Abstract
Objective
To compare the clinical and radiographic effectiveness of A PRF Plus as an adjuctive material to osseous bone graft in socket preservation and ridge augmentation.
Methods
Twenty patients with need to preserve extraction socket in non-molar sites planning for further prosthetic rehabilitation were divided into two groups. Test Group (Group A) was treated with A PRF Plus membrane and Sybograf plus ™ (70% HA and 30 %β TCP) bone graft. The Control Group (Group B) was treated with Sybograf plus ™ (70% HA and 30% βTCP) bone graft. Both groups had same socket preservation surgical technique.
Results
Both Group A and Group B showed significant improvement in clinical and radiographic parameters. Mean socket length, Vertical Resorption reduction in Group A was 1.48 whereas in Group B was 1.67 which is statistically significant. (p ≤ 0.05). Changes in Horizontal width reduction at 1,3, and 5 mm depth of the socket for both groups were not statistically significant. The Gain in socket fill for Group A and B 6 months postoperatively was 1185.30HU ± 473.21 and 966.60 HU ± 273.27 respectively. But intergroup comparison was not statistically significant. (p = 0.17). There were no significant statistical differences in postoperative pain in Group A and Group B as subjects experienced moderate amount of pain. The assessment of post-operative swelling showed that only 30% subjects in Group A reported with swelling. Whereas 80% subjects in Group B complained of post-operative swelling.
Conclusion
The results of the present study proved utilisation of A PRF Plus as a promising adjunct to conventional regenerative therapy for socket preservation.
Keywords: Extraction socket, Socket preservation, Osseous bone graft, A PRF Plus, Implant, Ridge preservation, Esthetics
1. Introduction
The present study aims to evaluate the clinical and radiographic efficacy of A PRF Plus as an adjunctive material to Osseous bone graft in socket preservation and ridge augmentation. Implant placement though considered as most preferred treatment option for tooth replacement; it is not possible to place implant in all given bone morphology. Improperly managed tooth extraction socket, further adds up to normal bony changes expected during first year after tooth extraction, specifically at first three months, where 2/3 rd of the alveolar bone loss occurs.1
“Preserving the bone’’ during tooth extraction is the major treatment strategy for future implant placement and for aesthetically acceptable fixed/removable prosthesis. Recognition of these clinically substantial alveolar changes after tooth extraction has led to use of numerous materials and techniques to benefit alveolar bone regeneration as well as ameliorate shrinkage. Socket preservation is a therapeutic approach following tooth extraction. This procedure is developed to limit effect of post extraction absorption, maintain hard and soft tissue contour of ridge.2 Also, to boost socket fill and enhance bone quality prior to placement of implant. It aims to maintain stable ridge volume to optimize functional as well as aesthetic outcomes.
Ridge preservation using Guided Bone Regeneration (GBR) technique has shown improvement in ridge width and height dimensions. Various regenerative techniques using bone grafts like autografts, allografts, alloplast and xenografts or in combination with resorbable and non-resorbable membranes have been described by authors for socket preservation.3 Recently, Synthetic nanocrystalline hydroxyapatite and beta-tricalcium phosphate composite is one of the most favoured bone substitutes for periodontal regeneration. It stabilizes coagulum within socket avoiding possible reduction of hard tissue volume essential for bone regeneration.4 Commercially available this type of bone graft (Sybograf Plus) particles is mixed with blood clot in alveolar socket which stimulate osteogenic cells by adhesive glycoprotein, fibronectin and type 1 collagen combined with β-tricalcium promoting osteogenesis.
Recent concepts in periodontal regenerative medicine namely ‘Platelet rich fibrin (PRF)’ are chosen additives for enhanced regeneration. Various studies have delineated potential of plasma concentrates rich in growth factors and cytokines, namely ‘platelet-derived growth factor (PDGF)’, ‘transforming growth factor β’ ‘vascular endothelial growth factor (VEGF)’, and ‘platelet-derived endothelial growth factor (PDEGF)’. These factors stimulate hard and soft tissue repair and regeneration. They have successfully been used in form of membrane for management of socket preservation.5
Recently literature has hypothesized that by reducing centrifugation speed (G-force), an upsurge in leukocyte numbers might be attained within PRF matrix aiding in wound healing process.6 This hypothesis was used for formulation of A-PRF plus which has an increase in several growth factors within the PRF matrix scaffold and facilitated wound healing capacity.
Preserving or reconstructing extraction socket of a failed tooth enhances our ability to achieve ideal functional and aesthetic prosthetic reconstruction following implant therapy. The present study aims to evaluate the efficacy of A PRF Plus with/without Osseous bone graft in socket preservation and ridge augmentation.
2. Material and methods
The IEC number is – 711/2017.
The CTRI registration number is - CTRI/2017/12/010879.
2.1. Subject and selection criteria
The subjects for study were selected from outpatient Department of Periodontology, Manipal College of Dental Sciences, Manipal. Patients with mobile teeth in maxillary anterior region (Incisor to premolar) in need of extraction and willing for implant placement were selected. As all patients are not willing for immediate implant placements, they were recruited for socket preservation and implant placement on later date. The subjects belonged to either sex and were between 20 and 55 years of age. The study was approved by institutional ethical committee, KMC Manipal.
2.2. Inclusion and exclusion criteria
The Inclusion criteria was patients above 20 years of age who are systemically healthy. Patients in need of extraction (Grade III mobility, root stumps) from incisor to premolar in maxilla and willing for implant placement. Patients who do not want to go for immediate implant placement.
The Exclusion criteria was Patients on anti-inflammatory or antibiotics drugs for past 6 months. Patients with abusive habits such as smoking. Patients who are pregnant or lactating and/or any other systemic disease.
2.3. Sample size
Sample size was determined with following method for each group which came out to be 10 per group.
As there were two groups, total sample size of the study was 20.
Repeated Measure ANOVA
4. Methodology
Following screening examination, each participant had received a session of oral prophylaxis and polishing with rubber cup and low abrasive paste including proper oral hygiene instructions. The adjacent tooth at site of interest if carious was restored prior to surgery.
Patients fulfilling the inclusion criteria after extraction of tooth were examined clinically. Intactness of buccal cortical plate was examined and assessed. Site was randomly allocated in two groups using lottery method using envelopes. The Co-investigator was responsible for allocation concealment. The radiographic expert was blinded.
