Supplemental Digital Content is available in the text.
Key Words: nurse practitioners, cost decomposition, Medicare, primary care
Abstract
Background:
Although recent research suggests that primary care provided by nurse practitioners costs less than primary care provided by physicians, little is known about underlying drivers of these cost differences.
Research Objective:
Identify the drivers of cost differences between Medicare beneficiaries attributed to primary care nurse practitioners (PCNPs) and primary care physicians (PCMDs).
Study Design:
Cross-sectional cost decomposition analysis using 2009–2010 Medicare administrative claims for beneficiaries attributed to PCNPs and PCMDs with risk stratification to control for beneficiary severity. Cost differences between PCNPs and PCMDs were decomposed into payment, service volume, and service mix within low-risk, moderate-risk and high-risk strata.
Results:
Overall, the average PCMD cost of care is 34% higher than PCNP care in the low-risk stratum, and 28% and 21% higher in the medium-risk and high-risk stratum. In the low-risk stratum, the difference is comprised of 24% service volume, 6% payment, and 4% service mix. In the high-risk stratum, the difference is composed of 7% service volume, 9% payment, and 4% service mix. The cost difference between PCNP and PCMD attributed beneficiaries is persistent and significant, but narrows as risk increases. Across the strata, PCNPs use fewer and less expensive services than PCMDs. In the low-risk stratum, PCNPs use markedly fewer services than PCMDs.
Conclusions:
There are differences in the costs of primary care of Medicare beneficiaries provided by nurse practitioners and MDs. Especially in low-risk populations, the lower cost of PCNP provided care is primarily driven by lower service volume.
To control the rising cost of health care and curb overutilization of services,1,2 the health care industry is shifting away from a system that rewards volume to one that incentivizes efficiency and value.3 In October 2019, the US Department of Health and Human Services announced plans to transition 50% of Medicaid and 100% of Medicare fee-for service reimbursements to alternative payment models [ie, bundled payment, accountable care organizations (ACOs), or patient-centered medical homes] by 2025.4 These changes challenge clinicians to provide care more efficiently by holding them accountable for the cost and quality of their care. Nurse practitioners (NPs) are well suited for these goals.5,6 Study results consistently indicate that the quality of primary care provided by NPs is comparable and sometimes better than physicians.7–13 However, less is known about the efficiency of NP practice patterns and their effect on costs.
Although prior systematic reviews on the costs of NP-provided care are inconclusive,9,14–17 recent research suggests that NP-provided care costs less than care provided by primary care physicians (PCMDs).18–22 Results from utilization studies show that compared with PCMDs, NPs order comparable or fewer prescriptions,14,19,23,24 but more follow-up and specialist visits.14,18,25 Patients who receive care from NPs are also associated with lower emergency and inpatient use even after case-mix adjustment.20,21,26 A few studies report that NPs order more diagnostic imaging than PCMDs,27,28 whereas others find the rates of low-value imaging, overuse of antibiotics, and unnecessary referrals between the 2 types of clinicians are comparable.29,30 In prior work examining the cost of primary care provided to Medicare beneficiaries, the costs of NP-provided services were 18% less than their physician counterparts. Beneficiaries cared for by NPs had significantly lower inpatient and evaluation and management (E&M) costs, even after accounting for different reimbursement rates between clinicians.31
The research described in this article examines the reasons behind NPs’ lower costs relative to physicians. We apply a novel approach to decompose the cost difference into 3 factors; payment, service volume, and service mix, using Medicare 2009–2010 administrative claims and controlling for beneficiary severity and case-mix. Traditional decomposition analysis examines the drivers of costs or prices over many years to identify the underlying causes of inflationary trends. In our analysis, however, we examine the drivers of costs cross-sectionally between 2 types of clinicians, rather than 2 points of time.
METHODS
Sample
The sample was constructed by obtaining a random sample of NPs and PCMDs from a list of all clinicians with independent Medicare National Provider Identification numbers in 2009–2010. As NP panels are smaller than PCMD panels in Medicare, we purposefully weighted our sample to include approximately two-thirds NP beneficiaries and one-third PCMD beneficiaries (Table 1). We then gathered all claims for beneficiaries treated by these clinicians. Because each of the selected beneficiaries saw multiple clinicians, gathering all of their claims led to a number of additional clinicians captured in the sample. This process resulted in 85,820 beneficiaries with 1 or more claims with a NP specialty code (“50”) and 9422 unique NPs (Table 1). For PCMDs we used part B specialty codes “08”=family medicine or “11”=internal medicine to capture 382,124 beneficiaries and 68,069 unique PCMDs.
TABLE 1.
