Abstract
Introduction
Osteoarthritis of the first carpometacarpal joint is a common degenerative disease and surgical treatment includes resection suspension interposition arthroplasty (RSIA) with or without temporary transfixation of the first metacarpal. One major drawback includes proximalization of the first metacarpal during the postoperative course. Specific data comparing different transfixation techniques in this context is sparse.
Materials and methods
In this retrospective study, we measured the trapezial space ratio (TSR) in 53 hands before and after RSIA to determine the proximalization of the first metacarpal depending on the type of Kirschner (K)-wire transfixation. We, therefore, compared transfixation of the first metacarpal to the scaphoid with one K-wire (1K) to transfixation of the first metacarpal with two K-wires (2K), either to the carpus (2Ka), or to the second metacarpal (2Kb), or to both second metacarpal and carpus (2Kc).
Results
While preoperative TSR did not differ between group 1K and 2K (p = 0.507), postoperative TSR was significantly higher in group 2K compared to 1K (p = 0.003). Comparing subgroups, postoperative TSR was significantly higher in group 2Kc than 1K (p = 0.046), while we found no significant difference comparing either group 2Ka or 2Kb to 1K (p = 0.098; p = 0.159). Neither did we find a significant difference within 2K subgroups, comparing group 2Ka and 2Kb (p = 0.834), 2Ka and 2Kc (p = 0.615), or 2Kb and 2Kc (p = 0.555).
Conclusions
The results of our study suggest that transfixation with two K-wires should be preferred to transfixation with one K-wire after RSIA. Specifically, transfixation from first to second metacarpal and from first metacarpal to carpus resulted in least proximalization of the first metacarpal postoperatively.
Keywords: CMC1 joint, Osteoarthritis, Resection suspension arthroplasty, Saddle joint, First metacarpal proximalization, K-wire transfixation
Introduction
Osteoarthritis of the first carpometacarpal joint occurs predominantly in women and shows an increasing prevalence with age [1–3]. The disease exhibits an age-adjusted radiographic prevalence of 15% in women and 7% in men 30 years of age or older [2]. Amongst others, biomechanical factors are assumed to contribute to the development of osteoarthritis of the first carpometacarpal joint. Joints with low congruence are susceptible to increased wear of cartilage, which in turn increases the risk of osteoarthritis [4–7]. Additionally, the great range of motion, small contact areas of the joint surfaces and intensive usage exacerbate this issue [8]. In postmenopausal women, a hormonally mediated weakening of the trapeziometacarpal ligaments is discussed, which can additionally lead to decreased joint stability [9]. Obesity and positive family history are considered as risk factors as well [10, 11]. Many patients only suffer from mild symptoms. However, the disease can lead to heavy pain, loss of grip strength and instability of the first carpometacarpal joint in a subset of patients, leading to a pronounced functional impairment of the hand and restrictions in daily routine. During the early stages of the disease, treatment goals are relieving symptoms and slowing the progress while operative procedures are implemented in later stages. Many operative techniques, including ligament reconstruction and/or ligament interposition, have been described by multiple authors [12–15]. A fundamental element of such procedures is the resection of the trapezial bone. Additionally, most techniques create a suspension arthroplasty using either a strip of the flexor carpi radialis tendon or the abductor pollicis longus tendon, with or without interposition to avoid an impingement between the first metacarpal base and the scaphoid [16]. Burton and Pellegrini described a method of postoperative Kirschner (K)-wire transfixation from the first metacarpal to the scaphoid to ensure postoperative stabilization during healing [17], which was also used by others later on [18–20]. However, from a biomechanical point of view, a transfixation of the first metacarpal to the scaphoid seems less suited to limit proximalization of the first metacarpal, as the K-wire lies longitudinally to the direction of muscle traction. Thus, a more horizontal vector of transfixation would be more appropriate.
Data on the actual shrinkage of the resection cavity of the trapezium are sparse and includes only small case numbers [17, 21].
