Abstract
Background
Many acceptable treatment options exist for distal radius fractures (DRFs); however, a simultaneous comparison of all methods is difficult using conventional study designs.
Questions/purposes
We performed a network meta-analysis of randomized controlled trials (RCTs) on DRF treatment to answer the following questions: Compared with nonoperative treatment, (1) which intervention is associated with the best 1-year functional outcome? (2) Which intervention is associated with the lowest risk of overall complications? (3) Which intervention is associated with the lowest risk of complications requiring operation?
Methods
Ten databases were searched from inception to July 25, 2019. Search and analysis reporting adhered to Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines. Included studies were English-language RCTs that assessed at least one surgical treatment arm for adult patients with displaced DRFs, with less than 20% loss to follow-up. We excluded RCTs reporting on patients with open fractures, extensive bone loss, or ipsilateral upper extremity polytrauma. Seventy RCTs (n = 4789 patients) were included. Treatments compared were the volar locking plate, bridging external fixation, nonbridging external fixation, dynamic external fixation, percutaneous pinning, intramedullary fixation, dorsal plating, fragment-specific plating, and nonoperative treatment. Subgroup analyses were conducted for intraarticular fractures, extraarticular fractures, and patients with an average age greater than 60 years. Mean (range) patient age was 59 years (56 to 63) and was similar across all treatment groups except for dynamic external fixation (44 years) and fragment-specific plating (47 years). Distribution of intraarticular and extraarticular fractures was approximately equal among the treatment groups other than that for intramedullary fixation (73% extraarticular), fragment-specific plating (66% intraarticular) [13, 70], and dorsal plating (100% intraarticular). Outcomes were the DASH score at 1 year, total complications, and reoperation. The minimum clinically important different (MCID) for the DASH score was set at 10 points. The analysis was performed using Bayesian methodology with random-effects models. Rank orders were generated using surface under the cumulative ranking curve values. Evidence quality was assessed using Grades of Recommendation, Assessment, Development and Evaluation (GRADE) methodology. Most studies had a low risk of bias due to randomization and low rates of incomplete follow-up, unclear risk of bias due to selective reporting, and high risk of bias due to lack of patient and assessor blinding. Studies assessing bridging external fixation and/or nonoperative treatment arms had a higher overall risk of bias while studies with volar plating and/or percutaneous pinning treatment arms had a lower risk of bias.
Results
Across all patients, there were no clinically important differences in terms of the DASH score at 1 year; although differences were found, all were less than the MCID of 10 points. Volar plating was ranked the highest for DASH score at 1 year (mean difference -7.34 [95% credible interval -11 to -3.7) while intramedullary fixation, with low-quality evidence, also showed improvement in DASH score (mean difference -7.75 [95% CI -14.6 to -0.56]). The subgroup analysis revealed that only locked volar plating was favored over nonoperative treatment for patients older than 60 years of age (mean difference -6.4 [95% CI -11 to -2.1]) and for those with intraarticular fractures (mean difference -8.4 [95% CI -15 to -2.0]). However, its clinical importance was uncertain as the MCID was not met. Among all patients, intramedullary fixation (odds ratio 0.09 [95% CI 0.02 to 0.84]) and locked volar plating (OR 0.14 [95% CI 0.05 to 0.39]) were associated with a lower complication risk compared with nonoperative treatment. For intraarticular fractures, volar plating was the only treatment associated with a lower risk of complications than nonoperative treatment (OR 0.021 [95% CI < 0.01 to 0.50]). For extraarticular fractures, only nonbridging external fixation was associated with a lower risk of complications than nonoperative treatment (OR 0.011 [95% CI < 0.01 to 0.65]), although the quality of evidence was low. Among all patients, the risk of complications requiring operation was lower with intramedullary fixation (OR 0.06 [95% CI < 0.01 to 0.85) than with nonoperative treatment, but no treatment was favored over nonoperative treatment when analyzed by subgroups.
Conclusion
We found no clinically important differences favoring any surgical treatment option with respect to 1-year functional outcome. However, relative to the other options, volar plating was associated with a lower complication risk, particularly in patients with intraarticular fractures, while nonbridging external fixation was associated with a lower complication risk in patients with extraarticular fractures. For patients older than 60 years of age, nonoperative treatment may still be the preferred option because there is no reliable evidence showing a consistent decrease in complications or complications requiring operation among the other treatment options. Particularly in this age group, the decision to expose patients to even a single surgery should be made with caution.
Level of Evidence
Level I, therapeutic study.
Introduction
Although closed reduction and casting is often the treatment of choice for stable, nondisplaced fractures, operative fixation is recommended for displaced or unstable distal radius fractures (DRFs) [8]; there is concern for functional limitations if they are left untreated beyond 4 weeks [73, 78, 95, 113]. Fixed-angle volar plating is the most common method of internal fixation for displaced DRFs and is preferred by nearly 85% of hand and wrist surgeons [105]. Other methods of surgical fixation include bridging or nonbridging external fixation, percutaneous pinning, dorsal plating, fragment-specific plating, and intramedullary fixation. The fixation choice is largely guided by patient and fracture characteristics; however, surgeon preference continues to play a large role in this decision, and the superiority of one method to another continues to be contentious [14, 64, 73].
There is a relative abundance of studies exploring DRF treatment, including numerous meta-analyses of pooled data from randomized controlled trails (RCTs) (Supplemental Digital Content 1; http://links.lww.com/CORR/A441). Many pairwise comparisons have been made including internal and external fixation [125, 126, 128, 134, 135, 137], dynamic or nonbridging and static external fixation [20, 41, 86], volar locking plates and external fixation [26, 32, 74, 122, 123], volar locking plates and percutaneous K-wires [4, 17, 30, 108, 109, 136, 140], and volar locking plates and intramedullary fixation [139]. Important between-study differences have been identified, including subtle differences in functional outcomes and complication profiles [23, 127]. Unfortunately, all traditional meta-analyses can only compare two treatment options at a time, thereby excluding large numbers of studies regarding DRF treatment. In addition, we have observed that not all contemporary treatment approaches have been compared head to head in RCTs, preventing the inclusion of these approaches in traditional meta-analyses. Multiarm RCTs have been performed, but they are limited by sample size, and comparing all potential treatment arms in one trial would be impractical [3, 23, 126]. Ultimately, despite the number of RCTs and meta-analyses, no consensus has been reached by major orthopaedic and hand surgery associations on the ideal DRF treatment [14, 73].
Considering the limitations of existing studies, a network meta-analysis (NMA) offers several advantages [58]. Unlike a traditional direct meta-analysis, an NMA leverages direct and indirect comparisons using network relationships of common treatment arms [16, 28, 38, 119]. The relative effect of treatments that have not been directly compared, or directly compared in only a few studies, can be estimated using a common comparator, such as nonoperative treatment [28, 121]. This facilitates the inclusion of outcome data from nearly all published RCTs on the treatment of DRFs in the final analysis, thereby generating more-complete, evidence-based effect estimates of treatment.
Therefore, we asked the following questions: Compared with nonoperative treatment, (1) which intervention is associated with the best 1-year functional outcome? (2) Which intervention is associated with the lowest risk of overall complications? (3) Which intervention is associated with the lowest risk of complications requiring surgery?
Materials and Methods
Search Strategy
This systematic review and NMA was conducted in compliance with the Cochrane Handbook for Systematic Reviews of Interventions [47] and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for NMAs [54, 87] (Supplemental Digital Content 2; http://links.lww.com/CORR/A442). We comprehensively searched 10 electronic databases to identify relevant RCTs, including MEDLINE, Embase, Cumulative Index to Nursing & Allied Health Literature (CINAHL), Web of Science, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Latin American and Caribbean Center on Health Sciences Information, Physiotherapy Evidence Database, the WHO’s International Clinical Trials Registry Platform, and ClinicalTrials.gov. Search terms were generated through consultation with clinical epidemiologists (AK, HJ) (Supplemental Digital Content 2; http://links.lww.com/CORR/A442). The unaltered study protocol is available for reference (Supplemental Digital Content 3; http://links.lww.com/CORR/A443).
Selection Criteria
Inclusion criteria were RCTs with two or more treatment arms, at least one of which involved a surgical intervention. We selected English-language studies with adult patients (age 18 years or older) with DRF that were published either as a full-text article or abstract. Minimum follow-up duration was 3 months. The included surgical interventions were determined before the study search. Treatment groups included a volar locking plate, bridging external fixation, nonbridging external fixation, dynamic external fixation, percutaneous pinning (any technique), intramedullary fixation, dorsal plating, fragment-specific plating, and nonoperative treatment. Nonoperative treatment, a common control group, was defined as below-elbow plate or fiberglass casting for a duration meeting the standard of care according to the authors’ respective institutions, typically 30 to 45 days. We included trials reporting any of our predetermined outcomes of interest and excluded trials solely comparing implant properties or variations in treatment application. If multiple studies reported on the same outcomes for the same patient population, we included only the most recent publication. However, if different outcomes of interest or different timepoints were reported, we included both studies. We excluded studies if nonrandom loss to follow-up was > 20% [66]. In addition, we excluded trials from the quantitative analysis if they involved patients who had open fractures, extensive bone loss, or ipsilateral upper extremity polytrauma. There was no restriction on publication date. Observational studies, case series, case reports, biomechanical cadaver studies, basic science studies, review articles, correspondence, and comments were excluded.