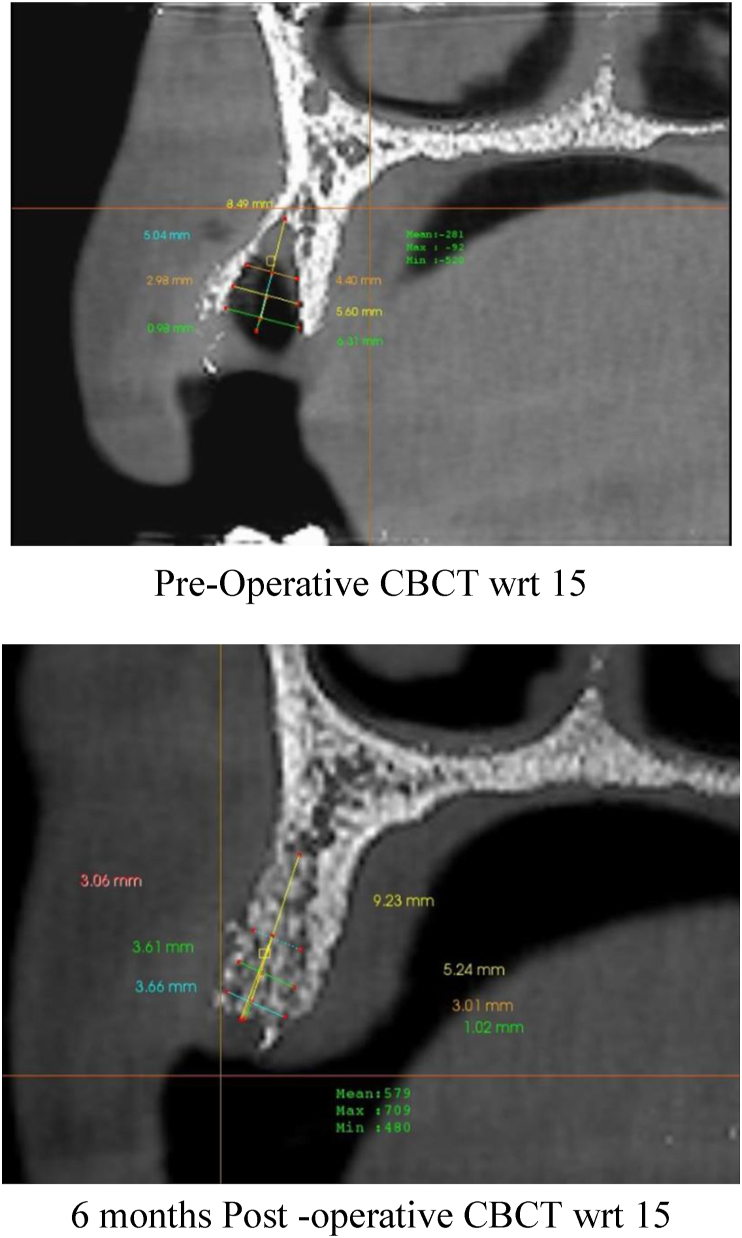
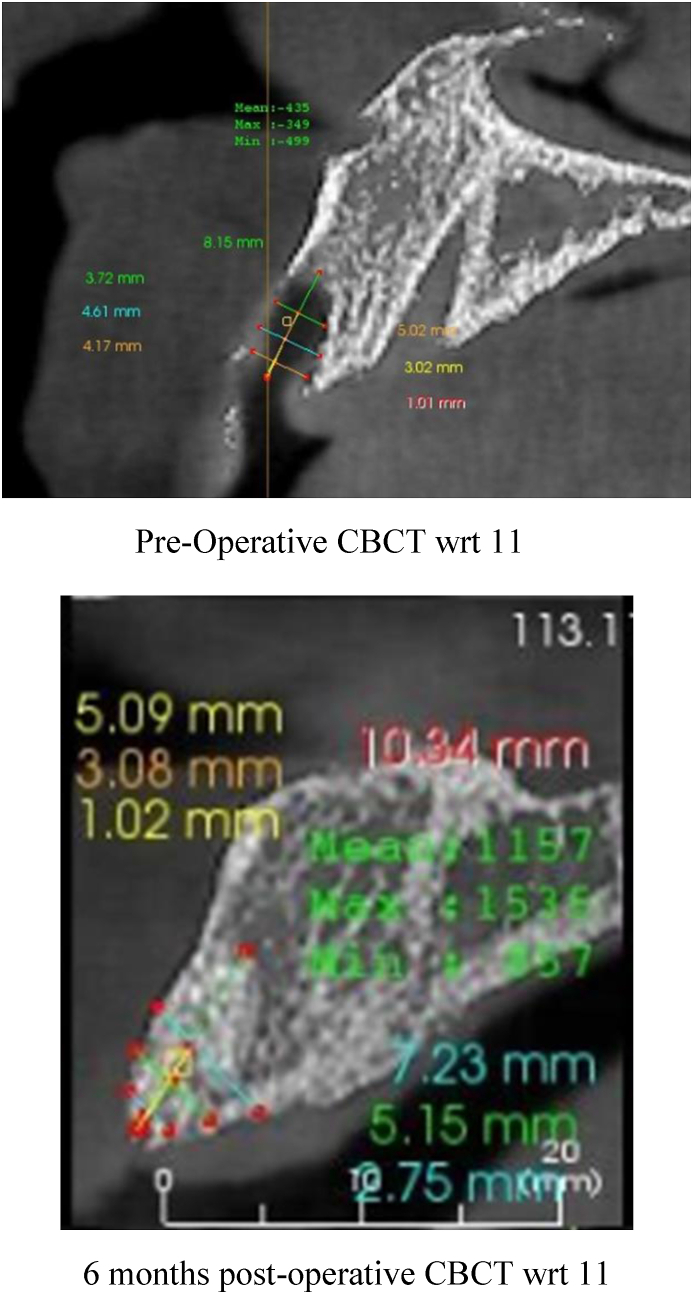
CBCT images were obtained with i-CAT (17–19) unit. CBCTs were taken instantly post extraction (T1) and after 6 months of healing of socket (T2). Exposure parameters were adjusted according to indication of imaging for the patient. Image assessment and measurements were done under standard conditions of illumination by a single trained observer using the Anatomage 5.3 version (In Vivo)
4.1. Software
The measurements were made on the cross-sectional slice using the linear measurement tools.
For standardisation, the measurements were done on a single cross section slice taken at the “centre of the socket’’ The midpoint of the distance between the socket linings was measured (on axial section) and was chosen as the ‘centre of the socket’. Once the centre of the socket was determined, the corresponding cross sectional slice only was used for all the measurements.