To evaluate the influence of temporary K-wire transfixation on the proximalization of the first metacarpal bone, we retrospectively analyzed different methods of K-wire transfixation during resection suspension interposition arthroplasty (RSIA) by radiographic means.
Materials and methods
Collective
All patients having undergone RSIA in our clinic for osteoarthritis of the first carpometacarpal joint between 2005 and 2019 were retrospectively analyzed. For analysis, pre- and postoperative radiographs of the thumb were necessary. Thus, patients without adequate radiographs or follow-up were excluded. Of the remaining cases, those were included which had either received K-wire transfixation of the first metacarpal base to the scaphoid (group 1K, Fig. 1a), or two K-wires for transfixation of the first metacarpal (group 2K). Group 2K was further divided into subgroups according to the manner of transfixation: transfixation of the first metacarpal to the carpus (group 2Ka, Fig. 1b), to the second metacarpal (group 2Kb, Fig. 1c) or to both carpus and second metacarpal (group 2Kc, Fig. 1d).
Fig. 1.
Methods of transfixation. Patients received transfixation with one K-wire from the first metacarpal to the scaphoid (group 1K, a), or with two K-wires from the first metacarpal to the carpus (group 2Ka, b), from the first to second metacarpal (group 2Kb, c) or from the first to both second metacarpal and carpus (group 2Kc, d)
To evaluate the influence of K-wire transfixation on proximalization of the first metacarpal, the trapezial space ratio (TSR) was measured for each group and subgroup via preoperative as well as postoperative radiographs as described below.
Calculation of the TSR
The TSR is a measurement of the space occupied by the trapezial bone and was calculated as described by Kadiyala et al. [22]. Conventional X-ray images of the affected thumb were taken. The distance between the subchondral surfaces of the first metacarpal base and the distal scaphoid was measured. Likewise, the length of the proximal phalanx of the thumb was measured between the subchondral surface of the base and the distal aspect of the first proximal phalanx (Fig. 2) and rounded to 0.1 mm. The TSR was calculated as the ratio of these two measurements and was rounded to three decimal places.
Fig. 2.

Calculation of the TSR. The TSR is calculated as the fraction of height of the trapezial space and the length of the proximal phalanx of the thumb
Operating technique and follow-up treatment
RSIA was performed as described by Beckenbaugh-Linscheid [23] by different senior physicians in our clinic. Mainly, a radiographic stage three of the first CMC osteoarthritis after Eaton and Littler was found preoperatively (Table 1). The stage had no influence on the manner of transfixation. Patients both with and without thumb adduction were included in the analysis. At first, the trapezial bone is resected via a dorsal incision [24]. Then a strip of about one-third of the flexor carpi radialis tendon is prepared, leaving it attached distally. Then it is pulled through a hole drilled through the base of the first metacarpal, led back to the tendon insertion and sutured to itself. This results in the first metacarpal base being suspended from the second metacarpal base. The rest of the strip of the flexor carpi radialis tendon is used as a spacer for the resected trapezial bone. At the end of the operation, K-wire transfixation of the first metacarpal base was performed during distraction of the thumb ray as described above. For transfixation, K-wires of 1.2 mm ± 0.1 mm were used. Time of K-wire removal was depicted from patient records. Immobilization of the thumb took place in a cast or an orthosis for 5 weeks postoperatively. After immobilization, the patients received physiotherapy, increasing the load on the hand gradually.
Table 1.
Biometrical data and radiographic stages of first CMC osteoarthritis in collective
| Group | Number of female patients | Number of male patients | Mean age (years) | Radiographic stage of first CMC osteoarthritis after Eaton and Littler | |||
|---|---|---|---|---|---|---|---|
| I | II | III | IV | ||||
| 1K | 16 | 4 | 68.0 | – | 4 | 12 | 5 |
| 2Ka | 9 | – | 56.3 | – | 2 | 5 | 2 |
| 2Kb | 6 | 2 | 57.1 | – | 2 | 4 | 2 |
| 2Kc | 13 | 2 | 60.0 | – | 2 | 9 | 4 |
Statistical analysis
GraphPad Prism 7.0 (GraphPad Software Inc., La Jolla, CA, USA) was used for statistical analysis. Descriptive statistics were expressed as mean and standard deviation. Shapiro–Wilk test was used to assess data normality. An unpaired t test or Mann–Whitney test was used, as appropriate. Significance was set at a p value < 0.05.
