Abstract
Whereas some prior studies have explored whether alcohol increases the risk for victimization and/or whether distress resulting from victimization increases the risk for alcohol use, few studies have simultaneously tested these bidirectional hypotheses among a high-risk sample (i.e., undergraduate women), while including both sexual assault (SA) and intimate partner violence (IPV) victimization, and while exploring potential moderating effects of PTSD symptoms on these paths. Among 631 college women, the present study tested these bidirectional associations using cross-lagged panel models across two measurement periods (i.e., Time 1 [T1] and Time 2 [T2], six months later). Results suggested that T1 alcohol use increased risk for T2 SA (but not T2 IPV victimization), and PTSD symptoms moderated this association; at lower levels of PTSD symptoms, there were no significant associations between alcohol use and subsequent SA victimization, whereas at higher levels of PTSD symptoms, alcohol use predicted subsequent SA victimization. By contrast, the opposite directional hypothesis was not supported; neither T1 lifetime SA nor IPV were associated with T2 drinking, regardless of the level of their PTSD symptoms. Prevention and intervention efforts should simultaneously address risk factors for alcohol use and victimization using trauma-informed practices.
Keywords: intimate partner violence, unwanted sexual experiences, drinking, alcohol, PTSD, university students
1. Introduction
Sexual assault (SA) and intimate partner violence (IPV) are common among college women (Edwards et al., 2015; Fedina et al., 2018). College students are more likely to use alcohol than their same-age peers (Johnston et al., 2016), and both SA and IPV are associated with increased alcohol use (Dworkin et al., 2017; Shorey et al., 2011). However, it is unclear whether this is because alcohol use is associated with increased victimization risk, alcohol use increases following victimization (Shorey et al., 2011), or both (i.e., bidirectional associations), and whether these associations vary by the level of trauma-related distress (i.e., PTSD symptoms). Understanding the directionality of these associations could aid in developing violence prevention education and trauma-informed treatment. Thus, this study’s purpose was to test these two models within a prospective (cross-lagged panel) design among undergraduate women, a population at risk for SA, IPV, and heavy alcohol use.
1.1. Alcohol Use as a Risk Factor for Victimization
Perpetrators are always responsible for acts of SA or IPV. However, alcohol use may be associated with increased victimization risk via several mechanisms. First, college women who drink more frequently or heavily are often in settings (e.g., bars, parties), where they may be more likely to encounter perpetrators, consistent with routine activities theory (Gilbert et al., 2018; Mustaine & Tewksbury, 2002; Testa & Livingston, 2009). Perpetrators may also be drinking, which increases their disinhibited behavior, aggressiveness, or discounting cues of partner disinterest (consistent with theories of alcohol myopia, Steele & Josephs, 1990, and proximal effects of IPV, Crane et al., 2015). In addition, perpetrators may target intoxicated women who either cannot resist or are unable to consent (Kilpatrick et al., 2007; Testa et al., 2003). Lastly, alcohol use may impair risk perception (Cattaneo et al., 2007; Testa et al., 2003) via physiological effects on cognitive processes (e.g., decision-making, reaction time). Such impacts may thwart successful verbal or physical resistance to perpetrators (Macy et al., 2007).
1.2. Alcohol Use as a Consequence of Victimization
Another potential hypothesis is that victimization leads to increased alcohol use. Longitudinal studies (e.g., Shorey et al., 2011) and a meta-analysis (Dworkin et al., 2017) have found associations between victimization and alcohol use. The self-medication hypothesis (Khantzian, 1997) posits that alcohol use may represent an avoidant coping strategy wherein the survivor drinks to distract from psychological symptoms (Fossos et al., 2011; Kaysen et al., 2007; Khantzian, 1997; Parks et al., 2008; Parks et al., 2014; Ullman et al., 2013). Longitudinal studies with female undergraduates have indicated that SA (Lindgren et al., 2012) and IPV (Øverup et al., 2015) were related to more subsequent alcohol-related problems, associations mediated by coping drinking motives.
1.3. Bidirectional Associations
Some studies have simultaneously assessed bidirectional associations between alcohol use and victimization. Three studies have indicated that drinking was a predictor of sexual victimization (Gidycz et al., 2007; Mouilso et al., 2012; Testa, VanZile-Tamsen, & Livingston, 2007), but not that drinking increased following sexual victimization (Gidycz et al., 2007; Mouilso et al., 2012; Testa, Livingston, & Hoffman, 2007). None of these studies examined IPV victimization. Several studies found support for bidirectional associations between alcohol use and incapacitated SA in college and community women (Bryan et al. 2016; Norris et al., 2019).
With respect to alcohol use, a meta-analysis of longitudinal studies among adolescent and adult women showed positive bidirectional effects between IPV and alcohol use (Devries et al., 2014). However, fewer studies have focused on college samples. Shorey and colleagues (2016) found that college women reported higher rates of physical, sexual, and psychological IPV victimization on drinking (vs. nondrinking) days. By contrast, Parks and colleagues (2008) found that drinking increased the day after verbal, but not sexual or physical aggression, and Gomez and colleagues (2019) found no significant association between day-level drinking and IPV victimization among a sample of community college women. In a 5-year longitudinal study of 989 college women, Parks et al. (2014) found that severe sexual (but not physical) victimization was related to increased drinking. The literature in this area has varied widely in terms of assessment of type of abuse (physical, sexual, psychological victimization), measurement of drinking (frequency, quantity, alcohol-related problems, coping motives), and population (college students, women, adults), likely contributing to variation in results.
