Abstract
Background
During a pandemic, it is paramount to understand volume changes in Level I trauma so that with appropriate planning and reallocation of resources, these facilities can maintain and even improve life-saving capabilities. Evaluating nonaccidental and accidental trauma can highlight potential areas of improvement in societal behavior and hospital preparedness. These critical questions were proposed to better understand how healthcare leaders might adjust surgeon and team coverage of trauma services as well as prepare from a system standpoint what resources will be needed during a pandemic or similar crisis to maintain services.
Questions/purposes
(1) How did the total observed number of trauma activations, defined as patients who meet mechanism of injury requirements which trigger the notification and aggregation of the trauma team upon entering the emergency department, change during a pandemic and stay-at-home order? (2) How did the proportion of major mechanisms of traumatic injury change during this time period? (3) How did the proportion and absolute numbers of accidental versus nonaccidental traumatic injury in children and adults change during this time period?
Methods
This was a retrospective study of trauma activations at a Level I trauma center in New Orleans, LA, USA, using trauma registry data of all patients presenting to the trauma center from 2017 to 2020. The number of trauma activations during a government mandated coronavirus 2019 (COVID-19) stay-at-home order (from March 20, 2020 to May 14, 2020) was compared with the expected number of activations for the same time period from 2017 to 2019, called “predicted period”. The expected number (predicted period) was assumed based on the linear trend of trauma activations seen in the prior 3 years (2017 to 2019) for the same date range (March 20, 2020 to May 14, 2020). To define the total number of traumatic injuries, account for proportion changes, and evaluate fluctuation in accidental verses nonaccidental trauma, variables including type of traumatic injury (blunt, penetrating, and thermal), and mechanism of injury (gunshot wound, fall, knife wound, motor vehicle collision, assault, burns) were collected for each patient.
Results
There were fewer total trauma activations during the stay-at-home period than during the predicted period (372 versus 532 [95% CI 77 to 122]; p = 0.016). The proportion of penetrating trauma among total activations was greater during the stay-at-home period than during the predicted period (35% [129 of 372] versus 26% [141 of 532]; p = 0.01), while the proportion of blunt trauma was lower during the stay-at-home period than during the predicted period (63 % [236 of 372] versus 71% [376 of 532]; p = 0.02). The proportion of gunshot wounds in relation to total activations was greater during the stay-at-home period than expected (26% [97 of 372] versus 18% [96 of 532]; p = 0.004). There were fewer motor vehicle collisions in relation to total activations during the stay-at-home period than expected (42% [156 of 372] versus 49% [263 of 532]; p = 0.03). Among total trauma activations, the stay-at-home period had a lower proportion of accidental injuries than the predicted period (55% [203 of 372] versus 61% [326 of 532]; p = 0.05), and there was a greater proportion of nonaccidental injuries than the predicted period (37% [137 of 372] versus 27% [143 of 532]; p < 0.001). In adults, the stay-at-home period had a greater proportion of nonaccidental injuries than the predicted period (38% [123 of 328] versus 26% [123 of 466]; p < 0.001). There was no difference between the stay-at-home period and predicted period in nonaccidental and accidental injuries among children.
Conclusion
Data from the trauma registry at our region’s only Level I trauma center indicate that a stay-at-home order during the COVID-19 pandemic was associated with a 70% reduction in the number of traumatic injuries, and the types of injuries shifted from more accidental blunt trauma to more nonaccidental penetrating trauma. Non-accidental trauma, including gunshot wounds, increased during this period, which suggest community awareness, crisis de-escalation strategies, and programs need to be created to address violence in the community. Understanding these changes allows for adjustments in staffing schedules. Surgeons and trauma teams could allow for longer shifts between changeover, decreasing viral exposure because the volume of work would be lower. Understanding the shift in injury could also lead to a change in specialists covering call. With the often limited availability of orthopaedic trauma-trained surgeons who can perform life-saving pelvis and acetabular surgery, this data may be used to mitigate exposure of these surgeons during pandemic situations.
Level of Evidence
Level III, therapeutic study.
Introduction
Level I trauma centers are comprehensive regional hospitals that function as tertiary care facilities capable of providing total care for every aspect of injuries. Trauma remains the leading cause of death for people between 1 and 44 years old [5], thus commanding a large share of hospital resources and funding. Because of the volume of resources used at these facilities, such as personal protective equipment, medical devices, medications, and required personnel, volume alterations can greatly restrict access to care and alter cost of care.
The World Health Organization declared the outbreak of coronavirus 2019 (COVID-19) a public health emergency of international concern on January 30, 2020 and a pandemic on March 11, 2020 [31, 32]. With the rapid depletion of resources both nationally and worldwide [20], public health measures were taken to minimize the disease transmission rate and adjust resources to continue providing care for all patients and minimize the inpatient burden caused by COVID-19 [1]. These measures most notably took the form of stay-at-home orders, which have been shown to decrease the COVID-19 transmission rate compared with areas without such mandates [9, 16].