Screening
The search was completed on July 25, 2019. The search was augmented by a manual review of references from included studies and relevant systematic reviews. Studies were screened using Mendeley (Version 1.19.3, Mendeley Limited, London, UK). Three teams of two reviewers each (TW, AK, FK, LG, JG, KG) screened all titles, abstracts, and full-text articles independently and in duplicate. Discrepancies were resolved by automatic inclusion at the title and abstract stages and by involvement of a senior author (HJ) at the full-text stage.
Outcomes of Interest
The outcomes of interest were as follows: (1) functional score: DASH score at 1 year postoperatively [129]. The minimum clinically important difference (MCID) was established as 10 points based on published values [31]. (2) Complications: major listed complications including infection, complex regional pain syndrome, tenosynovitis, tendon rupture, tendinitis, and nerve injury. (3) Risk of complication requiring surgery, including any need for surgery after the index procedure and excluding planned external fixation or pin removal. For surgical treatment options, this constitutes reoperation, and for all patients, an unplanned operation. Considering functional outcome, we chose to use the DASH score alone as it is the most commonly reported quantitative functional score in the DRF literature. Considering that the DASH was published in 1996, studies predating this time were excluded from the functional analysis. Although many different scores have been used, this decision was made to avoid the potential pitfalls of combining functional scores.
Data Extraction
Data were abstracted in duplicate by a team of four reviewers (TW, LG, JG, KG) using a piloted extraction document (Microsoft Excel 16.2, Redmond, WA, USA), which was designed a priori. Discrepancies were resolved through consultation with a fifth reviewer (HJ). Abstracted data included country of origin, RCT methods, patient demographics, fracture pattern, treatment details, follow-up duration, and loss to follow-up. Routine removal of percutaneous K-wires and/or external fixation pins was not recorded as a reoperation, while removal of internal hardware (such as screws) qualified as a complication requiring operation. Means and standard deviations were collected; medians were used in lieu of means if mean values were not available [93]. If a 95% confidence interval was reported as the measure of variability, the SD was approximated [48]. When no measure of variance was reported, the SD was imputed using a p value or a weighted average of variances observed in other included studies [48, 77].
Quality Assessment
The quality of each included study was evaluated in duplicate using the Cochrane Risk of Bias tool, and the Cochrane Confidence in Network Meta-Analysis (CINeMA) tool was used for the risk of bias assessment specific to NMAs [18, 46]. Risk of bias domains were rated according to predefined criteria (Supplemental Digital Content 2; http://links.lww.com/CORR/A442). Of note, loss to follow-up less than 5% was considered low risk of bias, while loss great than 20% was considered to pose a high risk of bias. Disagreement was resolved through consultation with the senior author (HJ). The overall quality of the evidence was determined and ranked per the Grades of Recommendation, Assessment, Development and Evaluation approach for NMAs [43, 97].
Study Characteristics
The final search identified 16,724 studies; 223 studies underwent full-text review, of which 75 were included in the systematic review and 70 (n = 4789 patients) in the NMA (Fig. 1). Included studies were published between 1989 and 2019. Reflecting trends in surgical technique, most studies involving volar plating [6, 11, 19, 23, 24, 33, 37, 39, 40, 49, 59, 60, 63, 71, 79, 81, 82, 89, 90, 92, 98, 102, 104, 106, 110, 117, 131, 132] or intramedullary fixation [15, 35, 36, 94, 107, 138] (87% and 89%, respectively) were published since 2010, while approximately half of all studies involving external fixation [1, 2, 5, 7, 27, 44, 45, 50-52, 55, 61, 62, 65, 67-69, 83, 88, 99-101, 111, 134] or percutaneous fixation [3, 4, 9, 10, 12, 42, 72, 75, 80, 84, 96, 103, 114, 115, 120, 130, 133] (56% and 44%, respectively) were published before 2010 (Supplemental Digital Content 4; http://links.lww.com/CORR/A444). Studies included 19 unique pairwise comparisons. Two studies had three treatment arms. Fifty-three percent (37 of 70) of studies had a mean patient age older than 60 years, while 74% of all patients (3543 of 4789) were female (Table 1). Follow-up was 12 months or longer in all studies (median [range] 24 months [12 to 240]) and sample sizes were typically small (median [range] 61 patients [9 to 231]). Twenty-four percent (17 of 70) of studies only included intraarticular fractures, while 24% (17 of 70) only included extraarticular fractures (Supplemental Digital Content 4; http://links.lww.com/CORR/A444).
Fig. 1.
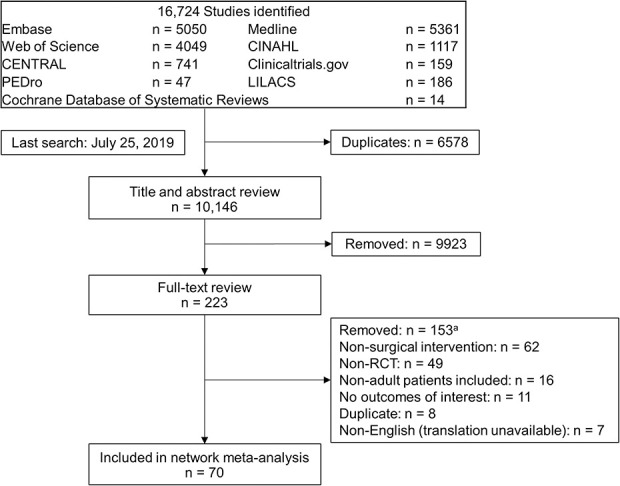
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram for study screening. aFive studies examined novel interventions or modifications of interventions that were not found in other studies and were therefore excluded from the network meta-analysis.
Table 1.
Network patient and fracture characteristics
| Fracture Pattern | |||||||
| Treatment group | Patients, number | Treatment arms, number | Mean age in years (range) | % female | Intraarticular | Extraarticular | Not specified |
| Volar locking plate | 1441 | 36 | 62 (36 to 80) | 79 | 683 (47) | 566 (39) | 192 (13) |
| Bridging external fixation | 910 | 31 | 56 (39 to 74) | 70 | 476 (49) | 308 (32) | 180 (19) |
| Percutaneous pinning | 843 | 17 | 59 (41 to 73) | 76 | 235 (28) | 364 (43) | 244 (29) |
| Nonoperative | 810 | 24 | 61 (32 to 78) | 75 | 355 (44) | 455 (56) | 0 (0) |
| Intramedullary fixation | 285 | 10 | 60 (48 to 72) | 77 | 30 (11) | 209 (73) | 46 (9) |
| Nonbridging external fixation | 212 | 8 | 63 (62 to 64) | 79 | 45 (21) | 91 (43) | 76 (36) |
| Dynamic external fixation | 127 | 4 | 44 (34 to 54) | 48 | 49 (39) | 40 (31) | 38 (30) |
| Fragment-specific plating | 97 | 6 | 47 (24 to 60) | 75 | 64 (66) | 9 (9) | 24 (25) |
| Dorsal plate | 64 | 3 | 59 (45 to 74) | 61 | 64 (100) | 0 (0) | 0 (0) |
For fracture pattern, values are number of patients with proportion listed in parentheses.
Study Quality
Most studies had a low risk of randomization bias, low or unclear risk of allocation bias, and low risk of bias secondary to low rates of incomplete follow-up (Fig. 2). The risk of bias because of selective reporting and other factors was largely unclear. Because of the nature of surgical management, blinding of patients and outcome assessors was largely infeasible, and thus the risk of performance and detection bias was high in most studies. Studies including bridging external fixation and/or nonoperative treatment arms had a higher overall risk of bias, with 23% (7 of 31) and 21% (5 of 24) of studies at high risk of bias, respectively. Studies including volar plating and/or percutaneous pinning treatment arms had a lower risk, with only 6% (2 of 36) and 6% (1 of 17) of studies being rated as having a high risk of bias, respectively.
Fig. 2.
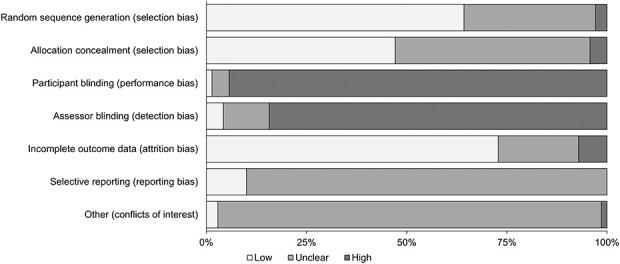
Risk of bias for the included studies.