Results
Between 2005 and 2019, there were 117 RSIA performed in a total of 107 patients. There were 10 patients, who had received RSIA on both hands. 59 cases with no adequate postoperative radiograph or follow-up were excluded from the study. Of the remaining 58 cases, 21 cases were included with one K-wire, transfixating the first metacarpal base to the scaphoid (group 1K). There was one case with one K-wire transfixation from the first to second metacarpal and four cases with one K-wire transfixating the first metacarpal to the trapezoid bone. Those two techniques of K-wire transfixation were not included in our analysis due to the small number of cases. There were 32 cases with two K-wires in total (group 2K). Of those 32 cases, there were 9 cases in group 2Ka (first metacarpal to carpus), 8 cases in group 2Kb (first to second metacarpal), and 15 cases in group 2Kc (first metacarpal to both carpus and second metacarpal). In group 1K, we found a gender distribution of 16 women to four men (one woman having had received RSIA on both hands), in group 2Ka of 9 women only, in group 2Kb of 6 women to 2 men and in group 2Kc of 13 women to 2 men (Table 1). The average age in the collective was 62 years at the time of the operation. No revision surgeries were necessary. K-wire removal took place after 13.6 ± 8.1 days on average. Follow-up radiographs were obtained 257 ± 251 days postoperatively on average. Follow-up did not differ much comparing group 1 vs. 2K (286 days ± 297 vs. 250 days ± 221).
Preoperatively, we observed an average TSR of 0.392 ± 0.069 in group 1K. Postoperatively, the TSR decreased to 0.174 ± 0.058 in this group. In group 2K, there was a preoperative TSR of 0.402 ± 0.073, which decreased to 0.22 ± 0,078 after surgery. When analyzing 2K subgroups, a decrease from a preoperative TSR of 0.386 ± 0.065 to a postoperative TSR of 0.212 ± 0.047 for group 2Ka could be shown. A similar trend was observed for group 2Kb (preoperative TSR = 0.436 ± 0.051, postoperative TSR = 0.207 ± 0.045) and group 2Kc (preoperative TSR = 0.394 ± 0.085, postoperative TSR = 0.231 ± 0.105). Statistical analysis revealed no difference between the preoperative TSR of group 1K and 2K (p = 0.507) as well as between the preoperative TSR of 1K and 2K subgroups (1K vs. 2Ka, p = 0.829, 1K vs. 2Kb: p = 0.139, 2Kc: p = 0.958). Within 2K subgroups, there was also no significant difference between preoperative TSR (2Ka vs. 2Kb: p = 0.139, 2Ka vs. 2Kc: p = 0.414, 2Kb vs. 2Kc: p = 0.215) (Fig. 3a). Postoperative TSR was significantly higher in group 2K compared to 1K (p = 0.003). Additionally, subgroup 2Kc showed a higher postoperative TSR value compared to 1K (p = 0.046). No difference could be shown between group 1K and 2Ka (p = 0.098) or 1K and 2Kb (p = 0.159), however, with a trend towards higher TSR values in 2K subgroups without reaching statistical significance with respect to group 1K. Again, postoperative TSR values within 2K subgroups did not differ (2Ka vs. 2Kb: p = 0.843, 2Ka vs. 2Kc: p = 0.615, 2Kb vs. 2Kc: p = 0.555) (Fig. 3b).
Fig. 3.
