Abstract
Non-melanoma skin cancers (NMSCs) are the most common malignancies diagnosed in Caucasian populations. Basal cell carcinoma (BCC) is the most frequent skin cancer, followed by squamous cell carcinoma (SCC). Unfortunately, most European cancer registries do not record individual types of NMSC. To evaluate the incidence of primary BCCs and SCCs regarding age, sex, tumour site and tumour subtype to determine trends in epidemiology of both cancers. Retrospective analysis of BCCs and SCCs diagnosed and treated across seven sites in Poland from 1999 to 2019. We recorded 13,913 NMSCs occurring in 10,083 patients. BCC represented 85.2% of all cases. SCC patients were older than BCC patients (77.1 ± 11.3 years vs. 70.1 ± 12.3 years, p < 0.01). The nodular subtype was the most common subtype of BCC, followed by the superficial and infiltrative subtypes. The superficial BCC subtype was more common on photoprotected areas (p < 0.01), whereas the nodular BCC subtype occurred on the face (p < 0.01). The high-risk SCC subtypes were more common on face compared to low-risk SCC subtypes (p < 0.01). BCC and SCC are common malignancies developing at various ages and anatomical sites. These data underline the need for better registration policies regarding NMSC in order to improve prevention and treatment strategies for these tumours.
Subject terms: Cancer epidemiology, Cancer prevention, Head and neck cancer, Cancer, Oncology, Cancer epidemiology
Introduction
Non-melanoma skin cancers (NMSCs) are the most common human malignancies, with steadily rising incidence. The term NMSC refers to all non-melanoma malignant neoplasms affecting the skin. The main types of NMSC, basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), account for about 99% of all NMSCs1. Other NMSCs include Merkel cell carcinoma, sebaceous carcinoma, apocrine adenocarcinoma and other rare tumours2,3. BCC is the predominant type, with a BCC to SCC ratio between 1:1 and 10:1 depending on the population, ethnic group and sex4–6. Although NMSC are 18–20 times more frequent than cutaneous melanoma, there is little epidemiological data for those tumour types7–9. Only a few studies have examined the separate incidence of BCCs and SCCs, because in most European countries different types of NMSC are not distinguished from each other in national cancer registry data. Any tumour diagnosis based on histopathology and site is coded according to the International Classification of Diseases 11th Revision (ICD-11). Cutaneous melanoma is coded as C43, therefore the data for this diagnosis is reliable. A non-homogeneous NMSC group receives a single code (C44) to cover all NMSCs, therefore separate data on BCCs, SCCs, and other malignancies of the skin is not available making separate diagnoses of NMSCs difficult to count and assess accurately.
We retrospectively collected, processed, and analysed data on the incidence of separate diagnoses within NMSC group across seven sites in Poland. The aim of the study was to analyse the incidence of primary BCCs and SCCs depending on the site of the lesion, sex and age of the patients to determine epidemiological trends and characteristics of both tumour types.
Patients and methods
We retrospectively searched histopathological databases for records between 1999 and 2019 in multiple tertiary oncology and dermatology centres in Poland, including Gdansk (north Poland), Gliwice (south Poland), Lodz (two sites, central Poland), Rzeszow (southeast Poland), Warsaw (central Poland), and Wroclaw (southwest Poland). All consecutive patients aged 18 years old and above (those centres do not treat children) with histopathologically confirmed BCC or SCC were included in the study. The database and methods were conducted similarly to our previous study10.
The National Comprehensive Cancer Network (NCCN) guidelines were followed to classify the tumour subtype. High-risk BCC subtypes included: infiltrative, micronodular, morpheaform, mixed with aggressive subtype (tumour consisting of more than one subtype, of which at least one is an aggressive subtype) and BCC with carcinosarcomatous differentiation. Low-risk BCC subtypes included: nodular, superficial, fibroepithelial, keratotic and mixed (nodular with superficial). High-risk SCC subtypes included: desmoplastic, acantholytic, carcinosarcomatous and adenosquamous. Low-risk SCC subtypes included: keratoacanthomatous and verrucous.
BCC with mixed histologic subtypes is defined as tumour that is composed of two or more growth patterns within the same lesion. For mixed cases the following rules for classification have been followed: when aggressive subtype predominated in the lesion, the tumour was defined with the most high-risk subtype that was mentioned; when non-aggressive subtype predominated aggressive subtype, the tumour was defined as mixed with aggressive subtype; when tumour consisted of two non-aggressive histologic subtypes it was defined as mixed (nodular with superficial). If there was a discordance between the initial biopsy specimen subtype and the wide excision, then the tumour subtype was classified based on wide excision.
The population studied was fairly homogenous in regards to ethnic group. Data included patients diagnosed in national health centres as well as in private hospitals. Patients’ age and sex, site of the cancer, and histopathological diagnosis were recorded. Recurrent tumours were identified and excluded by comparison with data from earlier diagnoses. Patients were divided into 5-year age intervals for further analysis. The data were analysed statistically by analysis of variance with post-hoc comparisons, the Student’s t-test, and χ2 test with Yates correction, if required. Statistical significance was observed for p values of less than 0.01.
We also extracted data regarding incidence rates of NMSC between 1999 and 2019 from the Polish National Health Fund database registries using C44.0–C44.9 of ICD-10 coding and compared them to our data10.
The Human Research Ethics Committee of the Medical University of Lodz, Poland approved the study (RNN/209/18/KE). All institutions the subjects’ information was sourced from obtained the informed consent. The data used encrypted identification of the subjects, thus written consent was not required from the patients. All procedures and methods were conducted in accordance Declaration of Helsinki10.
Compliance with ethics guidelines
Approval for this study was obtained from the Human Research Ethics Committee of the Medical University of Lodz, Poland (RNN/2019/18/KE). All methods and procedures were conducted in accordance with the relevant guidelines and regulations as well as with the updated Declaration of Helsinki.