Mix of Services & Mean Allowed Amounts for Beneficiaries Attributed to PCNPs and PCMDs
| PCNP (N=85,820) | PCMD (N=382,124) | |||||||
|---|---|---|---|---|---|---|---|---|
| Service Category | Total Service Units | Units of Service Per Beneficiary | Mean Allowed Amount Per Unit | Mean Expected Allowed Amount Per Unit | Total Service Units | Units of Service Per Beneficiary | Mean Allowed Amount Per Unit | Mean Expected Allowed Amount Per Unit |
| Durable medical equipment | 3172 | 0.04 | $121 | $47 | 19,885 | 0.05 | $96 | $44 |
| Standard imaging | 343,865 | 4.01 | $44 | $56 | 2,046,006 | 5.35 | $43 | $47 |
| Advanced imaging | 64,426 | 0.75 | $110 | $125 | 425,765 | 1.11 | $119 | $117 |
| Office visit | 493,113 | 5.75 | $57 | $88 | 3,437,565 | 9.00 | $62 | $78 |
| Home visit | 32,553 | 0.38 | $94 | $143 | 43,873 | 0.11 | $95 | $130 |
| Specialist visit | 170,732 | 1.99 | $60 | $80 | 733,543 | 1.92 | $71 | $80 |
| Consultation | 7 | 0.00 | $158 | $315 | 68 | 0.00 | $114 | $127 |
| Other OP visit | 680,470 | 7.93 | $93 | $117 | 2,921,426 | 7.65 | $118 | $122 |
| General services | 195,036 | 2.27 | $207 | $171 | 1,109,755 | 2.90 | $193 | $145 |
| Anesthesia | 24,271 | 0.28 | $176 | $152 | 169,362 | 0.44 | $185 | $147 |
| Major procedures | 29,721 | 0.35 | $608 | $436 | 210,229 | 0.55 | $624 | $433 |
| Minor procedures | 240,171 | 2.80 | $76 | $74 | 1,473,579 | 3.86 | $84 | $69 |
| Endoscopy, oncology, and dialysis | 42,184 | 0.49 | $221 | $180 | 289,985 | 0.76 | $233 | $172 |
| Ordinary lab test | 885,387 | 10.32 | $22 | $31 | 4,184,198 | 10.95 | $24 | $28 |
| Other lab test | 112,991 | 1.32 | $40 | $49 | 834,901 | 2.18 | $41 | $42 |
| Other Medicare | 119,575 | 1.39 | $14 | $21 | 314,275 | 0.82 | $18 | $24 |
PCMD indicates primary care physicians; PCNP, primary care nurse practitioners.
Attribution of Beneficiaries to Primary Care Clinicians
First, we calculated the proportion of a beneficiary’s care provided by clinicians using primary care paid amounts, categorized by Berenson-Eggers Type of Service categories (BETOS). To focus on primary care, E&M services were limited to new (M1A: 99201–99205) and established office visits (M1B: 99211–99215), home visits (M4A: 99340–99345; 99347–99350) or nursing home visits (M4B: 99304–99306; 99307–99310), which excluded inpatient, emergency department, and specialist services. Next, each beneficiary was assigned to the clinician who provided the highest proportion of E&M paid amounts as long as that clinician accounted for 30% or more of total E&M paid amounts.32 The minimum threshold was designed to ensure a strong relationship between each beneficiary and clinician dyad. This process identified primary care nurse practitioners (PCNPs). In the rare case of ties [2 or more clinicians with the same percent of E&M paid amounts (N=206)], 1 primary care clinician was randomly selected.
Risk Stratification
To account for differences in beneficiary severity, we used a regression-based, risk-adjustment model to stratify the sample into sufficiently homogenous risk strata (Table, Supplemental Digital Content 1, http://links.lww.com/MLR/C158). We estimated a risk-adjustment regression model that included demographics and Elixhauser comorbidities33,34 for the pooled sample of PCMD and PCNP beneficiaries. This model made no adjustment for PCNP or PCMD attribution. With predicted values from our regression model, we considered the expected cost of individual beneficiaries as a proxy for individual beneficiary risk. This variable for risk profile allowed us to group beneficiaries into 3 strata, defined as low (30% of total population), moderate (40%), and high risk (30%). This stratification enabled us to study the 2 tails of the risk distribution separately from the larger population in the middle of the distribution. To test whether the proportion of PCNP attributed beneficiaries was lower or higher than the proportion of PCMD attributed beneficiaries, we conducted bivariate comparisons of PCNP and PCMD attributed beneficiaries within each risk strata.
Cost Measures
Once attributed beneficiaries were divided into risk strata, the analytic approach decomposed the total payment difference by comparing clinician services based on 3 components: payment, service volume, and service mix. To facilitate the decomposition analysis, we created a standardized “market basket” of outpatient services derived from the BETOS Primary Care Service Categories (PCSCs). BETOS reduces thousands of individual procedure codes into meaningful groups such as E&M, imaging, tests, and procedures. We refined the original BETOS groups slightly (parsing out advanced imaging from the imaging category) to better examine utilization patterns. The resulting 15 PCSCs are standardized groups of similar services (Table, Supplemental Digital Content 2, http://links.lww.com/MLR/C159, which lists PCSCs based on BETOS categories) that form the market-basket used for the decomposition analysis.
Dependent Variable
Total payment difference is the total expenditures for PCMD assigned beneficiaries minus the total expenditures for PCNP assigned beneficiaries. To capture expenditures we use Medicare allowed amounts that include Medicare payments, copays and deductibles for services in the BETOS PCSCs.
