Abstract
Background
The Global Alignment and Proportion (GAP) score, based on pelvic incidence-based proportional parameters, was recently developed to predict mechanical complications after surgery for spinal deformities in adults. However, this score has not been validated in an independent external dataset.
Questions/purposes
After adult spinal deformity surgery, is a higher GAP score associated with (1) an increased risk of mechanical complications, defined as rod fractures, implant-related complications, proximal or distal junctional kyphosis or failure; (2) a higher likelihood of undergoing revision surgery to treat a mechanical complication; and (3) is a lower (more proportioned) GAP score category associated with better validated outcomes scores using the Oswestry Disability Index (ODI), Scoliosis Research Society-22 (SRS-22) and the Short Form-36 questionnaires?
Methods
A total of 272 patients who had undergone corrective surgeries for complex spinal deformities were enrolled in the Scoli-RISK-1 prospective trial. Patients were included in this secondary analysis if they fulfilled the original inclusion criteria by Yilgor et al. From the original 272 patients, 14% (39) did not satisfy the radiographic inclusion criteria, the GAP score could not be calculated in 14% (37), and 24% (64) did not have radiographic assessment at postoperative 2 years, leaving 59% (159) for analysis in this review of data from the original trial. A total of 159 patients were included in this study,with a mean age of 58 ± 14 years at the time of surgery. Most patients were female (72%, 115 of 159), the mean number of levels involved in surgery was 12 ± 4, and three-column osteotomy was performed in 76% (120 of 159) of patients. The GAP score was calculated using parameters from early postoperative radiographs (between 3 and 12 weeks) including pelvic incidence, sacral slope, lumbar lordosis, lower arc lordosis and global tilt, which were independently obtained from a computer software based on centralized patient radiographs. The GAP score was categorized as proportional (scores of 0 to 2), moderately disproportional (scores of 3 to 6), or severely disproportional (scores higher than 7 to 13). Receiver operating characteristic area under curve (AUC) was used to assess associations between GAP score and risk of mechanical complications and risk of revision surgery. An AUC of 0.5 to 0.7 was classified as “no or low associative power”, 0.7 to 0.9 as “moderate” and greater than 0.9 as “high”. We analyzed differences in validated outcome scores between the GAP categories using Wilcoxon rank sum test.
Results
At a minimum of 2 years’ follow-up, a higher GAP score was not associated with increased risks of mechanical complications (AUC = 0.60 [95% CI 0.50 to 0.70]). A higher GAP score was not associated with a higher likelihood of undergoing a revision surgery to treat a mechanical complication (AUC = 0.66 [95% 0.53 to 0.78]). However, a moderately disproportioned GAP score category was associated with better SF-36 physical component summary score (36 ± 10 versus 40 ± 11; p = 0.047), better SF-36 mental component summary score (46 ± 13 versus 51 ± 12; p = 0.01), better SRS-22 total score (3.4 ± 0.8 versus 3.7 ± 0.7, p = 0.02) and better ODI score (35 ± 21 versus 25 ± 20; p = 0.003) than severely disproportioned GAP score category.
Conclusion
Based on the findings of this external validation study, we found that alignment targets based on the GAP score alone were not associated with increased risks of mechanical complications and mechanical revisions in patients with complex adult spinal disorders. Parameters not included in the original GAP score needed to be considered to reduce the likelihood of mechanical complications.
Level of Evidence
Level III, diagnostic study.
Introduction
Adult spinal deformities can result in symptoms of back and leg pain, lower-limb neurologic deficits, and compensatory mechanisms that lead to inefficient energy expenditure [1, 4, 18, 23]. In patients who fail to respond adequately to nonoperative treatment, surgical corrections have been shown to improve their health-related quality of life outcomes [26, 27, 34]. One of the main goals of surgery is restoration of sagittal alignment, which has a direct effect on postoperative pain and functional outcomes [12]. To achieve a balanced sagittal alignment of the postoperative spine, complex surgical techniques with increased magnitude and complexity are often used, and high complication rates have been reported in this patient population [2, 5, 7, 9, 11, 24, 25, 29-31]. Failure to restore an appropriate sagittal alignment (that is, overcorrection or undercorrection) has been considered the main cause of mechanical complications and revision surgery [6, 10, 32]. Using a prospective, multicenter, international study (Scoli-RISK-1) database, we reported that implant failure was among the most frequently encountered non-neurologic adverse events (9.1% of all non-neurologic adverse events, occurring in 14.7% of patients) [8, 20]. The ability to anticipate mechanical complications accurately after surgery to treat adult spinal deformities is of great clinical importance.
