Abstract
Background
Most conditions in orthopaedic surgery are preference-sensitive, where treatment choices are based on the patient’s values and preferences. One set of tools increasingly used to help align treatment choices with patient preferences are question prompt lists (QPLs), which are comprehensive lists of potential questions that patients can ask their physicians during their encounters. Whether or not a comprehensive orthopaedic-specific question prompt list would increase patient-perceived involvement in care more effectively than might three generic questions (the AskShareKnow questions) remains unknown; learning the answer would be useful, since a three-question list is easier to use compared with the much lengthier QPLs.
Question/purpose
Does an orthopaedic-specific question prompt list increase patient-perceived involvement in care compared with the three generic AskShareKnow questions?
Methods
We performed a pragmatic randomized controlled trial of all new patients visiting a multispecialty orthopaedic clinic. A pragmatic design was used to mimic normal clinical care that compared two clinically acceptable interventions. New patients with common orthopaedic conditions were enrolled between August 2019 and November 2019 and were randomized to receive either the intervention QPL handout (orthopaedic-specific QPL with 45 total questions, developed with similar content and length to prior QPLs used in hand surgery, oncology, and palliative care) or a control handout (the AskShareKnow model questions, which are: “What are my options? What are the benefits and harms of those options? How likely are each of those benefits and harms to happen to me?”) before their visits. A total of 156 patients were enrolled, with 78 in each group. There were no demographic differences between the study and control groups in terms of key variables. After the visit, patients completed the Perceived Involvement in Care Scale (PICS), a validated instrument designed to evaluate patient-perceived involvement in their care, which served as the primary outcome measure. This instrument is scored from 0 to 13, with higher scores indicating higher perceived involvement.
Results
There was no difference in mean PICS scores between the intervention and control groups (QPL 8.3 ± 2.3, control 8.5 ± 2.3, mean difference 0.2 [95% CI -0.53 to 0.93 ]; p = 0.71.
Conclusion
In patients undergoing orthopaedic surgery, a QPL does not increase patient-perceived involvement in care compared with providing patients the three AskShareKnow questions. Implementation of the three AskShareKnow questions can be a more efficient way to improve patient-perceived involvement in their care compared with a lengthy QPL.
Level of Evidence
Level II, therapeutic study.
Introduction
Most orthopaedic conditions have multiple treatment options that involve various tradeoffs, including risks, benefits, and costs. These conditions can be classified as “preference-sensitive conditions,” indicating that a discussion of these tradeoffs and the patient’s goals and preferences can inform an individual patient’s treatment method [5]. For example, patients with knee or hip arthritis must weigh the potential risks and benefits of trying to adapt to their conditions against those of steroid injection, therapy, or surgery. For preference-sensitive conditions, it is critical to ensure that the patient’s preferences are heard during the decision-making process to influence the treatment plan [9, 29].
Models such as shared decision making (SDM) are useful in engaging the patient as a key stakeholder while formulating the treatment plan. SDM is a model of collaboration where physicians and patients work together to determine which treatment is most consistent with the patient’s values and preferences through the bidirectional transfer of information between patient and physician [4]. Health decisions centered on patient preferences have higher decision quality, reduced costs, and are linked to improved health outcomes [18, 36]. Educational tools like decision aids are the focus of many SDM interventions and demonstrate positive outcomes, such as increasing patient knowledge, decreasing patient decisional conflict, and improving adherence to the treatment plan as well as improving physical function [39]. However, owing to the time and resources to develop and implement point-of-care educational tools, the adoption of SDM aids is not widespread [1, 8, 16, 27]. There may be other approaches to improve SDM that could more easily integrate into clinic workflows.
