Abstract
Objective:
To assess the state of peer-reviewed literature surrounding uptake and adherence of antiretroviral therapy (ART) among HIV-positive women who use drugs (WWUD).
Methods:
Consistent with PRISMA-ScR guidelines, we conducted a scoping literature review on ART uptake and adherence among WWUD, searching PubMed, Embase, CINAHL, PsycInfo, and Sociological Abstracts. Eligibility criteria included: reporting at least one ART uptake or adherence related result among WWUD aged 18 or older; peer-reviewed; published in English between 1996-2018.
Results:
Our search identified 6,735 studies; 86 met eligibility requirements. ART uptake ranged from 30% to 76% and adherence ranged from 27% to 95%. Substance use, co-morbid psychiatric disorders, and side effects emerged as the primary ART uptake and adherence barriers among this population. Few facilitators were identified.
Conclusion:
This study is the first scoping review to look at ART uptake and adherence among WWUD globally. The wide range in uptake and adherence outcomes indicates the need for gold standard assessments, which may differ between high and low resource settings. This study offers rich insight into uptake and adherence barriers and facilitators, primarily at the intrapersonal level. More research is needed to examine interventions that focus on additional levels of the SEM (e.g., community and policy levels). These review findings can inform ART interventions, future research, and offer guidance to other support services with WWUD, such as PrEP interventions.
Keywords: Antiretroviral therapy (ART), Women who use drugs (WWUD), Scoping review
1. Introduction
Human Immunodeficiency Virus (HIV) prevalence ranged from 0% - 65% among women who use drugs (WWUD) globally(Larney et al., 2015). WWUD experience higher rates of HIV compared to men who use drugs in most countries, almost 20% higher in some regions(Larney et al., 2015). Antiretroviral therapy (ART) has proven effective in significantly reducing mortality and Acquired Immune Deficiency Syndrome (AIDS)-related morbidity (Ellis et al., 2017; EuroCoord, 2012). In 2015, the World Health Organization (WHO) recommended that all persons living with HIV(PLWH) initiate ART regardless of CD4+ T-cell count, including people who use drugs (PWUD) (Pinkham and Malinowska-Sempruch, 2008; WHO, 2017). The vast majority of HIV treatment research does not pertain to WWUD, with little documentation of viral load, mortality, and barriers and facilitators to uptake and adherence (Azim et al., 2015; Deshko, 2015; Larney et al., 2015; Metsch et al., 2015).
Greater time on ART improves CD4+ T-cell counts and reduces individuals’ risk of progressing to AIDS. However, WWUD on ART appear to progress to AIDS and death at a faster rate than other woman; AIDS-related mortality occurred at a threefold greater rate among cocaine-using women(Cook et al., 2007). Survival is lower for women who inject drugs (WWID) compared to women exposed through high-risk heterosexual contact(Grigoryan et al., 2009). WWID have a greater risk of death compared with men who have sex with men (MSM) (Hall et al., 2006). ART success depends on uptake and adherence. Challenges to care engagement and retention may affect the ability of WWUD to optimize ART adherence and improve health outcomes.
The Social-Ecological Model (SEM) delineates the levels which influence health and associated behaviors at the intrapersonal, interpersonal, organizational, structural, and policy levels(McLeroy et al., 1988). Factors influencing ART uptake and adherence for PWUD occur at each of these levels. At the intrapersonal level, substance use among PWUD, including alcohol consumption and injection frequency, is associated with failure to engage in care(Heimer et al., 2017). Interpersonally, social support is associated with better access to care among PWUD(Ghosh et al., 2017; Matsuzaki et al., 2018). Organizationally, characteristics of clinics, such as long wait times, poor facilities, discriminatory and cultural competence of staff(Grau et al., 2017), and lack of confidentiality, are cited as reasons why PWUD do not access health centers(Gwadz et al., 2016; Kiriazova et al., 2017). At the structural level, stigma and discrimination deter PWUD from seeking services, especially in areas where drug use is criminalized, with PWUD reporting higher levels of stigma from health service providers, family, friends, and law enforcement(El-Bassel et al., 2014). Homelessness and incarceration are associated with lower levels of engagement at varying levels of the HIV care cascade(Milloy et al., 2012; Mizuno et al., 2015). At the policy level, health insurance affects care use among PWUD(Heimer et al., 2017). Gender is known to impact HIV care cascade outcomes (Green et al., 2020), however, analyses of gender differences and understanding of how factors across a SEM specifically impact care engagement and retention among WWUD is lacking.
We chose to conduct a scoping review to assess current research and identify knowledge gaps (Arksey and O’Malley, 2005). The ensuing scoping review assesses the state of peer-reviewed literature on ART uptake and adherence among cisgender WWUD. Results will provide future direction for research and programming.
2. Materials and Methods
2.1. Search Strategy
The review was completed using PRISMA-ScR guidelines(Tricco et al., 2018). A review protocol was developed to guide the process, and updated throughout (Tricco et al., 2018). An informationist from Welch Medical Library developed and conducted the literature search with input from the research team. We searched PubMed, Embase, CINAHL Plus, PsycINFO, and Sociological Abstracts for peer-reviewed English language publications from 1996, the year the 11th International AIDS Conference highlighted the effectiveness of highly active antiretroviral therapy (HAART) (Infante et al., 2009), and January 2018. Our search strategies were developed using a combination of controlled vocabulary and keywords to define the concepts ART, uptake and adherence, and a broad at-risk population of women who sell sex and/or use drugs. Studies which only focused on women who sell sex were excluded for a separate analysis. Searches were conducted on 11 January 2018. The PubMed search strategy is provided as a supplementary material (Appendix 1)*.
2.2. Inclusion Criteria
This review focuses solely on WWUD or studies of PWUD that contained findings disaggregated by gender. We included studies that reported on ART uptake and adherence among cisgender women who use drugs aged 18 years or older; reported at least one empirical quantitative or qualitative ART result; published in a peer-reviewed journal; and published in English. Alcohol was included as a drug. Studies were excluded for the following reasons: wrong study type (not empirical studies); wrong outcomes; and wrong target populations. Studies explicitly focused on transgender women or men, or which included these populations in addition to cisgender women but did not stratify results were excluded.
2.3. Study Selection
Two reviewers independently screened the titles and abstracts of each article to exclude records that clearly did not meet the inclusion criteria. The reviewers used Covidence, a systematic review production tool. The team met regularly to resolve conflicts. A similar process was followed in reviewing the full text of each article to determine eligibility.
2.4. Risk of Bias Assessment and Critical Appraisal of Individual Sources of Evidence
Consistent with scoping review guidelines (Peters et al., 2015; Tricco et al., 2018), we did not complete a formal risk of bias assessment. Comparing bias across study designs was not feasible. Critical appraisal of evidence sources was conducted. The extraction process included a section for study limitations, assessed by both independent extractors and then discussed by the study team during extraction meetings. Summaries and key points are included in the limitations section of the discussion.
2.5. Data Abstraction and Analysis
Two team members independently extracted the data for each record. To ensure consistency in data extraction and for data management, we developed a standardized extraction spreadsheet, which was piloted before the extraction began. Our form included the following: country where the research was conducted; study design; study sample characteristics (sample size, population); ART uptake and adherence findings; and study limitations. Our data manager merged the spreadsheets regularly and highlighted discrepancies. The team met weekly to review extracted data and resolve conflicts. In no instances were authors contacted for additional information.
Tables 3 shows key extracted results including: author names, publication year, study country, study design, and ART uptake and adherence findings. Findings are categorized into three themes: 1) uptake prevalence/ adherence outcomes; 2) barriers/facilitators; and 3) gender differences (when applicable). Consistent with prior papers which have utilized an adapted social ecological model (SEM) framework to understand HIV risk and treatment behaviors and overall care engagement among vulnerable populations of women(Baral et al., 2013; Ma et al., 2017), we utilized a modified SEM framework to guide the research, including: intrapersonal, interpersonal, organizational, structural, and policy levels(McLeroy et al., 1988). We categorized barriers and facilitators into the five SEM levels in Tables 1 and 2, and used the modified SEM model to organize narrative presentation of results, based on the SEM framework and prior literature examining the same factors. Descriptive and multivariate data were abstracted when available; when adjusted data were available, corresponding unadjusted data were not reported. Systematic narrative synthesis was used to summarize and present key findings and characteristics of the included studies(Greenhalgh et al., 2005). The narrative synthesis explores the relationship and findings both within and between the included studies.
Table 3.
Uptake and adherence of ART among women who use drugs
| Uptake and/or Adherence | Author, Year | Study Analytical Design; Location | Setting Characteristics; Sample Characteristics | Substances | Uptake Prevalence or Adherence Outcomes | Barriers/Facilitators | Gender Differences |
|---|---|---|---|---|---|---|---|
| Uptake & Adherence | (Demas, Schoenbaum et al. 1998) | Cross-sectional; Bronx, New York | Montefiore Medical Center; Drug users living with HIV | Heroin, cocaine, crack cocaine, speedball | Uptake: Women started ART earlier than men, 41.2% (14/34) had started by 1990, compared with 23.5% (16/68) of men. Adherence: Antiretroviral treatment duration was significantly lower for women (M = 45.0, SD = 36.0) compared with men (M = 69.7, SD = 35.3) (p = 0.001). |
||
| Adherence | (Moatti, Carrieri et al. 2000) | Cross-sectional; Marseilles Avignon, Nice and the Paris suburbs, France | Hospital departments; IDUs living with HIV | Injection drug use | 63.5% of females were adherent. | There was no significant difference in male and female odds of being adherent/nonadherent. | |
| Adherence | (Williams, Bowen et al. 2000) | Cross-sectional; Washington DC | Unspecified; illicit drug users living with HIV | Illicit drug use (injection) or smoked crack cocaine | Trading sex for drugs was found to have a negative correlation with perceived compliance (r = −0.338, p = 0.068). | Gender did not show a correlation with perceived compliance with AZT dosing. | |
| Uptake | (Stein, Urdaneta et al. 2000) | Unspecified/cross-sectional; Rhode Island | HIV clinics; IDU living with HIV | Illicit drugs, injection, alcohol | There was no significant difference in ARV use by gender | ||
| Adherence | (Stein, Rich et al. 2000) | Unspecified/cross-sectional; Rhode Island | HIV clinics; IDU living with HIV | Illicit drugs, injection, alcohol | Gender was not associated significantly with any of the four measures of adherence [Ever take drug holiday; Not on schedule all the time in last month; Number of pills skipped (>1) in last day; Number of times off schedule (>1) in last day] | ||
| Uptake | (Sambamoorthi, Warner et al. 2000) | Unspecified/cross-sectional; New Jersey | Unspecified; IDU diagnosed with AIDS | IDU, MMT | 76.1% of female drug users were using ARV. | No significant difference in receipt of ARV by gender was found. | |
| Uptake & Adherence | (Turner, Newschaffer et al. 2000) | Retrospective cohort; New York, USA | Unspecified; Women living with HIV | Illicit drug use (opioid, cocaine, amphetamine, hallucinogen, other psychostimulant, or unspecified drug dependence or abuse) | Uptake: An increased proportion of women on ART treatment were also on methadone treatment, reported current illicit drug use, self-reported smoking or drinking during pregnancy. Women treated with methadone had 72% greater odds (aOR: 1.72; 95% CI: 1.18, 2.51) of having antiretroviral therapy prescribed compared with nonusers. Adherence: Prior illicit drug users showed a trend toward greater adherence. Compared with nonusers, prior illicit drug users on methadone were 72% more likely to be adherent based on the pharmacy-based measure of adherence. (aOR: 1.72: 95% CI: 1.18, 2.51) |
||