Statistical Analysis
Statistical analysis was performed using RevMan 5.3 (Cochrane, London, UK), GraphPad Prism 8.2.0 (GraphPad Software, San Diego, CA, USA), and R 3.4.2 (Open Access Online). The NMA was conducted using Bayesian random-effects modeling, which is frequently used to analyze data with statistical heterogeneity [77, 118]. Noninformative priors were used. Prior distributions describe the uncertainty about a given effect measure. When using noninformative priors, all values in the plausible range of outcomes are assumed to have an equal likelihood of occurrence and only data from included studies are used during analysis [58, 118]. Using noninformative priors avoids introducing subjectivity and/or nonrandomized data into the analysis models. Trials with three or more arms were addressed by the statistical package without manipulation. Ranking diagrams, forest plots, and graphical frameworks were created for each outcome. Surface under the cumulative ranking curve (SUCRA) values were reported for each treatment group. The SUCRA score represents the likelihood that a given treatment will rank first in a specific category; a score closer to 1 indicates that treatment is more likely to represent the best treatment. Global inconsistency across each network model was described using the I2 value, representing the variation percentage across studies because of study heterogeneity. Incoherence (inconsistency between direct and indirect evidence) was assessed globally using the design-by-treatment interaction test and for individual comparisons using the Separating Indirect from Direct Evidence and node-splitting methods [21, 130]. Global network heterogeneity was moderate for DASH (I2 50%), substantial for complications (I2 77%), and moderate for complications requiring operation (I2 50%).
We conducted a subgroup analysis using three primary subgroups: (1) studies of intraarticular fractures only, (2) studies of extraarticular fractures only, and (3) studies with an average patient age older than 60 years. Interventions were included in the subgroup analysis if data for that intervention were available from at least two independent trials. For all outcomes, a meta-regression analysis was performed to determine whether the age of the included patients affected the pooled treatment estimates. Sensitivity analysis was conducted to determine whether inclusion of studies with less than 1-year follow-up influenced findings regarding complications or complications requiring operation; this was done by repeating the primary outcome analyses after excluding studies with less than 1-year follow-up.
The results of the network for DASH scores are reported as mean differences (MD) with 95% credible intervals. The MCID for DASH scores was established at 10 points, representing the best-available studies [31, 112]. Only studies reported after the publication of the DASH (1996) were included in the functional analysis [53]. Complications and complications requiring surgery are presented using odds ratios and 95% CIs, which were derived using the posterior distribution of the outcome in question and can be thought of as the Bayesian equivalent of confidence intervals. For studies that reported more complications than patients in a treatment arm, the value was set as equal to the sample size. For studies with the highest rate of complications, the network estimates will underestimate the true value. Comparisons were inferred to be statistically significant if the 95% CI of the MD did not cross 0 or if the 95% CI of the OR did not cross one. The number needed to treat was calculated using patient-expected event rates—the weighted average event rates for nonoperative treatment in each respective subgroup.
Results
Functional Outcomes (DASH Score) at 1 Year
There were no clinically important differences in terms of the DASH score at 1 year; although there were differences observed, all were lower than the MCID of 10 points (Table 2). Among all patients, volar plating was ranked the highest by the network (35 RCTs; MD -7.34 [95% CI -11 to -3.7]; SUCRA 0.86) (Supplemental Digital Content 5; http://links.lww.com/CORR/A445). In the intraarticular fracture subgroup (10 RCTs), volar plating was the only treatment associated with less disability at 1 year (MD -8.4 [95% CI -15 to -2]) compared with nonoperative treatment (Supplemental Digital Content 6; http://links.lww.com/CORR/A446). For these patients, bridging external fixation (MD -14 [95% CI -32 to 4.8]; SUCRA 0.80) was ranked the highest but the estimate was imprecise. No studies involved treatment of exclusively intraarticular fractures with either dynamic external fixation, nonbridging external fixation, or intramedullary fixation. In the subgroup of studies with an average patient age of 60 years or older (seven RCTs), volar plating still ranked the highest and was the only treatment associated with DASH scores better than nonoperative treatment (MD -6.4 [95% CI -11 to -2.1]; SUCRA 0.76) (Supplemental Digital Content 7; http://links.lww.com/CORR/A447).
Table 2.
GRADE summary table for DASH score at 1 year
| Group | Rank | Intervention | Mean difference (95% CI) | Quality of evidence |
| All patients | 1 | Volar locking plate | -7.3 (-11 to -3.7)a | Moderateb |
| 2 | Intramedullary fixation | -7.8 (-14.6 to -0.56)a | Very lowb,c | |
| Intraarticular | 1 | Bridging external fixation | -14 (-32 to 4.8) | Very lowc,d |
| 2 | Fragment-specific plating | -11 (-25 to 2.0) | Lowc | |
| 3 | Volar locking plate | -8.4 (-15 to -2.0)a | Moderatee | |
| Extraarticular | 1 | Volar locking plate | -4.6 (-10 to 1.4) | Lowd,f |
| 2 | Nonbridging external fixation | -6.0 (-15 to 3.1) | Very lowc,e | |
| Average age older than 60 years | 1 | Volar locking plate | -6.4 (-11 to -2.1)a | Moderateb |
| 2 | Percutaneous pinning | -7.3 (-22 to 7.1) | Very lowb,c,e |
Inferred to be statistically significant with a 95% CI for mean difference not crossing zero.
Downgraded for indirectness.
Downgraded two levels for imprecision.
Downgraded for risk of bias.
Downgraded for inconsistency.
Downgraded for imprecision.
Mean differences are relative to nonoperative treatment; rank based on SUCRA value; small sample size was considered in the evaluation of imprecision; MCID for DASH is 10 points; GRADE = Grading of Recommendations Assessment, Development and Evaluation.
Complications
Among all patients, intramedullary fixation, nonbridging external fixation, and volar plating were associated with fewer overall complications than nonoperative treatment (Table 3). In the network including all patients, (65 RCTs, Fig. 3) intramedullary fixation (OR 0.09 [95% CI 0.02 to 0.48]; SUCRA 0.89) was ranked highest (Supplemental Digital Content 8; http://links.lww.com/CORR/A448). The sensitivity analysis demonstrated that these findings were consistent when excluding studies involving only patients older than 60 years of age. The subgroup analysis of intraarticular fractures (18 RCTs) revealed that volar plating (OR 0.02 [95% CI < 0.01 to 0.50]; SUCRA 0.74) was the only treatment associated with a lower risk of complication than nonoperative treatment (Supplemental Digital Content 9; http://links.lww.com/CORR/A449). In the extraarticular subgroup (18 RCTs), only nonbridging external fixation (OR 0.01 [95% CI < 0.01 to 0.65]; SUCRA 0.95) was associated with a lower risk of complications than nonoperative treatment; it was ranked the highest by the network. In the subgroup of studies with average patient age older than 60 years (29 RCTs), there was no difference in the risk of complications between nonoperative treatment and any operative intervention (Supplemental Digital Content 10; http://links.lww.com/CORR/A450). Sensitivity analysis demonstrated that including studies with less than 1 year of follow-up did not influence findings.
Table 3.
GRADE summary table for risk of complications
| Group | Rank | Intervention | Odds ratio (95% CI) | NNT | Quality of evidence |
| All patients | 1 | Intramedullary fixation | 0.089 (0.02 to 0.84)a | 3 | Lowb,c |
| 2 | Volar locking plate | 0.14 (0.05 to 0.39)a | 3 | Moderatec,d | |
| 3 | Nonbridging external fixation | 0.16 (0.02 to 0.92)a | 3 | Lowc,e | |
| Intraarticular | 1 | Percutaneous pinning | 0.015 (< 0.01 to 1.1) | 2 | Lowe |
| 2 | Volar locking plate | 0.021 (< 0.01 to 0.50)a | 2 | Moderated | |
| Extraarticular | 1 | Nonbridging external fixation | 0.011 (< 0.01 to 0.65)a | 6 | Lowe |
| 2 | Intramedullary fixation | 0.10 (< 0.01 to 1.2) | 7 | Lowc,d | |
| Average age older than 60 years | 1 | Dorsal plate | 0.076 (< 0.01 to 3.0) | 4 | Very lowc,e,f |
| 2 | Intramedullary fixation | 0.13 (0.01 to 1.7) | 4 | Very lowb,c,d |
Inferred to be statistically significant with a 95% CI for mean difference not crossing zero.
Downgraded for inconsistency.
Downgraded for indirectness.
Downgraded for imprecision.
Downgraded two levels for imprecision.
Downgraded for risk of bias.
Odds ratios are relative to nonoperative treatment; rank based on SUCRA value; small sample size was considered in the evaluation of imprecision; GRADE = Grading of Recommendations Assessment, Development and Evaluation; NNT = number needed to treat.
Fig. 3.