Stay-at-home orders during the COVID-19 pandemic have changed the volume of injury presenting to trauma centers and reporting areas with studies to date demonstrating total trauma volume has decreased at their respective hospital systems. Although there has been some investigation into the make-up of the total trauma loss, the focus has been largely accidental trauma, such as motor vehicle collisions [26]. Only one publication addresses penetrating trauma during this period [19]; however, it did not further characterize mechanism of injury. The present study is currently the only study that we know of to investigate the various forms of accidental trauma during the stay-at-home period in addition to nonaccidental trauma and how proportions and absolute numbers change. COVID-19 infection rates have been shown to be higher in trauma patients [12] and in areas with more shootings [19], thus suggesting the need to focus resources and education in these areas.
Therefore, we asked, (1) How did the total observed number of trauma activations, defined as patients who meet mechanism of injury requirements which trigger the notification and aggregation of the trauma team upon entering the emergency department, change during a pandemic and stay-at-home order? (2) How did the proportion of major mechanisms of traumatic injury change during this time period? (3) How did the proportion and absolute numbers of accidental versus nonaccidental traumatic injury in children and adults change during this time period?
Patients and Methods
Study Design and Setting
This was a retrospective cross-sectional study at University Medical Center (UMC), a Level I trauma center in New Orleans, LA, USA, comparing the total number of trauma activations and type of traumatic injury during a government-mandated stay-at-home order (March 20, 2020 to May 14, 2020) with expected values for trauma activations and type of injury derived from a linear best fit model based on the previous 3 years’ data. The study received institutional review board approval before the start of the investigation.
Participants and Study Groups
We queried patient records from a trauma registry of all patients with trauma activations at UMC in 2017 to 2020 between the dates of March 20 and May 14. Trauma activations were defined as patients presenting to the emergency department that met the American College of Surgeons Committee of Trauma Guidelines (ACS COT) criteria for major trauma [22]. We excluded patients from the study if they were not activated as a trauma case. The stay-at-home group was defined as those patients who had trauma activations between March 20, 2020 and May 14, 2020. Pre-pandemic patients were defined as patients who had trauma activations between March 20 and May 14 in 2017, 2018, and 2019.
Since its opening in 2015, the volume of trauma at UMC has been steadily increasing annually. As such, the expected trauma volume for 2020 would be underestimated if based directly off data from the pre-pandemic period. Instead, we used a linear best fit model to predict the expected trauma volume for 2020 to account for the growing capacity of UMC.
Variables Studied and Their Definitions
Collected demographic variables included patient characteristics (age, race, gender) and type of traumatic injury (Table 1). Patient characteristics were collected for descriptive purposes and to investigate if there were any unexpected differences in patients presenting to the ED during the stay-at-home versus the pre-pandemic period. In particular, the pediatric (age < 18) and adult patient populations (age > 18) were examined for differences in accidental versus nonaccidental trauma.
Table 1.
Demographics of patients with trauma
| Factor | Pre-pandemic period % (n) (n = 1461) |
Stay-at-home period % (n) (n = 372) |
p value |
| Gender | 0.17 | ||
| Women | 25 (372) | 22 (82) | |
| Men | 75 (1089) | 78 (290) | |
| Racea | 0.92 | ||
| Asian | 1 (18) | 1 (3) | |
| Black | 52 (759) | 54 (201) | |
| White | 39 (577) | 38 (143) | |
| Hispanic/Latino | 6 (82) | 5 (19) | |
| Other | 2 (22) | 2 (6) | |
| Age groups in years | 0.45 | ||
| 0-18 | 12 (180) | 12 (44) | |
| 18-24 | 16 (235) | 17 (63) | |
| 25-35 | 25 (361) | 22 (82) | |
| 36-45 | 14 (198) | 17 (64) | |
| 46-55 | 14 (200) | 15 (54) | |
| 56-65 | 12 (170) | 10 (36) | |
| > 66 | 8 (117) | 8 (29) |
Race determined by patient self-report during initial patient evaluation.
We organized traumatic injury type by activation level (Table 2), injury type, and mechanism of injury. Activation level was based on physiologic criteria, anatomic criteria, and the mechanism of injury (see Appendix; Supplemental Digital Content 1, http://links.lww.com/CORR/A417). Injury types were broadly defined as blunt, penetrating, and thermal trauma. We classified the mechanism of injury as gunshot wounds, falls, knife or sharp wounds, motor vehicle collisions, assault with a blunt object, assault with bodily force, burns, miscellaneous injuries, and unspecified injuries, based on the ICD-9 and ICD-10 diagnosis codes.
Table 2.