Independent Variables
Payment is the average dollar amount for all goods and services in any PCSC. For example, the unit payment for “Advanced Imaging” is the mean allowed amount for all bills with an Advanced Imaging code (eg, V8900–V8920 for magnetic resonance imaging). These calculations were conducted separately for PCNP and PCMD attributed beneficiaries, with the denominator represented by the number of beneficiaries in each risk stratum attributed to either PCNPs or PCMDs (Table 1).
Service Volume is the proportion of the count of unique claims for each service within the PCSCs to the number of beneficiaries in each risk stratum attributed to each clinician type (Table 1), calculated separately for PCNP and PCMD attributed beneficiaries.
Service mix is the difference in the intensity of the combination of services provided by PCNPs versus PCMDs. For example, one group of clinicians may use more expensive treatments (eg, cardiac stress-test versus cardiac stress-test with cardiology interpretation) than another.
Analysis
We began with a descriptive analysis of the service mix of PCNP and PCMD attributed beneficiaries. In a parallel study, we established a statistically significant cost difference after controlling for patient, area and provider characteristics.31 That study used a method, pioneered by Oaxaca and Blinder,35,36 to decompose wage gaps, but has been applied to other health care-related topics such as racial disparities37,38 and income inequality in health status39 to understand the drivers of disparity. To avoid repeating the elaborate Oaxaca model, we used t tests to ensure statistically significant cost differences between PCNPs and PCMDs, in the overall population and within the 3 risk strata.
The statistically significant differences were then decomposed using the number of services and the mean payment for PCNP and PCMD attributed beneficiaries, respectively (ie, number of PCNP services×PCNP payment rate for the service in the BETOS PCSCs). These terms were rearranged to split out the 3 primary components: payment, service volume, and service mix (see Text, Supplemental Digital Content 3, http://links.lww.com/MLR/C160 for technical details). For example, the unit cost difference between PCNP and PCMD attributed beneficiaries was multiplied by the mid-point service utilization counts to determine an estimate of the “contribution” of the payment to the overall difference. Similar mathematical approaches estimated the contribution of volume and service mix to the overall difference. This, in turn, helped determine which factors within each of the PCSCs are driving the cost difference between the 2 types of clinicians groups. The result of this decomposition is a series of positive and negative contributions to the total payment difference for each PCSC category, across each risk strata.
RESULTS
Data on the mix of services and allowed Medicare payment used by PCNP and PCMD attributed beneficiaries in each of the 15 PCSCs is presented in Table 1. Overall, PCMD beneficiaries appear to use more office visits (9.00 office visits per PCMD beneficiary annually vs. 5.75 office visits per PCNP beneficiary annually) and lab tests (2.18 vs. 1.32) than PCNP attributed beneficiaries. The most common service in both groups is ordinary lab tests followed by hospital and office-based E&M visits and standard imaging. The mean payment is relatively similar for lab tests ($22 for PCNP attributed beneficiaries and $24 for PCMD attributed beneficiaries) and office visits ($57 for PCNP attributed beneficiaries and $62 for PCMD attributed beneficiaries), but somewhat higher for PCMD attributed beneficiaries in the category of hospital-based E&M visits ($118 for PCMD attributed beneficiaries and $93 for PCNP attributed beneficiaries), which includes services such as initial hospital E&M visit or a hospital critical care visit.
The results of beneficiary risk stratification, shown in Table 2, indicate the proportion of beneficiaries attributed to PCNPs decreases as beneficiary severity increases. PCNP beneficiaries make up 21% of the healthiest stratum but only 16% of the high-risk stratum. The mean expected costs for both groups are comparable across each risk stratum. However, for the observed costs, the object of our decomposition analysis, the costs of PCMD beneficiaries are always higher than PCNP beneficiaries, and increase among high-risk beneficiaries. The differences of expected versus observed costs between PCMDs and PCNPs are $42 versus $368, $36 versus $550, and $354 versus $1297 for the low-risk, moderate-risk, and high-risk stratum, respectively.
TABLE 2.
Observed and Expected Costs by Risk Stratum for PCMD and PCNP Attributed Medicare Beneficiaries (n=467,944)
| Risk Stratum | PCMD Mean Expected Costs | PCNP Mean Expected Costs | PCMD Mean Observed Costs | PCNP Mean Observed Costs | PCMD Beneficiary Count | PCNP Beneficiary Count | Total Beneficiary Count | % PCNP of Total |
|---|---|---|---|---|---|---|---|---|
| Low risk (30%) | $718 | $676 | $1450 | $1082 | 111,473 | 28,912 | 140,385 | 21 |
| Moderate risk (40%) | $2895 | $2859 | $2691 | $2141 | 152,382 | 34,798 | 187,180 | 19 |
| High risk (30%) | $7636 | $7283 | $7520 | $6222 | 118,269 | 22,110 | 140,379 | 16 |
PCMD indicates primary care physicians; PCNP, primary care nurse practitioners.