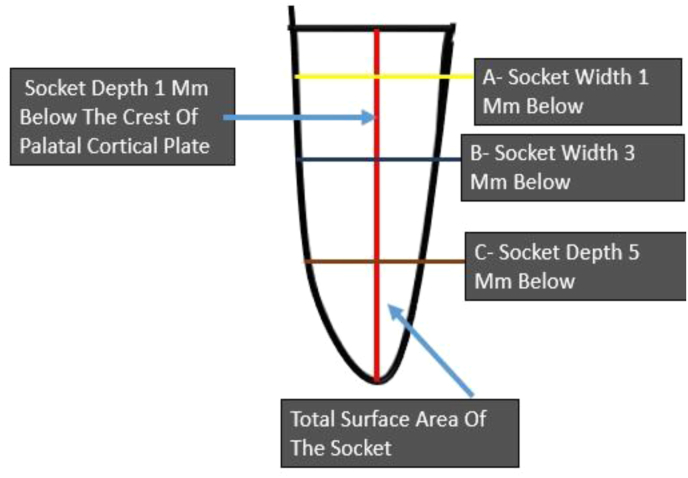
The following measurements at baseline were recorded (Fig. 1a, Fig. 1b).
-
1.
Mean width ridge difference between outer border of buccal and lingual cortical plate at Socket depth at 1, 3,5 mm.
-
2.
Vertical resorption measured by mean difference in length of socket immediately after extraction and 6 months post treatment.
-
3.
Density of extraction socket immediately after extraction and socket fill post treatment measured in Hounsfield units
Fig. 1a.
Schematic Diagram depicting measurements of extraction socket using I CAT CBCT.
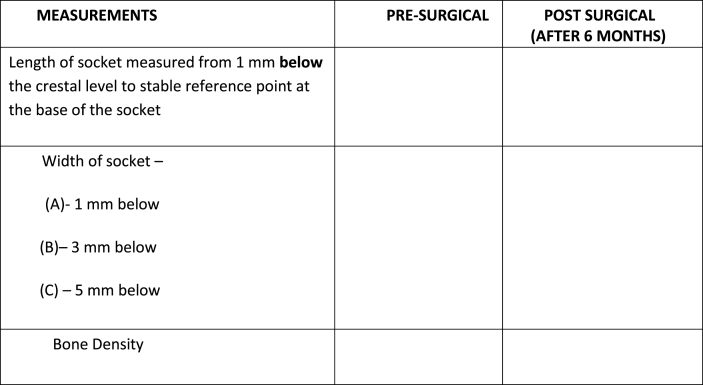
Fig. 1b.
Data collection Proforma.
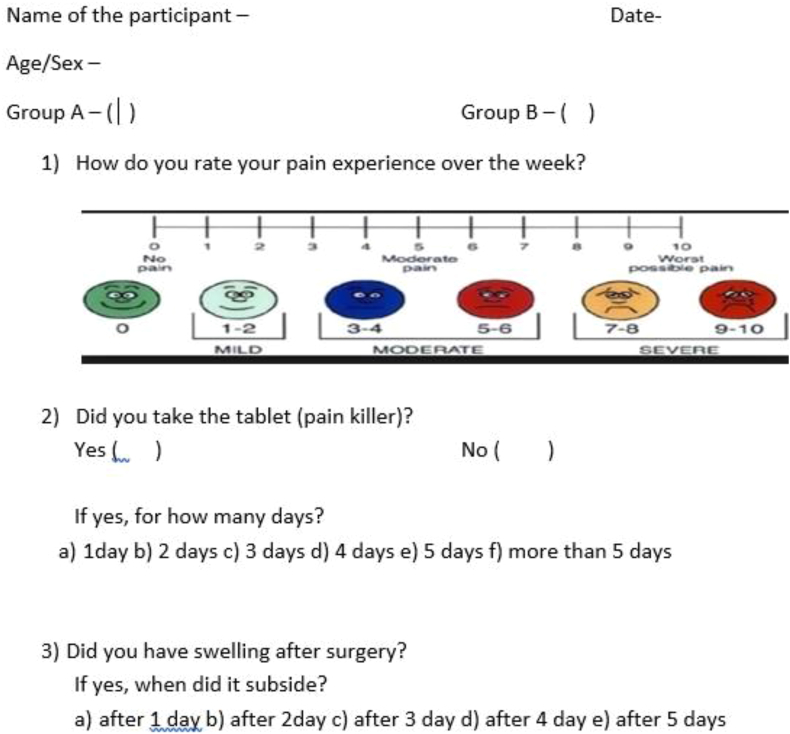
After 6 months the measurements taken by CBCT on day of surgery was repeated. On the day of suture removal, pain assessment was done by Questionnaire (Fig. 2).
Fig. 2.
Qualitative assessment done with Questionnaire.