Predicted and actual number of patients with trauma in 2020 based on trauma injury type and activation level
| Type of trauma | Percent of predicted patients with trauma % (n) (n = 532) | Percent of actual patients with trauma 2020 % (n) (n = 372) | p value |
| Blunt | 71 (376) | 63 (236) | 0.02 |
| Penetrating | 26 (141) | 35 (129) | 0.01 |
| Thermal | 3 (15) | 2 (7) | 0.37 |
| Tier 1 | 45 (237) | 50 (184) | 0.17 |
| Tier 2 | 56 (295) | 51 (188) |
We further categorized the mechanism of injury by intent (accidental versus nonaccidental) and respective subtypes (Table 3). Gunshot wounds were defined as injuries from the use of a firearm, as defined by US Federal law; that is, any weapon capable of expelling a projectile by explosive force [29]. These included handguns, shotguns, and rifles of any caliber or grade. Among gunshot wounds, law enforcement-related injuries defined as those sustained by either the suspect or the officer during an episode of confrontation. High-level falls were defined as those occurring from distances greater than standing height; those from standing height or below were termed same-level falls. Among motor vehicle collisions, those involving pedestrians or bicycles were named pedestrian motor vehicle collisions and bicycle motor vehicle collisions, respectively. Off-road vehicle referred to vehicles designed for driving over unpaved terrain only. This included dirt bikes and all-terrain vehicles. Mechanisms of injury that were explicit but extremely infrequent, such as being bitten by an alligator, were grouped together as miscellaneous. Information from mechanism of injury were further grouped into just assault type injuries (Table 4), as well as categorized into accidental versus nonaccidental type injuries (Table 5).
Table 3.
Predicted and actual number of patients with trauma in 2020 based on the mechanism of injury and injury category
| Mechanism of injury | Accidental vs nonaccidental | Category | Predicted number of patients with trauma in 2020, n (%)a (n = 532) |
Actual number of patients with trauma in 2020, n (%) (n = 372) |
p value |
| Gunshot wounds | Total | 18% (96) | 26% (97) | 0.004 | |
| Accidental | Accidental gunshot wound | 7% (7) | 3% (3) | 0.33 | |
| nonaccidental | Assault with firearm | 90% (86) | 87% (84) | > 0.99 | |
| Intentional self-harm | 3% (3) | 2% (2) | > 0.99 | ||
| Law enforcement-related | 0% (0) | 5% (5) | 0.03 | ||
| Falls | Total | 14% (74) | 14% (52) | > 0.99 | |
| Accidental | High-level falls | 29% (21) | 29% (15) | > 0.99 | |
| Same-level falls | 59% (44) | 62% (32) | 0.86 | ||
| nonaccidental | Intentional self-harm | 1% (1) | 8% (4) | 0.16 | |
| Unspecified | 11% (8) | 2% (1) | 0.08 | ||
| Knife or sharp wounds | Total | 8% (42) | 9% (32) | 0.71 | |
| nonaccidental | Assault | 75% (31) | 88% (28) | 0.24 | |
| Intentional self-harm | 11% (5) | 9% (3) | > 0.99 | ||
| Unspecified | 13% (5) | 3% (1) | 0.22 | ||
| Motor vehicle collisions | Total | 49% (263) | 42% (156) | 0.03 | |
| Accidental | Cars or trucks | 46% (120) | 62% (96) | 0.002 | |
| Bicycle | 6% (16) | 8% (12) | 0.55 | ||
| Motorcycles | 17% (46) | 14% (22) | 0.41 | ||
| Pedestrian | 17% (46) | 8% (13) | 0.01 | ||
| Off-road vehicles | 3% (7) | 7% (11) | 0.04 | ||
| nonaccidental | Assault | 1% (2) | 0% (0) | 0.53 | |
| Intentional self-harm | 0% (0) | 1% (2) | 0.14 | ||
| Unspecified | 10% (26) | 0% (0) | < 0.001 | ||
| Burns | Accidental | Total | 3% (13) | 2% (7) | 0.65 |
| Miscellaneous | Total | 5% (12) | 3% (26) | 0.24 | |
| Unspecified | Total | 1% (4) | 1% (5) | 0.50 |
Predicted values are based on rounded expected percentages; percentage values may not add up to total number in each category.
Table 4.
Predicted and actual patients with trauma in 2020 based on assault category
| Assault type | Predicted number of patients with trauma in 2020 (n = 532) | Actual number of patients with trauma in 2020 (n = 372) | p value |
| Total | 26 (136)a | 34 (127) | 0.01 |
| Blunt object | 4 (6) | 2 (3) | 0.50 |
| Firearm | 63 (86) | 69 (87) | 0.44 |
| Knife or sharp object | 23 (31) | 21 (27) | > 0.99 |
| Motor vehicle | 1 (2) | 0 (0) | 0.50 |
| Bodily force | 1 (2) | 0 (0) | > 0.99 |
| Unspecified | 7 (9) | 6 (8) | > 0.99 |
Predicted values are based on rounded expected percentages, percentage values may not add up to total number in each category.
Table 5.
