ABSTRACT
Programs aimed at boosting human papillomavirus (HPV)-related awareness are considered one of the most effective strategies for increasing vaccination uptake and eliminating HPV-associated cancers. Several US states have made strong commitments to this effort through legislation and dedicated funds. However, it is not known if these efforts have resulted in population-level increments in HPV awareness overtime. Using the Health Information National Trends Survey data, we examined the awareness of HPV and HPV vaccine in the US, between 2008 and 2018. Prevalence estimates and confidence intervals were calculated for HPV and HPV vaccine awareness. Further, we assessed awareness after stratifying by key sociodemographic characteristics. Overall, the awareness of HPV and HPV vaccine declined over time. The lowest awareness was among racial minorities, rural residents, male respondents, those aged 65 years and older, as well as those with the lowest educational and socioeconomic standing. Between 2013 and 2018, the awareness of HPV and HPV vaccine declined by almost 10% among males, those with a high school level of education or lower, and those who earned less than USD 35,000 per annum. In 2018, the awareness of HPV and HPV vaccine was highest among non-Hispanic whites (65.8% and 66.5%) and female adults (70.5% and 71.4%); however, these figures represented declines of about 5% from rates observed in 2008. Amidst a background of sub-optimal HPV vaccination uptake and a growing incidence of HPV-associated cancers in the US, HPV-related awareness within the general US population has declined over time. This calls for stricter enforcement of legislation aimed at boosting HPV awareness, as well as frequent evaluation of government-funded HPV awareness programs.
KEYWORDS: Human papillomavirus, HPV, vaccine, awareness, knowledge, sociodemographic
Introduction
Up to 14 million people in the United States (US) acquire new human papillomavirus (HPV) infections each year,1 with over 40,000 individuals from this population diagnosed with a new case of a HPV-associated cancer annually.2,3 Vaccination against HPV is highly effective at preventing HPV-associated cancers, yet the national HPV vaccination coverage remains low in the US.4 This culminated in failure of the US to achieve the Healthy People 2020 target of 80% HPV vaccination coverage. In 2017, less than 50% of adolescents in the US were up-to-date with HPV vaccination,5 a stark contrast to other high-income nations with highly successful vaccination programs.6,7
National and state-level action has been taken in a bid to improve HPV vaccination uptake and potentially eliminate associated disparities in cancer prevention and cancer-related outcomes.8–12 Recently, National Cancer Institute (NCI)-designated comprehensive cancer centers endorsed a goal of eliminating HPV-associated cancers via extensive gender-neutral HPV vaccination.13 In 2014, the President’s Cancer Panel Report identified the underuse of HPV vaccines as an area of public health concern and made recommendations aimed at addressing barriers to HPV vaccination.8 One recommendation was to employ multi-level interventions to achieve this purpose, including efforts aimed at effective utilization of communication strategies to boost awareness on the benefits, efficacy, and safety of the HPV vaccine.8
HPV-related awareness has been shown to promote HPV vaccination. One study found that parental knowledge of HPV was the strongest predictor of adolescent HPV vaccination among respondents in the US, UK, and Australia.14 Another study found that parents who had HPV knowledge were more likely to have intentions to allow HPV vaccination than those who were not knowledgeable about HPV.15 Studies show that a majority of the US population are aware of HPV and HPV vaccine,16–18 yet severe knowledge gaps continue to exist surrounding the more salient HPV-related details. For example, a study found that more than 60% of US women did not know if the HPV vaccine was successful in cancer prevention.19 Less than 1% of respondents in another study identified HPV infection as a risk factor for oropharyngeal cancer.20
Several US states have passed legislation and committed dedicated funding to promote awareness on HPV and HPV vaccination among school-goers and the general public.10–12 Some of these efforts have been in place since 2006 yet, it is not clear if these interventions are yielding population-level increments in HPV-related awareness. A study conducted in Los Angeles County, California documented increase in awareness between 2007 and 2011,21 while another study that examined two data time points of a national survey did not observe any changes in awareness of HPV.22 However, to the best of our knowledge, an assessment of HPV-related awareness, at the national level, over an extended period of time remains an unfilled gap in the literature.
Therefore, this study aims to describe the levels of awareness of HPV and HPV vaccine in the US over the 10-y period that followed the inception of HPV vaccination (2008 through 2018), using a nationally representative sample of US adults. Findings will inform recommendations that could successfully improve HPV-related awareness, and by association HPV vaccination uptake and prevention of related morbidities.
Materials and methods
The Health Information National Trends Survey (HINTS) is a nationally representative survey administered by the National Cancer Institute. The HINTS target population is all adults aged 18 or older in the civilian non-institutionalized population of the United States.23,24 Data used in this study comprised respondents of HINTS 3 (2008), HINTS 4, cycle 3 (2013); HINTS 4, cycle 4 (2014); HINTS 5, cycle 1 (2017); HINTS 5, cycle 2 (2018). Data collection periods data were January 2008 through May 2008 (HINTS 3), September through December 2013 (HINTS 4, cycle 3), August through November 2014 (HINTS 4, cycle 4), January through May 2017 (HINTS 5, cycle 1) and January through May 2018 (HINTS 5, cycle 2).