Using t tests, we confirmed that all cost differences between the 2 beneficiary groups (attributed to PCMDs or PCNPs) in the overall population and within low-risk, medium-risk, and high-risk strata were statistically significant (P-values<0.0001 for all 4 tests, results shown in Table, Supplemental Digital Content 4, http://links.lww.com/MLR/C161). Figure 1 shows the PCMD attributed beneficiary residual cost difference (PCMD beneficiary costs−PCNP beneficiary costs) by PCSC and risk stratum. The green bars represent the cost difference for low-risk beneficiaries and the red bars for high-risk beneficiaries across the PCSCs. The largest cost difference is for office visits for the sickest PCMD beneficiaries ($327), and other prominent areas include hospital/ER/nursing home visits ($280) and major procedures ($206). In regards to the “other” category, the costs of PCNP attributed beneficiaries and PCMDs attributed beneficiaries are equal.
FIGURE 1.
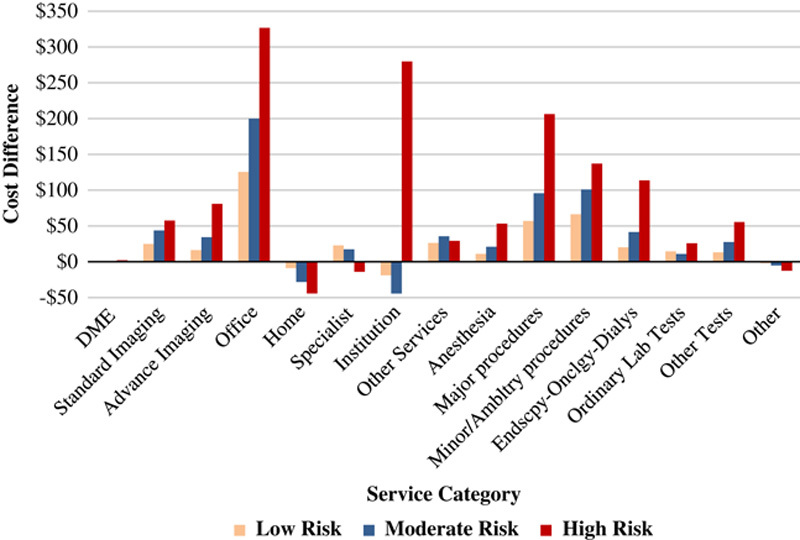
Cost difference (primary care physician attributed beneficiary cost−primary care nurse practitioner attributed beneficiary cost) by service categories across risk strata. DME indicates durable medical equipment.
The results of the cost difference decomposition by the 15 PCSCs for the low-risk and high-risk strata are shown in Table 3. The left panels show the results of decomposing the $368 cost difference in the low-risk stratum, resulting from the mean costs for PCMD and PCNP beneficiaries, respectively ($1450 and $1082). Similarly, we decompose the $1297 cost difference for the high-risk stratum in the right panel (PCMD=$7520 and PCNP=$6222).
TABLE 3.
Results of the Decomposition of the Cost Difference Between Medicare Beneficiaries Attributed to Primary Care Physicians and Those Attributed to Nurse Practitioners by Primary Care Service Category and Contributing Factors for Low-risk and High-risk Strata
| Low-risk Stratum (N=140,385) | High-risk Stratum (N=140,379) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Primary Care Service Categories | Payment Difference ($) | Service Mix Difference ($) | Service Volume Difference ($) | Sum All Differences ($) | % Contribution of Service Category | Payment Difference ($) | Service Mix Difference ($) | Service Volume Difference ($) | Sum All Differences ($) | % Contribution of Service Category |
| DME | 1.12 | 0.57 | 0.70 | 0.15 | 0 | 0.58 | 1.22 | 0.30 | 2.10 | 0 |
| Standard imaging/echo/ultrasound | 3.22 | 2.94 | 18.66 | 24.81 | 7 | 12.70 | 47.18 | 23.04 | 57.52 | 4 |
| Advance imaging | 3.07 | 4.90 | 8.30 | 16.27 | 4 | 19.44 | 49.39 | 12.01 | 80.84 | 6 |
| Office visits | 22.73 | 50.20 | 52.47 | 125.41 | 34 | 38.72 | 255.98 | 32.04 | 326.74 | 25 |
| Home visit | 0.16 | 11.76 | 2.81 | 8.78 | −2 | 0.50 | 49.41 | 4.62 | 44.28 | −3 |
| Specialist visits | 8.33 | 2.39 | 16.98 | 22.91 | 6 | 35.07 | 63.70 | 14.73 | 13.89 | −1 |
| Hospital/emergency department/nursing home visit | 19.82 | 67.74 | 28.98 | 18.94 | −5 | 443.85 | 325.03 | 161.02 | 279.84 | 22 |
| Other services | 0.80 | 0.10 | 25.56 | 26.25 | 7 | 136.32 | 81.18 | 84.29 | 29.16 | 2 |
| Anesthesia | 0.95 | 4.93 | 5.17 | 11.06 | 3 | 6.51 | 39.50 | 7.17 | 53.19 | 4 |
| Major procedures | 4.05 | 26.20 | 26.71 | 56.96 | 15 | 14.57 | 164.22 | 27.47 | 206.26 | 16 |
| Minor/ambulatory procedures | 6.60 | 25.33 | 34.38 | 66.31 | 18 | 46.40 | 67.13 | 23.60 | 137.13 | 11 |
| Endoscopy/oncology/dialyses | 2.17 | 8.34 | 9.67 | 20.18 | 5 | 22.49 | 73.70 | 17.52 | 113.72 | 9 |
| Ordinary lab tests | 4.09 | 6.20 | 24.73 | 14.44 | 4 | 61.95 | 66.83 | 30.78 | 25.90 | 2 |
| Other tests | 1.05 | 8.78 | 5.51 | 13.23 | 4 | 7.36 | 41.61 | 6.57 | 55.55 | 4 |
| Other | 0.64 | 3.96 | 1.42 | 1.89 | −1 | 11.67 | 27.80 | 3.56 | 12.57 | −1 |
| Total | 66.28 | 40.04 | 262.04 | 368.36 | 100 | 560.08 | 288.36 | 448.75 | 1297.20 | 100 |
DME indicates durable medical equipment; PCMD, primary care physicians; PCNP, primary care nurse practitioners.