Although restoring the sagittal plane’s alignment is central in surgeries for adult spinal deformity, the cutoff points of postoperative parameters to avoid poor outcomes remain controversial. The most commonly used targets are based on the Scoliosis Research Society-Schwab classification, whose regional sagittal alignment modifier cutoffs were determined by health-related quality of life measures [28]. However, although postoperative radiographic alignments fall within these targets, 31.7% of patients had implant-related complications, 52.6% of whom subsequently underwent revision surgeries [30]. Yilgor et al. [33] first proposed the Global Alignment and Proportion (GAP) score that made use of pelvic incidence-based proportional parameters to predict mechanical complications in a cohort of adult spinal deformity patients after posterior fusion of four or more levels. Although the GAP score’s ability to predict mechanical complications was high in the validation cohort in their original study, attempts to validate this score externally suffered from several methodological limitations: They did not follow the original methodology, they had a small sample size, they used patient cohorts that did not fulfil the original inclusion criteria, or they had unclear definitions of mechanical complications [3, 16]. Thus, it is not possible to draw definitive conclusions from the outcomes of these studies, and the association between the GAP score and mechanical complications in patients after surgical fusion for adult spinal deformity remains uncertain. Thus, a robust external validation study is required.
We therefore applied the strict methodology for the inclusion criteria and definitions of mechanical complications and revisions as described in the original study [33] for the GAP score and asked whether after adult spinal deformity surgery, is a higher GAP score associated with (1) an increased risk of mechanical complications, defined as rod fractures, implant-related complications, proximal or distal junctional kyphosis or failure; (2) a higher likelihood of undergoing revision surgery to treat a mechanical complication; and (3) is a higher GAP score category associated with worse validated outcomes scores using the Oswestry Disability Index (ODI), Scoliosis Research Society-22 (SRS-22) and the Short Form-36 questionnaires?
Patients and Methods
Overview
We performed a retrospective analysis of a previous prospective, multicenter study that recruited patients after fusion for adult spinal deformity with minimum of 2 years follow-up as part of the Scoli-RISK-1 trial. From this cohort, the GAP score was applied to patients who fulfilled these inclusion criteria: (1) age ≥ 18 years; (2) at least one of the following radiological parameters preoperatively: scoliosis ≥ 20°, sagittal vertical axis (SVA) ≥ 5 cm, thoracic kyphosis > 60°, pelvic tilt > 25°; (3) undergone ≥ four-vertebrae posterior instrumented fusion; and (4) minimum of 2 years follow-up. Patients were excluded from this secondary analysis if they had neuromuscular disease, active infections, trauma or tumors, if a full-length radiograph was not available at baseline, early postoperative period (between 3 and 12 weeks) or latest follow-up, or if the planned uppermost instrumented vertebra was within a previously fused segment.
There were 272 patients in the original Scoli-RISK-1 cohort. Patients with fewer than four levels of fusion (0.7%; 2 of 272), those who dropped out before the 2-year timepoint (20%; 55 of 272), those without postoperative whole-spine standing radiographs at 2 years (24%; 64 of 272), and those whose GAP score could not be calculated on 3- to 12-week radiographs because of missing data (14%; 37 of 272) were excluded, leaving 159 patients (58%) were included in the current analysis (Table 1). The baseline characteristics and radiographic parameters used to calculate the GAP score were similar between the patients who were included in this study and those who were excluded (Table 2).
Table 1.
Patient selection
| Selection criteria | Number of patients (n = 272) |
| Patients aged ≥ 18 years, % (n) | 100 (272) |
| Patients who had at least one radiographic event at baseline, % (n) | 86 (233) |
| Patients who underwent an operation of ≥ four vertebrae posterior levels, % (n) | 99 (270) |
| Patients with 2-year follow-up visit, % (n) | 80 (217) |
| Radiographic assessments at 2-year visit available, % (n) | 76 (208) |
| Patients whose GAP score could be calculated based on 6-week radiologic data, % (n) | 86 (235) |
| Patients selected for analysis, that is, met all inclusion criteria, % (n) | 58 (159) |
Table 2.
Comparison between patients included and excluded from the current analysis
| Variable | Excluded n = 113 | Included n = 159 | Total n = 272 | p value |
| Age, mean ± SD | 56 ± 17 | 58 ± 14 | 57 ± 15 | 0.40a |
| Sex, % (n) | 0.04b | |||
| Male | 40 (45) | 28 (44) | 33 (89) | |
| Female | 60 (68) | 72 (115) | 67 (183) | |
| Race, % (n) | 0.15c | |||
| White or Caucasian | 84 (95) | 75 (120) | 79 (215) | |
| East Asian | 15 (17) | 21 (33) | 18 (50) | |
| Other | 1 (1) | 4 (6) | 3 (7) | |
| Patients with previous spine surgeries, % (n) | 62 (70) | 62 (99) | 62 (169) | 0.96b |
| GAP category, % (n) | 0.07b | |||
| Proportioned | 12 (9)d | 5 (8) | 7 (17)d | |
| Moderately disproportioned | 41 (31)d | 35 (55) | 37 (86)d | |
| Severely disproportioned | 47 (36)d | 60 (96) | 56 (132)d |
t test.