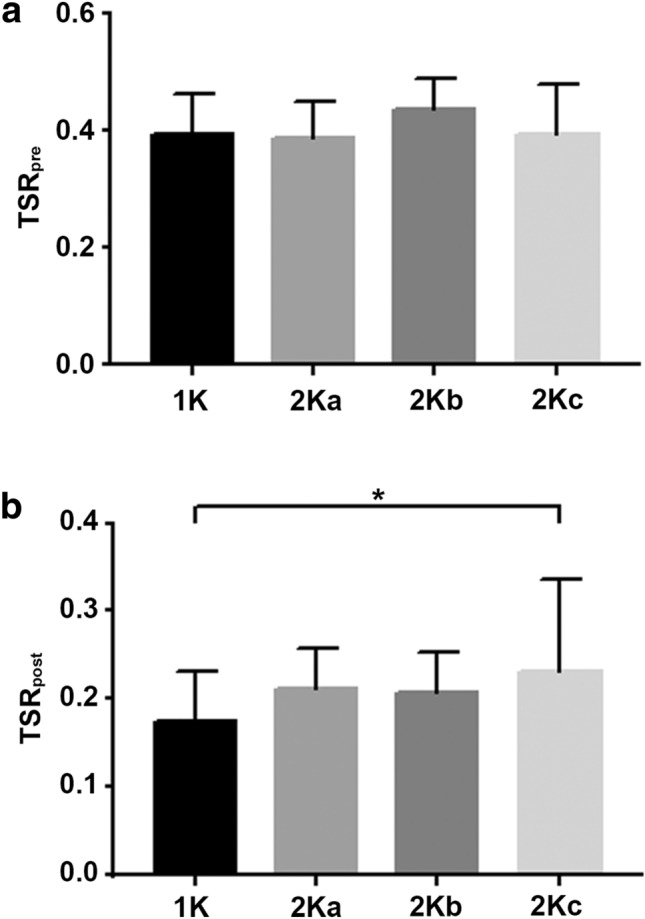
a Preoperative TSR-values. Preoperative TSR-values (TSRpre) did not differ between group 1K and 2Ka, b or c. We found no significant difference between 2Ka and 2Kc (p = 0.414), 2Kb and 2Kc (p = 0.215) or 2Ka and 2Kb (p = 0.139). Statistical significance between groups was tested with two-tailed unpaired t test or two-tailed Mann–Whitney test as appropriate. *p < 0.05. b Postoperative TSR-values. Postoperative TSR-values (TSR post) were significantly higher in group 2Kc compared to 1K (p = 0.046. No significant difference was found when comparing group 2Ka or 2Kb to 1K (p = 0.098, p = 0.159, respectively) and within 2K subgroups [p (2Ka vs. 2Kb) = 0.843, p (2Ka vs. 2Kc) = 0.615, p (2Kb vs. 2Kc) = 0.555]. Statistical significance between groups was tested with two-tailed unpaired t test. *p < 0.05
Discussion
Due to its extraordinary anatomy, the first carpometacarpal joint with its high degree of thumb movement is especially susceptible to osteoarthritic changes [8]. Long-term follow-up studies after surgical therapy of symptomatic advanced osteoarthritis of the first carpometacarpal joint through RSIA show largely positive subjective and objective treatment outcomes [25–30]. An obvious and generally acknowledged problem is that the distance between the first metacarpal base and the scaphoid decreases in the long term after resection of the trapezial bone. This can lead to an impingement with corresponding clinical symptoms [31, 32]. Furthermore, a recent study showed the importance of maintaining thumb length due to an inverse correlation of thumb length with overall Disabilities of the Arm, Shoulder, and Hand (DASH) scores and specific DASH questions involving high-strength activities [33]. To address this problem, different concepts with ligament reconstruction [34], tendon interposition [25], joint replacement [35–37], or spacers have been proposed [38, 39]. However, the earlier propagated use of silicon interposition resulted in rapid abrasion and fast reduction of the resection cavity [40–42], which is why larger registers dissuade their use [43].