One potential SDM tool is the question prompt list (QPL). A QPL is a bank of possible questions that patients can use during their visit with a physician that covers a variety of topics, ranging from diagnosis, treatment, and outcomes to financial support, emotional support, and medications [7, 10, 13, 42, 43]. Prior studies have used several methods to develop QPLs, with most using a physician panel and some including patient feedback in addition to the physician panel. QPLs facilitate the conversation between patients and their physicians; they increase the number of questions asked by patients, increase information provided by physicians, reduce patient anxiety, improve patient recall, and increase patient satisfaction with their consultation [6, 20, 22, 32, 44]. QPLs have been shown to be successful in other fields but have yet to be explored in orthopaedic surgery. Given these demonstrated benefits, we sought to evaluate tools that could improve patient-perceived involvement in their care within an orthopaedic surgery population. Because QPLs are a comprehensive list of questions, often having more than 30 questions, we chose to evaluate the comparative effectiveness of a QPL against a three-question handout that has also been studied before [37, 38]. This pragmatic design was chosen to mimic normal clinical care that compares two clinically acceptable interventions; we felt that determining whether a three-question list is easier to use than the much lengthier QPLs would be important, since the latter would be more efficient in practice and easier for patients to use.
In this study, we therefore asked: Does an orthopaedic-specific question prompt list increase patient-perceived involvement in care compared with the three generic AskShareKnow questions?
Methods
Study Design and Setting
We conducted a pragmatic, randomized controlled trial (RCT) at the outpatient orthopaedic surgery clinic of a tertiary academic medical center. A pragmatically designed RCT is conducted with the goals of resembling clinical care in the conduct of the study and comparing two clinically acceptable interventions to provide results that are applicable to multiple settings (comparative effectiveness) rather than a highly controlled setting/comparator that lacks generalizability (exploratory trial focused on efficacy) [12, 28]. Pragmatic trials therefore do not include blinding or sophisticated study designs, and they attempt to mimic routine clinical care. As such, a comparison of two tools used and studied in medicine today (QPL and three generic questions) provides results that can more readily inform care. This study was approved by our institutional review board and was conducted from August 2019 to November 2019. This study was registered on clinicaltrials.gov (NCT03912168).
Participants
New patients visiting an outpatient orthopaedic surgery clinic who were older than 18 years of age, fluent and literate in English, and able to make informed consent were eligible for the study.
Study Patients and Randomization
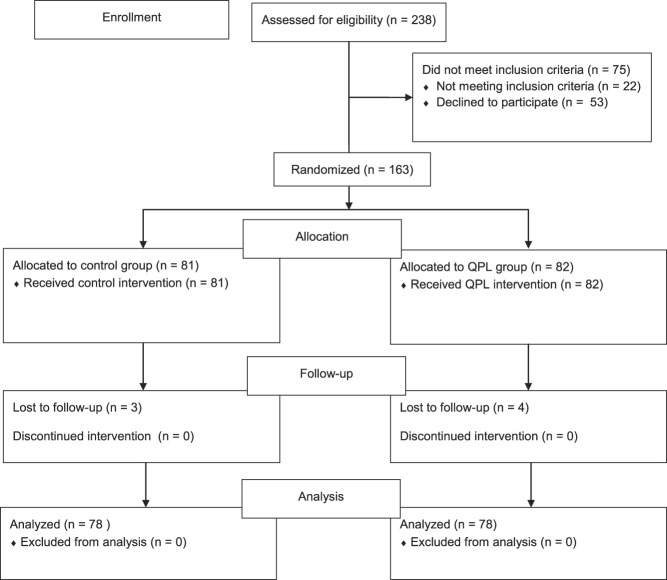
We followed the Consolidated Standards of Reporting Trials (CONSORT) criteria when designing our RCT [34]. We screened 238 patients for inclusion in this study. We deemed 22 patients ineligible for participation: 18 patients due to lack of English fluency or literacy and four patients who were younger than 18 years of age. Fifty-three patients declined to participate. The remaining 163 patients were randomized using a 1:1 allocation (Fig. 1). Three patients were lost to follow-up in the control group, and four in the intervention group. This left 78 participants in the QPL group, and 78 in the control group, for a total of 156 patients for analysis.