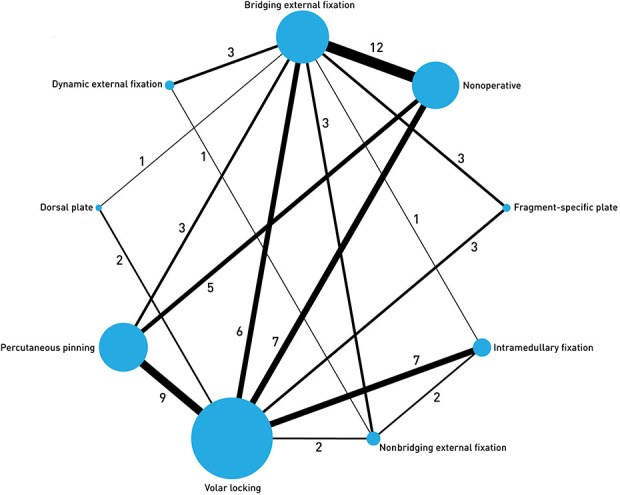
The network geometry for complications. Node size is proportionate to the number of patients in the specified treatment arm. Line thickness is proportionate to the number of studies. Numbers represent the number of studies directly comparing respective interventions.
Risk of Complications Requiring Operation
Among all patients, intramedullary fixation, nonbridging external fixation, bridging external fixation, and percutaneous pinning were associated with a lower risk of complications requiring operation than nonoperative treatment, with intramedullary fixation (OR 0.06 [95% CI < 0.01 to 0.85]; SUCRA 0.89) being ranked highest by the network (Supplemental Digital Content 11; http://links.lww.com/CORR/A451). In the intraarticular subgroup (15 RCTs), there was no difference in the risk of complications requiring operation between any surgical intervention and nonoperative treatment (Supplemental Digital Content 12; http://links.lww.com/CORR/A452); percutaneous pinning (OR 0.09 [95% CI < 0.01 to 5.3]; SUCRA 0.83) was ranked the highest by the network. In the extraarticular subgroup (16 RCTs), there was no difference in the risk of complications requiring operation between any surgical intervention and nonoperative treatment; intramedullary fixation (OR 0.02 [95% CI < 0.01 to 2.7]; SUCRA 0.79) was ranked the highest (Table 4). After excluding studies exclusively enrolling patients older than 60 years of age (43 RCTs remaining), all interventions except dorsal plating [40, 56, 57] and dynamic external fixation were associated with a lower risk of complications requiring operation than nonoperative treatment (Supplemental Digital Content 13; http://links.lww.com/CORR/A453). In this subgroup, nonbridging external fixation (OR 0.01 [95% CI < 0.01 to 0.10]; SUCRA 0.94) was ranked the highest. In the subgroup of studies with an average patient age older than 60 years (22 RCTs), no treatment was associated with a lower risk of complications requiring surgery than nonoperative treatment (Table 4); bridging external fixation (OR 0.03 [95% CI < 0.01 to 3.5]; SUCRA 0.84) was ranked the highest. Sensitivity analysis demonstrated that including studies with less than 1 year of follow-up did not influence findings.
Table 4.
GRADE summary table for risk of complications requiring operation
| Group | Rank | Intervention | Odds ratio (95% CI) | NNT | Quality of evidence |
| All patients | 1 | Intramedullary fixation | 0.06 (< 0.01 to 0.85)a | 7 | Lowb,c |
| 2 | Volar locking plate | 0.17 (0.02 to 1.04) | 7 | Moderateb | |
| 3 | Nonbridging external fixation | 0.01 (< 0.01 to 0.25)a | 7 | Lowb,d | |
| 4 | Bridging external fixation | 0.08 (< 0.01 to 0.60)a | 7 | Lowd,e | |
| 5 | Percutaneous pinning | 0.07 (< 0.01 to 0.60)a | 7 | Moderated | |
| Intraarticular | 1 | Percutaneous pinning | 0.09 (< 0.01 to 5.3) | 6 | Very lowd,f |
| 2 | Bridging external fixation | 0.17 (< 0.01 to 7.2) | 6 | Very lowd,e,f | |
| Extraarticular | 1 | Intramedullary fixation | 0.02 (< 0.01 to 2.7) | 11 | Lowf |
| 2 | Bridging external fixation | 0.10 (< 0.01 to 4.5) | 12 | Very lowd,f | |
| Average age older than 60 years | 1 | Bridging external fixation | 0.03 (< 0.01 to 3.5) | 7 | Lowf |
| 2 | Intramedullary fixation | 0.16 (< 0.01 to 11) | 8 | Very lowc,f |
Inferred to be statistically significant with a 95% CI for mean difference not crossing zero.
Downgraded for imprecision.
Downgraded for indirectness.
Downgraded for inconsistency.
Downgraded for risk of bias.
Downgraded two levels for imprecision.
Odds ratios are relative to nonoperative treatment; rank based on SUCRA value; small sample size was considered in the evaluation of imprecision; GRADE = Grading of Recommendations Assessment, Development and Evaluation; NNT = number needed to treat.
Discussion
The treatment of DRFs remains an area of controversy with many uncertainties, despite the publication of numerous RCTs and meta-analyses. Clinical practice guidelines are inconclusive regarding preferred treatment, partly because of the wide range of accepted treatment options. In this situation, the ability to simultaneously compare multiple treatment arms is advantageous. Therefore, the aim of this study was to conduct an NMA of all available RCT evidence on the treatment of DRFs. We found that overall, there were no clinically important differences in terms of the DASH score at 1 year among all the surgical treatment options; although differences were found, all were less than the MCID of 10 points. Relative to the other options, volar plating was associated with a lower complication risk, particularly in patients with intraarticular fractures, while nonbridging external fixation was associated with a lower complication risk in patients with extraarticular fractures. For patients older than 60 years, nonoperative treatment may still be the preferred option because there is no reliable evidence showing a consistent decrease in complications or complications requiring operation among the other treatment options.
Limitations
Although an NMA can be a powerful tool, care must be taken when interpreting findings. The reliability of findings is largely determined by the volume of evidence for each treatment and the number of intertreatment comparisons [85]. For treatments with small sample sizes, inferences are driven by relatively few comparisons and are therefore lower quality, regardless of the total size of the network [85, 130]; many quality-of-evidence evaluations were downgraded for this reason. Regarding subgroups, prospectively planned subgroup analyses are considered more robust than retrospectively planned analyses [116]. For this analysis, the subgroup of studies with an average patient age older than 60 years was used because there was an insufficient number of studies exclusively on elderly patients. It was not planned a priori and therefore findings from this subgroup may be at greater risk of bias. Further, this subgroup can, at best, act as a weak proxy, because patients younger than 60 years were included by necessity. The confidence in conclusions from this subgroup should be low and used primarily for generating hypotheses rather than making treatment decisions. Conducting an NMA assumes transitivity, or in the case of surgical treatment for DRF, that interventions have the same indications and can be equally randomized. In certain instances, this assumption is only weakly held. Several interventions included in the present network may have different indications. For example, intramedullary fixation is used more often in patients with extraarticular fractures while dorsal plating [40, 56, 57] is used more often in patients with intraarticular fractures. Conclusions drawn from the entire body of evidence may be influenced by confounding variables that are no longer randomized, and readers should have low confidence in these findings. Subgroups with common treatment indications (age and fracture pattern) are less likely to suffer from this limitation; therefore, network findings may be more reliable.
It is important to consider the sample size underlying each treatment and comparison. Sample size is part of the quality of evidence determination and contributes to imprecision according to GRADE methodology. In several instances, evidence quality was downgraded specifically due to small samples. Findings with low quality evidence are highly likely to be influenced by further research in the form of appropriately powered RCTs. The final notable limitation is the inclusion of studies with follow-up of 3 months (7% [5 of 70 studies]) and six months (14% [10 of 70 studies]). Sensitivity analysis demonstrated that inclusion of these studies did not influence our qualitative results. However, inclusion of these studies may influence the treatment effect size through a small over-representation of short-term complications (such as, infection, neuropathy) over long-term complications (including nonunion, posttraumatic arthritis) [29].
Functional Outcomes (DASH Score) at 1 Year
Across all subgroups, we found no clinically meaningful differences in the DASH score at 1-year between any treatment options. Volar plating, a top-ranked intervention across all subgroups, has previously been associated with improved long-term outcomes over other treatment options, although subsequent studies have found these improvements to be clinically unimportant [17, 25, 34, 136]. Despite being clinically unimportant to the average patient (demonstrated by our study subgroups), some patients may still see a benefit based on variables not accounted for within our broad subgroups. Our findings expand on the existing literature, suggesting that surgical management is unlikely to result in noticeable long-term improvement for most patients relative to nonoperative management, regardless of fracture pattern (that is, intraarticular versus extraarticular) or patient age. However, volar plating has been shown to result in clinically meaningful short-term functional improvements, and this potential benefit should be discussed with patients [34, 98]. Seven studies reported upper extremity functional scores other than DASH (the Mayo Wrist Score, Michigan Hand Questionnaire, and the patient-rated wrist evaluation) and were excluded from the functional analysis. These studies represent a small proportion of total patients, and therefore excluding them is unlikely to substantially influence our findings.
Complications
Across all patients, we found many surgical treatments reduced the complication risk relative to nonoperative treatment, however, the quality of evidence was generally low. In patients with intraarticular fractures, volar plating was associated with a lower complication risk. This finding is consistent with past analyses (which pooled fracture types) and may contribute to a preference for volar plating [105, 136]. Interestingly, we found no surgical treatment was associated with a lower complication risk in older patients. Previous analysis has demonstrated that surgery may in fact be associated with an increased complication risk in this population [9, 28, 124]. Considering this information and our own findings, the benefit of performing surgery in this patient population should be questioned.
