Abstract
The formation of herd immunity through vaccination is a key point in overcoming the coronavirus disease 2019 (COVID-19) pandemic. To acquire herd immunity, a high vaccination rate is required, which is necessary to instill confidence in the public regarding the effectiveness and safety of the vaccine. In the real-world setting, thorough preparation of components, such as priority setting, vaccine delivery, logistics, and side-effect monitoring is necessary to overcome vaccine hesitancy. Each country prioritizes vaccination since healthcare workers, nursing facility residents, and the elderly population, and similar trends are found between countries. Vaccination is performed at large centers and medical institutions operated by the country, and variations are dependent on the environment of each country. The transport of mRNA vaccines is a challenging task, and to this end, each government is striving for safe distribution. In addition, each authority operates a surveillance system to monitor the safety of vaccines, and Korea needs to produce evidence for monitoring effects and side effects with expertise. Even after the acquisition of herd immunity, COVID-19 is highly likely to remain an endemic infectious disease, and a higher immunity level may be required because of variants of the virus. If the spread of variants of concern continues, a booster vaccination may be required. Therefore, non-pharmaceutical interventions, such as social distancing, wearing a mask, and epidemiological investigation should be maintained.
Keywords: COVID-19, Vaccination Vaccine Priority, Social Distancing
Graphical Abstract
INTRODUCTION
Coronavirus disease 2019 (COVID-19) has caused worldwide damage and is still prevalent as of February 2021. The third wave, which started in November 2020, is affecting most countries, including the United States, the United Kingdom, and Europe.1 In response to the pandemic, countries around the world have applied non-pharmaceutical interventions, such as quarantine, diagnostic testing, contact tracing, social distancing, and wearing masks.2 Some countries have successfully blocked outbreaks, but most countries have just delayed the outbreak. When most pandemic infectious diseases spread in the community, the outbreak continues until herd immunity is established and several waves of the outbreak have occurred.3
Unlike the pandemic of the past, humans have succeeded in developing vaccines for multiple platforms based on advanced biotechnology, and vaccinations began in the US in December 2020. On January 28, 2021, the Republic of Korea also announced a plan to initiate COVID-19 vaccination. To achieve the national goal of herd immunity, it is important to review the cases of the countries, which have already started vaccination, and to establish a thorough plan by collecting sound scientific evidence. This article summarizes Korea's vaccination plan and reviews preparations in major countries. In particular, examples and evidence of vaccination priority, logistics, storage, and side effect monitoring, and provide a scientific basis for possible problems after vaccination are presented in this article. In addition, topics of social change after vaccination have been discussed.
VACCINATION STRATEGY OF COVID-19 IN KOREA
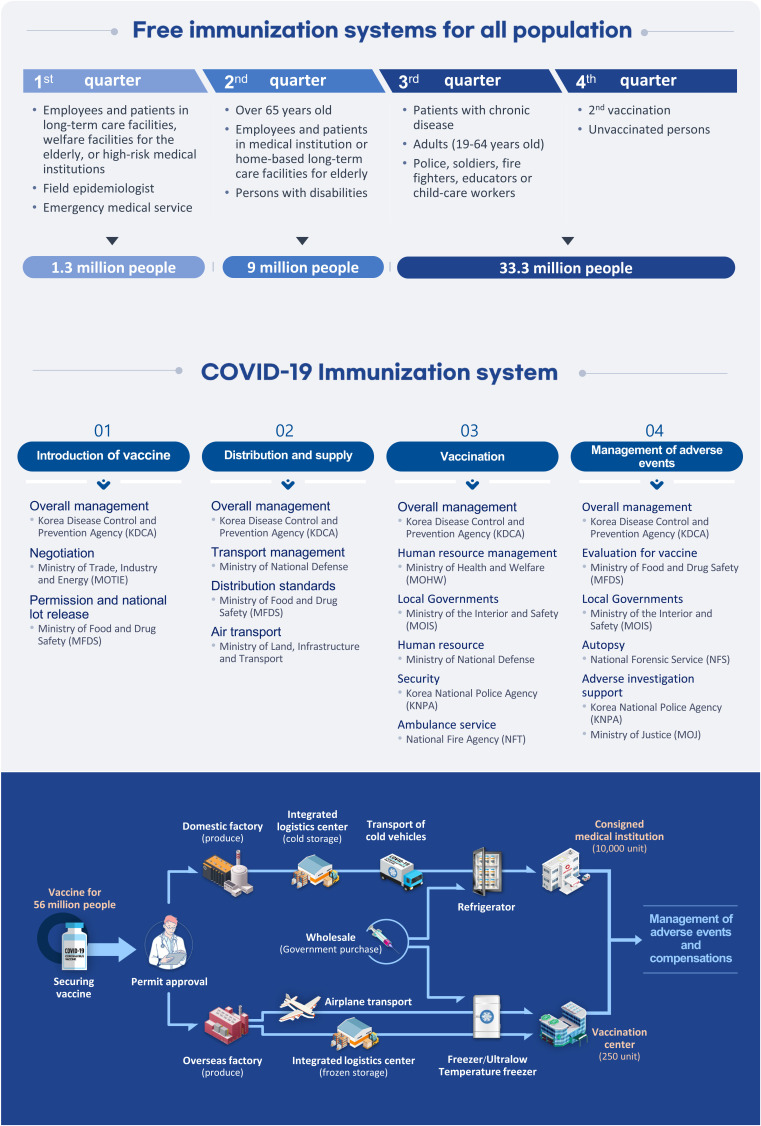
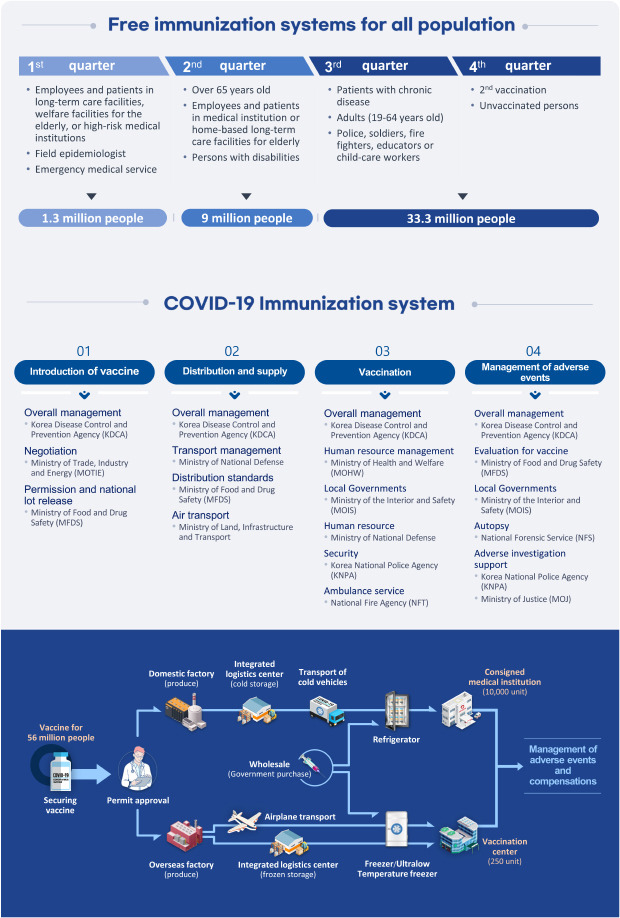
The initial phase of vaccination will start in February 2021. The priority target is 60,000 health-care workers who are directly related to COVID-19. In addition, vaccinations are provided for the elderly in nursing homes and long-term care facilities, as well as for inpatients and workers in mental rehabilitation hospitals. Vaccinations will begin in March for the first responders, such as workers at high-risk medical institutions and epidemiological investigators. Vaccinations for high-risk groups will start in May. High-risk groups include individuals who are 65 years of age or older, disabled, and healthcare professionals. The rest of the population will be vaccinated from July onwards.4
The government of the Republic of Korea had specified the time of formation of herd immunity in November 2021 and proposed the goal of completing vaccinations for 70% of the population. Therefore, 70% of the population must complete the first vaccination by at least the end of October 2021. This is because the second dose of vaccination is given an average of 1 month after the first dose, and the complete protection effect is exerted only after the second dose.
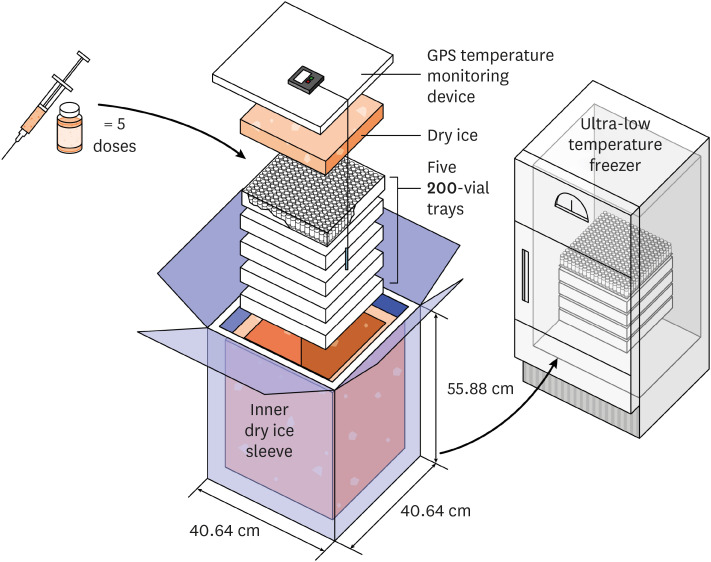
In Korea, vaccination centers will be installed for each region, starting with at least four centers, and the number of centers will increase sequentially to 250 by the second half of 2020. These vaccination centers will handle mRNA vaccines that require cryogenic storage. Other types of vaccines will be implemented at 10,000 pre-designated private medical institutions where existing systems, such as influenza vaccines, are generally maintained (Fig. 1).