Fig. 1.
Flowchart of study enrollment and allocation; QPL = question prompt list.
The QPL group had a mean age of 55.2 ± 19.7 years and was 54% (42 of 78) women and the three-question group had a mean age of 54.6 ± 16.1 years and was 59% (46 of 78) women. Fifty-six percent (88 of 156) of respondents were women. There were no demographic differences between the QPL group and the control group (Table 1).
Table 1.
Demographics
| Parameter | Question prompt list group (n = 78) | Three-question group (n = 78) | p value |
| Age in years | 55 ± 20 | 55 ± 16 | 0.84 |
| Women | 54% (42) | 59% (46) | 0.62 |
| Education | 0.12 | ||
| High school graduate | 19% (15) | 33% (26) | |
| Bachelor’s degree | 37% (29) | 32% (25) | |
| Master’s/other graduate degree | 21% (16) | 15% (12) | |
| Doctorate | 13% (10) | 14% (11) | |
| Trade school | 9% (7) | 3% (2) | |
| Some high school | 1% (1) | 3% (2) | |
| No answer | 0% (0) | 0% (0) | |
| Marital status | 0.61 | ||
| Married | 58% (46) | 46% (37) | |
| Domestic partnership | 5% (4) | 8% (6) | |
| Single, never married | 21% (17) | 21% (17) | |
| Single, divorced/separated | 8% (6) | 15% (12) | |
| Single, widowed | 5% (4) | 6% (5) | |
| No answer | 1% (1) | 1% (1) | |
| Racea | 0.77 | ||
| White/Caucasian | 52 | 49 | |
| Black | 3 | 1 | |
| Hispanic | 7 | 11 | |
| Asian | 12 | 8 | |
| Hawaiian/Pacific | 0 | 0 | |
| Other | 1 | 1 | |
| No answer | 1 | 1 | |
| Employment status | 0.02 | ||
| Full-time employee | 31% (24) | 42% (33) | |
| Part-time employee | 8% (6) | 14% (11) | |
| Retired | 36% (28) | 23% (18) | |
| No work outside the home | 0% (0) | 1% (1) | |
| Disabled | 9% (7) | 15% (12) | |
| Unemployed | 6% (5) | 3% (2) | |
| Student | 10% (8) | 1% (1) | |
| No answer | 0% (0) | 0% (0) | |
| Annual salary in USD | 0.08 | ||
| < 50,000 | 20% (15) | 24% (19) | |
| 50,000-100,000 | 27% (20) | 16% (13) | |
| 100,000-150,000 | 19% (14) | 22% (17) | |
| 150,000-200,000 | 12% (9) | 9% (7) | |
| 200,000-250,000 | 5% (4) | 5% (4) | |
| 250,000+ | 17% (3) | 20% (16) | |
| No answer | 3% (3) | 3% (3) | |
| Insurance typea | 0.93 | ||
| Medicaid | 7 | 5 | |
| Medicare | 29 | 30 | |
| Private | 43 | 44 | |
| No health insurance | 0 | 0 | |
| Other | 13 | 15 | |
| No answer | 0 | 0 | |
| Patient specialty | 0.95 | ||
| Sports | 18% (14) | 22% (17) | |
| Spine | 12% (9) | 12% (9) | |
| Joint | 30% (24) | 28% (22) | |
| Foot/ankle | 19% (15) | 16% (13) | |
| Trauma | 9% (7) | 9% (7) | |
| Hand | 12% (9) | 13% (10) |
Data are presented as mean ± SD or % (n). p values were calculated by Fisher exact tests for categorical variables, and a two-sample t test for our continuous variable (age).
Percentages are not shown, as people could select multiple options and percentages would not equal 100%. Data are presented as n.