Accidental versus nonaccidental trauma in adults and pediatric patients
| Adult | Child | |||||
| Type | Predicted adult trauma, % (n) (n = 466)a | Actual adult trauma % (n) (n = 328) | p value | Actual pediatric trauma % (n) (n = 44) | Predicted pediatric trauma % (n) (n = 66)a |
p value |
| Accidental | 58 (269) | 55 (182) | 0.53 | 50 (22) | 56 (37) | 0.56 |
| nonaccidental | 26 (123) | 38 (123) | < .001 | 43 (19) | 29 (19) | 0.18 |
| Other | 16 (74) | 7 (23) | 7 (3) | 14 (9) | ||
Predicted values are based on rounded expected percentages, percentage values may not add up to total number in each category.
Primary and Secondary Study Outcomes
The primary outcome of the study was to assess whether the stay-at-home order affected the number of trauma activations. This was calculated by comparing the actual number of trauma injuries in 2020 to the expected number of trauma injuries projected from the volume of patient’s treated in 2017 to 2019 between the dates of March 20 and May 14.
The secondary study outcome was to assess whether the mechanism of injury, including the intent of the injury (accidental versus nonaccidental) and type of injury during the stay-at-home period was different than the predicted period. We assessed this by comparing actual injuries during the stay-at-home period with the predicted values.
Statistical Analysis
Categorical variables were compared using Yates’s chi-square and Fisher’s exact test. The total trauma volume per year was compared using a one-way repeated-measures ANOVA with Bonferroni’s post hoc test analysis. The mean number of daily trauma activations increased from 2017 (8.38 ± 3.53) to 2018 (8.53 ± 4.30) to 2019 (9.18 ± 4.26) (Fig. 1), with a slight linear trend (p = 0.04, η2 = 0.08). Because of the linear trend in the data from 2017 to 2019, we used a linear regression curve to predict the expected trauma patient number in 2020 (predicted period) compared with that during the stay-at-home period. The observed number of trauma activations during the stay-at-home period was less than the expected number of trauma activations (372 versus 532) that was predicted based on a linear regression equation (Y=22.50*X-44918) of patients from 2017, 2018, and 2019 (372 versus 532 [95% CI 77 to 122]; p = 0.02). We then compared these predicted values (predicted period) with the actual values as reported by the registry (stay-at-home). P values of less than 0.05 were considered statistically significant, and confidence intervals associated with these values are provided when measurements of the degree of uncertainty or certainty in a sampling method were indicated [14]. The analysis was conducted using IBM SPSS Statistics for Macintosh, Version 24.0 (IBM Corp, Armonk, NY, USA). There were no outliers and the data were normally distributed at each timepoint, as assessed by a boxplot and Shapiro-Wilk’s test (p > 0.05).
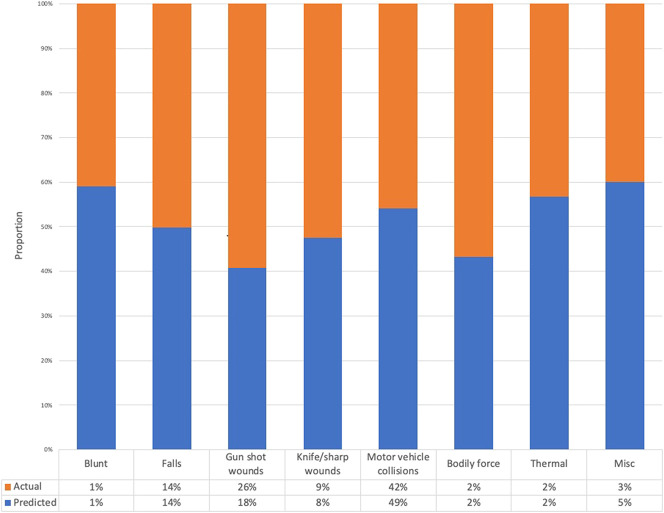
Fig. 1.
This graph shows the predicted number of patients with trauma injuries and the actual number during the stay-at-home period, based on the mechanism of injury.
Patient Demographics
There were 1461 total trauma injuries in the pre-pandemic period, and 372 injuries during the stay-at-home period. Most patients in the pre-pandemic period (76% [1089 of 1461]) and stay-at-home (78% [290 of 372]) were men. Most trauma patients in the pre-pandemic period (52% [759 of 1461]) and stay-at-home period (54% [201 of 372]) were Black. There was no difference in gender, race, or age between the pre-pandemic years (2017 to 2019) and the stay-at-home period in 2020 (Table 1).
Results
Observed versus Predicted Number of Trauma Activations During COVID-19
Among the trauma activations, there was no difference in the proportions of Tier 1 activations (45% [237 of 532] versus 50% [184 of 372]; p = 0.17) and Tier 2 (56% [295 of 532] versus 51% [188 of 372] p = 0.17) activations (between the stay-at-home and predicted periods (Table 2).
