Abstract
Ethnopharmacological relevance
The novel coronavirus disease (COVID-19) outbreak in Wuhan has imposed a huge influence in terms of public health and economy on society. However, no effective drugs or vaccines have been developed so far. Traditional Chinese Medicine (TCM) has been considered as a promising supplementary treatment of this disease due to its clinically proven performance in many severe diseases, like severe acute respiratory syndrome (SARS). Meanwhile, many reports suggest that the side-effects (SE) of TCM prescriptions cannot be ignored in treating COVID-19 as it often leads to dramatic degradation of the patients’ physical condition. Systematic evaluation of TCM regarding its latent SE becomes a burning issue.
Aim
In this study, we used an ontology-based side-effect prediction framework (OSPF) developed from our previous work and Artificial Neural Network (ANN)-based deep learning, to evaluate the TCM prescriptions officially recommended by China for the treatment of COVID-19.
Materials and methods
The OSPF developed from our previous work was implemented in this study, where an ontology-based model separated all ingredients in a TCM prescription into two categories: hot and cold. A database was created by converting each TCM prescription into a vector which contained ingredient dosages, corresponding hot/cold attribution and safe/unsafe labels. This allowed for training of the ANN model. A safety indicator (SI), as a complement to SE possibility, was then assigned to each TCM prescription. According to the proposed SI, from high to low, the recommended prescription list could be optimized. Furthermore, in interest of expanding the potential treatment options, SIs of other well-known TCM prescriptions, which are not included in the recommended list but are used traditionally to cure flu-like diseases, are also evaluated via this method.
Results
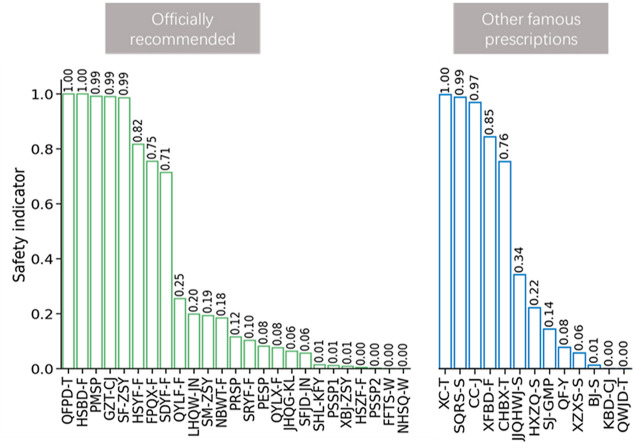
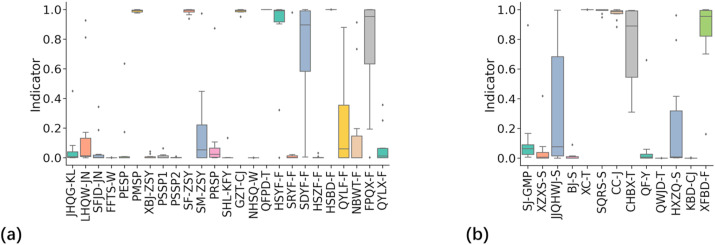
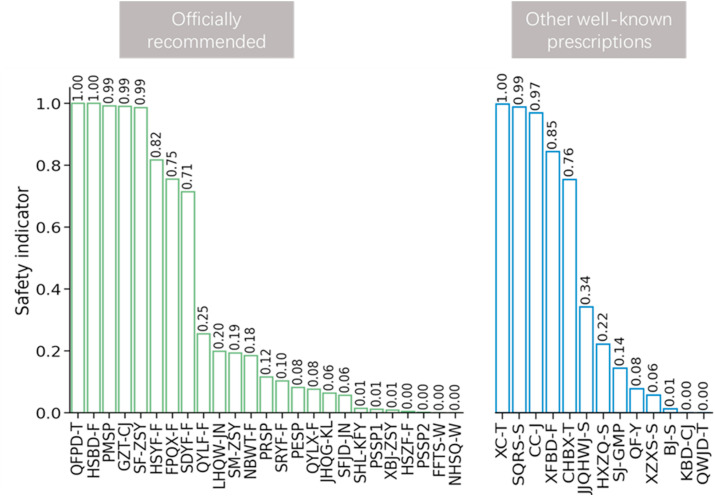
Based on SI, QFPD-T, HSBD-F, PMSP, GCT-CJ, SF-ZSY, and HSYF-F were the safest treatments in the recommended list, with SI scores over 0.8. PESP, QYLX-F, JHQG-KL, SFJD-JN, SHL-KFY, PESP1, XBJ-ZSY, HSZF-F, PSSP2, FFTS-W, and NHSQ-W were the prescriptions most likely to be unsafe, with SI scores below 0.1. In the additional lists of other TCM prescriptions, the indicators of XC-T, SQRS-S, CC-J, and XFBD-F were all above 0.8, while QF-Y, XZXS-S, BJ-S, KBD-CJ, and QWJD-T's indicators were all below 0.1.