Fig. 1. COVID-19 vaccination plan of the Republic of Korea.
COVID-19 = coronavirus disease 2019.
The vaccines that have been confirmed to be introduced in Korea are viral vector vaccines (manufacturer: AstraZeneca, JNJ), mRNA vaccines (manufacturer: Pfizer/bioNTech, Moderna), and a protein subunit vaccine (manufacturer: NovaVax) is under contract. The mRNA vaccine has been reported to have an efficacy of 95%5,6 and is currently being used in several countries. The efficacy of the viral vector vaccine has been reported to be lower than that of the mRNA vaccine, but it also meets the minimum efficacy criteria of the World Health Organization and has the advantage of being easy to store and inoculate. The viral vector vaccine and protein sub-unit vaccine, for which the results of a new interim phase 3 clinical trial were announced at the end of January 20207,8 reported relatively high efficacy, but a study conducted in South Africa showed a decrease in efficacy. This suggests that the effectiveness of existing vaccines using the original genomic sequence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) may be low against the variant of concern (VOC) B.1.351 (Table 1).
Table 1. Summary of the coronavirus disease 2019 vaccines introduced in the Republic of Korea.
| Manufacturer | Platform | Doses | Progress | Time of introduction in Korea4 | Contracted doses | Overall Efficacy | Efficacy in United Kingdom (B.1.1.7 as dominant variant) | Efficacy in South Africa (B.1.351 as dominant variant) |
|---|---|---|---|---|---|---|---|---|
| Pfizer/BioNtech | mRNA | 2 | Currently in use | February 2021 (COVAX facility) | 20 million doses (for 10 million people) | 95%5 | No biologically significant difference from previous variants9 | Not available |
| 3rd quarter of 2021 (government contract) | ||||||||
| Moderna | mRNA | 2 | Currently in use | 2nd quarter of 2021 | 40 million doses (for 20 million people) | 94%6 | No significant impact of neutralizing titers against B.1.1.710 | 6-fold reduction in neutralizing titers was observed against the B.1.351 variant10 |
| Astra Zeneca | Adenovirus-vector | 2 | Currently in use | February 2021 | 20 million doses (for 10 million people) | 62%a11 | 74.6%13 | Limited efficacy against mild disease14 |
| 82%b12 | ||||||||
| JNJ | Adenovirus-vector | 1 | Phase 3 clinical trial completed (interim) | 2nd quarter of 2021 | 6 million doses (for 6 million people) | 66%c7 | 86%d | 57% |
| Novavax | Protein subunit | 2 | Phase 3 clinical trial completed (interim) | Contract in progress | 40 million doses (for 20 million people) | 89%8 | 89% | 60% (HIV-negative population) |
| 49% (including HIV-positive population) |
HIV = human immunodeficiency virus.
aWith standard dose; bA longer prime-boost interval; cFor moderate to severe disease prevention; dPost-hoc analysis in the United States.
VACCINATION RATE AND EPIDEMIC TRENDS IN MAJOR COUNTRIES
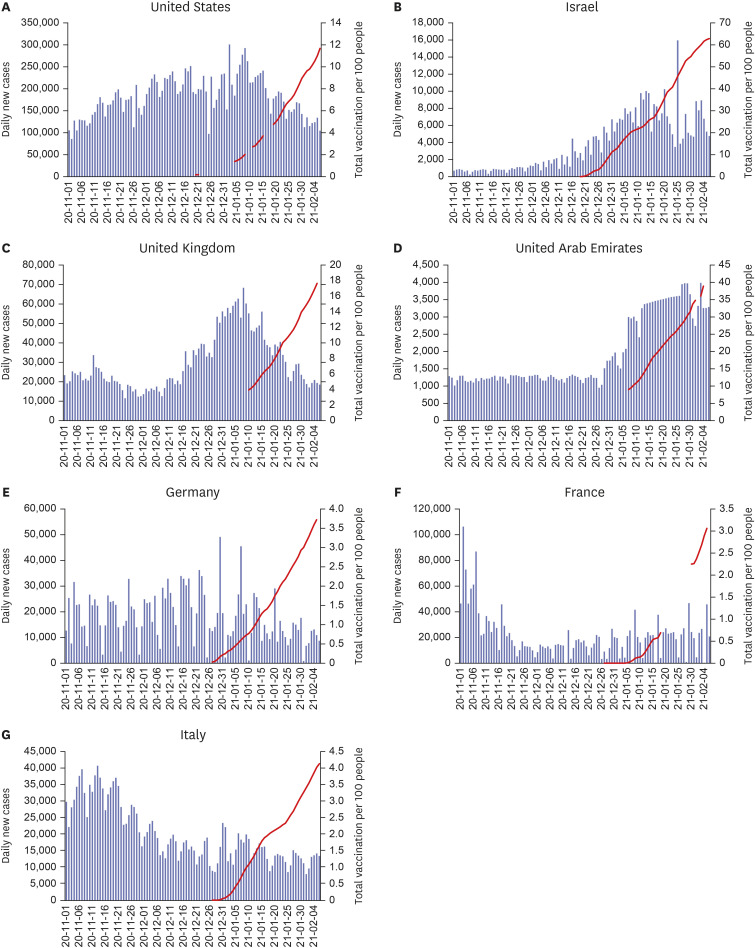
By January 31, 2021, a total of 59 countries had begun vaccination, and by January end, Israel had the highest vaccination rate of 54.7 doses per 100 persons, and then the vaccination rates were 33.7, 13.9, 10.0, 9.4, 3.2, 2.8, and 2.3 doses per 100 persons in the United Arab Emirates, UK, Bahrain, US, Italy, Germany, and France, respectively.15 The Israeli Health Maintenance Organization made a promising report that out of a population of 163,000 individuals, 10 days after the second vaccination, only 31 got infected by COVID-19.16 In countries where vaccination is underway in early February 2021, a decrease in the number of confirmed cases per day is observed (Fig. 2). However, the interpretation of the effect of the overall reduction of confirmed cases deserves attention.
Fig. 2. Trends in vaccination rates and coronavirus disease 2019 confirmed cases in major vaccination countries (Due to the limitation of information on the vaccination rate, total vaccination rates per 100 people were expressed as a discontinuous value in some intervals).
PRIORITY SETTING OF VACCINATION
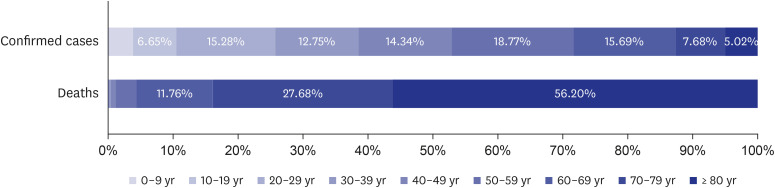
The Republic of Korea has selected healthcare workers related to COVID-19, residents of long-term care facilities for the elderly, and workers as priority groups for COVID-19 vaccination. This is an approach to prevent a collapse of the medical system and reduce mortality. Until January 2021, only 5% of the confirmed cases of COVID-19 in Korea were over 80 years old, but they account for 56.2% of the deaths (Fig. 3)17 and COVID-19 outbreak in long-term care facilities has been severely fatal.18 Until now, COVID-19 infection by medical staff during work has not been commonly found in Korea,19 but it has been shown that even with low exposure risk, healthcare workers are under emotional stress.20 Damage to medical staff due to self-isolation after exposure is also an important factor to consider.
Fig. 3. Proportion of confirmed cases of coronavirus disease 2019 and deaths by age in the Republic of Korea (until January 31, 2021).
Countries around the world have prioritized COVID-19 vaccination and have issued guidelines accordingly. At the community transmission stage, the World Health Organization suggests that high-risk healthcare workers and adult populations according to age-specific risk should be prioritized in the context of limited vaccine availability.21 In the United States, healthcare workers and long-term care facility residents are the top priority. The same trend is being followed in the UK, Germany, France, Canada, Australia, Sweden, and Japan. Prioritization tailored to the characteristics of minorities and national health risk factors is unique to each country. Australia and Canada have prioritized vaccinations for indigenous communities, while Saudi Arabia has a serious health problem caused by obesity, so the priority is determined according to the body mass index. In other words, the priorities for vaccination are determined from the viewpoint of maintaining the medical system, protecting the elderly population, and minorities. Although there are detailed adjustments that reflect the characteristics of each country, they are the same in a large framework (Table 2).