Changes in Trauma Mechanisms During the Stay-at-Home Order
When we examined the types of trauma in relation to the total number of activations, we found that the proportion of blunt trauma was lower during stay-at-home period compared with the predicted period (63% [236 of 372] versus 71% [376 of 532]; p = 0.02), while there was a greater proportion of penetrating trauma (35% [129 of 372] versus 26% [141 of 532]; p = 0.01). No differences were seen in the proportion of thermal trauma. The proportion of gunshot wounds in relation to total activations was greater than expected during the stay-at-home period (26% [97 of 372] versus 18% [96 of 532]; p = 0.004) (Fig. 1). There were fewer motor vehicle collisions in relation to total activations than expected during the stay-at-home period (42% [156 of 372] versus 49% [263 of 532]; p = 0.03) (Table 3). When we studied the mechanisms of traumatic injuries in relation to the total number of activations, we found there were no differences between the stay-at-home and predicted periods in the proportions of assault with a blunt object, assault with bodily force, burns, falls, or knife or sharp wounds (Table 4).
Proportion of Accidental versus Nonaccidental Injuries
With respect to total trauma activations, the stay-at-home period had a lower proportion of accidental injuries than the predicted period (55% [203 of 372] versus 61% [326 of 532]; p = 0.05), and there was a greater proportion of nonaccidental injuries than the predicted matched date period (37% [137 of 372] versus 27% [143 of 532]; p < 0.001). When we examined accidental injuries among adults and children, we found no difference between the stay-at-home period and predicted period (Table 5).
There were fewer motor vehicle collisions during the stay-at-home period than expected (42% [156 of 372] versus 49% [263 of 532]; p = 0.03). However, motor vehicle collisions involving cars or trucks comprised a greater proportion of total activations than expected (62% [96 of 156] versus 46% [120 of 263]; p = 0.002) (Fig. 1). The stay-at-home period also had a greater proportion of off-road vehicle collisions in relation to total activations than the predicted period (7% [11 of 156] versus 3% [7 of 263]; p = 0.04). There were fewer pedestrian-involved motor vehicle collisions during the stay-at-home period than during the predicted period (8% [13 of 156] versus 17% [46 of 263]; p = 0.01), representing more than 93% fewer instances of pedestrian versus motor vehicle collisions than expected.
The proportion of all nonaccidental injuries compared with total activations was greater than predicted during the stay-at-home period compared with predicted period (37% [137 of 372] versus 27% [143 of 532]; p < 0.001). When we studied nonaccidental injuries in adults specifically, we found that total activations were greater than predicted during the stay-at-home period compared with the predicted period (38% [123 of 328] versus 26% [123 of 466]; p < 0.001). There was no difference in nonaccidental injuries in children (Table 5).
The proportion of assault injuries in relation to total activations was greater during the stay-at-home period compared with the predicted period (34% [127 of 372] versus 26% [136 of 532]), although there was no difference in the proportion for any of the assault subcategories alone. Law enforcement-related gunshot wounds (n = 5, including two suspect and three police officer injuries) were greater in proportion to total activations during the stay-at-home period than during the predicted period (5% [5 of 97] versus 0% [0 of 96]; p = 0.03). Finally, there was no change in the number of intentional self-harm injuries in relation to total activations between the stay-at-home period and the predicted period (3% [11 of 372] versus 2% [9 of 532]; p = 0.20).
Discussion
Hospitals in major urban areas during the peak spread of COVID-19 were forced to adjust resources to keep intensive care units available for an increase in COVID-19 admissions while maintaining the ability to care for both trauma and medical events not related to the pandemic. This included the recruitment of physicians from specialties that do not routinely provide intensive medical care [15]. Many centers, both domestic and abroad, reported having nursing duties and staffing of medical wards performed by surgical subspecialists to meet demand [6, 13, 24, 30]. Understanding a change in volume is paramount to effectively resource allocation. Identifying potentially preventable nonaccidental trauma could further mitigate the amount of trauma presenting during a crisis. With more accurate volume predictions, call teams could potentially work longer shifts, limiting an individual’s viral exposure and decreasing the potential for quarantine. The continued nonaccidental trauma in the context of decreased overall human activity found in this study also suggests that violence-mitigation strategies in the community should be explored.
Limitations
There are several limitations to this study. First, the predictive modeling for the expected volume of trauma patients during the stay-at-home period was limited to the use of a linear trend model. This linear relationship of the pre-pandemic data was, however, validated by a repeated measures ANOVA with trend analysis. Given the trauma center opening in 2015 and the increasing overall volume at the center, we felt a linear trend model best captured expected volume for 2020. However, this linear trend model may have overpredicted expected numbers compared with an average of the preceding years.
Second, the year-to-year variability of major social events in New Orleans may affect the predictive ability of model, especially with the tourist-heavy nature of the city. However, the study period of March 20 to May 14 in 2017 through 2020 were consistent in excluding large city events such as Mardi Gras, the St. Patrick’s Day Parade, and Jazz Fest. Therefore, it was felt that no correction for catchment population was necessary.