| Uptake | (Schroeder 2001) | Cross-sectional; Baltimore, MD | Unspecified; IDU living with HIV | Injection illicit drugs (heroin & cocaine) | Gender was not associated with ART use. | ||
| Adherence | (Avants, Margolin et al. 2001) | Longitudinal cohort; New Haven, Connecticut | Methadone maintenance program; IDU living with HIV | Heroin, cocaine | There was no association between gender and nonadherence (p > 0.05). | ||
| Adherence | (Altice, Mostashari et al. 2001) | Cross-sectional; New Haven, Connecticut, US | Ambulatory prison HIV clinics; Prior drug users living with HIV | Heroin only, cocaine only, speedball | Male gender was found to be associated with higher ART adherence (90% in male vs. 78% in female, p=0.03) | ||
| Adherence | (Tedaldi, Willard et al. 2002) | Retrospective analysis; Philadelphia | A University; Pregnant women living with HIV | Cocaine | Of the cohort, 79% reported use of tobacco and/or illicit drugs (62% tobacco, 21% cocaine). Neither factor was significantly associated in the continuation of ART therapy postpartum (p = 0.38). | ||
| Adherence | (Arnsten, Demas et al. 2002) | Cohort; Bronx, New York | Urban clinics; Drug users living with HIV | Heroin, cocaine (including crack) | In multivariate analysis, the best predictive model for adherence included only active cocaine use (B = −18.7; p = 0.02 and an interactive term representing gender and depression (B = − 8.5, p = 0.05). This interaction term indicated that women who screened positive for depression had poorer adherence than women with a negative depression screen. | Female gender was significantly associated with worse adherence. The association between depression and adherence was not observed in men. |
|
| Adherence | (Howard, Arnsten et al. 2002) | Prospective cohort; New York (Bronx), Baltimore , Providence and Detroit | Multicenter; Women living with HIV | Cocaine, alcohol, injecting drugs | The mean adherence among those reporting use of cocaine or heroin by any route during the study period was 34%, compared with 57% among those not using drugs (p = 0.0002). | Active drug use (p = 0.002), alcohol use at least one day per week during the study period (p = 0.04) and an interaction between active drug use and time (p = 0.002) were significantly associated with lower adherence from a multivariate analysis. | |
| Adherence | (Mellins, Havens et al. 2002) | Cross-sectional; Unspecified | Inner-city medical center; Women living with HIV | Alcohol and drugs | Mental health and substance abuse were the factors most strongly associated with missed pills. Participants with a current psychiatric (OR: 8.76; 95% CI: 1.77, 43.38) or substance abuse disorder (OR: 9.49; 95% CI: 1.86, 47.94) were more likely to report missing pills in the past two days than participants without a disorder and the odds of missing pills increased as psychological distress increased, although this last finding was of borderline significance. | ||
| Adherence | (Bouhnik, Chesney et al. 2002)) | Crosss-ectional; France | Unspecified; IDU living with HIV | IDU, DMT Opiates, anxiolytics, cannabis, alcohol | Gender was not associated with adherence among ex-IDU or opiatedependent patients. | ||
| Adherence | (Gebo, Keruly et al. 2003) | Cross-sectional; Baltimore , MD | Johns Hopkins University HIV Clinic; People living with HIV | Heroin, cocaine, alcohol, any illicit drug, injected or inhaled | The factors significantly associated with non-adherence in women were active heroin use within 6 months of the interview (aOR: 8.26; 95% CI: 1.66, 41.7). | ||
| Uptake | (Pach, Cerbone et al. 2003) | Prospective cohort and ethnographic subsample; Washington, D.C. | Predominantly African American neighborhoods; IDU living with HIV | Injection drug use | 48.7% of female drug users were on ARV medication. | Gender was not associated with being on ARV medication. | |
| Adherence | (Powell-Cope, White et al. 2003) | Mixed methods 1) Qualitative - focus groups, 2) Quantitative-Pilotintervention; Florida | Unspecified; Women with history of substance abuse living with HIV | Illicit drugs or alcohol | Of the 24 women in the reminder intervention trial, 33% admitted to missing one or more doses in the past two weeks; this proportion changed to 30% at one month and remained at 30% two months. | At baseline, the most common reasons for missing medications were forgetting due to various circumstances (e.g. sleeping, being busy, change in schedule) and feeling depressed or overwhelmed. Women also commonly responded that feeling too good or feeling too sick were barriers to adherence. Wanting to avoid side effects became a less common barrier over time. At first follow-up fewer women missed a dose (p=0.05) than at baseline due to sleeping through a dose or being busy with other things. Feeling too good and change in daily routine tended (p=0.07) to be less common causes of poor adherence. At second follow-up, being busy with other things and feeling too good were significantly less common problems with adherence than at baseline. Overall, most reasons that women reported missing medications were less frequent in the follow-up waves. Although side effects were a lesser concern, most women acknowledged that side effects made them question whether they should continue antiretroviral medications. Women reported that gastrointestinal effects, such as nausea, vomiting and diarrhea, as well as fatigue were especially troublesome. |
|
| Adherence | (Turner, Laine et al. 2003) | Retrospective cohort; New York | Unspecified; Drug users living with HIV | Illicit drug abuse classified as: drug dependence of unspecified type; heroin or cocaine abuse or dependence; or other drug abuse or dependence (i.e., amphetamine, hallucinogens, marijuana , barbiturates) | Adherence was greater in persons of both genders who were diagnosed with depression. In women, adherence was significantly poorer for those with heroin or cocaine abuse. In both genders, psychiatric care and/or antidepressants were not associated with significantly higher proportions of adherent patients. The positive effect of psychiatric care on adherence alone was similar in women and men but the association did not achieve statistical significance in separate models by gender. A smaller positive association was observed for antidepressant therapy alone but was also not statistically significant. After adjustment, antidepressant therapy had a small but significant positive association that was similar by gender. Women without mental health care and without diagnosed depression had significantly lower adjusted odds of adherence (OR, 0.65; 95% CI, 0.51 to 0.82) compared to their male counterparts, while the adjusted odds ratios for the groups of women with psychiatric care and/or antidepressant therapy did not differ significantly. |
Less than one fifth of women were adherent compared with one quarter of men (p = 0.001). No gendered difference was found concerning the association of depression, psychiatric care, or antidepressants and adherence. After adjustment for patient demographic, substance abuse, clinical, and health care factors, an overall model of the entire study cohort showed that women had significantly lower adjusted odds of adherence than men (OR: 0.67; 95% CI: 0.58, 0.78). The adjusted odds of adherence were 90% greater among those women with depression who received both psychiatric care and antidepressant therapy, compared with those receiving neither type of care but only 26% greater in men. Among persons without the diagnosis of depression, longitudinal drug treatment showed a significant positive association only for men. Psychiatric care had a somewhat stronger positive association with adherence for women without diagnosed depression than for men in this subgroup |
|
| Adherence | (Mellins, Kang et al. 2003) | Longitudinal cohort; New York City | Large inner-city medical center; Women living with HIV | Alcohol and drugs | Women living with HIV meeting criteria for psychiatric (OR: 14.30; 95% CI: 2.88, 71.00) or substance abuse disorders (OR: 7.32; 95% CI: 1.55, 34.45) at baseline were more likely than women who didn’t meet diagnostic criteria to report missing pills at the follow-up interview. | ||
| Adherence | (O’Connell, Braitstein et al. 2003) | Retrospective cohort; British Columbia | HIV/AIDS Drug Treatment; IDUs living with HIV | Injection drug use | Among female injection drug users (IDUs), 27% had greater than 95% adherence. | Among injection drug users, a higher proportion of men (49%) had 95% adherence than women (27%). | |
| Uptake | (Warner, Wei et al. 2003) | Unspecified/retrospective cohort; New Jersey | Unspecified; Women living with HIV | Injection drugs, alcohol, opiates | ART use was significantly more likely for women who had received substance abuse treatment (SAT) (OR: 2.12; 95% CI: 1.73, 2.60) and marginally significant for women without substance abuse histories (OR: 1.40; 95% CI: 1.00, 1.97) Compared to other months, ART use was significantly more likely in the ante- and postpartum months among women without substance abuse histories compared to those who received SAT. |
||
| Uptake &Adherence | (Palepu, Horton et al. 2004) | Prospective cohort; Boston | Unspecified; Individuals with alcohol problems living with HIV | Alcohol | Uptake: 56.16% (41/73) of female drug users received antiretroviral therapy. Adherence: 82.5% of females reported 30-day adherence to ART. |
Uptake: There was no significant difference between males and females receiving ART. Adherence: There was no significant difference in 30-day adherence between males and females (p = 0.23). Gender was not associated with 30-day adherence (aOR: 0.71; 95% CI: 0.37, 1.28). |
|
| Adherence | (Samet, Horton et al. 2004) | Prospective cohort; Boston, US | HIV Diagnostic Evaluation Unit; Persons with alcohol problems and living with HIV | Alcohol | There was no association between the odds of being fully adherent and gender (p = 0.80). | ||
| Uptake & Adherence | (Sharpe, Lee et al. 2004) | Unspecified/cross-sectional; 12 states in the USA | Unspecified; Black women living with HIV | Crack cocaine, other drugs such as heroin or marijuana | Uptake: A larger proportion of crack users, 42% (133/302) reported taking no antiretroviral medicines compared with nonusers, 30% (136/446) and users of other drugs, 32% (142/441). Adherence: Crack users (OR: 0.37, 95% CI: 0.24, 0.56) and users of other drugs (OR: 0.47, 95% CI: 0.36, 0.68) were less likely than non-drug users to take their ART medicines exactly as prescribed. |
||
| Adherence | (Wagner and Ryan 2004) | Intervention study; Los Angeles | Community based organizations and clinics; Drug users living with HIV | heroin, cocaine, methamp hetamine | Women’s (n=5) adherence level (92%) was significantly higher than that of the male participants (64%; p = 0.05). | ||
| Uptake | (Rusch, Nixon et al. 2004) | Cross-sectional; British Columbia | AIDS Service Organization; Illicit drug users living with HIV | IDU (current and former) | A comparison of current, former and never injectors showed an increasing trend with regard to percentage on ART. Current injection was associated with not being on therapy when compared to either non-injectors or former injectors. |
There was no significant association between gender and current ART use. | |
| Adherence | (Berg, Demas et al. 2004) | Prospective cohort; Bronx, New York | Substance Abuse Treatment Program; Current or former drug users living with HIV | Injection drugs, crack, cocaine, heroin, alcohol | Women in this study had a median adherence rate of 46% (IQR 18% to 77%). | Among women, alcohol use (p = .003), heroin use (p <=.04), and significant medication side effects (p = .002) were independently associated with worse adherence. In multivariate analysis with an all gender population and an interaction term for gender and alcohol use, problem alcohol use had a significant negative impact on adherence for women only (mean adherence 57% for women without problem drinking vs. 25% for women with problem drinking; p = .003). |
Women were less adherent to HAART than men, with a median adherence rate of 46% (IQR 18% to 77%) for women compared to 73% (IQR 30% to 93%) for men (p = .04). Problem alcohol use was significantly associated with worse adherence among females but not males. |
| Adherence | (Waldrop-Valverde and Valverde 2005) | Unspecified/cross-sectional; Miami-Dade County, Florida | Unspecified; IDU living with HIV | Opiates, Cocaine, Crack-Cocaine, Marijuana, Alcohol | Gender was not associated with adherence. | ||
| Uptake | (Wood, Kerr et al. 2006) | Prospective cohort; Vancouver, Canada | Unspecified; IDU living with HIV | IDU, cocaine, heroin, methadone | There was no difference in time to first ART use comparing males to females. | ||
| Adherence | (Haug, Sorensen et al. 2005) | Cross-sectional; California, US | Unspecified; Methadone maintenance patients living with HIV | MMT | Women’s ART adherence by various measures was as follows: 1) Medication Adherence MEMS ontime openings, 58%, 2) Selfreport ontime yesterday, 78%, 3) Selfreport ontime 2/4 days ago, 78%. | At the end of the 4-week baseline observation period, there were no differences between men and women on medication adherence as measured objectively by MEMS cap openings or by self-reports all patients from MMT. | |
