Supplemental Digital Content is Available in the Text.
Keywords: patient monitoring, patient safety, video monitor technician, video monitoring
Abstract
Background:
Sitters are often used in the inpatient setting as a measure to ensure safety of patients with cognitive and behavioral concerns.
Problem:
Sitters are costly, and evidence is lacking that their presence produces safer outcomes. Continuous video monitoring is a safe alternative; yet, there is a lack of best practices and implementation strategies.
Approach:
A large academic medical center in the Pacific Northwest introduced continuous video monitoring as an adjunct measure to replace sitter use when appropriate. Adoption of the technology was influenced by nurse enculturation, leader standard work (standard parameters used by nurse leaders for process improvement), data tracking management, and patient/family feedback.
Outcomes:
Continuous video monitoring is a bridge for the nursing staff to enhance safety for patients and an additional safety intervention when sitter use is not reasonable.
Conclusion:
Utilizing technology such as continuous video monitoring can relieve sitters to allow for optimal productivity, increased safety, cost reduction, and nurse/family satisfaction.
Enhancing patient safety while optimizing resources is a continued area of focus for the global health care environment. Sitters, or one-to-one observers, are commonly used in the inpatient setting to meet monitoring needs of high-risk patients. Yet, sitters are a costly intervention that is resource intensive. Research is lacking that supports the use of sitters as a measure to reduce falls or improve safety outcomes.1 The level of care that patients with cognitive impairments and/or behavioral concerns require in inpatient setting often includes additional monitoring interventions. Inpatient sitter needs continue to expand, as there is a high prevalence of mental health conditions and low rates of access to care within the community.2 In addition to mental health disparities, adult and pediatric patient populations require additional inpatient monitoring for suicide risk, substance withdrawal, delirium, fall risk, eating disorders, elopement, and general safety concerns.
Continuous video monitoring (CVM) of patients is an advancing technology with a growing body of literature that can assist organizations in meeting operational demands and provide safe optimal care. The specific aim of this article is to report systemwide results of CVM implementation at a large academic medical center and associated best practices identified through project implementation.
PROBLEM
Multiple compounding factors result in the increased demand for additional safety monitoring in the inpatient setting. One such factor is that mental health conditions are on the rise in all age groups. Fifty percent of Americans will meet the criteria for a Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) sometime in their life, with first onset usually in childhood or adolescence.3 Among adolescents, major depressive episodes at the age of 12 to 17 years increased 52% in 2017.4 Americans have a lack of available resources within the community, to treat these conditions appropriately. More than 10 million adults have an unmet need for mental health treatment; 70% of youth with major depression are still in need of treatment.5 When needs cannot be met within the community, patients are driven into the inpatient setting whether for an acute medical need and/or for escalation of behavioral needs.
Delirium is another frequently occurring condition that predisposes the need for one-to-one sitter utilization within the inpatient setting. It is associated with poor outcomes, functional and cognitive decline, increased length of stay, and mortality.6 The overall prevalence of delirium is 50% in hospitalized elderly persons.7
Other conditions raise acuity within the inpatient setting. Adult and pediatric patient populations require additional inpatient monitoring for suicide risk, substance withdrawal, fall risk, eating disorders, elopement, and general safety concerns. Providing one-to-one care for all is costly, ineffective, and resource-intensive.
At a large academic Magnet-designated medical center in the Pacific Northwest of the United States, nursing leadership identified that the need for sitters was rising and lack of alternative resources was present. This impacted staff satisfaction, patient safety, and productivity. CVM was identified as a solution. As a newer technology, CVM has promising results related to patient falls and overall safety. One study suggested that video monitoring decreased sitter usage while decreasing falls by 35%.8 Another study proposed that there was a 47.1% decrease in sitter costs when video monitoring and nurse-driven sitter protocols were employed.9 This study also suggested that technology alone does not create successful sitter-reduction program, but utilizing clinical nurses as the change agents was important to widespread use and belief in the effectiveness of technologies.9
In one organization, there was a 100% decrease in patient falls through pilot studies on units with high fall risk patients.10 Additional studies suggested that CVM was perceived by the nursing staff, video monitoring technicians (VMTs), and patients as helpful in protecting overall safety while in the inpatient setting.8–12
The goal of the leadership within the organization was to foster a safe environment that upholds the hospital values for respect and dignity of patients and staff, while maintaining safety and financial stability through improved resource allocation. Continuous video monitoring appeared to be an evidence-based solution and a feasible option to improve productivity and safety in all patient populations throughout the inpatient setting.