Conclusions
In total, there were 10 TCM prescriptions with indicators over 0.8, suggesting that they could be considered in treating COVID-19, if suitable. We believe this work could provide reasonable suggestions for choosing proper TCM prescriptions as a supplementary treatment for COVID-19. Furthermore, this work introduces a novel and informative method which could help create recommendation list of TCM prescriptions for the treatment of other diseases.
Keywords: Covid-19, Side effect, Deep learning, Artificial intelligence, Novel corona virus, Traditional Chinese medicine
Graphical abstract
1. Introduction
The novel coronavirus disease (COVID-19) outbreak in Wuhan City has now spread worldwide, affecting more than 28 million people, with over 900,000 deaths reported (World Health Organization, 2020). Though it is suggested that the fatality rate of COVID-19 is relatively low compared to other infamous infectious diseases, the high contagiousness of this disease has created a formidable challenge. This has provoked a serious response from many governments all over the world, especially China (Zhao et al., 2020). Additionally, although some drugs seem to be promising in the treatment of COVID-19, no drug has yet been officially confirmed to be safe and effective in curing the disease (Yu et al., 2020). This situation needs to change in order to block and eliminate the spread of COVID-19.
In effort to put forth solutions, Traditional Chinese Medicine (TCM) has been considered as a prospective supplementary treatment, due to its proven clinical performance in treating many chronic diseases, mental disorders, and even SARS (Hao et al., 2017; Kim et al., 2008; Ren et al., 2019; Xiang et al., 2019). The Chinese government and other official institutes have published a list of TCM prescriptions recommended for each disease stage of the COVID-19 infection (released by National Health Commission & National Administration of Traditional Chinese Medicine, on March 3, 2020). However, there is a lack of reasonable and reliable criteria for evaluating TCM. Moreover, as there are many side effects (SE) reported in its application, it is recommended to take into account the SIs of TCM prescriptions and products. This is especially important in treating COVID-19, which could lead to dramatic degradation of the patients’ physical condition.
Artificial Intelligence (AI) has been widely applied to tasks that aim to identify features among many relationship-unknown objects (Krittanawong et al., 2017; Lecun et al., 2015). As one emerging technology of AI, the Artificial Neural Network (ANN) is becoming increasingly mature in describing relationships among pairwise data (Zhang et al., 2020). Furthermore, this technology has already provided a suitable approach towards high-accuracy TCM SI prediction with an ontology-based prediction model (Yao et al., 2019). Utilizing deep learning, recent research have also predicted possible modern antiviral drugs for COVID-19 (Beck et al., 2020).
In this work, by combining the deep learning method and SI prediction, we employed an ontology-based side-effect prediction framework (OSPF) to evaluate TCM prescriptions that are officially recommended for COVID-19 in China. We then reorganized the recommended prescription list based on proposed SI values. Moreover, in effort to expand potential treatment options, we also examine the safety of other well-known TCM prescriptions which are found in traditional flu-treatment books, but not in the recommended list of treating COVID-19. We believe this work will provide reasonable suggestions for choosing proper TCM prescriptions which might function as supplementary treatments for COVID-19. This work also provides a novel and informative approach to curating a more reasonable recommendation list of TCM prescriptions for the treatment of other diseases.