1.4. Moderating Effects of PTSD Symptoms
PTSD may moderate associations between alcohol use and later IPV and SA. Prior research suggests that women with PTSD are at higher risk of victimization (Messman-Moore et al., 2009). This may be because PTSD is associated with chronic hyperarousal (e.g., exaggerated startle), which may lead to difficulties differentiating among threatening stimuli (Yehuda & LeDoux, 2007), and/or chronic hyperarousal (e.g., numbing, resulting in greater immobility in response to threat (Lanius et al., 2017). Similarly, alcohol use may attenuate risk recognition and ability to assertively respond, due to cognitive effects of alcohol on information processing and impaired motor functioning and consciousness (Cattaneo et al., 2007; Macy et al., 2007). This is important because assertive resistance is associated with less completed rape (Brecklin & Ullman, 2005). The effects of alcohol use and PTSD on victimization may therefore be synergistic, leading to difficulties in women’s ability to resist perpetrators using assertive responses (e.g., fight back, yell) known to be associated with reduced risk for completed rape (Dardis et al., 2018). In addition, alcohol use may influence PTSD symptoms, as prior research suggests that alcohol may initially decrease symptoms through emotional blunting/negative reinforcement, but maintain or exacerbate symptoms over time through avoidance and rebound distress (Stewart, 1996). Alcohol use or PTSD severity alone may increase risk victimization risk, but their combination may be especially potent.
Second, when considering the directional association between victimization and future alcohol use, PTSD symptoms and alcohol use are often comorbid in trauma survivors (e.g., Debell et al., 2014; Pietrzak et al., 2011), especially survivors of violence (e.g., Najdowski & Ullman, 2009; Ullman & Filipas, 2001). Among young adults, presence of PTSD symptoms, not trauma exposure itself, has been associated with greater risk for subsequent alcohol consequences (Read et al., 2012). Further, Kaysen et al. (2014) found that, among a community sample of SA survivors, daily increases in PTSD symptoms were associated with increased risk of same-day drinking. To our knowledge, prior studies with college women have not tested PTSD symptoms as moderators of the associations between IPV victimization and alcohol use. As noted above, the self-medication hypothesis has been used to explain this association, using mediation models. However, some studies of community or college women have found a main effect of SA on alcohol use (Bryan et al. 2016; Norris et al., 2019; Ullman, 2016), while others have not in college women (Gidycz et al., 2007; Mouilso et al, 2012; Testa et al., 2007), even in a longitudinal study controlling for initial alcohol use (Blayney et al., 2016). This may be because heavy alcohol use is normative and relatively stable for many college women (McCauley et al., 2010; Mohler-Kuo et al., 2004). One possibility may be that victimization leads to increases in alcohol-related behaviors only in the context of greater PTSD, as lower PTSD symptoms do not overwhelm one’s capacity to cope (i.e., PTSD symptoms may moderate associations between victimization and alcohol use). In sum, PTSD symptoms may moderate either pathway, such that heavy alcohol use combined with high PTSD symptoms leads to increased future victimization, or victimization and high PTSD symptoms lead to heightened alcohol use.
1.5. The Current Study
The present study tests directional associations among alcohol use, IPV, and SA victimization and moderated associations by PTSD in college women across two timepoints within a cross-lagged panel design. We hypothesized that heavier alcohol use at Time 1 (T1) would be associated with increased risk for SA and IPV victimization at Time 2 (T2), six months later (Hypothesis 1; H1). Likewise, we hypothesized that T1 SA victimization and/or IPV would each be related to increased T2 alcohol use at 6-month follow-up (H2). Prior research on PTSD as a moderator did not lead to clear a priori hypotheses for either SA or IPV, so we tested whether PTSD symptoms moderated associations between (a) T1 alcohol use predicting T2 SA or IPV victimization (Research Question #1 and #2; RQ1 and RQ2, respectively), or (b) T1 SA or IPV victimization predicting T2 alcohol use (RQ3 and RQ4, respectively).
2. Method
2.1. Procedures
This is a secondary analysis of data from a larger intervention trial of an intervention aiming to improve social reactions to disclosure of SA/IPV (Edwards et al., 2020), which took place at a medium-size public university in the northeastern United States. The study was approved by the university’s IRB committee. The university’s Dean of students sent emails to randomly selected, full-time undergraduate students with study information and a direct link to an online (Qualtrics) 20-minute survey. We also provided study information by emailing professors with classes of 60+ students, visiting classrooms, and posting fliers. Overall, 1,831 students started the survey, of which 1,268 qualified, consented, and completed T1. Participants were randomized to the 2-session intervention group or control (waitlist) group; with a T2 6-month follow-up survey. Participants received $15 and $25 gift cards T1 and T2 surveys.
2.2. Participants
Of the 1,268 baseline participants, 889 participants (70.1%) completed the T2 survey. Among these, we selected women participants (71.0%; N=631). There were no significant differences in attrition for demographic variables (i.e., age, sexual orientation, year in college, race/ethnicity) nor by T1 focal constructs of interest. Sample demographics are shown in Table 1. Overall, participants were young, predominantly White Non-Hispanic, and heterosexual.
Table 1.
Demographics (N=631)
| Variable | n | M (SD)/% |
|---|---|---|
| Age | 631 | 19.48 (1.16) |
| Year in College | ||
| First | 173 | 27.4% |
| Second | 180 | 28.5% |
| Third | 146 | 23.1% |
| 4th and beyond | 132 | 20.9% |
| Race/Ethnicity | ||
| White | 568 | 90.4% |
| Asian/Asian American | 29 | 4.6% |
| Black/African American | 8 | 1.3% |
| American Indian or Alaska Native | 2 | 0.3% |
| Multiracial | 21 | 3.3% |
| Hispanic/Latino | 33 | 5.2% |
| Sexual Orientation | ||
| Heterosexual/Straight | 549 | 87.0% |
| Bisexual | 42 | 6.7% |
| Not sure | 13 | 2.1% |
| Pansexual | 10 | 1.6% |
| Lesbian | 7 | 1.1% |
| Asexual | 6 | 1.0% |
| Other (e.g., demisexual) | 2 | 0.3% |
| Decline to answer | 2 | 0.3% |
| T2: Whether Dated or in Relationship in Past 6 Months | ||
| Yes | 433 | 68.6% |
| No | 198 | 31.4% |
2.3. Measures
2.3.1. SA victimization
At T1, participants were asked if they ever experienced unwanted sexual contact or intercourse (0=no, 1=yes), with two questions: “In your lifetime, have you had sexual contact with someone when you didn’t want to?” and “In your lifetime, have you had sexual intercourse with someone when you didn’t want to?” (Banyard et al., 2007; Ward et al., 1991) after receiving a definition of unwanted behavior (i.e., “situations where you were certain at the time that you did not want to engage in the sexual experience and you either communicated in some way (e.g., you said no; you protested; you said you didn’t want to; you physically struggled; you cried) or you were intimidated or forced by someone or you were incapacitated (e.g., drunk, passed out)”. At T2, participants received questions about the previous 6 months. At both T1 and T2, responses were coded 0 if they said no to the two items and 1 if they said yes to either item.