INITIAL IMPLEMENTATION PROCESS
Market research and system determination
Nursing leadership conducted a market research assessment on available CVM vendors. Screening criteria included available technology solutions, literature reviews on program effectiveness, and overall vendor outcomes. Two of the 3 vendors were in business for less than 6 months and did not have adequate outcome metrics to warrant further evaluation. The vendor of choice, Avasure, offered a desirable product that allowed for 2-way communication to a secure centralized station, 360-degree display with pan/tilt/zoom, night vision via automatic infrared illuminator, and emergent STAT alarm functionality. For patients with language barriers, the product offers 16 prerecorded prompts in 4 different languages. The vendor provided Online Reporting of Nursing Analytics to assist in tracking, reporting, analyzing, and impro-ving overall performance related to video monitoring process improvement and outcome determination.
Steering committee formation and organizational approvals
The CVM Steering Committee was organized with multiple representatives including nursing leadership, clinical nursing staff, Clinical Technology Services, Psychiatric Professional Practice Leader, Marketing, Department of Quality Management, Nursing Resource Management (ancillary float pool), and Nursing Administration. The group met biweekly initially, moved to monthly postimplementation, and then quarterly 1 year postimplementation. The CVM Steering Committee proposed purchasing of CVM technology through budgeting and finance to use discretionary capital funds. The total cost of the program was approximately $184 459 for video monitoring technology and another $60 000 for implementation of operating expenses. In addition, the committee sought and gained approval from the Clinical Enterprise Information Technology Acquisition and Retention Committee to ensure proper network and security clearance via the organizations secure Wi-Fi network.
CVM station and staffing
Space is often lacking in large organizations, thus the repurposing of a waiting room was needed to achieve a centralized station within the inpatient setting that allowed for access to the main hospital. The station comprised 2 large ergonomically approved viewing stations, one computer desk station, and a large whiteboard for Daily Management System tracking. The staffing structure consisted of scheduling 2 certified nursing assistants from the ancillary float pool around the clock and 7 days a week. For every 12-hour shift, there are 2 technicians present at all times. The VMT is responsible for monitoring patients, communicating with clinical staff members, and electronic health care record documentation in the CVM flow sheet. The video monitoring runner (VMR) is responsible for daily triage of cameras, sitter auditing, sitter awareness, and break relief. The VMTs and VMRs received specialized training related to anticipation of at-risk behaviors, system functionality, determination of adverse events, chain of resolution, and basic Lean management principles related to data tracking.
Development of policy, procedure, and patient criteria
Clearly defining inclusion and exclusion criteria for CVM with the input from clinical nurses allowed for clear expectations for clinical staff members. Inclusion criteria for pediatric and adult patients included drug/alcohol withdrawal, delirium, restlessness, confusion (acute or chronic), safety restraints, medication device protection, elopement risk, general safety concerns, fall prevention, eating disorders, and low/moderate suicide risk. Adult and pediatric exclusion criteria included behavioral restraints, seclusion, high-risk suicide, and failure of a 2-hour trial period on camera. Pediatric exclusion criteria also included all phases of eating disorder during mealtimes.
Enforcement of the 2-hour trial was not to dismiss nursing judgment but rather to ensure consideration of CVM if the patient met inclusion criteria and to address resource allocation considerations. The definition of a failed trial includes 3 STAT alarms in 30 minutes, nursing clinical judgment, and/or the ability of the VMT to monitor patient behaviors in conjunction with other patients on video monitoring. The CVM Steering Committee developed a Sitter Decisional algorithm to help nurses with clinical decision-making in relation to the use of a sitter or CVM as an intervention (see Supplemental Digital Content, Figure 1, available at: http://links.lww.com/JNCQ/A756). In addition, the steering committee created a Request Process algorithm, which highlighted throughput of the cameras within the organization. The Nurse Practice Council, a committee comprised of nurse leadership, clinical nurses, and administrative leadership, obtained all documents and gave final approval.