Chi-square test.
Fisher's exact test.
For patients excluded from the current analysis, information sufficient to calculate the GAP score was only available in 76 patients.
The mean (range) age of the analyzed patients at the time of surgery was 58 ± 14 years (18 to 80), and the median number of levels involved in the surgery was 11 (4 to 23). Sixty-two percent (99 of 159) had previous spine surgery. The median total operative time was 405 minutes (interquartile range [IQR] 329 to 499 minutes), with a median estimated total blood loss of 2000 mL (IQR 1500 to 3000 mL). Seventy-five percent (120 of 159) of the patients underwent a three-column osteotomy.
Ethical approval was waived for the analysis and publication of a retrospective review of anonymized data obtained from an institutional review board-approved prospective clinical trial.
Participants in the Scoli-RISK-1 Study
Patients between 18 and 80 years of age were prospectively recruited into the Scoli-RISK-1 trial if they were undergoing surgery for adult spinal deformity and met any one of the following criteria: (1) a major Cobb angle of ≥ 80o in the coronal and/or sagittal planes; (2) congenital or revision spinal deformity undergoing corrective osteotomy; (3) presence of preoperative myelopathy; (4) ossification of the ligamentum flavum, or ossification of the posterior longitudinal ligament with a deformity; or (5) patients who had undergone corrective osteotomy or three-column osteotomy. The Scoli-RISK-1 trial was registered with clinicaltrials.gov under NCT01305343, but registration is not required for this secondary data analysis of the primary clinical trial.
Validation of the GAP Score Using the Scoli-RISK-1 Cohort
The following radiographic parameters were obtained by using a computerized software-based service provided by Nemaris Inc (New York, USA) using centralized patient radiographs taken between 3 and 12 weeks postoperatively: pelvic incidence, sacral slope, L1-S1 lordosis, L4-S1 lordosis, and global tilt. We calculated GAP parameters from the ideal sacral slope, lumbar lordosis, and global tilt, as described by Yilgor et al. [33]. The GAP score, which was calculated by adding the scores for relative pelvic version, relative lumbar lordosis, lordosis distribution index, relative spinopelvic alignment, and the age factor, can range from 0 to 13 points. A GAP score of 0 to 2 was considered to indicate a proportioned spinopelvic state, 3 to 6 as a moderately disproportioned state, and 7 or higher as a severely disproportioned state.
Distribution of GAP scores and Mechanical Complications
The mean (range) postoperative GAP score was 7 ± 3 (0 to 13). Five percent (8 of 159) of the patients had a proportional spinopelvic state according to the GAP score, whereas 35% (55 of 159) and 60% (96 of 159) had moderately and severely disproportioned states, respectively (Fig. 1).
Fig. 1.
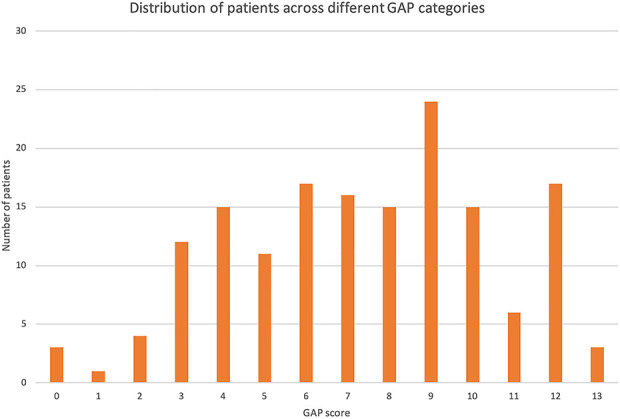
This graph shows the distribution of patients across different GAP categories.
Twenty-eight percent (44 of 159) of the patients had mechanical complications: 11% (17 of 159) had proximal junctional kyphosis, 19% (31 of 159) had other implant-related complications, and 2% (3 of 159) had distal junctional kyphosis or failure. Sixteen percent (25 of 159) of patients underwent revision surgery for mechanical complications.
Primary and Secondary Study Outcomes
Our primary study outcome was to determine the association between the GAP score and the occurrence of any mechanical complications. Postoperative radiographs between 12 weeks and final follow-up were assessed for the following mechanical complications: (1) rod fractures (single or double rods, symptomatic or incidental findings); (2) proximal junctional kyphosis, defined as ≥ 10° increase in kyphosis between the uppermost instrumented vertebra (UIV) and UIV+2 between early postoperative and follow-up radiographs; (3) proximal junctional failure, defined as fracture of UIV or UIV + 1, pullout of UIV instrumentation, or presence of sagittal subluxation; (4) distal junctional kyphosis or failure, defined as ≥ 10° increase in kyphosis between the lowermost instrumented vertebra (LIV) and LIV-1 between early postoperative and follow-up radiographs, or pullout of LIV instrumentation; and (5) implant-related complications, such as screw loosening, pullout or fracture, interbody graft, hook or set screw dislodgement; or failure because of adverse events identified independently by two authors (KYHK, KMCC). Additionally, a clinical endpoint committee evaluated all reported complications for its accuracy and re-categorized as necessary.