2.3.2. IPV victimization
At T1, participants responded to four questions from the Revised Conflict Tactics scale Short Form (Straus & Douglas, 2004) asking about lifetime verbal/psychological or physical IPV (0=no, 1=yes) from a partner, including, “insulted or swore or shouted or yelled at me,” “punched or kicked or beat me up,” and “pushed, shoved, or slapped me.” At T2, participants were asked the same questions about the previous 6 months and were coded as 0 if they said no to all items and 1 if they said yes to any item.
2.3.3. Posttraumatic stress symptoms
At T1, participants responded to the PTSD Checklist for DSM-5 (Weathers et al., 2013). Those reporting lifetime SA or IPV answered questions about the most traumatic, emotional, intense lifetime SA or IPV experience. In order to have a measurable baseline for participants who might later experience IPV or SA, those who reported no lifetime T1 victimization answered the questions in reference to the “most traumatic or stressful lifetime event” (e.g., death/loss, surgery, life-threatening event to yourself other someone else, other similar intense event”). Twenty items such as “How much were you bothered by repeated, disturbing, and unwanted memories of the stressful experience?” were asked about the past month with responses ranging from 0=not at all to 4=extremely. Final score of 20 items was a sum of items (range=0–80; α=.95). Probable PTSD cutoff corresponds to a score of 33 (Bovin et al., 2015).
2.3.4. Alcohol use
At both timepoints, participants were asked, “In the past 30 days, have you ever, even just one time, consumed any kind of alcoholic beverage?” Response options were 0=no and 1=yes. Participants responding yes received several alcohol measures, including the Daily Drinking Questionnaire (Collins et al., 1985), which assesses average number of drinks for each day of a typical week in the past 30 days. Responses were summed for a total weekly drinks score.
2.4. Statistical Analysis
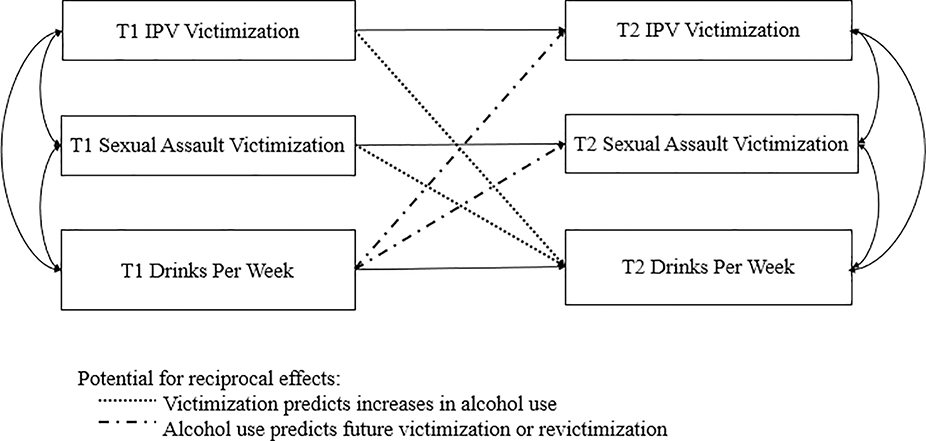
Cross-lagged analyses (Figure 1) tested the competing hypotheses that (a) T1 alcohol use predicted T2 victimization and (b) T1 victimization (SA or IPV) predicted T2 alcohol use. Within a cross-lagged panel model, the autoregressive associations (i.e., T1 to T2 association of the same variable), are controlled. The model was run using structural equation modeling in R, with the lavaan package, (v3.6, Rosseel, 2012) and full information maximum likelihood estimation. Intervention condition was a covariate. Finally, moderation was tested for the cross-lagged paths with interactions of T1 PTSD with each predictor individually. For significant interactions, we probed simple slopes at lower (1 SD below), average (mean), and higher (1 SD above) levels of PTSD symptoms.
Figure 1.
Hypothesized Cross-Lagged Model
Note: T1=Time 1; T2=Time 2.
3. Results
3.1. Descriptive Statistics
At T1, 39.9% (n=252) reported lifetime SA victimization, including 38.8% (n=238) who reported unwanted sexual contact and 25.0% (n=154) who reported unwanted sexual intercourse. Additionally, at T1, 37.2% (n=235) of women reported lifetime IPV, including 37.0% (n=231) women who experienced psychological/verbal IPV and 9.6% (n=60) who experienced physical IPV. At T2, 10.8% (n=68) of women reported SA victimization, including 9.9% (n=62) who reported unwanted sexual contact and 5.2% (n=32) who reported unwanted sexual intercourse. Also, at T2, 15.5% (n=98) reported IPV victimization within the past 6 months; this included 9.6% (n=60) women who experienced psychological/verbal IPV and 2.6% (n=16) women who experienced physical IPV (see bivariate associations in Table 2). Cross-sectionally and prospectively, T1 SA or IPV were associated with higher T1 and T2 weekly drinking.
Table 2.
Descriptive Statistics and Bivariate Associations among Constructs of Interest
| Variable | %/N or M (SD) | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. T1 SA | 39.9% (252) | .31*** | .26*** | .19*** | .27* | .09*** | .17*** |
| 2. T1 IPV | 37.2% (235) | -- | .14*** | .11** | .12** | .28*** | .13** |
| 3. T1 Drinks per Week | 6.46 (6.84) | -- | .08* | .18*** | .08* | .74*** | |
| 4. T1 PTSD Symptoms | 14.76 (15.44) | -- | .13** | .08* | .08* | ||
| 5. T2 SA | 10.8% (68) | -- | .16*** | .16*** | |||
| 6. T2 IPV | 15.5% (98) | -- | .08* | ||||
| 7. T2 Drinks per Week | 6.76 (7.06) | -- | |||||
Notes. IPV=Intimate Partner Violence; PTSD=Posttraumatic Stress Disorder. SA and IPV are dichotomous variables; correlations with these variables are point biserial, whereas remaining correlations are Pearson correlations.