HINTS 3 utilized a dual-mode design of data collection, with survey for a fraction of respondents (n = 4,092) obtained through telephone using random digit dial (RDD) and a survey questionnaire used for the remaining fraction (n = 3,582). HINTS 4 and HINTS 5 were administered via mailed questionnaire. HINTS 4, cycle 3, had a total of 3,185 respondents; HINTS 4, cycle 4, had a total of 3,677 respondents; HINTS 5, cycle 1, had a total of 3,285 respondents; and HINTS 5, cycle 2, had a total of 3,504 respondents. For HINTS 3, HINTS 4, and HINTS 5, cycle 1, three strata were applied: (1) addresses in areas with high concentrations of minority populations; (2) addresses in areas with low concentrations of minority populations; and (3) addresses located in counties comprising Central Appalachia, regardless of minority population. In HINTS 5, cycle 2, two strata were used and include (1) addresses in areas with high concentration of minority population, and (2) addresses in areas with low concentration of minority population.
Awareness of HPV and HPV vaccine
Awareness of HPV was assessed based on responses of “yes” or “no” to the survey question – “Have you ever heard of HPV? HPV stands for Human Papillomavirus. It is not HIV, HSV, or herpes.” While awareness of HPV vaccine was assessed based on responses of “yes” or “no” to the survey question – “A vaccine to prevent HPV infection is available and is called the cervical cancer vaccine or HPV shot. Before today, have you ever heard of the cervical cancer vaccine or HPV shot?”
Across study years (2008–2018), the outcome questions and response options were the same in both (1) target population and (2) phrasing.
Participant characteristics
Awareness of HPV and HPV vaccine was stratified by key sociodemographic characteristics including gender, age, race/ethnicity, level of education, rural-urban residence, and household annual income. Gender was classified as male or female. Age was categorized as 18–34 y, 35 to 49 y, 50 to 64 y, and 65 y or older. Race/ethnicity was categorized as non-Hispanic white, non-Hispanic black, and Hispanic. Level of education was categorized as high school graduate or less, post-high school or some college (a combination of post-high school training other than college and some college training), and college graduate or postgraduate. Rural or urban residence was defined using the US Department of Agriculture’s (USDA) 2003 Rural-Urban Continuum Codes. Codes 1 to 3 were categorized as urban, while codes 4 to 9 were categorized as rural. Household annual income was categorized as less than USD 35,000, USD 35, 000 to USD 49,999, USD 50, 000 to USD 74,999, and USD 75,000 or more.
Statistical analysis
Data were weighted to be representative of the US population. The computation of the full-sample weights consisted of the following steps: calculating household-level base weights; adjusting for household nonresponse; calculating person-level initial weights; and calibrating the person-level weights to population counts (also known as control totals). Replicate weights were calculated using the ‘delete one’ jackknife replication method and are used in our analysis to calculate accurate standard error of estimates.25 Weighted prevalence and associated 95% confidence intervals of awareness of HPV and HPV vaccine were calculated for overall study sample, for all study years. Further, HPV and HPV vaccine awareness were estimated after stratifying the study population by key sociodemographic factors. The Survey Procedures of SAS software (SAS for Windows, v9.4) were used for all the data processing and statistical analyses.
Results
Following initial increments in HPV awareness after the inception of the national HPV vaccination program, awareness of both HPV and HPV vaccine within the general population has steadily declined since 2013 (Figure 1). Declines were also observed when examining respondents by key sociodemographic attributes (Figures 2 and 3).
Figure 1.
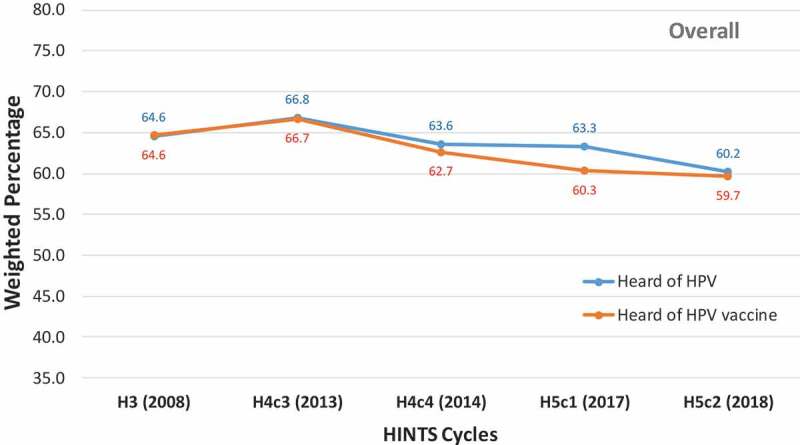
Awareness of HPV and HPV vaccine among US adults, Health Information National Trends Survey 2008–2018
Figure 2.
