Abstract
There is limited research on the short-term effects of ACEs on Black children and youth. Black children and youth are disproportionately exposed to abuse, neglect, and other victimizations (Drake et al. 2009; Wade et al. Journal of Family Issues, 17(3), 283–316, 2014). Investigating ACEs will provide a broader understanding of childhood trauma on developmental processes. The current study investigates how ACES impacts psychological distress, substance use, and delinquency among Black children and youth. Hypotheses were tested using a subsample of longitudinal data from 265 participants who were recruited from six school districts in Southeast Michigan. ACEs at T1 significantly predicted depressive symptoms at T2 (β = .19, p < .05), which in turn predicted substance use (β = .20, p < .05), and delinquency (β = .19, p < .05). Psychological distress also mediated the associations between ACEs and substance use, and delinquency. To engage youth in prevention/interventions and practice, it is important to understand the contexts in which they develop i.e. having knowledge on the specific type of victimization instances that Black youth may experience more than their peers as well as the social factors. Therefore, taking a trauma-informed approach that will acknowledge the adverse childhood experiences that youth went through and to understand how these experiences shape their development through adolescence may be efficacious.
Keywords: ACEs, Black, Youth, Distress, Substance use, Delinquency
Introduction
Childhood experiences have long been regarded as having a significant impact on developmental trajectory (Anda et al. 2006; Dube et al. 2003: Fox and Rutter 2010; Rutter 1996). Both positive and negative impacts of childhood experiences are well documented in the literature (Dube et al. 2003; Hardt and Rutter 2004) as well as the role nature and nurture play in regard to developmental outcomes. This developmental lens emerged early but has more recently come to the forefront as we attempt to better understand how experience, nested in environment, plays out relative to disparities in physical and mental health, learning, and behavior (Fox et al., 2010; Sameroff 2010; Shonkoff 2010; Shonkoff et al. 2012). The Adverse Childhood Experiences (ACEs) study (Felitti et al. 1998) brought renewed attention to the issue of exposure to traumatic events in childhood (ACEs). Results of the ACEs study explicate that experiencing four or more categories of ACEs predict higher rates of chronic diseases compared to those who have not experienced ACEs. Similar findings are reported between ACEs and sexual risk behaviors, drug abuse, and depression (Burke et al. 2011). These studies elucidate that ACEs are cumulative and as adolescent report more adverse childhood experience, they report more long-term negative health outcomes across multiple populations and contexts (Logan-Greene et al. 2016).
However, there is limited research on the short-term effects of ACEs on children and youth, specifically Black children and youth. Specific to this discussion is that Black children and youth (ages 7–18) are disproportionately exposed to abuse, neglect, and other victimizations (Drake et al. 2009; Wade et al. 2014). This disproportionate exposure places Black children and youth at elevated risk for negative health outcomes. Investigating the ACEs among Black children and youth is necessary to provide a broader understanding of childhood trauma on development.
Black children and youth are the most vulnerable to victimization compared to other racial/ethnic groups (U.S. Department of Health and Human Services 2016). Victimization has been broadly defined as harm caused by another human being in violation of social norms, including but not limited to abuse, neglect, and exposure to violence, sex crimes, or bullying (Finkelhor 2011). The numbers are compelling. Black children and youth were victimized 82% more than their White counterparts and 74% greater than Hispanic children and youth (U.S. Department of Health and Human Services 2016). These statistics support this study whose aim to identify that ACEs among Black children and youth is related to increased risk of experiencing subsequent and co-occurring victimization (i.e. neglect, medical neglect, and psychological abuse) (Wade et al. 2014).
Social Learning Theory
Social Learning Theory plays an integral role in the connection between experiencing ACEs and the negative behaviors associated with it. Social Learning Theory explains that children often begin to mirror actions or behaviors they observe in their peers or social circle (Fox et al. 2015). This theory was demonstrated in a study which tested the role of ACEs and other social factors among juvenile serious, violent, and chronic offenders and showed that significantly high percentage of children who admired anti-social peers were serious, violent, and chronic offenders – highlighting the role of social learning theory in play (Fox et al. 2015). Another social factor which was highly correlated with juvenile serious, violent, and chronic offenders was the presence of having at least one family member already in prison (Fox et al. 2015). This correlation again shows the impact social learning can have on negative behaviors when assessed in addition to ACEs. Victimization of the Black youth and children is a potential source of social learning, where victimization leads to them being exposed to and a witness to violence, harm against social norms and bullying behaviors which ultimately could be linked to externalization behaviors in their later life as delinquency.