Kadiyala et al. examined 15 patients with symptomatic degenerative first carpometacarpal osteoarthritis before and after surgical treatment with ligament reconstruction and tendon interposition arthroplasty. They found a TSR of 0.372 ± 0.084 in preoperative and of 0.270 ± 0.078 in postoperative X-rays of thumbs with symptomatic first carpometacarpal osteoarthritis [22]. Having found a TSR reduction of 43% in comparison to healthy thumbs, they emphasized the importance of ligament reconstruction and tendon interposition for maintaining the length of the thumb, which is essential for grip function [44]. In 1986, Burton and Pellegrini described excellent postoperative results after RSIA and transfixation of the first metacarpal to the scaphoid for osteoarthritis of the first carpometacarpal joint. They described that proximalization of the first metacarpal averaged only 11% of the initial arthroplasty space versus nearly 50% loss of height with silicone implants [17]. However, the role of K-wire transfixation in preventing proximalization is not clear yet, as multiple studies have shown no clinical benefit after ligament reconstruction and transfixation compared to trapeziectomy alone [19].
To the best of our knowledge, this is the first study to correlate proximalization of the first metacarpal to the manner of K-wire transfixation after RSIA. We were able to show that transfixation with two K-wires seems to be superior to transfixation with one K-wire when it comes to preventing proximalization of the first metacarpal (represented by higher TSR values) in the postoperative course. However, when analyzing 2K subgroups, we only found a statistical difference between group 2Kc and 1K, although there was a trend towards higher postoperative TSR values in group 2Ka and 2Kb compared to 1K.
This indicates an important role of transfixating the first metacarpal to two different structures, namely second metacarpal and carpus. This results in two different vectors of transfixation, thus preventing subsidence in either direction during the postoperative healing process by a “blocking” function of each K-wire.
One limitation of this study is its retrospective character, leading to only a small number of included cases in spite of the large number of RSIA performed at our institution. Some patients were lost to follow up and in other cases, no adequate radiographic examination was available. Furthermore, the technique of K-wire transfixation was heterogeneous, leading to several subgroups with exclusion of some subgroups due to the small number of cases. We want to emphasize that the presented data cannot give a direct impression of the clinical impairment of the patients [21], as this is solely a morphologic study. The examination of x-rays without a survey of clinical or subjective data can naturally not compare pre- and postoperative symptom scores, like the DASH score. However, we know from previous research, that loss of trapezial hight correlates inversely with clinical outcome [33], making it necessary to find ways to limit proximalization of the first metacarpal.
Additionally, it seems advisable to ensure a position of the first metacarpal as distal as possible to maintain physiological anatomical conditions from a biomechanical point of view. This can both prevent painful impingement between the first metacarpal base and the scaphoid and on the other side enables a physiological direction of pull and force development of the involved extrinsic and intrinsic thumb muscles. We conclude based on measurements of the radiographic morphology, that an anatomical reconstruction of the first metacarpal position should be valued highly to avoid potential disadvantages for the patient. Upon deciding to stabilize the first metacarpal base postoperatively, a preferably rigid manner of K-wire transfixation should be chosen to maintain a maximal distance between the first metacarpal base and the scaphoid in the long term. Thus, we propose to transfixate the first metacarpal to the second metacarpal as well as to the carpus after RSIA.
Funding
Open Access funding enabled and organized by Projekt DEAL. There is no funding source.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no potential conflict of interest.