T1=Time 1. T2=Time 2.
p < .05.
p < .01.
p < .001.
3.2. Cross-Lagged Panel Model (H1 and H2)
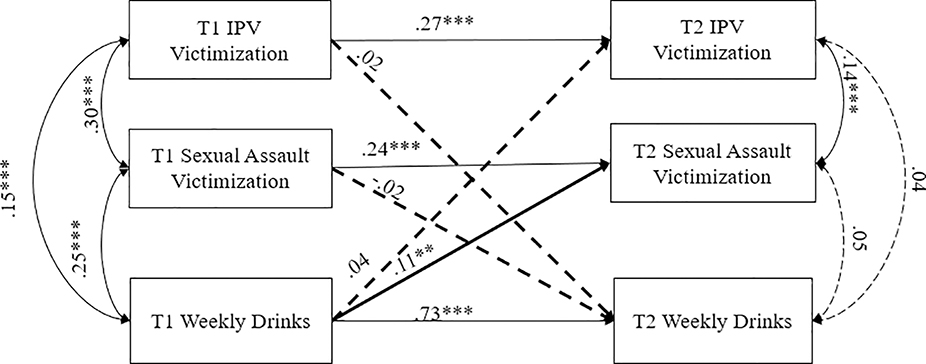
The hypothesis that alcohol would be significantly associated with future victimization (H1) was partially supported (Figure 2); higher average weekly drinks were related to increased risk of T2 SA (β=.11, p=.006). However, the path from T1 drinks per week to IPV was nonsignificant (β=.04, p=.327). The hypothesis that victimization predicts alcohol use (H2) was not supported for lifetime T1 IPV (β=.02, p=.457) or T1 SA (β=−.02, p=.442). Intervention condition was not associated with changes in any T2 outcomes (p’s>.05). The model fit the data well, χ2(8)=9.43, p=.307, CFI=.998, RMSEA=.017 [90% CI=<0.001-.051, p=.940]).
Figure 2.
Cross-Lagged Model for Drinks Per Week Variable
Notes. IPV = intimate partner violence; T1=Time 1; T2=Time 2. ***p <.001, **p <.01, *p <.05, ±p <.10. Dotted lines represent nonsignificant paths; paths of interest are bolded.
3.3. Moderation Model (RQ1-RQ4
Relevant to RQ1, PTSD symptomatology moderated the effects of T1 drinks per week on T2 SA (β=.10, p=.013). This model fit the data well (see Table 3). At lower levels of PTSD, the association between T1 weekly drinking and T2 SA victimization was nonsignificant (β=.002, p=.964). At mean levels of PTSD, (β=.10, p=.015) and higher levels of PTSD (1 SD above the mean; β=.19, p<.001), there was a positive association between T1 weekly drinking and T2 SA. In the presence of this interaction, the main effect of PTSD on T2 SA was marginal (β=.08, p=.056). There was also no main effect of PTSD on T2 IPV (β=.05, p=.180) or T2 drinks per week (β=.03, p=.371). By contrast, PTSD did not moderate the association between alcohol use and T2 IPV (RQ#2; β=−.02, p=.672). The main effects of PTSD on T2 IPV (β=.05, p=.173), and T2 drinks per week (β=.03, p=.371) were nonsignificant. However, there was a significant main effect of PTSD on T2 SA (β=.08, p =.040).
Table 3.
Moderated and Main Effects (RQ #1–4)
| Moderation Path Tested | ||||||||
|---|---|---|---|---|---|---|---|---|
| T1 Alcohol →T2 SA (RQ#1) | T1 Alcohol → T2 IPV (RQ#2) | SA → T2 Alcohol (RQ #3) | IPV → T2 Alcohol (RQ #4) | |||||
| Model Statistics | χ2(16)=26.53, p=.047, CFI=.986, RMSEA=.032 (90% CI[.004, .054], p=.908 | χ2(16)=32.48, p=.009, CFI=.978, RMSEA=.041 (90% CI[.020, .061], p=.759 | χ2(16)=448.26, p<.001, CFI=.627, RMSEA=.209 (90% CI[.193, .226], p<.001 | χ2(16)=363.79, p<.001, CFI=.674, RMSEA=.187 (90% CI[.170, .204], p<.001 | ||||
| β | p | β | p | β | p | β | p | |
| Moderation Effect (with PTSD) | .10 | .013 | −.02 | .672 | −.005 | .904 | .01 | .776 |
| Main Effect: PTSD→T2 SA | .08 | .056 | .08 | .040 | .08 | .039 | .08 | .039 |
| Main Effect: PTSD→T2 IPV | .05 | .180 | .05 | .173 | .04 | .291 | .05 | .245 |
| Main Effect: PTSD→T2 Alcohol | .03 | .371 | .03 | .371 | .04 | .331 | .02 | .522 |
Bolded results are significant at p <.05; italicized results are marginally significant at p <.10.
Finally, assessing RQ3 and RQ4, neither moderation model fit the data well, and moderation by PTSD symptomatology was not supported for either the path from T1 SA to T2 weekly drinks (β=−.005, p=.904, RQ3) or for the path from T1 IPV to T2 weekly drinks (β=.01, p=.776; RQ4). Intervention condition was not associated with changes in any of the T2 outcome variables across the four moderation analyses (p’s>.05).1
4. Discussion
The purpose of this study was to examine bidirectional associations between SA and IPV victimization and alcohol use among college women, and to test whether PTSD symptoms moderated these associations. Results partially supported H1, that alcohol use is associated with subsequent victimization, and generally supported the hypothesis that PTSD moderates the association between T1 alcohol use and T2 SA, but not IPV. The opposite directional (self-medication) hypothesis was not supported. The association between T1 alcohol use and T2 SA found in the present study is consistent with prior longitudinal research among college women (Gidycz et al., 2007; Mouilso et al., 2012). The present study extends this literature by including both SA and IPV, and assessing moderation by PTSD symptoms.