ACEs, Internalizing, and Externalizing Behaviors
Vulnerability associated with ACEs is documented in the literature as an important predictor of health disparities among the Black population (Evans and English 2002; Logan-Greene et al. 2016; Nurius et al. 2016; Wade et al. 2014). Indeed, a strong association exists between ACEs and psychiatric illnesses, such as depression, anxiety, and post-traumatic stress disorder (PTSD) (Douglas et al. 2010). Germane to this discussion, a study of Black young adults (aged 22–24), reporting more categories of ACEs was associated with more frequent psychological distress, more frequent anxiety, and lower life satisfaction (Mersky et al. 2013). Current research reporting associations between ACEs and internalizing behaviors focus on young adults and utilize cross-sectional designs. Examining internalizing factors (i.e. psychological distress, anxiety) that may account for potential causal pathways in developmental trajectory holds potential to be an efficacious step to decreasing negative health outcomes among Black children and youth. The present study is designed to meet this need.
In this study, we examine the longitudinal association between ACEs and psychological distress among Black children and youth. Using a longitudinal study design is significant because it allows for analysis of how different ACEs can be associated with psychological distress and eventual negative impact on health in the same sample group over time. The key point is to ensure that the developmental changes are observed overtime to identify a correlation in the Black children and youth based on the high risk of special circumstances and experiences such as victimization that this sample group experiences.
In addition to internalizing behaviors (e.g., psychological distress, anxiety), ACEs are associated with externalizing behaviors, such as substance use, delinquency, or violence perpetration (Duke et al. 2010). Mersky et al. (2013) reported associations between ACEs and substance use among ethnically minority children which included Black and Hispanic children Duke et al. (2010) reported, among a sample of middle school students (males and females, 73% white), experiencing at least 1 ACE was associated with delinquency and interpersonal violence perpetration (bullying, dating violence, and physical violence). These study findings show how ACEs can affect externalizing behaviors among a sample of Black young adults and White youth. Since, the past studies have focused on a mixture of ethnicities in their samples, the present study will focus entirely on Black youth and children, an understudied group that has elevated risk for externalizing behaviors such as substance use, and delinquency because of the disproportionate effects of ACEs in their community.
Due to stigma and marginalization of the Black youth and children, it is important to focus on how ACEs affect them separately from the general public. The youth and children age group (7–13 years) represents the developmental stage where mental health symptoms can start to develop which would later on emerge in adulthood as mental health issues such as depression (Mersky et al. 2013). Utilizing the same sample group to identify a link between ACEs and externalizing behavior can also potentially assist in promoting interventions that target marginalized youth in a younger age in order to prevent externalization of behaviors in adulthood.
From previous research there is evidence that shows that internalizing and externalizing of behaviors do happen simultaneously such as depression in adolescence is correlated with negative externalization of behavior such as delinquency (Akse et al. 2007). A study by Akse et al. (2007) found that there is no clear directional relationship between the two types of behaviors, yet they are known to happen concurrently and the third risk factor which connects these two behaviors is still unknown. This missing link between the two types of behaviors warrants the need to study how experiencing of ACEs impacts this correlation over time.
Summary and Hypotheses
Cross-sectional studies demonstrate that ACEs are associated with psychological distress, mental health outcomes, and externalizing behaviors (substance use, delinquency) (Exner-Cortens et al. 2013; Roberts and Klein 2003; Schad et al. 2008). While valuable, cross-sectional designs cannot establish a causal relationship between ACEs and negative health outcomes. The very few longitudinal studies that have attempted to investigate causal pathways over time focus on adult sample, thus research is needed to investigate the long-term consequences of ACEs among black children and youth.