| Adherence | (Liu, Longshore et al. 2006) | Cross-sectional; Los Angeles County and surrounding areas | Community organizations and clinics); Women living with HIV | Non-crack cocaine, crack cocaine, and heroin | Lifetime heroin use was not statistically related to greater than 90% adherence (OR: 0.45; 95% CI: 0.15, 1.39). | ||
| Adherence | (Waldrop-Valverde, Ownby et al. 2006) | Cross-sectional; Unspecified | Unspecified; IDU living with HIV | Opiates, Crack-Cocaine, Cocaine, Marijuana, Heroin, Alcoho | Gender was not associated with adherence in correlational analyses. | ||
| Uptake | (Burke-Miller, Cook et al. 2006) | Longitudinal cohort; USA (Brooklyn, the Bronx, Washington DC, Chicago, Los Angeles, and the San Francisco Bay Area) | Urban clinics; Women living with HIV | crack, cocaine, heroin, amphetamines | Women who reported use of illegal drugs were less likely to subsequently report HAART use (OR: 0.60; 95% CI: 0.49, 0.75). | ||
| Adherence | (Touloumi, Pantazis et al. 2006) | Prospective cohort; Europe | Unspecified; Adults living with HIV | Injection drug use | Women were more likely to have a treatment interruption than men among IDU. Comparing women to men, the adjusted hazard ratio of having a treatment interruption was 1.63 (p = 0.020) among IDUs. | ||
| Adherence | (Palepu, Tyndall et al. 2006) | Cohort; Vancouver, Canada | Unspecified; IDUs living with HIV | Injection drug use | Male gender was not associated with ≥95% adherence to HAART in unadjusted or adjusted analyses. | ||
| Adherence | (Lopez, Jones et al. 2007) | Unspecified/Pre-post test/Intervention study; Florida’s Miami-Dade County, New York City and the New Jersey metropolitan area | Unspecified; Women living with HIV | Marijuana, crack, cocaine, methadone, alcohol | At baseline, never drug users had adherence rates of 93% (SD = 19.7), former users had adherence rates of 95% (SD = 13) and current users reported adherence rates of 91% (SD = 19). For those women who were adherent <80% of the time, never users had adherence rates of 51.5%, former users had adherence rates of 61.5% and current users reported adherence rates of 58.5%. |
Self-reported adherence did not differ between these three [never, former, current users] groups (p = 0.96). Among both former users and current users, no relationships were found between adherence and the prescription of a particular medication. There was no association between perceived necessity of medication (p = 0.92), concerns regarding medication (p = 0.28) and overall levels of adherence (p = .62). |
|
| Uptake | (Cook, Grey et al. 2007) | Longitudinal cohort; USA (Brooklyn, NY; the Bronx, NY; Chicago, IL; Los Angeles, CA; San Francisco/Bay Area, CA, and Washington, DC) | Six medical and university consortia sites nationwide; Women living with HIV | Crack, cocaine, heroin, amphetamine use | Compared to women with no depression or illicit drug use, HAART use was significantly less likely among women with depression plus illicit drug use, and also less likely among women with recent illicit drug use alone. With some small variations in early study visits, the lowest proportions of women on HAART were those with depression plus drug use throughout the time period studied. The next lowest proportions were among women who used illicit drugs but did not screen positive for depression. Conversely, the largest proportion of women on HAART was the group of women reporting neither depression nor recent illicit drug use, followed closely by those women who screened positive for depression, but reported no illicit drug use. |
||
| Uptake & Adherence | (Theall, Clark et al. 2007) | Longitudinal cohort; New Orleans, Louisiana | HIV Outpatient Clinic; Women living with HIV | Alcohol | Uptake: There were fewer women binge drinkers on ART than women non-binge drinkers (45% vs. 60%, p < 0.05). Alcohol consumption patterns were associated with ART use; women who drank more frequently and who binged were less likely (p < 0.05) to be on ART. Adherence: Binge drinking was not associated with taking medicine as prescribed. |
||
| Adherence | (Kim, Palepu et al. 2007) | Prospective observational cohort; Boston, MA | Unspecified; Persons living with HIV | Alcohol | After adjustment, gender was not associated with discontinuation of ART amongst people with a history of alcohol problems. | ||
| Uptake | (Abatemarco, Catov et al. 2008) | Retrospective cohort; New Jersey, US | Unspecified; Women who delivered a live birth, living with HIV | Illegal drug use | Evidence of drug use (OR: 0.31; 95% CI: 0.20, 0.46) was associated with decreased odds of receiving two arms of ZDV prophylaxis. Illegal drug use was associated with a reduced likelihood of ZDV receipt, compared with no illegal drug use during or prior to pregnancy (OR: 0.42; 95% CI: 0.25, 0.72). |
||
| Adherence | (Applebaum, Richardson et al. 2009) | Cross-sectional; Boston, MA | Clinical research site; IDU living with HIV | Alcohol and illicit drug use | At least 95% adherence to medication regimens was reported by 68.2% of women The mean adherence ratio was 0.890 for women. |
This analysis also revealed that for women, an absence of alcohol dependence (p = 0.05) and non-endorsement of specific concerns about medication side effects (i.e., missed taking your medications because you wanted to avoid side effects (P = 0.05) and missed taking your medications because you felt sick/ill from side effects (p = 0.02) were significant predictors of adherence. | The proportion of women whose adherence ratio was equivalent to 0.95 or greater was not significantly different than the proportion for men (p = 0.54). |
| Adherence | (Kang, Goldstein et al. 2008) | Cross-sectional; East Harlem in New York City | Not-specified; Drug users living with HIV | Alcohol, crack, cocaine, heroin | For women, having close relationships with family (mother, father or siblings) was negatively associated with use of HIV medications (p = 0.04). For both men and women, use of HIV medications was positively associated with being married and with attendance in HIV support groups, but negatively associated with childhood sexual abuse experience. |
Use of HIV medications did not differ between men and women. | |
| Adherence | (Kavasery, Galai et al. 2009) | Prospective cohort; Baltimore, MD | Unspecified; IDU living with HIV | Injection drug use | In multivariate analyses, being female (RH: 1.36: 95% CI: 1.02, 1.82) was associated with a higher probability of having an NTI. | ||
| Adherence | (Mellins, Havens et al. 2009) | Cross-sectional; Bronx, NY; Philadelphia, PA; Durham, NC; St. Louis, MO; Seattle, WA; Boston, MA; Chicago, IL; and Detroit, MI | Urban and rural sites; Persons diagnosed with mental and substance abuse disorders and living with HIV | Substance abuse disorder (e.g. alcohol, other drugs) | Gender was not associated with ARV adherence. | ||
| Adherence | (Friedman, Marshal et al. 2009) | Cross-sectional; Baltimore, MD, Chicago, IL, and Los Angeles, CA | Unspecified; People living with HIV | Marijuana, cocaine, crack cocaine, heroin/speedball, methadone, sedatives, speed/met hamphetamine, injection drug use, alcohol use | Analyses by sexual orientation and gender showed that associations for marijuana, crack cocaine, heroin, alcohol use, use of any drug, use of 2 drugs and adherence were significant only for the heterosexual males, and not significant for female subgroup (after adjusting for educational achievement, income, race, age, physical health, mental health, and employment status). | ||
| Uptake | (Uhlmann, Milloy et al. 2010) | Prospective cohort; Vancouver, Canada | Unspecified; IDU living with HIV | Cocaine, heroin | Gender was not associated with ART initiation. | ||
| Adherence | (Krusi, Milloy et al. 2010) | Prospective cohort; Vancouver, Canada | Unspecified; Drug users living with HIV | injection drug use (heroin, cocaine or methamp hetamine injecting) and non-injection drug use (crack or crystal methamp hetamine smoking) | 36.9% (n=76) of females had adherence >=95%. | Female gender was significantly negatively associated with antiretroviral therapy adherence. | |
| Adherence | (Feaster, Mitrani et al. 2010) | Randomized controlled trial; Unspecified | General Clinic Research Center; Women living with HIV and substance abuse disorder | Cocaine, alcohol and illicit drugs | The probability of taking prescribed HIV ART medications was not significantly different across intervention conditions [family-ecosystem intervention vs psycho-educational health group]. However, the model predicted an increase in those taking prescribed medications from 79% at baseline to 88% at 12 months among participants in SET (a family-ecosystem intervention). Those in HG (a psycho-educational health group) started at 87% and increased to 88% at 12 months. There was a significant Time × Treatment interaction (B = −1.14, p < .05) for % pills taken. |
||
| Uptake | (Vallecillo, Sanvisens et al. 2010) | Cross-sectional; Barcelona, Spain | Hospital detoxification units; Drug users living with HIV | stimulants (cocaine) and depressants (opiates, alcohol) | 39.66% (71/179) of female drug users were on ART. | Gender was not associated with being on ART at admission to substance abuse treatment. | |
| Uptake & Adherence | (Bailey, Townsend et al. 2011) | Prospective observational cohort; Nine countries (Belgium, Denmark, Germany, Italy, the Netherlands, Poland, Spain, Sweden and the UK) | Unspecified; Pregnant women living with HIV | Injection drug use | Uptake: Among women diagnosed with HIV after conception, IDU history was associated with not receiving ART. A quarter (24/106) of pregnancies among current IDUs had no antenatal ART compared with 8% (20/249) of pregnancies among ex-IDUs (χ2=13.89, p<0.01). Adherence: Women with history of IDU were more likely to receive NO antenatal ART (aOR: 2.91; 95% CI: 1.55, 5.44) Among women diagnosed with HIV preconception, history of IDU was associated with not receiving ART (aOR 2.00; 95% CI: 1.06,3.77), but not with short duration of ART (p = 0.810). |
||
| Uptake | (Neblett, Hutton et al. 2011) | Retrospective cohort; Baltimore , MD | Johns Hopkins HIV Clinic; Women living with HIV | Heroin, cocaine, alcohol | Current illicit drug use was associated with delayed cART initiation (HR: 0.73; 95% CI: 0.59, 0.91, p < 0.01) after adjusting for age, race, CD4, HIV RNA, and hepatitis C status. There was no interactive effect between alcohol and drug use or alcohol use and hepatitis C status on outcomes of time to cART initiation or time to death. |
||
| Adherence | (Copenhaver, Lee et al. 2011) | Pre-post intervention study; New Haven, CT | Inner-city clinic; IDUs living with HIV | Heroin, cocaine | The 3H+ intervention is a 4 session, group, theory driven, behavioral intervention specifically designed to address sex- and drug-related transmission risk behavior and antiretroviral adherence among HIV-infected IDU. A significant intervention effect was demonstrated, with an increase in antiretroviral adherence self-efficacy from pre-intervention (mean = 5.22, SD = 2.45) to post-intervention (mean = 6.64, SD = 2.06). | Males and females both benefited equally well from the intervention to increase adherence. | |
| Uptake & Adherence | (Tapp, Milloy et al. 2011) | Prospective cohort; Vancouver, Canada | Unspecified; IDU living with HIV | Injection drug use, heroin, cocaine, crack | Uptake: 30% (62) women were on ART in the six-month period prior to the baseline interview. | Adherence: Female gender (aOR: 0.70; 95% CI: 0.53, 0.93) was independently and negatively associated with 95% adherence to ART. |
|
| Adherence | (Palepu, Milloy et al. 2011) | Longitudinal cohort; Vancouver, Canada | Unspecified; IDUs living with HIV | Injection drug use, illicit drugs other than cannibinoids | Female sex was negatively associated with ART adherence (OR: 0.69; 95% CI: 0.52, 0.89). | ||
| Uptake | (Kissin, Mandel et al. 2011) | Surveillance, prospective assessment; St. Petersburg, Russia | Unspecified; Pregnant women living with HIV | Injection drug use | 44% of women initiated ARVs in 2004, and 54% initiated ARVs in 2008. | Between 2004 to 2008, initiation of antiretroviral prophylaxis at ≤28 weeks gestation increased less among IDU (44% to 54%) than non-drug users (45% to 72%) For most of the study years considered, IDUs were more likely than non-IDUs to have later initiation or incomplete antiretroviral prophylaxis. |
|
| Adherence | (Kang, Deren et al. 2011) | Prospective cohort; New York and Puerto Rico | Unspecified; Drug users living with HIV | Heroin or cocaine | Women with depressive symptoms were less likely to use HIV medications, as compared with women without such symptoms (31% vs. 78%). | Females were more likely than males to use HIV medication at follow-up (aOR: 11.29; 95% CI: 1.77, 72.17) Unlike men, women with depressive symptoms were less likely than women with no depressive symptoms to use HIV medications. |
|
| Adherence | (Elenga, Hanf et al. 2012) | Matched case control; Cayenne, French Guiana | Cayenne General Hospital; Pregnant women living with HIV | Marijuana, crack, cocaine, alcohol | Using drugs (marijuana, crack, cocaine) was associated with less than four weeks of treatment (aOR: 6.27; 95% CI: 1.26, 31.13), whereas using alcohol or tobacco were not associated with less than four weeks of treatment (p = 0.506). | ||
