Abstract
Aims
Valvular heart disease can be identified by calcification on coronary computed tomography angiography (CCTA) and has been associated with adverse clinical outcomes. We assessed aortic and mitral valve calcification in patients presenting with stable chest pain and their association with cardiovascular risk factors, coronary artery disease, and cardiovascular outcomes.
Methods and results
In 1769 patients (58 ± 9 years, 56% male) undergoing CCTA for stable chest pain, aortic and mitral valve calcification were quantified using Agatston score. Aortic valve calcification was present in 241 (14%) and mitral calcification in 64 (4%). Independent predictors of aortic valve calcification were age, male sex, hypertension, diabetes mellitus, and cerebrovascular disease, whereas the only predictor of mitral valve calcification was age. Patients with aortic and mitral valve calcification had higher coronary artery calcium scores and more obstructive coronary artery disease. The composite endpoint of cardiovascular mortality, non-fatal myocardial infarction, or non-fatal stroke was higher in those with aortic [hazard ratio (HR) 2.87; 95% confidence interval (CI) 1.60–5.17; P < 0.001] or mitral (HR 3.50; 95% CI 1.47–8.07; P = 0.004) valve calcification, but this was not independent of coronary artery calcification or obstructive coronary artery disease.
Conclusion
Aortic and mitral valve calcification occurs in one in six patients with stable chest pain undergoing CCTA and is associated with concomitant coronary atherosclerosis. Whilst valvular calcification is associated with a higher risk of cardiovascular events, this was not independent of the burden of coronary artery disease.
Keywords: aortic valve, mitral valve, computed tomography, computed tomography coronary angiography
Introduction
Valvular heart disease is an important cause of morbidity and mortality worldwide and shares similar risk factors with coronary artery disease.1 Incidental calcification of the aortic or mitral valve on computed tomography (CT) may identify patients with previously undiagnosed valvular heart disease. Coronary CT angiography (CCTA) is now a widely used non-invasive imaging modality, frequently the first-line investigation for patients with suspected coronary artery disease.2,3 Therefore, the identification of incidental valvular calcification on CCTA represents a potentially important opportunity for screening and patient risk stratification.4–7
Aortic valve calcification is an established marker of aortic stenosis, with the aortic valve calcium score on CT associated with hemodynamic severity of aortic stenosis on echocardiography.8–10 Robust sex-specific aortic valve CT calcium score thresholds for severe aortic stenosis have been proposed, validated,11,12 and recommended in recent international guidelines for the assessment of aortic stenosis severity when echocardiographic assessments are discordant.13 Mitral valve annular calcification is also a frequent finding on CCTA and may be associated with mitral valve dysfunction.14,15 Previous studies have suggested that patients with aortic stenosis and mitral valve calcification have an increased frequency of cardiovascular mortality beyond that related to the valve, including an increased risk of myocardial infarction (MI) and stroke, although the mechanisms underlying these associations remain unclear.7,16,17
In this study, we identified the prevalence and severity of incidental aortic and mitral valve calcification in patients undergoing CT as part of the Scottish COmputed Tomography of the HEART (SCOT-HEART) trial, and assessed their association with cardiovascular risk factors, coronary artery disease, and cardiovascular outcomes.
Methods
Study design
In the SCOT-HEART multicentre randomized controlled trial, 4146 patients with suspected angina due to coronary artery disease were randomized to undergo either standard care or standard care and CT.18The primary results of the SCOT-HEART trial have been published previously.19–21 Of the 1778 patients who subsequently underwent CT, 1769 images were available for analysis and included in this sub-study. Imaging included non-contrast CT for coronary artery calcium score and CCTA. The study was approved by the local ethics committee and participants provided written informed consent. The data underlying this article will be shared on reasonable request to the corresponding author.
Demographic information and cardiovascular risk factors
Demographic information and information on cardiovascular risk factors were collected prospectively within the SCOT-HEART trial and obtained from the SCOT-HEART database.
Computed tomography
CT imaging was performed using a 64 (Brilliance 64, Philips Medical Systems, Netherlands and Biograph mCT, Siemens, Germany) or 320 multidetector (Aquilion ONE, Toshiba Medical Systems, Japan) scanner. Non-contrast electrocardiogram-gated CT for coronary calcium scoring and contrast-enhanced CCTA were performed as described previously.18
Assessment of valvular calcification
All CCTA images were visually assessed for the presence of aortic or mitral valve/annulus calcification (Figure 1). Quantitative assessment of the aortic valve and mitral calcification was performed on non-contrast CT imaging using the Agatston scoring method as previously described.12,15,22Non-contrast images with 3-mm slices and 3-mm increment were assessed using semi-automatic software (VScore, Vital Images, USA). A threshold of 130 Hounsfield units was used for the identification of calcification. For cases where the location of the valve was uncertain on non-contrast images, contrast-enhanced CCTA was used to visually confirm the anatomy.
