Abstract
Background
The coronavirus disease 2019 pandemic has resulted in a rapid pivot toward telemedicine owing to closure of in-person elective clinics and sustained efforts at physical distancing worldwide. Throughout this period, there has been revived enthusiasm for delivering and receiving orthopaedic care remotely. Unfortunately, rapidly published editorials and commentaries during the pandemic have not adequately conveyed findings of published randomized trials on this topic.
Questions/purposes
In this systematic review and meta-analysis of randomized trials, we asked: (1) What are the levels of patient and surgeon satisfaction with the use of telemedicine as a tool for orthopaedic care delivery? (2) Are there differences in patient-reported outcomes between telemedicine visits and in-person visits? (3) What is the difference in time commitment between telemedicine and in-person visits?
Methods
In accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, we conducted a systematic review with the primary objective to determine patient and surgeon satisfaction with telemedicine, and secondary objectives to determine differences in patient-reported outcomes and time commitment. We used combinations of search keywords and medical subject headings around the terms “telemedicine”, “telehealth”, and “virtual care” combined with “orthopaedic”, “orthopaedic surgery” and “randomized.” We searched three medical databases (MEDLINE, Embase, and the Cochrane Library) in duplicate and performed manual searches to identify randomized controlled trials evaluating the outcomes of telemedicine and in-person orthopaedic assessments. Trials that studied an intervention that was considered to be telemedicine (that is, any form of remote or virtual care including, but not limited to, video, telephone, or internet-based care), had a control group that comprised in-person assessments performed by orthopaedic surgeons, and were reports of Level I original evidence were included in this study. Studies evaluating physiotherapy or rehabilitation interventions were excluded. Data was extracted by two reviewers and quantitative and qualitive summaries of results were generated. Methodological quality of included trials was assessed using the Cochrane Risk of Bias tool, which uniformly rated the trials at high risk of bias within the blinding categories (blinding of providers, patients, and outcome assessors). We screened 133 published articles; 12 articles (representing eight randomized controlled trials) met the inclusion criteria. There were 1008 patients randomized (511 to telemedicine groups and 497 to control groups). Subspecialties represented were hip and knee arthroplasty (two trials), upper extremity (two trials), pediatric trauma (one trial), adult trauma (one trial), and general orthopaedics (two trials).
Results
There was no difference in the odds of satisfaction between patients receiving telemedicine care and those receiving in-person care (pooled odds ratio 0.89 [95% CI 0.40 to 1.99]; p = 0.79). There were also no differences in surgeon satisfaction (pooled OR 0.38 [95% CI 0.07 to 2.19]; p = 0.28) or among multiple patient-reported outcome measures that evaluated pain and function. Patients reported time savings, both when travel time was excluded (17 minutes shorter [95% CI 2 to 32]; p = 0.03) and when it was included (180 minutes shorter [95% CI 78 to 281]; p < 0.001).
Conclusion
Evidence from heterogeneous randomized studies demonstrates that the use of telemedicine for orthopaedic assessments does not result in identifiable differences in patient or surgeon satisfaction compared with in-person assessments. Importantly, the source studies in this review did not adequately capture or report safety endpoints, such as complications or missed diagnoses. Future studies must be adequately powered to detect these differences to ensure patient safety is not compromised with the use of telemedicine. Although telemedicine may lead to a similar patient experience, surgeons should maintain a low threshold for follow-up with in-person assessments whenever possible in the absence of further safety data.
Level of Evidence
Level I, therapeutic study.
Introduction
Telemedicine refers to the use of telecommunication technology to assess and treat patients [40]. This technology typically takes the form of video, telephone, or an interactive webpage, among other media. Much of the outcomes data on telemedicine come from other medical fields, such as internal medicine, psychiatry, and preventative health [7]. In orthopaedics, the provision of ancillary services such as physiotherapy and rehabilitation has been studied more extensively than surgeon-provided assessments [27,38]. The coronavirus disease 2019 (COVID-19) pandemic has resulted in the worldwide closure of elective medical and surgical clinics and has been followed by sustained efforts at physical distancing [33,34]. Throughout this period of global practice reconfiguration, there has been revived enthusiasm for telemedicine, leading to practice changes which have the potential to continue long-term, well-beyond the acute stages of the pandemic.