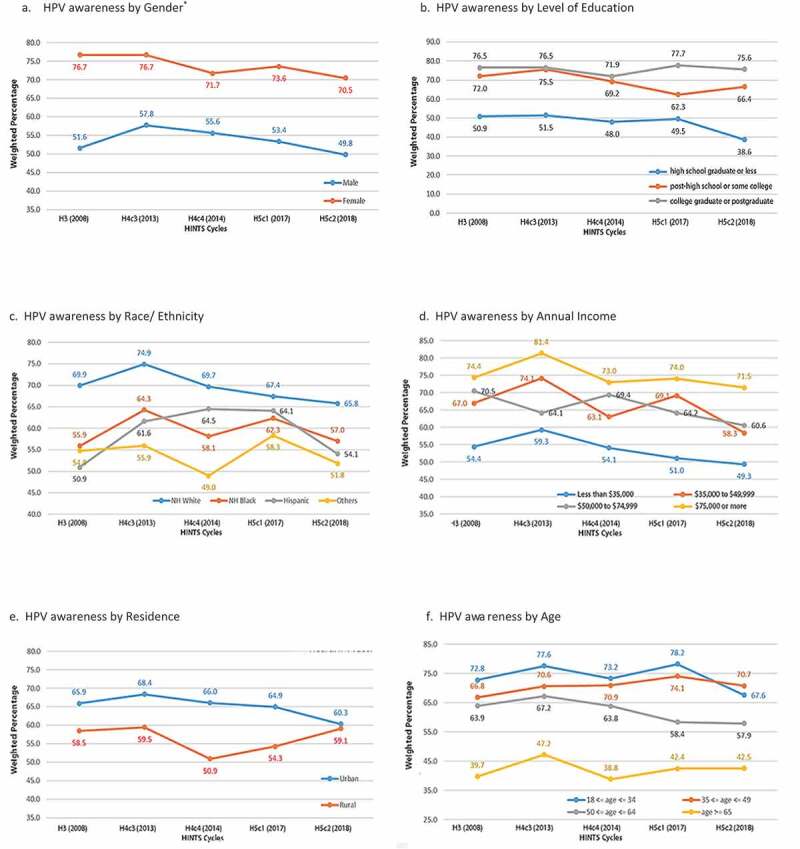
HPV awareness among US adults, by sociodemographic factors, Health Information National Trends Survey 2008–2018
Figure 3.
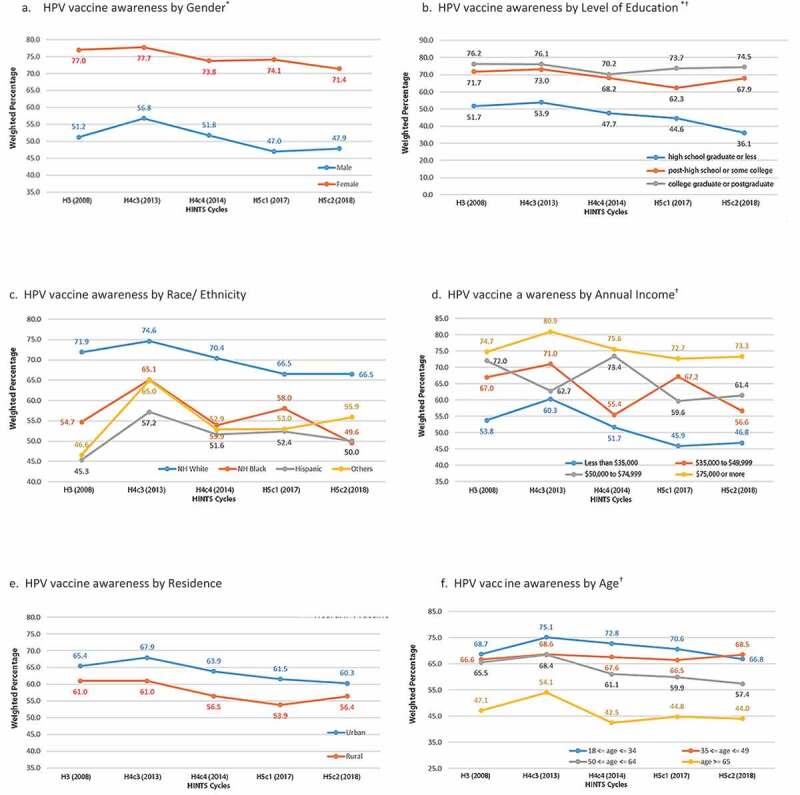
HPV vaccine awareness among US adults, by sociodemographic factors, Health Information National Trends Survey 2008–2018
HPV awareness
HPV awareness reduced by 6.2% and 8% among female and male adults, respectively, between 2013 and 2018 (Figure 2a). Declines in HPV awareness were modest among those who had had some post-high school or college education or graduated college (Figure 2b). On the other hand, larger declines were observed among those with high school education or lower, with HPV awareness decreasing by over 12% in this population between 2008 and 2018. In 2018, while 75.6% of college graduates reported having heard about HPV, only 38.6% of those with high school education or lower had ever heard of HPV. Despite a 9.1% decline in HPV awareness between 2013 and 2018, non-Hispanic whites maintained awareness rates that were higher than both non-Hispanic blacks and Hispanics, throughout the study period (Figure 2c).
