Abstract
Gait modifications are used in the rehabilitation of musculoskeletal conditions like osteoarthritis and patellofemoral pain syndrome. While most of the research has focused on the biomechanical and clinical outcomes affected by gait modification, the process of learning these new gait patterns has received little attention. Without adequate learning, it is unlikely that the modification will be performed in daily life, limiting the likelihood of long-term benefit. There is a vast body of literature examining motor learning, though little has involved gait modifications, especially in populations with musculoskeletal conditions. The studies that have examined gait modifications in these populations are often limited due to incomplete reporting and study design decisions that prohibit strong conclusions about motor learning. This perspective draws on evidence from the broader motor learning literature for application in the context of modifying gait. Where possible, specific gait modification examples are included to highlight the current literature and what can be improved on going forward. A brief theoretical overview of motor learning is outlined, followed by strategies that are known to improve motor learning, and finally, how assessments of learning need to be conducted to make meaningful conclusions.
Keywords: Gait: Gait Training, Movement, Walking
Introduction
Walking is a skilled movement fundamental to daily life, and the loss of walking ability can negatively impact quality of life and functional independence.1 Restoration of independent, functional, and stable gait, what we would call gait retraining, is an important clinical objective following disease or injury, such as after experiencing a stroke2 or undergoing a lower limb amputation.3 In contrast, gait modification is a therapeutic approach that does not aim to restore gait but instead aims to alter gait characteristics to achieve a specific therapeutic effect.
Gait modification, in the context of both walking and running, is a growing treatment approach for musculoskeletal (MSK) conditions. Generally, gait modifications aim to optimize some specific component of function through modifying spatiotemporal, kinematic, or joint load variables. In recent years, changing foot position during walking (toe-in or toe-out) has received increased attention for managing knee osteoarthritis due to its ability to decrease deleterious knee loads.4 The treatment of running-related injuries, such as patellofemoral pain syndrome, may also benefit from gait modifications, including changes in foot strike pattern, cadence, or hip joint biomechanics.5–7 However, without motor learning, gait modifications are less likely to be consistently performed in real-world settings, thus limiting the biomechanical (and potentially the clinical) effect. While a focus on the biomechanical and clinical effects has dominated the literature, the process of learning the modifications themselves is only recently receiving more attention.
While there are many strategies that can be implemented to augment and measure motor learning, very few have received direct comparisons in MSK populations. However, we can begin to develop a framework from the existing data collected in healthy populations.8–10 Several methods of feedback are common to gait modification, including visual or auditory feedback, while fewer studies have used haptic feedback.4,5,7 A progressive reduction in feedback frequency is almost invariably used, as this is known to improve motor learning.11 Assessments of learning are necessary to track progress, and several options are available to the clinician or research. A simple test is performance of the modification without any feedback, while more complex strategies like assessing performance on a related task6 or while performing additional cognitive tasks12 may better inform how well the modification can be performed in real-world environments. Unfortunately, the methods, assessment strategies, and completeness of reporting in gait modification interventions vary substantially, limiting the possible conclusions about motor learning. If not learned, the modification is unlikely to be performed outside of the laboratory or clinical setting, which may mask any long-term treatment effects. Without consistent methods and reporting, it is difficult to determine the best strategies for facilitating and evaluating learning in gait modification.
To provide a platform for future MSK-relevant gait modification research to build on, we have gathered evidence from the broader motor learning literature largely conducted in healthy populations, the upper limb, and in discrete tasks. However, the transferability of these results to gait modification is still unclear. As a result, we have used these data to help guide our recommendations. Given this, we have provided examples in clinical populations undergoing gait modification whenever possible both to demonstrate the state of the research today and what can be improved on going forward. We intend this article to be a guide (see Fig. 1 for a visual summary), given the current evidence, for clinicians and researchers interested in implementing gait modification interventions and wishing to optimize motor learning and assessment.
Figure 1.
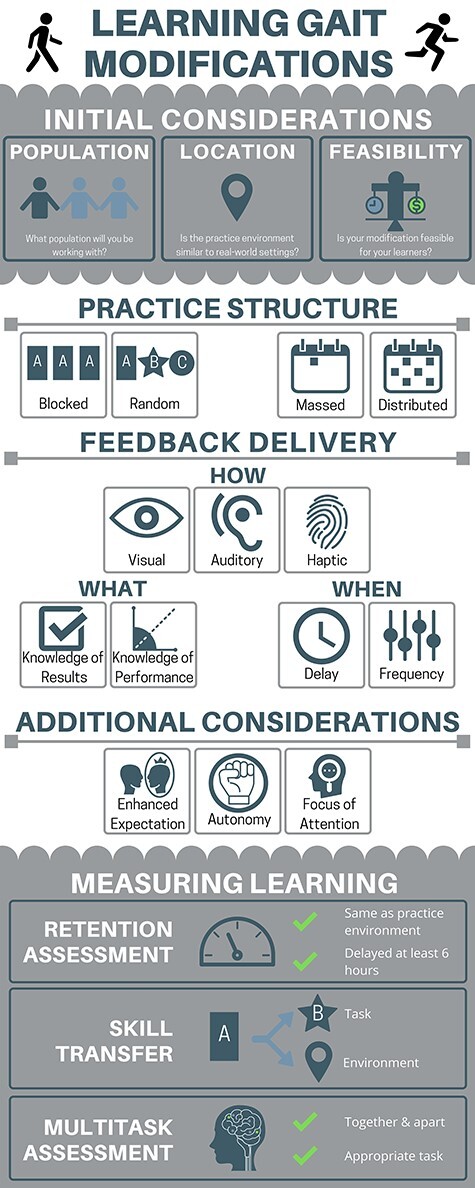
Visual summary of motor learning in gait modification. Clinicians and researchers should consider the specific population they are working with to determine what modification is most relevant. Determining the location in which the modification will be trained, and where it may be ultimately performed, is necessary to inform the feasibility of many other aspects of the motor learning intervention. Distributed practice schedules that use a blocked structure are supported by the evidence, but random practice may offer benefits when performing the modification in more variable settings (eg, real-world). There are many options for feedback delivery, and feasibility (eg, equipment and time) may ultimately dictate these decisions. Finally, retention tests are the foundation of assessing motor learning. However, including either a transfer test or multitask assessment will help understand the current state of learning, so long as assessments are fully reported.