Our secondary study outcomes were to determine the association between the GAP score and the occurrence of mechanical revisions, and between the GAP category and validated outcome scores. Mechanical revisions were defined as any additional surgery performed to treat a mechanical complication stated above. Validated outcome scores were collected as part of the original prospective trial, which included ODI, SRS-22 and the Short Form-36 questionnaires.
Statistical Analysis
Descriptive statistics were used to present demographics and radiographic parameters. Categorical data are presented using absolute frequency and percentages; continuous data are presented as the mean with SDs for normally distributed data or median and interquartile ranges for non-normally distributed data. Using a receiver operator characteristic curve, we calculated the area under the curve (AUC) to assess the association between the GAP score and the likelihood of mechanical complications, and that of revision surgery to treat a mechanical complication. An AUC of 0.5 to 0.7 was classified as no or low associative power, 0.7 to 0.9 as moderate and > 0.9 as high. Additionally, we analyzed differences in validated outcome scores between the GAP categories using Wilcoxon rank sum test. Significance was defined as p < 0.05. All statistical analyses were performed using SAS (version 9.4, SAS Institute Inc, Cary, NC, USA).
Results
GAP Score and Risk of Mechanical Complications
Mechanical complications were found in 13% (1 of 8) patients with proportioned GAP scores, 24% (13 of 55) patients with moderately disproportioned GAP scores, and 31% (30 of 96) patients with severely disproportioned GAP scores (Fig. 2). Using receiver operating characteristic curve, we found that higher postoperative GAP scores were not associated with increased risks of mechanical complications with minimum of 2 year follow-up (AUC = 0.60 [95% CI 0.50 to 0.70]).
Fig. 2.
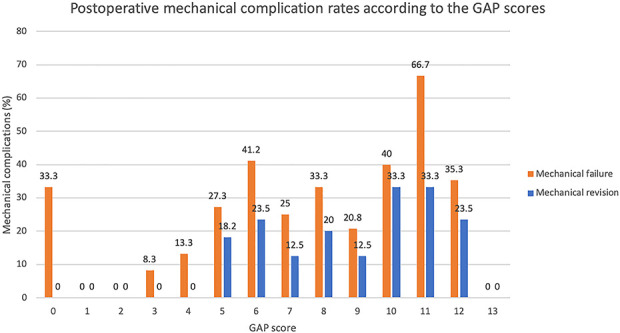
This graph shows postoperative mechanical complication rates according to GAP scores.
GAP Score and Revision Surgery
Mechanical revision surgeries were performed in 0% (0 out of 8) patients with proportioned GAP scores, 11% (6 of 55) patients were moderately disproportioned GAP scores, and 20% (19 of 96) patients with severely disproportioned GAP scores. Using receiver operating characteristic curve, we found that higher postoperative GAP scores were not associated with increased risks of mechanical revision during a minimum of 2 years’ follow-up (AUC = 0.66 [95% CI 0.53 to 0.78]).
GAP Category and Validated Outcomes Scores
In all four validated outcome measures, we found lower (better) gap score category was associated with better quality-of-life status at minimum of 2 years’ follow-up. Moderately disproportioned GAP score category was associated with a better SF-36 physical component summary score (40 ± 11 versus 36 ± 10; p = 0.047), a better SF-36 mental component summary score (46 ± 13 versus 51 ± 12; p = 0.01), a better SRS-22 total score (3.4 ± 0.8 versus 3.7 ± 0.7; p = 0.02) and a better ODI score (35 ± 21 versus 25 ± 20; p < 0.001) than severely disproportioned GAP score category (Table 3).
Table 3.
Comparison of postoperative health-related quality of life scores at 24 months by GAP categories
| Health-related quality of life measure | GAP category | p valuea | ||
| Proportioned (n = 8) | Moderately disproportioned (n = 55) | Severely disproportioned (n = 96) | ||
| SF-36 physical component summary | 44 ± 8 | 40 ± 11 | 36 ± 10 | 0.047 |
| SF-36 mental component summary | 48 ± 7 | 51 ± 12 | 46 ± 13 | 0.01 |
| SRS total score | 3.5 ± 0.5 | 3.7 ± 0.7 | 3.4 ± 0.8 | 0.02 |
| ODI | 27 ± 18 | 25 ± 20 | 35 ± 21 | 0.001 |
Comparison was made between moderately and severely disproportioned groups only; data are presented as the mean ± SD.