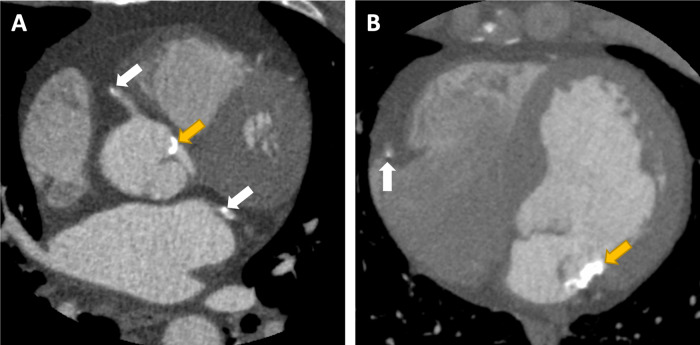
Figure 1.
Calcification of the aortic (A) and mitral (B) annulus (yellow arrow in patients with co-existing coronary artery disease (white arrow).
Clinical outcomes
Outcome information was obtained from national electronic health linkage data provided by the electronic Data Research and Innovation Service (eDRIS) of the National Health Service (NHS) Scotland. Outcomes were confirmed by review of the patient health records where required. Surgical coding information was used to identify patients who underwent aortic or mitral valve surgery using the OPCS (Office of Population Censuses and Surveys) 4 Classification of Surgical Operations and Procedures.
Statistical analysis
The primary composite endpoint of this sub-study was cardiovascular mortality, non-fatal MI, or non-fatal stroke. Quantitative data are presented as mean and standard deviation or, if the data were not normally distributed, median and interquartile intervals. Statistical significance was assessed using Pearson’s χ2 test, Fisher’s exact test, Students t-test, or Mann–Whitney U test, as appropriate. Correlations were assessed using Spearman’s rank order correlation (0–0.19 very weak, 0.2–0.39 weak, 0.40–0.59 moderate, 0.6–0.79 strong, and 0.8–1 very strong). Hazard ratios (HRs) and 95% confidence intervals (CIs) are presented. Ordinal regression analysis was performed to assess the effect of cardiovascular risk factors on aortic and mitral valve calcification. Multivariable analysis was performed including valvular calcification, coronary artery calcification, and the presence of obstructive coronary artery disease. Outcome data were analysed using Cox proportional hazards regression and presented graphically using cumulative incidence plots of the time to the first event. Statistical analysis was performed using R version 3.5.0 (R Foundation for Statistical Computing, Vienna, Austria). A statistically significant difference was defined as a two-sided P-value <0.05.
Results
Study population
Of the 4146 patients recruited into the study, 2073 were randomized to CT and 1769 CT scans were available and of suitable quality for analysis. Valvular calcification (Table 1) was identified in 273 (15%) patients, with aortic valve calcification occurring in 241 (14%) patients, mitral calcification in 64 (4%) patients, and combined aortic and mitral calcification in 32 (2%) patients. After 4.82 ± 1.13 years of follow-up, 53 patients had met the composite endpoint: cardiovascular mortality (n = 4), non-fatal MI (n = 38), or non-fatal stroke (n = 11).
Table 1.
