenging behaviors [OR 1.47 (95%CI 1.07–2.03)] compared to the group without change, suggesting that CaY with better daily living skills were those whose challenging behaviors decreased the most.
Finally, an increase in subject age decreased the probability to belong to improved group membership with reported improved communicative abilities [OR 0.80 (95%CI 0.71–0.89)] compared to the group without change. In other words, younger children were those for whom more progress in communication were observed by the parents.Table 3 .
Table 3.
Risk factors for change in sleep, challenging behaviors and communicative abilities.
| Variable | Change in sleep |
Change in challenging behaviors |
Change in communicative abilities |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Crude OR |
Adjusted OR* |
Crude OR |
Adjusted OR* |
Crude OR |
Adjusted OR* |
||||||||
| OR (95%CI) | Pvalue | OR (95%CI) | Pvalue | OR (95%CI) | Pvalue | OR (95%CI) | Pvalue | OR (95%CI) | Pvalue | OR (95%CI) | Pvalue | ||
| Child's age (years) | Improvement | 0.87 (0.77–0.98) | 0.06 | 0.88 (0.80–0.97) | 0.04 | 0.76 (0.69–0.84) | <0.01 | 0.80 (0.71–0.89) | <0.01 | ||||
| Worsening | 0.98 (0.91–1.09) | 0.97 (0.90–1.04) | . | 0.99 (0.90–1.09) | 1.00 (0.90–1.11) | ||||||||
| ADOS comparison score | Improvement | 0.71 (0.55–0.9) | 0.01 | 0.70 (0.53–0.91) | 0.01 | 0.92 (0.75–1.14) | 0.68 | 1.07 (0.90–1.27) | 0.41 | ||||
| Worsening | 1.06 (0.90–1.26) | 1.08 (0.90–1.30) | 1.01 (0.85–1.19) | . | 1.16 (0.92–1.46) | ||||||||
| Communication SS (units = 10) | Improvement | 0.99 (0.76–1.27) | 0.55 | 1.09 (0.87–1.36) | 0.68 | ||||||||
| Worsening | 0.91 (0.76–1.08) | 1.07 (0.90–1.28) | . | ||||||||||
| Daily living skills SS (units = 10) | Improvement | 1.04 (0.77–1.41) | 0.12 | 1.26 (0.96–1.66) | 0.11 | 1.47 (1.07–2.03) | <0.01 | 0.98 (0.79–1.20) | 0.78 | ||||
| Worsening | 0.82 (0.67–1.01) | 0.95 (0.78–1.17) | . | 0.86 (0.67–1.10) | 0.91 (0.70–1.19) | ||||||||
| Socialization SS (units = 10) | Improvement | 1.03 (0.75–1.41) | 0.90 | 1.10 (0.82–1.47) | 0.49 | 1.03 (0.82–1.29) | 0.90 | ||||||
| Worsening | 0.96 (0.78–1.19) | 0.93 (0.75–1.17) | . | 0.96 (0.72–1.27) | |||||||||
| Number of children living in home | Improvement | 1.10 (0.74–1.64) | 0.77 | 1.39 (0.97–1.97) | 0.19 | 1.14 (0.86–1.52) | 0.58 | ||||||
| Worsening | 1.10 (0.83–1.45) | 1.15 (0.85–1.55) | . | 1.16 (0.80–1.67) | |||||||||
| Outing during quarantine with child No vs Yes | Improvement | 1.43 (0.63–3.29) | 0.29 | 1.16 (0.55–2.43) | 0.35 | 0.58 (0.30–1.09) | 0.12 | ||||||
| Worsening | 0.712 (0.34–1.33) | . | 0.71 (0.38–1.31) | . | 0.51 (0.21–1.22) | ||||||||
| Continuity of care during quarantine Yes vs No | Improvement | 1.68 (0.59–4.80) | 0.72 | 1.55 (0.62–3.89) | 0.78 | 3.50 (1.47–8.38) | 0.04 | ||||||
| Worsening | 1.48 (0.74–2.95) | . | 1.00 (0.51–1.96) | . | 0.87 (0.38–2.03) | ||||||||
| Continuity of care during quarantine Not usually under care vs No | Improvement | 0.85 (0.09–8.32) | . | 0.83 (0.14–5.03) | . | 1.17 (0.21–6.64) | . | ||||||
| Worsening | 1.13 (0.30–4.35) | . | 0.64 (0.17–2.41) | . | 0.82 (0.15–4.43) | . | |||||||
| Adequation between rooms number and inhabitants: rooms number < inhabitants vs rooms number ≥ inhabitants | Improvement | 1.28 (0.49–3.34) | 0.87 | 1.50 (0.64–3.53) | 0.65 | 2.78 (1.40–5.50) | 0.01 | ||||||
| Worsening | 1.09 (0.55–2.17) | . | 1.18 (0.58–2.41) | . | 1.46 (0.56–3.80) | ||||||||
| Access to an Outdoor Yes vs No | Improvement | 1.99 (0.24–16.39) | 0.81 | 3.46 (0.40–29.59) | 0.47 | 6.54 (0.83–51.37) | 0.19 | ||||||
| Worsening | 1.06 (0.34–3.29) | . | 0.94 (0.31–2.83) | . | 1.51 (0.32–7.11) | ||||||||
| Single parent family Yes vs No | Improvement | 2.35 (0.94–5.87) | 0.01 | 3.00 (1.06–8.51) | <0.01 | 1.62 (0.69–3.85) | 0.24 | 0.39 (0.18–0.86) | 0.05 | ||||
| Worsening | 2.53 (1.31–4.88) | . | 3.63 (1.76–7.49) | 1.82 (0.91–3.66) | . | 1.11 (0.48–2.55) | |||||||
Other factors (Responder of the questionnaire and the child's sex) have been tested in univariate analysis, but were not associated with the change of one of the three behaviors.