SF-36 = Short Form-36; SRS = Scoliosis Research Society; Oswestry Disability Index = ODI.
Discussion
The prevalence of radiographic and clinically symptomatic mechanical complications after surgery for adult spinal deformity has been reported to be 30%, and more than 50% of these patients underwent a revision surgery to treat them. Yilgor et al. [33] proposed a new pelvic incidence-based proportional method of analyzing the sagittal alignment, known as the GAP score, to predict mechanical complications in patients undergoing surgery for adult spinal deformity. Although the GAP score performs accurately on internal validation, it has not been validated externally using the same inclusion criteria and strict definitions of mechanical complications as described in the original study. We therefore applied the GAP score as additional analysis on the Scoli-RISK-1 database. We found that higher GAP scores were not associated with increased risks of mechanical complications nor revision surgeries due to mechanical complications. However, we found that moderately proportioned GAP score category was associated with better validated outcome scores than severely proportional GAP score category.
Limitations
This study had several limitations. First only 159 of the 272 patients in the Scoli-RISK-1 database could be included in the study because of the strict inclusion criteria. The Scoli-RISK-1 study was initiated to provide a complete risk profile of neurologic and non-neurologic adverse events after surgeries to treat complex adult spinal deformities, and a 6-week postoperative radiograph was not mandatory. Although our analyses showed the baseline characteristics did not differ between patients who were included in this current study and those who were not, we cannot rule out the possibility of selection bias. Second, patients included in the Scoli-RISK-1 database had more complex deformities than those described in the original GAP study [33], and the magnitude of correction was substantial. However, the GAP score should be able to predict the mechanical outcomes of patients who undergo more complex surgeries. Third, the patients were not equally distributed among each GAP score category since the original Scoli-RISK-1 study was powered to evaluate neurologic complications after surgery for complex spinal deformities only. We used as many patients as possible from the original cohort who matched the inclusion criteria to perform external validation, but there was a lower statistical power than might be expected in a planned validation study. The statistical analysis was based on only eight patients in the GAP proportioned group with a broad confidence interval of mechanical revision; it is possible that the statistical significance may have varied if more patients from the original cohort could have been included. In addition, the health-related quality of life scores could not be reliably compared for the GAP proportioned group. However, the GAP score was developed to evaluate mechanical complications only, and outcome scores only indirectly reflected the consequences of sagittally-malaligned spines.
GAP Score and Risk of Mechanical Complications
We found no association between the postoperative GAP score and mechanical failures two years after surgery. The original study that described the GAP score showed that it was highly predictive of mechanical complications in its validation cohort, with an AUC of 0.92 [33]. However, the external validity of the GAP score has not been established. Bari et al. [3] studied 149 patients and did not find any association between the GAP score and mechanical failure. However, the patient population in that study was not matched to the population originally described in terms of patient characteristics and the number of levels fused. Although Bari et al. [3] argued that the GAP score described a general spinopelvic state that should apply to all lumbosacral surgeries, their study methodology did not follow the strict criteria of an external validation study, therefore rendering their interpretation based on these results is inconclusive. Jacobs et al. [16] studied 39 patients from two centers and compared the predictive value of the GAP score and that of Schwab sagittal modifiers for mechanical complications. Both classification systems could predict radiographic mechanical complications, but the GAP score was superior (p = 0.03). However, only a small number of patients were included, and one of the original Schwab classification parameters was not available for analysis.
Although our present study was not designed and powered to validate the GAP score, we included a large number of patients and followed the strict inclusion criteria and definitions of mechanical complications. The narrow focus on sagittal alignment does not consider other non-mechanical risk factors, including neurologic disorders [13], visual impairment, and vestibular dysfunction, which may impact balance. Moreover, a mathematical approach using formulae is not necessarily predictive in large cohorts because of heterogeneity in patient factors, surgical variations, and postoperative regimens. Inoue et al. [15] found that three or more medical comorbidities and smoking were major risk factors for mechanical failure. Recently, a study found that the multifidus and erector muscles play a role in the maintenance of spinopelvic alignment [17], and a lower thoracolumbar muscle volume was associated with the development of proximal junctional kyphosis in one series [19]. The lack of association between the postoperative GAP score and mechanical complications demonstrated by our study suggests factors other than radiologic parameters are important in the occurrence of mechanical complications after surgeries for adult spinal deformity.
