Abstract
Background
Lesions of the posterior segment of the medial meniscus are the most common intraarticular lesions associated with ACL injuries. Ramp lesions are tears in the peripheral attachment of the posterior horn of the medial meniscus. Such injuries are difficult to detect on preoperative MRI. Arthroscopically, the prevalence of these lesions can reach 24%. Anatomical descriptions of the posterior horn of the medial meniscus are becoming clearer, however, histological descriptions are lacking, especially with regard to the presence or absence of capillaries.
Questions/purposes
The present qualitative histologic study focused on the posterior segment of the medial meniscus and the meniscocapsular and meniscotibial junctions. Specifically, the objective of this study was to analyze the posterior segment of the medial meniscus and the meniscosynovial junction and to determine whether the meniscus tibial ligament exists.
Methods
We dissected 10 unpaired cadaveric knees (five male, five female, age range 55 to 66 years), five left and five right, from the French “Don du corps” body donation program via a posterior approach to the posteromedial capsule. We excluded specimens with intra-articular abnormalities (ACL rupture, meniscal tear, arthrosis) preceding dissection by arthrotomy. We thus accessed the posterior segment of the medial meniscus and the meniscosynovial junction. The proximal capsule, posterior segment of the medial meniscus, entire meniscal capsular-tibial junction, and a fragment of the tibia were removed en bloc. For each knee, three sagittal spaced sections of the posterior segment of the medial meniscus (Zone 4 as defined by Śmigielski) were performed. Two experienced pathologists performed qualitative histological analysis on the 30 samples after Hematoxylin and eosin staining, and Safranin O staining.
Results
Macroscopically, the meniscotibial attachments were pellucid and homogeneous, as were the meniscocapsular attachments; however, the meniscocapsular attachments appeared to be denser in both the anterior and posterior regions of the capsule. Microscopy of the meniscosynovial junction revealed loose collagen fibers that were partially oriented but not parallel, a cellular network featuring a few fibroblasts and adipocytes, and several capillaries. No between-attachment histologic differences were apparent; both tissues shared a site of attachment to the posterior horn of the medial meniscus. We did not detect the meniscotibial ligament, macroscopically or microscopically.
Conclusions
A ramp lesion may not be a ligamentous injury because the meniscotibial ligament was not detected. Rather, it appears that a ramp lesion is a tear in the common attachment point between the posterior horn of the medial meniscus and meniscocapsular and meniscotibial junctions. This structure is vascularized, and contains nonoriented low cellularity collagen of moderate density.
Clinical Relevance
Based on our results, a better rationale for the recommendation of surgical repair of a ramp appears to be needed, given the absence of a meniscotibial ligament, and the presence of capillaries in the meniscocapsular and meniscotibial attachments.
Introduction
Lesions in the posterior segment of the medial meniscus are the intraarticular lesions that are most commonly associated with ACL ruptures [9]. Of these, ramp lesions, as described by Strobel [16], correspond to tears in the posterior meniscocapsular junction at the level of the posterior horn of the medial meniscus; such lesions are present in 16% to 24% of all ACL tears [5, 13, 14].
The anatomy of the posterior horn of the medial meniscus is becoming better described [3, 12]; the meniscocapsular and meniscotibial attachments are in Zone 4 as described by Śmigielski et al. [12]. The superior part of the meniscus periphery in Zone 4 does not attach to the capsule. In contrast, the inferior part attaches to the tibia via loose connective tissue, forming the meniscotibial attachments, and for some authors, it corresponds to the meniscotibial ligament (Fig. 1) [3, 10, 12].
Fig. 1.

This drawing shows the meniscotibial ligament as illustrated by Peltier et al. [10] (yellow = site of the tear). Reprinted by permission from Springer Nature: Springer, Knee Surgery, Sports Traumatology, Arthroscopy. The role of the meniscotibial ligament in posteromedial rotational knee stability. A. Peltier, T. Lording, L. Maubisson, R. Ballis, P. Neyret, S. Lustig, Copyright (2015).