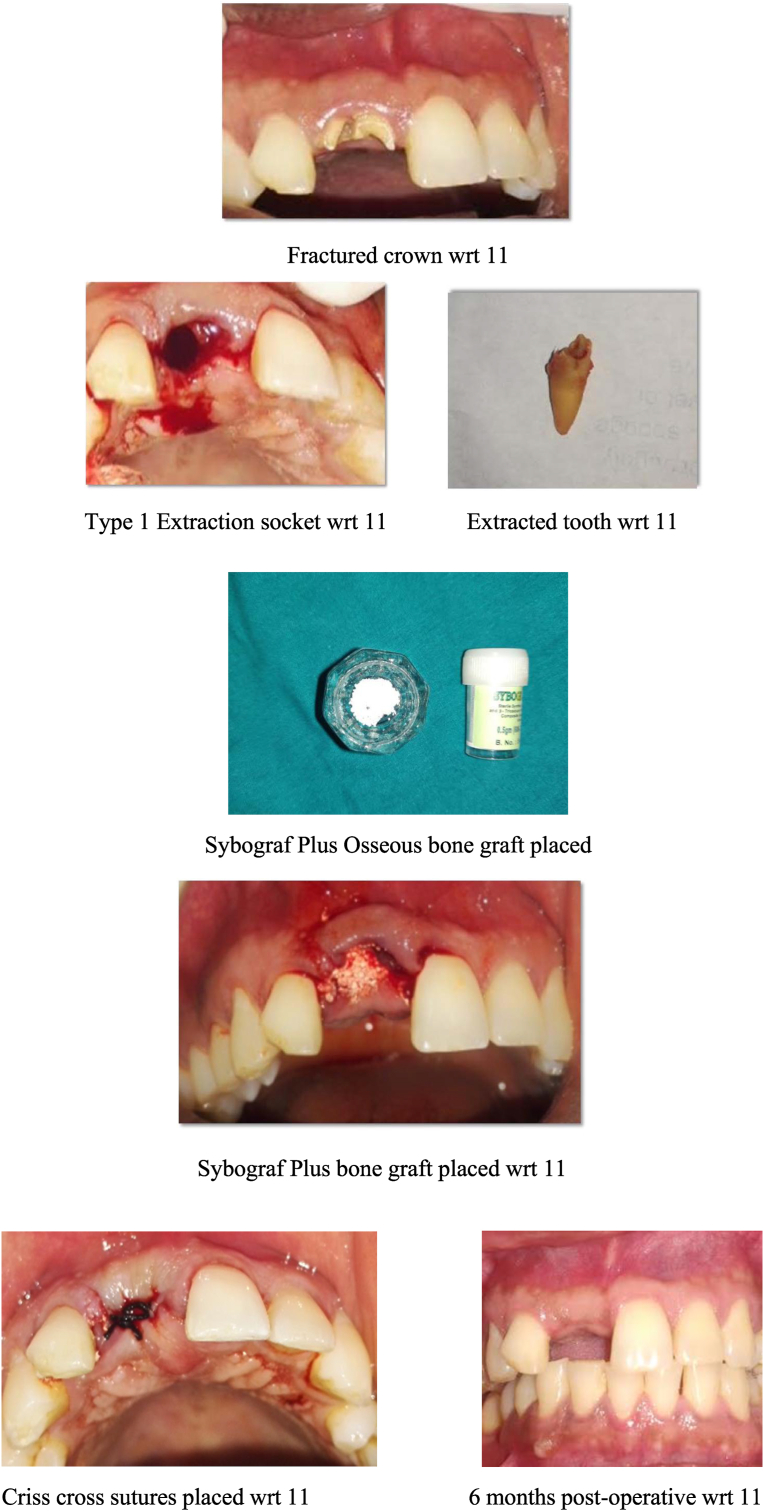
After setting up the armamentarium, area to be operated was anesthetized using 2% lignocaine hydrochloride with 1: 200000 adrenaline by infiltration anaesthesia. Extraction was carried out atraumatically. Subsequent to atraumatic extraction, height of buccal and palatal bone plate was clinically inspected at mid buccal and mid lingual region with aid of periodontal probe. Height was measured till base of socket. This facilitated to measure amount of vertical bone loss on buccal plate in comparison to palatal plate.
Subsequent to extraction Using I-CAT CBCT machine, baseline measurements of the clinical parameters were taken. To assess radiographic parameters, CBCTs were taken instantly post extraction (T1) and after 6 months of healing of socket (T2). Superimposition was done with help of original DICOM data. The measurements as mentioned were assessed in centre of extraction socket in millimetres.
With #15 blade, intrasulcular incision was made elevating marginal gingiva and adjacent interdental papilla. Flap reflection was done by Periosteal elevator resulting in exposure of crestal bone around socket. This aided in direct visualization and measurement of crestal bone level. Bone curette was used to debride extraction socket if granulation tissue is present. Randomization by lottery method was used for dividing sockets into two groups.
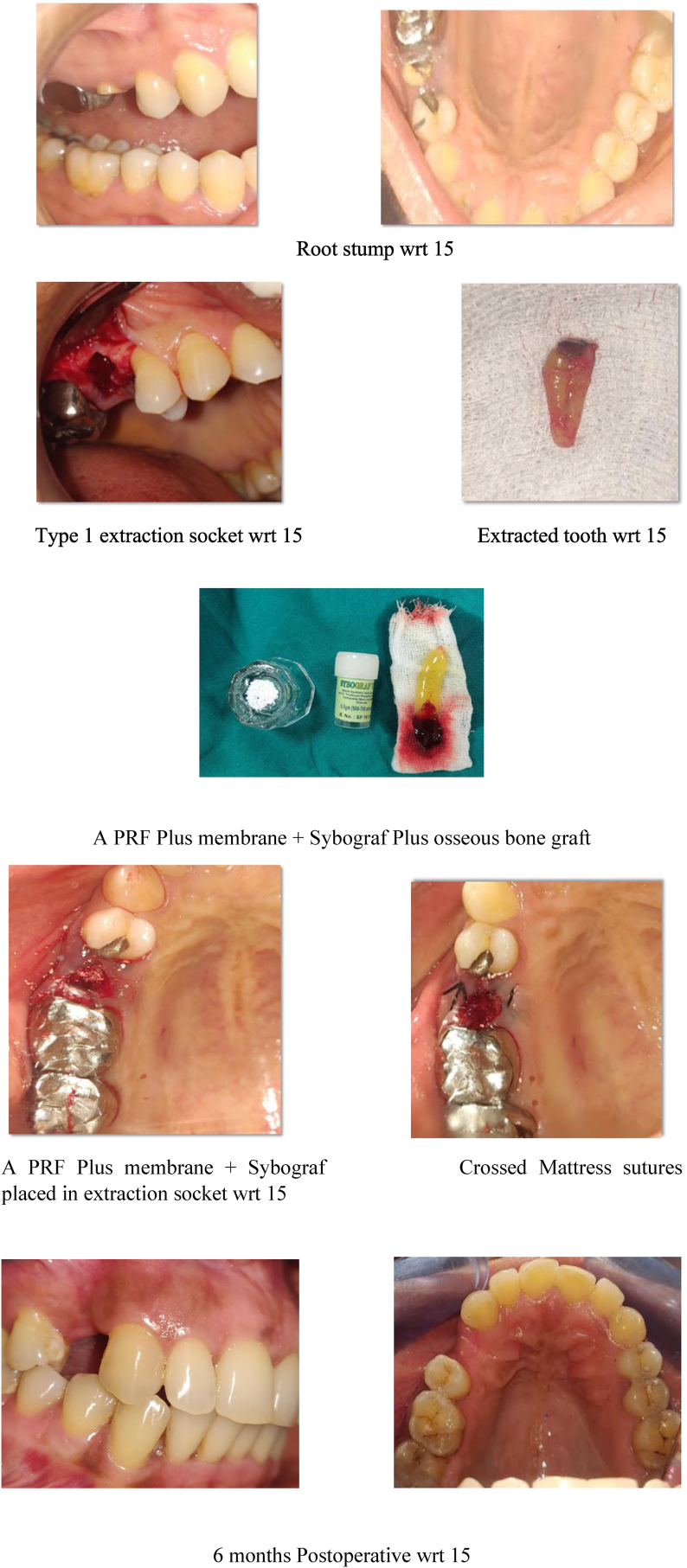
Test Group – Sybograf plus (70% HA and 30% βTCP) mixed with A PRF plus membrane was condensed into extraction socket upto crestal level. Collagen sponge (Collasponge ™) as membrane was utilized to cover graft material (Fig. 3a, Fig. 3b)
Fig. 3a.