Figure 2 summarizes the decomposition results shown in Table 3 and illustrates several key findings. First, as beneficiary risk increases from low to high, the cost difference between PCNPs and PCMDs decreases from 34.1% to 25.7% and then 20.8%. Higher service volume is the largest driver of difference in the low-risk and medium-risk strata, decreasing from 24.2% of the difference ($262 of total gap of $368) in the low-risk group to 7.2% ($449 of total difference of $1297) in the high-risk group. The other 2 factors driving the increased costs are higher payments to clinicians (levels of unit costs per service category) and choice of more expensive combinations of services. In particular, in the high-risk strata, payment becomes the largest driver (9.0%) whereas payment only accounts for 3.7% of the difference in the low-risk strata. Service mix remains relatively stable across the 3 risk strata, explaining 3.7% of the variance in the low-risk group, 5.5% in the medium-risk group, and 4.6% in the high-risk group.
FIGURE 2.
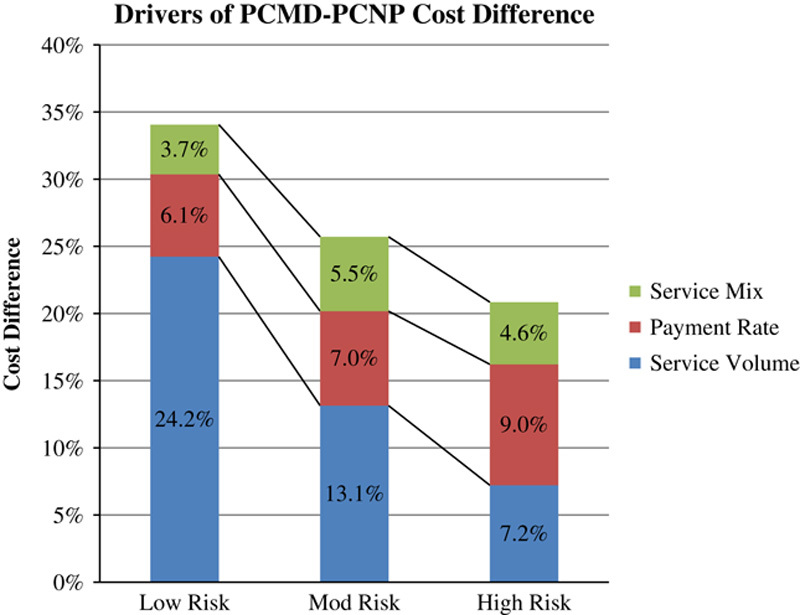
Decomposition of the cost difference between primary care physician attributed Medicare beneficiaries and primary care nurse practitioner attributed Medicare beneficiaries into payment rate, service volume, and service mix. PCMD indicates primary care physicians; PCNP, primary care nurse practitioners.
DISCUSSION
When explaining the increase in health care costs and spending in the United States, the conventional answer among health care economists is “It’s the prices, stupid.”40 Although our findings show that price, or payment, plays a role, it is the lower volume of services ordered by PCNPs that is the major driver of cost differences between PCNP and PCMD attributed Medicare beneficiaries. Overall, study results show a sizable cost difference between PCNP and PCMD attributed beneficiaries, which is consistent with prior findings.31 At the same time, our results indicate that cost differences between PCNPs and PCMDs narrow as beneficiary severity increases (low risk: 34.1% to high risk: 20.8%). Cost differences within the low-risk cohort may reflect differences in the resource utilization between PCNPs and PCMDs in the primary care setting, while specialists may play a larger role in driving the total cost of care in the high-risk cohort.
The decomposition of these cost differences revealed that service volume is the largest driver of cost difference between PCNPs and PCMDs in both low-risk and high-risk cohorts. Among low-risk beneficiaries, the 34% cost difference is comprised of 24% service volume, 6% payment, and 4% service mix—volume is far more important than payment. In the high-risk cohort, the overall difference of 21% is composed of 7% service volume, 9% payment, and 4% service mix. This relative increase in volume by sicker PCNP attributed beneficiaries could reflect a transfer of higher acuity to specialty care, which is associated with a higher volume of services. However, service mix and payment remain relatively constant across risk stratification, highlighting service volume as the major driver of cost difference. This finding suggests that PCMD attributed beneficiaries receive more services, but not more complex or more costly services, than clinically similar PCNP attributed beneficiaries.