Table 2. Priorities for COVID-19 vaccination in major countries.
| Country/international organization | Stage/phase | Priority | |
|---|---|---|---|
| World Health Organization,21 Strategic Advisory Group of Experts on Immunization | Community transmission | ||
| Stage 1. Very limited vaccine availability, 1%–10% of national population | • 1a: Health workers at high to very high risk | ||
| • 1b: Older adults defined by age-based risk | |||
| Stage 2. Limited vaccine availability, 11%–20% of national population | • Older adults not covered in Stage I | ||
| • Groups with comorbidities or health states determined to be at significantly higher risk | |||
| • Health workers engaged in immunization delivery | |||
| • High-priority teachers and school staff | |||
| Stage 3. Moderate vaccine availability, 21%–50% of national population | • Remaining teachers and school staff | ||
| • Other essential workers outside health and education sectors (police officers, municipal services, transportation workers, etc.) | |||
| • Pregnant women | |||
| • Health workers at low to moderate risk | |||
| • Personnel needed for vaccine production and other high-risk laboratory staff | |||
| • Social/employment groups at elevated risk | |||
| Clusters of cases | |||
| Stage 1. Very limited vaccine availability, for 1%–10% of national population | • Health workers at high to very high risk of acquiring and transmitting infection | ||
| • Older adults defined by age-based risk, in areas with high transmission or anticipated high transmission | |||
| • Emergency reserves for outbreak response or mitigation | |||
| Stage 2. Limited vaccine availability, for 11%–20% of national population | • Health workers at high to very high risk of acquiring and transmitting infection | ||
| • Older adults defined by age-based risk, in the rest of the country | |||
| • Groups with comorbidities or health states determined to be at significantly higher risk and sociodemographic groups at significantly higher risk, in areas with high transmission or anticipated high transmission | |||
| Stage 3. Moderate vaccine availability, for 21%–50% of national population | • Primary and secondary teachers and school staff | ||
| • Other essential workers outside health and education sectors and social/employment groups at elevated risk, in areas with high transmission or anticipated high transmission | |||
| • Health workers at low to moderate risk, country-wide | |||
| • Age groups at high risk of transmission, country-wide | |||
| • Personnel needed for vaccine production and other high-risk laboratory staff | |||
| • Pregnant women | |||
| United States22/Centers for Disease Control and Prevention & Advisory Committee on Immunization Practices | Phase 1a | • Health care workers | |
| • Long-term care facility residents | |||
| Phase 1b | • Frontline essential workers | ||
| • Persons aged ≥ 75 yr | |||
| Phase 1c | • Persons aged 65–74 yr | ||
| • Persons aged 16–64 yr with high-risk medical conditions | |||
| • Essential workers not recommended for vaccination in Phase 1b | |||
| Phase 2 | • All persons aged ≥ 16 yr who have not been vaccinated | ||
| United Kingdom23/Joint Committee on Vaccination and Immunisation | Phase 1 | • Residents in a care home for older adults and their carers | |
| • Persons aged ≥ 80 yr | |||
| • Frontline health and social care workers | |||
| • Persons aged ≥ 75 yr | |||
| • Persons aged ≥ 70 yr | |||
| • Clinically extremely vulnerable individuals | |||
| • Persons aged ≥ 65 yr | |||
| • All individuals aged 16–64 yr with underlying health conditions | |||
| • Persons aged ≥ 60 yr | |||
| • Persons aged ≥ 55 yr | |||
| • Persons aged ≥ 50 yr | |||
| Next phase | • First responders; military personnel | ||
| • Those involved in the justice system, teachers, transport workers, and public servants essential to the pandemic response | |||
| Germany24/Robert Koch Institute | Phase 1 | • Residents at nursing homes | |
| • People aged > 80 yr | |||
| • Employees of medical facilities at very high risk | |||
| • Staff at nursing homes | |||
| Phase 2 | • Persons aged 75–79 yr | ||
| • Other high risk health workers | |||
| • Dementia patients | |||
| • Dementia center staff | |||
| • People with Down's syndrome | |||
| Phase 3 | • Persons aged 70–74 yr | ||
| • Transplant patients | |||
| • Persons at high risk with underlying health conditions | |||
| • Residents of shelters for the homeless or asylum seekers | |||
| • People who are close contacts of pregnant women | |||
| • Those who work in close contact with people at high risk | |||
| • Other health workers | |||
| Phase 4 | • Persons aged 65–69 yr | ||
| • Persons with underlying health conditions | |||
| • Health workers at low risk | |||
| • Teachers | |||
| • Socially vulnerable groups | |||
| Phase 5 | • Persons aged 60–64 yr | ||
| • People in particularly relevant positions in state institutions | |||
| • Retail workers | |||
| • Police | |||
| • Essential workers | |||
| Phase 6 | • Persons aged < 60 yr | ||
| Australia25/Australian Technical Advisory Group on Immunisation | Phase 1: Those who have an increased risk, of developing severe disease or dying from COVID-19 | • Older adults | |
| • People with pre-existing underlying select medical conditions | |||
| • Aborigines and Torres Strait Islanders | |||
| Phase 2: Those who are at increased risk of exposure and hence of being infected with and transmitting SARS-CoV-2 to others at risk of severe disease or are in a setting with high transmission potential | • Health and aged care workers | ||
| • Other care workers | |||
| • People in other settings at an increased risk of virus transmission | |||
| Phase 3: Those working in services critical to societal functioning | • Selected essential services personnel | ||
| • Other key occupations required for societal functions | |||
| Canada26/National Advisory Committee on Immunization | Stage 1 | • Residents and staff of congregate living settings that provide care for seniors | |
| • Adults ≥ 70 yr of age, beginning with adults ≥ 80 yr of age, then decreasing the age limit in 5-year increments to age 70 yr as supply becomes available | |||
| • Health care workers | |||
| • Adults in indigenous communities | |||
| Stage 2 | • Health care workers not included in the initial rollout | ||
| • Residents and staff of all other congregate settings (e.g., quarters for migrant workers, correctional facilities, homeless shelters) | |||
| • Essential workers | |||
| France27/Haute Autorité de Santé (French National Authority of Health) | Phase 1 | • Patients in home care | |
| • Health professionals aged over 65 and/or with comorbidity | |||
| Phase 2 | • Persons aged > 75 yr | ||
| • Persons aged > 65 with comorbidity | |||
| • Persons aged > 65 yr | |||
| • Health professionals aged > 50 yr and/or with comorbidity | |||
| Phase 3 | • Persons aged > 50 yr | ||
| • Persons aged < 50 with comorbidity | |||
| • Essential workers | |||
| Phase 4 | • Essential workers | ||
| • Workers with public contact | |||
| • People in precarious situation (the homeless, prisoners) | |||
| Phase 5 | • All persons aged > 18 years regardless of medical conditions | ||
| Sweden28,29/Folkhälsomyndigheten, The Public Health Agency of Sweden | Priority groups | • People who live in elderly care homes or receive at-home care, primarily those aged > 70 yr | |
| • Healthcare and care workers who have close contact with vulnerable people | |||
| • Other adults who share a household with people receiving at-home care | |||
| Japan30/Ministry of Health, Labour and Welfare | Priority groups | • Medical and other workers at risk | |
| • People aged > 65 yr | |||
| • People with one of 14 types of underlying health conditions (chronic respiratory diseases, cardiac diseases, obesity, diabetes and cancer) | |||
| China31/The National Health Commission | Priority groups | • Front-line workers | |
| • Those aged 18–59 years employed at ports | |||
| • Delivery companies | |||
| • The transportation industry | |||
| • Health and sanitation | |||
| • Public servants | |||
| • Police and firefighters | |||
| • Utilities, aged-care | |||
| • Telecommunications | |||
| • People whose work or studies overseas | |||
| Saudi Arabia32,33/Ministry of Health | Stage 1 | • Citizens and residents aged ≥ 65 yr | |
| • Professionals who are at the highest risk | |||
| • People who are obese and have a BMI of > 40 kg/m2 | |||
| • Persons with immune deficiency including organ transplant recipients or those taking immunosuppressive drugs | |||
| • Persons with two or more chronic diseases including asthma, diabetes, chronic kidney disease, chronic heart disease | |||
| Stage 2 | • Citizens aged > 50 yr | ||
| • Health practitioners | |||
| • Those who have one of the following chronic diseases: asthma, diabetes, chronic kidney disease, chronic heart disease | |||
| • Persons with active cancer | |||
| • Persons with obesity and BMI 30–40 kg/m2 | |||
| Stage 3 | • All citizens and residents who consent to being vaccinated | ||
| Israel34,35/Ministry of Health | Priority groups | • Medical staff - anyone with patient contact | |
| • Medical staff | • Residents in welfare institutions (care home centers) and their caregivers | ||
| • People aged > 60 yr | • Persons aged > 40 yr | ||
| • Those with high risk conditions | • Persons with immune deficiencies | ||
| • Patients with cystic fibrosis or severe restrictive disorder due to muscular dystrophy | |||
| • Close caregivers of elderly | |||
| • Burial facility workers | |||
| • Prisoners and wardens | |||
| • Pregnant women or women planning to be pregnant | |||
| • Preschool and school teachers | |||
COVID-19 = coronavirus disease 2019, BMI = body mass index.