Third, the generalizability of the results for future stay-at-home orders may be limited. Louisiana was among the early hotspots for COVID-19 infection in the United States [18]. Although the stay-at-home order began on March 20, 2020, schools, businesses, and festivities had already begun closing as early as March 11, 2020. Knowledge of the pandemic could have affected the habits of the population before the formal institution of the mandate, such that the results may not reflect the changes in activity caused by a sudden stay-at-home order. Variation in adherence to the stay-at-home order was also a consideration because population adherence to the mandate could not be determined. However, the present study demonstrates enough activity was altered by the stay-at-home order such that the number and proportions of traumatic injury were substantially changed and could be a surrogate marker for adherence. However, moving forward, because a relatively early stay-at-home order period was examined, this may underestimate future adherence due to later quarantine fatigue.
Fourth, the identification of the mechanism of injury was limited to coding by ICD-9 and ICD-10 diagnosis codes. Due to the user-dependent nature of the initial reporting, the data entered in the registry are subject to variability [34]. However, the trauma registry is overseen by a dedicated team that directly interviews all patients and family that are admitted to the trauma center. Additionally, the findings are confirmed by faculty during daily morning meetings discussing admissions and mechanisms. Prior work found that in certain trauma activations, ICD-10 codes have had substantial agreement with direct interview, with increased accuracy among broader classifications [2]. Some reported mechanisms of injury were either unspecified or too vague to qualify as part of any of the major types of traumatic injury groups. Both unspecified and miscellaneous mechanisms, however, were evenly and randomly distributed across all years and only contributed to a small percentage of the total number of traumas.
Lastly, this trauma registry did not categorize domestic assault or violence. Increasing awareness of domestic violence as a substantial mechanism of injury could allow providers to better treat and provide resources to survivors [7]. Early data demonstrated increased risks for victims of domestic violence and assault as well as increased violence toward adolescents and children [17, 21]. The full impact of COVID-19 on individual behavior and physical and mental health may not be apparent until 1 year after the pandemic. Multiple cities have reported increased domestic violence during mandatory stay-at-home periods [4]. Because musculoskeletal injury is a common physical condition in the emergency department (28%) second only to head and neck trauma (40%), in instances of domestic violence, providers need better tools to identify victims [3]. Future studies could address this limitation by using a screening program in the emergency department to detect partner or domestic violence [8].
Observed versus Predicted Number of Trauma Activations During COVID-19
The trauma registry data from Southeast Louisiana’s only Level I trauma center indicated that the stay-at-home order had a substantial effect on the number of trauma injuries, with total activations being less than 70% of the predicted value. There was also a change in the proportions of mechanisms of injury compared with predicted modeling. Similar decreases in trauma activations have been demonstrated at other Level I trauma centers in the United States and other impacted countries worldwide [11, 13]. In a period of normal patient activity, attendings typically are on call for no more than 24 hours. With this reduction in volume, teams can potentially work longer shifts to decrease exposure risks and implement strategic turnovers to mitigate exposure risk [23].
Changes in Trauma Mechanisms During the Stay-at-Home Order
At our trauma center, motor vehicle collisions accounted for the highest number of activations for all years of available data. During the stay-at-home period, motor vehicle collision-related trauma was 40% less than predicted. This is consistent with the finding that there was 64% less motor vehicle traffic in New Orleans than during the same time period in 2019, according to the TomTom traffic index [28]. Similarly, in California, the University of California Davis Road Ecology Center demonstrated a 20% to 50% reduction in vehicle traffic on major highways during a shelter-in-place order, resulting in a 50% reduction in motor vehicle collisions and associated traumatic injuries [25]. Therefore, motor vehicle collisions could be used as a surrogate marker for adherence to a stay-at-home order in a major city.
Proportion of Accidental Versus Nonaccidental Injuries
Nonaccidental injuries in adults were more frequent than predicted, while both nonaccidental and accidental injuries in children did not change. Furr et al. [10] conducted a meta-analysis of posttraumatic stress disorder related to natural or man-made disasters, finding that studies that examined psychological and behavioral changes within 1 year after a disaster were more likely to observe effects. The second-largest volume of trauma activations at this trauma center were gunshot wounds, which rose disproportionally during the stay-at-home period in New Orleans relative to its predicted value. Based on the previous years’ data, the predicted number of gunshot wounds for the stay-at-home period was 96. There were 97 observed gunshot wounds, demonstrating the number of gunshot wounds was essentially unchanged by the stay-at-home order in contrast to all other mechanisms which decreased. Given the decrease in most other types of trauma during this time, the percentage of gunshot wounds increased to 26% of trauma activations compared with the predicted 18%. This data is in line with those of other major cities including New York City, Chicago, Los Angeles, and Baltimore, where gun violence has increased during the COVID-19 pandemic [27]. In prior studies of trauma decrease during the pandemic [12, 19, 26, 33], there was no examination of nonaccidental trauma. This data can be used to plan surgical team coverage by allowing for longer shifts for both surgeons and nurses to limit viral exposure. With polytrauma volume decreasing, departmental leadership can also use nonorthopaedic trauma surgeons to take more call, preserving the trauma-trained surgeons from quarantine, who nearly exclusively are the surgeons performing life-saving pelvis and acetabular fracture care. The method used can also be replicated at regional institutions to identify how their specific community needs and volume changes. In urban communities that parallel our demographics, we also suggest implementation of community outreach programs to facilitate de-escalation strategies and conflict resolution within the population.