Patients were randomized via block randomizer by a member of the research team (DJM, AL, SLE) into the intervention or active control group, and patients received the corresponding handout as well as an information sheet about the study before their encounter with their surgeon [35]. Patients in each group then had a standard office visit with their orthopaedic surgeon. The surgeon was not informed of which handout the patient had received, but the handout was in the room at the time of the visit. Written consent was obtained from all patients.
Intervention
We evaluated a list of questions from previously developed and studied QPLs in palliative care, oncology, and hand surgery [10, 11, 13, 22, 32, 33, 43, 44]. Questions that could be applied to orthopaedic surgery were extracted, and additional questions that could be applicable to orthopaedic surgery were added. These were reviewed by all members of the research team to ensure face validity (six orthopaedic surgeons [MJG, SH, MS, LC, DFA, RNK] from six subspecialties [trauma, spine, sports, foot and ankle, total joint, and hand]). All surgeons determined the questions posed in the QPL were acceptable to ask in the course of routine clinical care for orthopaedic conditions. A patient advisory panel comprised of patients who had undergone orthopaedic surgery also reviewed the QPL for missing questions, unnecessary questions, or questions that were difficult to understand. This feedback was incorporated into a final version of the QPL that contained a bank of 45 questions patients can choose to ask, grouped into the following categories: diagnosis, treatment, outcomes, and support (Supplemental Digital Content 1, http://links.lww.com/CORR/A481). The QPL was written at a fifth grade reading level [40]. The intervention group received this QPL.
We compared the QPL with an active control group who received a handout containing the three ASK questions from the AskShareKnow (ASK) model. The ASK model was created to prompt patients to ask questions that provide information to make an informed choice [38]. Use of these three questions has been shown to increase information given to participants, to increase consideration of patient preferences, and to increase observed patient involvement in family practice consultations in prior studies [37, 38]. We selected this question model for its simplicity and generalizability as a comparator since it would have the added benefit in implementation efficiency (only three questions) if found to have similar effectiveness compared with a more comprehensive list. The three-question ASK handout has previously been tested in a variety of fields, including family practice, obstetrics, secondary care, and hospital settings [3, 15, 23, 37].
The three-question ASK handout was written at a fifth grade reading level and included the following questions: (1) What are my options? (2) What are the possible benefits and harms of those options? (3) How likely are each of those benefits and harms to happen to me?
Outcome Measures
After the conclusion of the consultation, patients completed a demographics survey (age, gender, marital status, race, education, employment status, household income, and insurance type) and the Perceived Involvement in Care Scale (PICS). The PICS is a 13-item validated yes-or-no questionnaire, measuring the constructs of three subscales: perceived clinician facilitation of patient involvement (subscale A, five questions), perceived level of information exchange between patient and provider (subscale B, four questions), and perceived level of the patient’s own involvement in medical decision making (subscale C, four questions). It is scored from 0 to 13, with higher scores indicating greater patient perceived involvement in care [21].
Statistical Analysis
We conducted an a priori power analysis for the purpose of our study that was based on a prior SDM study conducted in orthopaedic surgery which found a difference of 1.5 on the PICS scale that was deemed clinically important [26]. We elected to use a difference of 1 to ensure a large, diverse sample size for this study. With a difference of 1 point in PICS score and an SD of 2.15, we found that a sample size in each group of 74 yielded a power of 80% with an alpha error of 5%. This led to an overall sample size of 148 patients. We conducted an intention-to-treat analysis; however, all patients were treated as they were assigned. We calculated descriptive statistics for patient demographics. The mean PICS scores and subscale scores between the two groups were compared with a two-sample Student t-test. Analyses were done using R software (R Core Team, Vienna, Austria) [31].
Results
Formal QPL versus Generic Three-question Tool
There was no difference in mean PICS scores between the two groups (QPL 8.32 ± 2.32, control 8.46 ± 2.29; p = 0.71). Although the three-question handout resulted in a higher score on subscale A (perceived clinician facilitation of patient involvement) than did the QPL, the difference was very small and unlikely to be clinically important (QPL 3.4 ± 0.79, control 4.22 ± 1.16; difference 0.82 [95% CI 0.51 to 1.13]; p < 0.001). There were no differences for subscales B and C of PICS (Table 2).
