ABSTRACT
Rotaviruses (RVs) are a leading cause of viral gastroenteritis among children younger than 5. The incidence of RV disease can be reduced through the widespread use of vaccination, but coverage is low in many countries, including Italy. This fact reflects the poor consideration given to the RV vaccine, both by the population and by healthcare workers. Peoples’ opinions are strictly dependent on the attitude of doctors and nurses. The aim of this work is the evaluation of healthcare workers’ knowledge, attitudes and opinions regarding RV vaccination. The results of two surveys were compared; the first was carried out in 2017, soon after the Italian National Immunization Plan introduced the recommendation for the RV vaccine. The second was performed at the end of 2018, approximately 1 year after the adoption of a Law that introduced new compulsory vaccinations, not including the RV vaccine. In 2017, 182 questionnaires were collected, and 111 in 2018. An increase was observed in the percentage of participants who reported recommending the RV vaccine and a significant increase was found in the coverage the participants claimed to reach. Education of healthcare workers after the introduction of compulsory vaccination may prompt them to actively offer also recommended vaccines.
KEYWORDS: Rotavirus, healthcare worker, immunization, physicians, knowledge, attitudes
Rotaviruses (RVs) are double-stranded segmented RNA virus, that represent the leading cause of viral gastroenteritis among children younger than 5 years of age. Patients mostly recover without treatment but Rotavirus gastroenteritis (RVGE) can lead to severe dehydration, requiring hospitalization for treatment with intravenous fluid. RVGE is particularly severe in low-income countries due to difficult access to rehydration therapy and other medical treatments in settings characterized by poor hygienic conditions. RV infection can remain asymptomatic or after approximately a two-days incubation period lead to acute gastroenteritis with mild to severe diarrhea, vomiting and fever. RV infection is highly contagious; the virus is present in the stool of an infected person and can survive for quite a long time on contaminated surfaces, including people’s hands.1,2
Globally, it is estimated that RV infection causes approximately 25 million medical examinations, 2 million hospital admissions and 215,000 deaths every year.3 Mortality is low in Europe, but the impact of RVGE on families and society is significant from an economic point of view, due to the increase in health care costs and the productivity loss.4,5 In Italy, over 250,000 cases of RVGE occur every year, resulting in approximately 125,000 pediatric medical visits, 52,000 emergency room visits, 14,500 hospital admissions and 5 to 11 deaths.6
In industrialized countries, like Italy, viruses cause 23–34% of nosocomial infections and 65–90% of them are acute gastroenteritis in pediatric wards.7,8 Nosocomial RVGE causes prolonged hospitalization, which directly and indirectly increases both costs for the healthcare system and mortality in preterm infants.9 Therefore, it is important to reduce the incidence of RV disease through the wide use of vaccination.10 In 1999 a highly effective rotavirus vaccine was withdrawn from the market because of its association with cases of intussusception. Two live, attenuated, second-generation RV vaccines were licensed in 2006; both are administered orally and show high efficacy and safety profiles. The WHO recommended that these vaccines be introduced for routine vaccination in both industrialized and developing countries.11
In high and upper-middle income countries the lack of serious sequelae causes a worrying underestimation of the potential risk of the disease that results from the infection, in both the population and the scientific community.12–15 Moreover, although the efficacy and safety of this vaccine have been widely demonstrated, and several studies have shown that the risk of intussusception as a side effect is very low, the fear persists.16–20 Both fear and underestimation of the risk resulted in a low vaccination coverage in several countries. According to the latest available data, several European countries recorded a coverage between 61% and 93%.21–25 For other countries where the vaccine is recommended, the few available data show lower levels.26
In Italy, in February 2017, with the National Vaccination Prevention Plan (PNPV) 2017–2019, the RV vaccine was universally recommended to all children older than 6 weeks of age.27 However, the June 2017 law introducing new mandatory vaccines did not included the RV vaccine among them.28 Therefore, the contrast between mandatory and recommended vaccination increased the doubts about the usefulness of RV vaccination. The RV vaccination coverage in 2018 was 17%, very far from the target of 75% set by the PNPV 2017–2019 for the same year.27,29–31
Since opinion of the population is closely related to that of physicians’, the latter’s positive attitude toward RV vaccination is very important.32 A recent Italian study that examined parents’ opinions about vaccination showed that receiving information from physicians and nurses had a stronger association with the level of knowledge and vaccination adherence.33
Nevertheless, there are few studies that investigate the knowledge, opinions and attitudes of healthcare workers about RV vaccination.