Motor Learning: A Brief Overview
There are different forms of motor learning with varied relevance to learning MSK-related gait modification. Gait modification involves the process of motor skill learning, broadly defined as the acquisition of a novel motor pattern.13 Another form of learning describes the process of combining a series of discrete tasks into a single action, known as motor sequence learning.14 Motor adaptation describes transient adjustments of a motor pattern based on internal or external feedback factors (eg, split-belt walking).13,15 Examining motor adaption often involves inducing visual distortions16 or physical perturbations during gait, like differences in treadmill belt speeds.17 Since motor adaptation research has largely targeted neurological rehabilitation and is typically not used in MSK-related rehabilitation, a deeper discussion of this form of learning (and others) is beyond the scope of this article (see18,19). However, we draw on examples of these motor learning forms to help inform how gait modifications are learned and evaluated. However, it is important to note that the transferability of results between different forms of learning is unclear.
Motor skill learning is a complex phenomenon, specifically defined as “a set of processes associated with practice or experience leading to relatively permanent changes in the capability for skilled movement.”13 This relative permanence, a core feature of motor learning, distinguishes it from transient changes in skill proficiency that often occurs within practice. More specifically, this distinction separates motor performance—the observable execution of a skill in a specific temporal and environmental context—and motor learning—the more permanent change in skill execution with practice or experience. Motor performances are subject to temporary factors such as motivation, feedback, attention, or practice structure,20,21 and when these factors are removed, the effect on motor performance may dissipate (performance worsens). Over time, accumulating practice can lead to performance improvements maintained well after practice, and independent of practice-related temporary factors, referred to as learning. This distinction was highlighted by a review of 41 studies, though the studies primarily involved upper limb tasks in healthy participants.20 Most of the included studies (63%) found that measures of learning immediately after practice vs measures delayed by some time were incompatible, suggesting practice-related temporary factors contaminate measures of learning that are conducted too close in time to practice.20
In 1967, Fitts and Posner22 proposed that learning progressed through 3 contiguous but overlapping stages, each characterized by distinct behaviors (Fig. 2). While other theories of motor learning exist, and the readers are encouraged to investigate them (see 23–26), Fitts and Posner’s22 model is a relatively straightforward framework for researchers and clinicians to conceptualize learning progression. This model provides context for larger timescale changes in behavior; however, it does not necessarily capture changes that may occur within a practice, or in the hours that follow.
Figure 2.
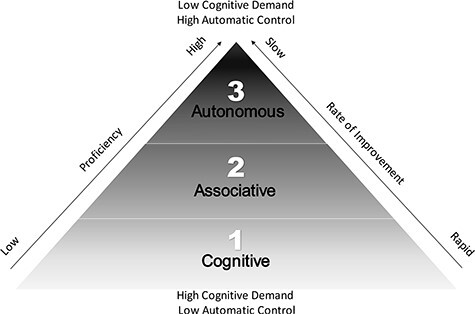
Fitts and Posner’s 3-stage model of learning. (1) The cognitive (acquisition) stage consists of the learner attempting to problem solve for what motor patterns need to be executed to perform the skill correctly.20,22 During this stage, motor performance is variable, improvement can be rapid, and task requires substantial attention.22,43,96 (2) The associative stage is identified by a slowing of the improvement rate and the increase in performance consistency. Here, attentional demands for executing the skill begin to decrease while proficiency remains high. (3) Finally, the autonomous stage involves a high level of performance with minimal attentional demands.97 Reaching this stage are often exemplified by the capability to perform multiple skills simultaneously (eg, singing while playing guitar).
Shorter term changes in motor learning are better explained by the development of motor memories, a representation of the motor skill.27 These motor memories are formed through 2 processes, encoding and consolidation, and realized through memory retrieval.28 Encoding of the motor memory occurs during practice (acquisition phase) as use-dependent neural plasticity.29 Accumulating practice with or without feedback present30 drives this process, which is associated with better stimuli identification, connections between the goal/target and previous performance, and determination of the motor adjustments needed to improve subsequent performance.20,28 Once practice is completed, offline processes take over to consolidate the motor memory and render it more permanent.20 Consolidation is characterized by a slow improvement in performance between practice sessions and stabilization of the motor memory (increased resistance to interfering motor memories or additional attentional demands).31,32 Studies that interrupted the consolidation process by transcranial magnetic stimulation at various time points after practicing upper-limb tasks suggest that consolidation takes at least 4 to 6 hours.32–34 Once consolidated, motor memories can be retrieved at a later time, but this temporarily renders the memory unstable. While this process may risk interference with the memory, it also allows for new information to be integrated into the memory, an update based on the current or changing demands.35,36
Gait modification interventions ultimately aim to permanently improve the ability to execute a new gait pattern. When measuring learning, it is essential to make the distinction between transient changes in motor performance and the more permanent consolidation-dependent changes associated with learning. Otherwise, results from gait modifications will not represent actual learning and will overestimate performance.
Improving Motor Learning of Gait Modifications
The broader motor learning literature reports a plethora of strategies that improve motor learning,37–41 though few have been tested in the context of gait modification. The goal of this section is to step through several foundational concepts that modulate motor learning. Clinical examples specific to gait modifications are included where available and supplemented with data from healthy populations.
Practice Structure
The tasks performed in practice can be arranged in a blocked manner, where only 1 task is repeated over the practice or several (dis)similar tasks can be randomly arranged over the practice.42,43 While blocked practice may improve performance during practice, random practice improves motor learning despite poorer performance during practice.20 The reduced practice performance during random practice may be a result of higher cognitive demands44 and interference between task-related information each time the task is switched (contextual interference effect).45 However, this switching may result in stronger and more flexible motor memories.42 Although not specifically gait modification, unilateral split-belt motor adaptation in healthy walkers provides some insight into the effect of random practice.46 Random changes in velocity induced every 20 steps resulted in similar balance adaptions to a linearly increasing velocity (non-random), but later testing showed greater learning in the random group. Notably, the 20-step block condition resulted in superior learning compared with a third group where velocity randomly changed on a step-by-step basis, potentially due to the latter condition being overly difficult. Random practice can be implemented with relative ease so long as the feedback strategy can be easily manipulated. How frequently to vary the target or task is unclear, though the aforementioned study would suggest that a random-blocked approach may be better for learning than a purely random or blocked approach, and it may be more practical to implement too.
Unfortunately, we are unaware of any MSK-related gait modification studies that have specifically compared different practice structures, most having used a blocked structure. For example, Hunt et al47 instructed a 15° toe-out angle increase in people with knee osteoarthritis by using the same toe-out target each practice spread over 16 weeks. Evidence from a study of healthy participants learning to increase foot height during swing showed blocked practice resulted in superior learning compared with random practice.9 While both studies successfully modified gait using blocked practice, learning was assessed only in the laboratory setting. Such a setting likely biases blocked practice as there is little need for a flexible motor memory due to a highly controlled environment, unlike real-world settings where it is arguably more important that the modification be performed. This is also supported by a review of motor learning studies involving primarily upper body tasks.42 With more available wearable-sensor systems, real-world practice and assessments of learning are becoming more feasible. For example, runners at a high risk of developing a running-related injury used a consumer sport watch to successfully increase step rate and track performance during at-home running.48 While using a shoe-embedded pressure sensor, healthy participants successfully learned to medialize foot pressure during outdoor walking (a modification ultimately targeted at knee osteoarthritis).