During follow-up after ACL reconstruction in patients who have a medial meniscus that is initially considered healthy, the medial meniscus sometimes deteriorates, despite effective ACL reconstruction knee stabilization [11]. Stephen et al. [15] concluded that posterior, medial meniscocapsular lesions place excessive stress on the ACL.
Management of ramp lesions during ACL reconstruction procedures is still controversial. Some authors advocate surgical repair of all meniscal ramp lesions at the time of ACL reconstruction, based on an elevated risk of persistent instability and biomechanical reconstruction graft failure if the lesion remains untreated [1, 7, 10]. However, given vascularization of the capsule and the red-red zone of the meniscus, some clinical studies have reported that the tears healed without surgical treatment [6, 20]. To our knowledge, no study has had as its main objective the qualitative histological analysis of the meniscocapsular and meniscotibial attachments of the posterior horn of the medial meniscus.
Thus, the present histologic study focused on the posterior segment of the medial meniscus and the meniscocapsular and meniscotibial junctions. Specifically, the objective of this study was to analyze the posterior segment of the medial meniscus and the meniscosynovial junction and to determine whether the meniscus tibial ligament exists.
Materials and Methods
Specimen Preparation
From May 2016 to October 2018, we studied 10 fresh-frozen, cadaveric knee specimens (mean [range] cadaver age, 61 years [55 to 66], five left and five right knees, nonpaired, from five males and five females) with no evidence of prior injury or previous surgery. The specimens were received from the French “don du corps” body donation program. All specimens were stored at -20° C and thawed at room temperature for 24 hours before preparation. Before the study, each specimen underwent arthrotomy to confirm the absence of intraarticular conditions, such as minimal articular cartilage wear, ligament tears, and meniscal tears or prior meniscal surgery. All dissections were performed by a senior orthopaedic surgeon (RDF, GLH) or a junior surgeon (QN) under supervision.
In the prone position, the approach was posterior, direct, and via the popliteal region. The hamstring and gastrocnemius muscles were identified, isolated, and sectioned, revealing the posterior knee capsule. The capsule was opened at its most proximal part, at the lower end of the femur, to allow access to the posterior segment of the medial meniscus and its meniscosynovial junction (Fig. 2).
Fig. 2.

This photograph shows a medial view of a right knee and the medial meniscus posterior segment in situ after sagittal sectioning of the medial tibial plateau; F = medial femoral condyle; M = medial meniscus posterior segment; T = tibial plateau; * = meniscosynovial junction; ant = anterior; sup = superior.
We divided the medial meniscus at its posterior root and the midposterior segment junction, allowing isolation of the posterior segment of the medial meniscus. Using osteotomes, we excised the posterior portion of the medial tibial plateau, ensuring inclusion of the proximal capsule, posterior segment of the medial meniscus, entire meniscosynovial junction, and a tibia fragment in one block. Each piece was then cut in half, providing a macroscopic section that passed through the posterior segment of the medial meniscus.
Histologic Analysis
When dissections were completed, the samples were sent to our pathology laboratory for qualitative histological analysis. The posterior horn of the medial meniscus was our area of interest. All tissues were fixed in 10% (v/v) neutral-buffered formalin at room temperature for 24 hours, then in a formic acid solution for 8 days (to ensure complete decalcification). Subsequently, the samples were rinsed in phosphate-buffered saline and stored in phosphate-buffered saline at 4° C before manual paraffin processing. Paraffin processing was performed as follows: tissues were dehydrated in baths of 75% and 100% v/v ethanol, cleared using three changes of xylene, and paraffin-infiltrated with three changes of paraffin wax at 60 °C under continuous agitation. Tissues embedded in paraffin were solidified in cassettes, placed on ice, and sagittally sectioned in a 6-µm thickness in three areas (Fig. 3): one lateral, one medial, and one central for a total of 30 samples. These sections were performed in Zone 4 as described by Śmigielski [12], which is where the ramp lesions are reported to occur [13, 17, 18]. Before sections were stained, they were dried in an oven at 60° C for 2 hours, deparaffinized with two changes of xylene, and rehydrated in water. Hematoxylin and eosin staining and Safranin O staining was then performed to determine the presence of collagen and the evaluation of its density and orientation/organization of the meniscocapsular and meniscotibial attachments relative to the posterior medial meniscus, the presence of cell nuclei and their morphology, in particular fibroblasts, and finally to identify the presence of capillaries. All images were obtained using an optical microscope fitted with an automatic slide scanner (Pannoramic MIDI, 3DHISTECH, Hongria) at 10 x, 20 x, and 50 x magnification.