The aim of this work is the evaluation of the results of two surveys carried out in 2017, immediately after the recommendation of RV vaccination by the PNPV 2017–2019, and again at the end of 2018, approximately one year after the mandatory vaccination law. Furthermore, the results of a previous study,34 carried out before RV vaccination was recommended, were available for discussion.
A questionnaire on knowledge and opinions about RV vaccination modified from one used in previous study34 was administered to healthcare workers during a cycle of vaccination counseling courses, carried out in 2017 (between April and June) and in 2018 (between October and November) in three towns in the north, two in the center and three in the south of Italy. The participants were doctors and nurses who were involved in vaccine administration and/or counseling. All participants completed the anonymous questionnaire prior to the beginning of the courses.
In the questionnaire a question about the change in the legislative situation regarding the RV vaccine was added. In the 2018 questionnaire, one question about the main motivation for acceptance of the vaccination was added. Moreover, the question about the reasons for refusal was modified in the 2018 questionnaire by adding the fact that the vaccine is not mandatory; eliminating the cost (since the vaccination is recommended and free of charge) and the practical difficulties associated with receiving the vaccine. Skepticism toward the vaccine was the only common answer choice. The 2018 questionnaire is shown in Figure 1.
Figure 1.
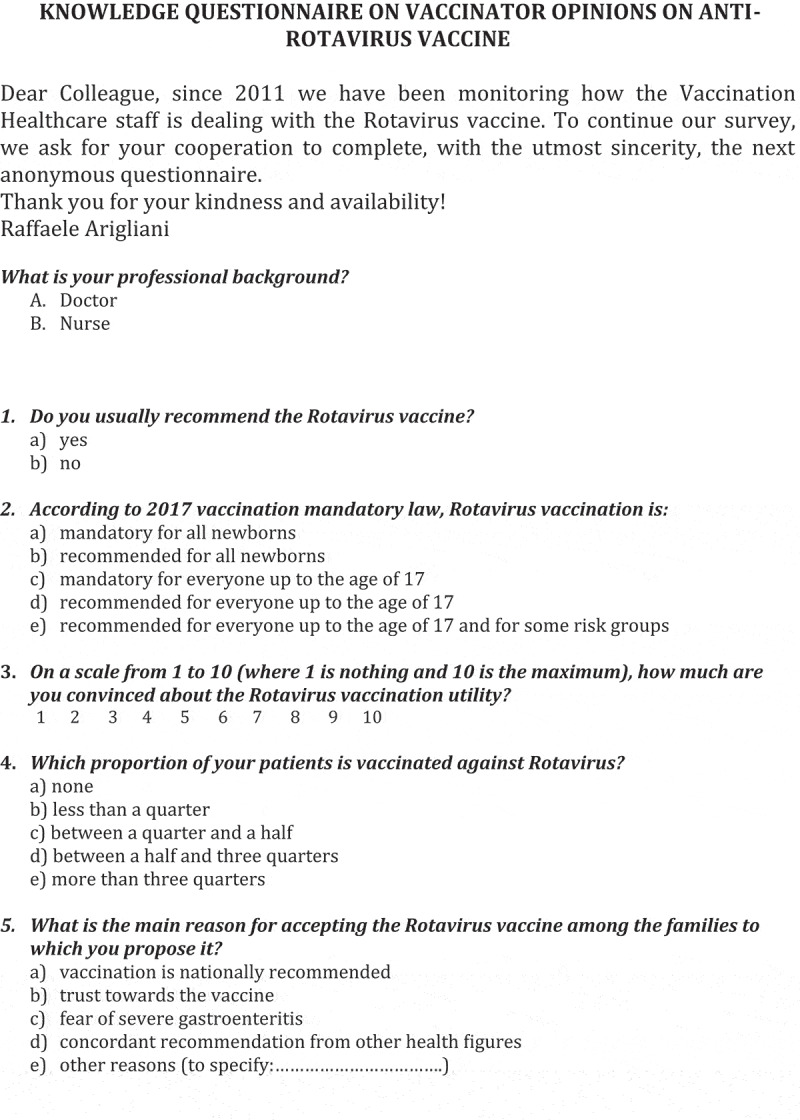
Questionnaire 2018
Figure 1.