| Adherence | (Rosen, Black et al. 2013) | Cross-sectional; US | 14 sites across 12 states in the US; Adults living with HIV | alcohol, cannabis, heroin, cocaine, other | Men were more adherent than women, but the relationship between alcohol or cannabis use and adherence was the same for men and women. | ||
| Adherence | (Werb, Milloy et al. 2013) | Prospective cohort; Vancouver, Canada | Unspecified; IDU living with HIV | Injection drug use, heroin, cocaine or other illicit drugs | 47.1 % of females (n = 248) reported discontinued ART use. | Female gender (aHR: 1.23; 95% CI: 1.03, 1.46) was associated with an increased risk of ART discontinuation. | |
| Adherence | (Kreitchmann, Harris et al. 2012) | Prospective cohort; Argentina, Brazil, and Peru | Unspecified; Women living with HIV | Alcohol, marijuana, cocaine/crack, heroin/opiates | The probability of non-perfect adherence was over threefold higher for those who were currently using alcohol at the time of the 6-month visit compared to those who were not (OR: 3.04; 95% CI: 1.34, 6.90). | ||
| Adherence | (Gonzalez, Mimiaga et al. 2013) | Unspecified/longitudinal; Boston | Methadone clinics; Drug users living with HIV | Opiates, cocaine, sedatives, alcohol, marijuana | 59.62% of women were adherent to ART medications | Gender was significantly related to medication adherence (b = −.22, p = .02); men reported higher rates of adherence than women (M = 73.59, SD = 25.76 and M = 59.62, SD = 28.56; respectively). | |
| Adherence | (Kalichman, Grebler et al. 2013) | Prospective cohort; Atlanta, GA | Unspecified; Alcohol drinkers living with HIV | Alcohol | 56.41% of women (22/39) reported skipping their medications if they have been drinking alcohol. | ||
| Adherence | (Mann, Milloy et al. 2012) | Prospective cohort; Vancouver | Unspecified; IDU living with HIV | Injection drug use - Heroin, Cocaine, Crack Cocaine | 72.6% of females had less than 95% adherence. | In univariate analyses, female gender (OR: 0.62; 95% CI: 0.44, 0.87) was associated with lower adherence to ART. | |
| Uptake | (Hanna, Buchacz et al. 2013) | Prospective cohort; United States and Canada | Clinical sites; People living with HIV | Injection drug use, non-injection drug use, alcohol | History of IDU was associated with less timely ART initiation among females (aHR 0.64 vs. aHR: 0.87). | Female IDU had less timely ART initiation compared to male IDU (aHR: 0.64 vs. aHR: 0.81). | |
| Adherence | (Waldrop-Valverde, Dong et al. 2013) | Prospective cohort; South Florida | HIV care clinics; Drug users living with HIV | Cocaine, Alcohol, Marijuana | Gender was not associated with any measure of adherence (self adherence, percent dose, percent days, schedule). | ||
| Adherence | (Tucker, Simpson et al. 2013) | Prospective cohort; Alabama | Rural HIV clinic; Substance users living with HIV | Alcohol or illicit drug use | Gender was not associated with adherence. | ||
| Adherence | (Surratt, Kurtz et al. 2013) | Unspecified/cross-sectional; South Florida | Unspecified; Substance abusers living with HIV | Cocaine, heroin | In the multivariate model, male gender was associated with increased odds of ARV diversion (aOR: 1.99; 95% CI: 1.34, 2.96). | ||
| Adherence | (Reddon, Milloy et al. 2014) | Prospective cohort; Vancouver, Canada | Unspecified; Illicit drug users living with HIV | Illicit drug users | From multivariate analyses, female gender was associated with ART discontinuation (aHR: 1.43; 95% CI: 1.11, 1.85). | ||
| Uptake | (Goodness, Palfai et al. 2014) | Unspecified cohort; St. Petersburg, Russia | Inpatient and Outpatien HIV and substance use care sites; Heavy drinkers living with HIV | Alcohol | Males had higher odds of initiating ART than females (AOR: 2.51; 95 % CI: 1.19 to 5.29). | ||
| Adherence | (Wilson, Sikkema et al. 2014) | Unspecified/Cross-sectional; New York City | Unspecified; People living with HIV | Cocaine, crack | For women, the effect of psychological distress was associated with decreased adherence, mediated by drug use (β = −.32, p = 0.018). | For men, psychological distress did not significantly predict drug use nor did drug use significantly predict HAART adherence. However, for women these paths demonstrated strong effects. | |
| Uptake | (Solomon, Srikrishnan et al. 2014) | Randomized clinical trial; Chennai, India | Substance Abuse Research Center; Drug users living with HIV | Injection and non-injection drug use | Gender was not associated with ART initiation. | ||
| Adherence | (Slawson, Milloy et al. 2015) | Prospective cohort; Vancouver | Vancouver’s Downtown Eastside (DTES); Illicit drug users living with HIV | Cannabis, heroin, cocaine, crack cocaine, alcohol | Female gender was not associated with optimal adherence after adjustment. | ||
| Adherence | (Bailey, Thorne et al. 2014) | Prospective cohort; Ukraine | Regional HIV/AIDS centers; Pregnant women living with HIV | Alcohol, marijuana, illicit drugs | There was some evidence of an association between current smoking and reporting of ≥1 missed dose during pregnancy (p = 0.07), but not between history of illicit drug use and adherence. In the year following delivery, current smokers were more likely to report ≥1 missed dose, as were women with a history of illicit drug use and those not using a treatment adherence program (p = 0.08 for latter two factors). |
||
| Uptake | (Zhao, Shi et al. 2015) | Cohort; China | Chinese National Center for AIDS/STD Control and Prevention; MMT clients living with HIV | MMT clients | 52.99% (549/1036) of female drug users were ART-treated. | Gender was not associated with accessing antiretroviral therapy in unadjusted or adjusted analyses. | |
| Adherence | (Tsuyuki and Surratt 2015) | Cross-sectional; South Florida | Unspecified; Substance abuser living with HIV | “Recent substance use” | Being male was associated with significantly increased odds of ARV diversion (selling or trading ART medications) (aOR: 2.28; 95% CI: 1.35, 3.85). | ||
| Adherence | (Azar, Wood et al. 2015) | Prospective cohort; Vancouver, Canada | Urban; IDU living with HIV | IDU - heroin and cocaine, Ampheta mine, MMT | 49.76% of females were <95% adherent. | Female sex (aOR: 0.77; 95% CI: 0.68, 0.87) was negatively associated with optimal adherence to ART. | |
| Adherence | (Joseph, Kerr et al. 2015) | Prospective cohort; Vancouver, British Columbia (BC), Canada | Unspecified; Illicit drug users living with HIV | Illicit drugs other than cannabis | Individuals who achieved optimal adherence were more likely to be male (aOR: 0.69; 95% CI: 0.51, 0.93). | ||
| Uptake | (Jarlais, Arasteh et al. 2016) | Unspecified; NYC | Mount Sinai Beth Israel drug detoxification and methadone maintenance programs; PWID living with HIV | Heroin, cocaine, speedball, crack cocaine | Among PWID, there was no difference between females and males on receiving ART. Among NIDU, females were less likely to report receiving ART than their male counterparts. | ||
| Adherence | (Surratt, Kurtz et al. 2015) | Cross-sectional; South Florida | Unspecified; Substance abusers living with HIV | Cocaine, heroin | Gender was not associated with missed ARVs because of diversion (selling or trading ART medications). | ||
| Uptake & Adherence | (Vallecillo, Mojal et al. 2016) | Longitudinal study; Barcelona, Spain | Drug treatment center; IDU living with HIV | Injection drug use, cocaine, heroin | Uptake: 32.6 % (43) of female drug users were naive to cART. | Uptake: A higher number of men were naive to cART than women (76.7 % vs. 57.3 %; p= 0.022). Adherence: Gender was not associated with non-structured treatment interruptions (NTI) in multivariate analysis. *Treatment interruptions (TI), whether physician-directed (structured) or patient-initiated (non-structured; NTI) |
|
| Adherence | (Bach, Wood et al. 2015) | Prospective observational cohort; Vancouver, Canada | Urban; PWID living with HIV | Heroin, cocaine, crack cocaine | Male gender (HR: 0.71; 95% CI: 0.58, 0.86) was negatively associated with ART discontinuation [defined as 90 days off ART following previous enrollment] | ||
| Adherence | (Kalichman, Kalichman et al. 2015) | Prospective cohort; Atlanta, GA | Unspecified; Substance users living with HIV | Alcohol, Cocaine, Cannabis, Opiates, Oxycodone, Propoxyphene (PPx), Phencyclidine (PCP), Barbiturates, Benzodia zepines, Amphetamine, Methamphetamine, Methadone, 3,4-methylene dioxymet hampheta mine | 43.51% of females (57/131) intentionally missed ART when using drugs. | Women were significantly more likely to intentionally miss their medications than men (OR: 1.57; 95% CI: 1.04, 2.35.) | |
| Adherence | (Hayashi, Wood et al. 2016) | Prospective cohort; Vancouver, Canada | Vancouver’s Downtown Eastside neighborhood; Drug users living with HIV | Crack cocaine, opioids | 47.6% of female crack cocaine users (69/145) reported ≥95% pharmacy refill adherence for antiretrovirals. | ||
| Adherence | (Puskas, Kaida et al. 2017) | Cohort; British Columbia | Unspecified; Persons living with HIV | Injection drug use | Of women PWID, 47.8% of those with indigenous ancestry and 58.7% of those without indigenous ancestry attained optimal adherence (>95%) over the observational period. | Overall, women PWID were significantly less likely to be optimally adherent then men PWID (57.0 vs. 77.1%; p < 0.001). This remained true within stratified analyses, in both women PWID with indigenous ancestry (47.8% vs. 57.7%, p <0.001) or without indigenous ancestry (58.7% vs. 66.9%, p<0.001). | |
| Uptake | (Hoots, Finlayson et al. 2017) | Cross-sectional; United States, (20 participating cities) | Unspecified; PWID living with HIV | Injection drug use | From 2009 – 2015, ARV use among females increased (aPR: 1.15; 95% CI: 1.06, 1.24). In 2009, 50% of females reported using ARVs, in 2012, 62% of females reported using ARVs, and in 2015, 72% of females reported using ARVs. |
Table 1.
Factors Associated with Uptake
| Factors | Total findings | Uptake Facilitator | Uptake Barrier | No effect |
|---|---|---|---|---|
| Intrapersonal | 16 | 1 | 15 | 0 |
| Substance use | 14 | 0 | 14 | 0 |
| Poor mental health | 1 | 0 | 1 | 0 |
| Prior use of ART | 1 | 1 | 0 | 0 |
| Interpersonal | 0 | 0 | 0 | 0 |
| Organizational | 2 | 0 | 0 | 0 |
| Drug abuse treatment | 2 | 2 | 0 | 0 |
| Community | 0 | 0 | 0 | 0 |
| Public policy | 0 | 0 | 0 | 0 |
Table 2.
Factors associated with adherence
| Factors | Total findings | Adherence Facilitator | Adherence Barrier | No effect |
|---|---|---|---|---|
| Intrapersonal | 34 | 1 | 25 | 8 |
| Substance use | 21 | 0 | 14 | 7 |
| Poor mental health | 7 | 1 | 6 | 0 |
| Side-effects | 3 | 0 | 3 | 0 |
| ART beliefs | 2 | 0 | 1 | 1 |
| Forgetting | 1 | 0 | 1 | 0 |
| Interpersonal | 3 | 1 | 2 | 0 |
| Diversion | 3 | 0 | 3 | 0 |
| Relationships | 2 | 1 | 1 | 0 |
| Sex work | 1 | 0 | 1 | 0 |
| Organizational | 6 | 5 | 3 | 0 |
| Adherence Intervention | 4 | 3 | 1 | 0 |
| Mental Health Treatment | 1 | 1 | 1 | 0 |
| Substance Use Treatment | 1 | 1 | 1 | 0 |
| Community | 0 | 0 | 0 | 0 |
| Public Policy | 0 | 0 | 0 | 0 |
2.6. Terminology
There were disparities in terminology and consistency around the use of sex and gender in reviewed articles. When discussing PWUD, gender terminology was more commonly used, (i.e., women), however, some authors used sex terminology (i.e. female). In no instance was the nuance of sex or gender categories discussed. Terminology for drug use varied throughout included studies; some authors specified injection practices (e.g. women injection drug users) while others did not (e.g., women who use drugs); some defined the individual by the behavior (e.g., injection drug user) others described an individual with a behavior (e.g., woman who injects drugs). We specify injection drug use when relevant, use gender terminology, and use person-centered terminology throughout the manuscript, with the exception of table 3 where we left the authors’ findings in their own terminology.
3. RESULTS
The database searches returned 6,735 records. After removing duplicates 4,592 records remained. A review of titles and abstracts revealed that 3,513 were not relevant, leaving 1,079 articles for full-text assessment. Of these, 963 records were excluded because of the following reasons: wrong population (627), wrong study design (227), wrong outcomes of interest (84), not in English (21), and duplicates (4). Many articles were excluded for multiple reasons, but were categorized only once, often to “wrong population”. In total, 86 articles were included in this review. Figure 1 presents a flow diagram for selection of articles.
Figure 1.
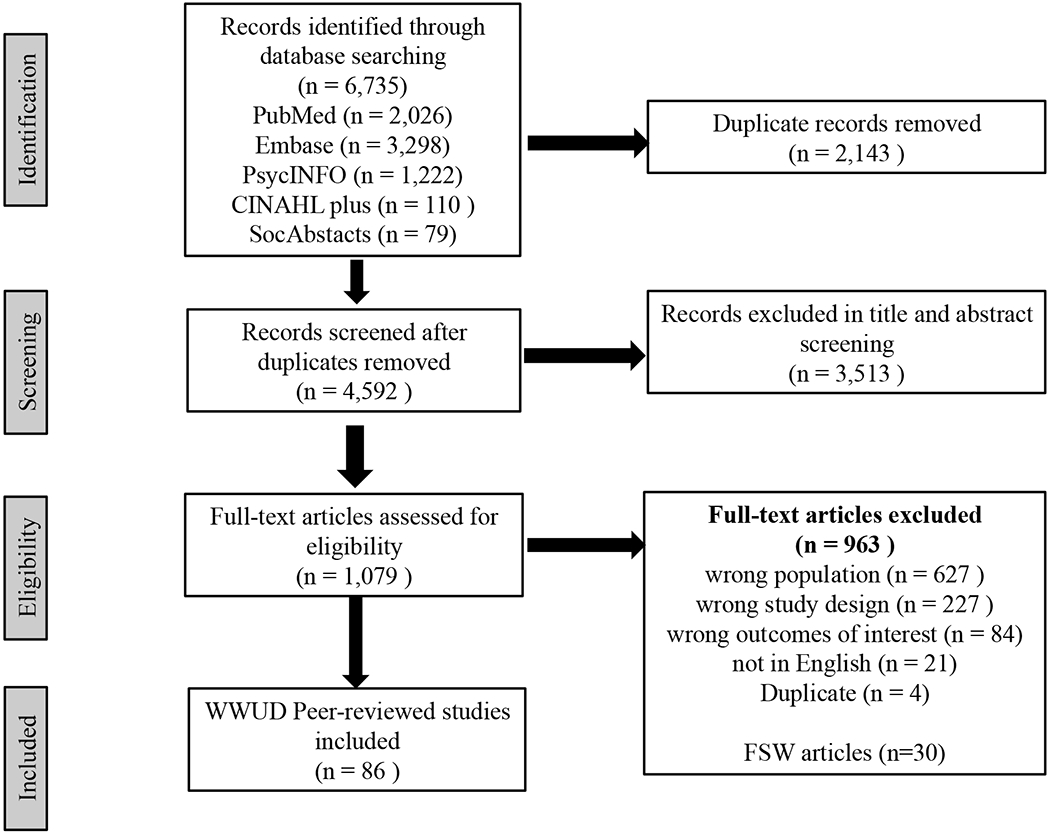
Selection of Sources Flow Chart
Among the 86 WWUD studies included in this review, 21% (n=18/86) did not specify the types of substance included in their study, giving general descriptors such as “illegal drug use”, “illicit drug use”, “injection drug use”, “non-injection drug use”, or “other drugs”. Among studies with specified substances (n=68), the most commonly included substances were cocaine (66%; 45/68), alcohol (51%; 35/68), and heroin (50%; 34/68) (Figure 2). Many studies included multiple substances.