Ethical approval
The study was granted approval by the institutional research ethics committee and is in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dahaghin S, Bierma-Zeinstra SM, Ginai AZ, Pols HA, Hazes JM, Koes BW. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study) Ann Rheum Dis. 2005;64(5):682–687. doi: 10.1136/ard.2004.023564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haara MM, Heliovaara M, Kroger H, Arokoski JP, Manninen P, Karkkainen A, Knekt P, Impivaara O, Aromaa A. Osteoarthritis in the carpometacarpal joint of the thumb. Prevalence and associations with disability and mortality. J Bone Joint Surg Am. 2004;86(7):1452–1457. doi: 10.2106/00004623-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Wilder FV, Barrett JP, Farina EJ. Joint-specific prevalence of osteoarthritis of the hand. Osteoarthritis Cartilage. 2006;14(9):953–957. doi: 10.1016/j.joca.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 4.Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004;32(3):447–457. doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- 5.Wilson DR, McWalter EJ, Johnston JD. The measurement of joint mechanics and their role in osteoarthritis genesis and progression. Rheum Dis Clin North Am. 2008;34(3):605–622. doi: 10.1016/j.rdc.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 6.Hunter DJ, Wilson DR. Imaging the role of biomechanics in osteoarthritis. Rheum Dis Clin North Am. 2009;35(3):465–483. doi: 10.1016/j.rdc.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 7.Hunter DJ, Wilson DR. Role of alignment and biomechanics in osteoarthritis and implications for imaging. Radiol Clin North Am. 2009;47(4):553–566. doi: 10.1016/j.rcl.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 8.Unglaub F, Langer MF, Hohendorff B, Jung M, Muller LP, Spies CK. Anatomy of the trapeziometacarpal joint in the context of arthroplasty. Orthopade. 2019;48(5):394–397. doi: 10.1007/s00132-019-03702-z. [DOI] [PubMed] [Google Scholar]
- 9.Clifton KB, Rodner C, Wolf JM. Detection of relaxin receptor in the dorsoradial ligament, synovium, and articular cartilage of the trapeziometacarpal joint. J Orthop Res. 2014;32(8):1061–1067. doi: 10.1002/jor.22640. [DOI] [PubMed] [Google Scholar]
- 10.Felson DT. Obesity and vocational and avocational overload of the joint as risk factors for osteoarthritis. J Rheumatol Suppl. 2004;70:2–5. [PubMed] [Google Scholar]
- 11.Spector TD, Cicuttini F, Baker J, Loughlin J, Hart D. Genetic influences on osteoarthritis in women: a twin study. BMJ. 1996;312(7036):940–943. doi: 10.1136/bmj.312.7036.940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eaton RG. Replacement of the trapezium for arthritis of the basal articulations: a new technique with stabilization by tenodesis. J Bone Joint Surg Am. 1979;61(1):76–82. doi: 10.2106/00004623-197961010-00014. [DOI] [PubMed] [Google Scholar]
- 13.Weilby A, Sondorf J. Results following removal of silicone trapezium metacarpal implants. J Hand Surg Am. 1978;3(2):154–156. doi: 10.1016/s0363-5023(78)80064-1. [DOI] [PubMed] [Google Scholar]
- 14.Epping W, Noack G. Surgical treatment of the saddle joint arthrosis. Handchir Mikrochir Plast Chir. 1983;15(3):168–176. [PubMed] [Google Scholar]
- 15.Burton RI. Basal joint arthritis. Fusion, implant, or soft tissue reconstruction? Orthop Clin North Am. 1986;17(3):493–503. doi: 10.1016/S0030-5898(20)32332-4. [DOI] [PubMed] [Google Scholar]
- 16.Elfar JC, Burton RI. Ligament reconstruction and tendon interposition for thumb basal arthritis. Hand Clin. 2013;29(1):15–25. doi: 10.1016/j.hcl.2012.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burton RI, Pellegrini VD., Jr Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg. 1986;11(3):324–332. doi: 10.1016/s0363-5023(86)80137-x. [DOI] [PubMed] [Google Scholar]