ENCULTURATION
Education
Education focused on the clinical nursing staff and was encouraged for those employees who would have indirect contact with CVM systems (housekeeping, transportation, case management, etc). Education opportunities consisted of unit in-services, leadership classes, champion classes, case management classes, and transitional care classes for community partners.
Clinical nurse champions were integral to the adoption of technology in all settings. Forty clinical nurse champions attended classes and learned the new organizational process and technology capabilities. From this point in time, the champions delivered educational materials to their corresponding units and educated nurses on the video monitoring process. With support from nurse leadership, clinical nurses were involved in all aspects of day-to-day operations of the video monitoring process. The VMTs stayed in continuous conversations with charge nurses and the clinical staff, which helped identify when sitters may be appropriate to transition to VMT monitoring. In addition, the VMTs began to attend the shift to shift charge nurse staff meetings. This collaboration further enhanced communication and throughput of patients who were eligible for video monitoring within the organization. Follow-up education 6 months postimplementation gave an opportunity to reinforce best practices and to communicate learnings and successes. The re-education event also allowed for additional input from the clinical staff and identification of potential barriers to utilization of the technology. Finally, monthly reports via division meetings and weekly newsletters assisted in sharing positive outcome metrics, utilization data, and highlighting creative use of the camera.
Leader standard work
Lean management principles are critical to continuous improvement and empower the frontline staff to solve problems, eliminate waste, standardize work, and improve value of care delivered to patients.13 Because Lean focuses on the frontline staff, it provides an opportunity to enculturate new systems and to identify barriers. The CVM program operates via Lean management principles including a functional Daily Management System. The Daily Management System allowed the VMTs and the clinical staff to be involved in process improvement initiatives through rapid improvement cycles, which promoted identification of barriers early on.
Our first improvement cycle focused on increasing overall video monitoring trials. One barrier identified was the lack of clarity around the CVM process. Thus, standard work for nurse leaders was an identified need. Leader Standard Work (LSW) consisted of a set of standard parameters nurse leaders would follow to check if the CVM process was successful. This became a best practice for continued process improvement and allowed escalation of barriers in real time, which included input from clinical staff members through the escalation structure (see Supplemental Digital Content, Figure 2, available at: http://links.lww.com/JNCQ/A757). This system starts with auditing sitters every 12 hours via an audit form completed by the charge nurse at the unit level. The VMTs gather audits through rounding and identify if sitters would benefit from a 2-hour trial. The CVM Nurse Manager allocates the data via a report and provides it to all nurse leaders daily. Nurse leaders then identify discrepancies in the process and follow up with charge nurses as appropriate. Barriers identified receive escalation at the adult inpatient huddle, where countermeasures can be identified to achieve process control.
The initiation of LSW allowed for tighter control and expectation setting across the organization. This organically improved the number of trials completed. After 2-hour trials increased, the success rate calculated at 80% to 90%, which further empowered enculturation of the technology as staff trusted the process and saw that CVM was a successful safety intervention.
Nurse-driven creative utilization
Some literature points to the use of video monitoring as an effective means to increase workforce safety.14 The VMTs are able to intervene when violent acts such as verbal abuse and physical assaults are escalating. Nursing staff communicates with the VMT regarding the risk for violence or verbal aggression during shift handoff. This allows for an increased awareness on the VMT side, which promotes anticipation of behavioral event escalation. The VMTs act early if they believe a Code Green is warranted. A Code Green, or behavioral code, is a collaborative interdisciplinary team response to significant behavioral dysregulation or lack of control leading to violent behavior, to themselves or others. The VMTs, safe in the monitoring room, can act quickly without issue if a patient is escalating and the nursing staff cannot safely advocate for themselves. This keeps both staff and patients safe in high-risk behavioral events.
Nursing staff also utilize CVM creatively related to predicted patient behaviors and trends. For example, nurses anticipate escalation of behaviors in patients who sundown or become increasingly disoriented in the evening, yet they clear or become less confused during the day. Identification of this trend enables the nursing staff to utilize CVM during daytime hours and one-to-one observation in the evening hours. The ability to use CVM in this way allocates resources and encourages nurses to work within their independent scope of practice in determining risk of patients based on trended behaviors. Moreover, enculturation is a secondary effect of nurse-driven creative use that promotes the utilization of CVM in daily practice.