Figure 2.
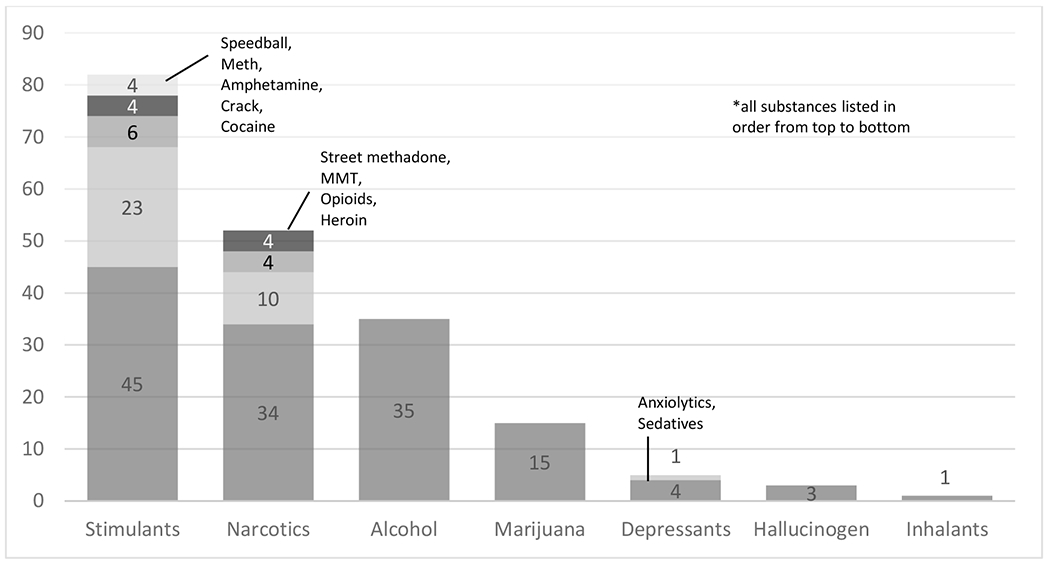
Categorization of substances in studies which included specified substances (n=68)
Note: Categorization of studies by specified substances was guided by the Drug Enforcement Administration (DEA) Resource Guide(Administration 2017), including: 1) Narcotics, 2) Stimulants, 3) Depressants, 4) Hallucinogens, 5) Marijuana/Cannabis, 6) Inhalants, and 7) Alcohol (not originally in the guide). Many studies included multiple substances.
Uptake findings are presented below, followed by adherence. Quantitative summaries of prevalence data for each outcome are offered, followed by narrative summaries of barriers and facilitators organized using the SEM. Analyses of gender difference are presented when applicable.
3.1. Uptake
Uptake was defined as ART initiation at any point. Twenty-eight studies reported uptake related findings (Table 3). Of those, nine reported uptake prevalence, ranging from 30% to 76%; variability is partially explained by differences in uptake assessment method, timing of assessment, ART eligibility, and ART status ascertainment. Measures included percentage of participants on ART (n=8) and percentage of ART initiation (n=1). Estimates of current use from the United States (U.S.) and Canada range from 48.7% to 76.1%(Hoots et al., 2017; Pach et al., 2003; Palepu et al., 2004; Sambamoorthi et al., 2000; Tapp et al., 2011). Current use was similar in China (53%)(Zhao et al., 2015) but slightly lower in Spain (39.7%, 32.6%) (Vallecillo et al., 2016; Vallecillo et al., 2010). Two studies investigated ART use trends. Current ART use has increased over time, from 50% in 2009 to 72% in 2015 in the U.S.(Hoots et al., 2017), and from 44% in 2004 to 54% in 2008 in Russia(Kissin et al., 2011).
Analyses of gender differences regarding uptake prevalence were conducted in 17 studies involving PWUD; 75% of these studies (n=12/17) found gender to be unrelated to ART use (Jarlais et al., 2016; Pach et al., 2003; Palepu et al., 2004; Palepu et al., 2011; Rusch et al., 2004; Sambamoorthi et al., 2000; Schroeder, 2001; Solomon et al., 2014; Uhlmann et al., 2010; Vallecillo et al., 2010; Wood et al., 2006; Zhao et al., 2015). Results varied among studies that found differences by gender (n=5/17). In the U.S., one study found women initiated ART earlier(Demas et al., 1998). However, WWID had less timely ART initiation in a different U.S. study, which included individuals from Canada(Hanna et al., 2013), and women who use non-injection drugs were less likely to receive ART in yet another U.S. study(Jarlais et al., 2016). In Spain, more women had been on ART(Vallecillo et al., 2016), whereas in Russia, women had lower odds of initiating ART(Goodness et al., 2014).
3.1.1. ART Uptake: Barriers and Facilitators
Intrapersonal factors associated with ART initiation among WWUD were examined in 14 studies, primarily in North America (U.S., n=8; U.S. and Canada, n=1; Canada, n=1, Russia, n=2; nine countries in Europe, n=1; unspecified, n=1). Substance use treatment programs at the organizational level were examined in two U.S. studies. No barriers or facilitators of uptake were studied at the interpersonal, structural, or policy level.
Drug use and depression were found to be ART uptake barriers, prior ART use was an ART facilitator. The majority of studies (86%, n=12/14) found that substance use was associated with lower ART uptake (Abatemarco et al., 2008; Bailey et al., 2011; Burke-Miller et al., 2006; Cook et al., 2007; Goodness et al., 2014; Hanna et al., 2013; Kissin et al., 2011; Neblett et al., 2011; Rusch et al., 2004; Sharpe et al., 2004; Theall et al., 2007; Warner et al., 2003). Three studies assessed injection drug use (IDU) specifically, and also found lower odds of uptake (Goodness et al., 2014; Kissin et al., 2011; Rusch et al., 2004). A European Union study found IDU history to be associated with lack of ART use during antenatal care (Bailey et al., 2011) and in the U.S. and Canada, IDU history among women was associated with less timely uptake compared to men who have sex with men (MSM) [adjusted hazard ratio (aHR): 0.64; 95% confidence interval (CI): 0.54, 0.75] (Hanna et al., 2013). Studies exploring specific substances found that women who used crack cocaine (Sharpe et al., 2004) or consumed alcohol (Theall et al., 2007) were less likely to use ART. The overlapping effects of depression and substance use were also explored; depressed WWUD were less likely to initiate highly active antiretroviral therapy (HAART) than non-depressed WWUD (Cook et al., 2007). Finally, prior ART use made WWUD more likely to initiate ART in the future (Goodness et al., 2014).
At the organizational level, two U.S. studies reported methadone maintenance treatment (MMT) and substance abuse treatment (SAT) as uptake facilitators; women on MMT had 72% greater odds [adjusted Odds Ratio (aOR): 1.72; 95% CI: 1.18, 2.51] of having ART prescribed compared with women not on MMT (Turner et al., 2000), and women who had received SAT were significantly more likely to use ART (OR: 2.12; 95% CI: 1.73, 2.60) (Warner et al., 2003).
3.2. Adherence
Sixty-six studies reported adherence related findings (see Table 3). Seventy-three percent of WWUD adherence studies (n=48/66) conducted analyses of gender differences. More studies found significant differences in adherence by gender (n=28) than not (n=20). Among the 28 studies reporting significant differences by gender, most (n=23) indicated men had greater adherence than women, while only 5 reported that women had greater adherence than men.
3.2.1. Adherence Outcomes and Measures
Adherence rates ranged 27% to 95% among studies reporting adherence outcomes (n=17/66), utilizing four methods to measure adherence: self-reported adherence (n=6), pharmacy refill records (n=6), adherence reminder devices (n=5), and pill count (n=1) (Note- One study utilized two methods). Fourteen studies used thresholds to categorize individuals as adherent, three reported multiple ways to categorize adherence. A 95% adherence cutoff was most common (n=9) followed by what was considered perfect adherence (100%; n=4). Two studies reported 80% or more adherence, and only one reported 75% and 85% cutoffs. In studies without a threshold, mean adherence was reported (n=3). ART discontinuation was reported in one study. Temporal trends in adherence measurement assessments and thresholds were examined in accordance with changes in guidelines, no clear correlations were observed. (Data not shown)
3.2.2. Adherence Barriers and Facilitators
Findings on adherence barriers and facilitators were included in 25 studies. The vast majority of findings are at the intrapersonal level, including substance use, mental health, and side effects. Some factors were identified at the interpersonal and organizational level, none at the structural or policy level.
Fourteen studies found substance use to negatively impact ART adherence; seven found no correlations and none found a positive association. Three studies explicitly compared adherence among former, current, and never PWUD with conflicting results. People who previously used drugs and are on methadone maintenance treatment were more adherent to ART than non-PWUD (Turner et al., 2000). Lifetime heroin use was not associated with adherence (> 90% ) (Liu et al., 2006), and adherence was similar across groups of prior, current, and never PWUD (Lopez et al., 2007). A U.S. study found problematic alcohol use to negatively impact ART adherence among women but not men (Berg et al., 2004). In a study with pregnant WWUD, drug use history was associated with decreased adherence during the postpartum year, but not during pregnancy (Bailey et al., 2014).
Six studies found mental health conditions to negatively impact ART adherence; three studies named depression (Arnsten et al., 2002; Kang et al., 2011; Powell-Cope et al., 2003), two studies named current psychiatric disorders (Mellins et al., 2002; Mellins et al., 2003) and one named psychological stress (Wilson et al., 2014). One study found that psychiatric care and antidepressants were associated with greater adherence among women diagnosed with depression, however, depression was more likely to negatively affect ART use for women than men(Turner et al., 2003).
In the U.S., additional individual level adherence barriers and facilitators were identified. Side effects were a main ART adherence barrier among WWUD in three U.S. studies(Applebaum et al., 2009; Berg et al., 2004; Powell-Cope et al., 2003), though wanting to avoid side effects became a less common barrier as time on treatment increased(Powell-Cope et al., 2003). One study determined that personal circumstances such as sleeping, being busy, change in schedule, forgetting, or feeling “too good” or “too sick” were common barriers to adherence(Powell-Cope et al., 2003). Another study found no association between perceived necessity of medication and concerns about medication with overall levels of adherence(Lopez et al., 2007). In Canada, WWUD with indigenous ancestry (47.8%) had lower adherence than WWUD without (58.7%)(Puskas et al., 2017).
At the interpersonal level, being married and attending support groups were positively associated, while having close family relationships or experiences of childhood sexual abuse were negatively associated with adherence (Kang et al., 2008). Trading sex for drugs was a barrier to adherence(Williams et al., 2000). Three studies examined gender and ART diversion, finding that the selling or trading of HIV medication illegally is associated with decreased adherence, among PWUD. In two studies, women were less likely to divert ART medications (Surratt et al., 2013; Tsuyuki and Surratt, 2015), whereas gender was unrelated to diversion in the other study(Surratt et al., 2015).
Among three U.S. studies examining the impact of adherence promoting interventions, two found a positive effect. (Copenhaver et al., 2011; Lopez et al., 2007) and one found no impact (Powell-Cope et al., 2003). One intervention study with several health promotion components, including medication adherence, found significant increases in reported adherence post-intervention(Lopez et al., 2007). A group intervention that focused on active healthcare participation and drug and sex-related risk reduction showed increased adherence post-intervention(Copenhaver et al., 2011). A timer-reminder intervention in the U.S. did not impact adherence(Powell-Cope et al., 2003).
4. DISCUSSION
This study is the first scoping review to assess ART uptake and adherence barriers and facilitators among WWUD globally, a population with high HIV prevalence worldwide(Des Jarlais et al., 2012; Larney et al., 2015). Our review found variability in ART uptake, ranging from 39% to 76%, with higher uptake reported in the U.S. and Canada and an increase over time. ART adherence ranged widely, from 27% to 91%. The variability found in our study, due in part to the method, time period, and threshold of the assessment utilized is similar to that reported in non-gender specific systematic reviews of PWUD(Bazzi et al., 2019; Malta et al., 2008). This variability may indicate a genuinely wide range in uptake and adherence globally, but more likely indicates a deficit in the research that is being conducted. As it stands, these data at a meta level hold very little meaning. The concept of uptake is particularly wide. Eight of the 86 included studies noted that the lack of a gold standard for adherence measurement was a major limitation, which is consistent with literature in the field of HIV and other medication adherence over multiple decades (Kreys, 2016; Lehmann et al., 2014; Vrijens et al., 2012). This underscores the need for ongoing efforts toward standardized and transparent operational definitions and measurements for data comparability(Berg and Arnsten, 2006; Williams et al., 2013), and indicates the complexity and challenge of this task. Research shows that adherence data differs across assessment method (Liu et al., 2001), and each approach comes with its own benefits and limitations. Best practices recommend assessing adherence via a triangulation of data sources (e.g. pill count, pharmacy refill data) and the development of a composite score, which may increase the validity and reliability of this measurement (Kreys, 2016; Lehmann et al., 2014; Vrijens et al., 2012). While gold standard assessments are needed, these may differ between high and low resource settings, where resources such as electronic pharmacy and insurance data might not always be available(Basu et al., 2019).