Characteristics of study participants
| All participants | Aortic valve calcification |
Mitral valve calcification |
|||
|---|---|---|---|---|---|
| P-value | P-value | ||||
| N | 1769 | 241 (14%) | 64 (4%) | ||
| Male | 997 (56%) | 178 (74%) | <0.001 | 41 (64%) | 0.206 |
| Age (years) | 58 ± 9 | 64 ± 7 | <0.001 | 65 ± 7 | <0.001 |
| Body mass index (kg/m2) | 30 ± 6 | 30 ± 5 | 0.896 | 30 ± 5 | 0.386 |
| Atrial fibrillation | 34 (2%) | 7 (3%) | 0.213 | 2 (3%) | 0.350 |
| Smoking status | |||||
| Current smoker | 330 (19%) | 37 (15%) | 0.007 | 5 (8%) | 0.007 |
| Ex-smoker | 593 (34%) | 102 (42%) | 32 (50%) | ||
| Non-smoker | 845 (48%) | 102 (42%) | 27 (43%) | ||
| Hypertension | 608 (35%) | 122 (51%) | <0.001 | 36 (57%) | <0.001 |
| Diabetes Mellitus | 196 (11%) | 45 (19%) | <0.001 | 14 (22%) | 0.005 |
| Family history CHD | 765 (45%) | 91 (38%) | 0.048 | 20 (32%) | 0.053 |
| Previous CHD | 178 (10%) | 39 (16%) | <0.001 | 11 (17%) | 0.054 |
| Previous PAD | 31 (2%) | 7 (3%) | 0.178 | 1 (2%) | 1 |
| Previous CVD | 79 (4%) | 27 (11%) | <0.001 | 6 (10%) | 0.059 |
| Total cholesterol concentration (mg/dL) | 192 ± 73 | 179 ± 74 | 0.003 | 182 ± 85 | 0.324 |
| Anginal symptoms | |||||
| Typical angina | 654 (37%) | 124 (51%) | <0.001 | 33 (52%) | 0.046 |
| Atypical angina | 432 (24%) | 66 (27%) | 11 (17%) | ||
| Non-anginal | 683 (39%) | 51 (21%) | 20 (31%) | ||
| Risk score | 17.9 ± 11.0 | 24.6 ± 11.1 | <0.001 | 25.5 ± 11.5 | <0.001 |
Data are presented as N (%), mean ± standard deviation, or median (interquartile range).
P-values represent comparison to total cohort.
CHD, coronary heart disease; CTCA, computed tomography coronary angiography; CVD, cerebrovascular disease; PAD, peripheral arterial disease. Bold values indicate statistical significance.
Aortic valve calcification
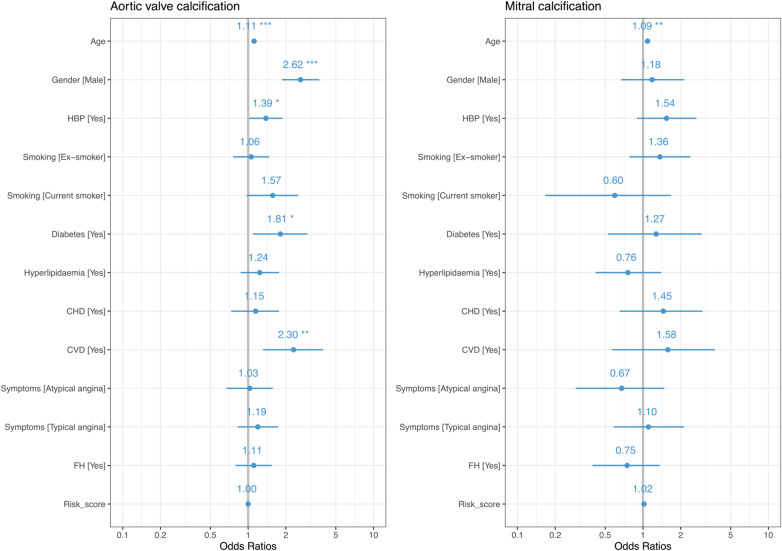
Independent predictors of the presence of aortic valve calcification (Figure 2) were age [odds ratio (OR) 1.11; 95% CI 1.08–1.15; P < 0.001], male sex (OR 2.62; 95% CI 1.87–3.70; P < 0.001), hypertension (OR 1.39, 95% CI 1.02–1.88; P = 0.037), diabetes mellitus (OR 1.81; 95% CI 1.09–2.97; P = 0.020), and a prior history of cerebrovascular disease (OR 2.30; 95% CI 1.32–3.96; P = 0.003).
Figure 2.
Multivariable analysis of cardiovascular risk factors and the presence of aortic valve or mitral calcification. Age (years); male gender compared to female gender; smoking status compared to non-smokers; total cholesterol concentration per unit increment; symptoms compared to those with non-anginal chest pain; Risk_score, ASSIGN cardiovascular risk score; AF, atrial fibrillation; BMI, body mass index; CHD, previous history of coronary heart disease; CVD, previous history of cerebrovascular disease; FH, family history of coronary heart disease; HBP, hypertension; PVD, previous history of peripheral vascular disease; *P < 0.05; **P < 0.01; ***P < 0.001.