The finding that alcohol use was associated with increased risk for future SA, especially among those with higher PTSD symptoms, suggests a complex intersection among these risk factors. It is possible that alcohol use and PTSD symptoms increase victimization risk in a synergistic fashion: alcohol use may affect information processing and motor functioning (Cattaneo et al., 2007; Macy et al., 2007), while PTSD symptoms may interfere with risk recognition and utilization of resistance strategies (Ullman et al., 2009). Because this study did not assess alcohol use in the context of victimization events, this could not be directly tested. Additional research using diary designs should explore daily associations between alcohol use, PTSD symptoms, and victimization risk. It is important to note that alcohol being related to victimization risk does not mean that alcohol per se is the cause of victimization; a woman may drink heavily in her home alone and not be victimized as no one is there to attack her. Indeed, alcohol may be a proxy for being in high-risk contexts (e.g., fraternity parties, bars) where women may be targeted. The confluence of high-risk situations, motivated perpetrators, and vulnerable targets likely increases risk for victimization (Mustaine & Tewksbury, 2002).
Notably, alcohol use was not associated with increased risk for IPV victimization. Although this contradicts previous research (Shorey et al., 2011), it is possible that these variables were unrelated because of our limited IPV assessment. Some prior research found that alcohol use was associated with verbal, but not physical, IPV (Parks et al., 2008); these could not be separated due to their overlap and the small individual sample sizes for each, but this should be assessed in future studies. In addition, other factors, such as proximal alcohol use by the victim (Shorey et al., 2016) or the perpetrator (Moore et al., 2011; Shorey et al., 2014) may better explain women’s risk for IPV.
By contrast, IPV and SA victimization did not predict increases in alcohol use over time. This contradicts some prior research, which found that sexual assault and incapacitated SA in particular are associated with subsequent increases alcohol use and consequences (Bryan et al., 2016; Norris et al., 2019). One potential explanation is that this association is specific to incapacitated rape, or that the lifetime timeframe of T1 SA/IPV was not sufficiently proximal to detect effects on subsequent drinking. Our broad measure of SA victimization included two lifetime items that could encompass child, adolescent, or adult experiences of completed rape and sexual coercion. The heterogeneity in time since victimization or victimization severity may dilute effects on recent distress and drinking. Future studies should explore alcohol consequences or coping motives. Whereas some studies have found support for mediating effects of drinking to cope (e.g., Fossos et al., 2011), Hawn and colleagues (2020) emphasize the importance of future research efforts exploring PTSD-specific drinking motives (e.g., drinking to alleviate hyperarousal, re-experiencing symptoms) rather than general coping motives.
There are some limitations to the present study, which was a secondary analysis of data from a randomized clinical trial of an intervention to improve college students’ responses to sexual assault disclosures (Authors, 2020). First, while the cross-lagged design permitted assessment across two timepoints, our measure of T2 alcohol use relates only to past-month alcohol use; therefore, we are unable to examine alcohol use across the entire interim. Future studies might incorporate diary designs to explore more proximal associations, or longer follow-up periods to examine longer-term effects. Including more than two assessments would strengthen confidence in results and permit testing of mediation. Second, this sample was largely demographically homogeneous, and results may not generalize to more diverse samples. Next, although alcohol use was assessed over the past month at T1, victimization was assessed over participants’ lifetimes, which may explain the support found for the risk hypothesis (both assessment periods are more proximal/recent) but not the self-medication hypothesis (as T1 victimization could have been recent or more distal). There may be other important mediators or moderators of these associations including PTSD-specific or tension-reduction motives (Ullman et al., 2005).
Additional limitations include limited 2-item screening questions which may not have fully captured SA and IPV experiences. Further, effects of IPV in this study may be underestimated given that only 69% of students were in intimate partnerships in the past 6 months at T2, and therefore could not have experienced T2 IPV. PTSD assessment also differed across participants. Those who reported victimization experiences were asked to anchor their PTSD symptoms to their victimization, but those without SA/IPV had their symptoms anchored to their most traumatic or stressful event. Thus, for those without IPV/SA, events may not meet the Criterion A trauma definition in DSM-5 (APA, 2013). Under such circumstances, this measure more accurately assesses stress/anxiety-related symptoms rather than PTSD. Finally, there was no data on childhood trauma available in this study, so future research is needed to assess and control for the role of this factor in both later victimization, PTSD, and drinking.
Despite these limitations, there are several implications from the present study. First, the finding that alcohol use increases risk for future SA victimization suggests the importance of addressing alcohol use in college students, including in the context of sexual violence prevention programs targeting both potential perpetrators and victims. For example, Gilmore et al. (2018) evaluated a combined alcohol use and sexual assault risk reduction program and found that the sexual assault risk reduction content reduced alcohol-induced blackouts and incapacitation, and a combined alcohol use and sexual assault risk reduction program reduced alcohol-induced blackouts only. In addition, the finding that alcohol use is especially associated with increased risk when PTSD symptoms are more severe suggests the need to address PTSD symptoms among college students. The finding that alcohol use is associated with future SA victimization risk (especially among those with higher PTSD symptoms) should not be seen as evidence for victims’ responsibility for assaults. Instead, our findings suggest that addressing both PTSD and alcohol use among college students as a whole, may reduce victimization risk.
Highlights.
Tests two theories of associations between alcohol use and victimization
T1 alcohol use increased risk for T2 sexual assault, not intimate partner violence
PTSD symptoms moderated this association; at higher levels, association was stronger
The self-medication hypothesis was not supported
Acknowledgments:
The authors owe a great deal of gratitude to the participants for the time and energy spent on this study. Thank you to Tori Oestmann and Samantha Moore who coded the data. We would also like to thank Jania Marshall, Caroline Leyva, Robert Eckstein, and Jane Stapleton for their contributions to the larger study, as well as the 20+ research assistants and program facilitators at University of New Hampshire, including Prentiss Phillips, Victoria Stanek, Allison Depuy, Drew Doyle, Lianna Nawn, Meredith Baker, Nicole Westfall, Lauren Flynn, Hannah Nordstorm, Kristina Kalla, Michael Green-Kelsey, Abi Beaulieu, Eleonora Giovine, Ross Jones, and Sarah Russo. Without these individuals, this project would not have been possible.