In this scoping review, an approximately equal number of studies reported significant differences in findings by gender (n=33), as those that did not (n=32), across uptake and adherence. Among those that found a difference, uptake findings were mixed and overwhelmingly women were seen to have less adherence. In our review process, we excluded many studies with PWUD relevant to our area of interest because they did not include gender disaggregated analysis. WWUD as a population has been underrepresented in the literature(Lal et al., 2015), complicated by the lack of gender disaggregated data from the majority of countries reporting HIV statistics among PWUD. This has resulted in few studies that are WWUD focused (Organization, 2014); prior reviews report challenges finding WWUD specific data(Anna Roberts, 2010). These findings indicate a broad need for more respectful inclusion of women in research, and more specifically more analysis by gender among HIV studies with PWUD, as well as more studies specifically focused on WWUD.
Overwhelmingly, studies explored barriers and facilitators of ART uptake and adherence among WWUD at the intrapersonal level, with history of drug use being the main barrier to uptake. Adherence studies included a few interpersonal and organizational barriers and facilitators. No studies investigated structural or policy level factors that may impact ART uptake and adherence, such as stigma, violence, drug use criminalization, healthcare services, health insurance, education, employment, housing, and incarceration, all factors which are known to impact HIV treatment among people who inject drugs (PWID)(Bazzi et al., 2019; DeBeck et al., 2017). For some WWID, gendered social norms result in increased stigma and discrimination(Des Jarlais et al., 2012). This has not been well explored in how it differs from general drug use stigma or how the norms impact HIV uptake and adherence. Additional structural factors should be explored.
While substance use emerged as a barrier to ART uptake and adherence, there were several limitations regarding the reporting of specificity of substance, route of administration, and temporality of drug use that limited nuanced understanding. When substances were assessed, crack and alcohol use as well as injection as a route of administration were associated with uptake barriers. There was wide discrepancy in study inclusion and definition regarding current (e.g. 3 days to 12 months), former, or ever drugs use. As using, cessation, and relapsing is a cycle, whether the participant is considered currently or formerly using drugs may depend on which phase of the cycle they are in during study enrollment. The variety of ways drug use was operationalized in these studies calls for both consistency in definition and further investigation into the relationships between substance use and ART uptake and adherence among WWUD, focusing on specific drug use characteristics and being more explicit in studies about how these categories are defined.
At the intrapersonal level, the majority of studies found that current or former substance use, as well as other mental health issues (e.g. depression, psychiatric disorders), were associated with ART uptake and adherence barriers. HIV-positive PWUD frequently have medical and psychiatric comorbidities, including substance-use disorders, that negatively affect health and complicate HIV treatment and prevention(Altice et al., 2010). Evidence demonstrates that substance use treatment improves the health behavior patterns of PWUD(Altice et al., 2010). A separation of HIV and substance use treatment services decreases engagement in both kinds of care(Magidson et al., 2019), while co-located programs have reported improvements in uptake, adherence, and reductions in mortality(Miller et al., 2018). A meta-analysis of opioid substitution therapy (OST) programs offered in North America, Europe, Indonesia and China found that OST was associated with increased ART uptake and decreased care attrition among PWUD, as well as an increase in viral suppression(Low et al., 2016). Mental health treatment programs have been found to independently improve health and HIV-related outcomes among a cohort of women, some of whom used drugs (Cook et al., 2006). HIV treatment programs that incorporate psychiatric treatments may bolster the effects of substance use treatment programs(Wechsberg et al., 2012), as recommending that patients cease substance use without treating underlying mental illnesses has had little efficacy(Basu et al., 2005). Finally, the recognition of the pervasive global experience of violence victimization and its subsequent impact on HIV outcomes supports the recommendation for incorporating a multi-level trauma informed care approach to HIV related interventions (Sales et al., 2016; Tenkorang et al., 2020). Taken together, these findings indicate the potential impact of increasing resources towards integrated programs offering HIV treatment and care connected to mental health and substance use treatment for WWUD.
At the interpersonal level, being married and attending support groups were adherence facilitators, while having close family relationships or experiences of childhood sexual abuse were adherence barriers. More insight is needed as to which types of relationships provide the most support, as it appears that not all interpersonal relationships improve adherence. Several important factors were not examined in association with adherence. One obvious omission was intimate partner violence (IPV), known to negatively impact Pre-exposure Prophylaxis (PrEP) uptake and adherence among WWUD (Glick et al., 2019). Another omission was sex work, though mentioned as an adherence barrier in one study. Concurrency between sex work and drug use is high; estimates of WWID engaged in sex work range between 15-66% in the USA, 20-50% in Eastern Europe, 10-25% in Central Asia, and 21-57% in China(Roberts et al., 2010). Sex work has a range of known uptake and adherence barriers for ART(Glick et al., 2020; Mountain et al., 2014)and PrEP(Glick et al., 2019), which should be considered when developing interventions for WWUD, as the chances of concurrency are great. Further, PWUD are more likely to report concurrent sex partners, unprotected sex, and have partners who also use drugs(Cleland et al., 2007) and WWUD have heightened sexual and drug use risk during relationships than their male counterparts(Cleland et al., 2007). More research is needed regarding interpersonal ART barriers and facilitators for WWUD, which could point to dyadic interventions that have been employed in HIV care trials(Cohen et al., 2012; Eshleman et al., 2017).
At the organizational level, substance use and mental health treatment interventions were found to be significantly associated with adherence. Gender specific considerations are important when delivering such interventions. As women are often caregivers, gendered resources and accommodations are necessary, such as varying hours or child-safe spaces.(Malinowska-Sempruch, 2015) Yet, women-focused programs often lack financial support(Carael et al., 2009). Intervention studies addressing health behaviors, including substance use and mental health, have been shown to facilitate adherence; increasing resources for gender specific interventions may further support the overall needs of WWUD.
4.1. Suggestions for future HIV research and interventions with WWUD
Findings from this scoping review have implications for HIV research on WWUD. Methodologically, standardized measurement of ART uptake and adherence, including optimal adherence level, and other barrier/facilitator-related indicators would enable direct comparisons across studies. Additionally, standardization on specificity of substance, route of administration, and temporality of drug use are needed, and short of that, being more explicit in studies about how these categories are defined. Finally, qualitative and mixed-methods studies are needed to explore nuances around ART barriers and facilitators. Further, the findings highlight a series of knowledge gaps regarding the ways in which factors spanning SEM levels may impact ART uptake and adherence. At the intra- and interpersonal levels, more insight is needed as to how different types of interpersonal relationships, IPV, and sex work engagement influence ART uptake and adherence. As no studies investigated structural or policy level factors that may impact ART uptake and adherence, insight on all of the following factors is needed: stigma, drug use criminalization, healthcare services, health insurance, education, employment, housing, food security, and incarceration. Overall, more research on WWUD is needed, including across more global locations, especially Africa, Asia, and Australia. Studies among PWUD should also include analyses of gender differences, to allow for differences by gender to be studied. Lastly, these findings offer intervention recommendations. WWUD need integrated HIV care that addresses co-occurring health issues such as IPV, mental health, and substance use. In addition, more gender-specific considerations should be employed within those programs. As women are often caregivers, gendered resources and accommodations may be necessary, such as varying hours of operation or creating child-safe spaces.
4.2. Limitations
Our findings have several limitations. First, differences in uptake and adherence measurements made a direct quantitative comparison of estimates difficult. Second, geographic variability was limited as the overwhelming majority of studies focused on a North American context, with some studies from Europe, only one study from China, India, and South America respectively, and no studies conducted in Africa and Australia. As such, generalizability of findings is limited, and more studies from diverse locations are needed. Third, while the review included two mixed-method studies, qualitative insights, which have the ability to explore nuances particularly applicable to barriers and facilitators, were limited. Fourth, had we been able to analyze results by specific substances in each study, further nuance in findings and implications of specific drugs on uptake or adherence may have emerged. However, due to the variety of substances used in each study, this level of analysis was not possible. Fifth, study participants must be 18 years and older to be included in our review. This disqualified studies that included younger people, most notable the WIHS study, which has contributed multiple manuscripts relevant to this topic(Dale et al., 2014; Lillie-Blanton et al., 2010; Zhang et al., 2018). Lastly, our aim was to conduct a broad review including various study designs and complementary viewpoints on the topic, however this limited our capacity to conduct systematic risk of bias assessment. Limitations assessed within the included studies ranged and included self-report biases (52%), generalizability issues (39%), limitations in their ability to measure variables that may have been related to uptake and adherence outcomes (26%), sample size (19%), cross-sectional study design (16%), and sampling bias (15%).
5. Conclusions
Our review aimed to assess the state of peer-reviewed literature on ART uptake and adherence among cisgender WWUD globally. We identified 86 studies, offering rich insight into ART uptake and adherence among WWUD. Our review found wide variability in ART uptake and adherence, largely due to inconsistencies in measurement, indicating a need for measurement standardization in the field. Barriers and facilitators were identified primarily at the intrapersonal level. Substance use, co-morbid psychiatric disorders, and side effects emerged as the primary barrier towards ART uptake and adherence among this population. Few facilitators were identified. More research is needed to understand the impact of factors at additional levels of the SEM (e.g., community, public policy) and the complex interaction between variables at different levels. This research should include qualitative and quantitative approaches and be conducted in various geographic contexts. Further, existing research with PWUD could benefit from including more analyses of gender differences and clarity on how substance use is defined. These review findings can inform ART interventions, future research, and offer guidance to other support services with WWUD, such as PrEP interventions.
Supplementary Material
Highlights.
Studies report ART uptake (30-76%) and adherence (27-95%) ranges among WWUD globally.
Adherence measurement and uptake definition are not consistent across literature.
Substance use, psychiatric disorders, and side effects were primary ART barriers, few facilitators were identified.
Many ART barriers/facilitators were identified at the intrapersonal level
More research is needed on ART barriers/facilitators at additional SEM levels.
Acknowledgments
We would like to thank all of the researchers who contributed to the studies included in this review.
Role of Funding Source
This work was supported by the NIH/NIDA (R34DA045619-02), the Drug Dependence Epidemiology Training Program, NIH/NIDA (T32DA007292), the Johns Hopkins University Hopkins Population Center (R24HD042854), and the Johns Hopkins University Center for AIDS Research.
Acronyms
- AIDS
acquired immune deficiency syndrome
- ART
antiretroviral therapy
- HAART
highly active antiretroviral therapy
- HIV
Human Immunodeficiency Virus
- IDU
injection drug use
- IPV
intimate partner violence
- MMT
methadone maintenance treatment
- MSM
men who have sex with men
- OST
opioid substitution therapy
- PLWH
persons living with HIV
- PrEP
Pre-exposure prophylaxis
- PWID
people who inject drugs
- PWUD
people who use drugs
- SAT
substance abuse treatment
- SEM
Social-Ecological Model
- U.S.
United States
- WHO
World Health Organization
- WWID
women who inject drugs
- WWUD
women who use drugs
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:10.1016/j.drugalcdep.2020.10821
Conflict of Interest
Susan Sherman is an expert witness in opioid legislation on the plaintiff’s side.
No other conflicts to declare.