For each regression, the modelisation reference group was behavior change.
* OR adjusted on the last Best estimate IQ.
4. Discussion
It is remarkable that during the Stage 3 phase of the pandemic, the results showed that while majority of CaY with ASD were able to go out regularly, one-third remained strictly confined at home as their parents feared transmission. Further, the interventions from special education services or private professionals were maintained for three quarters of the CaY; nevertheless, the interventions were adapted and mainly provided via telephone and telehealth services. Although not optimal, this level of interventions bodes well for the care of the CaY enrolled in the ELENA cohort during the COVID-19 pandemic but is not necessarily reflective of the country at large.
Concerning the impact of confinement on CaY in terms of sleep, nutrition, communication, as well as stereotypical and challenging behaviors, the parents reported mostly deterioration in challenging behaviors, with some worsening of sleep and stereotypical repetitive behaviors. These results suggest that CaY with ASD are likely to be adversely affected by containment measures, a finding that is congruent with studies of neurotypical CaY who show psychological effects of confinement including fear, irritability or sleep problems during the pandemic (Jiao et al., 2020; Orgilés et al., 2020; Pisano et al., 2020).
In terms of communication, the parents reported more progress than regression: almost one third of the parents reported improvement in language or social communication and interaction of their CaY. This finding can be interpreted in a number of ways. First, it is conceivable that the containment emergency measures can have a positive impact on CaY with ASD who are no longer exposed to stressful situations in their daily life, with reduced transitions between home and school, reduced aversive or sensory interactions and academic pressures. A previous study of the ELENA cohort on school inclusion in children and adolescents with ASD (Rattaz et al., 2020) found that there were more anxiety symptoms in children and adolescents who were attending school on a full-time basis as compared to those who were attending school part-time. An entire day of school may represent a considerable challenge for children with ASD, requiring them to maintain sustained attention, tolerate interactions with other students, as well as manage their sensory environment. Second, we hypothesized that being confined at home might alleviate parental stress, which might have an effect on improved perception of communication in the CaY. It would be congruent with previous studies showing alleviation of stress in children confined at home, who appeared as calmer (Pisano et al., 2020). Positive effects of containment also included greater proximity of the CaY to their parents, who were themselves more likely to be sequestered at home, with enhanced opportunity to engage with them.
In terms of the secondary study aim related to the risk and protective factors, greater improvement in sleep was reported for younger subjects, and in those with lower ASD symptom severity. Sleep disorders are one of the most burdensome and profound complaints among parents and caregivers of CaY with ASD, described in about 40–80% of individuals with ASD (Cohen et al., 2014), and are highly variable across time (Mazurek et al., 2019). The change in challenging behaviors were also significantly linked to subjects’ age; parents reported greater improvement in challenging behaviors for younger subjects. Such a relationship between age and improvement can also be viewed in the light of studies on developmental trajectories in ASD, with a higher curve in challenging behaviors in the earlier ages (Baghdadli et al., 2012).
Regarding family and sociodemographic factors, our results suggest that living in a single parent family is related to more variability (improvement or worsening) in sleep during confinement as well as less progress in communication. We can hypothesize that living in a single family, and consequently not having respite for household chores, professional activity, and taking care of the CaY with ASD, would constitute a supplementary source of stress during confinement, possibly leading to more difficulties for the CaY. We found no significant relationships between living conditions during confinement and parent reported behavior changes among the CaY, a finding not supported by previous results in neurotypical children (2020).
