Since the World Health Organization declared the outbreak of COVID-19 to be a global health emergency of international concern [1], increased anxiety and worry related to the immediate and long-term consequences of this pandemic have affected everybody's life to a great extent, and yet appear to be reasonable [2, 3]. Data from sampling of opinion polls around the world during the early months of the pandemic revealed significant levels of COVID-19-related worry [2]. Varying degrees of worry severity have been described across several populations and subgroups, worry being more present in places where the largest number of confirmed COVID-19 cases was found, as well as among groups with greater social vulnerabilities [3]. Further, distress related to COVID-19 may have a substantial negative impact on the most vulnerable subgroups, such as healthcare workers, older people, psychiatric patients, as well as individuals at risk of developing mental disorders [3, 4, 5].
From a clinical perspective, attention should be paid to the various manifestations of COVID-19 worry that may progress to become dysfunctional. Indeed, dysfunctional worry related to the COVID-19 pandemic, defined as a state of persistent worry about COVID-19 and its possible consequences that is perceived by the individual as difficult to control, with a number of related negative consequences (i.e., difficulties concentrating, trouble sleeping, constantly checking news and social media, marked loss of work productivity, and difficulties finding joy in everyday situations), has been reported among individuals from the general population [6]. A brief self-guided, online cognitive-behavioral intervention was found to reduce dysfunctional COVID-19 worry and associated behavioral symptoms [6].
Individuals may react differently to a health-threatening condition such as COVID-19, based on their own illness behavior. For instance, in the presence of flu-like symptoms (e.g., fever, fatigue, cough) which may be compatible with COVID-19, some persons may immediately seek medical help at the emergency room; others may call their primary care physician, follow recommendations, and stay at home; others again may not seek professional help and turn to self-medication. The question is when a certain manifestation of illness behavior can be judged as dysfunctional and thus is worthy of clinical attention.
The concept of illness behavior was introduced by Mechanic and Volkart [7] to describe the different ways in which individuals may perceive, evaluate, and react to certain physical symptoms. As specified by Mechanic [8], “illness behavior refers to the varying ways individuals respond to bodily indications, how they monitor internal states, define and interpret symptoms, make attributions, take remedial actions and utilize various sources of informal and formal care.” Illness behavior thus represents the result of different interacting variables, including those related to the illness (e.g., prevalence, predictability of outcomes, degree of threat), patient characteristics (e.g., demographics, cognitive representation of the illness, psychological distress and psychiatric disorders, personality, social support), and doctor's attitudes and behaviors (e.g., providing clear explanation, information, and reassurance). Indeed, it is influenced by subjective, social, and cultural determinants and may vary from one person to another and within the same individual according to the specific illness episode. Psychological responses that may arise are likely to influence the illness course, therapeutic response, and outcome. Illness behavior may substantially impact on the use of healthcare services, treatment adherence, and self-management behaviors [9].
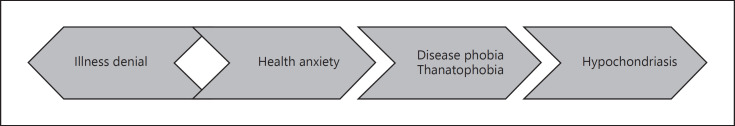
The clinical spectrum of illness behavior, as described in the Diagnostic Criteria for Psychosomatic Research − Revised [10, 11], may provide a comprehensive framework for a better understanding of the psychosocial consequences of the COVID-19 pandemic. As depicted in Figure 1, it encompasses a number of psychosomatic syndromes, including health anxiety, disease phobia, thanatophobia, hypochondriasis, and, at the opposite end of the spectrum, illness denial.
Fig. 1.
The clinical spectrum of illness behavior.
Health anxiety is characterized by a transient, generic worry about illness (possibly including COVID-19 infection), concern about pain, and bodily preoccupations that tend to respond to medical reassurance, even though new worries may subsequently ensue [10]. Within the context of the COVID-19 pandemic, health anxiety may be considered near the normal end of the spectrum.
When worry becomes more specific and does not respond to medical reassurance, then disease phobia may arise. It refers to the presence of a persistent, unfounded fear of suffering from a specific disease (including COVID-19 infection), with doubts remaining despite adequate medical examination and reassurance. Fears tend to manifest themselves in attacks rather than in constant, chronic worries as in hypochondriasis; panic attacks may also be present [10]. Not surprisingly, high scores in the SCL-90 phobia subscale were detected with an online survey from January 30 to February 3, 2020 among the general population in China [12].
Thanatophobia is characterized by attacks with the sense of impending death and/or conviction of dying soon, without being in a threatening situation or in real danger, despite adequate appraisal of the situation (e.g., positive test for COVID-19 while asymptomatic) and of management to be followed (e.g., self-quarantine) as provided by a physician, with opportunity for discussion and clarification. It is accompanied by marked and persistent fear and avoidance of external death-related stimuli (e.g., news regarding deaths due to COVID-19), exposure to which invariably provokes an immediate anxiety response.