Results
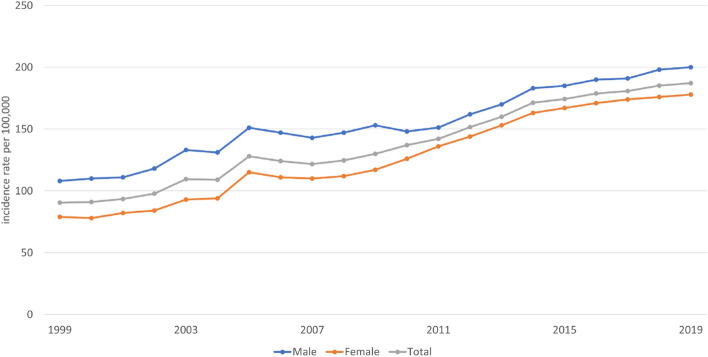
The data gathered from the Polish National Health Fund database showed an increasing trend of NMSC diagnoses between 1999 and 2019. The annual growth (5–7%) of incidence rates of C44 cases was observed between 2005 and 2014. The trend continued after 2014, although the growth rate slowed down with the annual increase rate not exceeding 2%. Figure 1 presents the incidence rates of cases classified as C44 per 100,000 person-years between 1999 and 2019 in relation to gender. The data gathered in our multicentre study confirmed that the incidence rates of BCCs and SCCs are growing.
Figure 1.
Incidence of cases diagnosed using ICD-10 code C44 between 1999 and 2019 according to the Polish National Health Fund per 100,000 person-years. ICD-10: International Classification of Diseases, 11th Revision.
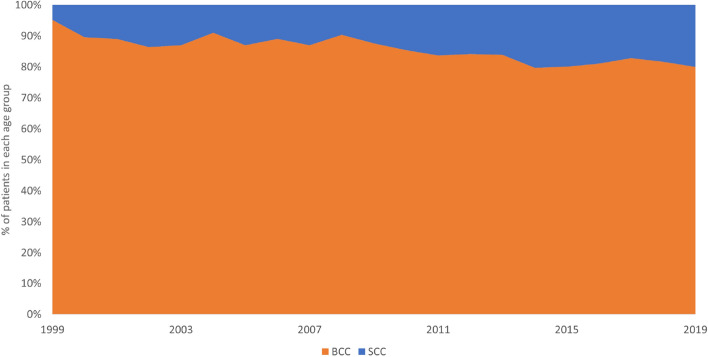
Over the 21-year study period, 10,083 patients were diagnosed with at least one excised and histologically confirmed BCC or SCC. Twenty-three percent of patients had more than one NMSC, resulting in a total of 13,913 NMSC cases (6899 men and 7014 women, ratio 0.98:1), including 11,848 BCCs and 2065 SCCs (BCC:SCC ratio 5.7:1; p < 0.01). Figure 2 presents annual BCC to SCC ratio. SCC comprised only 10% of all NMSC in 2000, but this figure was increasing gradually each year where SCC comprised 20% of all NMSC in 2019.
Figure 2.
Annual BCC to SCC ratio between 1999 and 2019.
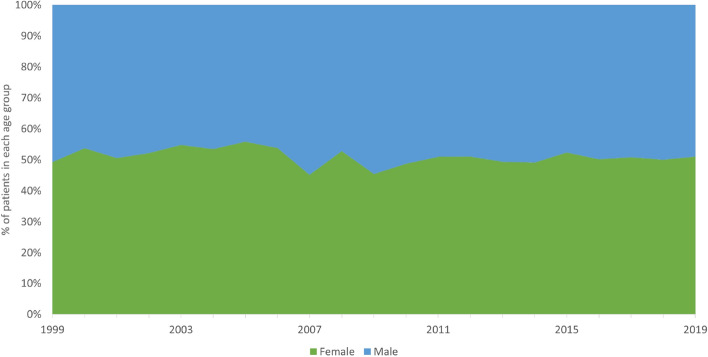
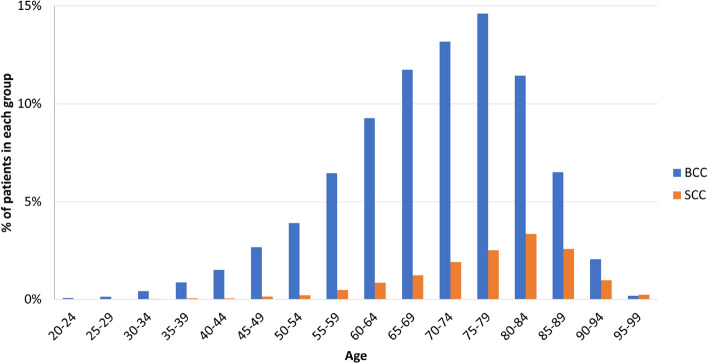
The mean age of patients with BCC was 70.1 ± 12.3 years (range 18–101 years), whereas of patients with SCC was 77.1 ± 11.3 years (range 19–102 years) (p < 0.01). Figure 3 presents male to female ratio for NMSCs which did not show any significant annual differences between genders over the analysed period.
Figure 3.
Male and female incidence rate for NMSC relation between 1999 and 2019.
There were 5881 men and 5967 women with BCC (ratio 0.99:1). The mean age of men was 70.9 ± 11.4 years and that of women was 71.4 ± 11.9 years (p = 0.28).
There were 1,018 men and 1,047 women with SCC (ratio, 0.97:1). The mean age of men was 75.9 ± 12.2 years and that of women was 77.2 ± 12.1 years (p < 0.01). Figure 4 presents the age-specific distributions for BCCs and SCCs.
Figure 4.
Age-specific incidence rates for NMSC (n = 13,913). SCC patients were significantly older than BCC patients (p < 0.01). NMSC non-melanoma skin cancer, SCC squamous cell carcinoma; BCC basal cell carcinoma.