Conclusion
Tertiary Level I trauma centers are essential and must retain the ability to take care of patients with trauma, and consequently planning and resource management are paramount during crises. With a decrease in trauma volume, healthcare leaders can adjust scheduling to limit exposure of health care providers to a viral agent by increasing the length of shifts worked and decreasing turnover. With the unexpected increase of nonaccidental trauma, this paper highlights that community programs centered on violence de-escalation should be instituted and highlighted to the community for violence mitigation which will also decrease hospital resource depletion.
Supplementary Material
Acknowledgments
We thank Vicki Holloway RHIA, CCS, for helping with the trauma registry data collection.
Footnotes
Each author certifies that neither he nor she, nor any members of his or her immeidate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
This work was performed at University Medical Center, Tulane University School of Medicine, New Orleans, LA, USA.
The first three authors contributed equally to this manuscript.
References
- 1.Bartsch SM, Ferguson MC, McKinnell JA, O'Shea KJ, Wedlock PT, Siegmund SS, Lee BY. The potential health care costs and resource use associated with COVID-19 in the United States. Health Affairs. 2020;39:927-935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beck B, Ekegren CL, Cameron P, Stevenson M, Judson R, Bucknill A, Edwards E, Gabbe B. Comparing ICD-10 external cause codes for pedal cyclists with self-reported crash details. Inj Prev. 2018;24:157-160. [DOI] [PubMed] [Google Scholar]
- 3.Bhandari M, Dosanjh S, Tornetta P, 3rd, Matthews D. Musculoskeletal manifestations of physical abuse after intimate partner violence. J Trauma. 2006;61:1473-1479. [DOI] [PubMed] [Google Scholar]
- 4.Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med. [Published online ahead of print April 28, 2020]. DOI: 10.1016/j.ajem.2020.04.077. [DOI] [PMC free article] [PubMed]
- 5.Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) Fatal Injury Data. Available at: https://www.cdc.gov/injury/wisqars/index.html. Accessed June 4, 2020.
- 6.Coccolini F, Perrone G, Chiarugi M, Di Marzo F, Ansaloni L, Scandroglio I, Marini P, Zago M, De Paolis P, Forfori F, Agresta F, Puzziello A, D'Ugo D, Bignami E, Bellini V, Vitali P, Petrini F, Pifferi B, Corradi F, Tarasconi A, Pattonieri V, Bonati E, Tritapepe L, Agnoletti V, Corbella D, Sartelli M, Catena F. Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020;15:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis JW, Parks SN, Kaups KL, Bennink LD, Bilello JF. Victims of domestic violence on the trauma service: unrecognized and underreported. J Trauma. 2003;54:352-355. [DOI] [PubMed] [Google Scholar]
- 8.Feldhaus KM, Koziol-McLain J, Amsbury HL, Norton IM, Lowenstein SR, Abbott JT. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. JAMA. 1997;277:1357-1361. [PubMed] [Google Scholar]
- 9.Friedson AI, McNichols D, Sabia JJ, Dave D. Did California's shelter-in-place order work? Early coronavirus-related public health effects. San Diego State University: National Bureau of Economic Research; Available at: https://www.nber.org/papers/w26992. Accessed June 5, 2020. [Google Scholar]
- 10.Furr JM, Comer JS, Edmunds JM, Kendall PC. Disasters and youth: a meta-analytic examination of posttraumatic stress. J Consult Clin Psych. 2010;78:765-780. [DOI] [PubMed] [Google Scholar]
- 11.Govern P. Fewer accidents, social distancing spur drop in trauma volumes. VUMC Reporter. Available at: https://news.vumc.org/2020/04/23/fewer-accidents-social-distancing-spur-drop-in-trauma-volumes/. Accessed June 6, 2020.
- 12.Hernigou J, Morel X, Callewier A, Bath O, Hernigou P. Staying home during "COVID-19" decreased fractures, but trauma did not quarantine in one hundred and twelve adults and twenty eight children and the "tsunami of recommendations" could not lockdown twelve elective operations. Int Orthop. 2020;44:1473-1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keeley C, Long TG, Cineas N, Villanueva Y, Bell D, Wallach AB, Mendez-Justiniano I, Jackson H, Boyle Schwartz D, Jimenez J, Salway RJ, Boudourakis L. Staffing up for the surge: Expanding the New York City public hospital workforce during the COVID-19 pandemic. Health Affairs.[Published online ahead of print June 11, 2020]. DOI: 10.1377/hlthaff.2020.00904. [DOI] [PubMed]
- 14.Leopold SS, Porcher R. Editorial: Threshold p values in orthopaedic research-We know the problem. What is the solution? Clin Orthop Related Res. 2018;476:1689-1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lockey SD. What's important: What is our role in the COVID-19 pandemic? J Bone Joint Surg Am. 2020;102:931-932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lyu W, Wehby GL. Comparison of estimated rates of coronavirus disease 2019 (COVID-19) in border counties in Iowa without a stay-at-home order and border counties in Illinois with a stay-at-home order. JAMA Netw Open. 2020;3:e2011102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marques ES, Moraes CL, Hasselmann MH, Deslandes SF, Reichenheim ME. Violence against women, children, and adolescents during the COVID-19 pandemic: overview, contributing factors, and mitigating measures. Cad Saude Publica. 2020;36:e00074420. [DOI] [PubMed] [Google Scholar]
- 18.Nowak J. See where New Orleans, rest of Louisiana ranks in per capita coronavirus cases, deaths The New Orleans Advocate. Available at: https://www.nola.com/news/coronavirus/article_d03835c6-7e54-11ea-a1dc-4fa29fa942ff.html. Accessed May 29, 2020.