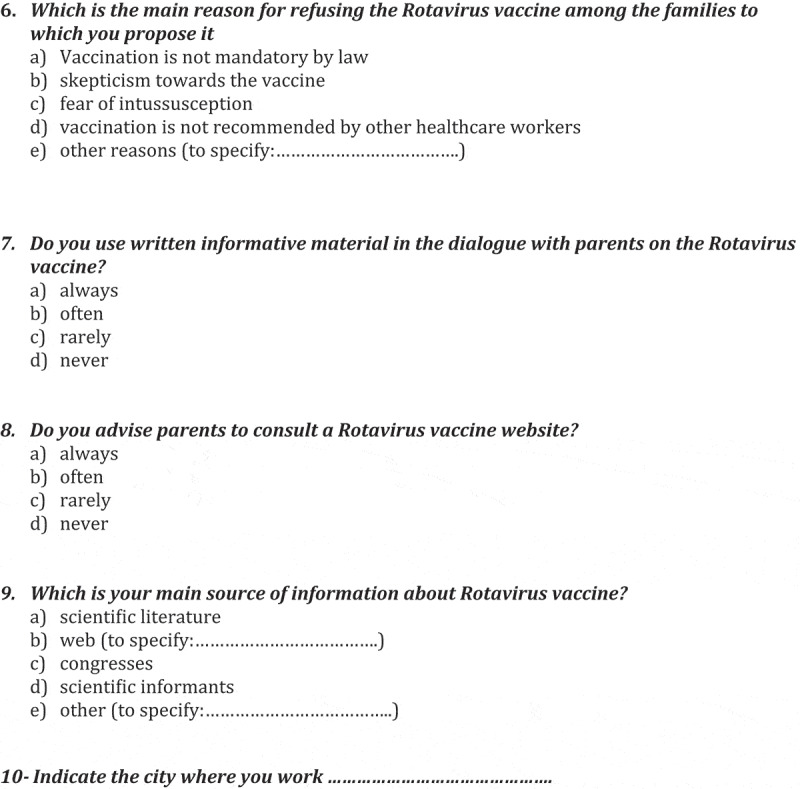
Continued
On the first page the questionnaire presents a brief description of the aim of the survey. The participants were asked to indicate their profession and place of work. The questionnaire was composed of several closed-ended questions that investigated knowledge and opinions regarding RV vaccination.
The obtained data were entered in an Excel spreadsheet and the results of the questionnaires were described by comparing the answers between the 2017 and 2018 surveys. To determine the statistical significance regarding the differences found in the comparison of the data, we used the Chi-squared test for contingency tables (Pearson’s Chi-squared and Fisher’s exact tests).
The participants were 182 in 2017 and 111 in 2018. The two samples are described in Table 1. The results of the questionnaires are summarized in Table 2. While in 2018 participants answered all questions (except for one answer to question 9), in 2017 many answers were missing. Comparing the answers between doctors and nurses in each survey, there were not significant differences, except for some questions.
Table 1.
Description of the participants to the 2017 and 2018 surveys
| 2017 | 2018 | ||
|---|---|---|---|
| Doctors | 99 (54%) | 83 (75%) | |
| Nurses | 83 (46%) | 28 (25%) | |
| Total respondents | 182 | 111 | |
| Coming from an Italian region of the | Nord | 51 (28%) | 33 (30%) |
| Center | 58 (32%) | 22 (20%) | |
| Sud | 73 (40%) | 55 (50%) | |
Table 2.