Practices can also be scheduled in a massed or distributed fashion, whereby sessions are completed in 1 contiguous block or spread out over time (eg, hours/days/months), with varying effects on motor learning.49 Again using the aforementioned foot-height trajectory task, Krishnan8 found superior learning in healthy participants with distributed practice (over 2 days) compared with massed practice (matched for total trials). It is certainly more common to see distributed practice schedules spread over days or weeks in gait modification research, particularly within intervention studies. However, the density of practice distribution may be dependent on cost, time, and availability factors, which could limit the optimization of a practice schedule in a clinical or research setting.
Feedback Delivery
Feedback is essential to guiding the learning process. Feedback can originate from intrinsic sources, including proprioceptive sensory afferents, providing information on limb position, or external sources, which convey task-relevant information via visual, auditory, and/or haptic modes, known as augmented feedback.38 Two primary categories of information can be derived from external feedbacks: specific characteristics of the performance itself (knowledge of performance) or whether the performance attempt was successful (knowledge of results).38,50 Healthy populations, runners with patellofemoral pain, and walkers with knee osteoarthritis were all able to modify relevant gait variables using knowledge of performance.4,5 While no direct comparisons between knowledge of performance and knowledge of results were made, evidence from upper-limb motor learning during stroke rehabilitation suggests that there is little difference in learning outcomes.51
Systematic reviews of running and walking modification found visual feedback approaches were most commonly used.4,5 Of the 12 walking modification studies in the review, 5 included people with knee osteoarthritis and found that visual and haptic feedback resulted in similarly successful modification performance.4 In the second review, 3 of 10 running studies included participants with patellofemoral pain syndrome who were successfully trained to modify foot strike and hip adduction angle using visual or auditory feedback.5 Visual feedback can be displayed on a projection screen, television screen, or a simple mirror.38 Augmented reality (3-dimensional images projected onto the environment and visualized through a headset) was also recently explored as another means of delivering visual feedback to modify gait in healthy participants.52 Auditory feedback can be discrete sounds or more complex sonification where variables are mapped to changes in sound amplitude or frequency.38 Haptic feedback uses small vibration motors affixed to the skin with specific instructions describing what a vibration means and how to alter gait accordingly.53,54 As real-world walking requires visual attention (eg, navigating a sideway), haptic or auditory feedback may be more appropriate for these settings as it does not interfere with visual navigation. Leveraging the growing use of wearable sensors, real-world feedback to modify gait is becoming more feasible,55 though testing in populations with MSK impairments is still lacking.
Using cues, instructions, or augmented feedback can direct attention toward internal foci (eg, bodily motion) or external foci (eg, a sound). External foci are thought to promote flexible, self-organized, and automatic motor control strategies,56 while internal foci require more cognitive resources and conscious control.56–58 Based on the constrained action hypothesis,59 an external focus of attention should result in superior learning of gait modifications compared with internal foci. Over several decades, a large body of evidence has manifested comparing internal and external foci, and the results of this work have strongly supported the superiority of external foci when learning various motor skills.21,39 However, many of these tasks involved discrete movements that potentially limit the transferability of these findings to gait modifications, though some evidence does exist in this context. A recent study by Moore et al10 showed that internal and external foci both successfully alter running patterns; however, differing kinematic responses occurred despite the hypothesis being that both foci would induce a flatter foot strike. Internal foci (“run with a flat foot”) elicited a flatter foot strike, while external foci (“run quietly”) induced more proximal changes (greater knee flexion), and a combination of internal and external foci resulted in both to lesser extents.10 Other similar work has confounded results due to mixing foci60,61 or examining barefoot running, which may bias distal kinematic changes.62 Therefore, it is unclear if external foci are superior compared with internal foci, at least for gait modification. However, the current evidence suggests that if a specific movement modification is desired an internal focus may be more appropriate (eg, foot strike pattern), while external foci may be better when a more abstract outcome (eg, lower joint forces) is desired but the specific movement solution matters less.63 Given the limited data, clinicians and researchers should consider their specific movement goals and emphasize the appropriate foci.
Feedback Timing
The amount of feedback provided within a practice session, or across multiple practice sessions, can affect motor learning. Evidence from upper-limb tracking tasks suggests high-frequency feedback (eg, 100% of performance attempts receive feedback) can boost performance during practice but may negatively affect motor learning.11 Conversely, lower frequency feedback (eg, 50% of attempts receive feedback) or a faded feedback design (progressive decrease in feedback frequency over time) can result in worse practice performance but superior motor learning compared with higher frequency feedback paradigms.11,64 These differential results are thought to occur due to a learner’s dependence on feedback for error detection and correction when feedback is frequently provided (see the Guidance Hypothesis37,65). Though no comparison with other feedback frequencies exist in the gait modification literature, faded feedback is often used to modify running and walking biomechanics in clinical populations.4,5 Bandwidth feedback uses performance error to time feedback delivery when an error threshold is exceeded.38 This method was successfully used to modify the toe-in angle of people with knee osteoarthritis over 6 weeks.66,67 However, it may be more difficult to administer bandwidth feedback without motion capture or wearable sensor systems. Until evidence emerges to suggest otherwise, a faded feedback design seems appropriate for gait modification.
The time between completing the motor skill and delivering feedback (feedback interval) is another subtle manipulation that can affect learning. Winstein50 suggested that quick delivery of feedback may be beneficial early in the learning process. However, it is important to avoid reliance on feedback for error detection. Therefore, some delay between completion of the task and feedback delivery is ultimately recommended as it may improve retention and internal error detection.50,68 Concurrent feedback, which is common in gait modification,4 inherently does not allow for such a delay; however, use of technological displays or haptic motors may facilitate more nuanced feedback timing capability.
When designing a gait modification intervention, practice structure and feedback delivery are fundamental components requiring careful consideration. Our current review and synthesis suggests that gait modifications can be successfully learned using blocked practice; however, we would argue that including random practice may better prepare the learner for real-world performance. While visual feedback is most common, auditory or haptic feedback could be combined with wearable sensing to facilitate real-world practice. Faded feedback paradigms are extensively used in gait modification research and are seemingly supported, though it has not been directly compared with other feedback frequencies. Bandwidth feedback may be an effective approach to modify gait, but it generally requires technological feedback systems that limit the clinical feasibility. However, advances in wearable technology should soon make more nuanced feedback strategies more feasible.