Finally, CVM gives additional time for the clinical nursing staff to don personal protective equipment when at-risk patients are in isolation rooms. Often, the verbal alerts from VMTs can defer the patient long enough so the clinical staff can safely enter rooms that may have additional precautions such as airborne or droplet isolation. This is increasingly useful during times of high isolation needs such as flu season or the most recent COVID-19 pandemic.
OUTCOMES 1 YEAR POSTIMPLEMENTATION
Cost savings
One 24-hour sitter at the bedside can cost upwards of $561 per day and/or $204 765 annually within the inpatient setting. In January 2017, the inpatient psychiatric unit closed within our organization. After this closure, there was a 142% increase in one-to-one observation needs. The continued upward trend of additional sitter needs in conjunction with growth of at-risk populations creates issues with determining a clear cost savings. Conservative estimates show that CVM saved $109 511 in the first 3 quarters of use. However, as we refined the LSW process and continued to work on enculturation, we achieved $86 407 cost savings in quarter 1 of 2019.
CVM provided additional resources beyond that of sitter replacement. This savings does not include adverse events prevented such as falls and line/drain/tube dislodgments. Additional metrics showed that VMTs reported an average of 2768 potential “fall events” prevented per month in 2019. Despite not knowing how many of these events would lead to a fall, we can estimate additional conservative cost savings related to reduction of falls in video-monitored patients.
Finally, the VMTs reported increased difficulty with maintaining lines, tubes, and drains. On average, it takes a clinical staff 10 seconds to enter the room on activation of the STAT alarm system. Within 10 seconds, a patient can easily remove their peripheral intravenous line (PIV). With an average of at least 3 PIV pulls per month, a securement product was trialed. This product consisted of a protective sleeve that covered the area between the hand and the upper arm. Since initiation of this sleeve, we had a 70% decrease in line pulls on trialed units. The sleeve is now a best practice and part of our daily standard work in which all patient admissions to CVM with a PIV receive a sleeve.
Privacy and patient/family comfort considerations
A feature of the CVM technology is the ability to place the patient on privacy mode when personal care and/or bathing are being provided. A best practice titled Privacy Pledge was created and consists of placing the patient on privacy mode immediately when care is initiated. The clinical nursing staff and VMTs set a mutual time in which the camera will be turned back on when care is complete. This ensures protection of patient privacy during times of vulnerability.
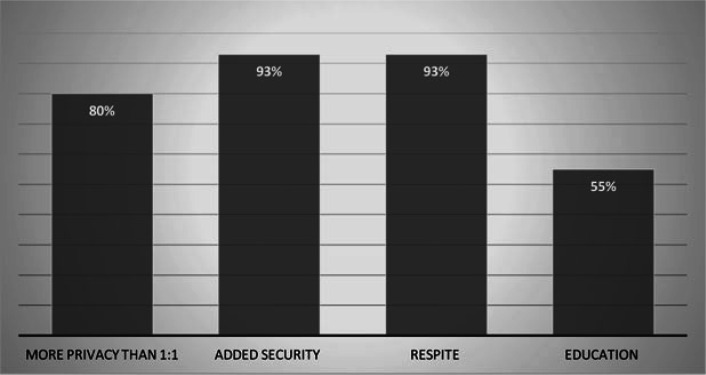
New technology can promote stress of not only staff members but also family members as they are likely unfamiliar with the functionality of the system and/or lack trust in its abilities. However, few articles address patient–family-centered approaches to CVM. One article suggest that video monitoring improves patient and family satisfaction,15 yet direct feedback from patients and families was not emphasized. To obtain direct feedback from patient family members, VMTs as part of their daily rounding used an online survey to assess overall comfort, security, and respite opportunities with CVM. Patients and families reported that they felt video monitoring provided more privacy than an in-person sitter 80% of the time. In addition, 93% of the time they reported video monitoring gave them a sense of added security.
Finally, 93% of family members indicated they received more respite opportunities because of the presence of the camera. Although these figures are promising, one area of opportunity is in relation to providing patient/family education during initiation of the video monitoring process. Only 55% of the time patients and/or families reported that they received the required education on initiation. However, many patients indicated this was due to the family member not being present during initiation and/or the patient being too confused to receive education at the time of initiation. Reminders or clinical alerts may be necessary to remind nurses to provide CVM education once the patient starts to clear or family members arrive (Figure).