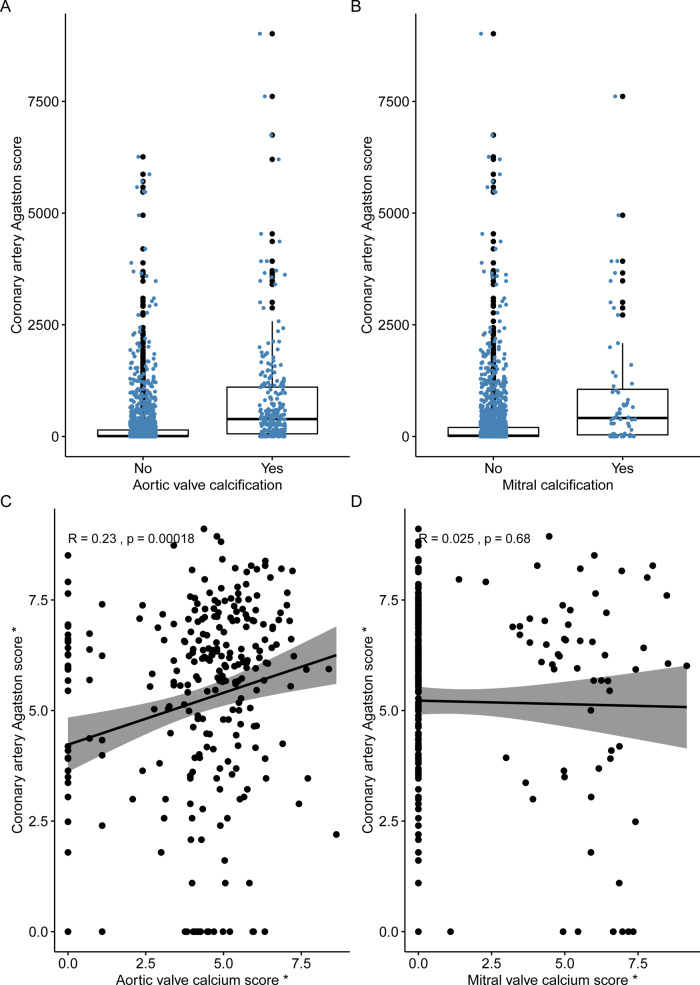
Patients with aortic valve calcification had a higher coronary artery calcium score [390 (interquartile range, IQR 61–1105) Agatston units (AU)] compared to those without aortic valve calcification [8 (IQR 0–145) AU, P < 0.001, Figure 3]. Patients with aortic valve calcification were also more likely to have non-obstructive (41%) or obstructive (51%) coronary artery disease than patients without aortic valve calcification (P < 0.001). However, 9% (n = 21/241) of patients with aortic valve calcification had no coronary artery calcification, and 80% (n = 907/1127) of patients with coronary artery calcification had no aortic valve calcification. A correlation was observed between the aortic valve calcium score and coronary artery calcium score, but this was only weak (r = 0.23, P < 0.001, Figure 3).
Figure 3.
Coronary artery calcification was higher in patients with both (A) aortic valve calcification and (B) mitral valve calcification than patients without. Correlation between coronary artery Agatston calcium score and (C) aortic valve calcium score and (D) mitral valve calcium score. *log transformed.
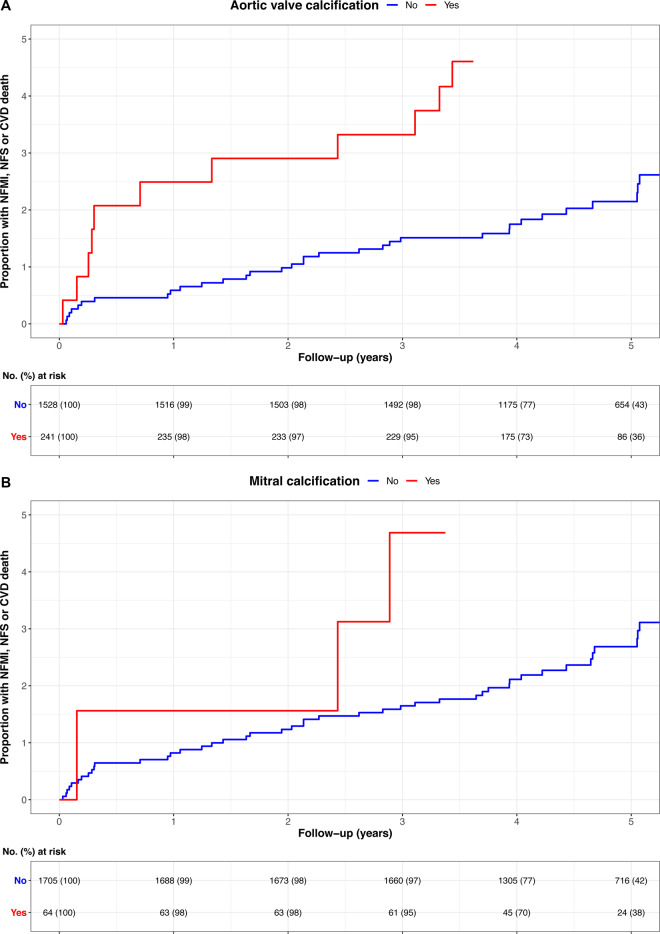
A higher proportion of patients with aortic valve calcification met the composite endpoint compared to patients without aortic valve calcification [6.6% (n = 16/241) vs. 2.4% (n = 37/1528), P = 0.002; HR 2.87; 95% CI 1.60–5.17; P < 0.001 (Figure 4)]. However, on multivariable analysis, only coronary artery calcium score was an independent predictor of the composite endpoint (Table 2).