HPV awareness also declined within socioeconomic strata, declining more than 5% in all income brackets, except those with annual income over USD 75,000, between 2008 and 2018 (Figure 2d). Awareness about HPV was highest among respondents in the highest income strata (USD 75,000 or more) and lowest among respondents with the least annual income (less than USD 35,000), throughout the study period. In 2018, 71.5% of adults who earned USD 75,000 or more had heard about HPV, while only 49.3% of adults who earned less than USD 35,000 had heard about HPV. HPV awareness was consistently higher among urban dwellers than rural dwellers (Figure 2e). In the overall study period, declines in HPV awareness were not observed among rural dwellers, largely due to an 8.2% increase in awareness between 2014 and 2018, such that by 2018 the awareness gaps between urban and rural residents narrowed significantly (60.3% vs. 59.1%). The least levels of HPV awareness were seen in respondents aged 65 y and older; and while the youngest members (18 to <35 y old) of the population had been the most aware of HPV, the 35–50-y-old cohort experienced sustained growth in awareness throughout the study period and in 2018 surpassed the 18- to <35-y-old cohort (Figure 2f). Specific weighted prevalence rates and associated confidence intervals are provided in the Appendix.
HPV vaccine awareness
HPV vaccine awareness declined by 8.9% and 6.3% among male and female adults, respectively, between 2013 and 2018 (Figure 3a). Compared to men, a higher proportion of women reported being aware of HPV vaccine in 2018 (71.4% vs. 47.9%). Declines in HPV vaccine awareness were modest among those who had had some post-high school or college education or graduated college. On the other hand, larger declines were observed among those with high school education or lower, with a more than 15% decline in HPV vaccine awareness in this population between 2008 and 2018. In 2018, while 74.5% of college graduates reported having heard about HPV vaccine, only 36.1% of those with high school education or lower were aware of HPV vaccine. Despite an 8.1% decline in HPV vaccine awareness between 2013 and 2018, non-Hispanic whites maintained awareness rates that were higher than both non-Hispanic blacks and Hispanics, throughout the study period.
HPV vaccine awareness also declined within all of socioeconomic strata. Awareness about HPV vaccine was highest among respondents in the highest income strata (USD 75,000 or more) and lowest among respondents with the least annual income (less than USD 35,000), throughout the study period. In 2018, 73.3% of adults who earned USD 75,000 or more had heard about the HPV vaccine, while only 46.8% of adults who earned less than USD 35,000 had heard about HPV vaccine. HPV vaccine awareness was consistently higher among urban dwellers than rural dwellers, however in 2018 awareness gaps substantially narrowed (60.3% in urban and 56.4% in rural dwellers). The least levels of HPV vaccine awareness were seen in respondents aged 65 y and older; and while the youngest members (18 to <35 y old) of the population had been the most aware of HPV vaccine, the 35–50-y-old cohort experienced sustained growth in awareness throughout the study period and in 2018 surpassed the 18- to <35-y-old cohort. Specific weighted prevalence rates and associated confidence intervals are provided in the Appendix.
Discussion
In this study examining the awareness of HPV and HPV vaccine over a 10-y period, we found that following an initial surge in awareness, sharp and sustained declines have occurred since 2013. In a 2017 study that analyzed the 2013/2014 HINTS, authors described the population-level awareness of HPV as, “the lowest since vaccine licensure.”26 Our study describes even lower awareness levels, which persist when the overall population is stratified by key sociodemographic characteristics. Furthermore, in addition to confirming previously documented disparities in HPV-related awareness in the US,18,26-30 this study provides evidence that these disparities have persisted over time and are worsening. Specifically, in the 10-y period that have followed the inception of HPV vaccination in the US, the lowest rates of awareness of HPV and HPV vaccine were among racial minorities, rural residents, males, as well as respondents with the lowest levels of education and socioeconomic standing. Approximately 44,000 HPV-related cancers occur annually, despite being vaccine-preventable. In order to increase HPV vaccination rates, it is crucial to increase population-level awareness about HPV and HPV vaccine. Therefore, the decrease in awareness found in our study is concerning and may have important clinical implications in the future.
The gender-related differences in awareness of HPV and HPV vaccine observed in our study are consistent with findings in previous studies that have shown females to be more aware of HPV and HPV vaccine than males.16,18,27-29,31 This has largely been attributed to widespread misconceptions about the utility of the vaccine, following its initial introduction and marketing as a girl-only vaccine. However, several years since the inception of gender-neutral HPV vaccination, gender disparities in HPV-related awareness still persists. This calls for dedicated efforts toward boosting awareness levels in the male population.