References
- Abatemarco DJ, Catov JM, Cross H, Delnevo C, Hausman A, 2008. Factors associated with zidovudine receipt and prenatal care among HIV-infected pregnant women in New Jersey. Journal of health care for the poor and underserved 19(3), 814–828. [DOI] [PubMed] [Google Scholar]
- Altice FL, Kamarulzaman A, Soriano VV, Schechter M, Friedland GH, 2010. Treatment of medical, psychiatric, and substance-use comorbidities in people infected with HIV who use drugs. The Lancet 376(9738), 367–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anna Roberts BM, Degenhardt Louisa, 2010. Women who inject drugs: A review of their risks, experiences and needs. National Drug and Alcohol Research Centre (NDARC), University of New South Wales, Australia. [Google Scholar]
- Applebaum AJ, Richardson MA, Brady SM, Brief DJ, Keane TM, 2009. Gender and other psychosocial factors as predictors of adherence to highly active antiretroviral therapy (HAART) in adults with comorbid HIV/AIDS, psychiatric and substance-related disorder. AIDS and behavior 13(1), 60–65. [DOI] [PubMed] [Google Scholar]
- Arksey H, O’Malley L, 2005. Scoping studies: towards a methodological framework. International journal of social research methodology 8(1), 19–32. [Google Scholar]
- Arnsten JH, Demas PA, Grant RW, Gourevitch MN, Farzadegan H, Howard AA, Schoenbaum EE, 2002. Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. Journal of general internal medicine 17(5), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azim T, Bontell I, Strathdee SA, 2015. Women, drugs and HIV. International Journal of Drug Policy 26, S16–S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey H, Thorne C, Malyuta R, Townsend CL, Semenenko I, Cortina-Borja M, 2014. Adherence to antiretroviral therapy during pregnancy and the first year postpartum among HIV-positive women in Ukraine. BMC public health 14, 993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey H, Townsend C, Cortina-Borja M, Thorne C, 2011. Insufficient antiretroviral therapy in pregnancy: missed opportunities for prevention of mother-to-child transmission of HIV in Europe. Antiviral therapy 16(6), 895–903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C, 2013. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC public health 13(1), 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu S, Chwastiak LA, Bruce RD, 2005. Clinical management of depression and anxiety in HIV-infected adults. Aids 19(18), 2057–2067. [DOI] [PubMed] [Google Scholar]
- Basu S, Garg S, Sharma N, Singh MM, 2019. Improving the assessment of medication adherence: Challenges and considerations with a focus on low-resource settings. Tzu-Chi Medical Journal 31(2), 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazzi AR, Drainoni M-L, Biancarelli DL, Hartman JJ, Mimiaga MJ, Mayer KH, Biello KB, 2019. Systematic review of HIV treatment adherence research among people who inject drugs in the United States and Canada: evidence to inform pre-exposure prophylaxis (PrEP) adherence interventions. BMC public health 19(1), 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KM, Arnsten JH, 2006. Practical and conceptual challenges in measuring antiretroviral adherence. Journal of acquired immune deficiency syndromes (1999) 43(Suppl 1), S79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berg KM, Demas PA, Howard AA, Schoenbaum EE, Gourevitch MN, Arnsten JH, 2004. Gender differences in factors associated with adherence to antiretroviral therapy. Journal of General Internal Medicine 19(11), 1111–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke-Miller JK, Cook JA, Cohen MH, Hessol NA, Wilson TE, Richardson JL, Williams P, Gange SJ, 2006. Longitudinal relationships between use of highly active antiretroviral therapy and satisfaction with care among women living with HIV/AIDS. American journal of public health 96(6), 1044–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carael M, Marais H, Polsky J, Mendoza A, 2009. Is there a gender gap in the HIV response? Evaluating national HIV responses from the United Nations General Assembly Special Session on HIV/AIDS country reports. JAIDS Journal of Acquired Immune Deficiency Syndromes 52, S111–S118. [DOI] [PubMed] [Google Scholar]
- Cleland CM, Des Jarlais DC, Perlis TE, Stimson G, Poznyak V, 2007. HIV risk behaviors among female IDUs in developing and transitional countries. BMC public health 7(1), 271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen MS, McCauley M, Gamble TR, 2012. HIV treatment as prevention and HPTN 052. Current opinion in HIV and AIDS 7(2), 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook J, Grey D, Burke-Miller J, Cohen M, Anastos K, Gandhi M, Richardson J, Wilson T, Young M, 2006. Effects of treated and untreated depressive symptoms on highly active antiretroviral therapy use in a US multi-site cohort of HIV-positive women. AIDS care 18(2), 93–100. [DOI] [PubMed] [Google Scholar]
- Cook JA, Grey DD, Burke-Miller JK, Cohen MH, Vlahov D, Kapadia F, Wilson TE, Cook R, Schwartz RM, Golub ET, Anastos K, Ponath C, Goparaju L, Levine AM, 2007. Illicit drug use, depression and their association with highly active antiretroviral therapy in HIV-positive women. Drug and alcohol dependence 89(1), 74–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copenhaver MM, Lee IC, Margolin A, Bruce RD, Altice FL, 2011. Testing an optimized community-based human immunodeficiency virus (HIV) risk reduction and antiretroviral adherence intervention for HIV-infected injection drug users. Substance abuse 32(1), 16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale S, Cohen M, Weber K, Cruise R, Kelso G, Brody L, 2014. Abuse and resilience in relation to HAART medication adherence and HIV viral load among women with HIV in the United States. AIDS patient care and STDs 28(3), 136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeBeck K, Cheng T, Montaner JS, Beyrer C, Elliott R, Sherman S, Wood E, Baral S, 2017. HIV and the criminalisation of drug use among people who inject drugs: a systematic review. The lancet HIV 4(8), e357–e374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demas P, Schoenbaum EE, Hirky AE, Wills TA, Doll LS, Hartel DM, Klein RS, 1998. The relationship of HIV treatment acceptance and adherence to psychosocial factors among injecting drug users. AIDS and Behavior 2(4), 283–292. [Google Scholar]
- Des Jarlais DC, Feelemyer JP, Modi SN, Arasteh K, Hagan H, 2012. Are females who inject drugs at higher risk for HIV infection than males who inject drugs: an international systematic review of high seroprevalence areas. Drug and alcohol dependence 124(1-2), 95–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deshko T, 2015. HIV reduction among women who inject drugs can be achieved through women-specific programs and global targets: a model from Ukraine. JAIDS Journal of Acquired Immune Deficiency Syndromes 69, S98–S99. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Shaw SA, Dasgupta A, Strathdee SA, 2014. Drug use as a driver of HIV risks: reemerging and emerging issues. Current opinion in HIV and AIDS 9(2), 150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis PK, Martin WJ, Dodd PJJP, 2017. CD4 count and tuberculosis risk in HIV-positive adults not on ART: a systematic review and meta-analysis. 5, e4165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eshleman SH, Hudelson SE, Redd AD, Swanstrom R, Ou S-S, Zhang XC, Ping L-H, Piwowar-Manning E, Porcella SF, Sievers MF, 2017. Treatment as prevention: characterization of partner infections in the HIV prevention trials network 052 trial. Journal of acquired immune deficiency syndromes (1999) 74(1), 112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EuroCoord, O.I.P.T.o.t.C.o.O.H.E.R.i.E.i., 2012. CD4 cell count and the risk of AIDS or death in HIV-Infected adults on combination antiretroviral therapy with a suppressed viral load: a longitudinal cohort study from COHERE. PLoS medicine 9(3), e1001194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh D, Krishnan A, Gibson B, Brown S-E, Latkin CA, Altice FL, 2017. Social network strategies to address HIV prevention and treatment continuum of care among at-risk and HIV-infected substance users: a systematic scoping review. AIDS and Behavior 21(4), 1183–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick JL, Russo R, Jivapong B, Rosman L, Pelaez D, Footer KH, Sherman SG, 2019. The PrEP Care Continuum Among Cisgender Women Who Sell Sex and/or Use Drugs Globally: A Systematic Review. AIDS and Behavior, 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glick JL, Russo RG, Huang AK-H, Jivapong B, Ramasamy V, Rosman LM, Pelaez DL, Sherman SG, 2020. ART Uptake and Adherence among Female Sex Workers (FSW) Globally: A Scoping Review [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodness TM, Palfai TP, Cheng DM, Coleman SM, Bridden C, Blokhina E, Krupitsky E, Samet JH, 2014. Depressive symptoms and antiretroviral therapy (ART) initiation among HIV-infected Russian drinkers. AIDS and behavior 18(6), 1085–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grau LE, Griffiths-Kundishora A, Heimer R, Hutcheson M, Nunn A, Towey C, Stopka TJ, 2017. Barriers and facilitators of the HIV care continuum in Southern New England for people with drug or alcohol use and living with HIV/AIDS: perspectives of HIV surveillance experts and service providers. Addiction science and clinical practice 12(1), 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green D, Tordoff DM, Kharono B, Akullian A, Bershteyn A, Morrison M, Garnett G, Duerr A, Drain PK, 2020. Evidence of sociodemographic heterogeneity across the HIV treatment cascade and progress towards 90 - 90 - 90 in sub - Saharan Africa–a systematic review and meta - analysis. Journal of the International AIDS Society 23(3), e25470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O, Peacock R, 2005. Storylines of research in diffusion of innovation: a meta-narrative approach to systematic review. Social science medicine 61(2), 417–430. [DOI] [PubMed] [Google Scholar]
- Grigoryan A, Hall HI, Durant T, Wei X, 2009. Late HIV diagnosis and determinants of progression to AIDS or death after HIV diagnosis among injection drug users, 33 US States, 1996–2004. PloS one 4(2), e4445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwadz M, de Guzman R, Freeman R, Kutnick A, Silverman E, Leonard NR, Ritchie AS, Muñoz-Plaza C, Salomon N, Wolfe H, 2016. Exploring how substance use impedes engagement along the HIV care continuum: A qualitative study. Frontiers in public health 4, 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall HI, McDavid K, Ling Q, Sloggett A, 2006. Determinants of progression to AIDS or death after HIV diagnosis, United States, 1996 to 2001. Annals of epidemiology 16(11), 824–833. [DOI] [PubMed] [Google Scholar]
- Hanna DB, Buchacz K, Gebo KA, Hessol NA, Horberg MA, Jacobson LP, Kirk GD, Kitahata MM, Korthuis PT, Moore RD, Napravnik S, Patel P, Silverberg MJ, Sterling TR, Willig JH, Lau B, Althoff KN, Crane HM, Collier AC, Samji H, Thorne JE, Gill MJ, Klein MB, Martin JN, Rodriguez B, Rourke SB, Gange SJ, 2013. Trends and disparities in antiretroviral therapy initiation and virologic suppression among newly treatment-eligible HIV-infected individuals in North America, 2001-2009. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 56(8), 1174–1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heimer R, Usacheva N, Barbour R, Niccolai LM, Uusküla A, Levina OS, 2017. Engagement in HIV care and its correlates among people who inject drugs in St Petersburg, Russian Federation and Kohtla - Järve, Estonia. Addiction 112(8), 1421–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoots BE, Finlayson TJ, Broz D, Paz-Bailey G, 2017. Antiretroviral Therapy Use Among HIV-Infected People Who Inject Drugs-20 Cities, United States, 2009-2015. Journal of acquired immune deficiency syndromes (1999) 75 Suppl 3, S392–s396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infante C, Sosa-Rubi SG, Cuadra SM, 2009. Sex work in Mexico: vulnerability of male, travesti, transgender and transsexual sex workers. Cult Health Sex 11(2), 125–137. [DOI] [PubMed] [Google Scholar]
- Jarlais DC, Arasteh K, McKnight C, Feelemyer J, Hagan H, Cooper HL, Campbell AN, Tross S, Perlman DC, 2016. Providing ART to HIV Seropositive Persons Who Use Drugs: Progress in New York City, Prospects for “Ending the Epidemic”. AIDS and behavior 20(2), 353–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang SY, Deren S, Colon HM, 2011. Differential gender effects of depression on use of HIV medications among HIV-positive Puerto Rican drug users. AIDS care 23(11), 1467–1471. [DOI] [PubMed] [Google Scholar]
- Kang SY, Goldstein MF, Deren S, 2008. Gender differences in health status and care among HIV-infected minority drug users. AIDS care 20(9), 1146–1151. [DOI] [PubMed] [Google Scholar]
- Kiriazova T, Lunze K, Raj A, Bushara N, Blokhina E, Krupitsky E, Bridden C, Lioznov D, Samet JH, Gifford AL, 2017. “It is easier for me to shoot up”: stigma, abandonment, and why HIV-positive drug users in Russia fail to link to HIV care. AIDS care 29(5), 559–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kissin DM, Mandel MG, Akatova N, Belyakov NA, Rakhmanova AG, Voronin EE, Volkova GV, Yakovlev AA, Jamieson DJ, Vitek C, Robinson J, Miller WC, Hillis S, 2011. Five-year trends in epidemiology and prevention of mother-to-child HIV transmission, St. Petersburg, Russia: results from perinatal HIV surveillance. BMC infectious diseases 11, 292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreys E, 2016. Measurements of medication adherence: in search of a gold standard. J Clin Pathways 2(8), 43–47. [Google Scholar]
- Lal R, Deb KS, Kedia S, 2015. Substance use in women: Current status and future directions. Indian journal of psychiatry 57(Suppl 2), S275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larney S, Mathers BM, Poteat T, Kamarulzaman A, Degenhardt L, 2015. Global epidemiology of HIV among women and girls who use or inject drugs: current knowledge and limitations of existing data. Journal of acquired immune deficiency syndromes (1999) 69(Suppl 2), S100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann A, Aslani P, Ahmed R, Celio J, Gauchet A, Bedouch P, Bugnon O, Allenet B, Schneider MP, 2014. Assessing medication adherence: options to consider. International journal of clinical pharmacy 36(1), 55–69. [DOI] [PubMed] [Google Scholar]