Social-Cognitive-Affective Aspects of Learning
Wulf and Lewthwaite69 recently proposed the optimizing performance through intrinsic motivation and attention for learning theory that encompasses 3 factors known to affect motor learning: expectancy, autonomy, and attention.21 Though this model in its entirety has yet to be implemented in a gait modification context, there are instances of subparts being applied. For example, an autonomy supportive environment was facilitated by allowing runners, who were at risk of injury, to determine their own practice schedule while learning to increase step rate.48 However, evidence in upper-limb tasks suggests that combining all 3 primary factors has additive benefits on motor learning,70 which should be tested in gait modification.
More positive expectations of future performances, which is related to self-efficacy—the prospective sense that one can perform the task and achieve the goal71—is predictive of learning discrete motor tasks.21,72 This can be facilitated by providing feedback that compares between peers (normative feedback)69 or delivering feedback only after successful attempts.38,73 Fostering autonomy can also improve motor learning, possibly through increasing learner engagement with the practice process.40 Autonomy can be increased by directly involving the learner in decisions regarding practice and feedback,21 which relates well to the drive for shared decision-making in clinical care.73 A decision as insignificant as choosing the color of a golf ball can improve learning outcomes of a simple golf putting task.74 Similarly, more significant decisions about when and how often to receive feedback,75 or what order to practice a set of skills, can also enhance motor learning and performance,21,40 though this evidence largely comes from discrete tasks learned by healthy participants. The third component involves where attention is focused during practice. This was covered within the “Feedback Delivery” section, but it is worth reiterating that there is a large body of evidence in support of external foci for learning and performance, at least in discrete tasks.39
The optimizing performance through intrinsic motivation and attention for learning theory of motor learning69 provides additional tools for the clinician to consider when designing a gait modification intervention. The contents of feedback, particularly verbal feedback comparing peer-to-peer performance, can positively affect self-efficacy. Collaborating with the learner when designing the motor learning plan, such as when or how often to practice, supports autonomy and improves learning. Finally, attention should be directed externally where possible, such as displays or sounds from a sports watch, though internal foci has utility early in the learning process. With careful consideration of the language used for instruction and feedback, these strategies can be easily integrated into a gait modification program to improve learning.
Measuring Motor Performance and Learning
After deploying various strategies to improve motor learning in a gait modification intervention, it is important to assess the magnitude of learning. While direct measurement of motor learning is currently not possible,76 it can be inferred through measuring changes in behavior (eg, accuracy, error, etc) or neurophysiological phenomena. Given that neurophysiological measurements are generally not clinically feasible, we will only focus on behavioral measurements of learning. While it is often tempting to ascribe learning to changes in performance over a practice period (Fig. 3), these changes do not allow for consolidation and can lead to inappropriate conclusions about the extent to which a motor skill is learned. Instead, motor learning can be inferred through 3 different tests: delayed retention, skill transfer, and multitasking.13 While gait modification studies involving populations with MSK pathologies, or risk factors for them, have used these tests to infer learning, important details are frequently omitted, limiting the potential conclusions.77
Figure 3.
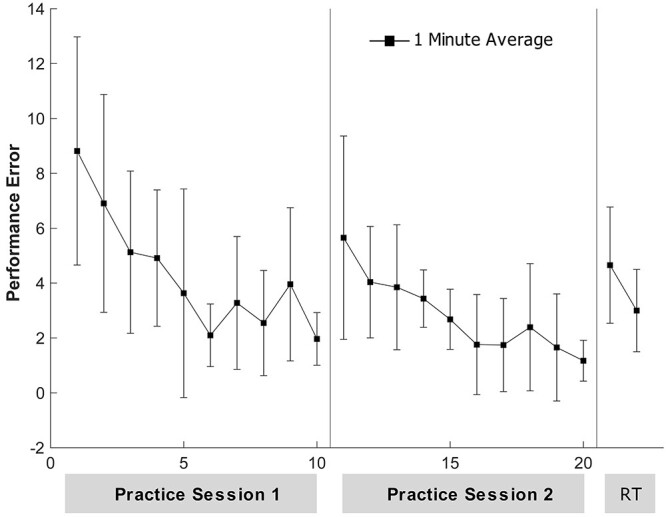
Representative learning curves. Hypothetical data from 2 practice sessions of a gait modification illustrate slowly improving performance as practice accumulates. Each data point represents a hypothetical 1-minute average of performance, and the error bars indicate SD. It is expected that a small performance loss between the end of practice 1 and the beginning of practice 2 occurs due to forgetting. Performance error typically lessens with accumulating practice; however, this does not suggest learning has occurred without a delayed retention test (RT). Additionally, although the performance curves might suggest significant improvements in performance have occurred over the 2 sessions, the retention test (RT) demonstrates that this improvement is not yet a permanent feature of their motor skill.
Retention tests occur after a practice period, but under the identical conditions that were present during practice and often without feedback present.13 Similar performance at retention compared with the end of practice suggests that learning has occurred. However, memory consolidation takes approximately 4 to 6 hours,28 so tests of retention within this time frame after practice are not appropriate.20 In a group with knee osteoarthritis, Richards et al12 directly examined the learning process of a toe-in gait pattern over 6 weeks. The median performance error at the immediate retention test after the first practice was 1.3° with 62% of steps ±2° of the target. However, when measured after 6 weeks of practice (a long-delayed retention), performance error was 3.6° and only 15% of steps were on target. This provides an example of how retention tests conducted too close to practice may falsely inflate learning outcomes. Future studies need to provide performance data from practice and delayed retention tests to more completely describe learning. Requiring that patients or participants return for delayed retention tests 6 hours post practice is often unreasonable. Instead, delayed retention tests can be performed at the next practice session before any practice has begun.
Another aspect of learning that can be inferred through behavioral means is the generalizability of a motor skill, which refers to the flexibility of a motor memory and whether it can be applied to a new context or skill.13 The transfer test is used to test generalizability by evaluating performance in a novel environment or on a related skill.13,20 Skill transfer may come in the form of positive transfer (better performance or faster learning) or negative transfer (worse performance or interference) between the practiced task and the transfer task.13,78 Although motor skill transfer is generally small, in cases where the 2 skills are very similar or the practiced skill is well learned, the magnitude of the transfer may be greater.79,80 Two studies of people with patellofemoral pain learning to reduce hip adduction angles during running used a single-leg squat as a transfer task.6,81 Only Willy et al6 found significant transfer, evidenced by reduced hip adduction during the squat, although both studies reported similar reductions (2–3°) that were maintained beyond 1 month post intervention. Given that many gait modifications are instructed in laboratory settings, and often using a treadmill,47,66,67,82,83 measuring performance during real-world gait may constitute a mild but highly applicable transfer test.