- 19.Qasim Z, Sjoholm LO, Volgraf J, Sailes S, Nance ML, Perks DH, Grewal H, Meyer LK, Walker J, Koenig GJ, Donnelly J, Gallagher J, Kaufman E, Kaplan MJ, Cannon JW. Trauma center activity and surge response during the early phase of the COVID-19 pandemic – the Philadelphia story. J Trauma Acute Care Surg. [Published online ahead of print June 29, 2020]. DOI: 10.1097/TA.0000000000002859. [DOI] [PMC free article] [PubMed]
- 20.Ranney ML, Griffeth V, Jha AK. Critical supply shortages - The need for ventilators and personal protective equipment during the Covid-19 pandemic. New Engl J Med. 2020;382:e41. [DOI] [PubMed] [Google Scholar]
- 21.Roesch E, Amin A, Gupta J, García-Moreno C. Violence against women during covid-19 pandemic restrictions. BMJ. 2020;369:m1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sasser SM, Hunt RC, Faul M, Sugerman D, Pearson WS, Dulski T, Wald MM, Jurkovich GJ, Newgard CD, Lerner EB. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61:1-20. [PubMed] [Google Scholar]
- 23.Schwartz AM, Wilson JM, Boden SD, Moore TJJ, Bradbury TLJ, Fletcher ND. Managing resident workforce and education during the COVID-19 pandemic: evolving strategies and lessons learned. JBJS Open Access. 2020;5:e0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheth PD, Simons JP, Robichaud DI, Ciaranello AL, Schanzer A. Development of a surgical workforce access team in the battle against COVID-19. J Vasc Surg. 2020;72:414-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shilling F, Waetjen D. Special report (update): Impact of COVID-19 mitigation on numbers and costs of California traffic crashes. UC Davis; 2020; Available at: https://roadecology.ucdavis.edu/files/content/projects/COVID_CHIPs_Impacts_updated_415.pdf. Accessed June 4, 2020. [Google Scholar]
- 26.Stoker S, McDaniel D, Crean T, Maddox J, Jawanda G, Krentz N, Best J, Speicher M, Siwiec R. The effect of shelter-in-place orders and the COVID-19 pandemic on orthopaedic trauma at a community level II trauma center. J Orthop Trauma.[Published online ahead of print June 8, 2020]. DOI: 10.1097/BOT.0000000000001860. [DOI] [PMC free article] [PubMed]
- 27.Sutherland M, McKenney M, Elkbuli A. Gun violence during COVID-19 pandemic: Paradoxical trends in New York City, Chicago, Los Angeles and Baltimore. Am J Emerg Med; [Published online ahead of print May 7, 2020]. DOI: 10.1016/j.ajem.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.TomTom. New Orleans Traffic. Available at: https://www.tomtom.com/en_gb/traffic-index/new-orleans-traffic/. Accessed June 3, 2020.
- 29.United States Congress. Gun Control Act of 1968. 18 U.S.C. § 921(a)(3)(c)1968. [Google Scholar]
- 30.Uppal A, Silvestri DM, Siegler M, Natsui S, Boudourakis L, Salway RJ, Parikh M, Agoritsas K, Cho HJ, Gulati R, Nunez M, Hulbanni A, Flaherty C, Iavicoli L, Cineas N, Kanter M, Kessler S, Rhodes KV, Bouton M, Wei EK. Critical care and emergency department response at the epicenter of the COVID-19 pandemic. Health Affairs. [Published online ahead of print June 11, 2020]. DOI: 10.1377/hlthaff.2020.00901. [DOI] [PubMed]
- 31.World Health Organization Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Available at: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov). Accessed May 1, 2020.
- 32.World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19. Available at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---29-june-2020. Accessed May 1, 2020.
- 33.Zagra L, Faraldi M, Pregliasco F, Vinci A, Lombardi G, Ottaiano I, Accetta R, Perazzo P, D'Apolito R. Changes of clinical activities in an orthopaedic institute in North Italy during the spread of COVID-19 pandemic: a seven-week observational analysis. Int Orthop. 2020; 44:1591-1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zoltie N, de Dombal FT. The hit and miss of ISS and TRISS. Yorkshire Trauma Audit Group. BMJ. 1993;307:906-909. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.