As documented in earlier studies,27,29,30,32,33 individuals with higher levels of education had significantly higher levels of awareness of HPV and HPV vaccine than those with the least educational accomplishments, while non-Hispanic whites had higher levels of awareness than all other racial/ethnic groups. Furthermore, consistent with other studies,27 HPV-related awareness were persistently at their lowest among those in the lowest income strata (annual income of <35,000 USD). Our finding of persistently low awareness levels among racial minorities and the under-educated, spanning several years, implies that existing strategies have not been effective at increasing awareness in these groups. Given that low socioeconomic status and under-education often coexist, particularly in ethno-racial minority populations, it is important to employ interventions that have a multidimensional approach to addressing barriers to HPV awareness.
Interventions should be customized to resonate with pertinent ethno-racial groups and simplified for assimilation at all educational levels. A study that used Spanish radionovelas as an educational tool to promote awareness of HPV in a rural Hispanic community demonstrated a remarkable degree of success.34 Similarly, an intervention that targeted a low-income Hispanic population in a medically underserved region in Southern California succeeded in increasing HPV-related awareness among participants, using an educational fotonovella.35 In utilizing tailored approaches that were adapted to the characteristics of the community, these interventions were well suited for the target population. More so, interventions at this level, complement larger-scale interventions at the state/national level by addressing the underlying intricate barriers that may be inaccessible to larger-scale interventions. Lastly, professionals who develop the awareness campaigns are most likely college educated and of higher socioeconomic status, this might result in contextual gaps in the design of awareness campaigns. Therefore, to make interventions more relevant to target populations, efforts should be made to incorporate direct contributions from members of these populations.
Consistent with an earlier study,36 awareness of HPV and HPV vaccine was higher among urban residents than rural residents. However, one positive from our study was that awareness of HPV among rural residents increased over the study period. This is important because while urban populations have a higher overall cancer incidence rate, rural populations have a higher incidence of behavior-related cancers, e.g. tobacco use and HPV-associated cancers.37 As such, the incidence of cancer in rural regions can be reduced by robust cancers prevention efforts such as HPV vaccination. Therefore, the observed increments in HPV awareness among rural residents in our study is a positive, given that widespread HPV awareness can boost HPV vaccination and thus, help dispel existing disparities. Nevertheless, continued efforts must be taken to further accelerate this progress.
The youngest members of the study population had the highest levels of awareness of HPV and HPV vaccine for the most part of the study period, while those aged 65 y and older persistently had the least awareness. This finding was consistent with another study18 and may be attributed to the fact that younger members of this population who satisfied age eligibility for vaccination may have been targets of awareness campaigns during the years that followed the HPV vaccine introduction. Another positive from our study is the consistently rising awareness of HPV and HPV vaccine among the 35- to 50-y-old cohort, an age group that likely consists of parents to children within age-eligibility for HPV vaccination. The over 65-y-old population most likely consists of grandparents and given the crucial role they play in families, efforts must be made to enhance their engagement in HPV awareness campaigns. In addition, given the impact of the coronavirus pandemic on long-term care facilities in the US, grandparents may become more constant fixtures in households and they should be equipped with adequate information to allow for meaningful contributions toward HPV vaccination decisions for their grandchildren.
This study is not without limitations. First, our estimation of lack of HPV-related awareness may be overestimated given that several factors beyond lack of knowledge could result in non-affirmative responses to survey questions that assess HPV-related knowledge.38 Second is the issue of low response associated with some cycles of HINTS, which could result in low-response bias. However, HINTS addresses potential for bias through modality coverage and survey sampling techniques.39 Furthermore, findings of a non-response bias study conducted by HINTS researchers revealed that demographic influences on nonresponse can be addressed by applying standard weighting procedures.40 These procedures were applied in the present study.
The US failed to achieve the Healthy People 2020 target of 80% HPV vaccination coverage. Given the associations between HPV-related awareness and HPV vaccination uptake,14,15 efforts must be geared toward addressing the declining awareness of HPV and HPV vaccine observed at the population level. While further studies are needed to unravel the underlying factors responsible for observed declines in HPV-related awareness within the general US population and specified sociodemographic groups, robust public health efforts must be undertaken to reverse ongoing trends and the negative impact it may have on HPV vaccination coverage. Research shows a high degree of trust in HPV information from health-care providers, particularly among minority populations;41 with physician recommendations shown to strongly predict HPV vaccination42 However, a national survey revealed that 48% of parents of adolescents received no HPV vaccination recommendations from their physicians.43 This represents a missed opportunity to fully engage parents on the importance and benefits of HPV vaccination. Physicians should be made aware of the crucial role they have to play in contributing to the promotion of population-level awareness of HPV and HPV vaccine.