The automaticity with which a skill is performed is indicative of the learning stage.22 Well-learned tasks can be performed concurrently with other tasks (high automaticity) without substantial regression in performance, while the opposite occurs during early learning stages.84 To examine automaticity, 2 or more tasks are performed concurrently (eg, a primary gait modification and a secondary cognitive task) and performance is measured on both tasks independently and together.85 Using a multitask paradigm, simultaneously performing a toe-in gait modification and a cognitive task (visual Stroop task), Richards et al12 examined the progression of learning over 6 weeks in people with knee osteoarthritis. By follow-up, performance working in multitask condition had improved by 1.8° (a 72% improvement). Despite these promising results, in this study and others,86,87 no information regarding performance on the secondary task (eg, Stroop or serial subtraction) was reported. It is imperative that this information is provided as the participants could have directed attention solely on performing the gait modification, substantially lowering performance on the secondary task (see Plummer and Eskes88 for a clinically relevant discussion). The difficulty of the secondary task should also be considered so performance and learning of the primary gait modification are not severely impacted. Word-list generation is a good choice due to its moderate difficultly89 and easy implementation in the clinical setting. Overall, for dual-task assessment to be useful in understanding the process of learning gait modifications, more thorough reporting of methods and results is needed.
Several factors affect tests of learning and need consideration when interpreting results. Transient psychological factors, including motivation and focus, can influence learning assessments much like practice performance.13 Pain is a common complaint in MSK conditions, with the potential to modulate attention, cognitive resources,90,91 and motor strategies.92 Although this has yet to be examined within gait modification interventions involving people with MSK conditions, evidence from experimental pain studies suggests that the presence of pain alters learning. After 2 groups (experimental pain vs no pain) learned to resist an ankle plantarflexion perturbation during walking, performance was similar between groups only when the delayed retention test was completed in the same condition as was practiced.93,94 This suggests the presence of pain may alter contextual factors associated with the learning process and limit the transfer of skills that are learned with pain to contexts without pain. Unfortunately, we lack direct evidence in populations with symptomatic MSK conditions. Speculating based on the currently available data, clinicians and researchers need to consider the contextual effect of pain during practice and tests of learning, aiming to facilitate learning in pain-free contexts when possible.95 If this is not possible, doing so in similar pain-related contexts could be helpful in obtaining consistent results. It may be necessary to remind patients that a reduction in performance during a significant pain flare is not necessarily indicative of poor learning or a lack of effort.
Future Directions
Motor learning is a complex process with many contributing factors. Learning takes place over time and is an iterative process as motor memories are formed (encoded), strengthened (consolidated), and repeatedly accessed for future performance (retrieved). Assessments of learning need to accommodate the consolidation phase of learning and therefore should occur at least 6 hours after practice. One of the principal limitations in gait modification research to date has involved the lack of well-defined retention testing and incomplete reporting of learning outcomes. Future gait modification studies can consult this review and the broader motor learning literature to guide study design and reporting practices.
Unfortunately, much of the motor learning literature that this review is informed by has involved healthy individuals, the upper limb, discrete and simple tasks, and motor sequence learning or motor adaptation. Gait modification is somewhat unique in that it involves the lower limbs, is a continuous and somewhat complex task (especially in real-world settings), and is neither sequential nor adaptive in nature. While we recognize the application of this broader motor learning literature to gait modification may not be perfect, it supplies a foundation of evidence to further examine within the context of gait modification. More studies comparing different practice structures or feedback strategies are needed to further inform how to optimally design a gait modification intervention and corroborate the extant findings.
Gait modification has significant potential in the management of MSK injuries and disease. Through better application of motor learning strategies and assessments, gait modification interventions have a higher probability of succeeding, at least from a performance and learning perspective. From there, researchers and clinicians, in concert, can more precisely determine the best-use cases and conditions in which gait modifications can elicit beneficial biomechanical and clinical effects.
Contributor Information
Jesse M Charlton, Graduate Programs in Rehabilitation Sciences, University of British Columbia, Vancouver, BC, Canada; Motion Analysis and Biofeedback Laboratory, University of British Columbia, Vancouver, BC, Canada.
Janice J Eng, Rehabilitation Research Program, Vancouver Coastal Health Research Institute, Vancouver, BC, Canada; Department of Physical Therapy, University of British Columbia, Vancouver, BC, Canada.
Linda C Li, Department of Physical Therapy, University of British Columbia, Vancouver, BC, Canada; Arthritis Research Canada, Richmond, BC, Canada.
Michael A Hunt, Motion Analysis and Biofeedback Laboratory, University of British Columbia, Vancouver, BC, Canada; Department of Physical Therapy, University of British Columbia, Vancouver, BC, Canada.
Author Contributions
Concept/idea/research design: J.M. Charlton, J.J. Eng, L.C. Li, M.A. Hunt
Writing: J.M. Charlton, M.A. Hunt
Data collection: J.M. Charlton
Project management: J.M. Charlton, M.A. Hunt
Consultation: J.J. Eng, L.C. Li
Funding
This study was supported by the Canada Research Chairs, Government of Canada; the Canadian Institutes of Health Research, Doctoral Research Award and New Investigator Award; and the Michael Smith Foundation for Health Research, Career Scholar Award. The funding source had no role in the study’s design, conduct, and reporting.
Disclosures
The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and reported no conflicts of interest.