Recently, case reports and expert opinions have pointed to the potential benefits of integrating telemedicine into orthopaedic practice [19, 33]. However, the adoption of telemedicine technology in the long-term must be done with care and continual reflection on the evidence. Past adoption of technologies based on surgeon-perceived superiority or even comparative observational data has been invalidated in the face of high-quality evidence from randomized controlled trials (RCTs) [13, 14, 26, 32]. In the context of telemedicine, this could mean compromising patients’ perceptions of care, poorer overall outcomes, or, at worst, increased complications because of treatment. Unfortunately, rapidly published editorials and commentaries during the pandemic have not adequately conveyed findings of published randomized trials on this topic [19, 28, 31, 33]. One study, which systematically reviewed the evidence on telemedicine to date, did not identify any orthopaedic publications [25]. We therefore sought to better summarize what is known by systematically reviewing and quantitatively pooling randomized trial data.
We therefore performed a systematic review and meta-analysis of randomized trials, in which we asked: (1) What are the levels of patient and surgeon satisfaction with the use of telemedicine as a tool for orthopaedic care delivery? (2) Are there differences in patient-reported outcomes between telemedicine visits and in-person visits? (3) What is the difference in time commitment between telemedicine and in-person visits?
Materials and Methods
We conducted a systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [18]. This review was not pre-registered. We searched three medical databases (MEDLINE, Embase, and the Cochrane library) from inception to April 2020 using a combination of medical subject headings and keywords (see Appendix 1; Supplemental Digital Content 1, http://links.lww.com/CORR/A428). We also manually searched Google Scholar, PubMed, and bibliographies of included studies. We did not include conference proceedings or unpublished abstracts. Pairs of reviewers screened abstracts and titles for potentially relevant studies.
Inclusion and Exclusion Criteria
We included studies published in any language that studied an intervention that was considered to be telemedicine (that is, any form of remote or virtual care including, but not limited to, video, telephone, or internet-based care), had a control (comparator) group that comprised in-person assessments performed by orthopaedic surgeons (regardless of subspecialty), and were reports of Level I original evidence (that is, randomized controlled trials). Studies evaluating physiotherapy or rehabilitation interventions were excluded.
Disagreements about which studies should be included were resolved by reviewing the full text, and further disagreements were resolved by consensus between the senior authors (HC, RM).
Relevant data, including trial details, participant demographics, nature of the intervention and control, patient satisfaction outcomes, appointment length, and disease-specific outcomes were extracted from included trials using standardized data collection forms. All studies were also evaluated for the risk of bias using the Cochrane Risk of Bias assessment tool. This involved an assessment of random sequence generation, allocation concealment, blinding (of participants, personnel, and/or outcome assessors), completeness of outcome data, and selective reporting bias. For trials that resulted in multiple publications, the cumulative reported data from all publications were considered.
Primary and Secondary Study Outcomes
Our primary study outcome was patient satisfaction. We evaluated this by comparing differences in the likelihood of satisfaction between groups, with ordinal or continuous outcome measures converted into binary outcomes using previously described methodology.
Our secondary study outcomes were surgeon satisfaction (differences in the likelihood of satisfaction), patient-reported outcome measures (standardized mean differences), and appointment length (with and without travel time, in minutes).
Search Results
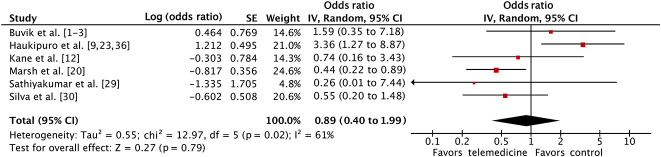
We screened 133 published articles, ultimately including 12 studies representing eight RCTs (that is, eight separate populations) in this review (Fig. 1) [1, 2, 3, 6, 9, 12, 20, 23, 29, 30, 36, 39]. There was almost-perfect agreement between reviewers for inclusion and exclusion of studies (kappa for agreement = 0.94 [95% CI 0.85 to 1.0]). There were 1008 patients randomized (511 to telemedicine groups and 497 to control groups). Subspecialties represented were hip and knee arthroplasty (two trials), upper extremity (two trials), pediatric trauma (one trial), adult trauma (one trial), and general orthopaedics (two trials).
Fig. 1.
This flowchart shows the studies that were included in and excluded from our systematic review.
Among these RCTs, seven were English-language articles and one was published in German. Five were conducted in North America and three were conducted in Europe. Six RCTs evaluated video-based interventions and two evaluated internet-based interventions. Seven studies were conventional head-to-head RCTs, and one was a randomized crossover trial. Sample sizes ranged from 23 to 402 participants. Interventions varied from completely telemedicine-based follow-up to combinations of in-person and telemedicine visits (Table 1).
Table 1.