2. Methods
An OSPF, developed in our previous work, was implemented for evaluation purposes where each medicine component (an herb, mineral, etc.) in a TCM compound prescription (CP) was classified into several categories, such as “hot”, “cold”, “towards heart”, and “towards kidney” (Wang et al., 2020). The classification was inspired by an ontology-based theory (Zhou et al., 2004), where the categories like “hot” or “cold” were considered as the fundamental ontology items for describing attributes of TCM medicines. In other words, in the strategy of OSPF, TCM components in compounds are summarized as attribution labels. For example, the herb GUIZHI (Cinnamomum cassia Presl) is generalized as a group of labels including “hot”, “neutral”, and “towards heart”.
Concomitantly, we collected information from the TCM drug datasets that reportedly cause major SE (Yao et al., 2019). As a complement, a group of TCM CPs coming from the ancient and prestigious TCM book, Shanghanzabinglun, was regarded as safe. To be more specific, 264 TCM CPs without side effects reported in the TCM books were recognized as the non-SE prescriptions, and the 73 SE-causing TCM CPs are introduced as complementary data.
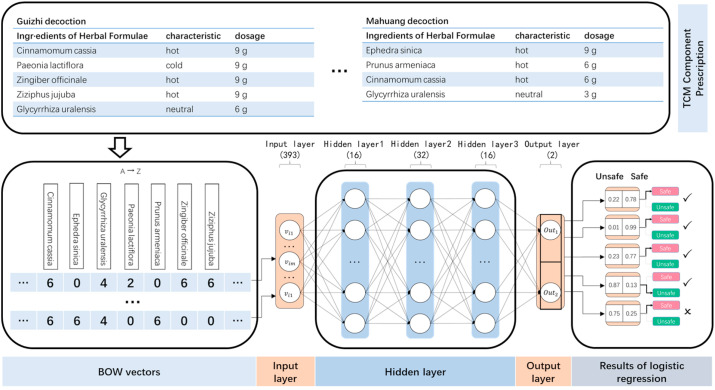
As shown in Fig. 1 , by considering a group of labels, one compound prescription could be vectorized as a group of data by the Bag-of-Word (BOW) model (Harris, 1954). In order to construct such a model, we first build a complete dictionary with size , containing names for all the ingredients in our TCM CP dataset. Then, each TCM CP can be represented by a different vector with the same length. The ith element in the vector is the dosage of this herb, with negative, positive, or neutral prefixes representing the attribute. In this work, we assume that all the prescriptions are independent of each other, which means inheritance and subordination among CP data are not considered.
Fig. 1.
Data stream of SI prediction.
An ANN model was then established to learn latent relationships between structures of TCM prescriptions and their SIs. As shown in Fig. 1, in the lower panel, the ANN contained 5 layers, where the input layer included 393 units for receiving BOW vectors. The output layer contained two units for outputting prediction. Three hidden layers, which included more than 60 units, were used to identify and remember the complex relationships between attributes of pharmaceutical ingredients in each prescription and their corresponding side effects. A 10-fold cross-validation was applied for training the ANN model and the TCM dataset was thus randomly separated into 10 sub-datasets. In each procedure, one of these 10 separations was picked as a test set, while the remaining nine sets were regarded as the training sets. Training and test sets were input into the ANN model sequentially to modify the neural cell parameters.
A list of officially recommended TCM CPs to treat COVID-19 as well as their associated side effects were digitalized into vectors of BOW and input into the well-trained ANN. The outputs of the ANN consisted of indicators, ranging from 0 to 1, representing the predicted safety possibilities of corresponding TCM CP inputs. We also evaluated the SIs of three common prescriptions in treating COVID-19, Qingfei Paidu Decoction (QFPD-F), Huashi Baidu Formula (HSBD-F), and Xuanfei Baidu Formula (XFBD-F).
Table 1 lists the officially recommended TCM and other popular CPs currently used to treat similar symptoms. The scientific names of all botanical plants within these CPs are listed in the supplemental material. In this paper, abbreviations are applied to simplify descriptions where the suffixes -GMP, -KFY, -KL/-CJ, -JN, -ZSY, -T, -W, and –S mean tablet, oral solution, drug granules, capsule, injection, soup, pill, and powder/solution, respectively.