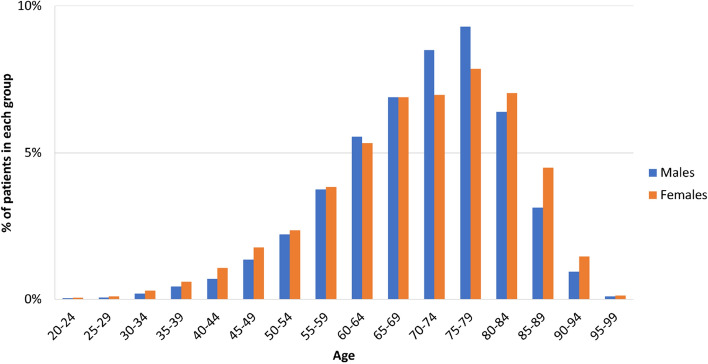
There was a predominance of women (p < 0.01) in the youngest group of NMSC patients (18–44 years). In patients 45–64 years, no significant difference in sex was observed (p = 0.96). In patients 65–79 years, a significant predominance of men was observed (p < 0.01), and in the oldest patients (80–102 years), women were significantly more prevalent (p < 0.01). Figure 5 presents the age-specific distributions of NMSCs in relation to gender.
Figure 5.
Age-specific incidence rates for NMSC in relation to sex; n = 13,913. In patients 18–44 years old, there was a significant predominance of women (p < 0.01). In patients 45–69 years old, there was no predominance in sex (p = 0.93). In patients 70–79 years old, there was a significant predominance of men (p < 0.01). In patients 80–102 years old, there was a significant predominance of women (p < 0.01).
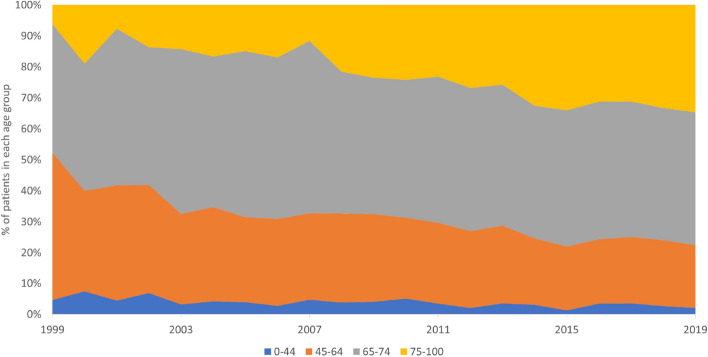
During the analysed period, the highest increase in incidence rates for NMSC was observed in the oldest group (over 75 years), while patients in age group between 65 and 74 years showed stable incidence rates. Figure 6 presents annual incidence rates in different age groups.
Figure 6.
Age-specific incidence rates for NMSC between 1999 and 2019.
A single histologically confirmed NMSC was observed in 7786 patients. In 2300 patients, multiple carcinomas were diagnosed. There were two, three, four, and more than four carcinomas in 1564, 389, 165, and 182 patients, respectively. There was no statistically significant relationship between sex and multiple lesions (p = 0.47).
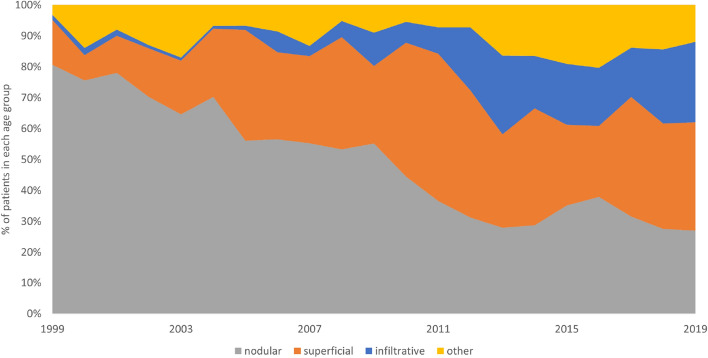
SCC subtype was registered in 976 cases including low-risk SCC in 814 cases (412 women, 402 men) and high-risk SCC in 162 cases (90 women, 72 men). Information regarding the subtype of BCC was registered in 5389 cases. Nodular (including the nodular and ulcerative subtype) BCC was the most frequent BCC subtype for both men and women (n = 2369, 44.0%; 1182 cases in men and 1187 cases in women). The other subtypes of BCC were superficial (n = 1641, 30.5%), infiltrative (n = 758, 14.1%), mixed superficial with nodular (n = 182, 3.4%) and mixed with aggressive subtype (n = 61, 1.1%), basosquamous (n = 181, 3.4%), adenoid (n = 25, 0.5%), pigmented (n = 23, 0.4%), micronodular (n = 14, 0.3%) and other (n = 135, 2.5%). Superficial BCCs were more common in women than in men (p < 0.01), whereas other BCC subtypes demonstrated no statistically significant relationship between sex and histopathological subtype (nodular BCC, p = 0.79; infiltrative BCC, p = 0.38; other BCC subtypes, p = 0.19) Table 1 presents the SCC and BCC subtypes according to two-tiered classification of BCCs (high and low risk subtypes) in relation to the patients’ gender and tumour’s site11,12. During the analysed period a significant increase in infiltrative subtype was observed (threefold increase between 2010 and 2019). Incidence of superficial BCC subtype increased by 1% annually, while nodular subtype incidence declined over the above period. Figure 7 presents distribution of BCC subtypes between 1999 and 2019.
Table 1.