Role of Funding Sources: Funding for this study was provided by the National Institute of Alcohol Abuse and Alcoholism (NIAAA) Grant R34AA024849 (PI: Edwards). Manuscript preparation for this article was additionally supported by National Institute of Alcohol Abuse and Alcoholism (NIAAA) Grant R00AA026317 (PI: Dworkin). NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. The findings and implications presented in this paper do not represent the official views of the NIH.
Funding for this study was provided by the National Institute of Alcohol Abuse and Alcoholism (NIAAA) Grant R34AA024849 (PI: Edwards). Manuscript preparation for this article was additionally supported by National Institute of Alcohol Abuse and Alcoholism (NIAAA) Grant R00AA026317 (PI: Dworkin). The findings and implications presented in this paper do not represent the official views of the NIH.
Footnotes
Conflict of Interest: All authors declare that they have no conflicts of interest.
Declaration of Interest: None.
Author Disclosures
All persons who meet authorship criteria are listed as authors, and all authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the manuscript. Furthermore, each author certifies that this material or similar material has not been and will not be submitted to or published in any other publication before its appearance in Addictive Behaviors.
Author Agreement
None of the original material contained in the manuscript has been published or submitted for publication elsewhere. All authors have approved the manuscript for submission, made substantial contributions to the conception, design, gathering, and/or interpretation of the data, and to the writing and intellectual content of the article.
Models were also tested using the peak number of drinks per week in the past month (Dimeff et al., 1999) and the number of heavy drinking episodes (defined as the number of times they had 5+ drinks in a two-hour period over the past month). Inconsistent with the model for weekly drinks, there were no main effects of either T1 peak drinks or heavy drinking episodes on T2 SA. However, consistent with the model for weekly drinks, PTSD symptomatology significantly moderated the effects of T1 heavy drinking episodes (p<.001) and peak drinks (p = .046) on T2 SA (but not IPV), such that the association was significant only at high levels of PTSD symptoms (RQ#1). There were no significant results in the opposite direction, as neither T1 SA nor IPV predicted T2 peak drinks or heavy drinking episodes, and PTSD symptomatology did not moderate these associations (p’s >.05).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Christina M. Dardis, Psychology, Towson University, 8000 York Road, Towson, MD 21252.
Sarah E. Ullman, Department of Criminology, Law and Justice, University of Illinois at Chicago, 1007 West Harrison Street, Chicago, IL 60607-7140.
Lindsey M. Rodriguez, Psychology, University of South Florida, 4202 E. Fowler Ave., Tampa, FL 33620.
Emily A. Waterman, Developmental Psychology, Bennington College, 1 College Drive, Bennington, VT, 05201.
Emily R. Dworkin, Psychiatry and Behavioral Sciences, University of Washington School of Medicine, 1100 NE 45th St. Ste. 300, Seattle, WA 98105.
Katie M. Edwards, Educational Psychology, Nebraska Center for Research on Children, Youth, Families, and Schools, University of Nebraska—Lincoln.
References
- American Psychological Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). American Psychiatric Pub. [Google Scholar]
- Banyard VL, Ward S, Cohn ES, Plante EG, Moorhead C, & Walsh W (2007). Unwanted Sexual Contact on Campus: A Comparison of Women’s and Men’s Experiences. Violence and Victims, 22(1), 52–70. 10.1891/vv-v22i1a004 [DOI] [PubMed] [Google Scholar]
- Blayney J, Read J, & Colder C (2016). Role of alcohol in college sexual victimization and postassault adaptation. Psychological Trauma : Theory, Research, Practice and Policy, 8 10.1037/tra0000100 [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28(11), 1379–1391. 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Brecklin LR, & Ullman SE (2005). Self-defense or assertiveness training and women’s responses to sexual attacks. Journal of Interpersonal Violence, 20(6), 738–762. 10.1177/0886260504272894 [DOI] [PubMed] [Google Scholar]
- Bryan AEB, Norris J, Abdallah DA, Stappenbeck CA, Morrison DM, Davis KC, George WH, Danube CL, & Zawacki T (2016). Longitudinal Change in Women’s Sexual Victimization Experiences as a Function of Alcohol Consumption and Sexual Victimization History: A Latent Transition Analysis. Psychology of Violence, 6(2), 271–279. 10.1037/a0039411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cattaneo LB, Bell ME, Goodman LA, & Dutton MA (2007). Intimate partner violence victims’ accuracy in assessing their risk of re-abuse. Journal of Family Violence, 22(6), 429–440. 10.1007/s10896-007-9097-8 [DOI] [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200. 10.1037/0022-006X.53.2.189 [DOI] [PubMed] [Google Scholar]
- Crane CA, Godleski SA, Przybyla SM, Schlauch RC, & Testa M (2016). The proximal effects of acute alcohol consumption on male-to-female aggression: A meta-analytic review of the experimental literature. Trauma, Violence, & Abuse, 17(5), 520–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dardis CM, Ullman SE, & Brecklin LR (2018). Chapter 6 - “It’s Worth the Fight!”: Women Resisting Rape In Orchowski LM & Gidycz CA (Eds.), Sexual Assault Risk Reduction and Resistance (pp. 111–133). Academic Press; 10.1016/B978-0-12-805389-8.00006-2 [DOI] [Google Scholar]
- Debell F, Fear NT, Head M, Batt-Rawden S, Greenberg N, Wessely S, & Goodwin L (2014). A systematic review of the comorbidity between PTSD and alcohol misuse. Social Psychiatry and Psychiatric Epidemiology, 49(9), 1401–1425. 10.1007/s00127-014-0855-7 [DOI] [PubMed] [Google Scholar]
- Devries KM, Child JC, Bacchus LJ, Mak J, Falder G, Graham K, … & Heise L (2014). Intimate partner violence victimization and alcohol consumption in women: A systematic review and meta‐analysis. Addiction, 109(3), 379–391. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Baer JS, Kivlahan DR, & Marlatt GA (1999). Brief alcohol screening and intervention for college students (BASICS). The Guilford Press. [Google Scholar]