- 18.Poulter RJ, Davis TR. Management of hyperextension of the metacarpophalangeal joint in association with trapeziometacarpal joint osteoarthritis. J Hand Surg Eur. 2011;36(4):280–284. doi: 10.1177/1753193411400359. [DOI] [PubMed] [Google Scholar]
- 19.Salem H, Davis TR. Six year outcome excision of the trapezium for trapeziometacarpal joint osteoarthritis: is it improved by ligament reconstruction and temporary Kirschner wire insertion? J Hand Surg Eur. 2012;37(3):211–219. doi: 10.1177/1753193411414516. [DOI] [PubMed] [Google Scholar]
- 20.Davis TR, Pace A. Trapeziectomy for trapeziometacarpal joint osteoarthritis: is ligament reconstruction and temporary stabilisation of the pseudarthrosis with a Kirschner wire important? J Hand Surg Eur. 2009;34(3):312–321. doi: 10.1177/1753193408098483. [DOI] [PubMed] [Google Scholar]
- 21.Wittemann M, Demir E, Sauerbier M, Germann G (2002) The Epping resection-suspension arthroplasty procedure. A standard procedure in the operative treatment of trapeziometacarpal osteoarthrosis? Handchirurgie, Mikrochirurgie, plastische Chirurgie: Organ der Deutschsprachigen Arbeitsgemeinschaft fur Handchirurgie: Organ der Deutschsprachigen Arbeitsgemeinschaft fur Mikrochirurgie der Peripheren Nerven und Gefasse. 34 (1):49–58. 10.1055/s-2002-22108 [DOI] [PubMed]
- 22.Kadiyala RK, Gelberman RH, Kwon B. Radiographic assessment of the trapezial space before and after ligament reconstruction and tendon interposition arthroplasty. J Hand Surg Br. 1996;21(2):177–181. doi: 10.1016/s0266-7681(96)80093-3. [DOI] [PubMed] [Google Scholar]
- 23.Horch RE, Unglaub F (2011) Rhizarthrose In:Towfigh H, Hierner R, Langer M, Friedel R (eds) Handchirurgie. Springer, Berlin, pp 1401–1411. 10.1007/978-3-642-11758-9_51
- 24.Hohendorff B, Unglaub F, Spies CK, Wegmann K, Muller LP, Ries C. Surgical approaches to the hand. Oper Orthop Traumatol. 2019;31(5):372–383. doi: 10.1007/s00064-019-0622-8. [DOI] [PubMed] [Google Scholar]
- 25.Tomaino MM, Pellegrini VD, Jr, Burton RI. Arthroplasty of the basal joint of the thumb. Long-term follow-up after ligament reconstruction with tendon interposition. J Bone Joint Surg Am. 1995;77(3):346–355. doi: 10.2106/00004623-199503000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Eaton RG, Glickel SZ, Littler JW. Tendon interposition arthroplasty for degenerative arthritis of the trapeziometacarpal joint of the thumb. J Hand Surg. 1985;10(5):645–654. doi: 10.1016/s0363-5023(85)80201-x. [DOI] [PubMed] [Google Scholar]
- 27.Nylen S, Johnson A, Rosenquist AM. Trapeziectomy and ligament reconstruction for osteoarthrosis of the base of the thumb. A prospective study of 100 operations. J Hand Surg Br. 1993;18(5):616–619. doi: 10.1016/0266-7681(93)90017-a. [DOI] [PubMed] [Google Scholar]
- 28.Halim MHL, Horch RE, Bach AD. Importance of ST arthroplasty in the treatment of STT osteoarthritis and concomitant basal thumb osteoarthritis. Handchir Mikrochir Plast Chir. 2019;51(3):185–192. doi: 10.1055/a-0900-4130. [DOI] [PubMed] [Google Scholar]
- 29.Kirchberger MC, Schnabl SM, Bruckner T, Muller LP, Oppermann J, Klum M, Unglaub F, Hahn P, Spies CK. Functionality of middle-aged women after resection-interposition arthroplasty of the trapeziometacarpal joint in comparison to a healthy control group. Arch Orthop Trauma Surg. 2014;134(5):735–739. doi: 10.1007/s00402-014-1966-z. [DOI] [PubMed] [Google Scholar]