Details of included trials
| Study | Country | Speciality (condition) | Sample size | Intervention description | Control description | Mean patient age (SD or range) | Follow-up period | Selection of reported outcome measures |
| Buvik et al. [1-3] | Norway | General orthopaedics (multiple orthopaedic conditions) | 402 | Live video-based first consult or follow-up visit conducted in a local health facility | In-person first consult or follow-up visit at an academic medical center | I: 48.0 (SD 24.0) C: 46.7 (SD 24.9) |
1 year | PROM Treatment decision Complications Satisfaction (surgeon/patient) Time Cost |
| Eberl et al. [6] | Germany | Upper extremity (elbow arthrolysis) | 23 | Live video-based postoperative follow-up visit conducted from home supplemented with interval photographs | In-person postoperative follow-up visit only | 42.6 (17 to 76) | 6 months | Outcome rating scale Assessment rating scale Costs |
| Haukipuro et al. [9, 23, 36] | Finland | General orthopaedics (multiple orthopaedic conditions) | 145 | Live video-based consultation or follow-up visit conducted in a local health facility | In-person consult or follow-up visit | I: 58.3 (SD 17.7) C: 55.1 (SD 17.3) |
1 year | Treatment decision Satisfaction (surgeon/patient) Time Cost |
| Kane et al. [12] | USA | Upper extremity (arthroscopic rotator cuff repair) | 66 | Live video-based postoperative follow-up at 2 weeks, 6 weeks, and 12 weeks | In-person postoperative follow-up at 2 weeks, 6 weeks, and 12 weeks | I: 60.6 (39 to 73) C: 59.8 (50 to 70) |
12 weeks | PROM Complications Satisfaction (surgeon/patient) Time |
| Marsh et al. [20] | Canada | Arthroplasty (THA/TKA) | 256 | Web-based (written) annual (> 12 months) postoperative follow-up | In-person annual postoperative (> 12 months) follow-up | I: 68.8 (SD 10.0) C: 66.4 (SD 11.5) |
Mean I: 5.0 (SD 3.4 C: 5.0 (SD 3.2, C) |
PROM Complications Satisfaction (patient) |
| Sathiyakumar et al. [29] | USA | Orthopaedic trauma (upper and lower extremity fractures) | 24 | Live video-based follow-up visits at 6 weeks and 6 months. In-person visits at 2 weeks and 3 months | All in-person follow-up visits | I: 36.8 (SD 14.7) C: 27.7 (SD 9.4) |
6 months | Complications Satisfaction Time |
| Silva et al. [30] | USA | Pediatrics (supracondylar distal humerus fractures) | 52 | Live video-based 4-week follow-up visit with self-cast removal. 1-week and final follow-up visits in-person | All in-person follow-up visits | I: 5.0 (2.6 to 9.4) C: 5.0 (1.9 to 10.8) |
8 weeks | PROM Satisfaction (patient) ROM Radiographic parameters Time Costs |
| Wood et al. [39] | Canada | Arthroplasty (THA/TKA) | 40 | Web-based (written) annual (> 12 months) postoperative follow-up | In-person annual postoperative (> 12 months) follow-up | Age 42.6 (17 to 72) | Mean 38 months | PROM Time Data completeness |
I = intervention; C = control; PROM = patient-reported outcome measures.
Six trials reported measures of patient satisfaction. Five reported ordinal or categorical variables and one reported continuous variables (VAS scores). Similarity between scales and conceptual measures warranted quantitative pooling. When multiple domains of satisfaction were reported, we pooled the overall satisfaction score; if this was not reported, we pooled the mean satisfaction score. Odds ratios of patients being satisfied or more than satisfied (that is, very or extremely) were calculated. For continuous measures, the standardized mean difference was calculated and converted to log-odds using previously described statistical methods [10].