Figure 4.
Cumulative incidence plot showing the association of the presence of (A) aortic valve calcification and (B) mitral calcification on the composite endpoint of cardiovascular death (CVD), non-fatal myocardial infarction (NFMI), or non-fatal stroke (NFS). The adverse outcomes associated with valve calcification were no longer evident once the burden of coronary atherosclerosis was considered in the multivariable model.
Table 2.
Univariable and multivariable analysis for aortic valve calcification and the composite endpoint of cardiovascular mortality, non-fatal myocardial infarction, or non-fatal stroke
| Univariable | Multivariable | |
|---|---|---|
| Aortic valve calcification |
2.87 (95% CI 1.60–5.17) P < 0.001 |
1.75 (95% CI 0.93–3.29) P = 0.081 |
| Coronary artery calcificationa |
1.18 (95% CI 1.10–1.27) P < 0.001 |
1.12 (95% CI 1.02–1.22) P = 0.022 |
| Obstructive coronary artery disease |
2.94 (95% CI 1.72–5.04) P < 0.001 |
1.50 (95% CI 0.76–2.98) P = 0.241 |
CI, confidence interval.
Per doubling.
Mitral valve calcification
The only independent predictor of the presence of mitral valve calcification (Figure 2) was age (OR 1.09; 95% CI 1.03–1.15; P = 0.002). Patients with mitral calcification had a higher coronary artery calcium score [413 (IQR 36–1056) AU] compared to those without mitral calcification [18 (IQR 0–202) AU, P < 0.001, Figure 4]. Patients with mitral calcification were also more likely to have both non-obstructive (45%) and obstructive (44%) coronary artery disease compared to patients without (P < 0.001). However, 14% (n = 9/64) of patients with mitral calcification had no coronary artery calcification, and 95% (n = 1072/1127) of patients with coronary artery calcification had no mitral calcification. There was no correlation between mitral valve calcium score and coronary artery calcium score (r = 0.03, P = 0.68, Figure 4).
Patients with mitral valve calcification were more likely to meet the composite endpoint compared to patients without mitral valve calcification [9.4% (n = 6/64) vs. 2.8% (n = 47/1705), P = 0.01]: HR 3.50; 95% CI 1.47–8.07; P = 0.004 (Figure 4). However, on multivariable analysis only coronary artery calcium score was an independent predictor of the composite endpoint (Table 3).
Table 3.
Univariable and multivariable analysis for mitral valve calcification and the composite endpoint of cardiovascular mortality, non-fatal myocardial infarction, or non-fatal stroke
| Univariable | Multivariable | |
|---|---|---|
| Mitral valve calcification | 3.45 (95% CI 1.50–8.07) P = 0.004 |
2.21 (95% CI 0.92–5.28) P = 0.075 |
| Coronary artery calcificationa |
1.18 (95% CI 1.10–1.27) P < 0.001 |
1.13 (95% CI 1.03–1.24) P = 0.012 |
| Obstructive coronary artery disease |
2.94 (95% CI 1.72–5.04) P < 0.001 |
1.54 (95% CI 0.78–3.06) P = 0.214 |
CI, confidence interval.
Per doubling.
Discussion
In this large multicentre randomized controlled trial of patients undergoing CT for stable chest pain, we have shown that valvular calcification is a common incidental finding, occurring in one in six patients. Aortic and mitral valve calcifications are associated with traditional cardiovascular risk factors and underlying coronary artery disease. Whilst patients with aortic or mitral calcification were three times more likely to suffer an adverse cardiovascular event, this effect was not independent of the burden of coronary artery disease. This indicates that the adverse prognosis associated with valve calcification in these patients is mediated by its association with coronary artery disease, rather than representing a direct causal effect.