The underlying reasons behind these differences are not clear, but may reflect differences in resources, coding, and incentives. PCMDs are more likely to practice in well-resourced settings, whereas PCNPs often practice in underserved and rural areas,41,42 where diagnostic equipment, laboratories, and treatment technologies are not readily available. However, the majority of PCNPs work in conventional office and hospital-based settings43 with similar access to resources as PCMDs. Alternatively, it is possible that PCMDs may be more disposed to practicing defensive medicine, ordering more services out of a concern for malpractice litigation. There may also be an influence of undercoding or overcoding E&M visits, the only PCSCs where clinician coding practice impacts the average payment. PCMDs are more likely to share practice ownership, be well versed in accurate coding practices and employ billing and coding staff. And, relative to PCNPs, PCMDs are far more likely to be owners or part-owners of laboratories, imaging centers, physical therapy, and rehabilitation centers that provide PCMDs an economic incentive to use such services. In contrast, PCNPs are less likely to share practice profits, or receive quality or productivity bonuses43 and therefore are not as invested in coding procedures, and may even under code.
Still, another possible explanation for the differences in use of services between PCNPs and PCMDs concerns possible differences in the practice style. It is conceivable that PCNPs spend more time taking patient histories which, in turn, may help make a diagnosis or rule out conditions that are causing the patient’s health problem without needing to order tests and diagnostic procedures. In contrast, due to time and productivity pressures, PCMDs may not spend as much time taking histories, and instead rely more on diagnostic tests. Such differences in practice style, coding, and incentives are all important areas for further research.
Implications for Policy and Research
As the number of Medicare beneficiaries increase from 60 million in 2019, 79 million in 2030, and 91 million in 2050,44 the number of PCNPs expands rapidly,45 and the number of physicians practicing in rural and underserved areas decreases,46 our findings have several implications for workforce policy and care delivery systems. Because more primary care will be provided by NPs in the future, results suggests that PCNPs’ conservative use of resources will help contain costs and overall spending growth and, with full integration of PCNPs into alternative payments models, achieve further savings.
Although the Affordable Care Act recognizes NPs as “Accountable Care Organization (ACO) professionals” and authorizes NPs to join ACOs, the claims-based assignment pathway prevents NP beneficiaries from ACO participation unless they are referred to physicians for additional primary care.47 In other words, some NPs and their beneficiaries are not eligible to receive ACO benefits, or could be made eligible through potentially redundant and unnecessary primary care visits. These contradictory regulations have prompted legislative efforts to improve beneficiary assignment to ACOs by allowing claims-based assignment of beneficiaries seen only by NPs.48 Results from this study suggest that NPs may enable ACOs to achieve greater cost-savings, while maintaining a high quality of care. Excluding beneficiaries seen only by NPs from ACOs needlessly restricts these stakeholders from achieving the full promise of alternative payment models.
The decomposition method used in this study offers an innovative way to understand differences in practice style in general. Rather than the original application of these methods to decompose inflationary trends over time, the technique used here teases apart care pattern differences in a 12-month period using the standard BETOS PCSCs. The policy advantage of this adaptation is that the specific elements in the decomposition are consistent with the major categories used in numerous studies that document price variation, overuse, and misuse as the major sources of wasteful spending in health care.49,50 By risk stratifying beneficiaries, our unique approach customizes potential policy solutions according to the impact of the underlying drivers of cost differences within each specific risk strata. The flexibility of the technique, and the minimal data requirements, makes this approach applicable to examining many health care cost questions, such as assessing sources of regional variation in pricing or determining the factors influencing more versus less efficient care.
Limitations
There are, of course, several limitations to be aware of when considering our results. First, we used a relatively conservative attribution method that left many beneficiaries unassigned to a primary clinician. Future analysis should explore different attribution techniques, particularly those that capture the provision of health care by teams of clinicians. Second, incident-to billing (ie, the Medicare policy that permits billing NP services under a physician’s National Provider Identification) means that some of the NP beneficiaries were inaccurately attributed to PCMDs. This may have affected the accuracy of attributing Medicare beneficiaries to PCMDs, but we do not believe this limitation materially affected our decomposition results. Although we were unable to explicitly adjust for quality outcomes, we held patient severity constant as a loose proxy for comparable work. Finally, we grouped services into categories that reflect typical primary and secondary care. However, different grouping of service codes may have produced different results.
CONCLUSIONS
Overall, evidence from our study indicates there are differences in the costs of primary care of Medicare beneficiaries provided by NPs and MDs. These differences mostly reflect the lower quantity of services provided by PCNPs relative to PCMDs, which are especially pronounced in the care of low-risk populations. The cost difference narrows in the high-risk cohort, reflecting a convergence of PCNP and PCMD practice style in regard to resource utilization and likely increased use of specialty care for sicker beneficiaries. For those concerned with lowering the cost of health care and reducing the growth of health care spending, our study provides new evidence that NPs are well suited to lower the cost of primary care for both low-risk and high-risk beneficiaries, and are valuable participants in the delivery of services under alternative payment models.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Burwell S. Setting value-based payment goals—HHS efforts to improve US health care. New Engl J Med. 2015;372:897–899. [DOI] [PubMed] [Google Scholar]
- 2.Medicare Payment Advisory Commission. A Data Book: Health Care Spending and the Medicare Program (Vol 2018). Washington, DC: Medicare Payment Advisory Commission; 2016. [Google Scholar]
- 3.Porter M. What is value in health care? New Engl J Med. 2010;363:2477–2481. [DOI] [PubMed] [Google Scholar]
- 4.Health and Human Services Secretary Alex Azar. Aligning for Shared Accountability. Paper presented at The Health Care Payment Learning & Action Network Summit; 2019.