BCC and SCC subtypes sites depending on the sex of the patients.
| Low-risk SCC | High-risk SCC | Low-risk BCC | High-risk BCC | |
|---|---|---|---|---|
| Men | ||||
| Face | 225 (61%)a | 47 (85%)a | 549 (57%)a | 350 (78%)a |
| Trunk | 46 (13%) | 0 (0%) | 263 (27%) | 37 (8%) |
| Upper limb | 32 (9%) | 2 (4%) | 62 (6%) | 13 (3%) |
| Lower limb | 41 (11%) | 0 (0%) | 44 (5%) | 4 (1%) |
| Scalp | 11 (3%) | 2 (4%) | 20 (2%) | 27 (6%) |
| Neck | 13 (4%) | 4 (7%) | 51 (5%) | 16 (4%) |
| n/d | 34 | 17 | 1059 | 85 |
| all | 402 | 72 | 2048 | 532 |
| Women | ||||
| Face | 275 (67%) | 82 (92%) | 549 (57%) | 364 (81%) |
| Trunk | 27 (7%) | 0 (0%) | 248 (26%) | 43 (10%) |
| Upper limb | 23 (6%) | 1 (1%) | 48 (5%) | 7 (2%) |
| Lower limb | 57 (14%) | 2 (2%) | 70 (7%) | 7 (2%) |
| Scalp | 2 (0%) | 1 (1%) | 25 (3%) | 18 (4%) |
| Neck | 12 (3%) | 3 (3%) | 55 (6%) | 12 (3%) |
| n/d | 4 | 1 | 1161 | 87 |
| all | 412 | 90 | 2166 | 548 |
Data are presented as n (%).
n/d not defined, BCC basal cell carcinoma, SCC squamous cell carcinoma.
aHigh-risk BCCs and SCCs were most common on the face (p < 0.01).
Figure 7.
Distribution of BCC subtypes between 1999 and 2019.
The mean age of the patients differed depending on various BCC subtypes. Patients with superficial BCC were slightly younger (67.7 ± 11.5 years), than patients with other subtypes (69.3 ± 12.7 years), and the difference was statistically significant (p < 0.01). Moreover, women with superficial BCC were younger than men with the same BCC subtype (67.0 ± 13.7 years vs. 68.6 ± 12.2 years; p < 0.01). On the other hand, patients with basosquamous BCC (72.2 ± 11.3 years), nodular BCC (69.4 ± 12.7 years), infiltrative BCC (71.1 ± 12.3 years) were on average older than patients with other subtypes.
Anatomical distribution of NMSCs was collected in 10,587 cases (8962 BCC cases and 1625 SCC cases). In both sexes, BCC and SCC lesions were located mainly on the face. Overall, BCC occurrence on the face was statistically more frequent when compared to SCC (p < 0.01). The second most frequent sites were the trunk for BCC (14.8%) and the lower limbs for SCC (11.8%). Table 2 presents the clinical characteristics of patients with BCC and SCC.
Table 2.
Clinical characteristics of patients with BCC and SCC.
| BCC | SCC | |
|---|---|---|
| Total number of lesions | 11,848 | 2065 |
| Mean age, years, total | 70.1a | 77.1a |
| Mean age, years, male | 70.1 | 75.9b |
| Mean age, years, female | 70.1 | 78.2b |
| Sex ratio (F/M) | 1.01 | 1.03 |
| Location | ||
| Face | 6500 (73%) | 1036 (64%) |
| Trunk | 1372 (15%) | 160 (10%) |
| Upper limbs | 316 (4%) | 128 (8%) |
| Lower limbs | 303 (3%)c | 192 (12%)c |
| Scalp | 186 (2%) | 44 (3%) |
| Neck | 285 (3%) | 65 (4%) |
BCC basal cell carcinoma, SCC squamous cell carcinoma, F/M female to male ratio.
aThe mean age of patients differed significantly between SCC and BCC patients (p < 0.01).
bThe mean age of SCC patients differed significantly between men and women (p < 0.01).
cSCC was significantly more common on the lower limbs than BCC (p < 0.01).
BCCs on the face were located most often on the nose (29.7%). Other areas on the face included the eye (16.2%), cheek (15.8%), temple (12.0%), forehead (11.4%), earlobe (9.1%), lips (3.2%), chin (1.4%), nasolabial folds (0.62%), and the jaw-line (0.62%).
While nodular and infiltrative BCC was located mainly on the face, superficial BCCs were most frequent on the trunk (p < 0.01). Lesions on the trunk were significantly more common in younger patients (67.3 ± 13.5 years), whereas lesions on the face occurred mainly in older patients (72.1 ± 11.9 years; p < 0.01). Women developed lesions on the trunk and upper limbs at a younger age than men (p < 0.01), whereas lesions on the face were more common in younger men than women (p < 0.01).
Discussion
NMSCs are the most common skin malignancies with rising incidence all over the world, mainly because of increased exposure to UV radiation and ozone depletion with sun-seeking behaviours and higher cumulative UV dose, connected with increased longevity, as contributing factors13,14. As already mentioned, the exact incidence of BCCs and SCCs is difficult to establish. Majority of cancer registries record these cancers under the term NMSC, instead of recording separate diagnoses. Previously published data indicated that BCCs comprise about 80% of all NMSCs and this incidence continues to rise13,14, which is consistent with the results of our multicentre study.
Although skin cancers may develop in children and young adults15, it is essentially a disease of the older population16,17. The European population is an aging one and as a consequence, a notable increase in the occurrence of all cancers is observed18,19. About 80% of cancers are diagnosed in patients older than 55 years, although the increase is observed in all age groups, regardless of sex. We observed an increasing trend for NMSC incidence in our study, which is consistent with data gathered from the Polish National Health Fund database.
Most patients with BCCs (95%) are between 40 and 79 years of age20,21. Our study also confirmed that SCC develops more frequently in older patients. Since 2012, the increase in the incidence of both BCC and SCC was observed among the older population. Interestingly, our findings showed that while the SCC incidence raised significantly also in younger population, the growth was significantly higher in the elderly, which is in line with the results of previous studies22,23.