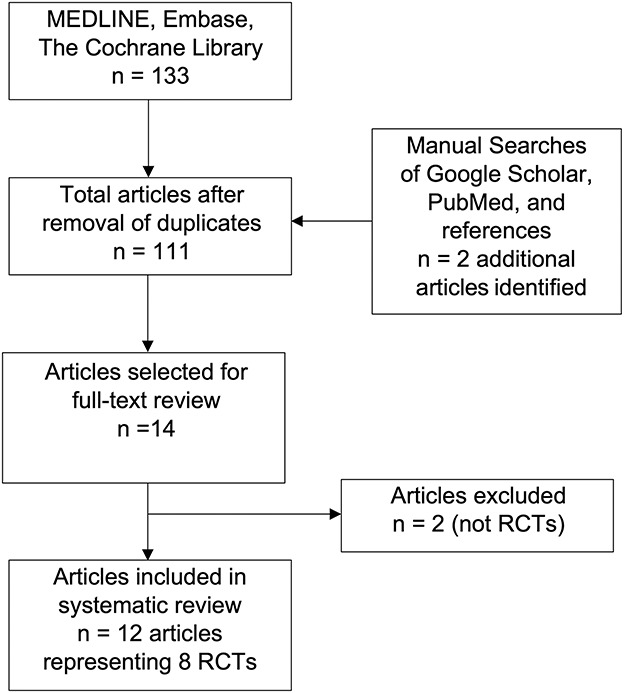
Study Methodological Quality
We assessed methodological quality of included studies using the Cochrane Risk of Bias (RoB1) tool. The assessments demonstrated that the inability to blind patients or surgeons and the lack of objective outcomes for blinded outcome assessors presented the greatest risk of bias among trials (Fig. 2). Random sequence generation, allocation concealment, and outcome reporting and follow-up were generally well-reported.
Fig. 2.
This figure summarizes the study quality of the included trials. Among the trials studied, the greatest risk of bias was due to the inability to blind patients and surgeons and the lack of objective outcomes for blinded outcome assessors.
Quantitative and Qualitative Analysis
We assessed outcomes data to determine their appropriateness for quantitative pooling (that is, a meta-analysis) or qualitative summarization. Owing to the clinically heterogeneous nature of the interventions reported in the included studies (phone, video, and internet-based), we decided a priori that we would use a random-effects model for all analyses. We reported statistical heterogeneity with the use of the I2 statistic alongside forest plots. Funnel plots were used to screen for publication bias for the main outcome; overall the plots were symmetric except for a single outlier small study [29] suggesting the possibility of small study bias. A post-hoc sensitivity analysis was undertaken to confirm that exclusion of this study did not change the results. For missing variance data, SDs were imputed using well-accepted methods [11]. In studies in which there was varied reporting of binary and continuous outcomes data, standardized mean differences were converted to natural log-odds and subsequently pooled using the generic-inverse variance method. The data analysis was performed using Review Manager Version 5.3 (Copenhagen, Denmark). Pooled means and 95% confidence intervals are reported. A p value of less than 0.05 was considered statistically significant.
Outcomes data that were deemed conceptually heterogeneous by the senior authors (HC, RM) were not pooled; this information was summarized qualitatively.
Results
Patient and Surgeon Satisfaction with Care Provided by Telemedicine
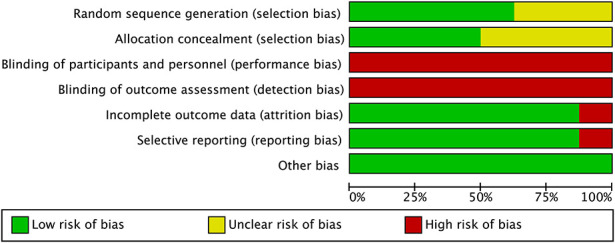
Patient Satisfaction
There was no difference in the odds of patient satisfaction between patients receiving telemedicine care and those receiving in-person care (pooled odds ratio 0.89 [95% CI 0.40 to 1.99]; p = 0.79) (Fig. 3). Overall, 92% (537 of 581) of patients were satisfied or more than satisfied (that is, very or extremely satisfied) after telemedicine visits and 93% (489 of 528) were satisfied after in-person visits. In an evaluation of only responses of “more than satisfied,” we found no between-group differences (pooled OR 0.82 [95% CI 0.41 to 1.61]; p = 0.56); 63% (366 of 581) of participants with telemedicine visits and 65% (342 of 528) of control participants were more than satisfied.
Fig. 3.
This forest plot summarizes the individual and pooled odds of satisfaction between patients receiving telemedicine care and those receiving in-person care.
Surgeon Satisfaction
There was no difference in the pooled odds of surgeon satisfaction between telemedicine and in-person visits (OR 0.38 [95% CI 0.07 to 2.19]; p = 0.28). Overall, 91% (417 of 457) of surgeon responses were rated as good or very good with the use of telemedicine compared with 94% (384 of 408) of responses with the control visits.
Patient-reported Outcomes
There were no reported differences in any measures of generic function (SF-12, EQ-5D), disease-specific function (WOMAC, Morrey Outcome Scale), or pain (VAS, Revised Faces Pain Scale) between the telemedicine and control visit groups (Table 2). The outcome measures used were heterogeneous across studies; therefore, quantitative pooling was not considered appropriate.
Table 2.