The more severe end of the clinical affirmative spectrum of illness behavior is represented by hypochondriasis, characterized by persistent fears, or the idea, of having a serious disease based on misinterpretation of bodily symptoms, despite adequate medical evaluation and reassurance. Within the context of the current pandemic, individuals may display fears of having COVID-19 that persist despite negative testing and seek multiple testing as they still worry about some physical symptoms. Further, cyberchondria was found to act as a risk factor for increased anxiety during the COVID-19 pandemic [13]. Specific psychotherapeutic strategies have been developed and validated in randomized controlled trials [11] to address resistance to reassurance, which is the key characteristic of hypochondriasis, with significant clinical benefits.
Conversely, illness denial, a clinical syndrome that has been neglected by traditional psychiatric nosography, pertains to patients who do not acknowledge the presence or severity of their physical illness as a reaction to symptoms, signs, diagnosis, or medical treatment, despite adequate appraisal of the medical situation and management to be followed. It may be associated with counterphobic behavior, delayed seeking of medical attention, or lack of compliance. In healthy subjects, it may concern one's own vulnerability to life-threatening diseases, resulting in unsafe health behaviors or nonattendance to preventive screenings. Within the context of the current COVID-19 pandemic, the concept of illness denial can be expanded to encompass nonadherence to preventive measures (e.g., physical distancing, mask wearing, cleaning hands, avoiding crowds) [14] which have been established to prevent the spread of COVID-19. The diagnostic criteria for illness denial [10] can be adapted to COVID-19, as shown in Table 1. Illness denial may increase the individual risk of getting or spreading COVID-19 and, in turn, it may contribute to worsening of the pandemic at the community level [15].
Table 1.
Diagnostic criteria for illness denial adapted to the COVID-19 pandemic (criteria A and B are required)
| Criterion A | persistent denial of being at risk of COVID-19 infection/transmission, associated with nonadherence to preventive measures, as a reaction to the established public actions for transmission containment at both the individual and community level |
| Criterion B | the subject has been provided an adequate appraisal of the public health emergency and related preventive measures to be followed |
This is, however, different from denialism about COVID-19, a socio-political phenomenon which has been inflated by authoritarian governments or politicians who try to deprive the general public of accurate information about the pandemic and actively oppose the prosecution of scientists, politicians, journalists, and others who may raise legitimate factual concerns about COVID-19 [16]. Twenty years ago, this journal warned against the risk of a loss of credibility associated with the financial conflicts of interest of researchers [17]. The current mistrust against the medical profession and medical institutions may also be seen as one of the hidden costs of not adequately addressing financial conflicts of interest in medicine [18].
The varying psychological responses observed during the COVID-19 pandemic can be effectively subsumed under the conceptual framework of illness behavior. Additional protective and vulnerability factors that could moderate its manifestations need to be considered, including psychological flexibility and resilience [19, 20], allostatic load/overload [21, 22], and psychological reactance [23, 24, 25]. Psychological flexibility, which constitutes a key feature of euthymia, is concerned with balance and integration of psychic forces that lead to resistance to stress [19, 20]. It guides actions and feelings to shape the future accordingly, and promotes resilience and anxiety/frustration tolerance. Therefore, it is conceivable that psychological flexibility may significantly affect the way in which a person experiences and reacts to COVID-19 and its consequences. Allostatic load reflects the cumulative effects of both life events and daily stressful experiences, and it has been acknowledged as a risk factor for both mental and medical outcomes [21, 22]. When environmental challenges exceed individual coping resources, allostatic overload ensues [22]. Comparably high levels of post-COVID-19 allostatic load were reported among medical and nonmedical workers in China [4], with psychological distress and dysfunctional illness behavior acting as risk factors for allostatic load. Conversely, COVID-19 illness-denying behaviors, particularly disregard of preventive measures, might be sustained by psychological reactance, a motivational force that leads individuals to fear loss of control [23], that was found to be associated with treatment nonadherence and resistance [24, 25]. Greater clinical attention should thus be devoted to the individual's psychological characteristics that may lead to dysfunctional responses to the current pandemic [4, 5, 6].
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
No funding was received.
Author Contributions
Both authors equally contributed to the paper.
References
- 1.World Health Organization (WHO) [Internet]. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) [cited 2020 Jan 30]. Available from: https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 2.Angus Reid Institute [Internet]. Half of Canadians taking extra precautions as coronavirus continues to spread around the globe [cited 2020 Apr 20]. Available from: https://angusreid.org/wp-content/uploads/2020/02/2020.02.04.Coronavirus.pdf.