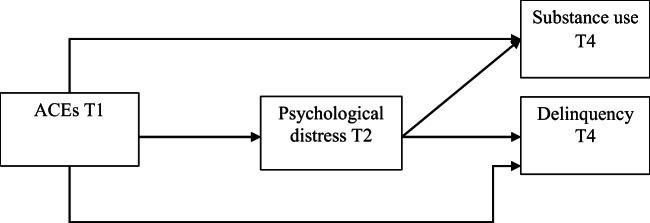
This research tests hypotheses regarding the longitudinal pathways that link ACES to multiple externalizing behaviors (substance use and delinquency) among Black children and youth. It is expected that ACEs will be associated with higher externalizing behaviors. Given research establishing ACEs as a contributor to depression and mood disorders, as well as the association between mood disorders and substance use, and delinquency we hypothesize that psychological distress will serve as a mediator. Hypotheses are outlined in Fig. 1.
Fig. 1.
Study Hypotheses
Methods
Study Design and Participants
Hypotheses were tested using a subsample of longitudinal data from 265 Black children and youth who were recruited from six school districts in Southeast Michigan. The school districts were selected based on community risk factors, developed from a composite rating of publicly available community data, including crime rate, poverty rate, minority composition, and percent rental properties. A stratified sample of schools was selected with two schools representing high, moderate, and low risk communities. Within each school district, two samples of students were randomly selected for the surveys; one sample in 6th grade and one in 9th grade, stratified by gender. Passive parental consent for participation was obtained during initial recruitment and repeated prior to each wave of data collection. Oral assent for students aged 11–12 and written assent for students aged 13–17. A Certificate of Confidentiality was obtained through the Centers for Disease Control and Prevention. The Institutional Review Board for both participating universities and the funding agency approved the data collection protocols.
At baseline, (Time 1, T1), the sample was comprised of 265 Black children and youth. Of those, 229 participants provided a second wave of data approximately 12 months later (Time 2, T2). For the third wave (Time 3, T3) 192 Black children and youth provided data, and the last wave (Time 4, T4) is comprised of 165 Black children and youth for an overall attrition rate of 27.9%. The present study utilized the first, second, and fourth wave of data. At the time of initial data collection, about half of the students were in the sixth grade (44.2%) and ninth grade (55.8%). Grade level was used a control in this study.
Measures
Adverse Childhood Experiences (ACEs)
ACEs was assessed using the Adverse Childhood Experiences (ACE) scale (Felitti et al. 1998). Developed using items from the Childhood Trauma Questionnaire (Bernstein et al. 1994), the Conflict Tactics Scale (Straus 1979), Schoenborn’s alcoholism study (1995), and Wyatt’s 1985 sexual abuse study, this ten-item scale is widely used to assess traumatic exposure in children and youth. Items include, “Did a parent or other adult in the household ever hit you so hard that you had marks or were injured? Or did you often feel that you didn’t have enough to eat, had to wear dirty clothes, and have no one to protect you?” Items were summed to form an index of trauma exposure.
Psychological Distress
Psychological Distress was assessed at Time 1 and Time 2 with 7-items from the K6+ Psychological Distress Scale (Kessler et al. 2002). It assesses nervousness, hopelessness, restlessness, depression, anger, and feelings of worthlessness. Participants reported the frequency during the past 4 weeks with which each of these occurred, ranging from 0 (none of the time) to 4 (all of the time). Cronbach’s α was .79 for Time 1 and .77 for Time 2. All items were averaged to create an index of psychological distress.
Substance Use
At Time 1 and Time 4, children and youth reported the number of times in the past year that they used alcoholic beverages, marijuana, other illegal drugs, and drank more than five alcoholic beverages on one occasion. Responses to these items were standardized and averaged to form a substance use index. Cronbach’s α was .79 for Time 1 and .81 for Time 4.
Delinquency
To assess delinquent and aggressive behavior within the last year, the 35-item Delinquency Scale from the National Youth Survey was utilized (Anderson and Dill 2000; Elliot et al. 1985). Children and youth reported how many times in the last year they have done things such as “Purposely damaged or destroyed property belonging to your parents or other family members.” Children and youth reported the frequency of during the past year with responses ranging from 0 (never) to 5 (10 or more times) Cronbach’s α was .80 for Time 1 and .81 for Time 4.