DELIVERY AND LOGISTICS OF VACCINATION
The Republic of Korea uses specialized vaccination centers and pre-designated private medical institutions to administer COVID-19 vaccination. In the United States, vaccinations are performed at hospitals, outpatient clinics, public health clinics, and mobile units, but Pfizer's vaccine may be precluded. There are three main vaccination centers in the UK: large venue vaccination center, hospital hub, and local vaccination service. Germany has a system similar to that of Korea (Table 3). The reason for using both large vaccination centers and local medical institutions for each country is to build an infrastructure that is suitable for the characteristics of different types of vaccines and enables mass-vaccination within a short time.
Table 3. COVID-19 vaccination facilities in major countries.
| Country | Vaccination facilities | |
|---|---|---|
| United States | • Hospitals | |
| • Large outpatient clinics | ||
| • Public health clinics | ||
| • Mobile units | ||
| • Clinics and doctors' offices | ||
| • Pharmacies and some grocery-store chains | ||
| • Long-term-care facilities | ||
| • Certain federally-run sites | ||
| • Pfizer's may preclude some sites36 | ||
| United Kingdom | People will be vaccinated at three main locations: | |
| • Vaccination centers and large-scale venues such as football stadiums, accessed by a national booking service | ||
| • Hospital hubs, using NHS Trusts across the country | ||
| • Local vaccination services, made up of sites led by general practice teams working together in already established primary care networks and pharmacy teams through community pharmacies37 | ||
| Germany | • A COVID-19 vaccine is initially distributed via vaccination centers set up by the federal states (hospitals or inpatient care facilities). Furthermore, there will be mobile vaccination teams that visit38 | |
| Australia | • 30–50 ongoing hospital hubs in urban and rural Australia | |
| • Hub locations to be finalized in conjunction with the States and Territories (will manage cold chain storage and administer Pfizer vaccine only)39 | ||
| Canada | • Every province is responsible for their own vaccine rollout plan.40,41 (Ex: Immunization clinics are being organized in 172 communities in British Columbia and will be overseen by local health authority. The clinics will be held at large centres including school gymnasiums, arenas, convention halls, community halls.) | |
| • Persons in Ontario will be vaccinated in the 17 hospital sites, in addition to UHN and The Ottawa Hospital | ||
| France | During phase 142 | |
| • The vaccines will be delivered to 100 hospitals that are able to store the vaccines at −80°C | ||
| Saudi Arabia | Saudi Arabia has set up large vaccination centers to inoculate residents against COVID-19, as part of its vaccination campaign launched in mid-December, 2020.43 | |
| Israel/Ministry of Health | • 196 immunization stations that will be open by the end of December, 2020 | |
| • 12 united established vaccination centers | ||
| • Hospitals will be vaccinating the population44 | ||
COVID-19 = coronavirus disease 2019.
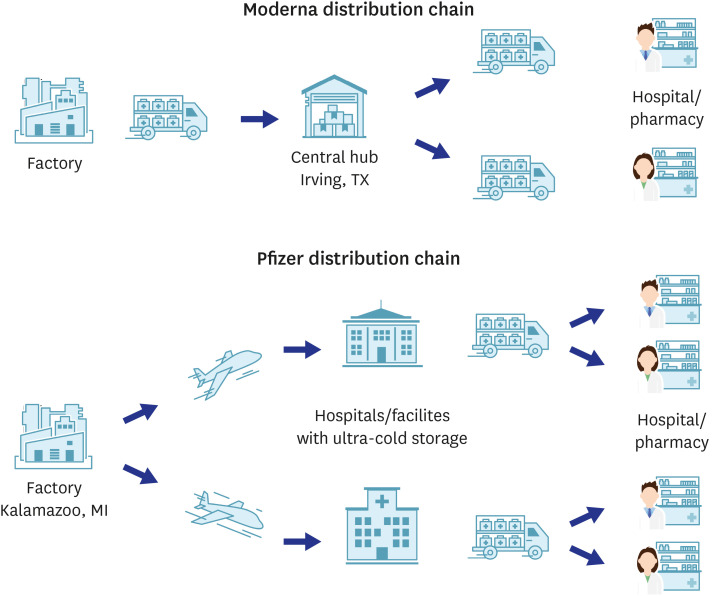
Most of the vaccination with Pfizer's mRNA vaccine, which is widely used, is being carried out at a pre-designated location. This is because the mRNA vaccine is difficult to store and transport. In particular, Pfizer's vaccine needs to be transported at a cryogenic temperature of −70°C, and thorough preparation is required from the packaging stage (Fig. 4). The United States has created a special system to transport Pfizer and Modena vaccines, and private companies, such as FedEx and United Parcel Service are participating as logistics partners. Both companies are responsible for the logistics of half of the country (Fig. 5). Canada, on the other hand, utilizes a state-led logistics system, where a multidisciplinary team, including the Canadian armed forces, are cooperating with private logistics companies to conduct transportation (Table 4).
Fig. 4. Pfizer and BioNTech's Ultra-cold delivery box (Redrawn from the Pfizer's original figure).
Fig. 5. Messenger RNA coronavirus disease 2019 vaccine distribution chains in the United States.
Table 4. Vaccine distribution in major countries.
| Countries | Vaccine | Storage, Transport, Logistics | |
|---|---|---|---|
| Overall | Pfizer/BioNTech | Thermal shipper (−80°C to −70°C) for up to 6 mon, 5 days after transfer to refrigerator | |
| Moderna | Freezer (−20°C) for up to 6 mon, up to 30 days | ||
| AstraZeneca | Refrigerator (2°C–8°C) for up to 6 mon | ||
| United States45,46 | Manufacturing factory: Kalamazoo, MI (Pfizer), Central Hub: Irving, Tx (Moderna) | ||
| Logistic partners: FedEx, UPS | |||
| • FedEx and UPS are each responsible for one half of the country | |||
| • Both UPS and FedEx will use high-tech tracking devices to monitor packages carrying the vaccines | |||
| • Pfizer has also installed its own tracking system on these boxes | |||
| • Vaccine shipments will be getting special treatment, including priority access at the airport | |||
| Australia47 | Logistic partners: DHL and Linfox | ||
| • Support vaccination for all, including people in rural and remote areas | |||
| • Required to track and report the temperature of the vaccines at all times | |||
| • Logistics partners will be responsible for transport and management of vaccination supplies such as needles, syringes, and personal protective equipment | |||
| Canada48 | An immunization NOC has been established as part of federal logistical coordination | ||
| • Supported by a multidisciplinary team of experts, including the Canadian Armed Forces | |||
| • FedEx Express Canada and Innomar Strategies will support the NOC with logistics and vaccines | |||
UPS = United Parcel Service, NOC = National Operations Centre.
CONCERNS RELATED TO VACCINATION
Certain topics must be prepared during the vaccination process. The issues below will be the most frequently asked questions before and after vaccination, and it is important to prepare answers based on scientific evidence.
Anaphylaxis after vaccination
Anaphylaxis after vaccination has been reported for the Pfizer vaccine. According to a report from the centers for disease control and prevention in the United States, a total of 1,893,360 individuals received one dose between December 14 and 23, 2020. and 21 individuals had anaphylaxis. This rate is 11.1 per million vaccinations. The median time from vaccination to the onset of symptoms was 13 minutes. Symptoms occurring within 15 minutes were 71% of the total, and within 30 minutes were 86%.49 The cause of anaphylaxis is presumed to be polyethylene glycol (PEG) and PEG derivatives, such as polysorbates.50 However, in Korea, since it is not possible to test for allergens in advance an observation period after vaccination of about 30 minutes is required, and vaccination facilities must be prepared for anaphylaxis. In addition, based on the US report, if about 60,000 people are inoculated with the first dose of Pfizer's vaccine in Korea, the probability that at least one anaphylaxis will occur is 48.3%. Given the impact of response to initial adverse events on the confidence of future vaccinations, health authorities should pay special attention.
Missed second dose
The second dose may be missed because of an unstable vaccine supply or personal reasons. The United States Advisory Committee on Immunization Practices allows the administration of a second dose within a four-day period (e.g., days 17–21). If more than 21 days have passed since the first dose was received, the second dose can be administered as soon as possible and the vaccination series will not need to be restarted.51
Flu-like symptom after vaccination
Symptoms, such as fever, chills, and muscle pain may appear briefly in approximately 10% after COVID-19 vaccination. If these symptoms appear within 48 hours after vaccination and disappear after a short period of time, this may be a symptom after vaccination. However, if an individual has respiratory symptoms (cough, shortness of breath, sore throat), it may be related to COVID-19 and may require a screening test for COVID-19.
Taking antipyretic analgesics before vaccination
There are considerations for taking premedication to relieve symptoms after vaccination. However, there is no recommendation to date, and some studies suggest that the use of antipyretic analgesics prior to vaccination may alter the immune response.52,53 Therefore, no special premedication is required.