An important positive finding regarding continuity of interventions provided to the CaY with ASD, was related to greater progress in communication. Courtenay et al. (2020) indicated that the impact of confinement on families is especially heightened where the usual supports of residential schools, day services, or respite care have been withdrawn due to the pandemic. Consistent with this finding, the CaY in the present study who progressed in communication were those who continued to benefit from specialized interventions during confinement, even if these interventions were mostly provided via telehealth tools.
In terms of risk and protective factors, the multivariate analysis demonstrated that CaY with greater ASD symptom severity scores, and those living in a single parent family, were the ones for whom their parents reported less sleep improvement, or more sleep worsening, respectively. These results suggest that ASD severity, and family characteristics, are key factors enabling sleep regulation in CaY with ASD.
Moreover, we found that decrease in challenging behaviors was more important in CaY with better daily living skills. In summary, CaY with ASD who are more dependent were less likely to adapt to changes in the home environment and more likely to experience difficulties in adjusting to their newly imposed confined lifestyle, potentially causing a heightened level of stress and expression of challenging behaviors. Such an indirect relationship between adaptive abilities and challenging behaviors is consistent with prior literature (Baeza-Velasco et al., 2014; Franchini et al., 2018).
Finally, even though several negative effects of the emergency containment and mitigation measures on the behaviors of CaY were reported, such as sleep and challenging behaviors, favorable effects were noted by the parents for some subjects in the communication domain. Greater progress in communication skills were more likely to be noted for younger subjects compared to older ones. This observation underscores the potential for early development of communicative abilities in children with ASD, and the need for early intervention to prevent delays (Landa, 2007). Although confinement could represent a distressing event for CaY with ASD impacting their behaviors, it may also reduce level of stress in some subjects in view of diminished opportunities for aversive sensory and social stimulation, that so often can contribute to stress and anxiety in some subjects (Rattaz et al., 2020). Understanding the reactions of CaY with ASD, and identifying risk and protective factors, is therefore essential to more selectively and appropriately address their needs, and to tailor present, and future interventions (Sprang and Silman, 2013). This is likely to empower CaY with ASD, as well as their parents, as they are likely to face future recurrence of COVID-19 and other outbreaks (Courtenay and Perera, 2020).
Several limitations should be note when interpreting our findings. First, the sample of subjects involved in the analyses had higher scores regarding cognitive adaptive levels than the other participants in the ELENA cohort, which limits the generalization of our results. The impact of containment and mitigation measures in CaY with ASD might be more important than what we observed in this study. Second, most of questionnaires were filled by only one parent (86.2%), however parents may have differing perspectives regarding the behaviors of their CaY with ASD. Further, a parent report can be influenced by their own stressful experience of the pandemic based on the home life and work circumstances, as well as time available with children, resources and supports. Likewise, the level of external supports and service availability for CaY with ASD varies across settings that may influence parent perspectives. Moreover, longitudinal studies are required to assess the longer lasting effects of confinement and mitigation on CaY with ASD during pandemics. Finally, the lack of a pre-lockdown baseline complicates the interpretation of the effects reported, however it would have been complicated to measure it due to unpredictability of epidemics.
Declaration of competing interest
The authors declare they have no conflict of interest.
Acknowledgments
We thank the contributing families, the ELENA cohort staff (Ela Miniarikova, Flore Couty, Florine Dellapiazza, Lee Audras-Torrent, Cécile Michelon, Myriam Soussana, Laetitia Ferrando and Christelle Vernhet) and the clinical team of Montpellier hospital. We express gratitude to the CNSA and DGOS for funding this research.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2021.02.041.
