Abstract
Objective:
To develop models to predict vaginal delivery in low-risk, nulliparous women contemplating elective induction of labor or expectant management at 39 weeks of gestation.
Methods:
We conducted a secondary analysis of a randomized controlled trial of planned elective induction of labor at 39 weeks versus expectant management for low-risk nulliparous women. Two groups were included for this analysis: 1) women who were randomized to the induction of labor group and underwent elective induction at 39 0/7-39 4/7 weeks of gestation and 2) women who were randomized to the expectant management group who experienced spontaneous labor or medically indicated delivery (including postdates). Multivariable logistic regression models were developed for each group using patient characteristics that would be available at the time of counseling. Model selection was based on k-fold cross-validation using backward elimination and variables that remained significant at p<0.05 were retained. In order to compare estimated with observed rates, the elective induction of labor model was then applied to each woman in both groups to estimate individualized predicted probabilities of vaginal delivery with elective induction of labor.
Results:
Of 6,106 women enrolled in the trial, 4,661 met criteria for this analysis. Vaginal delivery occurred in 80.6% of the 2,153 women in the elective induction of labor group and 77.2% of the 2,508 women in the expectant management group (p=0.005). The final elective induction of labor model included age, height, weight, and modified Bishop score (area under the receiver operating characteristic curve = 0.72 (95%CI 0.70-0.75)). The same variables were included in the final expectant management model (area under the curve = 0.70 (95%CI 0.67-0.72)). Across the range of predicted probability deciles derived from the elective induction of labor model, almost all women who underwent elective induction of labor at 39 weeks had a higher observed chance of vaginal delivery than expectant management.
Conclusions:
Irrespective of the individual predicted chance of vaginal delivery from elective induction of labor at 39 weeks, vaginal delivery is generally more frequent if elective induction of labor is undertaken rather than expectant management. These data can be used to counsel nulliparous women regarding their “customized” chances of vaginal delivery as they choose between elective induction of labor or expectant management at 39 weeks of gestation.
Clinical Trial Registration:
Précis:
Vaginal delivery is more frequent with induction of labor compared with expectant management in low-risk nulliparous women across a range of age, weight, height, and modified Bishop score combinations.
Induction of labor is common in the United States, with almost a quarter of women with singleton pregnancies undergoing induction of labor in 2012.1 In addition, the recently completed ARRIVE trial (A Randomized Trial of Induction Versus Expectant Management) demonstrated a reduction in cesarean delivery with no increase in adverse perinatal outcomes after elective induction of labor in low risk nulliparous women at 39 weeks of gestation compared with expectant management.2 Since some women desire induction of labor,3 the practice is likely to increase.
Although most studies show an increased likelihood of vaginal delivery with induction compared with expectant management,2–6 many factors are associated with the chance for vaginal delivery with induction of labor. Examples include body mass index (BMI), maternal age and the cervical Bishop score7–10 Women and their health care professionals desire to know their customized chance of achieving a vaginal delivery in order to facilitate patient counseling and shared decision making. Thus, we used granular data from the ARRIVE trial to develop models to predict an individual nulliparous woman’s chance of vaginal delivery with an elective induction of labor at 39 weeks’ gestation compared with expectant management.
Methods
This is a secondary analysis of the ARRIVE randomized trial undertaken from 2014-2017 by the Maternal–Fetal Medicine Units Network of the Eunice Kennedy Shriver National Institute of Child Health and Human Development of planned induction of labor at 39 weeks versus expectant management. Full details of the methods of this trial have been described previously.2 Briefly, women eligible for the trial were low-risk nulliparous women with a singleton pregnancy, no contraindications to vaginal delivery or plans for cesarean delivery, and a reliably dated gestation. Length of gestation was considered to be reliable if the woman was certain of the date of her last menstrual period and that date was consistent with results of ultrasonography performed before 21 0/7 weeks or if the date of the last menstrual period was uncertain but results were available from ultrasonography performed before 14 0/7 weeks. Consenting women were randomized between 38 0/7 and 38 6/7 weeks of gestation to either induction of labor at 39 0/7 to 39 4/7 weeks or expectant management (i.e., foregoing elective delivery before 40 5/7 weeks unless a medical indication arose and to have delivery initiated no later than 42 2/7 weeks). The study was approved by the institutional review board at each hospital, and each participant gave written informed consent.
Two groups were included for this analysis: 1) women who were randomized to the induction of labor group and underwent elective induction 39 0/7 – 39 4/7 weeks of gestation and 2) women who were randomized to the expectant management group who experienced spontaneous labor or medically indicated delivery (including postdates) on or after 39 0/7. Women who were lost to follow-up or withdrew consent (i.e., had missing delivery data), or who delivered prior to 39 0/7 weeks gestation in both groups were excluded from this analysis. Women in the induction of labor group were excluded if they were not electively induced 39 0/7 - 39 4/7. Women in the expectant management group were excluded if they were induced without a medical indication before 40 5/7 or if they had an elective cesarean without labor. Descriptive analyses used the χ2 or Fisher’s exact test for categorical variables and the Wilcoxon rank sum test for continuous variables.
Multivariable logistic regression models with the outcome of vaginal delivery were developed for each group (induction of labor and expectant management) using patient characteristics that would be available at the time of counseling. Eligible variables included maternal age, height, weight at first clinic visit, weight at randomization, average weight change per week (randomization weight minus first clinic weight divided by weeks of gestation between measurements), body mass index at randomization, smoking, previous pregnancy loss (<20 weeks), assisted conception (in vitro fertilization, ovulation induction, or artificial insemination), and modified Bishop score at randomization (score ranges from 0-12) and its components (dilation, effacement, and station).