- 30.Spies CK, Langer M, Hahn P, Muller LP, Unglaub F. The Treatment of primary arthritis of the finger and thumb joint. Dtsch Arztebl Int. 2018;115(16):269–275. doi: 10.3238/arztebl.2018.0269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kvarnes L, Reikeras O. Osteoarthritis of the carpometacarpal joint of the thumb. An analysis of operative procedures. J Hand Surg Br. 1985;10(1):117–120. doi: 10.1016/s0266-7681(85)80037-1. [DOI] [PubMed] [Google Scholar]
- 32.Dell PC, Brushart TM, Smith RJ. Treatment of trapeziometacarpal arthritis: results of resection arthroplasty. J Hand Surg Am. 1978;3(3):243–249. doi: 10.1016/s0363-5023(78)80088-4. [DOI] [PubMed] [Google Scholar]
- 33.Trumble T, Rafijah G, Heaton D. Thumb carpometacarpal arthroplasty with ligament reconstruction and interposition costochondral arthroplasty. J Wrist Surg. 2013;2(3):220–227. doi: 10.1055/s-0033-1351375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lins RE, Gelberman RH, McKeown L, Katz JN, Kadiyala RK. Basal joint arthritis: trapeziectomy with ligament reconstruction and tendon interposition arthroplasty. J Hand Surg. 1996;21(2):202–209. doi: 10.1016/S0363-5023(96)80101-8. [DOI] [PubMed] [Google Scholar]
- 35.Martinez de Aragon JS, Moran SL, Rizzo M, Reggin KB, Beckenbaugh RD. Early outcomes of pyrolytic carbon hemiarthroplasty for the treatment of trapezial-metacarpal arthritis. J Hand Surg. 2009;34(2):205–212. doi: 10.1016/j.jhsa.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 36.Vitale MA, Hsu CC, Rizzo M, Moran SL. Pyrolytic carbon arthroplasty versus suspensionplasty for trapezial-metacarpal arthritis. J Wrist Surg. 2017;6(2):134–143. doi: 10.1055/s-0036-1593735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jung M, Unglaub F. Arthroplasty of the TMT1 joint-a critical view. Orthopade. 2019;48(5):398–401. doi: 10.1007/s00132-019-03718-5. [DOI] [PubMed] [Google Scholar]
- 38.Cootjans K, Dreessen P, Vandenberghe D, Verhoeven N. Salvage revision arthroplasty after failed TMC joint prosthesis. Acta Orthop Belg. 2019;85(3):325–329. [PubMed] [Google Scholar]
- 39.Lenoir H, Erbland A, Lumens D, Coulet B, Chammas M. Trapeziectomy and ligament reconstruction tendon interposition after failed trapeziometacarpal joint replacement. Hand Surg Rehabil. 2016;35(1):21–26. doi: 10.1016/j.hansur.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 40.Swanson AB. Reconstruction of the thumb basal joints including flexible implant resection arthroplasty (author's transl) Orthopade. 1980;9(2):134–149. [PubMed] [Google Scholar]
- 41.Lehmann O, Herren DB, Simmen BR (1998) Comparison of tendon suspension-interposition and silicon spacers in the treatment of degenerative osteoarthritis of the base of the thumb. Annales de chirurgie de la main et du membre superieur: organe officiel des societes de chirurgie de la main=Annals of hand and upper limb surgery 17(1):25–30. 10.1016/s0753-9053(98)80017-3 [DOI] [PubMed]
- 42.Minami A, Iwasaki N, Kutsumi K, Suenaga N, Yasuda K. A long-term follow-up of silicone-rubber interposition arthroplasty for osteoarthritis of the thumb carpometacarpal joint. Hand Surg. 2005;10(1):77–82. doi: 10.1142/S0218810405002607. [DOI] [PubMed] [Google Scholar]
- 43.Krukhaug Y, Lie SA, Havelin LI, Furnes O, Hove LM, Hallan G. The results of 479 thumb carpometacarpal joint replacements reported in the Norwegian Arthroplasty Register. J Hand Surg Eur. 2014;39(8):819–825. doi: 10.1177/1753193413513988. [DOI] [PubMed] [Google Scholar]
- 44.Cai A, Pingel I, Lorz D, Beier JP, Horch RE, Arkudas A. Force distribution of a cylindrical grip differs between dominant and nondominant hand in healthy subjects. Arch Orthop Trauma Surg. 2018;138(9):1323–1331. doi: 10.1007/s00402-018-2997-7. [DOI] [PubMed] [Google Scholar]