The rising trend in the incidence of BCCs and SCCs may be due to numerous factors. An improved consciousness of cutaneous malignancies in the overall population due to skin cancer prevention campaigns may have led to more skin diagnoses and examinations of previously undiagnosed NMSC. Moreover, all physicians are more aware of skin cancers, which may also lead to an increased likelihood of skin cancers, including NMSC, being diagnosed24,25. Moreover, since 1990 air travel has become widely available and affordable to the general population in Poland, allowing people to travel to sunny destinations, where the skin is exposed to higher than usual and acute doses of UV radiation. Another factor in raised incidence of NMSC has been a substantial increase in sunbed use, particularly in younger population, over the past two decades. The sunbed use reached its peak of popularity between the 1990s and 2000s, but regulatory changes including a minimum age restriction of 18 years have been introduced only recently26.
Despite the overall increase in the incidence of both BCC and SCC between 1999 and 2019, it is noteworthy that BCC rates for people 40 years old and younger showed no substantial increase in our study. Studies conducted almost 20 years ago showed raised incidence of NMSC in women younger than 4027,28. Currently, these women are much older than 40, and we could have expected an increase in the incidence of NMSCs in this group of patients. Moreover, women who were 40–50 years of age in 2018 were those who, in the 1990s and 2000s, had used sunbeds extensively. Considering that the main factor of the lifetime potential for developing skin cancer is the sun exposure in childhood and adolescence29, although adult sun exposure also plays a role30–33, it could be hypothesised that in the following decades the frequency of BCCs in patients younger than 40 may stabilise or even decrease, providing proper introduction of skin cancer prevention programs reducing childhood and teenage sun exposure.
The incidence of BCCs rose more sharply in women than in men and in patients younger than 50 and older than 80. BCCs in men were most often reported in patients between 50 and 80 years old. Data reported by Eurostat in 2017 showed that women in the European Union live on average 5 years and 3 months longer than men34. Most studies indicate a higher risk for NMSC development in the elderly, which could explain the greater proportion of cancer in women in the older age group.
Older studies found that more men than women develop skin cancer35,36. This is probably due to the fact, that man used to receive more exposure to sunlight during outdoors work and sport activities. However, there have been recent changes in attitudes in recreational sun exposure and many people, regardless of gender, receive a considerable dose of UVR from a very early age. This has already led to a reversal of the sex ratio between patients with BCC as fewer young men than young women develop skin cancer. BCC located on the trunk is also more common in young people, especially women37.
In our study, most tumours were located on the face, followed by the trunk, lower and upper extremities, neck and scalp. The site distribution in described population is consistent with those previously reported38. In accordance with previous studies, BCCs were predominantly located in the chronically UV-exposed regions39.
In our study, men were not more susceptible than women to develop either BCC or SCC apart from the ear site as 16% of the facial BCCs occurring on the ear were found in men, whereas only 5% in women. It is more common for women to have hair covering the ears, and therefore this anatomic site is more protected from UV. More than 60% of all diagnosed subtypes of BCC on the ear were of aggressive subtype, which is in concordance with data gathered by Jarell et al.40. This information could help physicians to ensure that the suspected lesions on the ear are promptly biopsied and treated.
We revealed that nodular subtype is the most common subtype of BCC, but in our study, it accounted for only 44% of all BCC cases, not 60–80% indicated by other studies38,39. Recent data indicates that BCC is not homogenous and that various histological types present different clinical behaviour and could have a different background. It was also shown that certain histological subtypes of BCC develop more often in specific anatomical sites. In our study superficial BCC occurred predominantly on the trunk in both sexes, especially in younger patients. These observation supports the hypothesis of intermittent sun-exposure for development of superficial BCC, as the exposures to acute, higher UV doses are more likely to develop during youth, especially for women, and decrease as people age40,41.
In contrast, nodular BCC most frequently occurs on the face37,39. Our results support previous hypothesis that chronic cumulative sun exposure is more related to the nodular type of BCC (similarly to SCC)42–45. We also revealed that SCC, particularly on the face, was more frequently diagnosed in older patients. The median age of SCC patients was higher than that of BCC patients. Interestingly, SCC was presented more commonly on the lower limbs compare to BCC.
The incidence of high-risk BCC, including the infiltrative, micronodular, and morpheaform subtypes, was higher in our study than in previously reported European and Australian data42–45. Moreover, the most frequent location for infiltrative lesions was on the face, where surgical removal is more difficult, and the risk for incomplete excision is higher45,46.
A significant increase in infiltrative subtype was observed in all sites (threefold increase between 2010 and 2019). The underlying cause is not clear. However, recently improved biopsy techniques could improve the diagnosis of high-risk subtypes. Aggressive subtypes are infiltrative and often grow in the deep portion of the tumour. Hence, small biopsy specimens centred topographically may miss deeper infiltrative component. Moreover, the environmental changes related to the ultraviolet light exposure, ozone depletion in various parts of the world and genetic predisposition could be also etiological factors for increase in the incidence of infiltrative BCC21. However, this topic requires further research.
Our study showed that BCC with mixed histologic subtypes was observed in 4.5%. Other studies have indicated incidence of mixed subtypes between 11 and 39%47–50. The significantly lower number of mixed subtypes could be caused by the methodology where mixed cases have been classified as most high-risk subtype that was mentioned. BCCs showing mixed subtypes with a predominating aggressive pattern were registered not as a mixed subtype but as an aggressive subtype.
In most cases only the first histopathologically confirmed NMSC per patient is registered17, but as our results show, multiple lesions are relatively common. In our study multiple lesions were observed in 23% of patients, and 7% of patients had three or more lesions. Other studies revealed that around 30% of patients will develop subsequent skin cancers within 5 years of the first NMSC diagnosis17. In a 2002 survey 25% of people with diagnosed NMSC had at least two skin cancers treated in a 12-month period51. In our study, multiple primary NMSCs were common, and almost 9% of patients developed a second NMSC within 2 years. This is consistent with the results of previous studies51,52.
Conclusions
We present rare epidemiological data of different types of NMSC diagnosed and treated in central Europe in form of a large series of surgically treated BCCs and SCCs over a period of 12 years. The most frequent site of the lesions was face; however, we observed an increasing trend in the incidence of truncal tumours in younger patients. The distribution of histopathological subtypes confirmed the predominance of nodular BCCs, followed by superficial and infiltrative BCCs.