Table 1.
Cross-reference of Chinese and English names of TCM prescriptions used in this work. The scientific names of all botanical plants are listed in the supplemental material.
| Index | Chinese Name | Hanyu Pinyin | Abbreviation |
|---|---|---|---|
| 1 | 桑菊感冒片 | Sangju ganmaopian | SJ-GMP |
| 2 | 芎芷香苏散 | Xiongzhixiangsu san | XZXS-S |
| 3 | 加减羌活五积散 | Jiajianqianghuowuji san | JJQHWJ-S |
| 4 | 百解散 | Baijie san | BJ-S |
| 5 | 相传汤 | Xiangchuan tang | XC-T |
| 6 | 顺气人参散 | Shunqirenshen san | SQRS-S |
| 7 | 柴陈煎 | Chaichen jian | CC-J |
| 8 | 柴胡半夏汤 | Chaihubanxia tang | CHBX-T |
| 9 | 清肺饮 | Qingfei yin | QF-Y |
| 10 | 清瘟解毒汤 | Qingwenjiedu tang | QWJD-T |
| 11 | 藿香正气水 | Huoxiangzhengqi shui | HXZQ-S |
| 12 | 抗病毒冲剂 | Kangbingdu chongji | KBD-CJ |
| 13 | 金花清感颗粒 | Jinhuaqinggan keli | JHQG-KL |
| 14 | 连花清瘟胶囊 | Lianhuaqingwen jiaonang | LHQW-JN |
| 15 | 疏风解毒胶囊 | Shufengjiedu jiaonang | SFJD-JN |
| 16 | 防风通圣丸 | Fangfengtongsheng wan | FFTS-W |
| 17 | 初期方子 | Chuqifangzi | PESP |
| 18 | 中期方子 | Zhongqifangzi | PMSP |
| 19 | 血必静注射剂 | Xuebijing zhusheji | XBJ-ZSJ |
| 20 | 重症期方子1 | Zhongzhengqifangzi1 | PSSP1 |
| 21 | 重症期方子2 | Zhongzhengqifangzi2 | PSSP2 |
| 22 | 参附注射液 | Shenfu zhusheye | SF-ZSY |
| 23 | 生脉注射液 | Shengmai zhusheye | SM-ZSY |
| 24 | 恢复期方子 | HuifuqiFangzi | PRSP |
| 25 | 双黄连口服液 | Shuanghuanlian koufuye | SHL-KFY |
| 26 | 桂枝汤冲剂 | Guizhitang chongji | GZT-CJ |
| 27 | 牛黄上清丸 | Niuhuangshangqing wan | NHSQ-W |
| 28 | 清肺排毒汤 | Qingfeipaidu tang | QFPD-T |
| 29 | 寒湿郁肺方 | Hanshiyufen fang | HSYF-F |
| 30 | 湿热藴肺方 | Shireyunfei fang | SRYF-F |
| 31 | 湿毒郁肺方 | Shiduyufei fang | SDYF-F |
| 32 | 寒湿阻肺方 | Hanshizufei fang | HSZF-F |
| 33 | 化湿败毒方 | Huashibaidu fang | HSBD-F |
| 34 | 气营两燔方 | Qiyingliangfan fang | QYLF-F |
| 35 | 内闭外脱方 | Neibiwaituo fang | NBWT-F |
| 36 | 肺脾气虚方 | Feipiqixu fang | FPQX-F |
| 37 | 气阴两虚方 | Qiyinliangxu fang | QYLX-F |
| 38 | 宣肺败毒方 | Xuanfeibaidu fang | XFBD-F |
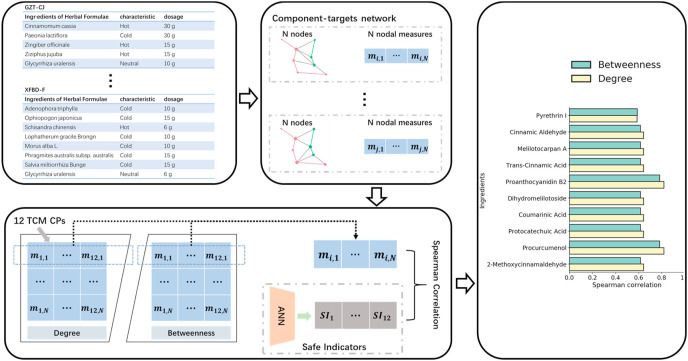
Finally, methods of network pharmacology were adopted to analyze the reasonability of SIs from an OSPF on a microscopic level. We first constructed an ingredient-target network for each of the TCM CPs, where represents a set of nodes in , and . is a set of edges in . Then, two traditional nodal measures between and were calculated for each network, , where and . Next, the SI of each ingredients-target network was calculated by the previously trained ANN model. Next, we calculated the Spearman correlation coefficient between all SIs and the nodal measures or on each node in to find the latent ingredients and targets which may be related to the SI of a TCM CP.