Linear and quadratic terms were evaluated for continuous variables. Model selection and internal validation was performed using k-fold cross-validation.11 Each group was randomly divided into 10 roughly equal parts (± 1 participant). Using backward elimination, a logistic regression model was chosen for each subset of 9 of the 10 parts, with variables significant at p<0.05. Validation for each of the 10 models was determined from the 1/10th part of the cohort that was not included in fitting each particular model. The final model for each group was the model with the highest area under the receiver operating characteristic curve (AUC) in the validation set, with the additional requirement that variables were present in at least 8 of the 10 models. For each of the final models, the AUC was estimated to characterize the classification ability of the models (0.5 was considered no better than chance, >0.5 to <0.7 poor, ≥0.7 to <0.8 acceptable, ≥0.8 to <0.9 excellent, ≥0.9 outstanding)11 and the Hosmer–Lemeshow test was used to evaluate model goodness of fit.
In order to describe the probability of vaginal delivery among those in the induction of labor group and the expectant management group across various patient characteristics and combinations, random scenarios of characteristics (significant variables in the final models) were chosen such that at least 2% of the cohort fit each scenario. For each scenario, the percent probability and Wald-test-based confidence limits of vaginal delivery if induced was estimated based on the elective induction of labor model and the percent probability and Wald-test-based confidence limits of vaginal delivery if expectantly managed was estimated. A model with both groups combined was used to estimate a p-value for the difference in the percent probability of vaginal delivery between elective induction of labor and expectant management.
In order to compare estimated with observed rates, the induction of labor model was then applied to each woman in both groups to estimate individualized predicted probabilities of vaginal delivery with induction of labor. Deciles of predicted probabilities of vaginal delivery associated with induction of labor were then plotted against the actual frequency of vaginal delivery observed in each group using locally weighted scatterplot smoothing.
We chose not to include race or ethnicity in the models owing to the increasing difficulty in categorizing individuals, the socially determined nature of those categories, and the related difficulty of using the model in other populations. However, we performed a sensitivity analysis that included socially-determined variables of race/ethnicity, insurance status, and employment status. No imputation for missing values was performed. A p-value < 0.05 was used to define statistical significance, and all tests were two tailed. Analyses were performed with SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
Of 6106 women who were randomized, 4661 met inclusion criteria for this analysis (2153 in the induction of labor group and 2508 in the expectant management group) (Figure 1). Among women with delivery onset on or after 39 0/7 weeks of gestation, those included in this analysis were generally similar to those excluded although some differences are noted (Appendix 2, available online at http://links.lww.com/xxx). Women excluded from analysis, for example, were slightly shorter and more likely Hispanic in both groups.
Figure 1.
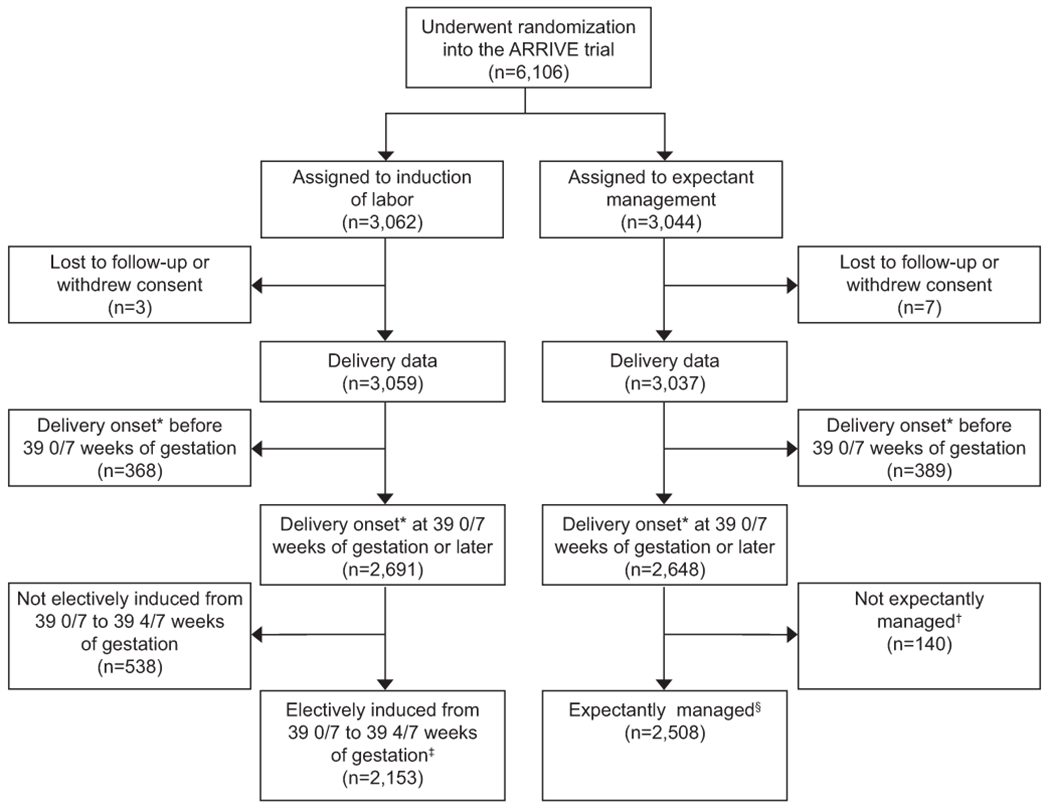
Flow diagram of the study population. *Onset defined as when the process of delivery started. †Women assigned to expectant management were excluded if an induction without a medical indication was initiated before 40 5/7 weeks of gestation or if they had an elective cesarean delivery without labor. ‡Induced, reason for induction was elective, and induction started 39 0/7 to 39 4/7 weeks of gestation (cervical ripening or oxytocin, whichever came first). §Spontaneous labor or medically indicated delivery on and after 39 0/7 weeks of gestation. ARRIVE, A Randomized Trial of Induction Versus Expectant Management.