Risk of Complications Requiring Operation
We found that most surgical treatment options reduced the risk of complications requiring reoperation when compared with nonoperative management across all patients. However, when analyzed by subgroup, we found no differences between any surgical treatment and nonoperative management. Interestingly, results from our analysis and others showing no difference between treatments differs from large registry data [4, 91, 113]. In a recent registry study of more than 36,000 patients with a mean follow-up of 4.2 years, treatment with a volar locking plate was associated with a greater risk of complications requiring reoperation than external fixation or percutaneous pinning [91]. It may be that most RCTs, and thus meta-analyses, are underpowered and/or have inadequate follow-up to capture differences in reoperation. With respect to patients of advanced age, our findings and the existing literature suggest that surgical intervention, regardless of type, does not reduce the risk of needing further surgery [76]. Therefore, avoiding initial operative management in favor of late intervention, only if necessary, may reduce the overall burden of surgery in these patients.
Conclusion
We found no clinically important differences favoring any surgical treatment option for 1-year functional outcome. However, volar plating was associated with a lower complication risk, particularly in patients with intraarticular fractures, while nonbridging external fixation was associated with a lower complication risk in patients with extraarticular fractures. For patients older than 60 years of age, nonoperative treatment may still be the preferred option because there is no reliable evidence showing a consistent decrease in complications or complications requiring operation among the other treatment options. Particularly in this age group, the decision to expose patients to even a single surgery should be made with caution.
Supplementary Material
Acknowledgments
The authors thank Gwendolyn Lovsted for her time and expertise designing and editing the figures found throughout this manuscript.
Footnotes
Each author certifies that neither he nor she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution waived approval for the reporting of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Division of Orthopaedic Surgery, McMaster University, Hamilton, ON, Canada.
References
- 1.Abbaszadegan H, Jonsson U. External fixation or plaster cast for severely displaced Colles’ fractures: prospective 1-year study of 46 patients. Acta Orthop Scand. 1990;61:528-530. [DOI] [PubMed] [Google Scholar]
- 2.Abramo A, Kopylov P, Geijer M, Tägil M. Open reduction and internal fixation compared to closed reduction and external fixation in distal radial fractures: a randomized study of 50 patients. Acta Orthop. 2009;80:478-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aita MA, Ferreira CH, Schneider Ibanez D, et al. Randomized clinical trial on percutaneous minimally invasive osteosynthesis of fractures of the distal extremity of the radius. Rev Bras Ortop. 2014;49:218-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anderson MS, Ghamsary M, Guillen PT, Wongworawat MD. Outcomes after distal radius facture treatment with percutaneous wire versus plate fixation: meta-analysis of randomized controlled trials. J Surg Orthop Adv. 2017;26:7-17. [PubMed] [Google Scholar]
- 5.Arora J, Kapoor H, Malik A, Bansal M. Closed reduction and plaster cast immobilization vs. external fixation in comminuted intraarticular fractures of distal radius. Indian J Orthop. 2004;38:113. [Google Scholar]
- 6.Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg. 2011;93:2146-2153. [DOI] [PubMed] [Google Scholar]
- 7.Atroshi I, Brogren E, Larsson GU, Kloow J, Hofer M, Berggren AM. Wrist-bridging versus non-bridging external fixation for displaced distal radius fractures: a randomized assessor-blind clinical trial of 38 patients followed for 1 year. Acta Orthop. 2006;77:445-453. [DOI] [PubMed] [Google Scholar]
- 8.Azad A, Kang HP, Alluri RK, Vakhshori V, Kay HF, Ghiassi A. Epidemiological and treatment trends of distal radius fractures across multiple age groups. J Wrist Surg. 2019;08:305-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azzopardi T, Ehrendorfer S, Coulton T, Abela M. Unstable extraarticular fractures of the distal radius: a prospective, randomised study of immobilisation in a cast versus supplementary percutaneous pinning. J Bone Joint Surg. 2005;87:837-840. [DOI] [PubMed] [Google Scholar]
- 10.Bahari-Kashani M, Taraz-Jamshidy MH, Rahimi H, et al. Outcomes of pin and plaster versus locking plate in distal radius intraarticular fractures. Trauma Mon. 2013;17:380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bartl C, Stengel D, Gebhard F, Bruckner T, ORCHID SG. The treatment of displaced Intraarticular distal radius fractures in elderly patients: a Randomized Multi-center Study (ORCHID) of open reduction and volar locking plate fixation versus closed reduction and cast immobilization. Dtsch Arztebl Int. 2014;111:779.25491556 [Google Scholar]
- 12.Belloti JC, Tamaoki MJ, Atallah AN, Albertoni WM, dos Santos JB, Faloppa F. Treatment of reducible unstable fractures of the distal radius in adults: a randomised controlled trial of De Palma percutaneous pinning versus bridging external fixation. BMC Musculoskelet Disord. 2010;11:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bisneto EN, de Paula EJ, de Resende MR, Júnior RM, Zumiotti AV. Distal radial fractures in patients over 60 years old: orthogonal plates versus volar plate. Rev Bras Ortop. 2010;45:590-595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.British Orthopaedic Association and British Society for Surgery of the Hand. Clinical practice guideline on best practice for management of distal radial fractures (DRFs). 2018. Available at: https://www.bssh.ac.uk/professionals/management_of_distal_radial_fractures.aspx. Accessed April 15, 2019.
- 15.Chappuis J, Boute P, Putz P. Dorsally displaced extraarticular distal radius fractures fixation: dorsal IM nailing versus volar plating. A randomized controlled trial. Orthop Traumatol Surg Res. 2011;97:471-478. [DOI] [PubMed] [Google Scholar]
- 16.Chaudhry H, Foote CJ, Guyatt G, et al. Network meta-analysis: users’ guide for surgeons: part II – certainty. Clin Orthop Relat Res. 2015;473:2172-2178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chaudhry H, Kleinlugtenbelt YV, Mundi R, Ristevski B, Goslings JC, Bhandari M. Are volar locking plates superior to percutaneous K-wires for distal radius fractures? A meta-analysis. Clin Orthop Relat Res. 2015;473:3017-3027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CINeMA: Confidence in network meta-analysis. Available at: cinema.ispm.unibe.ch. Accessed September 1, 2019.