Summary of reported outcome measures
| Study | Patient-reported treatment measure | Results |
| Buvik et al. [1-3] | EQ-QoL-VAS EQ-QoL-5D |
No differences |
| Eberl et al. [6] | Morrey Outcome scale | No differences |
| Haukipuro et al. [9, 23, 36] | ||
| Kane et al. [12] | VAS Pain | No differences |
| Marsh et al. [20] | WOMAC SF-12 |
No differences |
| Sathiyakumar et al. [29] | ||
| Silva et al. [30] | Pain (Revised Faces Pain Scale) | No differences |
| Wood et al. [39] | WOMAC SF-12 |
No differences |
QoL = quality of life.
Difference in Time Commitment between Telemedicine and In-person Visits
Time commitment for appointments was shorter for telemedicine visits in comparison to in-person visits. The mean visit length for telemedicine appointments was 19 ± 8) minutes when travel time was excluded and 27 ± 24) minutes when travel time was included. The mean visit length for in-person appointments was 79 ± 85) minutes when travel time was excluded and 313 ± 126) minutes when travel time was included. Further breakdown of allocated time within each appointment was not provided in the studies. Telemedicine visit length was shorter both when travel time was excluded (17 minutes shorter [95% CI 2 to 32]; p = 0.03) and when it was included (180 minutes shorter [95% CI 78 to 281]; p < 0.001).
Discussion
There has been renewed enthusiasm for telemedicine and its possibilities, with the COVID-19 pandemic functioning as a catalyst to accelerate widespread implementation. Although there is great enthusiasm of late for this topic [19, 28, 31, 33], we have seen little summative research on it [25], and there is none in our specialty of which we are aware. In this meta-analysis, we found that there were no differences in patient satisfaction scores, surgeon satisfaction scores, or patient-reported outcome measures between telemedicine and in-person appointments; however, patient time commitment was notably shorter than in-person assessments, both with and without travel time accounted for. Importantly, safety endpoints were not well measured by the source studies, so we could not evaluate them here.
Limitations
Our review has several limitations. The selection of satisfaction as our main outcome (both patient and surgeon) has well-described issues and limitations [4]. First, the instruments used to measure satisfaction were not uniform across studies, and in general they were not validated. Further the use of satisfaction as an outcome is known to demonstrate ceiling effects [22]—whereby at a certain high threshold, the measurement instruments are no longer able to detect differences in scores. Ceiling effects could partially account for the similar scores between telemedicine and in-person assessments in our analysis. In other words, it is possible that while patients and surgeons were highly satisfied with both telemedicine and in-person assessments, there may be differences in satisfaction that were not detectable. Future research is needed to explore the various domains of satisfaction—that is, which specific elements of the telemedicine (and in-person) visit patients and surgeons find satisfactory and unsatisfactory, and how these can be improved. Finally, satisfaction scores are more likely to measure satisfaction with the process of receiving care rather than the efficacy of the care itself [4]. Therefore, these scores are not necessarily reflective of objective treatment outcomes or patient-reported outcome measures.
The second most-important limitation was that safety-related outcomes were not consistently collected or reported across the included studies. Even a few severe complications or missed diagnoses can cause sufficient harm so as to negate the positive benefits of telemedicine (as it is currently practiced). As a nascent technology, it is plausible that many elements of the physical examination cannot be sufficiently replicated even with the integration of video-based technology. This lack of safety data is an issue that patients, surgeons, and policymakers must bear in mind when considering how to successfully integrate virtual medicine into clinical practice in the long term. Determining whether there are differences in safety endpoints and how to address these potential differences must be a priority in future research in telemedicine.
Heterogeneity of interventions, populations, and outcome measurements was also a major limitation in extrapolating our findings. As with any systematic review conducting a pooled analysis, the conclusions of our analysis are ultimately limited by the quality and heterogeneity of the data measured and reported in published trials. Not all trials reported each outcome, and even when the outcomes were reported, not all were similar enough to warrant a pooled analysis. Even when outcomes were similar enough to warrant pooling, there remained residual measurement heterogeneity. With appointment length, for instance, the studies were not specific in exactly what was included in appointment length (for example, x-ray time, or nurse or trainee assessment), and this could have varied between studies.
Many of our studies were also at a high risk of bias in several domains. Blinding was particularly difficult for the intervention being evaluated. We therefore cannot be certain that the outcomes are not unduly influenced by enthusiasm for a novel intervention among providers and patients. Incomplete outcome reporting was also an issue in some of the trials. Sathiyakumar et al. [29] had the highest proportion lost to follow-up, but it was also a small study which did not weigh heavily in the pooled quantitative analysis. A sensitivity analysis from which this study was excluded in the analysis did not alter the results. Each of the remaining studies reported no more than 10% missing data and this missing data was evenly distributed between treatment and control groups. For this reason, we did not feel missing data compromised the results of this meta-analysis.