Table 2.
Comparison of PICS scores between the QPL and three-question group
| Questionnaire | QPL – intervention group | Three questions – active control group | p value |
| PICS | 8.3 ± 2.3 | 8.5 ± 2.3 | 0.71 |
| PICS subscale A | 3.4 ± 0.7 | 4.2 ± 1.2 | < 0.001 |
| PICS subscale B | 3.1 ± 1.2 | 3.2 ± 1.2 | 0.19 |
| PICS subscale C | 1.1 ± 1.1 | 1.1 ± 1.0 | 0.24 |
All data presented as mean ± SD; QPL = question prompt list; PICS = Perceived Involvement in Care Scale.
Discussion
There is an increasing emphasis on implementing tools to improve patient involvement in the decision-making process in orthopaedic surgery. Two tools that are commonly used in other fields of medicine are QPLs, comprehensive lists of potential questions patients can ask their physician, and the three-question ASK handout (What are my options? What are the benefits and harms of those options? How likely are each of those benefits and harms to happen to me?). The comparative effectiveness of these tools in orthopaedic surgery has not been established. We compared a QPL developed for orthopaedic surgery and the three-question ASK handout questions to determine their effect on patient-perceived involvement in care. We used a pragmatic RCT design to compare the effectiveness of two tools already used in medicine to mimic real clinical care. We found that the orthopaedic-specific QPL did not increase patients’ perceived involvement in their care compared with the three generic questions. Therefore, a short, three-question list may be easier for patients to use and more efficient for surgeons to employ in practice as they seek to promote patient involvement in their care.
Limitations
Our study has some limitations. The QPL for this study was 45 questions, so patients may not have had time to review all questions before their encounter. The length allowed the QPL to be comprehensive (reviewed by both patients and physicians), and it was comparable or shorter than many existing QPLs. Additionally, we were not able to control whether patients may have generated their own list of questions before the visit, but such patients likely were randomized equally to both groups. This study was conducted at a single center and other patient populations may have a different experience with using QPLs. However, our tools were designed at the fifth-grade reading level, and we see no reason why other populations of varying race, age, gender, or other elements of demography would be more or less engaged by either tool. There are also other potential benefits of QPLs that were not measured in the context of our study. In an oncology study conducted by Clayton et al. [11], patients provided with QPLs asked more questions and discussed more issues during the visit. We chose to assess PICS, a commonly used measure that focuses on the patient perspective. There is no consensus on the best outcome measure for SDM interventions, so it is unknown whether using a different outcome measure would have produced different results. We were not powered to conduct analyses based on sociodemographic elements. Lastly, we were not able to blind the physicians to which study group the participants were assigned to, risking contamination. The surgeon was not informed as to which handout each patient was given; however, the handouts remained with the patient in the consultation room as we wanted patients to have access to the handout during their encounter. Because this was an exploratory, pragmatic study, we felt our randomization process was sufficient; however, future studies may consider larger cluster-randomized controlled trials to prevent the possibility of contamination.
Formal QPL versus Generic Three-question Tool
We found no difference in PICS scores between the two groups. We opted to compare our QPL intervention with an active control (comparative effectiveness) as opposed to no intervention (efficacy). We designed our study in this pragmatic way for two reasons: (1) There is already evidence which demonstrates that giving patients a three-question handout improves their involvement in their care [18], and (2) regardless of our results, we could provide surgeons with a result they could implement into their clinics, whether it was a QPL or the three-question ASK handout. Our results indicate that the three-question handout provides a comparable level of engagement as a comprehensive, 45-question, orthopaedic-specific handout, indicating that lengthy materials may not be necessary. As such, the three-question handout can be easily implemented into routine orthopaedic practice and reviewed by patients in a very short timeframe. Physicians can easily build this process into their existing workflows by providing the handout at check-in or placing them in patient rooms; the questions are self-explanatory and do not require additional time to facilitate usage compared with many common orthopaedic decision aids. Providing the three-question handout will prompt patients to engage, ask questions, and ensure involvement toward informed treatment decision.