Data Analysis Plan
Hypotheses were tested using structural equation modeling with Mplus 7 (Muthén 2010). Mplus allows for missing data to be modeled using full information maximum likelihood estimation, testing hypotheses with all data present and preserving the baseline sample size. Indirect effects were estimated for the mediation model using 95% bias corrected confidence intervals obtained from bootstrapping (Preacher et al. 2007). Outcome variables (substance use and delinquency) and psychological distress at T1 were controlled. Grade level was also used as a control. Following Bollen’s (1989) recommendations, we assessed goodness-of-fit with the Root Mean Square Error of Approximation (RMSEA; Browne and Cudeck 1992), comparative fit index (CFI; Bentler 1990), and the Tucker-Lewis Index (TLI; Gerbing and Anderson 1992).
Results
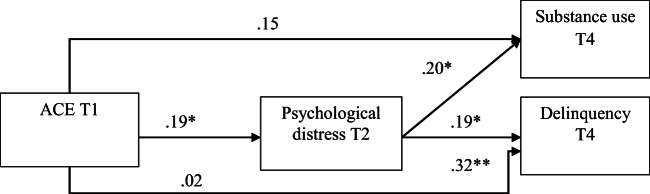
Table 1 includes the bivariate associations of all study variables. ACEs was significantly associated with all study variables (r = .13–.25). ACEs was positively correlated with psychological distress, substance use, and delinquency. This means that experiencing ACEs is associated with higher levels of the aforementioned internalizing and externalizing behaviors. Given these significant associations, we move forward with our mediation model. Figure 2 present the direct effect model showing direct effects from ACEs to substance use and delinquency.
Table 1.
Bivariate Associations of Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. ACEs T1 | 1 | |||||||
| 2. Psychological Dis T2 | .25** | 1 | ||||||
| 3. Psychological Dis T1 | .20** | .40** | 1 | |||||
| 4. Substance Use T4 | .24** | .31** | .19* | 1 | ||||
| 5. Substance Use T1 | .26** | .17* | .17** | .41** | 1 | |||
| 6. Delinquency T1 | .11 | .11 | −.12 | .39** | .06 | 1 | ||
| 7. Delinquency T4 | .13* | .09 | −.03 | .01 | −.05 | .01 | 1 | |
| 8. Grade Level | .21** | .29** | .29** | .25** | .24** | −.09 | .16* | 1 |
p < .05*, p < .01**, N = 265
Fig. 2.
Direct Effect Model. Note. N = 265,Controlled for baseline levels of outcome variables and grade level (not shown)
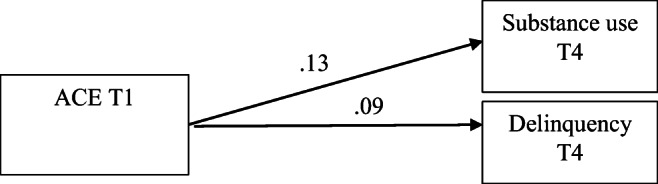
In Fig. 3, we present the full indirect effects model. ACEs at T1 significantly predicted psychological distress at T2 (β = .19, p < .05), which in turn predicted substance use (β = .20, p < .05), and delinquency (β = .19, p < .05). We tested the significance of indirect effects using bootstrapping procedures. Standardized indirect effects were computed for each of 5000 bootstrapped samples, and the 95% confidence interval was computed by determining the indirect effects at the 5th and 95th percentiles. The indirect effects of ACEs on substance use via psychological distress was significant (β = .05, 95% CI [.01, .10]). Lastly, the indirect effects of ACEs on delinquency via psychological distress was significant (β = .05, 95% CI [.00, .09]). Therefore, psychological distress served as a mediator of the associations between ACES and substance use, and delinquency.
Fig. 3.