Test group – clinical presentation.
Fig. 3b.
Test group – radiographic presentation.
Control Group – Sybograf plus (70% HA and 30% βTCP) was condensed into extraction socket up to crestal level. Collagen membrane was utilized to cover extraction socket.
In the present study a modification protocol ‘The concept of G force’ proposed by Choukroun et al. (2017) was used for preparation of PRF.6 Modification of the original preparation protocol (3000 rpm for 10 min) was done by reducing the applied centrifugation speed and time. Blood samples were collected without anticoagulant in 10-mL tubes. They were instantly centrifuged at 1300 rpm (208 g) for 8 min6 (Fig. 4a, Fig. 4b)
Fig. 4a.
Control group – clinical presentation.
Fig. 4b.
Control group – radiographic presentation.
The bone graft used in the present study is a sterile synthetic nanocrystalline β- Tricalcium phosphate plug (SYBOGRAF Plus-) size of 25 X 8 mm. The bone graft is submerged with patient’s own blood and triturated with a condenser to form a putty.
The flap is approximated with 4–0 non resorbable sutures using conventional crossed mattress suturing technique. All subjects were prescribed with 0.2% chlorhexidine mouthwash two times a day for 2 weeks. Ibuprofen 400 mg twice a day for three days and Amoxicillin 500 mg thrice a day for five days. Sutures were removed 10 days post-operatively. The patients were recalled at 6 months. All the clinical parameters were recorded again and CBCT analysis was repeated.
Statistical analysis was done using SPSS Software. Intragroup Analysis was done by Wilcoxon Sign Test.Intergroup Analysis was done by Mann – Whitney Test.
3. Results
In the present randomised control clinical study, a total of 20 sites in maxilla were selected which where, single non restorable teeth and indicated for extraction. 20 sites were grouped into two, Group A (Test Group -A PRF Plus membrane and Sybograf plus osseous graft) and Group B (Control Group - Sybograf plus osseous graft). The selection of number of sites was according to the WHO sample size calculator for power analysis.
The mean age of patients in Group A (Test Group) was 35 years with 5 female and 5 male patients whereas mean age group in Group B (Control Group) was 35.30 years with 4 female and 6 male patients. The comparison of age between groups showed no statistical difference (Table 1, Table 2). The Group A (Test.
Table 1.
Distribution of the subjects based on gender.
| Group A |
Group B |
|||
|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | |
| Females | 5 | 50.0 | 4 | 40.0 |
| Males | 5 | 50.0 | 6 | 60.0 |
| Total | 10 | 100.0 | 10 | 100.0 |
Table 2.
Distribution of the subjects based on age.
| N | Minimum | Maximum | Mean | Std. Deviation | |
|---|---|---|---|---|---|
| Group A | 10 | 20 | 60 | 35.10 | 13.428 |
| Group B | 10 | 19 | 60 | 35.30 | 12.720 |
Group) was treated with A PRF Plus membrane and Sybograf plus (70% HA and 30% β TCP) bone graft. The Group B (Control Group) was treated with Sybograf plus (70% HA and 30% β TCP) bone graft. Both groups had same socket preservation surgical technique.
The primary outcomes assessed were mean width ridge difference between outer border of buccal and palatal cortical plate at socket depth 1,3,5 mm and vertical resorption difference in socket. The secondary outcomes assessed were socket fill measured in Density of the extraction socket immediately after extraction and post treatment in Hounsfield units. Additionally, pain assessment questionnaire, surgical and post-surgical comfort was assessed on the day of suture removal.
The preoperative mean length of socket was 9.95 mm ± 2.16 in Group A which decreased to 8.46 mm ± 1.97 at 6 months. There was 1.48 mm reduction in socket length which is statistically significant. (p ≤ 0.05). In Group B, mean baseline value was 9.08 mm ± 2.04. At 6 months the mean length of socket decreased to 7.40 mm ± 1.88. The reduction observed in Group B was 1.67 which was statistically significant (p ≤ 0.05). However intergroup post-operative mean length changes showed mean difference of −0.22 (p = 0.70) which is not statistically significant (Table 3, Table 4).
Table 3.
Comparison of length, width of socket and bone density (pre and post) using wilcoxon sign TEST.
| Groups | Minimum | Maximum | Mean | Std. Deviation | Mean diff | P value | ||
|---|---|---|---|---|---|---|---|---|
| Length of socket | Group A | Pre | 6.00 | 12.35 | 9.95 | 2.16 | 1.48 | 0.028∗ |
| Post | 3.78 | 11.05 | 8.46 | 1.97 | ||||
| Group B | Pre | 5.20 | 12.00 | 9.08 | 2.04 | 1.67 | 0.025∗ | |
| Post | 4.20 | 10.34 | 7.40 | 1.88 | ||||
| Width of socket measured at 1 mm | Group A | Pre | 5.66 | 8.41 | 7.00 | 0.91 | 2.12 | 0.005∗ |
| Post | 3.79 | 5.87 | 4.87 | 0.71 | ||||
| Group B | Pre | 3.98 | 8.27 | 5.83 | 1.43 | 1.83 | 0.005∗ | |
| Post | 2.75 | 5.86 | 4.00 | 1.07 | ||||
| Width of socket measured at 3 mm | Group A | Pre | 5.07 | 7.87 | 6.54 | 1.07 | 1.68 | 0.005∗ |
| Post | 3.61 | 7.11 | 4.85 | 1.25 | ||||
| Group B | Pre | 3.19 | 8.32 | 5.62 | 1.75 | 0.59 | 0.11 | |
| Post | 3.00 | 8.61 | 5.02 | 2.02 | ||||
| Width of socket measured at 5 mm | Group A | Pre | 4.22 | 7.33 | 5.69 | 1.08 | 0.97 | 0.059 |
| Post | 3.06 | 7.01 | 4.71 | 1.30 | ||||
| Group B | Pre | 2.98 | 7.87 | 5.13 | 1.66 | 0.33 | 0.55 | |
| Post | 2.75 | 7.45 | 5.04 | 1.74 | ||||
| Bone density | Group A | Pre | −983 | −106 | −597.8 | 335.83 | −0.17 | 0.005∗ |
| Post | 565 | 1800 | 1185.30 | 473.21 | ||||
| Group B | Pre | −667 | −106 | −426.50 | 198.03 | −0.13 | 0.005∗ | |
| Post | 560 | 1452 | 966.60 | 273.27 | ||||
Table 4.