- 19.Costa ML, Achten J, Parsons NR, et al. Percutaneous fixation with Kirschner wires versus volar locking plate fixation in adults with dorsally displaced fracture of distal radius: randomised controlled trial. BMJ. 2014;349:g4807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cui Z, Yu B, Hu Y, Lin Q, Wang B. Dynamic versus static external fixation for unstable distal radius fractures: an up-to-date meta-analysis. Injury. 2012;43:1006–1013. [DOI] [PubMed] [Google Scholar]
- 21.Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29:932-944. [DOI] [PubMed] [Google Scholar]
- 22.Diaz-Garcia RJ, Oda T, Shauver MJ, Chung KC. A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. J Hand Surg. 2011;36:824-835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Drobetz H, Koval L, Weninger P, et al. Volar locking distal radius plates show better short-term results than other treatment options: a prospective randomised controlled trial. World J Orthop. 2016;7:687-694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Egol K, Walsh M, Tejwani N, McLaurin T, Wynn C, Paksima N. Bridging external fixation and supplementary Kirschner-wire fixation versus volar locked plating for unstable fractures of the distal radius: a randomised, prospective trial. J Bone Joint Surg Br. 2008;90:1214-1221. [DOI] [PubMed] [Google Scholar]
- 25.Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92:1851-1857. [DOI] [PubMed] [Google Scholar]
- 26.Esposito J, Schemitsch EH, Saccone M, Sternheim A, Kuzyk PRT. External fixation versus open reduction with plate fixation for distal radius fractures: a meta-analysis of randomised controlled trials. Injury. 2013;44:409-416. [DOI] [PubMed] [Google Scholar]
- 27.Földhazy Z, Ahrengart L. External fixation versus closed treatment of displaced distal radial fractures in elderly patients: a randomized controlled trial. Curr Orthop Pract. 2010;21:288-295. [Google Scholar]
- 28.Foote CJ, Chaudhry H, Bhandari M, et al. Network meta-analysis: users’ guide for surgeons: part I – credibility. Clin Orthop Relat Res. 2015;473:2166-2171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Forward DP, Davis TRC, Sithole JS. Do young patients with malunited fractures of the distal radius inevitably develop symptomatic post-traumatic osteoarthritis? J Bone Joint Surg Br. 2008;90:629-637. [DOI] [PubMed] [Google Scholar]
- 30.Franceschi F, Franceschetti E, Paciotti M, Cancilleri F, Maffulli N, Denaro V. Volar locking plates versus K-wire/pin fixation for the treatment of distal radial fractures: a systematic review and quantitative synthesis. Br Med Bull . 2015;115:91-110. [DOI] [PubMed] [Google Scholar]
- 31.Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (quickDASH). J Orthop Sports Phys Ther. 2014;44:30-39. [DOI] [PubMed] [Google Scholar]
- 32.Fu Q, Zhu L, Yang P, Chen A. Volar locking plate versus external fixation for distal radius fractures: a meta-analysis of randomized controlled trials. Indian J Orthop 2018;52:602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goehre F, Otto W, Schwan S, Mendel T, Vergroesen PP, Lindemann-Sperfeld L. Comparison of palmar fixed-angle plate fixation with K-wire fixation of distal radius fractures (AO A2, A3, C1) in elderly patients. J Hand Surg Eur Vol. 2014;39:249-257. [DOI] [PubMed] [Google Scholar]
- 34.Gouk CJC, Bindra RR, Tarrant DJ, Thomas MJE. Volar locking plate fixation versus external fixation of distal radius fractures: a meta-analysis. J Hand Surg Eur . 2018;43:954-960. [DOI] [PubMed] [Google Scholar]
- 35.Gradl G, Falk S, Mittlmeier T, Wendt M, Mielsch N, Gradl G. Fixation of intraarticular fractures of the distal radius using intramedullary nailing: a randomized trial versus palmar locking plates. Injury. 2016;47:S25-30. [DOI] [PubMed] [Google Scholar]
- 36.Gradl G, Mielsch N, Wendt M, et al. Intramedullary nail versus volar plate fixation of extraarticular distal radius fractures. Two year results of a prospective randomized trial. Injury. 2014;45:S3-8. [DOI] [PubMed] [Google Scholar]
- 37.Gradl G, Wendt M, Mittlmeier T, Kundt G, Jupiter JB. Non-bridging external fixation employing multiplanar K-wires versus volar locked plating for dorsally displaced fractures of the distal radius. Arch Orthop Trauma Surg. 2013;133:595-602. [DOI] [PubMed] [Google Scholar]
- 38.Greco T, Biondi-Zoccai G, Saleh O, et al. The attractiveness of network meta-analysis: a comprehensive systematic and narrative review. Heart Lung Vessel. 2015;7:133-142. [PMC free article] [PubMed] [Google Scholar]
- 39.Grewal R, MacDermid JC, King GJ, Faber KJ. Open reduction internal fixation versus percutaneous pinning with external fixation of distal radius fractures: a prospective, randomized clinical trial. J Hand Surg. 2011;36:1899-1906. [DOI] [PubMed] [Google Scholar]
- 40.Grewal R, Perey B, Wilmink M, Stothers K. A randomized prospective study on the treatment of intraarticular distal radius fractures: open reduction and internal fixation with dorsal plating versus mini open reduction, percutaneous fixation, and external fixation. J Hand Surg. 2005;30:764-72. [DOI] [PubMed] [Google Scholar]
- 41.Gu W-L, Wang J, Li D-Q, et al. Bridging external fixation versus non-bridging external fixation for unstable distal radius fractures: a systematic review and meta-analysis. J Orthop Sci. 2016;21:24–31. [DOI] [PubMed] [Google Scholar]
- 42.Gupta R, Raheja A, Modi U. Colles' fracture: management by percutaneous crossed-pin fixation versus plaster of Paris cast immobilization. Orthopedics. 1999;22:680-682. [PubMed] [Google Scholar]
- 43.Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol. 2011;64:380-382. [DOI] [PubMed] [Google Scholar]
- 44.Harley BJ, Scharfenberger A, Beaupre LA, Jomha N, Weber DW. Augmented external fixation versus percutaneous pinning and casting for unstable fractures of the distal radius—a prospective randomized trial. J Hand Surg. 2004;29:815-824. [DOI] [PubMed] [Google Scholar]
- 45.Hegeman JH, Oskam J, Van Der Palen J, Ten Duis HJ, Vierhout PA. Primary external fixation versus plaster immobilization of the intraarticular unstable distal radial fracture in the elderly. Aktuelle Traumatol. 2004;34:64-70. [Google Scholar]
- 46.Higgins J, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1.0. Cochrane Collaboration. Available at: https://training.cochrane.org/handbook/current. Accessed September 1, 2019.
- 48.Higgins J, Green S. Obtaining standard deviations from standard errors and confidence intervals for group means. Cochrane Handbook for Systematic Reviews of Interventions. Available at: https://training.cochrane.org/handbook/current/chapter-06. Accessed September 1, 2019.
- 49.Hollevoet N, Vanhoutie T, Vanhove W, Verdonk R. Percutaneous K-wire fixation versus palmar plating with locking screws for Colles' fractures. Acta Orthop Belg. 2011;77:180. [PubMed] [Google Scholar]
- 50.Horne JG, Devane P, Purdie G. A prospective randomized trial of external fixation and plaster cast immobilization in the treatment of distal radial fractures. J Orthop Trauma. 1990;4:30-34. [DOI] [PubMed] [Google Scholar]
- 51.Hove LM, Krukhaug Y, Revheim K, Helland P, Finsen V. Dynamic compared with static external fixation of unstable fractures of the distal part of the radius: a prospective, randomized multicenter study. J Bone Joint Surg. 2010;92:1687-1696. [DOI] [PubMed] [Google Scholar]
- 52.Howard PW, Stewart HD, Hind RE, Burke FD. External fixation or plaster for severely displaced comminuted Colles' fractures? A prospective study of anatomical and functional results. J Bone Joint Surg Br. 1989;71:68-73. [DOI] [PubMed] [Google Scholar]
- 53.Hudak PL, Amadio PC, Bombardier C, et al. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder, and hand). Am J Ind Med. 1996;29:602-608. [DOI] [PubMed] [Google Scholar]
- 54.Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162:777. [DOI] [PubMed] [Google Scholar]
- 55.Ismatullah Efficacy of plaster casting versus external fixation in comminuted distal radius fractures. J Postgrad Med Inst. 2012;26:311-316. [Google Scholar]
- 56.Jakubietz MG, Gruenert JG, Jakubietz RG. Palmar and dorsal fixed-angle plates in AO C-type fractures of the distal radius: is there an advantage of palmar plates in the long term? J Orthop Surg Res. 2012;7:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jakubietz RG, Gruenert JG, Kloss DF, Schindele S, Jakubietz MG. A randomised clinical study comparing palmar and dorsal fixed-angle plates for the internal fixation of AO C-type fractures of the distal radius in the elderly. J Hand Surg Eur Vol 2008;33:600-604. [DOI] [PubMed] [Google Scholar]
- 58.Jansen JP, Crawford B, Bergman G, Stam W. Bayesian meta-analysis of multiple treatment comparisons: an introduction to mixed treatment comparisons. Value Health. 2008;11:956-964. [DOI] [PubMed] [Google Scholar]
- 59.Jeudy J, Steiger V, Boyer P, Cronier P, Bizot P, Massin P. Treatment of complex fractures of the distal radius: a prospective randomised comparison of external fixation ‘versus’ locked volar plating. Injury. 2012;43:174-179. [DOI] [PubMed] [Google Scholar]
- 60.Karantana A, Downing ND, Forward DP, et al. Surgical treatment of distal radial fractures with a volar locking plate versus conventional percutaneous methods: a randomized controlled trial. J Bone Joint Surg. 2013;95:1737-1744. [DOI] [PubMed] [Google Scholar]