Our results are comparable to prior studies conducted using PICS as an outcome measure, which have found similarly high scores for PICS [24, 30, 41]. An observational study of orthopaedic patients found an average PICS score of 8.43 ± 2.3 [25], which is very similar to the scores in both groups of this study. We found a difference in favor of the control group for subscale A, perceived clinician facilitation of patient involvement. To understand why only this subscale was affected, future work should focus on analyzing the physician-patient interaction.
One of the key tenets of SDM calls for engaging patients in discussions about their health decisions. However, many studies indicate that patients are less engaged than they would like to be, and this is even more severe for patients in some minority groups [2, 19]. Several campaigns directed at encouraging patients to ask more questions, such as “Speak Up” and “Questions are the Answer,” are led by The Joint Commission and the Agency for Healthcare Research and Quality, respectively. Handouts that encourage patients to ask questions may help overcome the perception that patients should listen and not ask questions [14, 17]. As such, providing patients with three simple ASK questions in orthopaedic surgery may be a time-efficient process to improve shared decision making while also being easily incorporated into the workflow of a typical orthopaedic practice.
Conclusion
We found no difference in patient-perceived involvement when providing patients with two handouts of different lengths (45 versus three questions) and content (orthopaedic-specific versus generic questions). Based on our results with using PICS as the outcome, a shorter handout may be just as effective and more efficient at promoting patients’ engagement in their care. Future work can evaluate other outcome measures that may be influenced more by these handouts, such as number of questions asked, patient knowledge, or handout usage.
Supplementary Material
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
The institution of one or more of the authors (RNK) has received, during the study period, funding from the National Institutes of Health (K23AR073307-01 award) and the Orthopaedic Research and Education Foundation.
Each author certifies that neither he nor she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Adam JA, Khaw F-M, Thomson RG, Gregg PJ, Llewellyn-Thomas HA. Patient decision aids in joint replacement surgery: a literature review and an opinion survey of consultant orthopaedic surgeons. Ann R Coll Surg Engl. 2008;90:198-207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alston C, Paget L, Informed Medical Decisions Foundation, et al. Communicating with patients on health care evidence. Available at: https://nam.edu/perspectives-2012-communicating-with-patients-on-health-care-evidence/. Accessed May 18, 2020.
- 3.Baijens SWE, Huppelschoten AG, Van Dillen J, Aarts JWM. Improving shared decision-making in a clinical obstetric ward by using the three questions intervention, a pilot study. BMC Pregnancy Childbirth. 2018;18:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barry MJ, Edgman-Levitan S. Shared decision making--pinnacle of patient-centered care. N. Engl J Med. 2012;366:780-781. [DOI] [PubMed] [Google Scholar]
- 5.Bozic KJ. Orthopaedic healthcare worldwide: shared medical decision making in orthopaedics. Clin Orthop Relat Res. 2013;471:1412-1414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brandes K, Linn Annemiek J, van Weert, Julia CM. The characteristics and effectiveness of question prompt list interventions in oncology: a systematic review of the literature. Psychooncology. 24:245-252. [DOI] [PubMed] [Google Scholar]