Vaginal delivery occurred in 80.6% (95%CI 78.9%-82.3%) of the induction of labor group and 77.2% (95%CI 75.6%-78.8%) in the expectant management group (p=0.005). Characteristics by group and by delivery mode are shown in Table 1. For both groups, the k-fold cross- validation identified the following patient characteristics to be significantly associated with vaginal delivery: age, height, weight at randomization, and modified Bishop score at randomization. The area under the ROC curve (AUC) in the best validation sub-sample was 0.78 in the induction of labor group and 0.73 in the expectant management group. When these variables were applied to the entire sample size in each group, the AUC was 0.72 (95%CI 0.70-0.75) in the induction of labor final model and 0.70 (95%CI 0.67-0.72) in the expectant management final model. Model fit was good in each group’s final model (Hosmer-Lemeshow p-values were 0.62 and 0.24, respectively, with graphical displays of the observed and expected number of patients in each partition of the Hosmer-Lemeshow test shown in Appendix 3 [parts A-D], available online at http://links.lww.com/xxx). The final multivariable models in each group are presented in Table 2.
Table 1.
Baseline characteristics eligible for multivariable analysis, by group and by mode of delivery
| Elective induction of labor at 39 0/7-39 4/7 weeks n=2153 | Expectant management n=2508 |
|||||
|---|---|---|---|---|---|---|
| Delivery mode | P* | Delivery mode | P* | |||
| Vaginal n=1735 | Cesarean n=418 | Vaginal n=1936 | Cesarean n=572 | |||
| Age, yrs | 23 (20-28) | 25 (21-30) | <0.001 | 23 (20-28) | 25 (21-30) | <0.001 |
| BMI at randomization† | 30.1 (27.0-34.0) | 32.9 (29.6-38.2) | <0.001 | 29.8 (26.9-34.0) | 32.6 (28.6-37.7) | <0.001 |
| Height, m† | 1.63 (1.60-1.68) | 1.60 (1.55-1.65) | <0.001 | 1.63 (1.57-1.68) | 1.60 (1.57-1.65) | <0.001 |
| Weight at first clinic, kg† | 66 (58-78) | 71 (60-86) | <0.001 | 66 (57-78) | 71 (59-86) | <0.001 |
| Weight at randomization, kg† | 80 (71-93) | 85 (74-100) | <0.001 | 79 (70-91) | 86 (73-99) | <0.001 |
| Weight change per week from first clinic visit to randomization, kg† | 0.47 (0.36-0.60) | 0.49 (0.36-0.62) | 0.39 | 0.48 (0.36-0.61) | 0.48 (0.35-0.64) | 0.48 |
| Smoked cigarettes | 120 (6.9) | 33 (7.9) | 0.48 | 155 (8.0) | 47 (8.2) | 0.87 |
| Previous pregnancy loss | 388 (22.4) | 87 (20.8) | 0.49 | 479 (24.7) | 169 (29.6) | 0.02 |
| Assisted conception | 47 (2.7) | 17 (4.1) | 0.14 | 39 (2.0) | 22 (3.9) | 0.01 |
| Modified Bishop score at randomization† | 4 (2-5) | 3 (2-4) | <0.001 | 4 (2-5) | 3 (2-4) | <0.001 |
| Station score at randomization† | 0.007 | <0.001 | ||||
| 0 (includes floating or ballottable) | 894 (51.5) | 246 (58.9) | 1003 (51.8) | 369 (64.5) | ||
| 1 | 687 (39.6) | 150 (35.9) | 757 (39.1) | 181 (31.6) | ||
| 2+ | 154 (8.9) | 22 (5.3) | 175 (9.0) | 22 (3.9) | ||
| Dilation score at randomization† | <0.001 | <0.001 | ||||
| 0 | 667 (38.4) | 229 (54.8) | 740 (38.2) | 309 (54.0) | ||
| 2+ | 1068 (61.6) | 189 (45.2) | 1195 (61.8) | 263 (46.0) | ||
| Length score at randomization†‡ | 0.29 | 0.33 | ||||
| 0 | 16/97 (16.5) | 8/33 (24.2) | 20/98 (20.4) | 6/35 (17.1) | ||
| 1 | 40/97 (41.2) | 12/33 (36.4) | 37/98 (37.8) | 16/35 (45.7) | ||
| 2 | 32/97 (33.0) | 7/33 (21.2) | 32/98 (32.7) | 7/35 (20.0) | ||
| 3 | 9/97 (9.3) | 6/33 (18.2) | 9/98 (9.2) | 6/35 (17.1) | ||
| Effacement score at randomization†‡ | <0.001 | <0.001 | ||||
| 1 | 406/1638 (24.8) | 142/385 (36.9) | 445/1837 (24.2) | 187/537 (34.8) | ||
| 2 | 1073/1638 (65.5) | 216/385 (56.1) | 1194/1837 (65.0) | 314/537 (58.5) | ||
| 3 | 159/1638 (9.7) | 27/385 (7.0) | 198/1837 (10.8) | 36/537 (6.7) | ||
| Length or effacement score at randomization†‡ | <0.001 | <0.001 | ||||
| 0-1 | 462 (26.6) | 162 (38.8) | 502 (25.9) | 209 (36.5) | ||
| 2 | 1105 (63.7) | 223 (53.4) | 1226 (63.4) | 321 (56.1) | ||
| 3 | 168 (9.7) | 33 (7.9) | 207 (10.7) | 42 (7.3) | ||
Data are median (interquartile range) or n (%) unless otherwise specified.