Novel and more innovative channels to disseminate information on HPV and HPV vaccine to populations with low awareness should be considered. Dissemination of HPV educational materials via social media wields significant potential as a potent platform for promoting HPV awareness. Substantial HPV-related discourse has been reported on online forums such as Reddit.44 This study reports that HPV-related messaging increased from 162 messages in 2007 to 5311 messages in 2015.44 Hence, it is important that these platforms are furnished with the most up-to-date and evidence-based information. More so, the theme of HPV-related messaging is important. For example, framing HPV-related messaging to themes around HPV’s causal associations with cancers has been shown to boost interest levels and motivation to learn HPV-related information.45 Interventions should focus on widespread dissemination of tailored, yet detailed education on HPV and HPV vaccine, while also countering HPV- and other health-related misinformation that have become prevalent on online platforms.46 Finally, in light of evidence from this study showing declining population-level awareness of HPV and HPV vaccine, it is critical to conduct regular surveillance and result-oriented evaluations of public health programs aimed at promoting HPV awareness. In addition, future research on HPV vaccine knowledge should obtain data that could provide insight to the intrinsic barriers to HPV awareness; extensive qualitative surveys may be useful in this regard.
Supplementary Material
Funding Statement
The study was funded by the National Cancer Institute [P30CA016672 to S. Shete], the Betty B. Marcus Chair in Cancer Prevention (to S. Shete), and the Cancer Prevention Research Institute of Texas [Grant RP170259 to S. Shete]. A cancer prevention fellowship award supported by the Mrs. Harry C. Wiess Cancer Research Fund and the Laura and John Arnold Foundation (to O.G. Chido‐Amajuoyi). Susan G. Komen Graduate Training and Disparities Research Program [GTDR17497435 to I. Jackson] Cancer Prevention and Research Institute of Texas [RP170259]; Duncan Family Institute for Cancer Prevention and Risk Assessment; the Betty B. Marcus Chair in Cancer Prevention; Susan G. Komen Graduate Training and Disparities Research Program.
Disclosure of potential conflicts of interest
Authors declare no conflict of interest.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website.
References
- 1.Satterwhite CL, Torrone E, Meites E, Dunne EF, Mahajan R, Ocfemia MCB, Su J, Xu F, Weinstock H.. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex Transm Dis. 2013;40(3):187–93. doi: 10.1097/OLQ.0b013e318286bb53. [DOI] [PubMed] [Google Scholar]
- 2.Van Dyne EA, Henley SJ, Saraiya M, Thomas CC, Markowitz LE, Benard VB. Trends in human papillomavirus-associated cancers – United States, 1999–2015. MMWR Morb Mortal Wkly Rep. 2018;67(33):918–24. doi: 10.15585/mmwr.mm6733a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jemal A, Simard EP, Dorell C, Noone A-M, Markowitz LE, Kohler B, Eheman C, Saraiya M, Bandi P, Saslow D, et al. Annual report to the nation on the status of cancer, 1975–2009, featuring the burden and trends in human papillomavirus (HPV)–associated cancers and HPV vaccination coverage levels. JNCI. 2013;105(3):175–201. doi: 10.1093/jnci/djs491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walker TY, Elam-Evans LD, Yankey D, Markowitz LE, Williams CL, Fredua B, Singleton JA, Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years – United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(33):718–23. doi: 10.15585/mmwr.mm6833a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walker TY, Elam-Evans LD, Yankey D, Markowitz LE, Williams CL, Mbaeyi SA, Fredua B, Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 Years—United states, 2017. MMWR. Morbidity and Mortality Weekly Report. 2018;67:909–17. doi: 10.15585/mmwr.mm6733a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National HPV Vaccination Program Register . HPV vaccination coverage by dose number (australia) for males/females by age group in 2017. Updated 2018. [Accessed 2019 October28]. http://www.hpvregister.org.au/research/coverage-data.
- 7.Sinka K, Kavanagh K, Gordon R, Love J, Potts A, Donaghy M, Robertson C. Achieving high and equitable coverage of adolescent HPV vaccine in scotland. J Epidemiol Community Health. 2014;68(1):57–63. doi: 10.1136/jech-2013-202620. [DOI] [PubMed] [Google Scholar]
- 8.Accelerating H Vaccine uptake: urgency for action to prevent cancer. Bethesda (MD): National Cancer Institute; 2014. A report to the president of the United States from the President’s Cancer Panel. [Google Scholar]
- 9.Cartmell KB, Young-Pierce J, McGue S, Alberg AJ, Luque JS, Zubizarreta M, Brandt HM. Barriers, facilitators, and potential strategies for increasing HPV vaccination: A statewide assessment to inform action. Papillomavirus Res. 2018;5:21–31. doi: 10.1016/j.pvr.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Conference of State Legislatures HPV vaccine: State Legislation and Statutes ; 2020. [Accessed 2020. June 26]. Available from: http://www.ncsl.org/research/health/hpv-vaccine-state-legislation-and-statutes.aspx.