- 61.Kopylov P, Aspenberg P, Yuan X, Ryd L. Radiostereometric analysis of distal radius fracture displacement during treatment: a randomized study comparing Norian SRS and external fixation in 23 patients. Acta Orthop Scand . 2009; 72:57-61. [DOI] [PubMed] [Google Scholar]
- 62.Kopylov P, Runnqvist K, Jonsson K, Aspenberg P. Norian SRS versus external fixation in redisplaced distal radial fractures: a randomized study in 40 patients. Acta Orthop Scand. 1999;70:1-5. [DOI] [PubMed] [Google Scholar]
- 63.Koshimune M, Kamano M, Takamatsu K, Ohashi H. A randomized comparison of locking and non-locking palmar plating for unstable Colles’ fractures in the elderly. J Hand Surg Br. 2005;30:499-503. [DOI] [PubMed] [Google Scholar]
- 64.Koval K, Haidukewych GJ, Service B, Zirgibel BJ. Controversies in the management of distal radius fractures. J Am Acad Orthop Surg. 2014;22:566-575. [DOI] [PubMed] [Google Scholar]
- 65.Krishnan J, Wigg AE, Walker RW, Slavotinek J. Intraarticular fractures of the distal radius: a prospective randomised controlled trial comparing static bridging and dynamic non-bridging external fixation. J Hand Surg. 2003;28:417-421. [DOI] [PubMed] [Google Scholar]
- 66.Kristman V, Manno M, Côté P. Loss to follow-up in cohort studies: how much is too much. Eur J Epidemiol. 2004;19:751-760. [DOI] [PubMed] [Google Scholar]
- 67.Krukhaug Y, Ugland S, Lie SA, Hove LM. External fixation of fractures of the distal radius: a randomized comparison of the Hoffman compact II non-bridging fixator and the Dynawrist fixator in 75 patients followed for 1 year. Acta Orthop. 2009;80:104-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kulshrestha V, Roy T, Audige L. Dynamic vs static external fixation of distal radial fractures: a randomized study. Indian J Orthop. 201;45:527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Kumar K, Laghari MA, Bhutto IA, Lal K. Fracture of distal radius treated by Orthofix v/s plaster cast. J Liaquat Uni Med Health Sc. 2014;13:120-124. [Google Scholar]
- 70.Landgren M, Abramo A, Geijer M, Kopylov P, Tägil M. Fragment-specific fixation versus volar locking plates in primarily nonreducible or secondarily redisplaced distal radius fractures: a randomized controlled study. J Hand Surg. 2017;42:156-165. [DOI] [PubMed] [Google Scholar]
- 71.Landgren M, Jerrhag D, Tägil M, Kopylov P, Geijer M, Abramo A. External or internal fixation in the treatment of non-reducible distal radial fractures? A 5-year follow-up of a randomized study involving 50 patients. Acta Orthop. 2011;82:610-613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lenoble E, Dumontier C, Goutallier D, Apoil A. Fracture of the distal radius. A prospective comparison between trans-styloid and Kapandji fixations. J Bone Joint Surg Br. 1995;77:562-567. [PubMed] [Google Scholar]
- 73.Lichtman DM, Bindra RR, Boyer MI, et al. Treatment of distal radius fractures. J Am Acad Orthop Surg. 2010;18:180-189. [DOI] [PubMed] [Google Scholar]
- 74.Li-hai Z, Ya-nan W, Zhi M, et al. Volar locking plate versus external fixation for the treatment of unstable distal radial fractures: a meta-analysis of randomized controlled trials. J Surg Res. 2015;193:324-333. [DOI] [PubMed] [Google Scholar]
- 75.Ludvigsen TC, Johansen S, Svenningsen S, Saetermo R. External fixation versus percutaneous pinning for unstable Colles' fracture: Equal outcome in a randomized study of 60 patients. Acta Orthop Scand. 1997;68:255-258. [DOI] [PubMed] [Google Scholar]
- 76.Lutz K, Yeoh KM, MacDermid JC, Symonette C, Grewal R. Complications associated with operative versus nonsurgical treatment of distal radius fractures in patients aged 65 years and older. J Hand Surg. 2014;39:1280-1286. [DOI] [PubMed] [Google Scholar]
- 77.Ma J, Liu W, Hunter A, Zhang W. Performing meta-analysis with incomplete statistical information in clinical trials. BMC Med Res Methodol. 2008;8:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.MacIntyre NJ, Dewan N. Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther. 2016;29:136-145. [DOI] [PubMed] [Google Scholar]
- 79.Marcheix PS, Dotzis A, Benkö PE, Siegler J, Arnaud JP, Charissoux JL. Extension fractures of the distal radius in patients older than 50: a prospective randomized study comparing fixation using mixed pins or a palmar fixed-angle plate. J Hand Surg Eur. 2010;35:646-651. [DOI] [PubMed] [Google Scholar]
- 80.Mardani M, Asadi K, Hashemi-Motlagh K, Shakiba M. Distal radius fracture, a comparison between closed reduction and long arm cast vs. closed reduction and percutaneous pinning and short arm cast. Shiraz E Med J. 2011;12:155-161. [Google Scholar]
- 81.Martinez-Mendez D, Lizaur-Utrilla A, de-Juan-Herrero J. Intraarticular distal radius fractures in elderly patients: a randomized prospective study of casting versus volar plating. J Hand Surg Eur. 2018;43:142-147. [DOI] [PubMed] [Google Scholar]
- 82.McFadyen I, Field J, McCann P, Ward J, Nicol S, Curwen C. Should unstable extraarticular distal radial fractures be treated with fixed-angle volar-locked plates or percutaneous Kirschner wires? A prospective randomised controlled trial. Injury. 2011;42:162-166. [DOI] [PubMed] [Google Scholar]
- 83.McQueen MM. Redisplaced unstable fractures of the distal radius: a randomised, prospective study of bridging versus non-bridging external fixation J Bone Joint Surg Br. 1998;80:665-669. [DOI] [PubMed] [Google Scholar]
- 84.McQueen MM, Hajducka C, Court-Brown CM. Redisplaced unstable fractures of the distal radius: a prospective randomised comparison of four methods of treatment. J Bone Joint Surg Br. 1996;78:404-409. [PubMed] [Google Scholar]
- 85.Mills EJ, Thorlund K, Ioannidis JPA. Demystifying trial networks and network meta-analysis. BMJ. 2013;346:f2914-f2914. [DOI] [PubMed] [Google Scholar]
- 86.Modi CS, Ho K, Smith CD, Boer R, Turner SM. Dynamic and static external fixation for distal radius fractures—a systematic review. Injury. 2010;41:1006-1011. [DOI] [PubMed] [Google Scholar]
- 87.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535-b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Moroni A, Vannini F, Faldini C, Pegreffi F, Giannini S. Cast vs external fixation: a comparative study in elderly osteoporotic distal radial fracture patients. Scand J Surg. 2004;93:64-67. [DOI] [PubMed] [Google Scholar]
- 89.Mulders MA, Walenkamp MM, van Dieren S, Goslings JC, Schep NW. Volar plate fixation versus plaster immobilization in acceptably reduced extraarticular distal radial fractures: a multicenter randomized controlled trial. J Bone Joint Surg. 2019;101:787-796. [DOI] [PubMed] [Google Scholar]
- 90.Navarro CM, Ahrengart L, Törnqvist H, Ponzer S. Volar locking plate or external fixation with optional addition of K-wires for dorsally displaced distal radius fractures: a randomized controlled study. J Orthop Trauma. 2016;30:217-224. [DOI] [PubMed] [Google Scholar]
- 91.Navarro CM, Pettersson HJ, Enocson A. Complications after distal radius fracture surgery: results from a Swedish nationwide registry study. J Orthop Trauma. 2015;29:e36-42. [DOI] [PubMed] [Google Scholar]
- 92.Peng F, Liu Y, Wan Z. Percutaneous pinning versus volar locking plate internal fixation for unstable distal radius fractures: a meta-analysis. J Hand Surg Eur. 2018;43:158-167. [DOI] [PubMed] [Google Scholar]
- 93.Pinto RZ, Maher CG, Ferreira ML, et al. Drugs for relief of pain in patients with sciatica: systematic review and meta-analysis. BMJ. 2012;344:e497-e497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Plate JF, Gaffney DL, Emory CL, et al. Randomized comparison of volar locking plates and intramedullary nails for unstable distal radius fractures. J Hand Surg. 2015;40:1095-1101. [DOI] [PubMed] [Google Scholar]
- 95.Prada C, Chang Y, Poolman R, Johal H, Bhandari M. Best practices for surgeons: COVID-19 evidence-based scoping review. OrthoEvidence. Available at: https://myoe.blob.core.windows.net/docs/OE-Best-Practices-for-Surgeons-COVID-19-Evidence-Based-Scoping-Review.pdf. Accessed April 15, 2020. [Google Scholar]
- 96.Pritchett JW. External fixation or closed medullary pinning for unstable Colles fractures? J Bone Joint Surg Br. 1995;77:267-269. [PubMed] [Google Scholar]
- 97.Puhan MA, Schunemann HJ, Murad MH, et al. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630-g5630. [DOI] [PubMed] [Google Scholar]
- 98.Qu S, Zhang B, Shang K, et al. The efficacy of volar locking plates and external fixation for patients with unstable distal radial fractures: a meta-analysis. Int J Clin Exp Med. 2019;12:2097–2106. [Google Scholar]
- 99.Rahman O, Khan MQ, Rasheed H, Ahmad S. Treatment of unstable intraarticular fracture of distal radius: POP casting with external fixation. J Pak Med Assoc. 2012;62:358. [PubMed] [Google Scholar]
- 100.Rodríguez-Merchán EC. Plaster cast versus percutaneous pin fixation for comminuted fractures of the distal radius in patients between 46 and 65 years of age. J Orthop Trauma. 1997;11:212-217. [DOI] [PubMed] [Google Scholar]
- 101.Roh YH, Lee BK, Baek JR, Noh JH, Gong HS, Baek GH. A randomized comparison of volar plate and external fixation for intraarticular distal radius fractures. J Hand Surg. 2015;40:34-41. [DOI] [PubMed] [Google Scholar]