Looking at the worldwide epidemiological trends of NMSC, it is obvious that there is an urgent need to control the increasing incidence of NMSC and subsequent socioeconomic burden. Studying and understanding current epidemiological trends of NMSC is crucial to achieve an early and adequate control of those common skin cancers. We need to respond more actively to this “NMSC epidemic” to stabilise and ultimately decrease BCC and SCC rates in the future. Effective primary preventative skin cancer strategies need to be developed to avoid future impact on the Health Services.
Abbreviations
- BCC
Basal cell carcinoma
- BSC
Basosquamous cell carcinoma
- NMSC
Non-melanoma skin cancer
- SCC
Squamous cell carcinoma
Author contributions
M.C. planned the study design and the sample cohort. M.C., G.K.W., D.L., B.L., A.R., Martyna Sławińska, M.P., K.S., R.J.N., A.H., J.M., D.N., M.B.M., Z.M., J.P., R.B., A.Z., Michał Sobjanek, Monika Słowińska, K.W., A.B. and W.N. gathered the subjects’ data M.C. prepared the figures. M.C. and K.C analyzed the data and wrote the manuscript. M.C. prepared the tables M.C., J.N. and A.L. reviewed the data analysis and interpretations. A.R., W.O. and Małgorzata Skibińska revised the manuscript. M.U., A.W., J.N. and A.L. supervised the project.
Funding
The study was funded by Medical University of Lodz (Project No. 503/5‑064‑01/503‑1) and The National Centre of Science (Grant No. 2017/27/B/NZ5/02011). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data availability
The data that support the findings of this study is available from the corresponding author upon request.
Competing interests
The authors declare no competing interests.
Footnotes
The original online version of this Article was revised: The original version of this Article contained errors in the Affiliations. Affiliation 2 was incorrectly given as ‘Department of Bone Marrow Transplantation and Hematology-Oncology, The Maria Skłodowska-Curie Memorial Cancer Centre and Institute of Oncology, Branch in Gliwice, Gliwice, Poland’. The correct affiliation is listed as ‘Department of Bone Marrow Transplantation and Hematology-Oncology, Pathology, Maria Sklodowska-Curie National Research Institute of Oncology, Gliwice, Poland’. Additionally, Affiliation 3 was incorrectly given as ‘Department of Tumor Pathology, The Maria Skłodowska-Curie Memorial Cancer Centre and Institute of Oncology, Branch in Gliwice, Gliwice, Poland’. The correct affiliation is listed as ‘University of Technology, Faculty of Medicine, Rolna 43, 40-555, Katowice, Poland’.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
7/28/2021
A Correction to this paper has been published: 10.1038/s41598-021-94435-7
References
- 1.Katalinic A, Kunze U, Schäfer T. Epidemiology of cutaneous melanoma and non-melanoma skin cancer in Schleswig–Holstein, Germany: incidence, clinical subtypes, tumour stages and localization (epidemiology of skin cancer) Br. J. Dermatol. 2003;149:1200–1206. doi: 10.1111/j.1365-2133.2003.05554.x. [DOI] [PubMed] [Google Scholar]
- 2.Losquadro W. Anatomy of the skin and the pathogenesis of nonmelanoma skin cancer. Facial Plast. Surg. Clin. N. Am. 2017;25:283–289. doi: 10.1016/j.fsc.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Wollina U. Carcinosarcoma of skin (Sarcomatoid carcinoma). A rare non-melanoma skin cancer (case review) Georgian Med. News. 2017;263:7. [PubMed] [Google Scholar]
- 4.Hannuksela-Svahn A, Pukkala E, Karvonen J. Basal cell skin carcinoma and other nonmelanoma skin cancers in Finland from 1956 through 1995. Arch. Dermatol. 1999;135:781–786. doi: 10.1001/archderm.135.7.781. [DOI] [PubMed] [Google Scholar]
- 5.Harris RB, Griffith K, Moon TE. Trends in the incidence of nonmelanoma skin cancer in southeastern Arizona, 1985–1986. J. Am. Acad. Dermatol. 2001;45:528–536. doi: 10.1067/mjd.2001.114742. [DOI] [PubMed] [Google Scholar]
- 6.Koh D, Wang H, Lee J, Chia KS, Lee HP, Goh CL. Basal cell carcinoma, squamous cell carcinoma, and melanoma of the skin: analysis of the Singapore Cancer Registry data 1968–97. Br. J. Dermatol. 2003;148:1161–1166. doi: 10.1046/j.1365-2133.2003.05223.x. [DOI] [PubMed] [Google Scholar]
- 7.Eide MJ, Krajenta R, Johnson D, et al. Identification of patients with nonmelanoma skin cancer using health maintenance organization claims data. Am. J. Epidemiol. 2010;171:123–128. doi: 10.1093/aje/kwp352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malone JP, Fedok FG, Belchis DA, Maloney ME. Basal cell carcinoma metastatic to the parotid: report of a new case and review of the literature. Ear Nose Throat J. 2000;79(511–515):518–519. [PubMed] [Google Scholar]
- 9.Cherpelis BS, Marcusen C, Lang PG. Prognostic factors for metastasis in squamous cell carcinoma of the skin. Dermatol. Surg. 2002;28:268–273. doi: 10.1046/j.1524-4725.2002.01169.x. [DOI] [PubMed] [Google Scholar]
- 10.Ciążyńska M, Sławińska M, Kamińska-Winciorek G, et al. Clinical and epidemiological analysis of basosquamous carcinoma: results of the multicenter study. Sci. Rep. 2020;10(1):18475. doi: 10.1038/s41598-020-72732-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nedved D, Tonkovic-Capin V, Hunt E, et al. Diagnostic concordance rates in the subtyping of basal cell carcinoma by different dermatopathologists. J. Cutan. Pathol. 2014;41(1):9–13. doi: 10.1111/cup.12256. [DOI] [PubMed] [Google Scholar]