Finally, not all subspecialties of orthopaedic surgery were represented—indeed, for an exhaustive review such as ours, we had hoped for a larger number of trials to improve the external validity of our findings. Regardless, we feel that this is an important first step in identifying gaps in knowledge and facilitating further trials.
Patient and Surgeon Satisfaction with Care Provided by Telemedicine
We found no differences in satisfaction between patients treated via telemedicine and those treated in person, and no differences in satisfaction among surgeons using the two approaches; in the dataset we reviewed, satisfaction generally was high across the board. This is consistent with a systematic review assessing telemedicine use across all medical studies [25]. Based on a non-comparative qualitative analysis, the authors concluded that satisfaction among patients, as measured in different domains, was rated highly. However, that review did not identify any clinical trials or observational cohort studies in orthopaedics specifically or in any other surgical field.
Unique aspects of the orthopaedic visit differ from other specialties and demands focused study, which is why we undertook this review. Specifically, surgeons need to assess the patient’s symptom status, clinically examine the limb or joint, assess any incisions or lesions, and determine ROM (and its interval progress), among other factors. Patients often have questions for their surgeons about sequelae of the injury or treatment. Further, unspoken elements of an in-person visit may be associated with the patient’s care experience [21]. There is evidence to suggest that similar satisfaction scores between interventions—as demonstrated in our analysis—translates to a similar patient experience with the clinical interaction [8], consolidating support for the use of telemedicine in routine orthopaedic practice. Further research is required to explore the comparative differences in various domains of patient experience, specifically with validated patient-reported experience measures (PREMs), in a well-controlled (ideally) randomized manner.
Patient-reported Outcomes
Although we could not pool the results, we found no obvious differences in patient-reported outcomes between patients treated using telemedicine and those cared for in person. This finding is consistent with other similar studies of orthopaedic conditions (albeit focused on rehabilitation interventions) and other medical specialties, such as those in internal medicine and psychiatry [7]. A review of 15 studies of telerehabilitation (that is, remote technology-based rehabilitation) after orthopaedic surgery and found strong evidence to support its use after THA and TKA and moderate or weak evidence to support its use after upper-limb surgery [27]. A more focused systematic review of telerehabilitation in the setting of THA and TKA only demonstrated that there was moderate- and low-quality evidence in terms of pain and functional improvement, respectively, with telerehabilitation after TKA only, but this was not necessarily clinically important [37]. Focused trials in different orthopaedic subspecialties employing uniform patient-reported outcomes measures would facilitate meaningful meta-analyses in the future to better inform clinical practice and policy.
Difference in Time Commitment between Telemedicine and In-person Visits
Unsurprisingly, telemedicine visits took less time, a difference that was especially prominent when travel time was factored in. Time and cost savings for patients seen remotely is a benefit of telemedicine, even in the absence of requirements for physical distancing. Indeed, one of the original impetuses for telemedicine was to assess patients in remote settings [5, 15, 16, 17, 24, 35]. Our findings corroborate that reduced patient time commitment is a major advantage of telemedicine. Driving time, time off work, and appointment length can be reduced with the use of telemedicine technology. This also results in substantial cost savings for patients because of less time off work, less gas consumption or additional travel costs, and fewer lost opportunity costs [1]. The influence of time commitment for orthopaedic surgeons was not reported; whether telemedicine requires more, less, or the same time commitment from orthopaedic surgeons needs to be assessed.
Conclusion
Evidence from heterogeneous randomized studies demonstrates that the use of telemedicine for orthopaedic assessments does not result in identifiable differences in patient or surgeon satisfaction compared to in-person assessments. However, the possibility of measurement ceiling effects is high, which could have failed to discern real differences among the high satisfaction scores in both groups. Time commitment for patients was lower with the use of telemedicine than in-person appointments. Importantly, the source studies in this review did not adequately capture or report safety endpoints (such as complications or missed diagnoses). It is imperative that future comparative studies are adequately powered to detect these differences in complications to ensure patient safety is not compromised with the use of telemedicine. Although telemedicine may lead to a similar patient experience, orthopaedic surgeons should maintain a low threshold for follow-up with in-person assessments whenever possible in the absence of further safety data. Moreover, identification and study of specific elements of the telemedicine visit is needed to facilitate standardization toward high quality evidence-based implementation of telemedicine protocols.