Comparison of the mean difference (pre-post) between the groups using Mann-whitney TEST.
| Groups | Minimum | Maximum | Mean | Std. Deviation | Mean diff | P value | |
|---|---|---|---|---|---|---|---|
| Length of the socket | Group A | -.74 | 4.15 | 1.451 | 1.53 | −0.22 | 0.70 |
| Group B | −2.00 | 3.48 | 1.674 | 1.610 | |||
| Width of socket(1 mm) | Group A | 1.00 | 3.85 | 2.123 | .76 | 0.29 | 0.49 |
| Group B | .98 | 3.09 | 1.831 | .800 | |||
| Width of socket(3 mm) | Group A | .66 | 3.11 | 1.689 | .84 | 1.09 | 0.041a |
| Group B | -.86 | 2.17 | .596 | 1.08 | |||
| Width of socket(5 mm) | Group A | −1.41 | 2.88 | .974 | 1.28 | 0.37 | 0.65 |
| Group B | −1.93 | 2.98 | .598 | 1.59 | |||
| Bone density | Group A | −26 | −67 | −1783.10 | 772.09 | −390.0 | 0.17 |
| Group B | −20 | −66 | −1393.1 | 449.8 | |||
Significant.
Comparisons between change in horizontal width at 1 mm in Group A and Group B at 6 months postoperatively did not give any statistically significant difference. (p = 0.49) The Intergroup comparison showed horizontal width reduction at 3 mm postoperatively was less in Group B 0.596 mm ± 1.08 as compared to Group A 1.689 mm ± 0.84 which was statistically significant (p = 0.041). The comparisons amongst horizontal width resorption between Group A 0.97 mm ± 1.28 and Group B 0.59 mm ± 1.59 at 5 mm did not reveal any statistically significant difference. The mean difference in socket fill postoperatively in intergroup comparison did not show any statistically significant difference. (p = 0.17) (Table 3, Table 4)
There were no significant statistical differences in postoperative pain in Group A and Group B as subjects, as both of them experienced moderate amount of pain (Table 5). The assessment of post-operative swelling showed that only 30% subjects in Group A reported with swelling. Whereas 80% subjects in.
Table 5.
Distribution of the subjects based on pain rate
| Group A |
Group B |
|||
|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | |
| Mild | 2 | 20.0 | 3 | 30.0 |
| Moderate | 8 | 80.0 | 7 | 70.0 |
| Total | 10 | 100.0 | 10 | 100.0 |
Group B complained of post-operative swelling. In Group A subject’s maximum amount of days for swelling to subside was 3 days whereas in Group B subjects the postoperative swelling subsided in 5 days. The Group A subjects reported less discomfort and postoperative swelling on day of suture removal as compared to Group B patients (Table 5, Table 6).
Table 7.
Distribution of the subjects based on days to subside.
| Group A |
Group B |
|||
|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | |
| After 3 days | 3 | 30.00 | 0 | 00.0 |
| After 4 days | 0 | 00.0 | 3 | 30.0 |
| After 5 days | 0 | 00.0 | 5 | 50.0 |
| NA | 7 | 70.0 | 2 | 20.0 |
| Total | 10 | 100.0 | 10 | 100.0 |
Table 6.
Distribution of the subjects based on swelling.
| Group A |
Group B |
|||
|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | |
| Yes | 3 | 30 | 8 | 80.0 |
| No | 7 | 70 | 2 | 20.0 |
| Total | 10 | 100.0 | 10 | 100.0 |
4. Discussion
As clinicians we face challenges in providing prosthetic treatment to patients where there is deficient soft tissue and ridge volume in aesthetic areas. Socket augmentation facilitates resultant implant to be placed in an aesthetically and functionally ideal position.7
To evaluate the dimensional changes 6 month, follow up period was selected. All the previous studies followed the same protocol to see the earliest changes following regenerative methods.8 A 6 month follow up period is well validated in many regenerative studies, because time gap of 6 months following postsurgical socket grafting was necessary to best appreciate regenerative changes clinically and radiographically.
In the present study, CBCT was utilized to assess regenerative changes. CBCT is one of the most reliable and acceptable radiographic method for assessment of bone regeneration, to get precise dimensional changes, as well as to understand quality of bone quantified in terms of Hounsfield unit.9 It also has less exposure compared to CT. CBCTs taken with small FOV’s cause significant dose reduction and gives substantial additional information regarding bone regeneration. Studies have reported an effective dose of 5–140 μSv for small FOV (6 × 16cms) iCAT which is in comparison to the effective dose of 4 dental bitewings for F speed film being 38 μSv10,11 Hence considering the risk vs the benefit to the patient as well as to the community this research was designed and it warrants an evaluation of bone density during the pre and post-surgical procedures to assess the success of the intervention.
Mean age difference between Group A (Test Group -A PRF Plus membrane and Sybograf plus osseous graft) and Group B (Control Group - Sybograf plus osseous graft) was nonsignificant. Even though, there is no age or gender prediction for socket preservation procedures still younger age group might be given due consideration as preferential group for regenerative surgeries.12
The bone graft used in present study was a sterile synthetic nanocrystalline Hydroxyapatite β- Tricalcium phosphate (SYBOGRAF-Plus) -size of 25 X 8 mm. β-TCP is a 3-dimensional microporous alloplast, containing spaces into which bone ingrowth occurs. The microporous structure facilitates maximize blood clot stability during early healing.13 As organic components are present in material there is no chance of antigenicity. The efficacy of β- TCP in socket preservation has also been reported by Horowitz et al., 2009; Triveni et al., 2012 and Das et al., 2016.4,14,15
For our Test Group, along with bone graft mentioned above, Platelet Rich Fibrin was chosen as an additive regenerative material due to its well-known advantages like accelerated surgical wound healing, bone growth and maturation and graft stabilization.16Innovations in techniques and methods of PRF like Advanced Platelet rich fibrin Plus has demonstrated superiority compare to its predecessors, by release of highest growth plane.6
Recent systematic reviews by Avila-Ortiz (2014)17, Faria-Almeida (2019)18 reviewed effect of socket filling with bone grafts on prevention of post extraction alveolar ridge volume loss. They compared with tooth extraction alone in nonmolar sites. They stated that alveolar ridge preservation is beneficial in limiting physiologic ridge reduction in comparison to tooth extraction alone. Additionally, they concluded elevation of flap, utilisation of a membrane and application of xenograft or an allograft could be associated with superior outcomes. This could be particularly on midbuccal and midlingual height preservation.