In our study, valvular calcification was associated with a three-fold increased risk of cardiovascular death, MI, or stroke, but this was not independent of coronary artery calcium score, a marker of atherosclerotic plaque burden. Similar results were reported in a study of lung cancer screening patients, in whom aortic valve calcification did not provide incremental prognostic information over coronary calcification.23 This is in contrast to previous studies which reported an association between aortic stenosis or mitral valve calcification and adverse cardiovascular outcomes. In the Cardiovascular Health Study (CHS) study of patients over 65 years old, the presence of aortic stenosis on echocardiography was associated with a 50% increase in the risk of cardiovascular death and MI.24 In the Multi-Ethnic Study of Atherosclerosis (MESA) primary prevention study, the presence of aortic valve calcification was associated with a 72% increased risk of MI and 50% increase in the risk of cardiovascular events.25 However, similar to our study, this effect was no longer statistically significant after adjustment for cardiovascular risk factors, inflammatory biomarkers and coronary artery calcium score.25 We therefore provide further evidence to support the theory that cardiovascular events in patients with valvular calcification are driven by the association with coronary artery disease, rather than the presence of valvular heart disease itself.
In this study, we have confirmed the close association between valve calcification and both cardiovascular risk factors and coronary atherosclerosis. Similar to previous studies,15,26–28 we found that age, male sex, hypertension, diabetes, and prior history of cerebrovascular disease were independent predictors of aortic valve calcification, whilst age was the only independent predictors of mitral calcification. This suggests that there are overlapping but distinct mechanisms underlying these pathologies.
The vast majority of patients with aortic and mitral valve calcification had evidence of co-existent coronary calcification on CT calcium scoring, reflecting the pathological overlap between atherosclerosis and the early stages of both aortic and mitral valve calcification, as well as shared risk factors for these conditions.25,29–31 However, the correlation between coronary artery calcification and aortic valve calcium scores was poor, and there was no correlation with mitral calcium scores. Although most patients with valvular heart disease had obstructive or non-obstructive coronary artery disease, few patients with coronary artery disease had valvular heart disease. Thus, the presence of valvular heart disease could be a trigger to assess the coronary arteries, but the presence of coronary artery disease is not an indication for valvular assessment with echocardiography.
Our study has several limitations. This includes the small number of clinical events and that patients were managed according to routine clinical practice rather than having management prescribed on the basis of the imaging findings. The prevalence of valvular calcification and cardiovascular risk factors varies depending on the cohort studied. The age range of the SCOT-HEART population meant that mild calcification was the most common pathology and that the 5-year duration of follow-up might not have been sufficient for this early stage of disease to result in clinical events. In addition, the SCOT-HEART participants were recruited from cardiology outpatient clinics with suspected angina due to coronary artery disease. Although two-thirds of the patients were ultimately diagnosed as not having angina due to coronary artery disease, these results may not be representative of asymptomatic patients or the general population. Finally, we do not have data on the progression of valve calcification in this cohort which in other studies appears unrelated to cardiovascular risk factors but is most closely associated with the severity of baseline valve disease and calcification.
Conclusion
Valvular calcification is a frequent incidental finding on CCTA and is associated with cardiovascular risk factors and the presence of coronary artery disease. Whilst patients with aortic or mitral valve calcification demonstrate a three-fold increased risk of future adverse cardiovascular events, this appears to be mediated by co-existent coronary artery disease.
Supplementary data
Supplementary data are available at European Heart Journal - Cardiovascular Imaging online.
Funding
This trial was funded by the Chief Scientist Office of the Scottish Government Health and Social Care Directorates (CZH/4/588), with supplementary awards from Edinburgh and Lothian’s Health Foundation Trust and the Heart Diseases Research Fund. D.E.N. (CH/09/002, RG/16/10/32375, RE/18/10/33842) and M.C.W. (FS/11/014) are supported by the British Heart Foundation. M.C.W. is supported by the Chief Scientist Office of the Scottish Government Health (PCL/17/04). D.E.N. is the recipient of a Wellcome Trust Senior Investigator Award (WT103782AIA). P.D.A. is supported by a Heart Foundation of New Zealand Senior Fellowship (1844). A.J.M. is supported by a British Heart Foundation Accelerator Award Clinical Lectureship (AA/18/3/34220). E.v.B. is supported by the Scottish Imaging Network: A Platform of Scientific Excellence (SINAPSE). M.R.D. is supported by the British Heart Foundation (FS/14/78/31020) and the Sir Jules Thorn Biomedical Research Award 2015 (15/JTA). The Royal Bank of Scotland supported the provision of 320-multidetector CT for NHS Lothian and the University of Edinburgh. The Edinburgh Imaging facility QMRI (Edinburgh) is supported by the National Health Service Research Scotland (NRS) through National Health Service Lothian Health Board. The Clinical Research Facility Glasgow and Clinical Research Facility Tayside are supported by National Health Service Research Scotland (NRS).