Vaccinations for recovery after COVID-19 infection
Several previous studies have suggested that natural immunity by COVID-19 may not last long. There is also evidence that reinfection is possible.8,54 Therefore, vaccination is also necessary from the viewpoint of immunity boosting. There is also no evidence that vaccination schedules, doses, or platforms should be different from those of the general population.
Need for SARS-CoV-2 diagnostic test before vaccination
Phase 3 clinical trial results of multiple vaccines suggest that past COVID-19 infections do not affect the safety of the vaccine. Vaccination should be performed regardless of prior exposure to COVID-19. Testing for COVID-19 prior to vaccination is not recommended.51
Simultaneous vaccination with non-COVID-19 vaccines
Due to the lack of evidence, to date, most countries do not recommend simultaneous vaccination with other non-COVID-19 vaccines such as influenza. The US recommends that other vaccines be administered at least 14 days after the COVID-19 vaccine.51
Vaccine safety monitoring
Surveillance of the safety of the COVID-19 vaccine and transparent disclosure of results are the most important factors in gaining public confidence. In the Republic of Korea, during the 2020 seasonal influenza vaccination program, there was controversy over death after vaccination due to violation of cold chain regulations, excessive media attention, and fear of COVID-19.55 Later, through autopsy, epidemiological investigation, and comparison of mortality with the previous seasons, it was found that there was no scientific causal relationship. However, mass media has a great influence on the public during the period of crisis of infectious diseases.56 It is very important to establish a systematic surveillance protocol for safety as much as the effectiveness of vaccines.
Major countries are operating vaccine safety monitoring systems, but are strengthening their organizations and systems specifically to respond to COVID-19. The United States has already established a surveillance system, such as V-safe,57 and the baseline of adverse reactions is constantly being monitored and measured through the vaccine safety datalink.58 The UK collects vaccine adverse events through the ‘yellow card scheme’ and has created a specialized internet-based reporting tool for COVID-19. Internet-based adverse event reporting tools are also actively being used in Israel and other countries. Canada and Australia are building adverse reaction monitoring systems using mobile phone apps and short message services (Table 5).
Table 5. Vaccine safety monitoring and management in major countries.
| Countries | Surveillance system | Operating entity | Function | |
|---|---|---|---|---|
| USA59 | Existing safety monitoring systems | CDC | As people get vaccinated, CDC, FDA, and other federal partners will use the Existing Safety Monitoring Systems to conduct ongoing safety monitoring. | |
| General public; members of the military; veterans; tribal nations | FDA | Expanded Safety Monitoring Systems add an extra layer of safety monitoring, giving CDC and FDA the ability to evaluate COVID-19 vaccine safety in real time and make sure COVID-19 vaccines are safe. | ||
| Expanded safety monitoring systems | DOD | |||
| • CDC: V-safe | VA | |||
| • CDC: National Healthcare Safety Network | IHS | |||
| • FDA: Other large insurer/payer databases | ||||
| UK60 | The Yellow Card Scheme | The Medicines and Healthcare products Regulatory Agency | The system collects and monitors information on safety concerns about medicines, medical devices and e-cigarettes. This includes all adverse events as well as concerns related to product quality or counterfeit products. System contains COVID-19 yellow card reporting page. | |
| Germany61 | • Routine pharmacovigilance | Paul-Ehrlich-Institut responsible for monitoring the safety of vaccines and biomedicines. | Routine pharmacovigilance is based on established real-time monitoring of possible side effects. Smartphone app (SafeVac 2.0) will prospectively track the frequency and severity of adverse effects. | |
| • SafeVac 2.0 | ||||
| Australia62,63 | Passive surveillance | TGA | TGA collects reports of suspected side effects from health professionals and consumers and analyses them to detect signals for possible safety issues. | |
| • AEFI (adverse events following immunisation) | Some people who receive COVID-19 vaccines will be sent follow-up SMS messages with a survey to ask if they have experienced any potential side effects. | |||
| • DAEN (Database of Adverse Event Notifications) | ||||
| Active surveillance | ||||
| • AusVaxSafety | ||||
| • PAEDS (Paediatric Active Enhanced Disease Surveillance) | ||||
| Canada64 | CAEFISS | Public Health Agency of Canada | The system is a FPT public health post-market vaccine safety surveillance system. CAEFISS includes both passive (spontaneous reports from FPTs) and active surveillance. | |
| France65 | Pharmacovigilance | l'Agence nationale de sécurité du médicament et des produits de santé | The system monitor how well people are tolerating the new vaccines. And collects unwanted side-effects. | |
| Sweden66 | Suspected adverse reaction reports | MPA | Suspected adverse reaction reports are sent to the MPA by patients, consumers or health and welfare professionals. This can be done via electronic or paper forms or directly from health and welfare care record systems. | |
| Saudi Arabia67 | Sehhaty app | MOH | Saudi Arabia monitors side effects through mobile app, phone calls. | |
| The nearest medical facility | ||||
| 937 Call center | ||||
| Israel35 | Reporting an adverse event during or after COVID-19 vaccination | MOH | People can report any adverse event during or after getting coronavirus (COVID-19) vaccine through online form. | |
CDC = Centers for Disease Control and Prevention, FDA = Food and Drug Administration, DOD = Department of Defense, VA = Department of Veterans Affairs, IHS = Indian Health Service, COVID-19 = coronavirus disease 2019, TGA = Therapeutic Goods Administration, CAEFISS = The Canadian Adverse Events Following Immunization Surveillance System, FPT = federal, provincial and territorial, MPA = Swedish Medical Products Agency, MOH = Ministry of Health.
CHANGES AFTER STARTING VACCINATION
Even if vaccination begins this month, the social impact of COVID-19 will continue for the time being. Of course, by the first half of the year, most of the healthcare workers and elderlies living in long-term care facilities will be vaccinated; therefore, the death toll will decrease rapidly and the sustainability of the medical system will be guaranteed. However, even if herd immunity is established in November 2021, SARS-CoV-2 will not disappear from our society. The outbreak of clusters will go on, and SARS-CoV-2 will continue attacking the weakest link in society.68
Virus variants
Another factor that makes us impatient is the influx of worrisome variants. The VOC B.1.1.7, discovered in the UK, has been proven to have a faster propagation speed and is a dominant variant in Europe.69 It was also confirmed that the VOC found in South Africa reduced the effectiveness of the vaccine.8 Another VOC was also found in Brazil,70 and although this mutation was found in different countries, mutations in the same region were observed through convergent evolution. In other words, the global epidemic and its response act as selective pressures, and there is also a possibility of the acceleration of viral mutation. Viral mutations will continue if the pandemic persists, and humanity must strive for vaccination and worldwide dissemination. In addition, the ability of the vaccine platform to respond to the VOC should be utilized to the fullest, and evidence for boosting doses should be quickly accumulated.71
It is also necessary to make efforts to respond to the VOC of Korea itself. Korea already mandates the submission of diagnostic tests at the time of entry and polymerase chain reaction tests at the time of quarantine release for overseas travelers, and scientific evidence has already been accumulated.72 However, in addition to blocking overseas inflows, efforts to monitor the mutation of SARS-CoV-2 in Korea should continue. After all, viral mutation is a probabilistic problem.
Non-pharmaceutical interventions
Social distancing, epidemiological investigation, and diagnostic testing should be continued until the acquisition of herd immunity. In response to COVID-19, Korea is actively using non-pharmaceutical interventions, such as stepwise social distancing.2,73 In the first half of 2021, since vaccinations would not be available to the general population, social distancing should be followed until sufficient vaccination is achieved for the general population. However, social distancing entails enormous economic damage. In particular, at the end of the third wave, authorities and policymakers are facing opposition from small business owners and self-employed people. Pandemics are accompanied by serious socio-economic damage as well as the burden of diseases itself. Furthermore, policies, such as social distancing, increase damage. In countries that enforce strong social distancing, such as a lock-down, financial support is provided for the affected sectors (Table 6). Korea also needs a proactive approach regarding this.