- 12.McKenzie CA, Chen AC, Choy B, Fernández-Peñas P, Damian DL, Scolyer RA. Classification of high risk basal cell carcinoma subtypes: experience of the ONTRAC study with proposed definitions and guidelines for pathological reporting. Pathology. 2016;48(5):395–397. doi: 10.1016/j.pathol.2016.05.005. [DOI] [PubMed] [Google Scholar]
- 13.Murphy M, Mabruk M, Lenane P, et al. Comparison of the expression of p53, p21, Bax and the induction of apoptosis between patients with basal cell carcinoma and normal controls in response to ultraviolet irradiation. J. Clin. Pathol. 2002;55:829–833. doi: 10.1136/jcp.55.11.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kauvar AN, Cronin T, Roenigk R, et al. Consensus for nonmelanoma skin cancer treatment: basal cell carcinoma, including a cost analysis of treatment methods. Am. Soc. Dermatol. Surg. 2015;22:1–22. doi: 10.1097/DSS.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 15.de Vries E, Steliarova-Foucher E, Spatz A, et al. Skin cancer incidence and survival in European children and adolescents (1978–1997). Report from the automated childhood cancer information system project. Eur. J. Cancer. 2006;42:2170–2182. doi: 10.1016/j.ejca.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 16.Karagas MR, Greenberg ER, Spencer SK, et al. Increase in incidence rates of basal cell and squamous cell skin cancer in New Hampshire, USA. New Hampshire Skin Cancer Study Group. Int. J. Cancer. 1999;81:555–559. doi: 10.1002/(SICI)1097-0215(19990517)81:4<555::AID-IJC9>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 17.Flohil SC, de Vries E, Neumann HAM, et al. Incidence, prevalence, and future trends of primary basal cell carcinoma in the Netherlands. Acta Dermatol. Venerol. 2011;91:24–30. doi: 10.2340/00015555-1009. [DOI] [PubMed] [Google Scholar]
- 18.Krajowy Rejestr Nowotworów: www.onkologia.org.pl, Access: September 2019.
- 19.Didkowska I, Wojciechowska U, Zatoński W. Nowotwory złośliwe w Polsce w 2011roku; Publikacja wydana w ramach zadania „Rejestracja nowotworów złośliwych” Narodowego Programu Zwalczania Chorób Nowotworowych, Warszawa (2013)
- 20.Lesiak A, Slowik-Rylska M, Rogowski-Tylman M, et al. Risk factors in Central Poland for the development of superficial and nodular basal cell carcinomas. Arch. Med. Sci. 2010;6:270–275. doi: 10.5114/aoms.2010.13907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ciazynska M, Nartbutt J, Wozniacka A, Lesiak A. Trends in basal cell carcinoma incidence rates: a 16-year retrospective study of a population in central Poland. Adv. Dermatol. Allergol. 2018;35:47–52. doi: 10.5114/ada.2018.73164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Purdue MP, Freeman LE, Anderson WF, et al. Recent trends in incidence of cutaneous melanoma among US Caucasian young adults. J. Investig. Dermatol. 2008;128:2905–2908. doi: 10.1038/jid.2008.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jemal A, Saraiya M, Patel P, et al. Recent trends in cutaneous melanoma incidence and death rates in the United States, 1992–2006. J. Am. Acad. Dermatol. 2011;65:S17–25. doi: 10.1016/j.jaad.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 24.Valery PC, Neale R, Williams G, et al. The effect of skin examination surveys on the incidence of basal cell carcinoma in a Queensland community sample: a 10-year longitudinal study. J. Investig. Dermatol. Symp. Proc. 2004;9:148–151. doi: 10.1046/j.1087-0024.2003.09114.x. [DOI] [PubMed] [Google Scholar]
- 25.Levine JA, Sorace M, Spencer J, et al. The indoor UV tanning industry: a review of skin cancer risk, health benefit claims, and regulation. J. Am. Acad. Dermatol. 2005;53:1038–1044. doi: 10.1016/j.jaad.2005.07.066. [DOI] [PubMed] [Google Scholar]
- 26.Departament Nadzoru Rynku, UOKiK, Raport kontroli z urzadzen opalajacych UOKiK Warszawa, December 2010
- 27.Christenson LJ, Borrowman TA, Vachon CM, et al. Incidence of basal cell and squamous cell carcinomas in a population younger than 40 years. JAMA. 2005;294:681–690. doi: 10.1001/jama.294.6.681. [DOI] [PubMed] [Google Scholar]
- 28.Bivens MM, Bhosle M, Balkrishnan R, et al. Nonmelanoma skin cancer: is the incidence really increasing among patients younger than 40? A reexamination using 25 years of U.S. outpatient data. Dermatol. Surg. 2006;32:1473–1479. doi: 10.1111/j.1524-4725.2006.32358.x. [DOI] [PubMed] [Google Scholar]
- 29.Armstrong BK. How sun exposure causes skin cancer. In: Hill DJ, Elwood JM, English DR, editors. Prevention of Skin Cancer. Dordrecht: Kluwer; 2004. pp. 89–116. [Google Scholar]
- 30.Rosso S, Zanetti R, Pippione M, Sancho-Garnier H. Parallel risk assessment of melanoma and basal cell carcinoma: skin characteristics and sun exposure. Melanoma Res. 1998;8:573–583. doi: 10.1097/00008390-199812000-00013. [DOI] [PubMed] [Google Scholar]
- 31.Staples MP, Elwood M, Burton RC, Williams JL, Marks R, Giles GG. Non-melanoma skin cancer in Australia: the 2002 national survey and trends since 1985. Med. J. Aust. 2006;184(1):6–10. doi: 10.5694/j.1326-5377.2006.tb00086.x. [DOI] [PubMed] [Google Scholar]
- 32.Koh D, Wang H, Lee J, et al. Basal cell carcinoma, squamous cell carcinoma and melanoma of the skin: analysis of the Singapore Cancer Registry data 1968–97. Br. J. Dermatol. 2003;148:1161–1166. doi: 10.1046/j.1365-2133.2003.05223.x. [DOI] [PubMed] [Google Scholar]
- 33.Harris RB, Griffith K, Moon TE. Trends in the incidence of nonmelanoma skin cancers in southeastern Arizona, 1985–1996. J. Am. Acad. Dermatol. 2001;45:528–536. doi: 10.1067/mjd.2001.114742. [DOI] [PubMed] [Google Scholar]
- 34.Life expectancy at birth in the EU: men vs. women (https://ec.europa.eu/eurostat/) Accessed September, 2019.