Fig. 3.
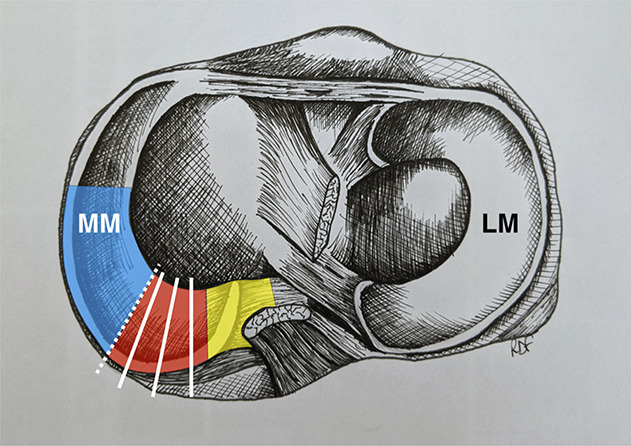
This anatomic drawing shows a superior view of the right tibial plateau. The red zone corresponds to zone 4 of Śmigielski [12] (posterior horn of the medial meniscus), in which the three sagittal sections (medial, central, lateral) for the histological study are represented (white lines). The yellow zone corresponds to Śmigielski zone 5 (posterior root) and the blue zone to Śmigielski zone 3. The hatched white line corresponds to the mid-posterior segment junction; MM = medial meniscus; LM = lateral meniscus.
Two experienced pathologists (IQR, PA) reviewed all the 30 histological samples and directly interpreted the results regarding qualitative findings.
Results
Macroscopy
The meniscosynovial junction was easily identifiable in situ and in the prepared blocks (Fig. 4). The meniscotibial and meniscocapsular attachments were pellucid and homogeneous, and appeared to be denser in appearance at the anterior and posterior portions of the capsule (Fig. 5). We did not detect a macroscopically distinctive ligamentous structure corresponding to the meniscotibial ligament in the meniscosynovial junction of the medial meniscus.
Fig. 4.
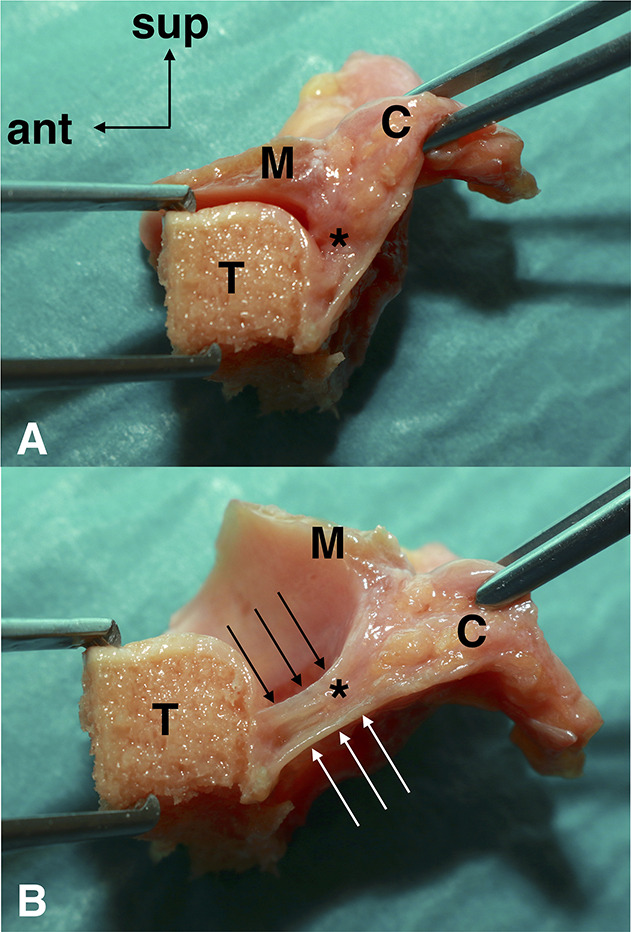
A-B This photograph shows one of the obtained specimens, including the capsule, medial meniscus posterior segment, meniscosynovial junction, and posterior edge of the tibial plateau. The (A) physiologic and (B) stretched specimens highlight the meniscosynovial junction. Anterior (black arrows) and posterior (white arrows) reinforcement of the distal capsule is shown. C = capsule; M = medial meniscus posterior segment; T = tibial plateau; * = meniscosynovial junction; ant = anterior; sup = superior. A color image accompanies the online version of this article.
Fig. 5.
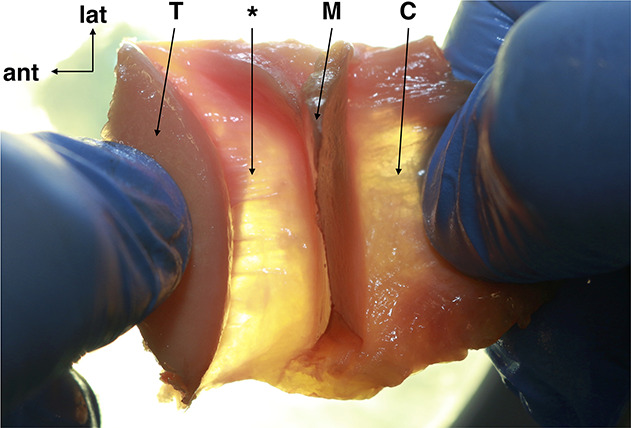