Table 6. Financial support for affected sectors in different countries.
| Countries | Supporting program | Detailed description | |
|---|---|---|---|
| UK74 | Self-Employment Income Support Scheme | • For self-employed people whose businesses have been adversely affected by COVID-19 | |
| • The first round of grants, for which claims closed on July 13, 2020 | |||
| - Up to 80% of average monthly trading profits | |||
| - For a period of 3 months, capped at an overall maximum of £7,500 | |||
| • The second round of grants, for which claims opened on August 17, 2020 and closed on October 19 | |||
| - Up to 70% of average monthly trading profits | |||
| - For a period of three months, capped at an overall maximum of £6,570 | |||
| • The third round of grants, for which applications opened on November 30, 2020 and will close on January 29, 2021, covers the period from the start of November 2020 until January 29, 2021 | |||
| - Up to 80% of average monthly trading profits | |||
| - For a period of 3 mon, capped at an overall maximum of £7,500 | |||
| • The fourth grant covering February 2021 to April 2021 | |||
| US75 | Paycheck Protection program | • Provides funds to pay up to 8 weeks of payroll costs, including benefits | |
| • Eligible | |||
| - Self-employed, nonprofits, veterans' organizations, tribal concerns, individuals, sole proprietorships, independent contractors | |||
| France76 | Solidarity Fund (Fond de Solidarité) | • Benefit from a direct tax rebate | |
| - If facing payment difficulties related to the virus, spread or defer payment of tax debt | |||
| - In the most difficult situations, a remission of direct taxes | |||
| - Postponing the deadline for payment of cotisation paid by self-employed | |||
| • Solidarity fund of up to €1,500 per month | |||
| • Interest-free loans with a national guarantee up to 25% of the annual income reported as of the previous year | |||
| - Repaid after 1 yr | |||
| Japan | Employment support fund77 | • Based on the average wage and the payment rate of vacation pay | |
| - Limit is 15,000 yen per person (per day) | |||
| Rent support fund78 | • Support rent fees for difficulty continuing business due to COVID-19 | ||
| - Decreased by more than 50% compared to the same month of the previous year | |||
| - Decreased by more than 30% compared to then same period of last year for consecutive 3 mon | |||
| • Up to 6 months of then rental fee | |||
| • Maximum 5 million yen for corporations | |||
| - 2.5 million yen for individual businesses | |||
| Germany79 | Soforthilfe (emergency aid program) | • Emergency aid program worth 50 billion euros | |
| • The temporary support will reimburse: | |||
| - 80 per cent of fixed costs, where turnover has dropped by more than 70 per cent | |||
| - 50 per cent where turnover has dropped by between 50 and 70 per cent | |||
| - 40 per cent where turnover has dropped by at least 40 and less than 50 per cent | |||
| - The maximum support is 150,000 euros for three months. | |||
| - For companies with up to 5 employees, the maximum sum that can be reimbursed is 9,000 euros for 3 mon. | |||
| - For companies with up to 10 employees, the maximum sum that can be reimbursed is 15,000 euros for 3 mon. | |||
| - In exceptional and justified cases – small businesses with extremely high fixed costs – support may be granted more than these ceilings. | |||
| • No obligation to repay it in the future. | |||
| Australia | Coronavirus supplement80 | • Subsidy for equivalent to $550 per 2 wk ($275 per wk) | |
| - Self-employed persons whose business is closed because of a decrease in customers or whose income has decreased. | |||
| Increasing the instant asset write-off81 | • From March 12, 2020 until December 31, 2020, the instant asset is written off: | ||
| - Threshold is $150,000 (up from $30,000). | |||
| - Eligibility range covers businesses with an aggregated turnover of less than $500 million (up from $50 million). | |||
| JobMaker Hiring Credit80 | • The JobMaker Hiring Credit will be: | ||
| - $200 per wk for each eligible employee aged 16 to 29 | |||
| - $100 per wk for each eligible employee aged 30 to 35 | |||
| Boosting cash flow for employers80 | • Providing up to $100,000 to eligible small and medium sized businesses and not-for-profits | ||
| Taiwan82 | Subsidy program for the self-employed | • Receive NT$10,000 (EUR 330) for up to 3 mon | |
| - Taiwan citizenship | |||
| - Enrolled in the labor insurance scheme through a professional union on or before March 31, 2020 | |||
| - Salary in March 2020 was NT$24,000 (EUR 700) or less | |||
| - Taxable income in 2018 was NT$408,000 (EUR 12,200) or less | |||
COVID-19 = coronavirus disease 2019, NT = New Taiwan dollar.
As epidemiological data on COVID-19 have accumulated, evidence has suggested that COVID-19 is less severe in adolescents and infants,83 and that its transmission in schools is not serious in Korea.84 Therefore, we can carefully consider resuming in-person classes as part of social reopening. In addition, vaccine trials for pregnant women and adolescents under the age of 18 are already in progress in the US and UK. To achieve sufficient herd immunity and prepare for social reopening, we need to secure additional vaccine supply and prepare scientific evidence to increase the indication of vaccines for adolescents, pregnant women, and children in the second half of this year with the results of overseas clinical trials and approval status.
‘Test and trace’ was the driving force to prevent a large-scale outbreak in Korea despite the continuing community transmission. However, diagnostic tests and epidemiological investigations are carried out by human power, and it is essential to consider continuously exhausting human resources. In addition, cases of not actively participating in epidemiological investigations or interfering with epidemiological investigations are increasing. This means that prior to demanding active participation of citizens, legal and ethical considerations, such as personal information protection, should be sufficiently undertaken in the epidemiological investigation process.
CONCLUSION
The COVID-19 pandemic still has a long way to run and just passed another turning point. The emergence of outbreak waves and VOCs during the hope of establishing herd immunity through vaccination is making the situation difficult. However, transparent communication and rational decision-making based on scientific evidence will be a beacon in overcoming this crisis.
ACKNOWLEDGMENTS
I am grateful to Professor Rugyeom Lee of Gachon University and Ms. Munkhzul Radnaabaatar, who helped collect and review the data in the article. In addition, I thank In Joong Kim, DVM, MS, PhD, DACVP and Tae Hyung Kim of Theragen Bio Co., Ltd. for providing the idea of the review.
Footnotes
Funding: This study was supported by grants for drawing figures and collecting review materials from the Gachon University Gil Medical Center (grant numbers 2019–11). The sponsors of the study were not involved in the study design, analysis, interpretation of data, and writing of the report; or the decision to submit the findings of the study for publication.
Disclosure: The author has no potential conflicts of interest to disclose.
References
- 1.McLellan A, Godlee F. Covid 19: Christmas relaxation will overwhelm services. BMJ. 2020;371:m4847. doi: 10.1136/bmj.m4847. [DOI] [PubMed] [Google Scholar]
- 2.Park Y, Huh IS, Lee J, Kang CR, Cho SI, Ham HJ, et al. Application of testing-tracing-treatment strategy in response to the COVID-19 outbreak in Seoul, Korea. J Korean Med Sci. 2020;35(45):e396. doi: 10.3346/jkms.2020.35.e396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mummert A, Weiss H, Long LP, Amigó JM, Wan XF. A perspective on multiple waves of influenza pandemics. PLoS One. 2013;8(4):e60343. doi: 10.1371/journal.pone.0060343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Korea Centers for Disease Control & Prevention. Free Vaccination for All Citizens of COVID-19 to Return to Daily Life. Cheongju: Korea Centers for Disease Control & Prevention; 2021. [Google Scholar]
- 5.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27):2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R, et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2020;384(5):403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson & Johnson. Johnson & Johnson announces single-shot Janssen COVID-19 vaccine candidate met primary endpoints in interim analysis of its Phase 3 ENSEMBLE Trial. [Cited Feb 1, 2021]. Available from: https://www.jnj.com/johnson-johnson-announces-single-shot-janssen-covid-19-vaccine-candidate-met-primary-endpoints-in-interim-analysis-of-its-phase-3-ensemble-trial.
- 8.Novavax. Novavax COVID-19 Vaccine Demonstrates 89.3% Efficacy in UK Phase 3 Trial. Published January 28, 2021. [Accessed Jan 31, 2021]. Available from: https://ir.novavax.com/news-releases/news-release-details/novavax-covid-19-vaccine-demonstrates-893-efficacy-uk-phase-3.
- 9.Muik A, Wallisch AK, Sänger B, Swanson KA, Mühl J, Chen W, et al. Neutralization of SARS-CoV-2 lineage B.1.1.7 pseudovirus by BNT162b2 vaccine-elicited human sera. Science. doi: 10.1126/science.abg6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moderna. Moderna COVID-19 vaccine retains neutralizing activity against emerging variants first identified in the U.K. and the Republic of South Africa. [Updated 2021]. [Accessed January 25, 2021]. https://investors.modernatx.com/news-releases/news-release-details/moderna-covid-19-vaccine-retains-neutralizing-activity-against.
- 11.Knoll MD, Wonodi C. Oxford-AstraZeneca COVID-19 vaccine efficacy. Lancet. 2021;397(10269):72–74. doi: 10.1016/S0140-6736(20)32623-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Voysey M, Costa Clemens SA, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. A. Single dose administration, and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine. [Updated 2021]. [Accessed January 28, 2021]. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3777268. [DOI] [PMC free article] [PubMed]
- 13.Emary KFW, Golubchik T, Aley PK, Ariani CV, Angus BJ, Bibi S, et al. Efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine against SARS-CoV-2 VOC 202012/01 (B.1.1.7) [Updated 2021]. [Accessed February 9, 2021]. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3779160.
- 14.The Guardian. Study shows Oxford Covid vaccine has less protection against South African variant. [Updated 2021]. [Accessed February 9, 2021]. https://www.theguardian.com/society/2021/feb/07/covid-vaccine-booster-variants-emerge-minister.
- 15.Our World in Data. Coronavirus (COVID-19) vaccinations. [Updated 2021]. [Accessed February 1, 2021]. https://ourworldindata.org/covid-vaccinations.