- 11.Hoss A, Meyerson BE, Zimet GD. State statutes and regulations related to human papillomavirus vaccination. Hum Vaccin Immunother. 2019;15(7–8):1519–26. doi: 10.1080/21645515.2019.1627817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keim-Malpass J, Mitchell EM, DeGuzman PB, Stoler MH, Kennedy C. Legislative activity related to the human papillomavirus (HPV) vaccine in the united states (2006–2015): A need for evidence-based policy. Risk Manag Healthc Policy. 2017;10:29–32. doi: 10.2147/RMHP.S128247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.NCI-Designated Cancer Centers . NCI-designated cancer centers endorse goal of eliminating HPV-related cancers. 2018.
- 14.Nickel B, Dodd RH, Turner RM, Waller J, Marlow L, Zimet G, Ostini R. and McCaffery K. Factors associated with the human papillomavirus (HPV) vaccination across three countries following vaccination introduction. Preventive Med Rep. 2017;8:169–76. doi: 10.1016/j.pmedr.2017.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mansfield LN, Onsomu EO, Merwin E, Hall NM, Harper-Harrison A. Association between parental HPV knowledge and intentions to have their daughters vaccinated. West J Nurs Res. 2018;40(4):481–501. doi: 10.1177/0193945916682953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gerend MA, Magloire ZF. Awareness, knowledge, and beliefs about human papillomavirus in a racially diverse sample of young adults. J Adolesc Health. 2008;42(3):237–42. doi: 10.1016/j.jadohealth.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 17.Suk R, Montealegre JR, Nemutlu GS, Nyitray AG, Schmeler KM, Sonawane K, Deshmukh AA. Public knowledge of human papillomavirus and receipt of vaccination recommendations. JAMA Pediatr. 2019;173(11):1099–102. doi: 10.1001/jamapediatrics.2019.3105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blake KD, Ottenbacher AJ, Rutten LJF, Grady MA, Kobrin SC, Jacobson RM, Hesse BW. Predictors of human papillomavirus awareness and knowledge in 2013: gaps and opportunities for targeted communication strategies. Am J Prev Med. 2015;48(4):402–10. doi: 10.1016/j.amepre.2014.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Domgue JF, Chido-Amajuoyi OG, Yu RK, Shete S. Beliefs about HPV vaccine’s successfulness at cervical cancer prevention among adult US women. JNCI Cancer Spectrum. 2019;3(4):pkzo64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luryi AL, Yarbrough WG, Niccolai LM, Roser S, Reed SG, Nathan CAO, Moore MG, Day T, Judson BL. Public awareness of head and neck cancers: A cross-sectional survey. JAMA Otolaryngology–Head & Neck Surg. 2014;140(7):639–46. doi: 10.1001/jamaoto.2014.867. [DOI] [PubMed] [Google Scholar]
- 21.Nonzee NJ, Baldwin SB, Cui Y, Singhal R. Disparities in parental human papillomavirus (HPV) vaccine awareness and uptake among adolescents. Vaccine. 2018;36(10):1243–47. doi: 10.1016/j.vaccine.2017.08.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wheldon CW, Krakow M, Thompson EL, Moser RP. National trends in human papillomavirus awareness and knowledge of human papillomavirus–related cancers. Am J Prev Med. 2019;56(4):e117-e123. doi: 10.1016/j.amepre.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 23.Nelson D, Kreps G, Hesse B, Croyle R, Willis G, Arora N, Rimer B, Vish Viswanath K, Weinstein N, Alden S, et al. The health information national trends survey (HINTS): development, design, and dissemination. J Health Commun. 2004;9(5):443–60. doi: 10.1080/10810730490504233. [DOI] [PubMed] [Google Scholar]
- 24.Hesse BW, Moser RP, Rutten LJF, Kreps GL. The health information national trends survey: research from the baseline. J Health Commun. 2006;11(S1):vii–xvi. doi: 10.1080/10810730600692553. [DOI] [PubMed] [Google Scholar]
- 25.Korn EL, Graubard BI. Analysis of health surveys. Vol. 323. John Wiley & Sons; 2011. https://www.wiley.com/en-us/Analysis+of+Health+Surveys-p-9780471137733 [Google Scholar]
- 26.Adjei Boakye E, Tobo BB, Rojek RP, Mohammed KA, Geneus CJ, Osazuwa-Peters N. Approaching a decade since HPV vaccine licensure: racial and gender disparities in knowledge and awareness of HPV and HPV vaccine. Hum Vaccin Immunother. 2017;13(11):2713–22. doi: 10.1080/21645515.2017.1363133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wisk LE, Allchin A, Witt WP. Disparities in human papillomavirus vaccine awareness among U.S. parents of preadolescents and adolescents. Sex Transm Dis. 2014;41(2):117–22. doi: 10.1097/OLQ.0000000000000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patel H, Jeve YB, Sherman SM, Moss EL. Knowledge of human papillomavirus and the human papillomavirus vaccine in European adolescents: A systematic review. Sex Transm Infect. 2016;92(6):474–79. doi: 10.1136/sextrans-2015-052341. [DOI] [PubMed] [Google Scholar]