Based on the χ2 test for categorical variables and the Wilcoxon rank sum test for continuous variables.
BMI missing in 9 in elective induction of labor (eIOL) group and 16 in expectant management (EM) group; height missing in 9 in eIOL group and 15 in EM group; weight at first clinic visit and weight change missing in 1 in eIOL group and 5 in EM group; weight at randomization missing in 2 in EM group; Bishop score (and its components) missing in 1 in EM group.
Patients had either effacement or length recorded.
Table 2.
Multivariable models for vaginal delivery, by group
| Baseline characteristics | Elective induction of labor at 39 0/7-39 4/7 weeks | Expectant management |
|---|---|---|
| OR (95% CI)* | OR (95% CI)* | |
| Age, yrs (per 5 yr increase) | 0.71 (0.64-0.79) | 0.71 (0.65-0.78) |
| Height, m (per 0.05 m increase) | 1.54 (1.42-1.68) | 1.35 (1.25-1.45) |
| Weight at randomization (38 weeks), kg (per 10 kg increase) | 0.77 (0.72-0.82) | 0.80 (0.75-0.84) |
| Modified Bishop score at randomization (38 weeks) (per 1 score increase) | 1.24 (1.16-1.32) | 1.24 (1.17-1.31) |
OR, odds ratio; CI, confidence interval.
All variables were significant at p<0.001.
Table 3 shows the probability of vaginal delivery among those in the induction of labor group and the expectant management group across various patient characteristics and combinations, and is sorted by the difference in these probabilities. Of 50 possible scenarios that each fit at least 2% of the cohort, the probability of vaginal delivery was higher for elective induction of labor compared with expectant management in all but one scenario, in which there was a 0.1 difference in the percent probability of vaginal delivery between the two groups. Of the six scenarios either favoring expectant management (n = 1) or when the elective induction of labor had a minimally (<1%) higher chance of vaginal birth (n = 5), all occurred in relatively shorter women (<1.57 meters; < 5.15 feet). The equations to determine the probability of vaginal birth for an individual low-risk nulliparous pregnancy at 39 weeks of gestation with elective induction of labor and with expectant management are provided in Appendix 4, available online at http://links.lww.com/xxx. Required data include maternal age, height, weight, and modified Bishop score at 38 weeks of gestation. Inclusion of socially-determined variables such as race and ethnicity in the multivariable analysis did not change the strength of association for age, height, weight or modified Bishop score.
Table 3.
Examples of customized probabilities for vaginal birth with elective induction of labor (eIOL) and expectant management (EM), based on their group-specific model
| Example | Age (yrs) | Height (m) | Weight at randomization (38 weeks) (kg) | Modified Bishop score at randomization (38 weeks) | Percent of women with these same characteristics* | Percent probability of vaginal delivery if induced (based on eIOL model)† | Percent probability of vaginal delivery if expectantly managed (based on EM model)† | Difference in percent probably of vaginal delivery between eIOL and EM |
|---|---|---|---|---|---|---|---|---|
| 1 | 28 | 1.52 | 71.01 | 4 | 2.90 | 70.1 (65.5-74.3) | 70.2 (66.1-74.0) | −0.1 |
| 2 | 23 | 1.56 | 100.83 | 1 | 2.38 | 53.0 (47.1-58.9) | 52.9 (47.5-58.1) | 0.2 |
| 3 | 31 | 1.52 | 67.32 | 3 | 2.08 | 63.0 (57.1-68.5) | 62.8 (57.7-67.6) | 0.2 |
| 4 | 25 | 1.53 | 63.90 | 5 | 3.22 | 82.4 (78.9-85.5) | 81.7 (78.5-84.5) | 0.7 |
| 5 | 20 | 1.55 | 78.19 | 6 | 4.14 | 87.0 (83.8-89.7) | 86.3 (83.4-88.8) | 0.7 |
| 6 | 30 | 1.54 | 73.04 | 4 | 3.30 | 69.8 (65.2-74.0) | 68.9 (64.8-72.7) | 0.9 |