References
- 1. Araujo IL, Castro MC, Daltro C, Matos MA. Quality of life and functional independence in patients with osteoarthritis of the knee. Knee Surg Relat Res. 2016;28:219–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Teasell RW, Bhogal SK, Foley NC, Speechley MR. Gait retraining post stroke. Top Stroke Rehabil. 2003;10:34–65. [DOI] [PubMed] [Google Scholar]
- 3. Hordacre B, Birks V, Quinn S, Barr C, Patritti BL, Crotty M. Physiotherapy rehabilitation for individuals with lower limb amputation: a 15-year clinical series. Physiother Res Int. 2013;18:70–80. [DOI] [PubMed] [Google Scholar]
- 4. Richards R, van den Noort JC, Dekker J, Harlaar J. Gait retraining with real-time biofeedback to reduce knee adduction moment: systematic review of effects and methods used. Arch Phys Med Rehabil. 2017;98:137–150. [DOI] [PubMed] [Google Scholar]
- 5. Agresta C, Brown A. Gait retraining for injured and healthy runners using augmented feedback: a systematic literature review. J Orthop Sports Phys Ther. 2015;45:576–584. [DOI] [PubMed] [Google Scholar]
- 6. Willy RW, Scholz JP, Davis IS. Mirror gait retraining for the treatment of patellofemoral pain in female runners. Clin Biomech. 2012;27:1045–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barton CJ, Bonanno DR, Carr J, et al. Running retraining to treat lower limb injuries: a mixed-methods study of current evidence synthesised with expert opinion. Brit J Sport Med. 2016;50:513–526. [DOI] [PubMed] [Google Scholar]
- 8. Krishnan C. Learning and interlimb transfer of new gait patterns are facilitated by distributed practice across days. Gait Posture. 2019;70:84–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Krishnan C, Dharia AK, Augenstein TE, et al. Learning new gait patterns is enhanced by specificity of training rather than progression of task difficulty. J Biomech. 2019;88:33–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moore IS, Phillips DJ, Ashford KJ, Mullen R, Goom T, Gittoes MRJ. An interdisciplinary examination of attentional focus strategies used during running gait retraining. Scand J Med Sci Sports. 2019;10:1–11. [DOI] [PubMed] [Google Scholar]
- 11. Winstein CJ, Schmidt RA. Reduced frequency of knowledge of results enhances motor skill learning. J Exp Psychol Learn. 1990;16:677–691. [Google Scholar]
- 12. Richards R, van der Esch M, van den Noort JC, Harlaar J. The learning process of gait retraining using real-time feedback in patients with medial knee osteoarthritis. Gait Posture. 2018;62:1–6. [DOI] [PubMed] [Google Scholar]
- 13. Schmidt RA, Lee TD. Motor Learning And Performance: From Principles To Application. Champaign, IL: Human Kinetics; 2018. [Google Scholar]
- 14. Doyon J, Penhune V, Ungerleider LG. Distinct contribution of the cortico-striatal and cortico-cerebellar systems to motor skill learning. Neuropsychologia. 2003;41:252–262. [DOI] [PubMed] [Google Scholar]
- 15. Hallett M, Grafman J. Executive function and motor skill learning. In: Schmahmann JD, ed. International Review of Neurobiology. Vol 41. Cambridge, MA: Academic Press; 1997:297-323. [DOI] [PubMed] [Google Scholar]
- 16. Kim SJ, Ogilvie M, Shimabukuro N, Stewart T, Shin JH. Effects of visual feedback distortion on gait adaptation: comparison of implicit visual distortion versus conscious modulation on retention of motor learning. IEEE Trans Biomed Eng. 2015;62:2244–2250. [DOI] [PubMed] [Google Scholar]
- 17. Yokoyama H, Sato K, Ogawa T, Yamamoto S-I, Nakazawa K, Kawashima N. Characteristics of the gait adaptation process due to split-belt treadmill walking under a wide range of right-left speed ratios in humans. PLoS One. 2018;13:e0194875–e0194875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Torres-Oviedo G, Vasudevan E, Malone L, Bastian AJ. Locomotor adaptation. In: Green AM, Chapman CE, Kalaska JF, Lepore F, eds. Progress in Brain Research. Vol 191. Cambridge, MA: Elsevier; 2011:65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bohm S, Mademli L, Mersmann F, Arampatzis A. Predictive and reactive locomotor adaptability in healthy elderly: a systematic review and meta-analysis. Sports Med. 2015;45:1759–1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kantak SS, Winstein CJ. Learning-performance distinction and memory processes for motor skills: a focused review and perspective. Behav Brain Res. 2012;228:219–231. [DOI] [PubMed] [Google Scholar]
- 21. Lewthwaite R, Wulf G. Optimizing motivation and attention for motor performance and learning. Curr Opin Psychol. 2017;16:38–42. [DOI] [PubMed] [Google Scholar]
- 22. Fitts PM, Posner MI. Human Performance. Oxford, UK: Brooks/Cole; 1967. [Google Scholar]
- 23. Snoddy GS. Learning and stability: a psychophysiological analysis of a case of motor learning with clinical applications. J Appl Psychol. 1926;10:1–36. [Google Scholar]
- 24. Adams JA. A closed-loop theory of motor learning. J Mot Behav. 1971;3:111–149. [DOI] [PubMed] [Google Scholar]
- 25. Schmidt RA. A schema theory of discrete motor skill learning. Psychol Rev. 1975;82:225–260. [Google Scholar]
- 26. Haken H, Kelso JA, Bunz H. A theoretical model of phase transitions in human hand movements. Biol Cybern. 1985;51:347–356. [DOI] [PubMed] [Google Scholar]
- 27. Fuster JM. Memory in the Cerebral Cortex: An Empirical Approach to Neural Networks in the Human and Nonhuman Primate . Vol 28. Cambridge, MA: MIT Press; 1995. [Google Scholar]
- 28. Robertson EM. From creation to consolidation: a novel framework for memory processing. PLoS Biol. 2009;7:e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Butefisch CM, Khurana V, Kopylev L, Cohen LG. Enhancing encoding of a motor memory in the primary motor cortex by cortical stimulation. J Neurophysiol. 2004;91:2110–2116. [DOI] [PubMed] [Google Scholar]
- 30. Wolpert DM, Diedrichsen J, Flanagan JR. Principles of sensorimotor learning. Nat Rev Neurosci. 2011;12:739–751. [DOI] [PubMed] [Google Scholar]
- 31. Krakauer JW, Shadmehr R. Consolidation of motor memory. Trends Neurosci. 2006;29:58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Robertson EM. New insights in human memory interference and consolidation. Curr Biol. 2012;22:R66–R71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kantak SS, Sullivan KJ, Fisher BE, Knowlton BJ, Winstein CJ. Neural substrates of motor memory consolidation depend on practice structure. Nat Neurosci. 2010;13:923–925. [DOI] [PubMed] [Google Scholar]