Results of 2017 and 2018 questionnaires with differences between the two surveys
| 2017 (N = 182) |
2018 (N = 111) |
||||
|---|---|---|---|---|---|
| Answer | N | %* | N | %* | |
| Question 1 | A | 138 | 76 | 91 | 82 |
| B | 40 | 22 | 20 | 18 | |
| p 0,364 (#) | |||||
| Question 2 | A | 8 | 4 | 2 | 2 |
| B | 163 | 90 | 105 | 95 | |
| C | 0 | 0 | 0 | 0 | |
| D | 1 | 1 | 3 | 3 | |
| E | 1 | 1 | 1 | 1 | |
| p 0,233 (##) | |||||
| Question 3 | 1 or 2 | 2 | 1 | 5 | 5 |
| 3 or 4 | 8 | 4 | 6 | 5 | |
| 5 or 6 | 23 | 13 | 7 | 6 | |
| 7 or 8 | 76 | 42 | 40 | 36 | |
| 9 or 10 | 71 | 39 | 53 | 48 | |
| p 0,092 | |||||
| Question 4 | A | 12 | 7 | 3 | 3 |
| B | 60 | 33 | 22 | 20 | |
| C | 46 | 25 | 28 | 25 | |
| D | 33 | 18 | 21 | 19 | |
| E | 20 | 11 | 37 | 33 | |
| p 0,000 (##) | |||||
| Question 6 | B** | 100 | 55 | 25 | 23 |
| A + C + D + E | 52 | 29 | 86 | 77 | |
| p 0,000 (##) | |||||
| Question 7 | A + B | 76 | 42 | 43 | 39 |
| C + D | 96 | 53 | 68 | 61 | |
| p 0,365 (#) | |||||
| Question 8 | A + B | 69 | 38 | 34 | 31 |
| C + D | 101 | 55 | 77 | 69 | |
| p 0,090 (#) | |||||
| Question 9 | A + C | 131 | 72 | 89 | 80 |
| B + D + E | 47 | 26 | 21 | 19 | |
| p 0,156 (##) | |||||
* The percentages are calculated on the total of participants
** B is the only common answer between 2017 and 2018 questionnaire
(#) Pearson chi2
(##) Fisher’s exact
In 2017, when participants were asked whether they normally recommended the RV vaccine (question 1), 76% of respondents said they routinely recommend it to their patients, while 2% did not respond. In 2018 the percentage rose to 82%; which is a result similar to that reached in 2006 in the United States.35 There was an increase, although not significant, in the percentage of participants who declared that they usually recommend the vaccine. Furthermore, the 2017 study, conducted just few months after the inclusion of the RV vaccine among recommended vaccinations, showed a significant increase (p < .01) in knowledge and more positive attitudes toward this vaccine compared to a similar survey conducted in 2015.34
In 2017, 90% of the interviewees knew that the vaccine was not compulsory but recommended for all newborns (question 2). In 2018 the percentage rose to 95% showing an increase, although not significant, in the knowledge about the Ministry of Health recommendations.28
When asked to rate how useful the vaccine was (question 3), on a 1 to 10 scale, there were no differences between the two surveys.
When participants were asked how many of their patients decided to get vaccinated (question 4), in 2017, 11% of the interviewees said that more than 75% of their patients choose to get vaccinated; in 2018, 33% gave the same answer with a significant increase (p < .001) over the time in the declared vaccination coverage. Moreover, if we compare our results with those obtained in 2015, in the absence of a regular recommendation, the increase seems to be greater (more than one half of participants indicated an adherence lower than 25%).34 These results can be explained by the fact that the official recommendations by the institutions make healthcare professionals more likely to recommend the vaccine. This fact has also been demonstrated in similar studies.35,36 Comparing official coverage data with those provided by our sample, an overestimation of the proportion of people who get vaccinated emerge probably because the participants in the training courses are the healthcare workers most involved in vaccination activity and are more interested in reaching high level coverage.