| 7 | 30 | 1.55 | 81.75 | 3 | 3.09 | 61.8 (57.2-66.3) | 60.9 (56.7-64.8) | 1.0 |
| 8 | 27 | 1.54 | 65.93 | 5 | 3.71 | 80.9 (77.2-84.1) | 79.8 (76.5-82.7) | 1.1 |
| 9 | 22 | 1.57 | 84.06 | 6 | 4.85 | 85.6 (82.5-88.3) | 84.5 (81.5-87.0) | 1.2 |
| 10 | 21 | 1.59 | 67.28 | 6 | 5.56 | 92.2 (90.0-93.9) | 90.6 (88.5-92.3) | 1.6 |
| 11 | 19 | 1.57 | 83.92 | 2 | 6.11 | 75.7 (71.9-79.1) | 74.0 (70.5-77.1) | 1.7 |
| 12 | 28 | 1.58 | 96.19 | 3 | 2.85 | 62.3 (58.4-66.1) | 60.5 (56.9-64.1) | 1.8 |
| 13 | 31 | 1.58 | 96.32 | 2 | 2.25 | 52.0 (46.6-57.4) | 50.2 (45.4-55.0) | 1.9 |
| 14 | 19 | 1.61 | 107.20 | 5 | 2.70 | 82.0 (78.0-85.4) | 80.1 (76.3-83.5) | 1.9 |
| 15 | 21 | 1.67 | 69.01 | 6 | 5.43 | 95.7 (94.3-96.8) | 93.7 (92.0-95.0) | 2.0 |
| 16 | 19 | 1.69 | 83.44 | 6 | 3.86 | 95.5 (93.9-96.6) | 93.2 (91.4-94.7) | 2.2 |
| 17 | 21 | 1.72 | 78.50 | 6 | 3.18 | 96.4 (95.1-97.4) | 94.2 (92.5-95.5) | 2.3 |
| 18 | 19 | 1.62 | 115.91 | 4 | 2.06 | 76.2 (71.2-80.6) | 73.9 (69.2-78.1) | 2.3 |
| 19 | 20 | 1.60 | 75.99 | 4 | 10.86 | 87.7 (85.6-89.5) | 85.4 (83.3-87.2) | 2.3 |
| 20 | 18 | 1.63 | 90.43 | 5 | 4.66 | 90.0 (87.7-91.9) | 87.7 (85.3-89.7) | 2.3 |
| 21 | 32 | 1.57 | 68.10 | 4 | 2.98 | 74.8 (70.3-78.9) | 72.1 (68.0-75.8) | 2.8 |
| 22 | 21 | 1.68 | 77.72 | 5 | 8.05 | 94.0 (92.5-95.3) | 91.3 (89.5-92.8) | 2.8 |
| 23 | 28 | 1.57 | 64.98 | 2 | 3.18 | 73.4 (69.3-77.2) | 70.3 (66.5-73.9) | 3.1 |
| 24 | 19 | 1.71 | 69.65 | 3 | 2.55 | 95.0 (93.3-96.2) | 91.8 (89.6-93.6) | 3.2 |
| 25 | 29 | 1.60 | 91.24 | 3 | 3.43 | 67.6 (64.3-70.8) | 64.4 (61.3-67.3) | 3.3 |
| 26 | 26 | 1.59 | 79.41 | 2 | 5.71 | 72.1 (69.0-75.0) | 68.8 (65.9-71.5) | 3.3 |
| 27 | 22 | 1.66 | 94.49 | 5 | 6.59 | 88.9 (86.7-90.7) | 85.5 (83.3-87.5) | 3.3 |
| 28 | 26 | 1.74 | 80.67 | 5 | 4.38 | 94.6 (92.9-95.9) | 90.9 (88.7-92.7) | 3.7 |
| 29 | 29 | 1.70 | 83.01 | 6 | 2.79 | 92.1 (89.9-93.9) | 88.2 (85.7-90.4) | 3.9 |
| 30 | 25 | 1.61 | 62.64 | 2 | 4.10 | 83.6 (80.6-86.2) | 79.5 (76.4-82.3) | 4.0 |
| 31 | 20 | 1.69 | 86.43 | 3 | 6.24 | 90.5 (88.5-92.2) | 86.4 (84.0-88.4) | 4.1 |
| 32 | 27 | 1.72 | 97.44 | 6 | 2.06 | 91.7 (89.3-93.5) | 87.5 (84.7-89.8) | 4.2 |
| 33 | 23 | 1.74 | 77.55 | 3 | 3.52 | 93.8 (92.0-95.3) | 90.0 (87.0-91.6) | 4.3 |
| 34 | 30 | 1.60 | 79.55 | 1 | 3.26 | 63.3 (58.1-68.2) | 58.9 (54.3-63.4) | 4.4 |
| 35 | 24 | 1.63 | 102.56 | 1 | 2.66 | 64.9 (60.0-69.5) | 60.4 (56.0-64.7) | 4.5 |
| 36 | 22 | 1.71 | 69.79 | 2 | 2.85 | 92.5 (90.3-94.2) | 88.0 (85.1-90.4) | 4.5 |
| 37 | 30 | 1.69 | 71.32 | 4 | 4.36 | 89.9 (87.5-91.9) | 84.9 (82.1-87.3) | 5.0 |
| 38 | 33 | 1.64 | 99.14 | 3 | 2.12 | 64.7 (59.7-69.4) | 59.3 (54.9-63.7) | 5.4 |
| 39 | 33 | 1.65 | 73.65 | 4 | 3.67 | 82.8 (79.2-85.9) | 77.4 (73.9-80.6) | 5.4 |
| 40 | 23 | 1.65 | 85.78 | 1 | 5.28 | 78.5 (74.9-81.7) | 73.0 (69.3-76.3) | 5.5 |
| 41 | 31 | 1.68 | 88.09 | 4 | 4.05 | 83.1 (80.2-85.7) | 77.2 (74.2-79.9) | 5.9 |
| 42 | 30 | 1.74 | 87.78 | 4 | 3.48 | 89.9 (87.4-92.0) | 83.9 (80.8-86.5) | 6.0 |
| 43 | 32 | 1.66 | 82.36 | 3 | 4.14 | 78.3 (74.8-81.5) | 72.0 (68.6-75.2) | 6.3 |
| 44 | 27 | 1.73 | 94.46 | 3 | 3.41 | 87.2 (84.6-89.4) | 80.7 (77.7-83.3) | 6.5 |
| 45 | 22 | 1.70 | 95.27 | 1 | 2.70 | 82.5 (78.7-85.7) | 75.8 (71.7-80.0) | 6.7 |
| 46 | 28 | 1.66 | 79.24 | 1 | 3.30 | 77.0 (72.9-80.7) | 70.3 (66.2-74.1) | 6.8 |
| 47 | 31 | 1.72 | 82.06 | 3 | 2.90 | 86.8 (83.7-89.3) | 79.9 (76.4-83.0) | 6.9 |
| 48 | 32 | 1.70 | 98.83 | 3 | 2.25 | 76.9 (72.8-80.5) | 69.2 (65.2-73.0) | 7.7 |
| 49 | 33 | 1.73 | 84.09 | 3 | 2.17 | 85.6 (81.9-88.6) | 77.8 (73.7-81.5) | 7.7 |
| 50 | 28 | 1.71 | 88.73 | 1 | 2.47 | 80.2 (76.0-83.8) | 72.0 (67.5-76.1) | 8.2 |
Bold indicates differences with p< 0.05 (based on a model with both eIOL and EM groups combined).