3. Result and discussion
Fig. 2 (a) and (b) shows the calculated SI of the recommended list and the additional list, respectively. Each data box contains 10 result points, while the small squares represent the mean values. As indicated in the figure, FFTS-W, PMSP, and SF-ZSY are the safest TCM prescriptions in the recommended list due to an SI score over 0.8. Whereas, JHQG-KL, LHQW-JN, SFJD-JN, XBJ-ZSY, and SHL-KFY are predicted as the least safe prescriptions, with SI below 0.2. Recently, an intensive debate about the effect of SHL-KFY on treating COVID-19 attracted the attention of the Chinese social media. The results from this study suggest that SHL-KFY should be excluded from the treatment plan due to safety concerns. As for the other common prescriptions in treating flu-like diseases, the indicators of XC-T, SQRS-S, CC-J, and CHBX-T were all above 0.8, while XZXS-S, SJ-GMP, QWJD-T, and KBD-CJ's indicators were are all below 0.2. Previous research has found that SHL-KFY and JHQG-KL do show side effects, which is consistent with our prediction (Chinese Pharmacists Association Therapeutic Drug Monitoring Pharmacist Branch, 2020; Niu et al., 2010; Yang wei, 2002). Moreover, a study analysis of 101 clinical samples revealed that HXZQ-S causes side effects including red hot and anaphylactic shock (Liu, 2017).
Fig. 2.
Prediction results of the TCM safety indicator (SI) in the group of (a) officially recommended list and (b) other common prescriptions in treating flu-like diseases.
Based on these results, a reorganized list is given in Fig. 3 based on averaged SI scores, where XC-T had the highest SI and KBD-CJ had the lowest. In total, there were seven TCM prescriptions with indicators over 0.8 suggested to be considered first in treating COVID-19, if suitable.
Fig. 3.
A reorganized list of TCM prescriptions based on the predicted mean SI score.
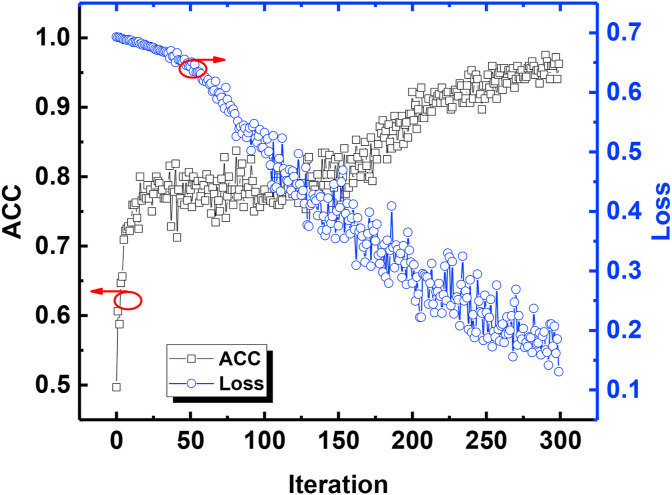
Training loss and accuracy of the ANN model were recorded to check the overfitting issue. As illustrated in Fig. 4 , training loss and accuracy of the training data showed opposite trends. The accuracy of training data gradually increased to around 0.95 as the training loss decreased to around 0.15, rendering the ANN model acceptable. The trend suggested that the more samples that are applied to the model, the closer the prediction of the model and data distribution in the training set would be. As a result, the model will provide an accurate prediction capability. Some important parameters, such as sensitivity rate, specificity rate, and the macro-f1 score of the trained ANN model, which were used for SI prediction, are provided in Table 2 .