When asked about the use of printed informative materials (question 7), in 2018, the answers were as follows: 39% of interviewees answered that they always or often provided parents with printed information about the vaccine (29% of doctors and 68% of nurses), whereas 61% did this rarely or never (71% of doctors and 32% of nurses). Similar data from the 2017 are reported in the table. Although there were no differences between the two years, in both surveys nurses responded that they used printed material more frequently than doctor (p < .001). This can be explained by the fact that nurses often deliver brochures and informative leaflets to the patient as supporting materials for their next interview with the doctors, who will explain verbally. Approximately the same percentage of doctor use the paper material in 2015.34
When survey participants were asked if they would advise parents to consult a website that provided information about the vaccine (question 8), in 2017, 38% of participants said they always or often recommended it (37% of doctors and 39% of nurses), while 55% did so rarely or never (58% of doctors and 53% of nurses). Seven percent of the participants did not respond. There were no differences between doctors and nurses in 2017. In 2018, 31% of the survey participants said they always or often advised parents to consult a website for information on the vaccine (23% of doctors and 54% of nurses), and 69% reported doing so rarely or never (77% of doctors and 46% of nurses). There was a significant difference (p < .01) between the doctors and nurses in 2018. Furthermore, doctors recommended websites significantly more in 2017 than in 2018 (p < .05). The percentage was similar between 2015 and 2017.34 The decrease seen in the 2018 survey may be due to the communication problems that followed the introduction of compulsory vaccinations. In fact, in Italy, healthcare professionals are unwilling to advise patients to use websites for information about vaccinations, often because patients may be unable to distinguish authoritative and reliable sources from ones that report false, incomplete or unsupported information. A similar attitude can be found also in a study conducted in US.35
To the question aimed at understanding which was the main source of information concerning the RV vaccine (question 9), in 2017, 72% of the interviewees indicated scientific literature and participation in scientific meetings (78% of doctors and 65% of nurses). For 26% of the interviewees, the main sources of information were websites and medical sales representatives (21% of doctors and 31% of nurses). Two percent of the sample did not respond. There were no differences between doctors and nurses in 2017. In 2018, for 80% of the interviewees the main source of information about the vaccine came from scientific literature and participation in scientific meetings (90% of doctors and 50% of nurses). One percent of the sample did not answer. There was a significant difference (p < .001) between doctors and nurses in 2018, with doctors using websites and medical sales representative less than nurses, as well as a significant difference (p < .05) between doctors in 2017 and 2018. The use of websites as sources of information significantly decreased between 2017 and 2018 among doctors, who prefer to use scientific literature and conferences.
The question aimed at understanding the main reason for vaccination acceptance among families (question 5) was added in 2018. Among the respondents, 50% indicated the fear of severe gastroenteritis and 24% considered the factor that influenced acceptance of the vaccination to be the recommendation at national level. There were no differences between doctors and nurses. Similar results emerged from a study conducted in Canada.37
When the participants were asked about the main reason for vaccination refusal by the families to which it was proposed (question 6), in 2017, most participants (55%) indicated skepticism toward the vaccine itself. The other causes of refusal of the vaccine constituted a total of 29% and included: a lack of knowledge due to a lack of information on this subject, failure of the pediatrician to recommend the vaccine and the cost of the vaccine. The percentage of non-respondent was quite high (16%). In 2018, as the main cause of vaccination refusal, 34% of the respondents indicated that it was not mandatory by law and skepticism toward the vaccine accounted for 23%. The other causes represented a total of 39% and included: the fear of intussusception (21%) and the lack of recommendation by other health professionals (18%). Five percent of the respondents indicated other causes as the main reason for refusing the vaccine. The indication of skepticism showed a significant decrease (p < .001) between 2017 and 2018.
It is essential that the results obtained are spread throughout the population and healthcare workers, accompanied by rigorous data of the effectiveness of education, promotion and active offer campaigns. The strength of this study lies on a consecutive investigation, carried out with a similar methodology, on people involved in the administration of the vaccination in different regions of Italy. The timing between the two surveys allows us to understand the impact of both recommendations and laws on the healthcare workers attitudes. The limitation of this study is represented by the fact that the operators most involved in the vaccination are used to participating in training courses regarding immunization, thus leading to an overestimation of favorable opinions and recommendations toward this vaccine without significant differences among the geographical areas.
In Italy the recent introduction of compulsory vaccinations shifted the efforts of the public health system at the expense of recommended vaccinations. A similar phenomenon may also affect other countries where a mandatory vaccinations system has recently been implemented.38–42
It seems that RV vaccination is becoming increasingly popular and we are confident that a greater vaccination coverage could be reached in a short time allowing to obtain an important reduction in severe cases of gastroenteritis. It seems that the education of healthcare workers after the introduction of compulsory vaccinations may prompt them to actively offer also recommended vaccines.