Indirect Effect Model. Note. N = 265, p < .10+ p < .05*, p < .01**, Controlled for baseline levels of outcome variables and grade level (not shown)
Discussion
Previous research reports ACEs in predicting internalizing and externalizing behaviors among black populations (Sheidow et al. 2014; Fitzpatrick and Boldizar 1993). The present study results were consistent with previous research. First, we found that ACEs were directly and positively associated with psychological distress i.e. the more children experience ACEs, the rate of psychological distress reporting is higher. Then, psychological distress was directly and positively linked to substance use and delinquency. Therefore, as children and youth report higher levels of psychological distress, they also report higher levels of substance use and delinquency. Lastly, psychological distress mediated the association between ACEs and substance use and delinquency showing a process where high levels of ACEs experiences was correlated with high rates of psychological distress which ultimately was linked with high levels of substance use and delinquency.
The present study is novel because it focuses entirely on black youth and children who have faced marginalization and victimization at significantly higher rates compared to other ethnicities. This particular sample group makes this study one of its kind because it follows the same group of individuals over time to observe how those heightened levels of victimization and high rates of ACEs has impacted the internalizing and externalizing of behaviors. This study replicates and extends a growing body of literature indicating that ACEs are a risk factor for negative health outcomes among black children and youth (Fitzpatrick and Boldizar 1993; Hammack et al. 2004; Li et al. 2007; Löfving-Gupta et al. 2017). Past research has focused mainly on the effects of ACEs on adults. The present study highlights the influences of ACEs during adolescence, a crucial developmental time period with many biological, cognitive, and social transitions. Youth who report past ACES may experience additional challenges such as poor mental health as they transition through adolescence because ACEs increases their vulnerability to substances and other risk behaviors. Our findings show that during early adolescence and adolescence, when youth go through ACEs, they are more likely to report psychological distress compared to those who did not report ACEs.
Additionally, our findings show that as youth report past ACES and transition through adolescence, they must also cope with psychological distress, which places them at elevated risk for negative health outcomes and future risk of delinquency. The present study examines psychological distress as a major negative health outcome. This study also supports evidence from Douglas et al. (2010), that anxiety and mood disorders are the mediator between ACEs and substance use risk. Future studies could examine the effects of other negative health outcomes among Black children and youth, such as anxiety or anger.
Although cross-sectional studies link ACEs to internalizing and externalizing behavior, few studies examine mechanisms through which ACEs confers risk behaviors over time. We found that psychological distress mediated the association between ACEs and substance use, and delinquency. Results of this study suggest that ACEs may be important in the development of psychological distress during adolescence. These findings are consistent with current literature linking ACEs to depression among young adult populations (Merrick et al. 2017). Emotional abuse and neglect during childhood and adolescence can have significant influence on developmental processes and have a lasting impact on mental health.
When a child is continuously humiliated, neglected, or abused--all forms of ACEs—the consequences can be far-reaching (Merrick et al. 2017). Black children and youth who are dealing with the difficult emotional consequences of ACEs and lack of ability to cope in a constructive way, may repeat what they have experienced in their childhood and engage in risky behaviors. This correlation refers back to the social learning theory framework, where the exposure and the observing of poor conditions during childhood could lead to risky behaviors such as delinquency in later life hence, highlighting the importance of early interventions for at-risk adolescent populations such as the Black children and youth. Previous research emphasized the interconnection of ACEs which means that exposure to one form of adversity significantly increases the odds of being exposed to another form of adversity (Dong et al. 2004; Merrick et al. 2017).
Our findings demonstrate a cumulative increase in risk for negative mental health and internalizing and externalizing behaviors with each additional ACE experienced. This triangular relationship builds upon the research of Akse et al. (2007) and provides evidence where a third possible risk factor for poor mental health and externalizing behaviors (or delinquency) could be the experiencing of various levels and number of ACEs in childhood. As Black children and youth experience more instance of ACEs, they report higher levels of psychological distress, substance use and delinquency and. This supports the evidence provided by Fox et al. (2015) and Duke et al. (2010) where there was a correlation between violence related delinquent behaviors and having at least one individual in their family who was also convicted or witnessing family dysfunction. It shows that experiencing various types of ACEs which exposes the Black youth to negative and violent behaviors and actions, increases the likelihood that they will perform the same action in their lives.