- 3.Fitzpatrick KM, Drawve G, Harris C. Facing new fears during the COVID-19 pandemic: the State of America's mental health. J Anxiety Disord. 2020 Oct;75:102291. doi: 10.1016/j.janxdis.2020.102291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peng M, Wang L, Xue Q, Yin L, Zhu BH, Wang K, et al. Post-COVID-19 epidemic: allostatic load among medical and nonmedical workers in China. Psychother Psychosom. 2020 Nov;:1–10. doi: 10.1159/000511823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Busch IM, Moretti F, Mazzi M, Wu AW, Rimondini M. What we have learned from two decades of epidemics and pandemics: a systematic review and meta-analysis of the psychological burden of frontline healthcare workers. Psychother Psychosom Forthcoming. doi: 10.1159/000513733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wahlund T, Mataix-Cols D, Olofsdotter Lauri K, de Schipper E, Ljótsson B, Aspvall K, et al. Brief online cognitive behavioural intervention for dysfunctional worry related to the COVID-19 pandemic: a Randomised Controlled Trial. Psychother Psychosom. 2020 Nov;((Nov)):1–9. doi: 10.1159/000512843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mechanic D, Volkart EH. Illness behavior and medical diagnoses. J Health Hum Behav. 1960;1((2)):86–94. [Google Scholar]
- 8.Mechanic D. Sociological dimensions of illness behavior. Soc Sci Med. 1995 Nov;41((9)):1207–16. doi: 10.1016/0277-9536(95)00025-3. [DOI] [PubMed] [Google Scholar]
- 9.Sirri L, Fava GA, Sonino N. The unifying concept of illness behavior. Psychother Psychosom. 2013;82((2)):74–81. doi: 10.1159/000343508. [DOI] [PubMed] [Google Scholar]
- 10.Fava GA, Cosci F, Sonino N. Current psychosomatic practice. Psychother Psychosom. 2017;86((1)):13–30. doi: 10.1159/000448856. [DOI] [PubMed] [Google Scholar]
- 11.Cosci F, Fava GA. The clinical inadequacy of the DSM-5 classification of somatic symptom and related disorders: an alternative trans-diagnostic model. CNS Spectr. 2016 Aug;21((4)):310–7. doi: 10.1017/S1092852915000760. [DOI] [PubMed] [Google Scholar]
- 12.Liu X, Luo WT, Li Y, Li CN, Hong ZS, Chen HL, et al. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect Dis Poverty. 2020 May;9((1)):58. doi: 10.1186/s40249-020-00678-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jungmann SM, Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: which factors are related to coronavirus anxiety? J Anxiety Disord. 2020 Jun;73:102239. doi: 10.1016/j.janxdis.2020.102239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Organization (WHO) [Internet]. Coronavirus disease (COVID-19) advice for the public [cited 2020 Dec 8]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
- 15.Falkenbach M, Greer SL. Denial and distraction: how the populist radical right responds to COVID-19 comment on “A scoping review of PRR parties' influence on welfare policy and its implication for population health in Europe”. Int J Health Policy Manag. 2020 Aug; doi: 10.34172/ijhpm.2020.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mian A, Khan S. Coronavirus: the spread of misinformation. BMC Med. 2020 Mar;18((1)):89. doi: 10.1186/s12916-020-01556-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fava GA. Conflict of interest and special interest groups. The making of a counter culture. Psychother Psychosom. 2001 Jan-Feb;70((1)):1–5. doi: 10.1159/000056218. [DOI] [PubMed] [Google Scholar]
- 18.Fava GA. The hidden costs of financial conflicts of interest in medicine. Psychother Psychosom. 2016;85((2)):65–70. doi: 10.1159/000442694. [DOI] [PubMed] [Google Scholar]
- 19.Fava GA, Guidi J. The pursuit of euthymia. World Psychiatry. 2020 Feb;19((1)):40–50. doi: 10.1002/wps.20698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guidi J, Fava GA. The emerging role of euthymia in psychotherapy research and practice. Clin Psychol Rev. 2020 Dec;82:101941. doi: 10.1016/j.cpr.2020.101941. [DOI] [PubMed] [Google Scholar]
- 21.Guidi J, Lucente M, Sonino N, Fava GA. Allostatic load and its impact on health: a systematic review. Psychother Psychosom. 2021;90((1)):11–27. doi: 10.1159/000510696. [DOI] [PubMed] [Google Scholar]
- 22.Fava GA, McEwen BS, Guidi J, Gostoli S, Offidani E, Sonino N. Clinical characterization of allostatic overload. Psychoneuroendocrinology. 2019 Oct;108:94–101. doi: 10.1016/j.psyneuen.2019.05.028. [DOI] [PubMed] [Google Scholar]
- 23.Brehm SS, Brehm JW. Psychological reactance: A theory of freedom and control. New York: Academic; 1981. [Google Scholar]
- 24.De Las Cuevas C, de Leon J. Reviving research on medication attitudes for improving pharmacotherapy: focusing on adherence. Psychother Psychosom. 2017;86((2)):73–9. doi: 10.1159/000450830. [DOI] [PubMed] [Google Scholar]
- 25.Fava GA, Cosci F, Guidi J, Rafanelli C. The deceptive manifestations of treatment resistance in depression: a new look at the problem. Psychother Psychosom. 2020;89((5)):265–73. doi: 10.1159/000507227. [DOI] [PubMed] [Google Scholar]