Footnotes
Each author certifies that he, nor any member of his immediate family, has funding or commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res . 2019; 21:e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buvik A, Bugge E, Knutsen G, Smabrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016;16:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buvik A, Bugge E, Knutsen G, Smabrekke A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: A randomised controlled trial. J Telemed Telecare. 2019;25:451-459. [DOI] [PubMed] [Google Scholar]
- 4.Ring D, Leopold SS. Editorial-Measuring satisfaction: Can it be done? Clin Orthop Relat Res. 2015;473:3071-3073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Delaigue S, Bonnardot L, Steichen O, Garcia DM, Venugopal R, Saint-Sauveur JF, Wootton R. Seven years of telemedicine in Medecins Sans Frontieres demonstrate that offering direct specialist expertise in the frontline brings clinical and educational value. J Glob Health. 2018;8:020414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eberl R, Kaminski A, Reckwitz N, Muhr G, Clasbrummel B. [The tele-visit as a telemedical technique in daily clinical practice. First results for elbow joint arthrolysis] [in German]. Unfallchirurg. 2006;109:383-390. [DOI] [PubMed] [Google Scholar]
- 7.Ekeland AG, Bowes A, Flottorp S. Effectiveness of telemedicine: a systematic review of reviews. Int J Med Inform. 2010;79:736-771. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez AI, Kortlever JTP, Rijk L, Ring D, Brown LE, Reichel LM. Is there a correlation between the patient-doctor relationship questionnaire and other patient-reported experience measures? Patient Exp J. 2020;7:44-50. [Google Scholar]
- 9.Haukipuro K, Ohinmaa A, Winblad I, Linden T, Vuolio S. The feasibility of telemedicine for orthopaedic outpatient clinics--a randomized controlled trial. J Telemed Telecare. 2000;6:193-198. [DOI] [PubMed] [Google Scholar]
- 10.Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated July 2019). Available at: www.training.cochrane.org/handbook. Accessed July 29, 2020. [Google Scholar]
- 11.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kane LT, Thakar O, Jamgochian G, Lazarus MD, Abboud JA, Namdari S, Horneff JG. The role of telehealth as a platform for postoperative visits following rotator cuff repair: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2020;29:775-783. [DOI] [PubMed] [Google Scholar]
- 13.Kim YH, Park JW, Kim JS. 2017. Chitranjan S. Ranawat Award: Does computer navigation in knee arthroplasty improve functional outcomes in young patients? A randomized study. Clin Orthop Relat Res. 2017:476:6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim YH, Yoon SH, Park JW. Does robotic-assisted TKA result in better outcome scores or long-term survivorship than conventional TKA? A randomized, controlled trial. Clin Orthop Relat Res. 2020;478:266-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Latifi R, Gunn JK, Bakiu E, Boci A, Dasho E, Olldashi F, Pipero P, Stroster JA, Qesteri O, Kucani J, Sulo A, Oshafi M, Osmani KL, Dogjani A, Doarn CR, Shatri Z, Kociraj A, Merrell RC. Access to specialized care through telemedicine in limited-resource country: Initial 1,065 teleconsultations in Albania. Telemed J E Health. 2016;22:1024-1031. [DOI] [PubMed] [Google Scholar]
- 16.Latifi R, Olldashi F, Dogjani A, Dasho E, Boci A, El-Menyar A. Telemedicine for neurotrauma in Albania: Initial results from case series of 146 patients. World Neurosurg. 2018;112:e747-e753. [DOI] [PubMed] [Google Scholar]
- 17.Lese A, Sraj S. Rural orthopedics: Providing orthopedic care in rural communities. Orthopedics. 2019;42:e350-e355. [DOI] [PubMed] [Google Scholar]
- 18.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH, 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. [Published online ahead of print April 14, 2020]. DOI: 10.5435/JAAOS-D-20-00380. [DOI] [PMC free article] [PubMed]
- 20.Marsh J, Bryant D, MacDonald SJ, Naudie D, Remtulla A, McCalden R, Howard J, Bourne R, McAuley J. 2014. Are patients satisfied with a web-based followup after total joint arthroplasty? Clin Orthop Relat Res. 2014;472:1972-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Menendez ME, Chen NC, Mudgal CS, Jupiter JB, Ring D. Physician empathy as a driver of hand surgery patient satisfaction. J Hand Surg Am. 2015;40:1860-1865.e2. [DOI] [PubMed] [Google Scholar]