This transillumination photograph shows one of the specimens after the entire block was unrolled, and it shows homogeneity of the meniscosynovial junction (*); M = medial meniscus posterior segment; T = posterior border of the tibial plateau; C = capsule; * = meniscosynovial junction; ant = anterior; lat = lateral. A color image accompanies the online version of this article.
Microscopy
Optical microscopy of the 30 meniscosynovial junctions (meniscocapsular and meniscotibial attachments) at 10 x (Fig. 6) and 20 x (Fig. 7) magnification revealed loose collagen fibers that were partially oriented but not parallel; it also revealed a network with a few fibroblasts with round nuclei and adipocytes between the posterior segment of the medial meniscus and posterior edge of the medial tibial plateau at any level of the posterior segment of the medial meniscus. The architecture described was similar in all samples from these 10 knees and there was no difference in the three sections (lateral, central, or medial) of each sample. There was no interobserver difference in the conclusions of the histological analyses. The histologic definition of a ligament is subjective [8]; however, to our knowledge, ligaments feature connective tissue with a central band of dense collagen surrounded by loose peripheral collagen fibers; in this dense structure most fibroblast cells have elongated nuclei although round nuclei are sometimes observed). No dense central collagen band was found in our 30 samples.
Fig. 6.

This optical microscopic image shows the meniscosynovial junction between the posterior segment of the medial meniscus and the posterior edge of the medial tibial plateau; M = medial meniscus posterior segment; T = tibial plateau; * = meniscosynovial junction; post = posterior; sup = superior (10 x magnification, hematoxylin, eosin, and Safranin O staining; scale bar 2000 µm). A color image accompanies the online version of this article.
Fig. 7.