- 35.Marks R, Jolley D, Dorevitch A, Selwood T. The incidence of non-melanocytic skin cancers in an Australian population: results of a five-year prospective study. Med. J. Aust. 1989;150:475–478. doi: 10.5694/j.1326-5377.1989.tb136588.x. [DOI] [PubMed] [Google Scholar]
- 36.MC Donald E, Epidemiology of skin cancer, 1975. In: E. McDonald (ed.), Neoplasms of the skin and malignant melanoma, 1975. 27–42.
- 37.Czarnecki D, Meehan C, O’Brien T, Leahy S, Nash C. The changing face of skin cancer in Australia. Int. J. Dermatol. 1991;30:715–717. doi: 10.1111/j.1365-4362.1991.tb02617.x. [DOI] [PubMed] [Google Scholar]
- 38.Ferreira FR, Pevide Bda C, Rodriques RF, et al. Differences in age and topographic distribution of the different histological subtypes of basal cell carcinoma, Taubaté (SP), Brazil. An Bras. Dermatol. 2013;88:726–730. doi: 10.1590/abd1806-4841.20132145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scrivener Y, Grosshans E, Cribier B. Variations of basal cell carcinomas according to gender, age, location and histopathological subtype. Br. J. Dermatol. 2002;147:41–47. doi: 10.1046/j.1365-2133.2002.04804.x. [DOI] [PubMed] [Google Scholar]
- 40.Jarell AD, Mully TW. Basal cell carcinoma on the ear is more likely to be of an aggressive phenotype in both men and women. J. Am. Acad. Dermatol. 2012;66(5):780–784. doi: 10.1016/j.jaad.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 41.McCormack CJ, Kelly JW, Dorevith AP. Differences in age and body site distribution of histological subtypes of basal cell carcinoma. A possible indicator of different causes. Arch. Dermatol. 1997;133:593–596. doi: 10.1001/archderm.1997.03890410049006. [DOI] [PubMed] [Google Scholar]
- 42.Buettner PG, Raasch BA. Incidence rates of skin cancer in Townsville. Australia. Int. J. Cancer. 1998;78:587–593. doi: 10.1002/(SICI)1097-0215(19981123)78:5<587::AID-IJC10>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 43.Marks R, Staples M, Giles GG. Trends in nonmelanocytic skin cancer treated in Australia: the second national survey. Int. J. Cancer. 1993;53:585–590. doi: 10.1002/ijc.2910530410. [DOI] [PubMed] [Google Scholar]
- 44.Bichakjian C, Olencki T, Aasi S, Alam M, Andersen J, Blitzblau R, et al. Basal Cell Carcinoma, NCCN Clinical Practice Guidelines in Oncology www.nccn.org (2018) [DOI] [PMC free article] [PubMed]
- 45.Raasch BA, Buettner PG, Garbe C. Basal cell carcinoma: histological classification and body-site distribution, epidemiology and health services research. Br. J. Dermatol. 2006;155:401–407. doi: 10.1111/j.1365-2133.2006.07234.x. [DOI] [PubMed] [Google Scholar]
- 46.Milroy CJ, Horlock N, Wilson GD, Sanders R. Aggressive basal cell carcinoma in young patients: Fact or fiction? Br. J. Plast. Surg. 2000;53:393–396. doi: 10.1054/bjps.1999.3267. [DOI] [PubMed] [Google Scholar]
- 47.Haws AL, Rojano R, Tahan SR, Phung TL. Accuracy of biopsy sampling for subtyping basal cell carcinoma. J. Am. Acad. Dermatol. 2012;66(1):106–111. doi: 10.1016/j.jaad.2011.02.042. [DOI] [PubMed] [Google Scholar]
- 48.Sexton M, Jones DB, Maloney ME. Histologic pattern analysis of basal cell carcinoma: study of a series of 1039 consecutive neoplasms. J. Am. Acad. Dermatol. 1990;23:1118–1126. doi: 10.1016/0190-9622(90)70344-H. [DOI] [PubMed] [Google Scholar]
- 49.Swetter SM, Yaghmai D, Egbert BM. Infiltrative basal cell carcinoma occurring in sites of biopsy-proven nodular basal cell carcinoma. J. Cutan. Pathol. 1998;25:420–425. doi: 10.1111/j.1600-0560.1998.tb01768.x. [DOI] [PubMed] [Google Scholar]
- 50.Cohen PR, Schulze KE, Nelson BR. Basal cell carcinoma with mixed histology: a possible pathogenesis for recurrent skin cancer. Dermatol. Surg. 2006;32(4):542–551. doi: 10.1111/j.1524-4725.2006.32110.x. [DOI] [PubMed] [Google Scholar]
- 51.Raasch BA, Buettner PG. Multiple nonmelanoma skin cancer in an exposed Australian population. Int. J. Dermatol. 2002;41:652–658. doi: 10.1046/j.1365-4362.2002.01573.x. [DOI] [PubMed] [Google Scholar]
- 52.Schinstine M, Goldman GD. Risk of synchronous and metachronous second nonmelanoma skin cancer when referred for Mohs micrographic surgery. J. Am. Acad. Dermatol. 2001;44:497–499. doi: 10.1067/mjd.2001.110646. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study is available from the corresponding author upon request.