- 102.Rozental TD, Blazar PE, Franko OI, Chacko AT, Earp BE, Day CS. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:1837-1846. [DOI] [PubMed] [Google Scholar]
- 103.Saddiki R, Ohl X, Hemery X, Vitry F, Dehoux E, Harisboure A. Dorsally displaced distal radius fractures: comparative study of Py's and Kapandji's techniques. Orthop Trauma Surg Res. 2012;98:61-67. [DOI] [PubMed] [Google Scholar]
- 104.Safi A, Hart R, Těknědžjan B, Kozák T. Treatment of extraarticular and simple articular distal radial fractures with intramedullary nail versus volar locking plate. J Hand Surg Eur. 2013;38:774-779. [DOI] [PubMed] [Google Scholar]
- 105.Salibian A, Bruckman K, Bekisz J, Mirrer J, Thanik V, Hacquebord J. Management of unstable distal radius fractures: a survey of hand surgeons. J Wrist Surg. 2018;08:335-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Saving J, Wahlgren SS, Olsson K, et al. Nonoperative treatment compared with volar locking plate fixation for dorsally displaced distal radial fractures in the elderly: a randomized controlled trial. J Bone Joint Surg. 2019;101:961-969. [DOI] [PubMed] [Google Scholar]
- 107.Schønnemann JO, Hansen TB, Søballe K. Randomised study of non-bridging external fixation compared with intramedullary fixation of unstable distal radial fractures. J Plast Surg Hand Surg. 2011;45:232-237. [DOI] [PubMed] [Google Scholar]
- 108.Shao J, Kong D, Yang T. Volar locking plate fixation versus kirschner wire fixation in distal radius fractures: a meta-analysis. Int J Clin Exp Med 2016;9:16230–16235. [Google Scholar]
- 109.Shen L, Wen M, Wang F. Volar locking plate versus percutaneous fixation for the treatment of distal radial fractures: a meta-analysis of randomized controlled trials. Int J Clin Exp Med 2016;9:7780-7793. [Google Scholar]
- 110.Sirniö K, Leppilahti J, Ohtonen P, Flinkkilä T. Early palmar plate fixation of distal radius fractures may benefit patients aged 50 years or older: a randomized trial comparing 2 different treatment protocols. Acta Orthop. 2019;90:123-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sommerkamp TG, Seeman M, Silliman J, et al. Dynamic external fixation of unstable fractures of the distal part of the radius. A prospective, randomized comparison with static external fixation. J Bone Joint Surg Am. 1994;76:1149-1161. [DOI] [PubMed] [Google Scholar]
- 112.Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am. 2013;38:641-649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Stinner DJ, Lebrun C, Hsu J, Jahangir AA, Mir H. The orthopaedic trauma service and COVID-19 – practice considerations to optimize outcomes and limit exposure. J Orthop Trauma. 2020;34:333-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Stoffelen DV, Broos PL. Kapandji pinning or closed reduction for extraarticular distal radius fractures. J Trauma. 1998;45:753-757. [DOI] [PubMed] [Google Scholar]
- 115.Strohm PC, Müller CA, Boll T, Pfister U. Two procedures for Kirschner wire osteosynthesis of distal radial fractures: a randomized trial. J Bone Joint Surg. 2004;86:2621-2628. [DOI] [PubMed] [Google Scholar]
- 116.Sun X, Briel M, Busse JW, et al. Credibility of claims of subgroup effects in randomised controlled trials: systematic review. BMJ. 2012;344:e1553. [DOI] [PubMed] [Google Scholar]
- 117.Tanaka H, Hatta T, Sasajima K, Itoi E, Aizawa T. Comparative study of treatment for distal radius fractures with two different palmar locking plates. J Hand Surg Eur. 2016;41:536-542. [DOI] [PubMed] [Google Scholar]
- 118.van de Schoot R, Broere JJ, Perryck KH, Zondervan-Zwijnenburg M, van Loey NE. Analyzing small data sets using Bayesian estimation: the case of posttraumatic stress symptoms following mechanical ventilation in burn survivors. Eur J Psychotraumatol. 2015;6:25216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Vannabouathong C, Hussain N, Guerra-Farfan E, Bhandari M. Interventions for distal radius fractures: a network meta-analysis of randomized trials. J Am Acad Orthop Surg. 2019;27:e596–e605. [DOI] [PubMed] [Google Scholar]
- 120.Venkatesh RB, Maranna GK, Narayanappa RK. A comparative study between closed reduction and cast application versus percutaneous k-wire fixation for extraarticular fracture distal end of radius. J Clin Diagn Res. 2016;10:RC05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wang J-H, Sun T. Comparison of effects of seven treatment methods for distal radius fracture on minimizing complex regional pain syndrome. Arch Med Sci. 2017;1:163–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wang J, Lu Y, Cui Y, Wei X, Sun J. Is volar locking plate superior to external fixation for distal radius fractures? A comprehensive meta-analysis. Acta Orthop Traumatol Turc. 2018;52:334–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wang J, Yang Y, Ma J, et al. Open reduction and internal fixation versus external fixation for unstable distal radial fractures: a meta-analysis. Orthop Traumatol Surg Res. 2013;99:321-331. [DOI] [PubMed] [Google Scholar]
- 124.Wang S, Liu M, Yang Q, et al. Safety and effectiveness of Kirschner wire and plate fixation for treating distal radial fracture in the elderly: a meta-analysis. Chinese J Tissue Eng Res. 2016;20:1361–1368. [Google Scholar]
- 125.Wei DH, Poolman RW, Bhandari M, Wolfe VM, Rosenwasser MP. External fixation versus internal fixation for unstable distal radius fractures. J Orthop Trauma. 2012;26:386-394. [DOI] [PubMed] [Google Scholar]
- 126.Wei DH, Raizman NM, Bottino CJ, Jobin CM, Strauch RJ, Rosenwasser MP. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate. J Bone Joint Surg Am . 2009;91:1568-1577. [DOI] [PubMed] [Google Scholar]
- 127.Wei J, Yang T-B, Luo W, Qin J-B, Kong F-J. Complications following dorsal versus volar plate fixation of distal radius fracture: a meta-analysis. J Int Med Res. 2013;41:265–275. [DOI] [PubMed] [Google Scholar]
- 128.Werber KD, Raeder F, Brauer RB, Weiss S. External fixation of distal radial fractures: four compared with five pins: a randomized prospective study. J Bone Joint Surg. 2003;85:660-666. [DOI] [PubMed] [Google Scholar]
- 129.Westphal T, Piatek S, Schubert S, Schuschke T, Winckler S. Reliability and validity of the upper limb DASH questionnaire in patients with distal radius fractures. Article in German. Z Orthop Ihre Grenzgeb. 2002;140:447-451. [DOI] [PubMed] [Google Scholar]
- 130.White IR, Barrett JK, Jackson D, Higgins JPT. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Res Synth Methods. 2012;3:111-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wilcke MK, Abbaszadegan H, Adolphson PY. Wrist function recovers more rapidly after volar locked plating than after external fixation but the outcomes are similar after 1 year: a randomized study of 63 patients with a dorsally displaced fracture of the distal radius. Acta Orthop. 2011;82:76-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Williksen JH, Frihagen F, Hellund JC, Kvernmo HD, Husby T. Volar locking plates versus external fixation and adjuvant pin fixation in unstable distal radius fractures: a randomized, controlled study. J Hand Surg. 2013;38:1469-1476. [DOI] [PubMed] [Google Scholar]
- 133.Wong TC, Chiu Y, Tsang WL, Leung WY, Yam SK, Yeung SH. Casting versus percutaneous pinning for extraarticular fractures of the distal radius in an elderly Chinese population: a prospective randomised controlled trial. J Hand Surg Eur. 2010;35:202-208. [DOI] [PubMed] [Google Scholar]
- 134.Xie X, Xie X, Qin H, Shen L, Zhang C. Comparison of internal and external fixation of distal radius fractures. Acta Orthop. 2013;84:286–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Yang Z, Yuan ZZ, Ma JX, Ma XL. Complications of open reduction and internal fixation versus external fixation for unstable distal radius fractures: a meta-analysis. Article in Chinese. Zhonghua Yi Xue Za Zhi. 2016;96:3833-3837. [DOI] [PubMed] [Google Scholar]
- 136.Youlden DJ, Sundaraj K, Smithers C. Volar locking plating versus percutaneous Kirschner wires for distal radius fractures in an adult population: a meta‐analysis. Anz J Surg . 2019;89:821-826. [DOI] [PubMed] [Google Scholar]
- 137.Yuan ZZ, Yang Z, Liu Q, Liu YM. Complications following open reduction and internal fixation versus external fixation in treating unstable distal radius fractures: grading the evidence through a meta-analysis. Orthop Traumatol Surg Res. 2018;104:95-103. [DOI] [PubMed] [Google Scholar]
- 138.Zehir S, Calbiyik M, Zehir R, Ipek D. Intramedullary repair device against volar plating in the reconstruction of extraarticular and simple articular distal radius fractures; a randomized pilot study. Int Orthop. 2014;38:1655-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Zhang B Chang H Yu K et al. Article. Intramedullary nail versus volar locking plate fixation for the treatment of extra-articular or simple intra-articular distal radius fractures: systematic review and meta-analysis. Int Orthop. 2017;41:2161-2169. [DOI] [PubMed] [Google Scholar]
- 140.Zong S-L, Kan S-L, Su L-X, Wang B. Meta-analysis for dorsally displaced distal radius fracture fixation: volar locking plate versus percutaneous Kirschner wires. J Orthop Surg Res. 2015;10:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