Conflict of interest: Outside the submitted work, Professor Van Beek reports research support from Siemens and personal fees or other financial activity from QCTIS Ltd, Mentholatum, InHealth, and Aidence. All other authors have declared no conflict of interest.
Supplementary Material
References
- 1. d'Arcy JL, Coffey S, Loudon MA, Kennedy A, Pearson-Stuttard J, Birks J et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: the OxVALVE Population Cohort Study. Eur Heart J 2016;37:3515–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute for Health and Clinical Excellence. Chest Pain of Recent Onset: Assessment and Diagnosis of Recent Onset Chest Pain or Discomfort of Suspected Cardiac Origin. Clinical Guideline 95. NICE, London 2016. [PubMed]
- 3. Knuuti J, Wijns W, Saraste A, Capodanno D, Barbato E, Funck-Brentano C et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: the Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC). Eur Heart J 2019;41:407–77. [DOI] [PubMed] [Google Scholar]
- 4. Barasch E, Gottdiener JS, Marino Larsen EK, Chaves PH, Newman AB. Cardiovascular morbidity and mortality in community-dwelling elderly individuals with calcification of the fibrous skeleton of the base of the heart and aortosclerosis (The Cardiovascular Health Study). Am J Cardiol 2006;97:1281–6. [DOI] [PubMed] [Google Scholar]
- 5. Kizer JR, Wiebers DO, Whisnant JP, Galloway JM, Welty TK, Lee ET et al. Mitral annular calcification, aortic valve sclerosis, and incident stroke in adults free of clinical cardiovascular disease: the Strong Heart Study. Stroke 2005;36:2533–7. [DOI] [PubMed] [Google Scholar]
- 6. Fox CS, Vasan RS, Parise H, Levy D, O’Donnell CJ, D’Agostino RB et al. Mitral annular calcification predicts cardiovascular morbidity and mortality: the Framingham Heart Study. Circulation 2003;107:1492–6. [DOI] [PubMed] [Google Scholar]
- 7. Clavel MA, Pibarot P, Messika-Zeitoun D, Capoulade R, Malouf J, Aggarval S et al. Impact of aortic valve calcification, as measured by MDCT, on survival in patients with aortic stenosis: results of an international registry study. J Am Coll Cardiol 2014;64:1202–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cowell SJ, Newby DE, Burton J, White A, Northridge DB, Boon NA et al. Aortic valve calcification on computed tomography predicts the severity of aortic stenosis. Clin Radiol 2003;58:712–6. [DOI] [PubMed] [Google Scholar]
- 9. Liu F, Coursey CA, Grahame-Clarke C, Sciacca RR, Rozenshtein A, Homma S et al. Aortic valve calcification as an incidental finding at CT of the elderly: severity and location as predictors of aortic stenosis. Am J Roentgenol 2006;186:342–9. [DOI] [PubMed] [Google Scholar]
- 10. Koos R, Kuhl HP, Muhlenbruch G, Wildberger JE, Gunther RW, Mahnken AH. Prevalence and clinical importance of aortic valve calcification detected incidentally on CT scans: comparison with echocardiography. Radiology 2006;241:76–82. [DOI] [PubMed] [Google Scholar]
- 11. Clavel MA, Messika-Zeitoun D, Pibarot P, Aggarwal SR, Malouf J, Araoz PA et al. The complex nature of discordant severe calcified aortic valve disease grading: new insights from combined Doppler echocardiographic and computed tomographic study. J Am Coll Cardiol 2013;62:2329–38. [DOI] [PubMed] [Google Scholar]
- 12. Pawade T, Clavel MA, Tribouilloy C, Dreyfus J, Mathieu T, Tastet L et al. Computed tomography aortic valve calcium scoring in patients with aortic stenosis. Circ Cardiovasc Imaging 2018;11:e007146. [DOI] [PubMed] [Google Scholar]
- 13. Falk V, Baumgartner H, Bax JJ, De Bonis M, Hamm C, Holm PJ et al. ; ESC Scientific Document Group. 2017 ESC/EACTS Guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg 2017;52:616–64. [DOI] [PubMed] [Google Scholar]
- 14. Labovitz AJ, Nelson JG, Windhorst DM, Kennedy HL, Williams GA. Frequency of mitral valve dysfunction from mitral anular calcium as detected by Doppler echocardiography. Am J Cardiol 1985;55:133–7. [DOI] [PubMed] [Google Scholar]