- 16.The Times of Israel. Vaccine found 92% effective in Israel, in first controlled result outside trials. [Updated 2021]. [Accessed January 28, 2021]. https://www.timesofisrael.com/vaccine-found-92-effective-in-israel-in-first-controlled-result-outside-trials/
- 17.Statistics Korea. COVID-19. [Updated 2021]. [Accessed February 1, 2021]. https://kosis.kr/covid/covid_index.do.
- 18.Kim T. Improving preparedness for and response to coronavirus Disease 19 (COVID-19) in long-term care hospitals in Korea. Infect Chemother. 2020;52(2):133–141. doi: 10.3947/ic.2020.52.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chung H, Kim EO, Kim SH, Jung J. Risk of COVID-19 transmission from infected outpatients to healthcare workers in an outpatient clinic. J Korean Med Sci. 2020;35(50):e431. doi: 10.3346/jkms.2020.35.e431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park C, Hwang JM, Jo S, Bae SJ, Sakong J. COVID-19 outbreak and its association with healthcare workers' emotional stress: a cross-sectional study. J Korean Med Sci. 2020;35(41):e372. doi: 10.3346/jkms.2020.35.e372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Health Organization. Who sage road map for prioritizing uses of COVID-19 vaccines in the context of limited supply. [Updated 2020]. [Accessed January 28, 2021]. https://www.who.int/docs/default-source/immunization/sage/covid/sage-prioritization-roadmap-covid19-vaccines.pdf?Status=Temp&sfvrsn=bf227443_2.
- 22.Dooling K, Marin M, Wallace M, McClung N, Chamberland M, Lee GM, et al. The advisory committee on immunization practices' updated interim recommendation for allocation of COVID-19 Vaccine - United States, December 2020. MMWR Morb Mortal Wkly Rep. 2021;69(5152):1657–1660. doi: 10.15585/mmwr.mm695152e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Joint Committee on Vaccination and Immunisation. Advice on priority groups for COVID-19 vaccination. [Updated 2020]. [Accessed January 28, 2021]. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/950113/jcvi-advice-on-priority-groups-for-covid-19-vaccination-30-dec-2020-revised.pdf.
- 24.Vygen-Bonnet S, Koch J, Bogdan C, Harder T, Heininger U, Kling K, et al. Beschluss der STIKO zur 1. Aktualisierung der COVID-19-Impfempfehlung und die dazugehörige wissenschaftliche Begründung. Epidemiol Bull. 2021;2:64–132. [Google Scholar]
- 25.Australian Technical Advisory Group on Immunisation. Preliminary advice on general principles to guide the prioritisation of target populations in a COVID-19 vaccination program in Australia. [Updated 2020]. [Accessed January 28, 2021]. https://www.health.gov.au/sites/default/files/documents/2020/11/atagi-preliminary-advice-on-general-principles-to-guide-the-prioritisation-of-target-populations-in-a-covid-19-vaccination-program-in-australia_0.pdf.
- 26.National Advisory Committee on Immunization. Guidance on the prioritization of initial doses of COVID-19 vaccine(s) [Updated 2020]. [Accessed January 28, 2021]. https://www.canada.ca/en/public-health/services/immunization/national-advisory-committee-on-immunization-naci/guidance-prioritization-initial-doses-covid-19-vaccines.html.
- 27.French National Authority for Health. COVID-19 vaccines: what prioritization strategy at the start of the campaign? [Updated 2020]. [Accessed January 28, 2021]. https://www.has-sante.fr/jcms/p_3221237/en/vaccins-covid-19-quelle-strategie-de-priorisation-a-l-initiation-de-la-campagne.
- 28.Folkhälsomyndigheten. Nationell plan för vaccinationmot COVID-19. [Updated 2020]. [Accessed January 28, 2021]. https://www.folkhalsomyndigheten.se/contentassets/f8703f0a29cc408fb788b60f87289e5b/nationell-plan-vaccination-covid-19.pdf.
- 29.The Local. COVID-19: what's Sweden's priority list for the vaccine? [Updated 2020]. [Accessed January 28, 2021]. https://www.thelocal.se/20201209/covid-19-whats-swedens-priority-list-for-the-vaccine.
- 30.Japantimes. Japan's COVID-19 vaccine plan prioritizes health care workers and older residents. [Updated 2020]. [Accessed January 28, 2021]. https://www.japantimes.co.jp/news/2020/12/25/national/japan-vaccine-older-people/
- 31.Washingtonpost. Outpacing Trump's operation warp speed, China to give coronavirus vaccine to 50 million in a month. [Updated 2021]. [Accessed January 28, 2021]. https://www.washingtonpost.com/world/asia_pacific/coronavirus-vaccine-china-lunar-new-year/2021/01/04/d9401354-4e34-11eb-a1f5-fdaf28cfca90_story.html.
- 32.Ministry of Health. Everything you need to know COVID-19 VACCINE. [Updated 2020]. [Accessed January 28, 2021]. https://www.moh.gov.sa/awarenessplateform/VariousTopics/Documents/COVID-19Vaccine-English.pdf.
- 33.Ministry of Health. News. MOH announces priority groups for COVID-19 vaccination; [Updated 2020]. [Accessed January 28, 2021]. https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2020-12-15-008.aspx. [Google Scholar]
- 34.Ministry of Health, Division of Epidemiology. COVID-19 vaccine priorities. [Updated 2020]. [Accessed January 28, 2021]. https://www.gov.il/BlobFolder/news/16122020-01/he/NEWS_Corona_corona-vaccine-priorities.pdf.
- 35.Ministry of Health. COVID-19 vaccination information. [Updated 2021]. [Accessed January 28, 2021]. https://govextra.gov.il/ministry-of-health/covid19-vaccine/en-covid19-vaccination-information/
- 36.Department of Health & Human Services. Fact sheet: explaining operation warp speed. [Updated 2021]. [Accessed January 28, 2021]. https://www.hhs.gov/coronavirus/explaining-operation-warp-speed/index.html.
- 37.Department of Health & Social Care. UK COVID-19 vaccines delivery plan. [Updated 2021]. [Accessed January 28, 2021]. https://www.gov.uk/government/publications/uk-covid-19-vaccines-delivery-plan/uk-covid-19-vaccines-delivery-plan.
- 38.Robert Koch Institute. COVID-19 and vaccination: Answers to frequently asked questions (FAQ) [Updated 2021]. [Accessed January 28, 2021]. Available from: https://www.rki.de/SharedDocs/FAQ/COVID-Impfen/gesamt.html.
- 39.Australian Government. Australia's COVID-19 vaccine national roll-out strategy. [Updated 2021]. [Accessed January 28, 2021]. https://www.health.gov.au/resources/publications/australias-covid-19-vaccine-national-roll-out-strategy.
- 40.British of Columbia. COVID-19 immunization plan. [Updated 2021]. [Accessed January 28, 2021]. https://www2.gov.bc.ca/gov/content/safety/emergency-preparedness-response-recovery/covid-19-provincial-support/vaccines.
- 41.Ontario. Ontario expands COVID-19 vaccine locations. [Updated 2020]. [Accessed January 28, 2021]. https://news.ontario.ca/en/release/59753/ontario-expands-covid-19-vaccine-locations.
- 42.Ministère des solidarités, de la santé. The vaccine strategy. [Updated 2020]. [Accessed January 28, 2021]. https://solidarites-sante.gouv.fr/grands-dossiers/la-vaccination-contre-la-covid-19/article/la-strategie-vaccinale.
- 43.Riyadh- Asharq Al-Awsat. High registration turnout to receive COVID-19 vaccine in Saudi Arabia. [Updated 2021]. [Accessed January 28, 2021]. https://english.aawsat.com/home/article/2751411/high-registration-turnout-receive-covid-19-vaccine-saudi-arabia.
- 44.Ministry of Health. The Minister of Health held tonight (Monday) a status assessment at the vaccine control center. [Updated 2020]. [Accessed January 28, 2021]. https://www.gov.il/en/departments/news/21122020-05.
- 45.The Wall Street Journal. U.S. starts delivery of Moderna's COVID-19 vaccine. [Updated 2020]. [Accessed January 28, 2021]. https://www.wsj.com/articles/u-s-starts-rollout-of-modernas-covid-19-vaccine-11608460200.
- 46.CNBC. Pfizer CNBC's COVID vaccine is now shipping. Here's how the U.S. plans to deliver it. [Updated 2020]. [Accessed January 28, 2021]. https://www.cnbc.com/2020/12/12/how-fedex-ups-plan-to-distribute-fda-approved-covid-vaccine-when-will-you-get-the-coronavirus-vaccine.html.
- 47.Department of Health. Contracts signed for roll out of COVID-19 vaccine. [Updated 2020]. [Accessed January 28, 2021]. https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/contracts-signed-for-rollout-of-covid-19-vaccine.
- 48.Government of Canada. Canada's COVID-19 immunization plan: saving lives and livelihoods. [Updated 2020]. [Accessed January 28, 2021]. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/canadas-reponse/canadas-covid-19-immunization-plan.html.