Percent of woman in the group with the same age ± 3 years, same height ± 0.07 m, same weight at 38 weeks of gestation ± 13 kg and same modified Bishop score at 38 weeks of gestation ± 1.
The equations to determine the probability of vaginal birth for an individual low-risk nulliparous pregnancy at 39 weeks of gestation with eIOL and with EM are provided in Appendix 4 (http://links.lww.com/xxx).
Across the range of predicted probability deciles derived from the elective induction of labor model, women who underwent elective induction of labor at 39 weeks had a higher observed chance of vaginal delivery than those who actually underwent expectant management (Figure 2).
Figure 2.
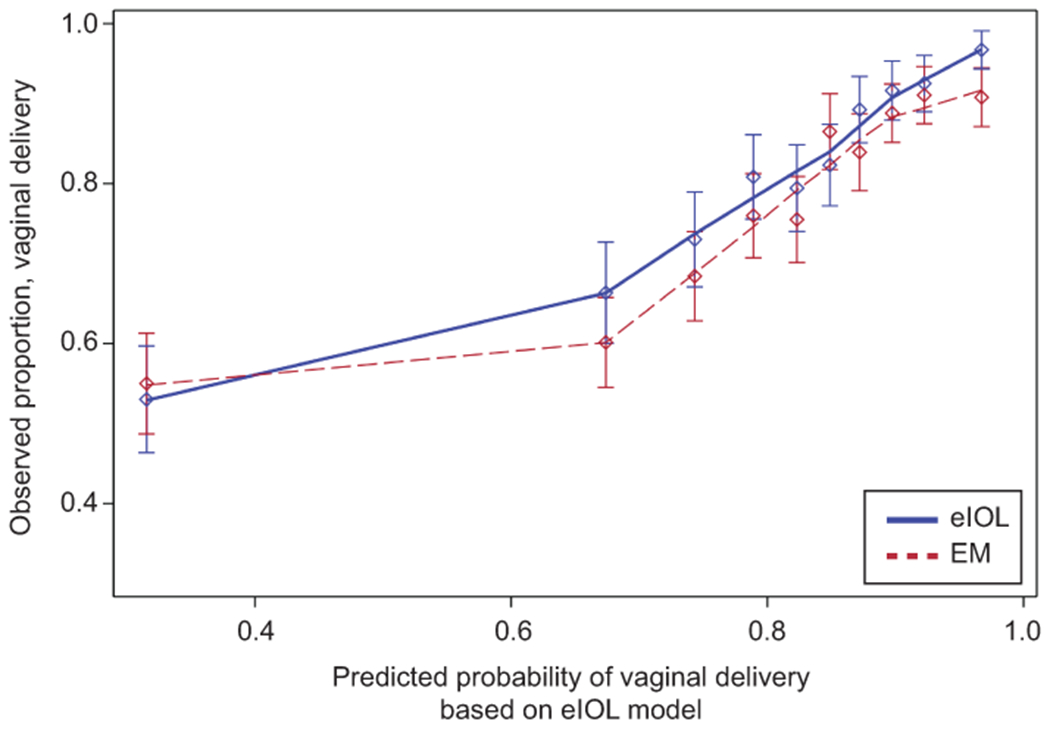
Observed and predicted* percent of women experiencing vaginal delivery for women undergoing either elective induction of labor (eIOL) at 39 weeks of gestation or expectant management (EM). *The predicted probability of vaginal delivery (%) for each decile was based on the eIOL model and cut-points were as follows: decile 1, <63.1; decile 2, 63.1–71.6; decile 3, 71.7–76.9: decile 4, 77.0–80.7; decile 5, 80.8–83.7; decile 6, 83.8–85.9; decile 7, 86.0–88.3; decile 8, 88.4–91.0; decile 9, 91.1–93.3; decile 10: ≥93.4.
Discussion
Most low-risk nulliparous women had an increased chance of vaginal delivery with elective induction of labor at 39 weeks compared with expectant management across a wide variety of characteristics (age, height, weight and modified Bishop score). These findings are consistent with observations of overall group comparisons in other randomized trials.13–15 However, our data expand on these studies by assessing the odds of vaginal delivery in elective induction of labor and expectant management over a wide range of attributes.
As expected, younger maternal age and higher Bishop scores were associated with an increased chance of vaginal delivery both in women undergoing elective induction of labor and expectant management, although rates were consistently higher with elective induction of labor. Others also have noted higher Bishop scores to be associated with successful induction of labor.7–10,16,17 The same is true for younger maternal age.9,16,18 An association between decreased BMI and vaginal delivery has been observed as well.8,16,18 However, results have been mixed for maternal height and weight as independent predictors of vaginal delivery.8,16 We noted increased height and decreased weight to be associated with vaginal delivery, which are reflected in the probabilities in Table 3.