Horizontal width changes are a selected criterion to assess efficacy of regenerative material used in socket grafting. Use of bone grafting along with additives used in the regenerative methods expected.to yield better post-operative results.19 In our present study, intra group comparison of horizontal width at HW 1 mm though showed significant difference, it was not the case at HW 3- and 5-mm. Systematic review by Jambhekar et al., 2015 assessed 32 RCTs studying 1354 sockets, addressing extraction by flapless technique with socket grafting. They provided dimensional information after three months of healing. They concluded mean loss of bucco-lingual width at ridge crest was lowest for xenografts (1.3 mm), followed by allografts (1.63 mm), alloplasts (2.13 mm) and sockets without any bone grafting material (2.79 mm).20 Thus result of the present study is aligned with systematic review results, which highlights the need for or importance of socket grafting with bone graft and additive material, rather than, leaving alone without socket grafting to stabilise socket dimension post extraction.
Utilisation of bone grafts with/without additives though resulted in better bone fill compare to non-grafting sites as mentioned in many previous studies.21 However, comparing different bone grafts for socket grafting has not shown, any one bone graft superior to the other bone grafts in terms of bone fill. Thus, the present study results in terms of bone fill, is in agreement with previous studies done by Horowitz et al., 2009; Triveni et al., 2012; Haugen HJ et al. 20194,14,22
The present study undoubtedly showed influence of A- PRF Plus on postoperative discomfort and pain. Test Group subjects reported less discomfort and postoperative swelling on day of suture removal as compared to Control Group patients. This study is in concordance with Temmerman A et al (2016)23 who reported that L-PRF as grafting material in post extraction sockets is an efficient and beneficial procedure to manage postoperative pain and also enhance soft tissue healing process. Possible explanations include release of elevated quantities of ‘transforming growth factor β-1 (TGF β-1)’, ‘platelet-derived growth factor AB (PDGF-AB)’, ‘vascular endothelial growth factor (VEGF)’ and ‘thrombospondin-1’ which stimulates biological functions namely chemotaxis, angiogenesis, proliferation, differentiation, modulation.6,16,23, 24,25,26
Although no attempts were made to augment soft tissue in present study, it did not lead to any compromised results. However combined soft and hard tissue augmentation may be utilized in further research protocol to assess combined effects.27 It is also to be noted that, sample size chosen in present study was good enough to assess results of the first ever report of utilisation of A- PRF Plus. Studies on a larger sample population may be warranted to understand usefulness of these growth factors. It is also to be noted that clinical and radiographic methods are appropriate measures to assess utilisation of regenerative methods in socket grafting,28 histologic assessment may further help in establishing effectiveness of Hydroxyapatite and β-TCP and A- PRF Plus membrane as biomaterials for socket preservation.
4. Conclusion
The application of A PRF Plus with osseous bone graft resulted in less vertical and horizontal changes compared to use of osseous bone graft alone. Furthermore, the use of A PRF Plus results in less postoperative discomfort and pain for the patients, especially during the early phases of healing. Presence of rich growth factors released slowly for a longer period of time helps in promoting regeneration of bone in extraction socket as well as aids in soft tissue healing Within the limitations of this Randomized control clinical trial, it can be concluded that the use of A PRF Plus as a socket filling material to achieve ridge preservation is promising adjunct to conventional regenerative therapy, during a six -month observation period.
Clinical relevance
Socket preservation is a therapeutic approach following tooth extraction. This procedure is developed to limit effect of post extraction absorption, maintain hard and soft tissue contour of ridge. Also, to boost socket fill and enhance bone quality prior to placement of implant. It aims to maintain stable ridge volume to optimize functional as well as aesthetic outcomes.
Statement of sources of funding for the study
This study has been self-funded by the Primary co-investigator – Dr. MANASI YEWALE. The study has not been given any Institutional funds or grants.
Disclosure of any conflicts of interests if applicable
Not applicable.
References
- 1.Van der Weijden F., Dell’Acqua F., Slot D.E. Alveolar bone dimensional changes of post-extraction sockets in humans: a systematic review. J Clin Periodontol. 2009 Dec;36(12):1048–1058. doi: 10.1111/j.1600-051X.2009.01482.x. [DOI] [PubMed] [Google Scholar]
- 2.Vignoletti F., Matesanz P., Rodrigo D., Figuero E., Martin C., Sanz M. Surgical protocols for ridge preservation after tooth extraction. A systematic review. Clin Oral Implants Res. 2012 Feb;23:22–38. doi: 10.1111/j.1600-0501.2011.02331.x. [DOI] [PubMed] [Google Scholar]
- 3.Darby I., Chen S.T., Buser D. Ridge preservation techniques for implant therapy. Int J Oral Maxillofac Implants. 2009 Oct 2;24(Suppl):260–271. [PubMed] [Google Scholar]
- 4.Horowitz R.A., Mazor Z., Miller R.J., Krauser J., Prasad H.S., Rohrer M.D. Clinical evaluation alveolar ridge preservation with a beta-tricalcium phosphate socket graft. Comp Cont Educ Dent. 2009 Nov 1;30(9):588–590. [PubMed] [Google Scholar]
- 5.Ehrenfest D.M., Rasmusson L., Albrektsson T. Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte-and platelet-rich fibrin (L-PRF) Trends Biotechnol. 2009 Mar 1;27(3):158–167. doi: 10.1016/j.tibtech.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 6.Fujioka-Kobayashi M., Miron R.J., Hernandez M., Kandalam U., Zhang Y., Choukroun J. Optimized platelet-rich fibrin with the low-speed concept: growth factor release, biocompatibility, and cellular response. J Periodontol. 2017 Jan;88(1):112–121. doi: 10.1902/jop.2016.160443. [DOI] [PubMed] [Google Scholar]