GAP Score and Revision Surgery
Likewise, we found no association between the postoperative GAP score and mechanical revision. In the validation cohort of the original description of the GAP score, Yilgor et al. [33] found that the mechanical revision rates were 3%, 21%, and 55% for the proportioned, moderately disproportioned, and severely disproportioned groups, respectively. The Cochran-Armitage test also showed a significant linear trend, with higher GAP scores being associated with higher rates of mechanical revisions (chi-square [1] = 19.4; p < 0.001). However, mechanical revisions may be due to a wide variety of reasons apart from alignment issues. Maier et al. [22] found that in 335 patients with adult spinal deformity, revision rates varied across eight different sites (range 6.3% to 31.9%; p = 0.001). They also reported that choosing a more caudal level of three-column osteotomy had a greater tendency to lead to revisions. Another study found higher revision rates were associated with the etiology of adult spinal deformity (degenerative and congenital) and the types of implant construct (hybrid constructs) [35]. A further possible factor that we were unable to differentiate from our current study is the contribution of previous spinal surgery. It is highly conceivable that violation of the posterior lumbar musculature and previous spinal reconstructions can contribute to higher revision rates. Hu and Lieberman [14] found that adult spinal deformity patients who had three or more previous operations had higher reoperation rates than those who only had one (22% versus 8%; p = 0.07). Mechanical revisions, therefore, may result from factors other than spinopelvic alignment alone.
GAP Score and Validated Outcome Scores
We found some associations between lower (better) GAP score category and better patient-reported outcomes scores; this is not surprising as the GAP score describes a spinopelvic state according to the sagittal physiological alignment of the normal spine that is most efficient for muscular forces to function [21]. Patients in the study described by Yilgor et al. [33] also found better health-related quality of life measures for patients with lower GAP score categories. However, the original purpose of the GAP score was to predict the occurrence of mechanical complications, and its association with outcome scores was not the primary intent. Nonetheless, this highlights the importance of sagittal balance in the treatment of adult spinal deformity [12].
Conclusions
Our external validation study using a prospective, multicenter database of patients with complex adult spinal deformities did not find any association between the GAP score and mechanical complications nor mechanical revisions. There is insufficient evidence to apply the GAP score in the surgical planning of adult spinal deformity in routine clinical practice currently. Future directions should include prospective trials powered specifically to study the predictive value of GAP score, strict patient inclusion criteria, and prospective documentation of all symptomatic and asymptomatic radiographic mechanical complications. This will improve our understanding of the multiple factors, including the different components of the GAP score, that give rise to mechanical complications in adult spinal deformity surgeries.
Acknowledgments
We thank the surgeons, collaborating centers’ clinical research personnel, and support staff for their active participation in the Scoli-RISK-1 study. We thank Christian Knoll Diplom FH, for statistical assistance.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Funding received to conduct Scoli-RISK-1 was from the Scoliosis Research Society and AO Foundation, AO Spine. The study was managed by AO Foundation and AO Spine through the AO Spine Knowledge Forum Deformity. Study support was provided directly through AO Spine's Research department and AO's Clinical Investigation and Documentation unit.
Each author certifies that neither he nor she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Department of Orthopaedics and Traumatology, Li Ka Shing Faculty of Medicine, The University of Hong Kong.
References
- 1.Ames CP, Scheer JK, Lafage V, Smith JS, Bess S, Berven SH, Mundis GM, Sethi RK, Deinlein DA, Coe JD, Hey LA, Daubs MD. Adult Spinal Deformity: Epidemiology, health impact, evaluation, and management. Spine Deform. 2016;4:310-322. [DOI] [PubMed] [Google Scholar]
- 2.Auerbach JD, Lenke LG, Bridwell KH, Sehn JK, Milby AH, Bumpass D, Crawford CH, 3rd, O'Shaughnessy BA, Buchowski JM, Chang MS, Zebala LP, Sides BA. Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976). 2012;37:1198-1210. [DOI] [PubMed] [Google Scholar]