- Dworkin ER, Menon SV, Bystrynski J, & Allen NE (2017). Sexual assault victimization and psychopathology: A review and meta-analysis. Clinical Psychology Review, 56, 65–81. 10.1016/j.cpr.2017.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards KM, Sylaska KM, Barry JE, Moynihan MM, Banyard VL, Cohn ES, Walsh WA, & Ward SK (2015). Physical Dating Violence, Sexual Violence, and Unwanted Pursuit Victimization: A Comparison of Incidence Rates Among Sexual-Minority and Heterosexual College Students. Journal of Interpersonal Violence, 30(4), 580–600. 10.1177/0886260514535260 [DOI] [PubMed] [Google Scholar]
- Fedina L, Holmes JL, & Backes BL (2018). Campus Sexual Assault: A Systematic Review of Prevalence Research From 2000 to 2015. Trauma, Violence, & Abuse, 19(1), 76–93. 10.1177/1524838016631129 [DOI] [PubMed] [Google Scholar]
- Fossos N, Kaysen D, Neighbors C, Lindgren KP, & Hove MC (2011). Coping motives as a mediator of the relationship between sexual coercion and problem drinking in college students. Addictive Behaviors, 36(10), 1001–1007. 10.1016/j.addbeh.2011.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gidycz, Loh C, Lobo T, Rich C, Lynn SJ, & Pashdag J. (2007). Reciprocal relationships among alcohol use, risk perception, and sexual victimization: A prospective analysis. Journal of American College Health, 56(1), 5–14. [DOI] [PubMed] [Google Scholar]
- Gilbert L, Sarvet AL, Wall M, Walsh K, Reardon L, Wilson P, Santelli J, Khan S, Thompson M, Hirsch JS, & Mellins CA (2018). Situational Contexts and Risk Factors Associated with Incapacitated and Nonincapacitated Sexual Assaults Among College Women. Journal of Women’s Health, 28(2), 185–193. 10.1089/jwh.2018.7191 [DOI] [PubMed] [Google Scholar]
- Gilmore AK, Bountress KE, Selmanoff M, & George WH (2018). Reducing Heavy Episodic Drinking, Incapacitation, and Alcohol-Induced Blackouts: Secondary Outcomes of a Web-Based Combined Alcohol Use and Sexual Assault Risk Reduction Intervention. Violence Against Women, 24(11), 1299–1313. 10.1177/1077801218787934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez J, Orchowski L, Pearlman DN, & Zlotnick C (2019). Alcohol use and intimate partner violence among community college women: an exploration of protective factors. Violence and gender, 6(3), 187–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawn SE, Cusack SE, & Amstadter AB (2020). A Systematic Review of the Self‐Medication Hypothesis in the Context of Posttraumatic Stress Disorder and Comorbid Problematic Alcohol Use—Hawn—- Journal of Traumatic Stress—Wiley Online Library. Journal of Traumatic Stress, Advance online publication. 10.1002/jts.22521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, & Schulenberg JE (2016). Monitoring the Future National Survey Results on Drug Use, 1975–2015: Overview, Key Findings on Adolescent Drug Use In Institute for Social Research. Institute for Social Research; https://eric.ed.gov/?id=ED578539 [Google Scholar]
- Kaysen D, Dillworth TM, Simpson T, Waldrop A, Larimer ME, & Resick PA (2007). Domestic violence and alcohol use: Trauma-related symptoms and motives for drinking. Addictive Behaviors, 32(6), 1272–1283. 10.1016/j.addbeh.2006.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaysen D, Stappenbeck C, Rhew I, & Simpson T (2014). Proximal relationships between PTSD and drinking behavior. European Journal of Psychotraumatology, 5, 1-N.PAG. 10.3402/ejpt.v5.26518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ (1997). The Self-Medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications. Harvard Review of Psychiatry, 4(5), 231–244. 10.3109/10673229709030550 [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Ruggiero KJ, Conoscenti LM, & McCauley J (2007). Drug-facilitated, Incapacitated, and Forcible Rape: A National Study: (667182007–001) [Data set]. American Psychological Association; 10.1037/e667182007-001 [DOI] [Google Scholar]
- Lanius RA, Rabellino D, Boyd JE, Harricharan S, Frewen PA, & McKinnon MC (2017). The innate alarm system in PTSD: Conscious and subconscious processing of threat. Current Opinion in Psychology, 14, 109–115. 10.1016/j.copsyc.2016.11.006 [DOI] [PubMed] [Google Scholar]
- Lindgren KP, Neighbors C, Blayney JA, Mullins PM, & Kaysen D (2012). Do drinking motives mediate the association between sexual assault and problem drinking? Addictive Behaviors, 37(3), 323–326. 10.1016/j.addbeh.2011.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macy RJ, Nurius PS, & Norris J (2007). Latent profiles among sexual assault survivors: Implications for defensive coping and resistance. Journal of Interpersonal Violence, 22(5), 543–565. 10.1177/0886260506298841 [DOI] [PubMed] [Google Scholar]
- McCauley JL, Calhoun KS, & Gidycz CA (2010). Binge Drinking and Rape: A Prospective Examination of College Women With a History of Previous Sexual Victimization. Journal of Interpersonal Violence, 25(9), 1655–1668. 10.1177/0886260509354580 [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Ward RM, & Brown AL (2009). Substance Use and PTSD Symptoms Impact the Likelihood of Rape and Revictimization in College Women. Journal of Interpersonal Violence, 24(3), 499–521. 10.1177/0886260508317199 [DOI] [PubMed] [Google Scholar]
- Mohler-Kuo M, Dowdall GW, Koss MP, & Wechsler H (2004). Correlates of rape while intoxicated in a national sample of college women. Journal of Studies on Alcohol, 65(1), 37–45. 10.15288/jsa.2004.65.37 [DOI] [PubMed] [Google Scholar]
- Moore TM, Elkins SR, McNulty JK, Kivisto AJ, & Handsel VA (2011). Alcohol use and intimate partner violence perpetration among college students: Assessing the temporal association using electronic diary technology. Psychology of Violence, 1(4), 315–328. 10.1037/a0025077 [DOI] [Google Scholar]
- Mouilso ER, Fischer S, & Calhoun KS (2012). A Prospective Study of Sexual Assault and Alcohol Use Among First-Year College Women. Violence and Victims, 27(1), 78–94. 10.1891/0886-6708.27.1.78 [DOI] [PubMed] [Google Scholar]