Acknowledgments
The authors thank Dr. Elisa Romiti for helping with the statistical analysis
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.WHO . Rotavirus vaccines WHO position paper. Weekly epidemiological record. 2013. No. 5, 2013, 88, 49–64. https://www.who.int/wer/2013/wer8805.pdf?ua=1.
- 2.Desselberger U. Rotaviruses. Virus Res. 2014;190:75‐96. doi: 10.1016/j.virusres.2014.06.016. [DOI] [PubMed] [Google Scholar]
- 3.Gualano MR, Thomas R, Gili R, Scaioli G, Voglino G, Zotti C. Cost-effectiveness estimates of vaccination against rotavirus in Piedmont, Italy. J Infect Public Health. 2018;11(6):867‐872. doi: 10.1016/j.jiph.2018.07.008. [DOI] [PubMed] [Google Scholar]
- 4.Soriano-Gabarró M, Mrukowicz J, Vesikari T, Verstraeten T. Burden of rotavirus disease in European Union countries. Pediatr Infect Dis J. 2006;25(1 Suppl):S7‐S11. doi: 10.1097/01.inf.0000197622.98559.01. [DOI] [PubMed] [Google Scholar]
- 5.Favaretti C, Di Pietro ML, Kheiraoui F, Capri S, Specchia ML, Cadeddu C, Lovato E, Di Nardo F, Ferriero AM, Mancuso A, et al. Health Technology Assessment della vaccinazione anti-rotavirus con il vaccino Rotarix. QIJPH. 2014;3(7):1–80. [Google Scholar]
- 6.Conforti G Rotavirus: dal racconto alla clinica. Società Italiana di Pediatria. 2016. [accessed 2019 October]. https://www.sip.it/wp-content/uploads/2017/09/Rotavirus.pdf.
- 7.Gervasi G, Capanna A, Mita V, Zaratti L, Franco E. Nosocomial rotavirus infection: an up to date evaluation of European studies. Hum Vaccin Immunother. 2016;12(9):2413‐2418. doi: 10.1080/21645515.2016.1183858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Valentini D, Ianiro G, Di Bartolo I, Di Camillo C, Boccuzzi E, Vittucci AC, Ruggeri FM, Monini M. Hospital-acquired rotavirus and norovirus acute gastroenteritis in a pediatric unit, in 2014-2015. J Med Virol. 2017. October;89(10):1768–74. PMID:28547892. doi: 10.1002/jmv.24866. [DOI] [PubMed] [Google Scholar]
- 9.Ruggeri FM, Fiore L. Vaccine preventable viral diseases and risks associated with waterborne transmission. Ann Ist Super Sanita. 2012;48(4):460–72. PMID: 23247141. doi: 10.4415/ANN_12_04_12. [DOI] [PubMed] [Google Scholar]
- 10.Burnett E, Parashar UD, Tate JE. Global impact of rotavirus vaccination on diarrhea hospitalizations and deaths among children <5 years old: 2006-2019 [published online ahead of print, 2020 Feb 25]. J Infect Dis. 2020:jiaa081. doi: 10.1093/infdis/jiaa081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO . Rotavirus vaccines. WHO position paper. Weekly Epidemiological record. 2007; No. 32, 2007, 82, 285–296. https://www.who.int/wer/2007/wer8232.pdf.