The correlation between experiencing ACEs and delinquency is significant because it demonstrates that delinquency can begin in adolescence or earlier (Fox et al. 2015) and thus should not be considered a behavior that will only affect these youth in their later life. It highlights the importance of targeted interventions in youth to prevent escalation to violent behaviors. Psychological distress also mediated the associations between the cumulative scale of ACEs and risk behaviors. Thus, it is the cumulative nature of ACEs that is a salient risk factor for negative health outcomes among Black children and youth. As they report categories of ACEs, each additional type adversity may heighten chances of negative health outcomes beyond the risk conferred by reporting ACE.
The correlation between ACEs and delinquency may also be impacted by other social factors such as poor financial position, mental health issues in parents, high community violence, lack of support from peers or parents, and lower socio-economic neighborhood (Duke et al. 2010). The impact of social factors once again relates back to the framework of the social learning theory, where the delinquent behavior may be happening because of the black youth observing those actions in their personal and social life. The impact of these factors alongside experiencing ACEs and delinquent behavior in black youth and children could possibly be a direction for future studies. Additionally, future studies can also look at the role gender plays in externalizing behaviors in Black youth and children.
Limitations and Implications
Several strengths and limitations of the study should be mentioned. This study uses self-report measures of study variables. This allows for the potential of self-report bias to inflate the associations between variables. Additionally, this is a unique sample of Black children and youth in the Midwestern United States. Therefore, findings may not be generalizable to those in other settings. These limitations notwithstanding, the present study highlights Black youth’s ACEs and how these experiences influence psychological distress and externalizing behaviors. The findings of this study provide new insights through the investigation of ACEs and how early experiences influence internalizing and externalizing behaviors among Black children and youth over time. Identification of psychological distress as the mediator between ACEs and substance use and delinquency is significant because it shows that if treatment of psychological distress was made a priority, then the risk for substance use and delinquent behavior could be reduced (Douglas et al. 2010). These interventions can also include an element of targeting at risk families by providing support to mothers in the early stages once the child is born. Duke et al. (2010) discussed of such an approach which was successful in reducing ACEs for children in communities that participated in this targeted intervention as compared to the general public who did not. When tailoring community programs geared towards reducing risk behaviors among this population, it may be important to use a trauma-informed approach.
To engage youth in prevention/interventions and practice, it is important to understand the contexts in which they develop i.e. having knowledge on the specific type of victimization instances that Black youth may experience more than their peers as well as the social factors. Therefore, taking a trauma-informed approach that will acknowledge the adverse childhood experiences that youth went through and to understand how these experiences shape their development through adolescence may be efficacious. Internalizing and externalizing of behaviors in youth that has experienced ACEs is not a permanent fixture and hence, can be changed to positive behaviors and mental health by timely and specific interventions (Duke et al. 2010).
Funding Information
This work was supported by the Centers for Disease Control and Prevention [U01-CE002115].
Compliance with Ethical Standards
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Akse J, Hale B, Engels R, Raaijmakers Q, Meeus W. Co-occurrence of depression and delinquency in personality types. European Journal of Personality. 2007;21:235–256. doi: 10.1002/per.604. [DOI] [Google Scholar]
- Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C. H., Perry, B. D., ... & Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174–186. [DOI] [PMC free article] [PubMed]
- Anderson CA, Dill KE. Video games and aggressive thoughts, feelings, and behavior in the laboratory and life. Journal of Personality and Social Psychology. 2000;78:772–790. doi: 10.1037/0022-3514.78.4.772. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J. Initial reliability and validity of a new retrospective measure of child abuse and neglect. The American Journal of Psychiatry. 1994;151(8):1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- Bollen KA. A new incremental fit index for general structural equation models. Sociological Methods & Research. 1989;17(3):303–316. doi: 10.1177/0049124189017003004. [DOI] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods & Research. 1992;21(2):230–258. doi: 10.1177/0049124192021002005. [DOI] [Google Scholar]
- Burke, N. J., Hellman, J. L., Scott, B. G., Weems, C. F., & Carrion, V. G. (2011). The impact of adverse childhood experiences on an urban pediatric population. Child abuse & neglect, 35(6), 408–413. [DOI] [PMC free article] [PubMed]
- Dong, M., Anda, R. F., Felitti, V. J., Dube, S. R., Williamson, D. F., Thompson, T. J., ... & Giles, W. H. (2004). The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child abuse & neglect, 28(7), 771–784. [DOI] [PubMed]
- Children’s Bureau Child Maltreatment 2016, (U.S. Department of Health & Human Services, 2016). https://www.acf.hhs.gov/sites/default/files/cb/cm2016.pdf.