Figure.
Patient and family comfort surveys.
CONCLUSION
The CVM program at our organization has provided a bridge for the nursing staff to utilize technology to enhance safety for patients and provide an additional intervention when sitter use is not reasonable or effective. Implementation of CVM reduced costs, improved resource allocation, and enhanced staff/patient family satisfaction. The CVM program is now part of our culture of safety. Implementing video monitoring systems and enculturation of technology can be intimidating. Thus, dissemination of learned best practices and standards for video monitoring is important, as technology will continue to expand in our global health care environment.
Supplementary Material
Footnotes
The authors acknowledge Lori Ellingson, Mariah Hayes, Melanie Jordan, Jo Harrington, and Dianne Wheeling.
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jncqjournal.com).
Published ahead of print: July 10, 2020
Contributor Information
JacQualine Renee Abbe, Email: abbe@ohsu.edu.
Christian O'Keeffe, Email: okeeffec@ohsu.edu.
REFERENCES
- 1.Greeley AM, Tanner EP, Mak S, Begashaw MM, Miake-Lye IM, Shekelle PG. Sitters as a patient safety strategy to reduce hospital falls: a systematic review. Ann Intern Med. 2020;172(5):317–324. doi:10.7326/M19-2628 [DOI] [PubMed] [Google Scholar]
- 2.Mental Health America. Ranking the states 2018. Accessed March 5, 2020. https://www.mhanational.org/issues/ranking-states-2018-0.
- 3.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi:10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- 4.Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset. 2005-2017. J Abnorm Psychol. 2019;128(3):185–199. doi:10.1037/abn0000410 [DOI] [PubMed] [Google Scholar]
- 5.Mental Health America. The state of mental health in America. Accessed March 5, 2020. https://www.mhanational.org/issues/state-mental-health-america.
- 6.Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911–922. doi:10.1016/S0140-6736(13)60688-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bellelli G, Morandi A, Di Santo SG, et al. “Delirium day”: a nationwide point prevalence study of delirium in older hospitalized patients using an easy standardized diagnostic tool. BMC Med. 2016;14:106. doi:10.1186/s12916-016-0649-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Votruba L, Graham B, Wisinski J, Syed A. Video monitoring to reduce falls and patient companion costs for adult inpatients. Nurs Econ. 2016;34(4):185–189. [PubMed] [Google Scholar]
- 9.Burtson P, Vento L. Sitter reduction through mobile video monitoring: a nurse-driven sitter protocol and administrative oversight. J Nurs Adm. 2015;45(7/8):363–369. [DOI] [PubMed] [Google Scholar]
- 10.Davis JE, Carter-Templeton H. Augmenting an inpatient fall program with video observation. J Nurs Care Qual. Published online April 6, 2020. doi:10.1097/NCQ.0000000000000486 [DOI] [PubMed] [Google Scholar]
- 11.Sand-Jecklin K, Johnson J, Tringhese A, Daniels C, White F. Video monitoring for fall prevention and patient safety: process evaluation and improvement. J Nurs Care Qual. 2019;34(2):145–150. doi:10.1097/NCQ.0000000000000355 [DOI] [PubMed] [Google Scholar]
- 12.Daley B, Fetherman B, Turner J. Staffing utilization and fall prevention with an electronic surveillance video system: a randomized controlled study. J Nurs Care Qual. Published online February 5, 2020. doi:10.1097/NCQ.0000000000000472 [DOI] [PubMed] [Google Scholar]
- 13.Po J, Rundall TG, Shortell SM, Blodgett JC. Lean management and U.S. public hospital performance: results from a national survey. J Healthc Manag. 2019;64(6):363–379. doi:10.1097/JHM-D-18-00163 [DOI] [PubMed] [Google Scholar]
- 14.Quigley PA, Votruba L, Kaminski J. Impact of patient-engaged video surveillance on nursing workforce safety: patient aggression/violence. J Nurs Care Qual. Published November 14, 2019. doi:10.1097/NCQ.0000000000000450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cournan M, Fusco-Gessick B, Wright L. Improving patient safety through video monitoring. Rehabil Nurs. 2018;43(2):111–115. doi:10.1097/RNJ.0000000000000089 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.