- 29.Marlow LA, Zimet GD, McCaffery KJ, Ostini R, Waller J. Knowledge of human papillomavirus (HPV) and HPV vaccination: an international comparison. Vaccine. 2013;31(5):763–69. doi: 10.1016/j.vaccine.2012.11.083. [DOI] [PubMed] [Google Scholar]
- 30.Marlow LA, Wardle J, Forster AS, Waller J. Ethnic differences in human papillomavirus awareness and vaccine acceptability. J Epidemiol Community Health. 2009;63(12):1010–15. doi: 10.1136/jech.2008.085886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Klug SJ, Hukelmann M, Blettner M. Knowledge about infection with human papillomavirus: A systematic review. Prev Med. 2008;46(2):87–98. doi: 10.1016/j.ypmed.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 32.Blake KD, Ciolino HP, Croyle RT. Population health assessment in NCI-designated cancer center catchment areas. Cancer Epidemiol Biomarkers Prev. 2019;28:428–30. doi: 10.1158/1055-9965.EPI-18-0811. [DOI] [PubMed] [Google Scholar]
- 33.Cates JR, Brewer NT, Fazekas KI, Mitchell CE, Smith JS. Racial differences in HPV knowledge, HPV vaccine acceptability, and related beliefs among rural, southern women. J Rural Health. 2009;25(1):93–97. doi: 10.1111/j.1748-0361.2009.00204.x. [DOI] [PubMed] [Google Scholar]
- 34.Kepka D, Coronado GD, Rodriguez HP, Thompson B. Evaluation of a radionovela to promote HPV vaccine awareness and knowledge among hispanic parents. J Community Health. 2011;36(6):957–65. doi: 10.1007/s10900-011-9395-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chan A, Brown B, Sepulveda E, Teran-Clayton L. Evaluation of fotonovela to increase human papillomavirus vaccine knowledge, attitudes, and intentions in a low-income hispanic community. BMC Res Notes. 2015;8(1):615. doi: 10.1186/s13104-015-1609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mohammed KA, Subramaniam DS, Geneus CJ, Henderson ER, Dean CA, Subramaniam DP, Burroughs TE. Rural-urban differences in human papillomavirus knowledge and awareness among US adults. Prev Med. 2018;109:39–43. doi: 10.1016/j.ypmed.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 37.Zahnd WE, James AS, Jenkins WD, Izadi SR, Fogleman AJ, Steward DE, Colditz GA, Brard L. Rural-urban differences in cancer incidence and trends in the united states. Cancer Epidemiol Biomarkers Prev. 2018;27(11):1265–74. doi: 10.1158/1055-9965.EPI-17-0430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ellis EM, Ferrer RA, Klein WM. Factors beyond lack of knowledge that predict “I don’t know” responses to surveys that assess HPV knowledge. J Health Commun. 2018;23(10–11):967–76. doi: 10.1080/10810730.2018.1554729. [DOI] [PubMed] [Google Scholar]
- 39.Cantor D, Coa K, Crystal-Mansour S, Davis T, Dipko S, Sigman R. Health information national trends survey (HINTS) 2007. Rockville (MD): Westat; 2009. [Google Scholar]
- 40.Finney Rutten LJ, Blake KD, Skolnick VG, Davis T, Moser RP, Hesse BW. Data resource profile: the national cancer institute’s health information national trends survey (HINTS). Int J Epidemiol. 49.1 (2020):17–17j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Clark CR, Baril NC, Achille E, Foster S, Johnson N, Taylor-Clark K, Gagne JJ, Olukoya O, Huisingh CE, Ommerborn MJ, et al. Trust yet verify: physicians as trusted sources of health information on HPV for black women in socioeconomically marginalized populations. Prog Community Health Partnerships: Res Educ Action. 2014;8(2):169–79. doi: 10.1353/cpr.2014.0019. [DOI] [PubMed] [Google Scholar]
- 42.Rosenthal S, Weiss TW, Zimet GD, Ma L, Good M, Vichnin M. Predictors of HPV vaccine uptake among women aged 19–26: importance of a physician’s recommendation. Vaccine. 2011;29(5):890–95. doi: 10.1016/j.vaccine.2009.12.063. [DOI] [PubMed] [Google Scholar]
- 43.Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: the impact of recommendation quality. Vaccine. 2016;34(9):1187–92. doi: 10.1016/j.vaccine.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lama Y, Hu D, Jamison A, Quinn SC, Broniatowski DA. Characterizing trends in human papillomavirus vaccine discourse on reddit (2007–2015): an observational study. JMIR Public Health Surveillance. 2019;5(1):e12480. doi: 10.2196/12480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Friedman AL, Shepeard H. Exploring the knowledge, attitudes, beliefs, and communication preferences of the general public regarding HPV: findings from CDC focus group research and implications for practice. Health Educ Behavior. 2007;34(3):471–85. doi: 10.1177/1090198106292022. [DOI] [PubMed] [Google Scholar]
- 46.Swire-Thompson B, Lazer D. Public health and online misinformation: challenges and recommendations. Annu Rev Public Health. 2019;41(2020):433–451. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