Fig. 4.
The ACC and loss of the model versus iteration number.
Table 2.
ANN results.
| Accuracy | Sensitive | Specificity | Macro-F1 | |
|---|---|---|---|---|
| Fold-1 | 0.935 | 0.996 | 0.716 | 0.854 |
| Fold-2 | 0.929 | 0.993 | 0.761 | 0.858 |
| Fold-3 | 0.926 | 0.996 | 0.700 | 0.847 |
| Fold-4 | 0.938 | 0.996 | 0.711 | 0.849 |
| Fold-5 | 0.935 | 0.997 | 0.756 | 0.878 |
| Fold-6 | 0.923 | 0.993 | 0.653 | 0.823 |
| Fold-7 | 0.923 | 0.996 | 0.713 | 0.847 |
| Fold-8 | 0.932 | 0.993 | 0.678 | 0.839 |
| Fold-9 | 0.938 | 0.996 | 0.676 | 0.851 |
| Fold-10 | 0.941 | 0.996 | 0.733 | 0.860 |
| Mean | 0.932 | 0.995 | 0.710 | 0.850 |
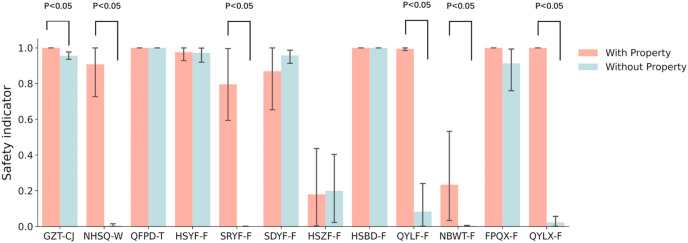
Fig. 5 specifically shows the SI scores of 12 TCM CPs from the Chinese Seventh Edition of the Diagnosis and Treatment, which are calculated with and without the category labels. In this work, a Wilcoxon rank-sum test was used to examine whether there was a significant difference between the two results (Wilcoxon, 1945). It is obvious that, for NHSQ-W, SRYF-F, QYLF-F, and QYLX-F, the prediction results are opposite. Nevertheless, for SDYF-F, NBWT-F, and FPQX-F, the results have a non-negligible difference. Therefore, it is of great significance to take category labels into account, in the SI evaluation (p < 0.05, BF corrected).
Fig. 5.
SI derived from two models: one contained the hot or cold property of herbs, whereas the other did not. The rank test was applied (p < 0.05, BF corrected).
As illustrated in Fig. 6 , taking 12 prescriptions from the Seventh Edition of the Diagnosis and Treatment as an example, it is clear that the ingredients of CPs play roles in related biological functions via targets, but the connection between the SE of a TCM CP and its ingredient-target relationship is still unclear. In detail, the SIs and each nodal measure of 12 pharmacology networks derived from the corresponding CP are significantly relevant (p < 0.05), as shown in Table 3 . A strong correlation indicates that the SI from our model can be interpreted as well, to some extent, by the pharmacological ingredients. This means the method used in this work can be supported by network pharmacology.
Fig. 6.
The process of analyzing the relationship between SIs derived from the 12 TCM CPs by an ANN model and the nodal measures throughout the ingredients-target networks of these TCM CPs. The Spearman correlation coefficient is significant (p < 0.05).
Table 3.