- 5.Naylor MD, Kurtzman ET. The role of nurse practitioners in reinventing primary care. Health Aff. 2010;29:893–899. [DOI] [PubMed] [Google Scholar]
- 6.Bodenheimer TS, Smith MD. Primary care: proposed solutions to the physician shortage without training more physicians. Health Aff. 2013;32:1881–1886. [DOI] [PubMed] [Google Scholar]
- 7.Kurtzman ET, Barnow BS. A comparison of nurse practitioners, physician assistants, and primary care physicians’ patterns of practice and quality of care in health centers. Med Care. 2017;55:615–622. [DOI] [PubMed] [Google Scholar]
- 8.Newhouse RP, Bass EB, Stanik-Hutt J, et al. Advanced practice nurse outcomes: 1990-2008: A systematic review. Nurs Econ. 2011;29:1–21. [PubMed] [Google Scholar]
- 9.Martínez-González NA, Djalali S, Tandjung R, et al. Substitution of physicians by nurses in primary care: a systematic review and meta-analysis. BMC Health Serv Res. 2014;14:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuo YF, Chen NW, Baillargeon J, et al. Potentially preventable hospitalizations in Medicare patients with diabetes: a comparison of primary care provided by nurse practitioners versus physicians. Med Care. 2015;53:776–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buerhaus P, Perloff J, Clarke S, et al. Quality of primary care provided to Medicare beneficiaries by physicians and nurse practitioners. Med Care. 2018;56:484–490. [DOI] [PubMed] [Google Scholar]
- 12.Yang Y, Long Q, Jackson SL, et al. Nurse practitioners, physician assistants, and physicians are comparable in managing the first five years of diabetes. Am J Med. 2018;131:276–283.e272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jackson GL, Smith VA, Edelman D, et al. Intermediate diabetes outcomes in patients managed by physicians, nurse practitioners, or physician assistants: a cohort study. Ann Intern Med. 2018;169:825–835. [DOI] [PubMed] [Google Scholar]
- 14.Laurant M, van der Biezen M, Wijers N, et al. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. 2018;7:Cd001271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Donald F, Kilpatrick K, Reid K, et al. Hospital to community transitional care by nurse practitioners: a systematic review of cost-effectiveness. Int J Nurs Stud. 2015;52:436–451. [DOI] [PubMed] [Google Scholar]
- 16.Martin-Misener R, Harbman P, Donald F, et al. Cost-effectiveness of nurse practitioners in primary and specialised ambulatory care: systematic review. BMJ Open. 2015;5(e007167):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jennings N, Clifford S, Fox AR, et al. The impact of nurse practitioner services on cost, quality of care, satisfaction and waiting times in the emergency department: a systematic review. Int J Nurs Stud. 2015;52:421–435. [DOI] [PubMed] [Google Scholar]
- 18.Kuo YF, Goodwin JS, Chen NW, et al. Diabetes mellitus care provided by nurse practitioners vs primary care physicians. J Am Geriatr Soc. 2015;63:1980–1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Van Der Biezen M, Adang E, Van Der Burgt R, et al. The impact of substituting general practitioners with nurse practitioners on resource use, production and health-care costs during out-of-hours: a quasi-experimental study. BMC Fam Pract. 2016;17:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morgan PA, Smith VA, Berkowitz TSZ, et al. Impact of physicians, nurse practitioners, and physician assistants on utilization and costs for complex patients. Health Aff. 2019;38:1028–1036. [DOI] [PubMed] [Google Scholar]
- 21.Muench U, Guo C, Thomas C, et al. Medication adherence, costs, and ER visits of nurse practitioner and primary care physician patients: evidence from three cohorts of Medicare beneficiaries. Health Serv Res. 2019;54:187–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith VA, Morgan PA, Edelman D, et al. Utilization and costs by primary care provider type: are there differences among diabetic patients of physicians, nurse practitioners, and physician assistants? Med Care. 2020;58:681–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Muench U, Perloff J, Thomas CP, et al. Prescribing practices by nurse practitioners and primary care physicians: a descriptive analysis of medicare beneficiaries. J Nurs Regul. 2017;8:21–30. [Google Scholar]
- 24.Jiao S, Murimi IB, Stafford RS, et al. Quality of prescribing by physicians, nurse practitioners, and physician assistants in the United States. Pharmacotherapy. 2018;38:417–427. [DOI] [PubMed] [Google Scholar]
- 25.Agarwal A, Zhang W, Kuo Y, et al. Process and outcome measures among COPD patients with a hospitalization cared for by an advance practice provider or primary care physician. PLoS One. 2016;11:e0148522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lutfiyya MN, Tomai L, Frogner B, et al. Does primary care diabetes management provided to Medicare patients differ between primary care physicians and nurse practitioners? J Adv Nurs. 2017;73:240–252. [DOI] [PubMed] [Google Scholar]