Induction of labor was associated with a higher chance of vaginal delivery than expectant management across nearly all of the scenarios and conditions, echoing one of the primary findings of the ARRIVE trial. This is illustrated in Figure 2. However, many women use absolute rather than relative risks in order to facilitate making medical decisions. For example, they might consider expectant management to be preferable to elective induction of labor if they have an 80% chance of success with expectant management, even if the chances are slightly higher (e.g. 82%) with elective induction of labor. In contrast, they may prefer elective induction of labor if the chance of success is only 40% with expectant management. Being able to give women reasonably precise chances for vaginal delivery with either induction of labor or expectant management can inform shared decision-making and patient centered medicine. This is especially important when considering elective induction of labor versus expectant management at 39 weeks of gestation because in most cases outcomes are excellent with both strategies.
Our study had important limitations. It was conducted during a narrow gestational age window in women with precise gestational dating. Also, most hospitals had teams of clinicians including obstetrics and gynecology residents and medical students involved in intrapartum care and pregnancies with serious medical or obstetric conditions were excluded. Further, there was potential bias in who consented to study participation. In addition, although we used a pragmatic design, the RCT setting is artificial. Accordingly, these data differ from those used to generate the VBAC success calculator, which is based on an observational cohort. Taken together, results are not generalizable beyond low-risk nulliparous women. In addition, some data that might have improved the model were unavailable such as estimated fetal weight. External validation and the addition of variables may improve the model and facilitate generalizability.
One of the factors most strongly associated with successful vaginal delivery after induction of labor is prior vaginal delivery.18 However, this was not applicable to our dataset, since only nulliparous women were studied. Indeed, nulliparity is associated with decreased success of induction (relative to multiparas with prior vaginal birth)8 and success rates are very high after induction in women with prior vaginal delivery.19,20 Similarly, medical and obstetric problems such as diabetes, chronic hypertension and known fetal growth restriction have all been linked to decreased chances of vaginal birth after induction.7,16,17 As with multiparity, these were all exclusions for our study and accordingly these factors cannot be evaluated in our model and serve as an additional limitation.
There were also numerous strengths of the analysis. The study was conducted in a large number of hospitals including both university and private settings. There was considerable racial, ethnic and geographic diversity among the population and a large number of women were studied. Induction protocols, labor management, and decisions as to when to perform cesarean deliveries were at the discretion of the health care professionals. Accordingly, results are not limited to only one induction strategy and our data reflect the “real world” conditions of a pragmatic trial.
In summary, irrespective of the individual predicted chance of vaginal delivery from elective induction of labor at 39 weeks, the actual occurrence of vaginal delivery is generally more frequent if elective induction of labor is undertaken rather than expectant management. Given the variance in individual feelings and beliefs about labor induction, these data can be used to counsel nulliparous women regarding their “patient centered” chances of vaginal delivery as they choose between elective induction of labor or expectant management at 39 weeks of gestation.
Supplementary Material
Authors’ Data Sharing Statement.
Will individual participant data be available (including data dictionaries)? Yes.
What data in particular will be shared? Individual de-identified data on all of the randomized participants, including baseline characteristics, details of delivery, pregnancy and neonatal outcomes and adverse events. Data may be truncated or combined to ensure confidentiality and privacy.
What other documents will be available? Other documents include the original data forms, the study protocol, a comprehensive data dictionary including variable names, formats, definitions and whether the variable has been recoded and how. Explanatory notes are also included.
When will data be available (start and end dates)? Data will be available by 3/2021 through NICHD Data and Specimens Hub (DASH), assuming IRB approval.
By what access criteria will data be shared (including with whom, for what types of analyses, and by what mechanism)? Terms and conditions for access are given at https://dash.nichd.nih.gov/.
Acknowledgements:
The authors thank Lindsay Doherty, M.S. for data and study management and Vinay Bhandaru, M.S. for statistical programming.
Funding: Supported by grants (HD40512, HD36801, HD27869, HD34208, HD68268, HD40485, HD40500, HD53097, HD40560, HD40545, HD27915, HD40544, HD34116, HD68282, HD87192, HD68258, HD87230) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) and the National Center for Advancing Translational Sciences (UL1TR001873). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Financial Disclosure
Robert M. Silver reports receiving funds from GestaVision. Edward K. Chien disclosed that money was paid to his institution from Alydia Health and Gestvision. Both were industry sponsored research projects without overlap with this study. Geeta K. Swamy disclosed receiving funds from GlaxoSmithKline, Pfizer, and SAOL. Ronald S. Gibbs disclosed that money was paid to him from Gestavision for consultation and ACI/Novavax for serving on the DSMB for a clinical trial of RSV vaccine. The other authors did not report any potential conflicts of interest.
Footnotes
A list of other members of the NICHD MFMU Network is available in Appendix 1, available online at http://links.lww.com/xxx.
Each author has confirmed compliance with the journal’s requirements for authorship.
Presented at the 2019 Annual Scientific Meeting of the Society for Maternal-Fetal Medicine, February 11-16, 2019, Las Vegas, NV.
Dr. Rouse, Associate Editor (Obstetrics) of Obstetrics & Gynecology, was not involved in the review or decision to publish this article.