Spearman correlation results.
| Ingredients name | r | p | Measure Type |
|---|---|---|---|
| Pyrethrin I | 0.587 | 0.045 | Betweenness |
| Pyrethrin I | 0.585 | 0.046 | Degree |
| Cinnamic Aldehyde | 0.615 | 0.033 | Betweenness |
| Cinnamic Aldehyde | 0.641 | 0.025 | Degree |
| Melilotocarpan A | 0.615 | 0.033 | Betweenness |
| Melilotocarpan A | 0.641 | 0.025 | Degree |
| Trans-Cinnamic Acid | 0.615 | 0.033 | Betweenness |
| Trans-Cinnamic Acid | 0.641 | 0.025 | Degree |
| Proanthocyanidin B2 | 0.782 | 0.003 | Betweenness |
| Proanthocyanidin B2 | 0.819 | 0.001 | Degree |
| Dihydromelilotoside | 0.615 | 0.033 | Betweenness |
| Dihydromelilotoside | 0.641 | 0.025 | Degree |
| Coumarinic Acid | 0.615 | 0.033 | Betweenness |
| Coumarinic Acid | 0.641 | 0.025 | Degree |
| Protocatechuic Acid | 0.615 | 0.033 | Betweenness |
| Protocatechuic Acid | 0.641 | 0.025 | Degree |
| Procurcumenol | 0.782 | 0.003 | Betweenness |
| Procurcumenol | 0.819 | 0.001 | Degree |
| 2-Methoxycinnamaldehyde | 0.615 | 0.033 | Betweenness |
| 2-Methoxycinnamaldehyde | 0.641 | 0.025 | Degree |
4. Conclusion
To conclude, this work provides an approach to the evaluation of TCM prescriptions included in the officially recommended list, as well as other well-known prescriptions for treating flu-like diseases. This work was conducted using OSPF and ANN-based deep learning methods. After training and testing the ANN model, results showed that QFPD-T, HSBD-F, PMSP, GCT-CJ, SF-ZSY, HSYF-F, XC-T, SQRS-S, CC-J, and XFBD-F were all recommended because of their SI scores over 0.8. Meanwhile, PESP, QYLX-F, JHQG-KL, SFJD-JN, SHL-KFY, PESP1, XBJ-ZSY, HSZF-F, PSSP2, FFTS-W, NHSQ-W, QF-Y, XZXS-S, BJ-S, KBD-CJ, and QWJD-T were not suggested to be used primarily because of their low scores. This work provided a reasonable suggestion for choosing proper TCM prescriptions as supplementary treatment for COVID-19. This work also provided a novel and informative approach to the assessment of a reasonable recommendation list of TCM prescriptions for other diseases.
Author contributions
Z.W. conceived the idea and wrote the main manuscript text and prepared all figures. L.L. established the artificial model and run the code. Z.W. and L.L. contributed equally to this work. M.S. and J.S. collected the data used in this work. J.Y., M.S., and J.S. prepared the table and revise the paper manuscript. Y.Y. supervised the whole procedure of this study and provided the fund. All authors discussed the results and reviewed the manuscript.
Acknowledgements
This work was supported in part by the National Natural Science Foundation of China under Grant 61370202. We thank LetPub (www.letpub.com) for its linguistic assistance during the preparation of this manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jep.2021.113957.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Beck B.R., Shin B., Choi Y., Park S., Kang K. 2020. Predicting Commercially Available Antiviral Drugs that May Act on the Novel Coronavirus ( 2019-nCoV ), Wuhan , China through a Drug-Target Interaction Deep Learning Model. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinese Pharmacists Association Therapeutic Drug Monitoring Pharmacist Branch Guidelines for drug treatment and pharmaceutical care of new coronavirus pneumonia and common comorbidities. Advers. Drug React. J. 2020;22:121–129. [Google Scholar]
- Hao P., Jiang F., Cheng J., Ma L., Zhang Y., Zhao Y. Traditional Chinese medicine for cardiovascular disease: evidence and potential mechanisms. J. Am. Coll. Cardiol. 2017;69:2952–2966. doi: 10.1016/j.jacc.2017.04.041. [DOI] [PubMed] [Google Scholar]
- Harris Z.S. Distributional structure. Word. 1954;10:146–162. doi: 10.1080/00437956.1954.11659520. [DOI] [Google Scholar]