- 34. Tanaka S, Honda M, Hanakawa T, Cohen LG. Differential contribution of the supplementary motor area to stabilization of a procedural motor skill acquired through different practice schedules. Cereb Cortex. 2010;20:2114–2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wymbs NF, Bastian AJ, Celnik PA. Motor skills are strengthened through reconsolidation. Curr Biol. 2016;26:338–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lee JLC, Nader K, Schiller D. An update on memory reconsolidation updating. Trends Cogn Sci. 2017;21:531–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Salmoni AW, Schmidt RA, Walter CB. Knowledge of results and motor learning: a review and critical reappraisal. Psychol Bull. 1984;95:355–386. [PubMed] [Google Scholar]
- 38. Sigrist R, Rauter G, Riener R, Wolf P. Augmented visual, auditory, haptic, and multimodal feedback in motor learning: a review. Psychon Bull Rev. 2013;20:21–53. [DOI] [PubMed] [Google Scholar]
- 39. Wulf G. Attentional focus and motor learning: a review of 15 years. Int Rev Sport Exer P. 2013;6:77–104. [Google Scholar]
- 40. Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance: a review of influential factors. Med Educ. 2010;44:75–84. [DOI] [PubMed] [Google Scholar]
- 41. Kal E, Prosee R, Winters M, van der Kamp J. Does implicit motor learning lead to greater automatization of motor skills compared to explicit motor learning? A systematic review. PLoS One. 2018;13:e0203591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Merbah S, Meulemans T. Learning a motor skill: effects of blocked versus random practice a review. Psychol Belg. 2011;51:15–48. [Google Scholar]
- 43. Schmidt RA, Wrisberg CA. Motor Learning and Performance: A Situation-Based Learning Approach. Champaign, IL: Human Kinetics; 2008. [Google Scholar]
- 44. Lage GM, Ugrinowitsch H, Apolinario-Souza T, Vieira MM, Albuquerque MR, Benda RN. Repetition and variation in motor practice: a review of neural correlates. Neurosci Biobehav Rev. 2015;57:132–141. [DOI] [PubMed] [Google Scholar]
- 45. Shea JB, Morgan RL. Contextual interference effects on the acquisition, retention, and transfer of a motor skill. J Exp Psychol Hum-L. 1979;5:179–187. [Google Scholar]
- 46. Hinkel-Lipsker JW, Hahn ME. The effects of variable practice on locomotor adaptation to a novel asymmetric gait. Exp Brain Res. 2017;235:2829–2841. [DOI] [PubMed] [Google Scholar]
- 47. Hunt MA, Charlton JM, Krowchuk NM, Tse CTF, Hatfield GL. Clinical and biomechanical changes following a 4-month toe-out gait modification program for people with medial knee osteoarthritis: a randomized controlled trial. Osteoarthr Cartil. 2018;26:903–911. [DOI] [PubMed] [Google Scholar]
- 48. Willy RW, Meardon SA, Schmidt A, Blaylock NR, Hadding SA, Willson JD. Changes in tibiofemoral contact forces during running in response to in-field gait retraining. J Sports Sci. 2016;34:1602–1611. [DOI] [PubMed] [Google Scholar]
- 49. Lee TD, Genovese ED. Distribution of practice in motor skill acquisition: different effects for discrete and continuous tasks. Res Q Exerc Sport. 1989;60:59–65. [DOI] [PubMed] [Google Scholar]
- 50. Winstein CJ. Knowledge of results and motor learning—implications for physical therapy. Phys Ther. 1991;71:140–149. [DOI] [PubMed] [Google Scholar]
- 51. Molier BI, Van Asseldonk EH, Hermens HJ, Jannink MJ. Nature, timing, frequency and type of augmented feedback; does it influence motor relearning of the hemiparetic arm after stroke? A systematic review. Disabil Rehabil. 2010;32:1799–1809. [DOI] [PubMed] [Google Scholar]
- 52. Karatsidis A, Richards RE, Konrath JM, et al. Validation of wearable visual feedback for retraining foot progression angle using inertial sensors and an augmented reality headset. J Neuroeng Rehabil. 2018;15:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Shull PB, Shultz R, Silder A, et al. Toe-in gait reduces the first peak knee adduction moment in patients with medial compartment knee osteoarthritis. J Biomech. 2013;46:122–128. [DOI] [PubMed] [Google Scholar]
- 54. Chen DKY, Haller M, Besier TF. Wearable lower limb haptic feedback device for retraining foot progression angle and step width. Gait Posture. 2017;55:177–183. [DOI] [PubMed] [Google Scholar]
- 55. Shull PB, Jirattigalachote W, Hunt MA, Cutkosky MR, Delp SL. Quantified self and human movement: a review on the clinical impact of wearable sensing and feedback for gait analysis and intervention. Gait Posture. 2014;40:11–19. [DOI] [PubMed] [Google Scholar]
- 56. Wulf G, McNevin N, Shea CH. The automaticity of complex motor skill learning as a function of attentional focus. Q J Exp Psychol A Hum Exp Psychol. 2001;54:1143–1154. [DOI] [PubMed] [Google Scholar]
- 57. Ellmers TJ, Young WR. Conscious motor control impairs attentional processing efficiency during precision stepping. Gait Posture. 2018;63:58–62. [DOI] [PubMed] [Google Scholar]
- 58. Yogev-Seligmann G, Sprecher E, Kodesh E. The effect of external and internal focus of attention on gait variability in older adults. J Mot Behav. 2017;49:179–184. [DOI] [PubMed] [Google Scholar]
- 59. Wulf G, Prinz W. Directing attention to movement effects enhances learning: a review. Psychon Bull Rev. 2001;8:648–660. [DOI] [PubMed] [Google Scholar]
- 60. Creaby MW, Franettovich Smith MM. Retraining running gait to reduce tibial loads with clinician or accelerometry guided feedback. J Sci Med Sport. 2016;19:288–292. [DOI] [PubMed] [Google Scholar]
- 61. Chow JY, Woo MT, Koh M. Effects of external and internal attention focus training on foot-strike patterns in running. Int J Spot Sci Coach. 2014;9:307–320. [Google Scholar]
- 62. Phan X, Grisbrook TL, Wernli K, Stearne SM, Davey P, Ng L. Running quietly reduces ground reaction force and vertical loading rate and alters foot strike technique. J Sports Sci. 2017;35:1636–1642. [DOI] [PubMed] [Google Scholar]
- 63. Peh SY, Chow JY, Davids K. Focus of attention and its impact on movement behaviour. J Sci Med Sport. 2011;14:70–78. [DOI] [PubMed] [Google Scholar]
- 64. Park JH, Shea CH, Wright DL. Reduced-frequency concurrent and terminal feedback: a test of the guidance hypothesis. J Mot Behav. 2000;32:287–296. [DOI] [PubMed] [Google Scholar]
- 65. Schmidt RA . Frequent Augmented Feedback Can Degrade Learning: Evidence and Interpretations. Tutorials in Motor Neuroscience. Dordrecht, Germany: Springer; 1991:59–75. [Google Scholar]