- 3.Bari TJ, Ohrt-Nissen S, Hansen LV, Dahl B, Gehrchen M. Ability of the Global Alignment and Proportion score to predict mechanical failure following adult spinal deformity surgery-validation in 149 patients with two-year follow-up. Spine Deform. 2019;7:331-337. [DOI] [PubMed] [Google Scholar]
- 4.Bess S, Line B, Fu KM, McCarthy I, Lafage V, Schwab F, Shaffrey C, Ames C, Akbarnia B, Jo H, Kelly M, Burton D, Hart R, Klineberg E, Kebaish K, Hostin R, Mundis G, Mummaneni P, Smith JS, International Spine Study Group. The health impact of symptomatic adult spinal deformity: comparison of deformity types to United States population norms and chronic diseases. Spine (Phila Pa 1976). 2016;41:224-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhagat S, Vozar V, Lutchman L, Crawford RJ, Rai AS. Morbidity and mortality in adult spinal deformity surgery: Norwich Spinal Unit experience. Eur Spine J. 2013;22 Suppl 1:S42-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bridwell KH, Baldus C, Berven S, Edwards C, 2nd, Glassman S, Hamill C, Horton W, Lenke LG, Ondra S, Schwab F, Shaffrey C, Wootten D. Changes in radiographic and clinical outcomes with primary treatment adult spinal deformity surgeries from two years to three- to five-years follow-up. Spine (Phila Pa 1976). 2010;35:1849-1854. [DOI] [PubMed] [Google Scholar]
- 7.Buchowski JM, Bridwell KH, Lenke LG, Kuhns CA, Lehman RA, Jr., Kim YJ, Stewart D, Baldus C. Neurologic complications of lumbar pedicle subtraction osteotomy: a 10-year assessment. Spine (Phila Pa 1976). 2007;32:2245-2252. [DOI] [PubMed] [Google Scholar]
- 8.Cerpa M, Lenke LG, Fehlings MG, Shaffrey CI, Cheung KMC, Carreon LY. Evolution and advancement of adult spinal deformity research and clinical care: an overview of the Scoli-RISK-1 study. Global Spine J. 2019;9:8S-14S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Charosky S, Guigui P, Blamoutier A, Roussouly P, Chopin D, Study Group on Scoliosis. Complications and risk factors of primary adult scoliosis surgery: a multicenter study of 306 patients. Spine (Phila Pa 1976). 2012;37:693-700. [DOI] [PubMed] [Google Scholar]
- 10.Cho KJ, Suk SI, Park SR, Kim JH, Kang SB, Kim HS, Oh SJ. Risk factors of sagittal decompensation after long posterior instrumentation and fusion for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2010;35:1595-1601. [DOI] [PubMed] [Google Scholar]
- 11.Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Choi WK, Lee KY, Lee SR. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2007;32:2232-2237. [DOI] [PubMed] [Google Scholar]
- 12.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30:2024-2029. [DOI] [PubMed] [Google Scholar]
- 13.Glassman SD, Coseo MP, Carreon LY. Sagittal balance is more than just alignment: why PJK remains an unresolved problem. Scoliosis Spinal Disord. 2016;11:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hu X, Lieberman IH. Revision adult spinal deformity surgery: Does the number of previous operations have a negative impact on outcome? Eur Spine J. 2019;28:155-160. [DOI] [PubMed] [Google Scholar]
- 15.Inoue S, Khashan M, Fujimori T, Berven SH. Analysis of mechanical failure associated with reoperation in spinal fusion to the sacrum in adult spinal deformity. J Orthop Sci. 2015;20:609-616. [DOI] [PubMed] [Google Scholar]
- 16.Jacobs E, van Royen BJ, van Kuijk SMJ, Merk JMR, Stadhouder A, van Rhijn LW, Willems PC. Prediction of mechanical complications in adult spinal deformity surgery-the GAP score versus the Schwab classification. Spine J. 2019;19:781-788. [DOI] [PubMed] [Google Scholar]
- 17.Katsu M, Ohba T, Ebata S, Oba H, Koyama K, Haro H. Potential role of paraspinal musculature in the maintenance of spinopelvic alignment in patients with adult spinal deformities. Clin Spine Surg . 2020;33:E76-E80. [DOI] [PubMed] [Google Scholar]
- 18.Kelly MP, Kim HJ, Ames CP, Burton DC, Carreon LY, Polly DW, Jr., Hostin R, Jain A, Gum JL, Lafage V, Schwab FJ, Shaffrey CI, Smith JS, Bess S, International Spine Study Group. Minimum detectable measurement difference for health-related quality of life measures varies with age and disability in adult spinal deformity: implications for calculating minimal clinically important difference. Spine (Phila Pa 1976). 2018;43:E790-E795. [DOI] [PubMed] [Google Scholar]
- 19.Kim DK, Kim JY, Kim DY, Rhim SC, Yoon SH. Risk factors of proximal junctional kyphosis after multilevel fusion surgery: more than 2 Years follow-up data. J Korean Neurosurg Soc. 2017;60:174-180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kwan KYH, Bow C, Samartzis D, Lenke LG, Shaffrey CI, Carreon LY, Dahl BT, Fehlings MG, Ames CP, Boachie-Adjei O, Dekutoski MB, Kebaish KM, Lewis SJ, Matsuyama Y, Mehdian H, Pellise F, Qiu Y, Schwab FJ, Cheung KMC. Non-neurologic adverse events after complex adult spinal deformity surgery: results from the prospective, multicenter Scoli-RISK-1 study. Eur Spine J. 2019;28:170-179. [DOI] [PubMed] [Google Scholar]