Contributor Information
Robert M. Silver, Department of Obstetrics and Gynecology of University of Utah Health Sciences Center, Salt Lake City, UT
Madeline Murguia Rice, George Washington University Biostatistics Center, Washington, DC
William A. Grobman, Northwestern University, Chicago, IL
Uma M. Reddy, Eunice Kennedy Shriver National Institute of Child Health and Human Development, Bethesda, MD
Alan T.N. Tita, University of Alabama at Birmingham, Birmingham, AL
Gail Mallett, Northwestern University, Chicago, IL
Kim Hill, Department of Obstetrics and Gynecology of University of Utah Health Sciences Center, Salt Lake City, UT
Elizabeth A. Thom, George Washington University Biostatistics Center, Washington, DC
Yasser Y. El-Sayed, Stanford University, Stanford, CA
Ronald J. Wapner, Columbia University, New York, NY
Dwight J. Rouse, Brown University, Providence, RI
George R. Saade, University of Texas Medical Branch, Galveston, TX
John M. Thorp, Jr, University of North Carolina at Chapel Hill, Chapel Hill, NC
Suneet P. Chauhan, University of Texas Health Science Center at Houston-Children’s Memorial Hermann Hospital, Houston, TX
Edward K. Chien, MetroHealth Medical Center-Case Western Reserve University, Cleveland, OH
Brian M. Casey, University of Texas Southwestern Medical Center, Dallas, TX
Ronald S. Gibbs, University of Colorado School of Medicine, Anschutz Medical Campus, Aurora, CO
Sindhu K. Srinivas, University of Pennsylvania, Philadelphia, PA
Geeta K. Swamy, Duke University, Durham, NC
Hyagriv N. Simhan, University of Pittsburgh, Pittsburgh, PA
George A. Macones, Washington University, Saint Louis, MO
References
- 1.Osterman MJ, Martin JA. Recent declines in induction of labor by gestational age. NCHS Data Brief 2014;155:1–8. [PubMed] [Google Scholar]
- 2.Grobman WA, Rice MM, Reddy UM, et al. Labor induction versus expectant management in low-risk nulliaparous women. N Engl J Med 2018;379:513–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sotiriadis A, Petousis S, Thilaganathan B, et al. Maternal and perinatal outcomes after elective induction of labor at 39 weeks in uncomplicated singleton pregnancy: a meta-analysis. Ultrasound Obstet Gynecol 2019;53:26–35. [DOI] [PubMed] [Google Scholar]
- 4.Darney BG, Snowden JM, Cheng YW, et al. Elective induction of labor at term compared with expectant management: maternal and neonatal outcomes. Obstet Gynecol 2013;122:761–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stock SJ, Ferguson E, Duffy A, et al. Outcomes of elective induction of labour compared with expectant management: population based study. BMJ 2012;344:e2838.doi: 10.1136/bmj.e2838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Osmundson S, Ou-Yang RJ, Grobman WA. Elective induction compared with expectant management in nulliparous women with an unfavorable cervix. Obstet Gynecol 2011;117:583–7. [DOI] [PubMed] [Google Scholar]
- 7.Sievert RA, Kuper SG, Jauk VC, et al. Predictors of vaginal delivery in medically indicated early preterm induction of labor. Am J Obstet Gynecol 2017;217:375e1–7. [DOI] [PubMed] [Google Scholar]
- 8.Levine LD, Downes KL, Parry S, et al. A validated calculator to estimate risk of cesarean after an induction o labor with an unfavorable cervix. Am J Obstet Gynecol 2018;254e1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schuit E, Kwee A, Westerhuis ME, et al. A clinical prediction model to assess the risk of operative delivery. BJOG 2012;119:915–23. [DOI] [PubMed] [Google Scholar]
- 10.Laughon SK, Zhang J, Troendle J, Sun L, Reddy UM. Using a simplified Bishop score to predict vaginal delvery. Obstet Gynecol 2011;117:805–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kohavi R A study of cross-validation and bootstrap for accuracy estimation and model selection. IJCAI’95 Proceedings of the 14th international joint conference on artificial intelligence-Volume 2 Mellish CS, ed. San Francisco, CA: Morgan Kaufmann Publishers Inc; 1995.) [Google Scholar]
- 12.Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression, 3rd Ed. Chapter 5, John Wiley and Sons, Hoboken, NJ: (2013). [Google Scholar]
- 13.Walker KF, Bugg GJ, Macpherson M, et al. Randomized trial of labor inudction in women 35 years of age or older. N Engl J Med 2016;374:813–22. [DOI] [PubMed] [Google Scholar]
- 14.Koopmans CM, Bijlenga D, Groen H, et al. Induction of labour versus expectant monitoring for gestational hypertension or mild preeclampsia after 36 weeks gestation (HYPITAT): A multicentre, open-label randomised controlled trial. Lancet 2009;374:979–88. [DOI] [PubMed] [Google Scholar]
- 15.Boers KE, Vligen SM, Bijlenga D, et al. Induction versus expectant monotoring for intrauterine growth restriction at term: randomised equivalence trial (DIGITAT). BMJ 2010;341;c7087 Doi: 10.1136/bmj.c7087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tolcher MC, Holbert MR, Weaver AL, et al. Predicting cesarean delivery after induction of labor among nulliparous women at term. Obstet Gynecol 2015;126:1059–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mardy AH, Ananth CV, Grobman WA, Gymafi-Bannerman C. A prediction model of vaginal birth after cesarean in the preterm period. Am J Obstet Gynecol 2016;215:513e1–7. [DOI] [PubMed] [Google Scholar]
- 18.Roland C, Warshak CR, DeFranco EA. Success of labor induction for preclampsia at preterm and term gestational ages. J Perinatol 2017;37:636–40. [DOI] [PubMed] [Google Scholar]
- 19.Jacquemyn Y, michiels I, Martens G. Elective induction of labour increases caesarean section rate in low risk nulliparous women. J Obstet Gynaecol 2012;32:257–9. [DOI] [PubMed] [Google Scholar]
- 20.Heinberg EM, Wood RA, Chambers RB. Elective induction of labor in multiparous women. Does it increase the risk of cesarean section? J Reprod Med 2002;47:399–403. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