- 12.Gilca V, Sauvageau C, McNeil S, Gemmill IM, Dionne M, Dobson S, Ouakki M, Lavoie F, Duval B. Setting priorities for new vaccination programs by using public health officers and immunization managers opinions. Vaccine. 2008. August 5;26(33):4204–09. PMID: 18582998. doi: 10.1016/j.vaccine.2008.05.061. [DOI] [PubMed] [Google Scholar]
- 13.Gilca V, Boulianne N, Dubé E, Sauvageau C, Ouakki M. Attitudes of nurses toward current and proposed vaccines for public programs: a questionnaire survey. Int J Nurs Stud. 2009. September;46(9):1219–35. PMID: 19349047. doi: 10.1016/j.ijnurstu.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 14.Dubé E, Gilca V, Sauvageau C, Bettinger JA, Boucher FD, McNeil S, Gemmill I, Lavoie F, Ouakki M, Boulianne N. Clinicians’ opinions on new vaccination programs implementation. Vaccine. 2012. June 29;30(31):4632–37. PMID: 22580354. doi: 10.1016/j.vaccine.2012.04.100. [DOI] [PubMed] [Google Scholar]
- 15.Çataklı T, Duyan-Çamurdan A, Aksakal-Baran FN, Güven AE, Beyazova U. Attitudes of physicians concerning vaccines not included in the national immunization schedule. Turk J Pediatr. 2018;60(3):290–97. PMID: 30511542. doi: 10.24953/turkjped.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 16.AIFA . Rapporto sulla sorveglianza postmarketing dei vaccini in Italia – anno. 2013. [accessed 2020 March]. http://www.agenziafarmaco.gov.it/content/rapporto-sulla-sorveglianza-postmarketing-dei-vaccini-italia-anno-2013-0
- 17.EMA . RotaTeq. Annex I. Summary of product characteristics. [accessed 2020 March]. https://www.ema.europa.eu/en/documents/product-information/rotateq-epar-product-information_en.pdf
- 18.EMA . Rotarix. Annex I. Summary of product characteristics. [accessed 2020 March]. https://www.ema.europa.eu/en/documents/product-information/rotarix-epar-product-information_en.pdf
- 19.Lu HL, Ding Y, Goyal H, Xu HG. Association Between Rotavirus Vaccination and Risk of Intussusception Among Neonates and Infants: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019;2(10):e1912458. Published 2019 Oct 2. doi: 10.1001/jamanetworkopen.2019.12458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.CDC . Rotavirus ACIP Vaccine Recommendations. [accessed 2020 March]. https://www.cdc.gov/vaccines/hcp/acip-recs/vacc-specific/rotavirus.html
- 21.ECDC . Vaccine Scheduler in all countries of the European Union. [accessed 2020 January]. https://vaccineschedule.ecdc.europa.eu/Scheduler/ByDisease?SelectedDiseaseId=32&SelectedCountryIdByDisease=−1
- 22.WHO . Rotavirus Vaccine Coverage. [accessed 2020 January]. https://gateway.euro.who.int/en/indicators/cah_32-rotavirus-vaccinecoverage/visualizations/#id=27510
- 23.WHO . Germany: WHO and UNICEF estimates of immunization coverage: 2018 revision. [accessed 2020 January]. https://www.who.int/immunization/monitoring_surveillance/data/deu.pdf
- 24.Walker JL, Andrews NJ, Atchison CJ, Collins S, Allen DJ, Ramsay ME, Ladhani SN, Thomas SL. Effectiveness of oral rotavirus vaccination in England against rotavirus-confirmed and all-cause acute gastroenteritis. Vacc X. 2019. January 4;1:100005. PMID: 31384727; PMCID: PMC6668223. doi: 10.1016/j.jvacx.2019.100005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Public Health England . National rotavirus immunisation programme update: preliminary vaccine coverage for England, February 2016 to July 2016. Health Protection Report. Weekly Rep. 2016;10(32):1–5. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/555048/hpr3216_rtvrs_VC.pdf. [Google Scholar]
- 26.WHO Europe . Rotavirus vaccine coverage. [accessed 2020 March]. https://gateway.euro.who.int/en/indicators/cah_32-rotavirus-vaccine-coverage/visualizations/#id=27510
- 27.Ministero della Salute . Piano Nazionale Prevenzione Vaccinale PNPV 2017-2018. [accessed 2019 October]. http://www.salute.gov.it/imgs/C_17_pubblicazioni_2571_allegato.pdf.