Trial registration number
Author contributions
AB, CR and MB conceived the study and drafted the manuscript. MP contributed to the conception of the research questions and protocol and she was involved in data analysis and the manuscript writing. JL contributed to the conception of the research questions and protocol, the creation of database and provided comments on the manuscript drafts. AB is the PI of ELENA cohort, she also participated in the design of the current study, drafted the work and revised it critically, with KM, for main intellectual content. All authors read and approved the final version to be published.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Adrien J.-L. De Boeck Supérieur; Louvain-la-Neuve: 2008. BECS : Batterie d'évaluation cognitive et socio-émotionnelle. (Pratiques psychologiques et recherches cliniques auprès des enfants atteints de TED). [Google Scholar]
- Alvarez J., Hunt M. Risk an resilience in canine search and rescue handlers after 9/11. J. Trauma Stress. 2005;18(5):497–505. doi: 10.1002/jts.20058. [DOI] [PubMed] [Google Scholar]
- American Psychidatric Association . 2013. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Baeza-Velasco C., Michelon C., Rattaz C., Baghdadli A. Are Aberrant Behavioral patterns associated with the adaptive behavior trajectories of teenagers with Autism Spectrum Disorders? Res Autism Spectr Disord. 2014;8(3):304–311. [Google Scholar]
- Baghdadli A., Assouline B., Sonié S., Pernon E., Darrou C., Michelon C., Picot M.-C., Aussilloux C., Pry R. Developmental trajectories of adaptive behaviors from early childhood to adolescence in a cohort of 152 children with autism spectrum disorders. J. Autism Dev. Disord. 2012;42(7):1314–1325. doi: 10.1007/s10803-011-1357-z. [DOI] [PubMed] [Google Scholar]
- Baghdadli A., Miot S., Rattaz C., Akbaraly T., Geoffray M.-M., Michelon C., Loubersac J., Traver S., Mortamais M., Sonié S. Investigating the natural history and prognostic factors of ASD in children: the multicEntric Longitudinal study of childrEN with ASD-the ELENA study protocol. BMJ open. 2019;9(6) doi: 10.1136/bmjopen-2018-026286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brondino N., Damiani S., Politi P. Effective strategies for managing COVID-19 emergency restrictions for adults with severe ASD in a daycare center in Italy. Brain Sci. 2020;10(7) doi: 10.3390/brainsci10070436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunet O., Lézine I., Josse D. 1997. Brunet-Lézine révisé: échelle de développement psychomoteur de la première enfance: BLR. Editions et applications psychologiques. [Google Scholar]
- Casagrande M., Favieri F., Tambelli R., Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavallera V., Nasir R., Munir K. 2020. Children and Adolescents with Developmental Disabilities in Humanitarian Settings, Child, Adolescent and Family Refugee Mental Health. Springer; pp. 195–212. [Google Scholar]
- Cohen S., Conduit R., Lockley S.W., Rajaratnam S.M., Cornish K.M. The relationship between sleep and behavior in autism spectrum disorder (ASD): a review. J. Neurodev. Disord. 2014;6(1):44. doi: 10.1186/1866-1955-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: an online parent survey. Brain Sci. 2020;10(6) doi: 10.3390/brainsci10060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtenay K., Perera B. COVID-19 and people with intellectual disability: impacts of a pandemic. Ir. J. Psychol. Med. 2020:1–21. doi: 10.1017/ipm.2020.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukor J., Wyka K., Jayasinghe N., Weathers F., Giosan C., Leck P., Roberts J., Spielman L., Crane M., Difede J. Prevalence and predictors of posttraumatic stress symptoms in utility workers deployed to the World Trade Center following the attacks of September 11, 2001. Depress. Anxiety. 2011;28(3):210–217. doi: 10.1002/da.20776. [DOI] [PubMed] [Google Scholar]
- Franchini M., Zöller D., Gentaz E., Glaser B., Wood de Wilde H., Kojovic N., Eliez S., Schaer M. Early adaptive functioning trajectories in preschoolers with autism spectrum disorders. J. Pediatr. Psychol. 2018;43(7):800–813. doi: 10.1093/jpepsy/jsy024. [DOI] [PubMed] [Google Scholar]
- Frankova H. The impact of COVID-19 on people with autism, learning disabilities and mental health conditions. Nurs. Resid. Care. 2020;22(6):1–3. [Google Scholar]
- Gotham K., Risi S., Dawson G., Tager-Flusberg H., Joseph R., Carter A., Hepburn S., McMahon W., Rodier P., Hyman S.L. A replication of the autism diagnostic observation Schedule (ADOS) revised algorithms. J. Am. Acad. Child Adolesc. Psychiatry. 2008;47(6):642–651. doi: 10.1097/CHI.0b013e31816bffb7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howlin P., Savage S., Moss P., Tempier A., Rutter M. Cognitive and language skills in adults with autism: a 40‐year follow‐up. JCPP (J. Child Psychol. Psychiatry) 2014;55(1):49–58. doi: 10.1111/jcpp.12115. [DOI] [PubMed] [Google Scholar]
- Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., Somekh E. Behavioral and emotional disorders in children during the COVID-19 epidemic. J. Pediatr. 2020;221:264. doi: 10.1016/j.jpeds.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman A.S., Kaufman N.L. 1983. K-ABC: Kaufman Assessment Battery for Children: Interpretive Manual. American Guidance Service. [Google Scholar]
- Kirby T. Efforts escalate to protect homeless people from COVID-19 in UK. Lancet Respir. Med. 2020;8(5):447–449. doi: 10.1016/S2213-2600(20)30160-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landa R. Early communication development and intervention for children with autism. Ment. Retard. Dev. Disabil. Res. Rev. 2007;13(1):16–25. doi: 10.1002/mrdd.20134. [DOI] [PubMed] [Google Scholar]
- Lansing M.D., Marcus L.M., Reichler R.J., Schopler E., Willaye E. PEP-3 Profil psycho-éducatif: psychoeducational profile. De Boeck Supérieur. 2010 [Google Scholar]
- Lord C., Rutter M., DiLavore P., Risi S., Gotham K., Bishop S. 2012. Autism Diagnostic Observation Schedule, (ADOS-2) Modules; pp. 1–4. [Google Scholar]
- Mazurek M.O., Dovgan K., Neumeyer A.M., Malow B.A. Course and predictors of sleep and co-occurring problems in children with autism spectrum disorder. J. Autism Dev. Disord. 2019;49(5):2101–2115. doi: 10.1007/s10803-019-03894-5. [DOI] [PubMed] [Google Scholar]
- Meier S.M., Petersen L., Schendel D.E., Mattheisen M., Mortensen P.B., Mors O. Obsessive-compulsive disorder and autism spectrum disorders: longitudinal and offspring risk. PloS One. 2015;10(11) doi: 10.1371/journal.pone.0141703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narzisi A. Handle the autism spectrum condition during coronavirus (COVID-19) stay at home period: ten tips for helping parents and caregivers of young children. Brain Sci. 2020;10(4) doi: 10.3390/brainsci10040207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés M., Morales A., Delveccio E., Mazzeschi C., Espada J.P. 2020. Immediate Psychological Effects of COVID-19 Quarantine in Youth from Italy and Spain. Available at: SSRN 3588552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the covid-19 pandemic. N. Engl. J. Med. 2020;383(6):510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Pisano L., Galimi D., Cerniglia L. 2020. A Qualitative Report on Exploratory Data on the Possible Emotional/behavioral Correlates of Covid-19 Lockdown in 4-10 Years Children in Italy. [Google Scholar]
- Qiao C.H., Wang L.Z., Lin J.R., Yao X.T., Chen G., Yao Y. 2020. A Survey Analysis of Psychological Impact on Chinese during Quarantine against COVID-19. [Google Scholar]
- Rattaz C., Munir K., Michelon C., Picot M.C., Baghdadli A. School inclusion in children and adolescents with autism spectrum disorders in France: report from the ELENA French cohort study. J. Autism Dev. Disord. 2020;50(2):455–466. doi: 10.1007/s10803-019-04273-w. [DOI] [PubMed] [Google Scholar]
- Rubin G.J., Wessely S. The psychological effects of quarantining a city. Br. Med. J. Int. Ed. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- Saurabh K., Ranjan S. Compliance and psychological impact of quarantine in children and adolescents due to covid-19 pandemic. Indian J. Pediatr. 2020;1 doi: 10.1007/s12098-020-03347-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow S.S., Cicchetti D.V., Balla D.A., Doll E.A. 2005. Vineland Adaptive Behavior Scales: Survey Forms Manual. American Guidance Service. [Google Scholar]
- Spinelli M., Lionetti F., Pastore M., Fasolo M. Parents' stress and children's psychological problems in families facing the COVID-19 outbreak in Italy. Front. Psychol. 2020;11(1713) doi: 10.3389/fpsyg.2020.01713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G., Silman M. Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med. Public Health Prep. 2013;7(1):105–110. doi: 10.1017/dmp.2013.22. [DOI] [PubMed] [Google Scholar]
- Wechsler D. vol. 22. NCS Pearson; San Antonio, TX: 2008. p. 498. (Wechsler Adult Intelligence Scale–Fourth Edition (WAIS–IV)). [Google Scholar]
- Wechsler D. NCS Pearson; Incorporated: 2014. WISC-V: Administration and Scoring Manual. [Google Scholar]
- Wechsler D. ECPA; 2014. WPPSI-IV, échelle d'intelligence de Wechsler pour enfants. [Google Scholar]
- World Health Organization . 2020. Mental Health and Psychosocial Considerations during the COVID-19 Outbreak, 18 March 2020. World Health Organization. [Google Scholar]
- Yan B., Huang Y. 2020. Prevalence and Risk Factors of Psychological Impacts Among the Quarantined Population during the COVID-19 Pandemic in China. Available at Research Square. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.