- Mustaine EE, & Tewksbury R (2002). Sexual Assault of College Women: A Feminist Interpretation of a Routine Activities Analysis. Criminal Justice Review, 27(1), 89–123. 10.1177/073401680202700106 [DOI] [Google Scholar]
- Najdowski CJ, & Ullman SE (2009). Prospective effects of sexual victimization on PTSD and problem drinking. Addictive Behaviors, 34(11), 965–968. 10.1016/j.addbeh.2009.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris AL, Carey KB, Walsh JL, Shepardson RL, & Carey MP (2019). Longitudinal assessment of heavy alcohol use and incapacitated sexual assault: A cross-lagged analysis. Addictive Behaviors, 93, 198–203. 10.1016/j.addbeh.2019.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Øverup CS, DiBello AM, Brunson JA, Acitelli LK, & Neighbors C (2015). Drowning the pain: Intimate partner violence and drinking to cope prospectively predict problem drinking. Addictive Behaviors, 41, 152–161. 10.1016/j.addbeh.2014.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks KA, Hsieh Y-P, Bradizza CM, & Romosz AM (2008). Factors influencing the temporal relationship between alcohol consumption and experiences with aggression among college women. Psychology of Addictive Behaviors, 22(2), 210–218. 10.1037/0893-164X.22.2.210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parks KA, Hsieh Y-P, Taggart C, & Bradizza CM (2014). A longitudinal analysis of drinking and victimization in college women: Is there a reciprocal relationship? Psychology of Addictive Behaviors : Journal of the Society of Psychologists in Addictive Behaviors, 28(4), 943–951. 10.1037/a0036283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25(3), 456–465. 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Colder CR, Merrill JE, Ouimette P, White J, & Swartout A (2012). Trauma and Posttraumatic Stress Symptoms Predict Alcohol and Other Drug Consequence Trajectories in the First Year of College. Journal of Consulting and Clinical Psychology, 80(3), 426–439. 10.1037/a0028210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y (2012). lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software, 48(1), 1–36. 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- Shorey RC, Moore TM, McNulty JK, & Stuart GL (2016). Do Alcohol and Marijuana Increase the Risk for Female Dating Violence Victimization? A Prospective Daily Diary Investigation. Psychology of Violence, 6(4), 509–518. 10.1037/a0039943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey RC, Stuart GL, & Cornelius TL (2011). Dating Violence and Substance Use in College Students: A Review of the Literature. Aggression and Violent Behavior, 16(6), 541–550. 10.1016/j.avb.2011.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shorey RC, Stuart GL, McNulty JK, & Moore TM (2014). Acute alcohol use temporally increases the odds of male perpetrated dating violence: A 90-day diary analysis. Addictive Behaviors, 39(1), 365–368. 10.1016/j.addbeh.2013.10.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele CM, & Josephs RA (1990). Alcohol myopia: Its prized and dangerous effects. American Psychologist, 45(8), 921–933. 10.1037/0003-066X.45.8.921 [DOI] [PubMed] [Google Scholar]
- Stewart S (1996). Alcohol Abuse in Individuals Exposed to Trauma: A Critical Review. Psychological Bulletin, 120, 83–112. 10.1037/0033-2909.120.1.83 [DOI] [PubMed] [Google Scholar]
- Testa M, & Livingston JA (2009). Alcohol Consumption and Women’s Vulnerability to Sexual Victimization: Can Reducing Women’s Drinking Prevent Rape? Substance Use & Misuse, 44(9–10), 1349–1376. 10.1080/10826080902961468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa M, Livingston JA, & Hoffman JH (2007). Does sexual victimization predict subsequent alcohol consumption? A prospective study among a community sample of women. Addictive Behaviors, 32(12), 2926–2939. 10.1016/j.addbeh.2007.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Testa M, Livingston JA, Vanzile-Tamsen C, & Frone MR (2003). The role of women’s substance use in vulnerability to forcible and incapacitated rape. Journal of Studies on Alcohol, 64(6), 756–764. 10.15288/jsa.2003.64.756 [DOI] [PubMed] [Google Scholar]
- Testa M, VanZile-Tamsen C, & Livingston JA (2007). Prospective Prediction of Women’s Sexual Victimization by Intimate and Nonintimate Male Perpetrators. Journal of Consulting and Clinical Psychology, 75(1), 52–60. 10.1037/0022-006X.75.1.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE (2016). Sexual revictimization, PTSD, and problem drinking in sexual assault survivors. Addictive Behaviors, 53, 7–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, & Filipas HH (2001). Predictors of PTSD Symptom Severity and Social Reactions in Sexual Assault Victims. Journal of Traumatic Stress, 14(2), 369–389. 10.1023/A:1011125220522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, & Starzynski LL (2005). Trauma exposure, posttraumatic stress disorder and problem drinking in sexual assault survivors. Journal of Studies on Alcohol, 66(5), 610–619. 10.15288/jsa.2005.66.610 [DOI] [PubMed] [Google Scholar]
- Ullman SE, Najdowski CJ, & Filipas HH (2009). Child sexual abuse, post-traumatic stress disorder, and substance use: Predictors of revictimization in adult sexual assault survivors. Journal of Child Sexual Abuse, 18(4), 367–385. 10.1080/10538710903035263 [DOI] [PubMed] [Google Scholar]
- Ullman SE, Relyea M, Peter-Hagene L, & Vasquez AL (2013). Trauma histories, substance use coping, PTSD, and problem substance use among sexual assault victims. Addictive Behaviors, 38(6), 2219–2223. 10.1016/j.addbeh.2013.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward SK, Chapman K, Cohn E, White S, & Williams K (1991). Acquaintance Rape and the College Social Scene. Family Relations, 40(1), 65–71. 10.2307/585660 [DOI] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). National Center for PTSD. [Google Scholar]
- Zinzow HM, Thompson MP, Goree J, Fulmer CB, Greene C, & Watts HA (2018). Evaluation of a College Sexual Violence Prevention Program Focused on Education, Bystander Intervention, and Alcohol Risk Reduction. College Student Affairs Journal, 36(2), 110–125. 10.1353/csj.2018.0019 [DOI] [Google Scholar]