- 27.Dietrich E, Leroux T, Santiago C, et al. Assessing practice pattern differences in the treatment of acute low back pain in the United States Military Health System. BMC Health Serv Res. 2018;18:720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hughes DR, Jiang M, Duszak R., Jr A comparison of diagnostic imaging ordering patterns between advanced practice clinicians and primary care physicians following office-based evaluation and management visits. JAMA Intern Med. 2015;175:101–107. [DOI] [PubMed] [Google Scholar]
- 29.O’Reilly-Jacob M, Perloff J, Buerhaus P. Comparing the rates of low-value back images ordered by physicians and nurse practitioners for Medicare beneficiaries in primary care. Nurs Outlook. 2019;67:713–724. [DOI] [PubMed] [Google Scholar]
- 30.Mafi JN, Wee CC, Davis RB, et al. Comparing use of low-value health care services among U.S. advanced practice clinicians and physicians. Ann Intern Med. 2016;165:237–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perloff J, DesRoches CM, Buerhaus P. Comparing the cost of care provided to Medicare beneficiaries assigned to primary care nurse practitioners and physicians. Health Serv Res. 2016;51:1407–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mehrotra A, Adams JL, Thomas JW, et al. The impact of different attribution rules on individual physician cost profiles. Ann Intern Med. 2010;152:649–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
- 34.Sharabiani MT, Aylin P, Bottle A. Systematic review of comorbidity indices for administrative data. Med Care. 2012;50:1109–1118. [DOI] [PubMed] [Google Scholar]
- 35.Oaxaca R. Male-female wage differentials in urban labor markets. Int Econ Rev. 1973;14:693–709. [Google Scholar]
- 36.Blinder AS. Wage discrimination: reduced form and structural estimates. J Hum Resour. 1973;8:436–455. [Google Scholar]
- 37.Sen B. Using the Oaxaca-Blinder decomposition as an empirical tool to analyze racial disparities in obesity. Obesity. 2014;22:1750–1755. [DOI] [PubMed] [Google Scholar]
- 38.Taber DR, Robinson WR, Bleich SN, et al. Deconstructing race and gender differences in adolescent obesity: Oaxaca-blinder decomposition. Obesity. 2016;24:719–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kino S, Kawachi I. How much do preventive health behaviors explain education- and income-related inequalities in health? Results of Oaxaca–Blinder decomposition analysis. Ann Epidemiol. 2020;43:44–50. [DOI] [PubMed] [Google Scholar]
- 40.Anderson GF, Reinhardt UE, Hussey PS, et al. It’s the prices, stupid: why the United States is so different from other countries. Health Aff. 2003;22:89–105. [DOI] [PubMed] [Google Scholar]
- 41.Graves JA, Mishra P, Dittus RS, et al. Role of geography and nurse practitioner scope-of-practice in efforts to expand primary care system capacity: health reform and the primary care workforce. Med Care. 2016;54:81–89. [DOI] [PubMed] [Google Scholar]
- 42.Xue Y, Smith JA, Spetz J. Primary care nurse practitioners and physicians in low-income and rural areas, 2010-2016. JAMA. 2019;321:102–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Buerhaus PI, DesRoches CM, Dittus R, et al. Practice characteristics of primary care nurse practitioners and physicians. Nurs Outlook. 2015;63:144–153. [DOI] [PubMed] [Google Scholar]
- 44.Medicare Payment Advisory Commission. Data Book, Section 2: Medicare Beneficiary Demographics. Washington, DC: Medicare Payment Advisory Comission; 2019. [Google Scholar]
- 45.Auerbach D, Staiger D, Buerhaus P. Growing ranks of advanced practice clinicians—implications for the physician workforce. New Engl J Med. 2018;378:2358–2360. [DOI] [PubMed] [Google Scholar]
- 46.Skinner L, Staiger DO, Auerbach DI, et al. Implications of an aging rural physician workforce. New Engl J Med. 2019;381:299–301. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Medicare & Medicaid Services. Medicare Shared Savings Program: Accountable Care Organizations—Pathways to Success. Vol 83 FR 417862018. 2018. Available at: https://www.federalregister.gov/documents/2018/08/17/2018-17101/medicare-program-medicare-shared-savings-program-accountable-care-organizations-pathways-to-success. Accessed March 17, 2020.
- 48.United States Congress. ACO Assignment Improvement Act of 2019-116th Congress. H.R. 900. 2019. Available at: https://www.congress.gov/bill/116th-congress/house-bill/900/text. Accessed March 15, 2020.
- 49.Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA. 2012;307:1513–1516. [DOI] [PubMed] [Google Scholar]
- 50.Cutler D. Putting Health Care Spending on a Sustainable Path, A Hearing before the Senate Budget Committee, 112th Congress, 1st Sess (2012). 2012. Available at: https://www.budget.senate.gov/imo/media/doc/davidcutler.pdf. Accessed November 15, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.