- 22.Nguyen C, Kortlever JT, Gonzalez AI, Ring D, Brown LE, Somogyi JR. Attempts to limit censoring in measures of patient satisfaction. J Patient Exp. [Published online ahead of print June 11, 2020]. DOI: 10.1177/2374373520930468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ohinmaa A, Vuolio S, Haukipuro K, Winblad I. A cost-minimization analysis of orthopaedic consultations using videoconferencing in comparison with conventional consulting. J Telemed Telecare. 2002;8:283-289. [DOI] [PubMed] [Google Scholar]
- 24.Olldashi F, Latifi R, Parsikia A, Boci A, Qesteri O, Dasho E, Bakiu E. Telemedicine for neurotrauma prevents unnecessary transfers: An update from a nationwide program in Albania and analysis of 590 patients. World Neurosurg. 2019;128:e340-e346. [DOI] [PubMed] [Google Scholar]
- 25.Orlando JF, Beard M, Kumar S. Systematic review of patient and caregivers' satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients' health. PLoS One. [Published online August 30, 2019]. DOI: 10.1371/journal.pone.0221848. eCollection 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Paavola M, Malmivaara A, Taimela S, Kanto K, Inkinen J, Kalske J, Sinisaari I, Savolainen V, Ranstam J, Järvinen TLN. Subacromial decompression versus diagnostic arthroscopy for shoulder impingement: randomised, placebo surgery controlled clinical trial. BMJ. 2018;362:k2860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pastora-Bernal JM, Martin-Valero R, Baron-Lopez FJ, Estebanez-Perez MJ. Evidence of benefit of telerehabitation after orthopedic surgery: a systematic review. J Med Internet Res . 2017;19:e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rao SS, Loeb AE, Amin RM, Golladay GJ, Levin AS, Thakkar SC. Establishing telemedicine in an academic total joint arthroplasty practice: Needs and opportunities highlighted by the COVID-19 pandemic. Arthroplast Today. [Published online ahead of print April 23, 2020]. DOI: 10.1016/j.artd.2020.04.014. [DOI] [PMC free article] [PubMed]
- 29.Sathiyakumar V, Apfeld JC, Obremskey WT, Thakore RV, Sethi MK. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopedic trauma population: a pilot study. J Orthop Trauma. 2015;29:e139-45. [DOI] [PubMed] [Google Scholar]
- 30.Silva M, Delfosse EM, Aceves-Martin B, Scaduto AA, Ebramzadeh E. Telehealth: a novel approach for the treatment of nondisplaced pediatric elbow fractures. J Pediatr Orthop B. 2019;28:542-48. [DOI] [PubMed] [Google Scholar]
- 31.Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the era of COVID-19: The virtual orthopaedic examination. J Bone Joint Surg Am. [Published online ahead of print June 17, 2020]. DOI: 10.2106/JBJS.20.00609. [DOI] [PMC free article] [PubMed]
- 32.Thorlund JB, Juhl CB, Roos EM, Lohmander LS. Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. BMJ. 2015;350:h2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vaccaro AR, Getz CL, Cohen BE, Cole BJ, Donnally CJ., 3rd Practice management during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28:464-470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vannabouathong C, Devji T, Ekhtiari S, Chang Y, Phillips SA, Zhu M, Chagla Z, Main C, Bhandari M. Novel coronavirus COVID-19: current evidence and evolving strategies. J Bone Joint Surg Am . 2020;102:734-744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verma S, Arora S, Kassam F, Edwards MC, Damji KF. Northern Alberta remote teleglaucoma program: clinical outcomes and patient disposition. Can J Ophthalmol 2014;49:135-40. [DOI] [PubMed] [Google Scholar]
- 36.Vuolio S, Winblad I, Ohinmaa A, Haukipuro K. Videoconferencing for orthopaedic outpatients: one-year follow-up. J Telemed Telecare. 2003;9:8-11. [DOI] [PubMed] [Google Scholar]
- 37.Wang HY, Yu GS, Li JH, Zhang SX, Lin YB. An updated meta-analysis evaluating limb management after total knee arthroplasty-what is the optimal method? J Orthop Surg Res. 2019;14:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang X, Hunter DJ, Vesentini G, Pozzobon D, Ferreira ML. Technology-assisted rehabilitation following total knee or hip replacement for people with osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord . 2019;20:506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wood G, Naudie D, MacDonald S, McCalden R, Bourne R. An electronic clinic for arthroplasty follow-up: a pilot study. Can J Surg . 2011;54:381-386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wootton R. 2001. Recent advances: Telemedicine. BMJ. 2001;323:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]