- Kim H.-Y., Shin H.-S., Park H., Kim Y.-C., Yun Y.G., Park S., Shin H.-J., Kim K. In vitro inhibition of coronavirus replications by the traditionally used medicinal herbal extracts, Cimicifuga rhizoma, Meliae cortex, Coptidis rhizoma, and Phellodendron cortex. J. Clin. Virol. 2008;41:122–128. doi: 10.1016/j.jcv.2007.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krittanawong C., Zhang H., Wang Z., Aydar M., Kitai T. Artificial intelligence in precision cardiovascular medicine. J. Am. Coll. Cardiol. 2017;69:2657–2664. doi: 10.1016/j.jacc.2017.03.571. [DOI] [PubMed] [Google Scholar]
- Lecun Y., Bengio Y., Hinton G. Deep learning. Nature. 2015;521:436–444. doi: 10.1038/nature14539. [DOI] [PubMed] [Google Scholar]
- Liu Song-song X.Y. Literature analysis of 101 cases of adverse reactions induced by huoxiangzhengqi liquid. Chinese J. Pharmacovigil. 2017;14:317. [Google Scholar]
- Niu H.L., Hui M., Xiao J.Y., Li Q.Z., Zhang Y.F., Zhou S.Q. Drug Stand; China: 2010. Study on Depressor Effect of Shuanghuanglian Injection. [Google Scholar]
- Released by National Health Commission & National Administration of Traditional Chinese Medicine on March 3, 2020) Diagnosis and treatment protocol for novel coronavirus pneumonia (trial version 7) Chin. Med. J. (Engl). 2020;133 [Google Scholar]
- Ren F., Ma Z., Shen Y., Li G., You Y., Yu X., Li Z., Chang D., Zhang P. Effects of Chaihu-Shugan-San capsule for psychogenic erectile dysfunction: study protocol of a randomized placebo-controlled trial. Medicine (Baltim.) 2019;98 doi: 10.1097/MD.0000000000017925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Li L., Yan J., Yao Y. IEEE Access; 2020. Approaching High-Accuracy Side Effect Prediction of Traditional Chinese Medicine Compound Prescription Using Network Embedding and Deep Learning; p. 1. [DOI] [Google Scholar]
- Wilcoxon F. Individual comparisons by ranking methods. Biometrics Bull. 1945;1:80–83. doi: 10.2307/3001968. [DOI] [Google Scholar]
- World Health Organization Coronavirus disease. Coronavirus Dis. Situat. Rep. 2020;119:2633. doi: 10.1001/jama.2020.2633. [DOI] [Google Scholar]
- Xiang Y., Guo Z., Zhu P., Chen J., Huang Y. Traditional Chinese medicine as a cancer treatment: modern perspectives of ancient but advanced science. Cancer Med. 2019;8:1958–1975. doi: 10.1002/cam4.2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang wei. Analysis of adverse reaction of shuanghuanglian preparation. Her. Med. 2002;62 doi: 10.3870/j.issn.1004-0781.2002.08.039. [DOI] [Google Scholar]
- Yao Y., Wang Z., Li L., Lu K., Liu R., Liu Z., Yan J. An ontology-based artificial intelligence model for medicine side-effect prediction: taking traditional Chinese medicine as an example. Comput. Math. Methods Med. 2019;2019 doi: 10.1155/2019/8617503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu F., Du L., Ojcius D.M., Pan C., Jiang S. Measures for diagnosing and treating infections by a novel coronavirus responsible for a pneumonia outbreak originating in Wuhan, China. Microb. Infect. 2020 doi: 10.1016/j.micinf.2020.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Nguyen H., Bui X.-N., Nguyen-Thoi T., Bui T.-T., Nguyen N., Vu D.-A., Mahesh V., Moayedi H. Developing a novel artificial intelligence model to estimate the capital cost of mining projects using deep neural network-based ant colony optimization algorithm. Res. Pol. 2020;66 doi: 10.1016/j.resourpol.2020.101604. [DOI] [Google Scholar]
- Zhao S., Lin Q., Ran J., Musa S.S., Yang G., Wang W., Lou Y., Gao D., Yang L., He D., Wang M.H. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X., Wu Z., Yin A., Wu L., Fan W., Zhang R. Ontology development for unified traditional Chinese medical language system. Artif. Intell. Med. 2004;32:15–27. doi: 10.1016/j.artmed.2004.01.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.