- 28.Ministero della Salute . LEGGE 31 luglio 2017, n. 119. (GU Serie Generale n.182 del 05-08-2017). [accessed 2019 October]. https://www.gazzettaufficiale.it/eli/id/2017/08/5/17G00132/sg
- 29.Costantino C, Restivo V, Tramuto F, Casuccio A, Vitale F. Universal rotavirus vaccination program in Sicily: reduction in health burden and cost despite low vaccination coverage. Hum Vaccin Immunother. 2018;14(9):2297‐2302. doi: 10.1080/21645515.2018.1471306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Report Osservatorio GIMBE 3/2019 . Vaccinazioni in età pediatrica: impatto dell’obbligo sulle coperture vaccinali in Italia. [accessed 2019 October]. https://www.gimbe.org/osservatorio/Report_Osservatorio_GIMBE_2019.03_Coperture_vaccinali_2018.pdf.
- 31.Ministero della Salute . Lettera circolare n. 24641. [accessed 2019 Oct]. http://www.trovanorme.salute.gov.it/norme/renderNormsanPdf?anno=2018&codLeg=65274&parte=1%20&serie=null
- 32.Sjögren E, Ask LS, Örtqvist Å, Asp M. Parental conceptions of the rotavirus vaccine during implementation in Stockholm: A phenomenographic study. J Child Health Care. 2017;21(4):476‐487. doi: 10.1177/1367493517734390. [DOI] [PubMed] [Google Scholar]
- 33.Napolitano F, Ali Adou A, Vastola A, Angelillo IF. Rotavirus Infection and Vaccination: knowledge, Beliefs, and Behaviors among Parents in Italy. Int J Environ Res Public Health. 2019. May 21;16(10):E1807. PMID: 31117274; PMCID: PMC6571979. doi: 10.3390/ijerph16101807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mita V, Arigliani M, Zaratti L, Arigliani R, Franco E. Italian Physicians’ Opinions on Rotavirus Vaccine Implementation. Pathogens. 2017;6(4):56. Published 2017 Nov 3. doi: 10.3390/pathogens6040056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patel MM, Janssen AP, Tardif RR, Herring M, Parashar UD. A qualitative assessment of factors influencing acceptance of a new rotavirus vaccine among health care providers and consumers. BMC Pediatr. 2007;7:32. Published 2007 Oct 18. doi: 10.1186/1471-2431-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Agyeman P, Desgrandchamps D, Vaudaux B, Berger C, Diana A, Heininger U, Siegrist CA, Aebi C. Interpretation of primary care physicians’ attitude regarding rotavirus immunisation using diffusion of innovation theories. Vaccine. 2009. July 30;27(35):4771–75. PMID: 19540950. doi: 10.1016/j.vaccine.2009.05.097. [DOI] [PubMed] [Google Scholar]
- 37..Dubé E, Gilca V, Sauvageau C, Bradet R, Bettinger JA, Boulianne N, Boucher FD, McNeil S, Gemmill I, Lavoie F. Canadian paediatricians’ opinions on rotavirus vaccination. Vaccine. 2011;29(17):3177‐3182. doi: 10.1016/j.vaccine.2011.02.044. [DOI] [PubMed] [Google Scholar]
- 38.Ward JK, Colgrove J, Verger P. Why France is making eight new vaccines mandatory. Vaccine. 2018;36(14):1801‐1803. doi: 10.1016/j.vaccine.2018.02.095. [DOI] [PubMed] [Google Scholar]
- 39.Federal Ministry of Health . The Bundestag adopts the Measles protection Act. [accessed 2020 March]. https://www.bundesgesundheitsministerium.de/measles-protection-act.html#c16712
- 40.Attwell K, Navin MC, Lopalco PL, Jestin C, Reiter S, Omer SB. Recent vaccine mandates in the United States, Europe and Australia: A comparative study. Vaccine. 2018;36(48):7377‐7384. doi: 10.1016/j.vaccine.2018.10.019. [DOI] [PubMed] [Google Scholar]
- 41.Bozzola E, Spina G, Russo R, Bozzola M, Corsello G. Villani A Mandatory vaccinations in European countries, undocumented information, false news and the impact on vaccination uptake: the position of the Italian pediatric society. Ital J Pediatr. 2018;44(1):67, 1‐4. Published 2018 Jun 14. doi: 10.1186/s13052-018-0504-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Drew L. The case for mandatory vaccination. Nature. 2019;575(7784):S58‐S60. doi: 10.1038/d41586-019-03642-w. [DOI] [PubMed] [Google Scholar]