This optical microscopic image shows the meniscosynovial junction, including a thin layer of scalloped collagen (arrows) but no identifiable ligamentous structure; M = medial meniscus posterior segment; T = posterior border of the medial tibial plateau; post = posterior; * = meniscosynovial junction; sup = superior (20 x magnification, hematoxylin, eosin, and Safranin O staining, scale bar 1000 µm). A color image accompanies the online version of this article.
At 50 x magnification (Fig. 8), the meniscosynovial junction revealed an endothelial surface coating of regular-sized cells covering the underlying collagenous network (corresponding to the denser part found during macroscopic analysis); several capillaries were observed within the meniscosynovial junction. At this magnification, we also observed dense posterior collagenous tissue corresponding to the joint capsule. No histologic differences between the two attachments were evident; these attachments merged near their shared attachment site to the posterior horn of the medial meniscus.
Fig. 8.

This optical microscopy image of the meniscosynovial junction shows (A) a surface coating (small black arrows) underlying low-density collagen tissue in which capillaries (*) were found and dense posterior collagenous tissue corresponded to (B) the joint capsule. post = posterior; sup = superior (50 x magnification, hematoxylin, eosin, and Safranin O staining, scale bar 500 µm). A color image accompanies the online version of this article.
Regardless of the magnification (10 x, 20 x, or 50 x), no ligament structure was detected in the meniscotibial and meniscocapsular attachments.
Discussion
The management of ramp lesions is not yet well established, despite their high frequency, especially in association with ACL rupture. Some authors recommend their repair, especially of the meniscotibial ligament [4, 18], while others suggest spontaneous healing [6, 20]. However, the precise histological description of the meniscocapsular and meniscotibial attachments of the posterior horn of the medial meniscus is limited [3, 12]. The specific objective of our study was to analyze the meniscocapsular and meniscotibial attachments and to determine whether the meniscotibial ligament was present. We found that (1) the meniscal synovial joint is a vascularized structure with collagen that is of medium density and partially oriented; however, we did not detect a ligament structure corresponding to the meniscotibial ligament. (2) There is no histological difference between the meniscocapsular and meniscotibial attachments, and this conclusion is in agreement with one of the rare histological studies on this anatomical region [3].
Limitations
Our study had several limitations. Our sample size can be considered small; however, we believe that its size was sufficient to make our conclusions, and we do not think the results would have been different with more cadaveric specimens. The French body donation program does not provide any information on the medical and surgical history of cadaveric specimens. To avoid any pathology that could have modified the histology of the meniscocapsular and meniscotibial attachments (minimal articular cartilage wear, ligament tears, and meniscal tears or meniscal surgery), we performed an arthrotomy to ensure the healthy state of the knees studied. The cadaveric specimens were all aged 55 to 65 years, which is much older than the patients who typically sustain repairable meniscal injuries or ramp lesions. Therefore, we did not perform a quantitative assessment of collagen type or collagen content. However, even if the density of collagen may decrease with age, we would not expect the organization of the structure studied to be modified, implying that is impossible for the meniscotibial ligament to disappear with age.
Since we have not detected the meniscotibial ligament, that is, the structure that surgeons think they are repairing by surgically treating the ramp lesions, it is reasonable to ask what is really being repaired during the procedure. We suggest that the treatment addresses a region involving a mixture of connective tissue, meniscus, and joint capsule but not a ligament.
Some clinical studies [4, 17, 18] recommend repairing all ramp lesions during ACL reconstruction procedures, and other biomechanical studies suggest that ramp lesions are associated with rotatory constraints, AP instability, and excessive stress on the ACL if they are not repaired during ACL reconstruction [1, 2, 7, 10, 15]. Therefore, it seems that ramp lesions may have a role in the biomechanical knee deterioration.
Our histological analyses found medium density collagen in our area of interest. This could theoretically allow surgical fixation of the ramp lesion; this also supports the two studies that claim successful repair of the posterior meniscosynovial junction after 2 years of follow-up [4, 18]. Given our findings, a biomechanical study on the resistance of the meniscocapsular and meniscotibial attachments seems necessary.