- Douglas KR, Chan G, Gelernter J, Arias AJ, Anton RF, Weiss RD, Brady K, Poling J, Farrer L, Kranzler HR. Adverse childhood events as risk factors for substance dependence: Partial mediation by mood and anxiety disorders. Addictive Behaviors. 2010;35(1):7–13. doi: 10.1016/j.addbeh.2009.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake, B., Lee, S. M., & Jonson-Reid, M. (2009). Race and child maltreatment reporting: Are Blacks overrepresented?. Children and youth services review, 31(3), 309–316. [DOI] [PMC free article] [PubMed]
- Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: Evidence from four birth cohorts dating back to 1900. Preventive Medicine. 2003;37(3):268–277. doi: 10.1016/S0091-7435(03)00123-3. [DOI] [PubMed] [Google Scholar]
- Duke N, Pettingell S, Mcmorris B, Borowsky I. Adolescent violence perpetration: Associations with multiple types of adverse childhood experiences. Pediatrics. 2010;125:778–786. doi: 10.1542/peds.2009-0597. [DOI] [PubMed] [Google Scholar]
- Elliot DS, Huizinga D, Ageton SS. Explaining delinquency and drug use. Beverly Hills: Sage; 1985. [Google Scholar]
- Evans GW, English K. The environment of poverty: Multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Development. 2002;73(4):1238–1248. doi: 10.1111/1467-8624.00469. [DOI] [PubMed] [Google Scholar]
- Exner-Cortens D, Eckenrode J, Rothman E. Longitudinal associations between teen dating violence victimization and adverse health outcomes. Pediatrics. 2013;131(1):71–78. doi: 10.1542/peds.2012-1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., ... & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. [DOI] [PubMed]
- Finkelhor D. Prevalence of child victimization, abuse, crime, and violence exposure. Violence against women and children: Mapping the terrain. 2011;1:9–30. [Google Scholar]
- Fitzpatrick KM, Boldizar JP. The prevalence and consequences of exposure to violence among African-American youth. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(2):424–430. doi: 10.1097/00004583-199303000-00026. [DOI] [PubMed] [Google Scholar]
- Fox NA, Rutter M. Introduction to the special section on the effects of early experience on development. Child Development. 2010;81(1):23–27. doi: 10.1111/j.1467-8624.2009.01379.x. [DOI] [PubMed] [Google Scholar]
- Fox BH, Perez N, Cass E, Baglivio MT, Epps N. Trauma changes everything: Examining the relationship between adverse childhood experiences and serious, violent and chronic juvenile offenders. Child Abuse & Neglect. 2015;46:163–173. doi: 10.1016/j.chiabu.2015.01.011. [DOI] [PubMed] [Google Scholar]
- Gerbing DW, Anderson JC. Monte Carlo evaluations of goodness of fit indices for structural equation models. Sociological Methods & Research. 1992;21(2):132–160. doi: 10.1177/0049124192021002002. [DOI] [Google Scholar]
- Hammack PL, Richards MH, Luo Z, Edlynn ES, Roy K. Social support factors as moderators of community violence exposure among inner-city African American young adolescents. Journal of Clinical Child and Adolescent Psychology. 2004;33(3):450–462. doi: 10.1207/s15374424jccp3303_3. [DOI] [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Child Psychology and Psychiatry. 2004;45(2):260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Hiripi E, Mroczek DK, Normand S-LT, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32:959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Li ST, Nussbaum KM, Richards MH. Risk and protective factors for urban African-American children and youth. American Journal of Community Psychology. 2007;39(1–2):21–35. doi: 10.1007/s10464-007-9088-1. [DOI] [PubMed] [Google Scholar]
- Löfving-Gupta, S., Willebrand, M., Koposov, R., Blatný, M., Hrdlička, M., Schwab-Stone, M., & Ruchkin, V. (2017). Community violence exposure and substance use: Cross-cultural and gender perspectives. European Child & AdolescentPpsychiatry, 1–8. [DOI] [PMC free article] [PubMed]
- Logan-Greene P, Kim BE, Nurius PS. Childhood adversity among court-involved children and youth: Heterogeneous needs for prevention and treatment. Journal of Juvenile Justice. 2016;5(2):68. [PMC free article] [PubMed] [Google Scholar]
- Merrick MT, Ports KA, Ford DC, Afifi TO, Gershoff ET, Grogan-Kaylor A. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abuse & Neglect. 2017;69:10–19. doi: 10.1016/j.chiabu.2017.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mersky, J. P., Topitzes, J., & Reynolds, A. J. (2013). Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the US. Child abuse & neglect, 37(11), 917–925. [DOI] [PMC free article] [PubMed]
- Muthén, L. K. (2010). Mplus users guide. Los Angeles, CA: Muthén & Muthén; 2010. Computer software and manual.