- Lillie-Blanton M, Stone VE, Snow Jones A, Levi J, Golub ET, Cohen MH, Hessol NA, Wilson TE, 2010. Association of race, substance abuse, and health insurance coverage with use of highly active antiretroviral therapy among HIV-infected women, 2005. American Journal of Public Health 100(8), 1493–1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Golin CE, Miller LG, Hays RD, Beck CK, Sanandaji S, Christian J, Maldonado T, Duran D, Kaplan AH, 2001. A comparison study of multiple measures of adherence to HIV protease inhibitors. Annals of internal medicine 134(10), 968–977. [DOI] [PubMed] [Google Scholar]
- Liu H, Longshore D, Williams JK, Rivkin I, Loeb T, Warda US, Carmona J, Wyatt G, 2006. Substance abuse and medication adherence among HIV-positive women with histories of child sexual abuse. AIDS and behavior 10(3), 279–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez E, Jones DL, Ishii M, Tobin JN, Weiss SM, 2007. HIV Medication Adherence and Substance Use: The Smartest Women’s Project. American journal of infectious diseases 3(4), 240–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low AJ, Mburu G, Welton NJ, May MT, Davies CF, French C, Turner KM, Looker KJ, Christensen H, McLean S, 2016. Impact of opioid substitution therapy on antiretroviral therapy outcomes: a systematic review and meta-analysis. Clinical Infectious Diseases 63(8), 1094–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma PH, Chan ZC, Loke AY, 2017. The socio-ecological model approach to understanding barriers and facilitators to the accessing of health services by sex workers: a systematic review. AIDS and Behavior 21(8), 2412–2438. [DOI] [PubMed] [Google Scholar]
- Magidson JF, Joska JA, Regenauer KS, Satinsky E, Andersen LS, Seitz-Brown C, Borba CP, Safren SA, Myers B, 2019. “Someone who is in this thing that I am suffering from”: The role of peers and other facilitators for task sharing substance use treatment in South African HIV care. International Journal of Drug Policy 70, 61–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malinowska-Sempruch K, 2015. What interventions are needed for women and girls who use drugs? A global perspective. JAIDS Journal of Acquired Immune Deficiency Syndromes 69, S96–S97. [DOI] [PubMed] [Google Scholar]
- Malta M, Strathdee SA, Magnanini MM, Bastos FI, 2008. Adherence to antiretroviral therapy for human immunodeficiency virus/acquired immune deficiency syndrome among drug users: a systematic review. Addiction 103(8), 1242–1257. [DOI] [PubMed] [Google Scholar]
- Matsuzaki M, Vu QM, Gwadz M, Delaney JA, Kuo I, Trejo MEP, Cunningham WE, Cunningham CO, Christopoulos K, 2018. Perceived access and barriers to care among illicit drug users and hazardous drinkers: findings from the Seek, Test, Treat, and Retain data harmonization initiative (STTR). BMC public health 18(1), 366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy KR, Bibeau D, Steckler A, Glanz K, 1988. An ecological perspective on health promotion programs. Health education quarterly 15(4), 351–377. [DOI] [PubMed] [Google Scholar]
- Mellins CA, Havens JF, McCaskill EO, Leu CS, Brudney K, Chesney MA, 2002. Mental health, substance use and disclosure are significantly associated with the medical treatment adherence of HIV-infected mothers. Psychology, Health and Medicine 7(4), 451–460. [Google Scholar]
- Mellins CA, Kang E, Leu CS, Havens JF, Chesney MA, 2003. Longitudinal study of mental health and psychosocial predictors of medical treatment adherence in mothers living with HIV disease. AIDS patient care and STDs 17(8), 407–416. [DOI] [PubMed] [Google Scholar]
- Metsch L, Philbin MM, Parish C, Shiu K, Frimpong JA, Giang LM, 2015. HIV testing, care, and treatment among women who use drugs from a global perspective: progress and challenges. Journal of acquired immune deficiency syndromes (1999) 69(0 2), S162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WC, Hoffman IF, Hanscom BS, Ha TV, Dumchev K, Djoerban Z, Rose SM, Latkin CA, Metzger DS, Lancaster KE, 2018. A scalable, integrated intervention to engage people who inject drugs in HIV care and medication-assisted treatment (HPTN 074): a randomised, controlled phase 3 feasibility and efficacy study. The Lancet 392(10149), 747–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milloy M-J, Kerr T, Bangsberg DR, Buxton J, Parashar S, Guillemi S, Montaner J, Wood E, 2012. Homelessness as a structural barrier to effective antiretroviral therapy among HIV-seropositive illicit drug users in a Canadian setting. AIDS patient care and STDs 26(1), 60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mizuno Y, Purcell DW, Knowlton AR, Wilkinson JD, Gourevitch MN, Knight KR, 2015. Syndemic vulnerability, sexual and injection risk behaviors, and HIV continuum of care outcomes in HIV-positive injection drug users. AIDS and Behavior 19(4), 684–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mountain E, Mishra S, Vickerman P, Pickles M, Gilks C, Boily M.-C.J.P.o., 2014. Antiretroviral therapy uptake, attrition, adherence and outcomes among HIV-infected female sex workers: a systematic review and meta-analysis. 9(9), e105645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neblett RC, Hutton HE, Lau B, McCaul ME, Moore RD, Chander G, 2011. Alcohol consumption among HIV-infected women: impact on time to antiretroviral therapy and survival. Journal of women’s health (2002) 20(2), 279–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization, W.H., 2014. Women who inject drugs and HIV: addressing specific needs. World Health Organization. [Google Scholar]
- Pach A 3rd, Cerbone FG, Gerstein DR, 2003. A qualitative investigation of antiretroviral therapy among injection drug users. AIDS and behavior 7(1), 87–100. [DOI] [PubMed] [Google Scholar]
- Palepu A, Horton NJ, Tibbetts N, Meli S, Samet JH, 2004. Uptake and adherence to highly active antiretroviral therapy among HIV-infected people with alcohol and other substance use problems: the impact of substance abuse treatment. Addiction (Abingdon, England) 99(3), 361–368. [DOI] [PubMed] [Google Scholar]
- Palepu A, Milloy MJ, Kerr T, Zhang R, Wood E, 2011. Homelessness and adherence to antiretroviral therapy among a cohort of HIV-infected injection drug users. Journal of urban health: bulletin of the New York Academy of Medicine 88(3), 545–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB, 2015. Guidance for conducting systematic scoping reviews. International journal of evidence-based healthcare 13(3), 141–146. [DOI] [PubMed] [Google Scholar]
- Pinkham S, Malinowska-Sempruch KJRh.m., 2008. Women, harm reduction and HIV. 16(31), 168–181. [DOI] [PubMed] [Google Scholar]
- Powell-Cope GM, White J, Henkelman EJ, Turner BJ, 2003. Qualitative and quantitative assessments of HAART adherence of substance-abusing women. AIDS care 15(2), 239–249. [DOI] [PubMed] [Google Scholar]
- Puskas CM, Kaida A, Miller CL, Zhang W, Yip B, Pick N, Montaner JS, Hogg RS, 2017. The adherence gap: a longitudinal examination of men’s and women’s antiretroviral therapy adherence in British Columbia, 2000-2014. AIDS (London, England) 31(6), 827–833. [DOI] [PubMed] [Google Scholar]
- Roberts A, Mathers B, Degenhardt L, 2010. Women who inject drugs: A review of their risks, experiences and needs. A report prepared on behalf of the Reference Group to the United Nations on HIV and Injecting Drug Use. Australia Sydney: National Drug and Alcohol Research Centre (NDARC), University of New South Wales. [Google Scholar]
- Rusch M, Nixon S, Schilder A, Braitstein P, Chan K, Hogg RS, 2004. Use of antiretroviral therapy among HIV positive individuals living in British Columbia. AIDS care 16(7), 914–922. [DOI] [PubMed] [Google Scholar]
- Sales JM, Swartzendruber A, Phillips AL, 2016. Trauma-informed HIV prevention and treatment. Current HIV/AIDS reports 13(6), 374–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sambamoorthi U, Warner LA, Crystal S, Walkup J, 2000. Drug abuse, methadone treatment, and health services use among injection drug users with AIDS. Drug and alcohol dependence 60(1), 77–89. [DOI] [PubMed] [Google Scholar]
- Schroeder JR, 2001. Social factors related to antiretroviral therapy use in injection drug users. AIDS and Behavior 5(4), 363–369. [Google Scholar]
- Sharpe TT, Lee LM, Nakashima AK, Elam-Evans LD, Fleming PL, 2004. Crack cocaine use and adherence to antiretroviral treatment among HIV-infected black women. Journal of community health 29(2), 117–127. [DOI] [PubMed] [Google Scholar]
- Solomon SS, Srikrishnan AK, Vasudevan CK, Anand S, Kumar MS, Balakrishnan P, Mehta SH, Solomon S, Lucas GM, 2014. Voucher incentives improve linkage to and retention in care among HIV-infected drug users in Chennai, India. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 59(4), 589–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surratt HL, Kurtz SP, Cicero TJ, O’Grady C, Levi-Minzi MA, 2013. Antiretroviral medication diversion among HIV-positive substance abusers in South Florida. American journal of public health 103(6), 1026–1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surratt HL, Kurtz SP, Levi-Minzi MA, Chen M, 2015. Environmental Influences on HIV Medication Adherence: The Role of Neighborhood Disorder. American journal of public health 105(8), 1660–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapp C, Milloy MJ, Kerr T, Zhang R, Guillemi S, Hogg RS, Montaner J, Wood E, 2011. Female gender predicts lower access and adherence to antiretroviral therapy in a setting of free healthcare. BMC infectious diseases 11, 86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenkorang EY, Asamoah-Boaheng M, Owusu AY, 2020. Intimate partner violence (IPV) against HIV-positive women in Sub-Saharan Africa: a mixed-method systematic review and meta-analysis. Trauma, Violence, and Abuse, 1524838020906560. [DOI] [PubMed] [Google Scholar]
- Theall KP, Clark RA, Powell A, Smith H, Kissinger P, 2007. Alcohol consumption, art usage and high-risk sex among women infected with HIV. AIDS and Behavior 11(2), 205–215. [DOI] [PubMed] [Google Scholar]
- Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, 2018. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Annals of internal medicine 169(7), 467–473. [DOI] [PubMed] [Google Scholar]
- Tsuyuki K, Surratt HL, 2015. Antiretroviral drug diversion links social vulnerability to poor medication adherence in substance abusing populations. AIDS and behavior 19(5), 869–881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner BJ, Laine C, Cosler L, Hauck WW, 2003. Relationship of gender, depression, and health care delivery with antiretroviral adherence in HIV-infected drug users. Journal of general internal medicine 18(4), 248–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner BJ, Newschaffer CJ, Zhang D, Cosler L, Hauck WW, 2000. Antiretroviral use and pharmacy-based measurement of adherence in postpartum HIV-infected women. Medical care 38(9), 911–925. [DOI] [PubMed] [Google Scholar]
- Uhlmann S, Milloy MJ, Kerr T, Zhang R, Guillemi S, Marsh D, Hogg RS, Montaner JS, Wood E, 2010. Methadone maintenance therapy promotes initiation of antiretroviral therapy among injection drug users. Addiction (Abingdon, England) 105(5), 907–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallecillo G, Mojal S, Roquer A, Samos P, Luque S, Martinez D, Martires PK, Torrens M, 2016. Low non-structured antiretroviral therapy interruptions in HIV-infected persons who inject drugs receiving multidisciplinary comprehensive HIV care at an outpatient drug abuse treatment center. AIDS and Behavior 20(5), 1068–1075. [DOI] [PubMed] [Google Scholar]
- Vallecillo G, Sanvisens A, Martinez E, Torrens M, Bolao F, Tor J, Muga R, 2010. Use of highly active antiretroviral therapy is increasing in HIV positive severe drug users. Current HIV research 8(8), 641–648. [DOI] [PubMed] [Google Scholar]
- Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, Dobbels F, Fargher E, Morrison V, Lewek P, 2012. A new taxonomy for describing and defining adherence to medications. British journal of clinical pharmacology 73(5), 691–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner LA, Wei W, McSpiritt E, Sambamoorthi U, Crystal S, 2003. Ante- and postpartum substance abuse treatment and antiretroviral therapy among HIV-infected women on Medicaid. Journal of the American Medical Women’s Association (1972) 58(3), 143–153. [PubMed] [Google Scholar]
- Wechsberg WM, Golin C, El-Bassel N, Hopkins J, Zule W, 2012. Current interventions to reduce sexual risk behaviors and crack cocaine use among HIV-infected individuals. Current HIV/AIDS reports 9(4), 385–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, W.H.O., 2017. Policy brief: Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations, 2016 update. Geneva. [PubMed] [Google Scholar]
- Williams AB, Amico KR, Bova C, Womack JA, 2013. A proposal for quality standards for measuring medication adherence in research. AIDS and Behavior 17(1), 284–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams M, Bowen A, Ross M, Freeman R, Elwood W, 2000. Perceived compliance with AZT dosing among a sample of African-American drug users. International journal of STD and AIDS 11(1), 57–63. [DOI] [PubMed] [Google Scholar]
- Wilson SM, Sikkema KJ, Ranby KW, 2014. Gender moderates the influence of psychosocial factors and drug use on HAART adherence in the context of HIV and childhood sexual abuse. AIDS care 26(8), 959–967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood E, Kerr T, Palepu A, Zhang R, Strathdee SA, Tyndall MW, Montaner JS, Hogg RS, 2006. Slower uptake of HIV antiretroviral therapy among Aboriginal injection drug users. The Journal of infection 52(4), 233–236. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Wilson TE, Adedimeji A, Merenstein D, Milam J, Cohen J, Cohen M, Golub ET, 2018. The impact of substance use on adherence to antiretroviral therapy among HIV-infected women in the United States. AIDS and Behavior 22(3), 896–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Shi CX, McGoogan JM, Rou K, Zhang F, Wu Z, 2015. Predictors of accessing antiretroviral therapy among HIV - positive drug users in China’s National Methadone Maintenance Treatment Programme. Addiction 110(Suppl 1), 40–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