With respect to the vasculature, we found many capillaries in the meniscosynovial junction; therefore, healing is theoretically possible. Several authors [4, 20] reported possible in vivo scarring of stable ramp lesions shorter than 1.5 cm. The relevant vasculature presumably developed from the vasculature of the joint capsule and meniscus in the red-red zone. However, we could not find any studies describing the meniscosynovial junction’s vasculature, therefore, a study focusing on the vascularization of the meniscosynovial junction is necessary to confirm this theory and to support the possibility of spontaneous healing of ramp lesions.
Recently, Vieira et al. [19] suggested that posteromedial instability was attributable to disruption of the important relationship between the tendon of the semimembranous muscle and the meniscosynovial junction. However, our study did not focus on this complex. The joint attachments of the meniscosynovial and meniscotibial junctions constitute a simple, single anatomic unit.
Conclusions
In summary, we have precisely analyzed the meniscotibial and meniscocapsular attachments of the posterior segment of the medial meniscus, which is the region where the lesions appear. We have found that it is a vascularized structure, with collagen that is of medium density and is partially oriented. However, no ligament structure corresponding to the meniscotibial ligament was detected. The numerous capillaries and the collagen that we found in this area theoretically suggest the possibility of healing, and surgical fixation of the ramp lesion may not be necessary. Based on our results, surgeons who recommend surgery to repair ramp lesions now need to provide a better rationale, especially with respect to the biomechanics, for their surgical indications. Tissue resistance and vascularization, as well as the nature of the posterior horn of the medial meniscus-semimembranous complex, should be explored in future studies.
Acknowledgments
We thank P. Alemany MD, for his help in the histological analysis of the samples. We thank S. Lustig MD, PhD, for granting authorization to use Fig. 1.
Footnotes
Each author certifies that he or she has no commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Brest University Hospital, Brest, France.
References
- 1.Ahn JH, Bae TS, Kang KS, Kang SY, Lee SH. Longitudinal tear of the medial meniscus posterior horn in the anterior cruciate ligament-deficient knee significantly influences anterior stability. Am J Sports Med. 2011;39:2187-2193. [DOI] [PubMed] [Google Scholar]
- 2.DePhillipo NN, Moatshe G, Brady A, Chahla J, Aman ZS, Dornan GJ, Nakama GY, Engebretsen L, LaPrade RF. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med. 2018;46:2422-2431. [DOI] [PubMed] [Google Scholar]
- 3.DePhillipo NN, Moatshe G, Chahla J, Aman ZS, Storaci HW, Morris ER, Robbins CM, Engebretsen L, LaPrade RF. Quantitative and qualitative assessment of the posterior medial meniscus anatomy: defining meniscal ramp lesions. Am J Sports Med. 2019;47:372-378. [DOI] [PubMed] [Google Scholar]
- 4.Li WP, Chen Z, Song B, Yang R, Tan W. The FasT-Fix repair technique for ramp lesion of the medial meniscus. Knee Surg Relat Res. 2015;27:56-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39:832-837. [DOI] [PubMed] [Google Scholar]
- 6.Liu X, Zhang H, Feng H, Hong L, Wang XS, Song GY. Is it necessary to repair stable ramp lesions of the medial meniscus during anterior cruciate ligament reconstruction? A prospective randomized controlled trial. Am J Sports Med. 2017;45:1004-1011. [DOI] [PubMed] [Google Scholar]