- 7.Brown RF, Shuk E, Leighl N, et al. Enhancing decision making about participation in cancer clinical trials: development of a question prompt list. Support Care Cancer. 2011;19:1227-1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bunzli S, Nelson E, Scott A, French S, Choong P, Dowsey M. Barriers and facilitators to orthopaedic surgeons’ uptake of decision aids for total knee arthroplasty: a qualitative study. BMJ Open. 2017;7:e018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clark JP, Hudak PL, Hawker GA, et al. The moving target: a qualitative study of elderly patients’ decision-making regarding total joint replacement surgery. J Bone Joint Surg Am. 2004;86:1366-1374. [PubMed] [Google Scholar]
- 10.Clayton J, Butow P, Tattersall M, et al. Asking questions can help: development and preliminary evaluation of a question prompt list for palliative care patients. Br J Cancer. 2003;89:2069-2077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clayton JM, Butow PN, Tattersall MHN, et al. Randomized controlled trial of a prompt list to help advanced cancer patients and their caregivers to ask questions about prognosis and end-of-life care. J Clin Oncol 2007;25:715-723. [DOI] [PubMed] [Google Scholar]
- 12.Dal-Ré R, Janiaud P, Ioannidis JPA. Real-world evidence: how pragmatic are randomized controlled trials labeled as pragmatic? BMC Med. 2018;16:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eggly S, Tkatch R, Penner LA, et al. Development of a question prompt list as a communication intervention to reduce racial disparities in cancer treatment. J Cancer Educ. 2013;28:282-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fleissig A, Glasser B, Lloyd M. Encouraging out-patients to make the most of their first hospital appointment: to what extent can a written prompt help patients get the information they want? Patient Educ Couns. 1999;38:69-79. [DOI] [PubMed] [Google Scholar]
- 15.Garvelink MM, Jillissen M, Knops A, Kremer JAM, Hermens RPMG, Meinders MJ. Implementation of the three good questions-a feasibility study in Dutch hospital departments. Health Expect. 2019;22:1272-1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gravel K, Légaré F, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals’ perceptions. Implement Sci. 2006;1:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Judson TJ, Detsky AS, Press MJ. Encouraging patients to ask questions: how to overcome “white-coat silence.” JAMA. 2013;309:2325-2326. [DOI] [PubMed] [Google Scholar]
- 18.Kaplan SH, Greenfield S, Gandek B, Rogers WH, Ware JE. Characteristics of physicians with participatory decision-making styles. Ann Intern Med. 1996;124:497-504. [DOI] [PubMed] [Google Scholar]
- 19.Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision-making and interpersonal behavior: evidence, models and interventions. Patient Educ Couns. 2006;61:319-341. [DOI] [PubMed] [Google Scholar]
- 20.Kinnersley P, Edwards A, Hood K, et al. Interventions before consultations to help patients address their information needs by encouraging question asking: systematic review. BMJ. 2008;337:a485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lerman CE, Brody DS, Caputo GC, Smith DG, Lazaro CG, Wolfson HG. Patients’ perceived involvement in care scale: relationship to attitudes about illness and medical care. J Gen Intern Med. 1990;5:29-33. [DOI] [PubMed] [Google Scholar]
- 22.Lim L, Chow P, Wong C-Y, et al. Doctor-patient communication, knowledge, and question prompt lists in reducing preoperative anxiety: a randomized control study. Asian J Surg. 2011;34:175-180. [DOI] [PubMed] [Google Scholar]
- 23.Lindig A, Hahlweg P, Frerichs W, Topf C, Reemts M, Scholl I. Adaptation and qualitative evaluation of Ask 3 Questions - a simple and generic intervention to foster patient empowerment. Health Expect. [Published online ahead of print August 1, 2020]. DOI: 10.1111/hex.13114. [DOI] [PMC free article] [PubMed]