- 66. Richards R, van den Noort JC, van der Esch M, Booij MJ, Harlaar J. Gait retraining using real-time feedback in patients with medial knee osteoarthritis: feasibility and effects of a six-week gait training program. Knee. 2018;25:814–824. [DOI] [PubMed] [Google Scholar]
- 67. Shull PB, Silder A, Shultz R, et al. Six-week gait retraining program reduces knee adduction moment, reduces pain, and improves function for individuals with medial compartment knee osteoarthritis. J Orthop Res. 2013;31:1020–1025. [DOI] [PubMed] [Google Scholar]
- 68. Swinnen SP, Schmidt RA, Nicholson DE, Shapiro DC. Information feedback for skill acquisition: instantaneous knowledge of results degrades learning. J Exp Psychol Learn. 1990;16:706–716. [Google Scholar]
- 69. Wulf G, Lewthwaite R. Optimizing performance through intrinsic motivation and attention for learning: the OPTIMAL theory of motor learning. Psychon Bull Rev. 2016;23:1382–1414. [DOI] [PubMed] [Google Scholar]
- 70. Wulf G, Lewthwaite R, Cardozo P, Chiviacowsky S. Triple play: additive contributions of enhanced expectancies, autonomy support, and external attentional focus to motor learning. Q J Exp Psychol. 2018;71:824–831. [DOI] [PubMed] [Google Scholar]
- 71. Wood R, Bandura A. Impact of conceptions of ability on self-regulatory mechanisms and complex decision making. J Pers Soc Psychol. 1989;56:407–415. [DOI] [PubMed] [Google Scholar]
- 72. Pascua LA, Wulf G, Lewthwaite R. Additive benefits of external focus and enhanced performance expectancy for motor learning. J Sports Sci. 2015;33:58–66. [DOI] [PubMed] [Google Scholar]
- 73. Hoffmann TC, Lewis J, Maher CG. Shared decision making should be an integral part of physiotherapy practice. Physiotherapy. 2020;107:43–49. [DOI] [PubMed] [Google Scholar]
- 74. Lewthwaite R, Chiviacowsky S, Drews R, Wulf G. Choose to move: the motivational impact of autonomy support on motor learning. Psychon Bull Rev. 2015;22:1383–1388. [DOI] [PubMed] [Google Scholar]
- 75. Chiviacowsky S, Thofehrn Lessa H. Choices over feedback enhance motor learning in older adults. J Motor Learn Dev. 2017;5:304–318. [Google Scholar]
- 76. Cahill L, McGaugh JL, Weinberger NM. The neurobiology of learning and memory: some reminders to remember. Trends Neurosci. 2001;24:578–581. [DOI] [PubMed] [Google Scholar]
- 77. Davis I. Optimising the efficacy of gait retraining. Brit J Sport Med. 2018;52:624–625. [DOI] [PubMed] [Google Scholar]
- 78. Seidler RD. Neural correlates of motor learning, transfer of learning, and learning to learn. Exerc Sport Sci Rev. 2010;38:3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Schmidt RA, Young DE. Transfer of movement control in motor skill learning. In: Cormier SM, Hagman JD, eds., Transfer of Learning: Contemporary Research and Applications. San Diego, CA: Academic Press; 1987: 47–79. [Google Scholar]
- 80. Rosalie SM, Müller S. A model for the transfer of perceptual-motor skill learning in human behaviors. Res Q Exerc Sport. 2012;83:413–421. [DOI] [PubMed] [Google Scholar]
- 81. Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Brit J Sport Med. 2011;45:691–696. [DOI] [PubMed] [Google Scholar]
- 82. Crowell HP, Davis IS. Gait retraining to reduce lower extremity loading in runners. Clin Biomech. 2011;26:78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Napier C, MacLean CL, Maurer J, Taunton JE, Hunt MA. Real-time biofeedback of performance to reduce braking forces associated with running-related injury: an exploratory study. J Orthop Sports Phys Ther. 2019;49:136–144. [DOI] [PubMed] [Google Scholar]
- 84. Remy F, Wenderoth N, Lipkens K, Swinnen SP. Dual-task interference during initial learning of a new motor task results from competition for the same brain areas. Neuropsychologia. 2010;48:2517–2527. [DOI] [PubMed] [Google Scholar]
- 85. MacPherson SE. Definition: dual-tasking and multitasking. Cortex. 2018;106:313–314. [DOI] [PubMed] [Google Scholar]
- 86. Cheung RTH, An WW, Au IPH, Zhang JH, Chan ZYS, MacPhail AJ. Control of impact loading during distracted running before and after gait retraining in runners. J Sports Sci. 2018;36:1497–1501. [DOI] [PubMed] [Google Scholar]
- 87. An WW, Ting KH, Au IPH, et al. Neurophysiological correlates of gait retraining with real-time visual and auditory feedback. IEEE Trans Neural Syst Rehabil Eng. 2019;27:1341–1349. [DOI] [PubMed] [Google Scholar]
- 88. Plummer P, Eskes G. Measuring treatment effects on dual-task performance: a framework for research and clinical practice. Front Hum Neurosci. 2015;9:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Patel P, Lamar M, Bhatt T. Effect of type of cognitive task and walking speed on cognitive-motor interference during dual-task walking. Neuroscience. 2014;260:140–148. [DOI] [PubMed] [Google Scholar]
- 90. Torta DM, Legrain V, Mouraux A, Valentini E. Attention to pain! A neurocognitive perspective on attentional modulation of pain in neuroimaging studies. Cortex. 2017;89:120–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Keogh E, Moore DJ, Duggan GB, Payne SJ, Eccleston C. The disruptive effects of pain on complex cognitive performance and executive control. PLoS One. 2013;8:e83272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Kofler M, Glocker FX, Leis AA, et al. Modulation of upper extremity motoneurone excitability following noxious finger tip stimulation in man: a study with transcranial magnetic stimulation. Neurosci Lett. 1998;246:97–100. [DOI] [PubMed] [Google Scholar]
- 93. Bouffard J, Bouyer LJ, Roy JS, Mercier C. Tonic pain experienced during locomotor training impairs retention despite normal performance during acquisition. J Neurosci. 2014;34:9190–9195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Bouffard J, Bouyer LJ, Roy JS, Mercier C. Pain induced during both the acquisition and retention phases of locomotor adaptation does not interfere with improvements in motor performance. Neural Plast. 2016;2016:8539096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Boudreau SA, Farina D, Falla D. The role of motor learning and neuroplasticity in designing rehabilitation approaches for musculoskeletal pain disorders. Man Ther. 2010;15:410–414. [DOI] [PubMed] [Google Scholar]
- 96. Nissen MJ, Bullemer P. Attentional requirements of learning: evidence from performance measures. Cogn Psychol. 1987;19:1–32. [Google Scholar]
- 97. Temprado JJ, Monno A, Zanone PG, Kelso JA. Attentional demands reflect learning-induced alterations of bimanual coordination dynamics. Eur J Neurosci. 2002;16:1390–1394. [DOI] [PubMed] [Google Scholar]