- 7.Garber D.A. The esthetic dental implant: letting restoration be the guide. J Am Dental Assoc. 1995 Mar 1;126(3):319–325. doi: 10.14219/jada.archive.1995.0175. [DOI] [PubMed] [Google Scholar]
- 8.Jung R.E., Philipp A., Annen B.M. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: a randomized controlled clinical trial. J Clin Periodontol. 2013 Jan;40(1):90–98. doi: 10.1111/jcpe.12027. [DOI] [PubMed] [Google Scholar]
- 9.Chappuis V., Engel O., Reyes M., Shahim K., Nolte L.P., Buser D. Ridge alterations post-extraction in the esthetic zone: a 3D analysis with CBCT. J Dent Res. 2013 Dec;92(12_suppl):195S–201S. doi: 10.1177/0022034513506713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.White S.C., Pharoah M.J. Mosby Elsevier; St. Louis, Missouri: 2009. Oral Radiology: Principles and Interpretation. [Google Scholar]
- 11.Ludlow J.B., Timothy R., Walker C. Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofacial Radiol. 2015;44(1):20140197. doi: 10.1259/dmfr.20140197. Erratum in: Dentomaxillofac Radiol. 2015;44(7):20159003. PMID: 25224586; PMCID: PMC4277438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shirota T., Donath K., Ohno K., Matsui Y., Michi K.I. Effect of age and radiation on bone healing adjacent to hydroxyapatite placed in the tibia of rats. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995 Mar 1;79(3):285–294. doi: 10.1016/s1079-2104(05)80221-5. [DOI] [PubMed] [Google Scholar]
- 13.Brkovic B.M., Prasad H.S., Rohrer M.D. Beta-tricalcium phosphate/type I collagen cones with or without a barrier membrane in human extraction socket healing: clinical, histologic, histomorphometric, and immunohistochemical evaluation. Clin Oral Invest. 2012 Apr 1;16(2):581–590. doi: 10.1007/s00784-011-0531-1. [DOI] [PubMed] [Google Scholar]
- 14.Triveni M.G., TarunKumar A.B., Jain V., Mehta D.S. Alveolar ridge preservation with β-TCP graft and platelet-rich fibrin. Int J Oral Implant Clin Res. 2012;3:96–100. [Google Scholar]
- 15.Das S., Jhingran R., Bains V.K., Madan R., Srivastava R., Rizvi I. Socket preservation by beta-tri-calcium phosphate with collagen compared to platelet-rich fibrin: a clinico-radiographic study. Eur J Dermatol. 2016 Apr;10(2):26. doi: 10.4103/1305-7456.178298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pan J., Xu Q., Hou J. Effect of platelet-rich fibrin on alveolar ridge preservation: a systematic review. J Am Dental Assoc. 2019 Sep 1;150(9):766–778. doi: 10.1016/j.adaj.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 17.Avila-Ortiz G., Elangovan S., Kramer K.W., Blanchette D., Dawson D.V. Effect of alveolar ridge preservation after tooth extraction: a systematic review and meta-analysis. J Dent Res. 2014 Oct;93(10):950–958. doi: 10.1177/0022034514541127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Faria-Almeida R., Astramskaite-Januseviciene I., Puisys A., Correia F. Extraction socket preservation with or without membranes, soft tissue influence on post extraction alveolar ridge preservation: a systematic review. J Oral Maxillofac Res. 2019 Jul;10(3) doi: 10.5037/jomr.2019.10305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shah R., Gowda T.M., Thomas R., Kumar T., Mehta D.S. Biological activation of bone grafts using injectable platelet-rich fibrin. J Prosthet Dent. 2019 Mar 1;121(3):391–393. doi: 10.1016/j.prosdent.2018.03.027. [DOI] [PubMed] [Google Scholar]
- 20.Jambhekar S., Kernen F., Bidra A.S. Clinical and histologic outcomes of socket grafting after flapless tooth extraction: a systematic review of randomized controlled clinical trials. J Prosthet Dent. 2015 May 1;113(5):371–382. doi: 10.1016/j.prosdent.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 21.Troiano G., Zhurakivska K., Lo Muzio L., Laino L., Cicciù M., Lo Russo L. Combination of bone graft and resorbable membrane for alveolar ridge preservation: a systematic review, meta-analysis, and trial sequential analysis. J Periodontol. 2018 Jan;89(1):46–57. doi: 10.1902/jop.2017.170241. [DOI] [PubMed] [Google Scholar]
- 22.Haugen H.J., Lyngstadaas S.P., Rossi F., Perale G. Bone grafts: which is the ideal biomaterial? J Clin Periodontol. 2019 Jun;46:92–102. doi: 10.1111/jcpe.13058. [DOI] [PubMed] [Google Scholar]
- 23.Temmerman A., Vandessel J., Castro A. The use of leucocyte and platelet-rich fibrin in socket management and ridge preservation: a split-mouth, randomized, controlled clinical trial. J Clin Periodontol. 2016 Nov;43(11):990–999. doi: 10.1111/jcpe.12612. [DOI] [PubMed] [Google Scholar]
- 24.Verma U.P., Yadav R.K., Dixit M., Gupta A. Platelet-rich fibrin: a paradigm in periodontal therapy–a systematic review. J Int Soc Prev Community Dent. 2017 Sep;7(5):227. doi: 10.4103/jispcd.JISPCD_429_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kumar R.V., Shubhashini N. Platelet rich fibrin: a new paradigm in periodontal regeneration. Cell Tissue Bank. 2013 Sep 1;14(3):453–463. doi: 10.1007/s10561-012-9349-6. [DOI] [PubMed] [Google Scholar]
- 26.Caruana A., Savina D., Macedo J.P., Soares S.C. From platelet-rich plasma to advanced platelet-rich fibrin: biological achievements and clinical advances in modern surgery. Eur J Dermatol. 2019 May;13(2):280. doi: 10.1055/s-0039-1696585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jung R.E., Ioannidis A., Hämmerle C.H., Thoma D.S. Alveolar ridge preservation in the esthetic zone. Periodontology. 2000;77(1):165–175. doi: 10.1111/prd.12209. 2018 Jun. [DOI] [PubMed] [Google Scholar]
- 28.Grimard B.A., Hoidal M.J., Mills M.P., Mellonig J.T., Nummikoski P.V., Mealey B.L. Comparison of clinical, periapical radiograph, and cone-beam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J Periodontol. 2009 Jan;80(1):48–55. doi: 10.1902/jop.2009.080289. [DOI] [PubMed] [Google Scholar]