- 24.McGarragle KM, Aronson M, Semotiuk K, et al. Patient-physician relationships, health self-efficacy, and gynecologic cancer screening among women with Lynch syndrome. Hered Cancer Clin Pract. 2019;17:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mertz K, Eppler S, Yao J, et al. Patient perceptions correlate weakly with observed patient involvement in decision-making in orthopaedic surgery. Clin Orthop Relat Res . 2018;476:1859-1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mertz K, Shah RF, Eppler SL, et al. A simple goal elicitation tool improves shared decision making in outpatient orthopedic surgery: a randomized controlled trial. Med Decis Making. 2020;40:766-773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.O’Donnell S, Cranney A, Jacobsen MJ, Graham ID, O’Connor AM, Tugwell P. Understanding and overcoming the barriers of implementing patient decision aids in clinical practice. J Eval Clin Pract. 2006;12:174-181. [DOI] [PubMed] [Google Scholar]
- 28.Patsopoulos NA. A pragmatic view on pragmatic trials. Dialogues Clin Neurosci. 2011;13:217-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Phelan EA, Deyo RA, Cherkin DC, et al. Helping patients decide about back surgery: a randomized trial of an interactive video program. Spine. 2001;26:206-211. [DOI] [PubMed] [Google Scholar]
- 30.Pietrolongo E, Giordano A, Kleinefeld M, et al. Decision-making in multiple sclerosis consultations in Italy: third observer and patient assessments. PLoS One. 2013;8:e60721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.R Core Team (2014). R: A language and environment for statistical computing . Vienna, Austria: R Foundation for Statistical Computing; Available at: http://www.R-project.org/. Accessed February 19, 2020. [Google Scholar]
- 32.Sansoni JE, Grootemaat P, Duncan C. Question prompt lists in health consultations: a review. Patient Educ Couns. 2015;98:1454-1464. [DOI] [PubMed] [Google Scholar]
- 33.Satteson ES, Roe AK, Eppler SL, Yao J, Shapiro LM, Kamal RN. Development and testing of a question prompt list for common hand conditions: an exploratory sequential mixed-methods study. J Hand Surg Am. 2020;45:1087.e1-1087.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med. 2010;152:726-732. [DOI] [PubMed] [Google Scholar]
- 35.Sealed Envelope Ltd Create a blocked randomisation list. Available at: https://www.sealedenvelope.com/simple-randomiser/v1/lists. Accessed May 21, 2020.
- 36.Sepucha KR, Atlas SJ, Chang Y, et al. Informed, patient-centered decisions associated with better health outcomes in orthopedics: prospective cohort study. Med Decis Making. 2018;38:1018-1026. [DOI] [PubMed] [Google Scholar]
- 37.Shepherd HL, Barratt A, Jones A, et al. Can consumers learn to ask three questions to improve shared decision making? A feasibility study of the ASK (AskShareKnow) Patient-Clinician Communication Model® intervention in a primary health-care setting. Health Expect. 2016;19:1160-1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shepherd HL, Barratt A, Trevena LJ, et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: a cross-over trial. Patient Educ Couns. 2011;84:379-385. [DOI] [PubMed] [Google Scholar]
- 39.Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011:CD001431. [DOI] [PubMed] [Google Scholar]
- 40.Stossel LM, Segar N, Gliatto P, Fallar R, Karani R. Readability of patient education materials available at the point of care. J Gen Intern Med. 2012;27:1165-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Suzuki M. Quality of life, uncertainty, and perceived involvement in decision making in patients with head and neck cancer. Oncol Nurs Forum. 2012;39:541-548. [DOI] [PubMed] [Google Scholar]
- 42.Walczak A, Henselmans I, Tattersall MHN, et al. A qualitative analysis of responses to a question prompt list and prognosis and end-of-life care discussion prompts delivered in a communication support program. Psychooncology. 2015;24:287-293. [DOI] [PubMed] [Google Scholar]
- 43.Walczak A, Mazer B, Butow PN, et al. A question prompt list for patients with advanced cancer in the final year of life: development and cross-cultural evaluation. Palliat Med. 2013;27:779-788. [DOI] [PubMed] [Google Scholar]
- 44.Yeh JC, Cheng MJ, Chung CH, Smith TJ. Using a question prompt list as a communication aid in advanced cancer care. J Oncol Pract. 2014;10:e137-141. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.