- 49.CDC COVID-19 Response Team; Food and Drug Administration. Allergic reactions including anaphylaxis after receipt of the first dose of Pfizer-BioNTech COVID-19 vaccine—United States, December 14–23, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(2):46–51. doi: 10.15585/mmwr.mm7002e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cabanillas B, Akdis C, Novak N. Allergic reactions to the first COVID-19 vaccine: a potential role of Polyethylene glycol? Allergy. doi: 10.1111/all.14711. [DOI] [PubMed] [Google Scholar]
- 51.CDC. Interim clinical considerations for use of mRNA COVID-19 vaccines currently authorized in the United States. [Updated 2021]. [Accessed January 28, 2021]. https://www.cdc.gov/vaccines/covid-19/info-by-product/clinical-considerations.html.
- 52.Culbreth MJ, Biryukov SS, Shoe JL, Dankmeyer JL, Hunter M, Klimko CP, et al. The use of analgesics during vaccination with a live attenuated Yersinia pestis vaccine alters the resulting immune response in mice. Vaccines (Basel) 2019;7(4):205. doi: 10.3390/vaccines7040205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saleh E, Moody MA, Walter EB. Effect of antipyretic analgesics on immune responses to vaccination. Hum Vaccin Immunother. 2016;12(9):2391–2402. doi: 10.1080/21645515.2016.1183077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Iwasaki A. What reinfections mean for COVID-19. Lancet Infect Dis. 2021;21(1):3–5. doi: 10.1016/S1473-3099(20)30783-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jung J. Epidemiologic evaluation and risk communication regarding the recent reports of sudden death after influenza vaccination in the COVID-19 pandemic. J Korean Med Sci. 2020;35(41):e378. doi: 10.3346/jkms.2020.35.e378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee YR, Lee JY, Park IH, Kim M, Jhon M, Kim JW, et al. The relationships among media usage regarding COVID-19, knowledge about infection, and anxiety: Structural model analysis. J Korean Med Sci. 2020;35(48):e426. doi: 10.3346/jkms.2020.35.e426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.CDC. V-safe after vaccination health checker. [Updated 2021]. [Accessed February 1, 2021]. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/vsafe.html.
- 58.CDC. Vaccine safety Datalink (VSD) [Updated 2020]. [Accessed February 1, 2021]. https://www.cdc.gov/vaccinesafety/ensuringsafety/monitoring/vsd/index.html.
- 59.CDC. Ensuring the safety of COVID-19 vaccines in the United States. [Updated 2021]. [Accessed February 1, 2021]. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety.html.
- 60.Parliament UK. Monitoring COVID-19 vaccine safety in national immunisation programmes. [Updated 2021]. [Accessed February 1, 2021]. https://post.parliament.uk/monitoring-covid-19-vaccine-safety-in-national-immunisation-programmes/
- 61.Paul-Ehrlich-Institut. Coronavirus and COVID-19. [Updated 2021]. [Accessed February 1, 2021]. https://www.pei.de/EN/newsroom/dossier/coronavirus/coronavirus-content.html;jsessionid=19526C06D00953CBA2E1084998E29C87.intranet232?nn=164146&cms_pos=5.
- 62.National Centre for Immunisation Research and Surveillance. Vaccine safety. [Updated 2020]. [Accessed February 1, 2021]. https://www.ncirs.org.au/health-professionals/vaccine-safety.
- 63.Australian Government. COVID-19 vaccine: information for consumers and health professionals. [Updated 2021]. [Accessed February 1, 2021]. https://www.tga.gov.au/covid-19-vaccine-information-consumers-and-health-professionals#report-side-effect.
- 64.Government of Canada. Canadian Adverse Events Following Immunization Surveillance System (CAEFISS) [Updated 2019]. [Accessed February 1, 2021]. https://www.canada.ca/en/public-health/services/immunization/canadian-adverse-events-following-immunization-surveillance-system-caefiss.html.
- 65.The Connexion. COVID-19 vaccine in France: side-effect monitoring increased. [Updated 2021]. [Accessed February 1, 2021]. https://www.connexionfrance.com/French-news/Covid-19-vaccine-in-France-Side-effect-monitoring-increased-as-vaccination-rolled-out.
- 66.Swedish Medical Products Agency. Management of suspected adverse reaction reports. [Updated 2020]. [Accessed February 1, 2021]. https://www.lakemedelsverket.se/en/reporting-adverse-reactions-events-and-incidents/suspected-adverse-reactions-from-medicinal-products/medicinal-products-for-humans/management-of-suspected-adverse-reaction-reports.
- 67.Ministry of Health. COVID-19 vaccine FAQs. [Updated 2021]. [Accessed February 1, 2021]. https://articlesen.covid19awareness.sa/COVID-19-Vaccine-FAQs.
- 68.Jung J, Noh JY, Cheong HJ, Kim WJ, Song JY. Coronavirus disease 2019 outbreak at nightclubs and distribution centers after easing social distancing: vulnerable points of infection. J Korean Med Sci. 2020;35(27):e247. doi: 10.3346/jkms.2020.35.e247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Volz E, Mishra S, Chand M, Barrett JC, Johnson R, Geidelberg L, et al. Transmission of SARS-CoV-2 Lineage B.1.1.7 in England: insights from linking epidemiological and genetic data. [Updated 2021]. [Accessed February 1, 2021]. https://www.medrxiv.org/content/10.1101/2020.12.30.20249034v2.
- 70.Naveca F, Nascimento V, Souza V, Corado A, Nascimento F, Silva G, et al. Phylogenetic relationship of SARS-CoV-2 sequences from Amazonas with emerging Brazilian variants harboring mutations E484K and N501Y in the Spike protein. [Updated 2021]. [Accessed February 1, 2021]. https://virological.org/t/phylogenetic-relationship-of-sars-cov-2-sequences-from-amazonas-with-emerging-brazilian-variants-harboring-mutations-e484k-and-n501y-in-the-spike-protein/585.
- 71.Tanne JH. COVID-19: Moderna plans booster doses to counter variants. BMJ. 2021;372(232):n232. doi: 10.1136/bmj.n232. [DOI] [PubMed] [Google Scholar]
- 72.Jung J, Jang H, Kim HK, Kim J, Kim A, Ko KP. The importance of mandatory COVID-19 diagnostic testing prior to release from quarantine. J Korean Med Sci. 2020;35(34):e314. doi: 10.3346/jkms.2020.35.e314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Park IN, Yum HK. Stepwise strategy of social distancing in Korea. J Korean Med Sci. 2020;35(28):e264. doi: 10.3346/jkms.2020.35.e264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gov UK. Check if you can claim a grant through the self-employment income support scheme. [Updated 2021]. [February 2, 2021]. https://www.gov.uk/guidance/claim-a-grant-through-the-coronavirus-covid-19-self-employment-income-support-scheme#other-help-you-can-get/
- 75.Coronavirus.gov. How do I apply for small business or self-employment benefits? [Updated 2020]. [February 2, 2021]. https://faq.coronavirus.gov/how-to-apply-for-benefits/
- 76.de l'Économie M. des Finances et de la Relance. Coronavirus COVID-19: Soutien aux entreprises. [Updated 2021]. [February 2, 2021]. https://www.economie.gouv.fr/covid19-soutien-entreprises/fonds-de-solidarite-pour-les-tpe-independants-et-micro#/
- 77.General KP. Information. [Updated 2021]. [Accessed February 2, 2021]. https://home.kpmg/xx/en/home/insights/2020/04/japan-government-and-institution-measures-in-response-to-covid.html.
- 78.Kyodo News. Japan's ruling bloc agrees on rent relief plan for virus-hit firms. [Updated 2020]. [Accessed February 2, 2021]. Available from: https://english.kyodonews.net/news/2020/05/cfd002fb6b3c-update1-japans-ruling-bloc-agrees-on-rent-relief-plan-for-virus-hit-firms.html.
- 79.The Federal Government. Temporary support for small and medium businesses. [Updated 2020]. [Accessed February 2, 2021]. https://www.bundesregierung.de/breg-en/search/ueberbrueckungshilfe-1760136.
- 80.Australian Government. Government response to coronavirus. [Updated 2020]. [Accessed February 2, 2021]. https://guides.dss.gov.au/guide-social-security-law/coronavirus.
- 81.Australian Taxation Office. Instant asset write-off for eligible businesses. [Updated 2020]. [Accessed February 2, 2021]. https://www.ato.gov.au/Business/Depreciation-and-capital-expenses-and-allowances/Simpler-depreciation-for-small-business/Instant-asset-write-off/
- 82.Lexology. Taiwan: COVID-19 relief measures for employees. [Updated 2020]. [Accessed February 2, 2021]. https://www.lexology.com/library/detail.aspx?g=83f1285d-94f4-4b0e-8e48-fe36bf7017aa.
- 83.Yoon Y, Kim KR, Park H, Kim S, Kim YJ. Stepwise school opening and an impact on the epidemiology of COVID-19 in the children. J Korean Med Sci. 2020;35(46):e414. doi: 10.3346/jkms.2020.35.e414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kim EY, Ryu B, Kim EK, Park YJ, Choe YJ, Park HK, et al. Children with COVID-19 after reopening of schools, South Korea. Pediatr Infect Vaccine. 2020;27(3):180–183. [Google Scholar]