- 21.Le Huec JC, Thompson W, Mohsinaly Y, Barrey C, Faundez A. Sagittal balance of the spine. Eur Spine J. 2019;28:1889-1905. [DOI] [PubMed] [Google Scholar]
- 22.Maier SP, Smith JS, Schwab FJ, Obeid I, Mundis GM, Klineberg E, Hostin R, Hart RA, Burton D, Boachie-Adjei O, Gupta M, Ames C, Protopsaltis TS, Lafage V, International Spine Study Group. Revision surgery after 3-column osteotomy in 335 patients with adult spinal deformity: intercenter variability and risk factors. Spine (Phila Pa 1976). 2014;39:881-885. [DOI] [PubMed] [Google Scholar]
- 23.Pellise F, Vila-Casademunt A, Ferrer M, Domingo-Sabat M, Bago J, Perez-Grueso FJ, Alanay A, Mannion AF, Acaroglu E, European Spine Study Group. Impact on health related quality of life of adult spinal deformity (ASD) compared with other chronic conditions. Eur Spine J. 2015;24:3-11. [DOI] [PubMed] [Google Scholar]
- 24.Pull ter Gunne AF, van Laarhoven CJ, Cohen DB. Incidence of surgical site infection following adult spinal deformity surgery: an analysis of patient risk. Eur Spine J. 2010;19:982-988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rampersaud YR, Moro ER, Neary MA, White K, Lewis SJ, Massicotte EM, Fehlings MG. Intraoperative adverse events and related postoperative complications in spine surgery: implications for enhancing patient safety founded on evidence-based protocols. Spine (Phila Pa 1976). 2006;31:1503-1510. [DOI] [PubMed] [Google Scholar]
- 26.Reid DBC, Daniels AH, Ailon T, Miller E, Sciubba DM, Smith JS, Shaffrey CI, Schwab F, Burton D, Hart RA, Hostin R, Line B, Bess S, Ames CP, International Spine Study Group. Frailty and health-related quality of life improvement following adult spinal deformity surgery. World Neurosurg. 2018;112:e548-e554. [DOI] [PubMed] [Google Scholar]
- 27.Riley MS, Bridwell KH, Lenke LG, Dalton J, Kelly MP. Health-related quality of life outcomes in complex adult spinal deformity surgery. J Neurosurg Spine. 2018;28:194-200. [DOI] [PubMed] [Google Scholar]
- 28.Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976). 2012;37:1077-1082. [DOI] [PubMed] [Google Scholar]
- 29.Sciubba DM, Yurter A, Smith JS, Kelly MP, Scheer JK, Goodwin CR, Lafage V, Hart RA, Bess S, Kebaish K, Schwab F, Shaffrey CI, Ames CP, International Spine Study Group. A comprehensive review of complication rates after surgery for adult deformity: a reference for informed consent. Spine Deform. 2015;3:575-594. [DOI] [PubMed] [Google Scholar]
- 30.Soroceanu A, Diebo BG, Burton D, Smith JS, Deviren V, Shaffrey C, Kim HJ, Mundis G, Ames C, Errico T, Bess S, Hostin R, Hart R, Schwab F, Lafage V, International Spine Study Group. Radiographical and implant-related complications in adult spinal deformity surgery: incidence, patient risk factors, and impact on health-related quality of life. Spine (Phila Pa 1976). 2015;40:1414-1421. [DOI] [PubMed] [Google Scholar]
- 31.Weistroffer JK, Perra JH, Lonstein JE, Schwender JD, Garvey TA, Transfeldt EE, Ogilvie JW, Denis F, Winter RB, Wroblewski JM. Complications in long fusions to the sacrum for adult scoliosis: minimum five-year analysis of fifty patients. Spine (Phila Pa 1976). 2008;33:1478-1483. [DOI] [PubMed] [Google Scholar]
- 32.Yagi M, Rahm M, Gaines R, Maziad A, Ross T, Kim HJ, Kebaish K, Boachie-Adjei O, Complex Spine Study Group. Characterization and surgical outcomes of proximal junctional failure in surgically treated patients with adult spinal deformity. Spine (Phila Pa 1976). 2014;39:E607-614. [DOI] [PubMed] [Google Scholar]
- 33.Yilgor C, Sogunmez N, Boissiere L, Yavuz Y, Obeid I, Kleinstuck F, Perez-Grueso FJS, Acaroglu E, Haddad S, Mannion AF, Pellise F, Alanay A, European Spine Study Group. Global Alignment and Proportion (GAP) score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am. 2017;99:1661-1672. [DOI] [PubMed] [Google Scholar]
- 34.Yoshida G, Boissiere L, Larrieu D, Bourghli A, Vital JM, Gille O, Pointillart V, Challier V, Mariey R, Pellise F, Vila-Casademunt A, Perez-Grueso FJ, Alanay A, Acaroglu E, Kleinstuck F, Obeid I, European Spine Study Group. Advantages and disadvantages of adult spinal deformity surgery and its impact on health-related quality of life. Spine (Phila Pa 1976). 2017;42:411-419. [DOI] [PubMed] [Google Scholar]
- 35.Zhu F, Bao H, Liu Z, Bentley M, Zhu Z, Ding Y, Qiu Y. Unanticipated revision surgery in adult spinal deformity: an experience with 815 cases at one institution. Spine (Phila Pa 1976). 2014;39:B36-44. [DOI] [PubMed] [Google Scholar]