- 7.Mouton C, Magosch A, Pape D, Hoffmann A, Nührenbörger C, Seil R. Ramp lesions of the medial meniscus are associated with a higher grade of dynamic rotatory laxity in ACL-injured patients in comparison to patients with an isolated injury. Knee Surg Sports Traumatol Arthrosc. 2020;28:1023-1028. [DOI] [PubMed] [Google Scholar]
- 8.Neri T, Dalcol P, Palpacuer F, Bergandi F, Prades JM, Farizon F, Philippot R, Peoc’h M. The anterolateral ligament is a distinct ligamentous structure: a histological explanation. Knee. 2018;25:360-366. [DOI] [PubMed] [Google Scholar]
- 9.Noyes FR, Chen RC, Barber-Westin SD, Potter HG. Greater than 10-year results of red-white longitudinal meniscal repairs in patients 20 years of age or younger. Am J Sports Med. 2011;39:1008-1017. [DOI] [PubMed] [Google Scholar]
- 10.Peltier A, Lording T, Maubisson L, Ballis R, Neyret P, Lustig S. The role of the meniscotibial ligament in posteromedial rotational knee stability. Knee Surg Sports Traumatol Arthrosc. 2015;23:2967-2973. [DOI] [PubMed] [Google Scholar]
- 11.Rochcongar G, Cucurulo T, Ameline T, Potel JF, Dalmay F, Pujol N, Sallé de Chou É, Lutz C, Ehkirch FP, Le Henaff G, Laporte C, Seil R, Gunepin FX, Sonnery-Cottet B, la SFA. Meniscal survival rate after anterior cruciate ligament reconstruction. Orthop Traumatol Surg Res. 2015;101:S323-S326. [DOI] [PubMed] [Google Scholar]
- 12.Śmigielski R, Becker R, Zdanowicz U, Ciszek B. Medial meniscus anatomy-from basic science to treatment. Knee Surg Sports Traumatol Arthrosc. 2015;23:8-14. [DOI] [PubMed] [Google Scholar]
- 13.Sonnery-Cottet B, Conteduca J, Thaunat M, Gunepin FX, Seil R. Hidden lesions of the posterior horn of the medial meniscus: a systematic arthroscopic exploration of the concealed portion of the knee. Am J Sports Med. 2014;42:921-926. [DOI] [PubMed] [Google Scholar]
- 14.Sonnery-Cottet B, Praz C, Rosenstiel N, Blakeney WG, Ouanezar H, Kandhari V, Vieira TD, Saithna A. Epidemiological evaluation of meniscal ramp lesions in 3214 anterior cruciate ligament-injured knees from the SANTI study group database: a risk factor analysis and study of secondary meniscectomy rates following 769 ramp repairs. Am J Sports Med. 2018;46:3189-3197. [DOI] [PubMed] [Google Scholar]
- 15.Stephen JM, Halewood C, Kittl C, Bollen SR, Williams A, Amis AA. Posteromedial meniscocapsular lesions increase tibiofemoral joint laxity with anterior cruciate ligament deficiency, and their repair reduces laxity. Am J Sports Med. 2016;44:400-408. [DOI] [PubMed] [Google Scholar]
- 16.Strobel MJ. Manual of Arthroscopic Surgery. Berlin Heidelberg; Springer-Verlag: 2002. [Google Scholar]
- 17.Thaunat M, Fayard JM, Guimaraes TM, Jan N, Murphy CG, Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5:e871-e875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thaunat M, Jan N, Fayard JM, Kajetanek C, Murphy CG, Pupim B, Gardon R, Sonnery-Cottet B. Repair of meniscal ramp lesions through a posteromedial portal during anterior cruciate ligament reconstruction: outcome study with a minimum 2-year follow-up. Arthroscopy. 2016;32:2269-2277. [DOI] [PubMed] [Google Scholar]
- 19.Vieira TD, Pioger C, Frank F, Saithna A, Cavaignac E, Thaunat M, Sonnery-Cottet B. Arthroscopic dissection of the distal semimembranosus tendon: an anatomical perspective on posteromedial instability and ramp lesions. Arthrosc Tech. 2019;8:e987-e991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yagishita K, Muneta T, Ogiuchi T, Sekiya I, Shinomiya K. Healing potential of meniscal tears without repair in knees with anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:1953-1961. [DOI] [PubMed] [Google Scholar]