- 15. Massera D, Trivieri MG, Andrews JPM, Sartori S, Abgral R, Chapman AR et al. Disease activity in mitral annular calcification. Circ Cardiovasc Imaging 2019;12:e008513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lancellotti P, Magne J, Dulgheru R, Clavel M-A, Donal E, Vannan MA et al. Outcomes of patients with asymptomatic aortic stenosis followed up in heart valve clinics. JAMA Cardiol 2018;3:1060–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Di Minno MND, Poggio P, Conte E, Myasoedova V, Songia P, Mushtaq S et al. Cardiovascular morbidity and mortality in patients with aortic valve calcification: a systematic review and meta-analysis. J Cardiovasc Comput Tomogr 2019;13:190–5. [DOI] [PubMed] [Google Scholar]
- 18. Newby DE, Williams MC, Flapan AD, Forbes JF, Hargreaves AD, Leslie SJ et al. Role of multidetector computed tomography in the diagnosis and management of patients attending the rapid access chest pain clinic, The Scottish computed tomography of the heart (SCOT-HEART) trial: study protocol for randomized controlled trial. Trials 2012;13:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.SCOT-HEART investigators. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): an open-label, parallel-group, multicentre trial. Lancet 2015;385:2383–91. [DOI] [PubMed] [Google Scholar]
- 20.SCOT-HEART Investigators, Newby DE, Adamson PD, Berry C, Boon NA, Dweck MR et al. Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med 2018;379:924–33. [DOI] [PubMed] [Google Scholar]
- 21. Williams MC, Hunter A, Shah ASV, Assi V, Lewis S, Smith J et al. Use of coronary computed tomographic angiography to guide management of patients with coronary disease. J Am Coll Cardiol 2016;67:1759–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827–32. [DOI] [PubMed] [Google Scholar]
- 23. Willemink MJ, Takx RA, Isgum I, de Koning HJ, Oudkerk M, Mali WP et al. Prognostic value of heart valve calcifications for cardiovascular events in a lung cancer screening population. Int J Cardiovasc Imaging 2015;31:1243–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Otto CM, Lind BK, Kitzman DW, Gersh BJ, Siscovick DS. Association of aortic-valve sclerosis with cardiovascular mortality and morbidity in the elderly. N Engl J Med 1999;341:142–7. [DOI] [PubMed] [Google Scholar]
- 25. Owens DS, Budoff MJ, Katz R, Takasu J, Shavelle DM, Carr JJ et al. Aortic valve calcium independently predicts coronary and cardiovascular events in a primary prevention population. JACC Cardiovasc Imaging 2012;5:619–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stewart BF, Siscovick D, Lind BK, Gardin JM, Gottdiener JS, Smith VE et al. Clinical factors associated with calcific aortic valve disease. Cardiovascular Health Study. J Am Coll Cardiol 1997;29:630–4. [DOI] [PubMed] [Google Scholar]
- 27. Eveborn GW, Schirmer H, Lunde P, Heggelund G, Hansen JB, Rasmussen K. Assessment of risk factors for developing incident aortic stenosis: the Tromso Study. Eur J Epidemiol 2014;29:567–75. [DOI] [PubMed] [Google Scholar]
- 28. Yan AT, Koh M, Chan KK, Guo H, Alter DA, Austin PC et al. Association between cardiovascular risk factors and aortic stenosis: the CANHEART Aortic Stenosis Study. J Am Coll Cardiol 2017;69:1523–32. [DOI] [PubMed] [Google Scholar]
- 29. Gondrie MJ, van der Graaf Y, Jacobs PC, Oen AL, Mali WP; On behalf of the PROVIDI Study Group. The association of incidentally detected heart valve calcification with future cardiovascular events. Eur Radiol 2011;21:963–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Atar S, Jeon DS, Luo H, Siegel RJ. Mitral annular calcification: a marker of severe coronary artery disease in patients under 65 years old. Heart 2003;89:161–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Barasch E, Gottdiener JS, Larsen EK, Chaves PH, Newman AB, Manolio TA. Clinical significance of calcification of the fibrous skeleton of the heart and aortosclerosis in community dwelling elderly. The Cardiovascular Health Study (CHS). Am Heart J 2006;151:39–47. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.