- Nurius PS, Green S, Logan-Greene P, Longhi D, Song C. Stress pathways to health inequalities: Embedding ACEs within social and behavioral contexts. International Public Health Journal. 2016;8(2):241–256. [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42(1):185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Roberts TA, Klein J. Intimate partner abuse and high-risk behavior in adolescents. Archives of Pediatrics and Adolescent Medicine. 2003;157(4):375–380 15. doi: 10.1001/archpedi.157.4.375. [DOI] [PubMed] [Google Scholar]
- Rutter M. Transitions and turning points in developmental psychopathology: As applied to the age span between childhood and mid-adulthood. International Journal of Behavioral Development. 1996;19(3):603–626. doi: 10.1177/016502549601900309. [DOI] [Google Scholar]
- Sameroff A. A unified theory of development: A dialectic integration of nature and nurture. Child Development. 2010;81(1):6–22. doi: 10.1111/j.1467-8624.2009.01378.x. [DOI] [PubMed] [Google Scholar]
- Schad MM, Szwedo DE, Antonishak J, Hare A, Allen JP. The broader context of relational aggression in adolescent romantic relationships: Predictions from peer pressure and links to psychosocial functioning. Journal of Children and Youth Adolescence. 2008;837(3):346–358. doi: 10.1007/s10964-007-9226-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenborn, C.A. (1995). Exposure to alcoholism in the family: United States 1988. Advance Data from Vital and Health Statistics, vol. 205. National Center for Health Statistics, Hyattsville MD. Publication PHS 95-1880. [PubMed]
- Sheidow AJ, Henry DB, Tolan PH, Strachan MK. The role of stress exposure and family functioning in internalizing outcomes of urban families. Journal of Child and Family Studies. 2014;23(8):1351–1365. doi: 10.1007/s10826-013-9793-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP. Building a new biodevelopmental framework to guide the future of early childhood policy. Child Development. 2010;81(1):357–367. doi: 10.1111/j.1467-8624.2009.01399.x. [DOI] [PubMed] [Google Scholar]
- Shonkoff, J. P., Garner, A. S., Siegel, B. S., Dobbins, M. I., Earls, M. F., McGuinn, L., ... & Committee on Early Childhood, Adoption, and Dependent Care. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232-e246. [DOI] [PubMed]
- Straus MA. Measuring intrafamily conflict and violence: The conflict tactics scales. Journal of Marriage and the Family. 1979;14:75–88. doi: 10.2307/351733. [DOI] [Google Scholar]
- Wade R, Shea JA, Rubin D, Wood J. Adverse childhood experiences of low-income urban children and youth. Pediatrics. 2014;134(1):e13–e20. doi: 10.1542/peds.2013-2475. [DOI] [PubMed] [Google Scholar]
- Wyatt GE. The sexual abuse of afro-American and white-American women in childhood. Child Abuse & Neglect. 1985;9(4):507–519. doi: 10.1016/0145-2134(85)90060-2. [DOI] [PubMed] [Google Scholar]