Abstract
Adrenocortical tumors (ACTs) are rare in children and should be treated as malignant tumors. A 12-year-old female patient was referred to our institute for acute abdomen and hypovolemic shock. She had symptoms of virilization, including lowered voice, beard growth, and hirsutism. An elevated level of dehydroepiandrosterone sulfate was observed, and computed tomography scan showed a large left adrenal mass with massive hemorrhage. Emergency transcatheter arterial embolization was successfully performed using N-buthyl-2-cyanoacrylate as an embolic material. She underwent surgical resection on the following day. Histopathological analysis showed strong degeneration of the tumor and its necrosis, and the tumor was diagnosed as ACT of unknown grade. To our knowledge, this is the first case of a ruptured ACT treated with transcatheter arterial embolization in a pediatric patient.
Keywords: Pediatric, Adrenocortical tumor, Rupture, Transarterial embolization, N-butyl-2-cyanoacrylate
Abbreviations: ACT, adrenocortical tumor; TAE, transcatheter arterial embolization; CT, computed tomography; DHEA-S, dehydroepiandrosterone sulfate; NBCA, n-butyl-2-cyanoacrylate
Introduction
Pediatric adrenocortical tumor (ACT) is extremely rare and has an incidence of 0.1-0.4 cases per million individuals [1]. It should be treated as a malignant neoplasm, although histopathologically, it is difficult to classify it as a carcinoma or adenoma. Rupture is a rare complication of ACTs. According to a literature review by Polistina et al., all 16 patients with ruptured adrenocortical carcinomas underwent surgery, and three of them were pediatric patients [2]. In this case report, we present the case of a 12-year-old female patient with virilization, who presented with acute abdomen and hemorrhagic shock due to a ruptured ACT. She underwent emergency transcatheter arterial embolization (TAE) to stabilize her general condition before undergoing elective surgery. To our knowledge, this is the first pediatric case of a ruptured ACT treated with TAE, which has only been reported so far in 2 adult patients with adrenocortical carcinoma and adenoma [3,4].
Case description
A 12-year-old girl with abdominal pain, vomiting, and hypovolemic shock was referred to our hospital in an emergency. She was 161.0 cm tall (+1.3 standard deviation [SD]) and weighed 49.6 kg (+0.4 SD). On admission, her level of consciousness was assessed and she was able to open her eyes to a stimulus; her body temperature was 35.9°C, heart rate was 184 beats per minute (bpm), blood pressure could not be measured, respiratory rate was 44 per minute, and blood oxygen saturation was 98% on 2 L of oxygen. Following rapid infusion of 500 mL extracellular fluid, her heart rate decreased to 130 bpm and blood pressure measured 83/48 Torr. Contrast-enhanced computed tomography (CT) of the abdomen (CTDI, 10.902 mGy) showed a left retroperitoneal tumor measuring 13 cm in diameter with massive hemorrhage between the spleen and left kidney (Fig. 1). The patient had shown signs of virilization over the past several years, including lowered voice, beard growth, and hirsutism. Laboratory results showed elevated levels of dehydroepiandrosterone sulfate (DHEA-S) (398 µg/dL; normal <68), although, the level of testosterone was within normal limits.
Fig. 1.
Coronal contrast-enhanced CT image shows a large left suprarenal retroperitoneal mass with massive hemorrhage measuring 13 cm in diameter (arrows).
The clinical diagnosis was hemorrhagic shock due to the spontaneous rupture of the left ACT, and emergency TAE was performed in order to restore hemodynamic stability. In the first session, we embolized the left superior adrenal artery using gelatin sponge slurry (Fig. 2). The middle adrenal artery was so thin that the gelatin sponge slurry did not flow into the vessel and the inferior adrenal artery could not be catheterized, even though a 1.7-F microcatheter was used. The hemodynamic state improved but only temporarily as the patient returned to the pre-shock vitals on the same day. During the second procedure, we selected the recanalized left superior adrenal artery as well as the middle (Fig. 3) and inferior adrenal arteries using a double coaxial microcatheter system consisting of an outer 2.6-F high-flow microcatheter and an inner 1.6-F thin microcatheter (Fig. 4). These arteries were embolized with 17% N-butyl-2-cyanoacrylate (NBCA) diluted with iodized oil. Her general condition improved enough to allow tumor resection on the next day. The histopathologic diagnosis was ACT of unknown grade due to strong tumor degeneration and necrosis. Almost no mitoses were observed microscopically (<1 per 10 high-power fields). The patient has been doing well for 1.5 years with no evidence of hormonal abnormality or tumor recurrence. The condition of virilization is improving gradually.
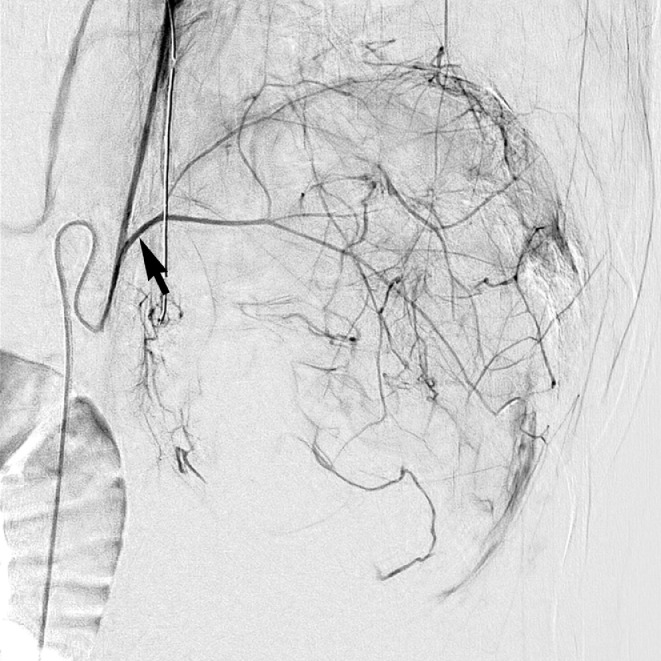
Fig. 2.
Left inferior phrenic arteriogram shows the left superior adrenal artery supplying the tumor (arrow).
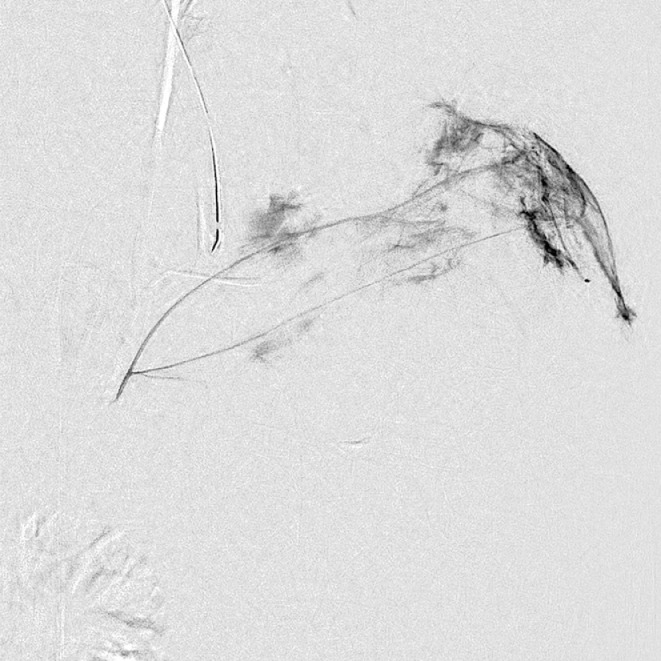
Fig. 3.
Left middle adrenal arteriogram shows the tumor stain.
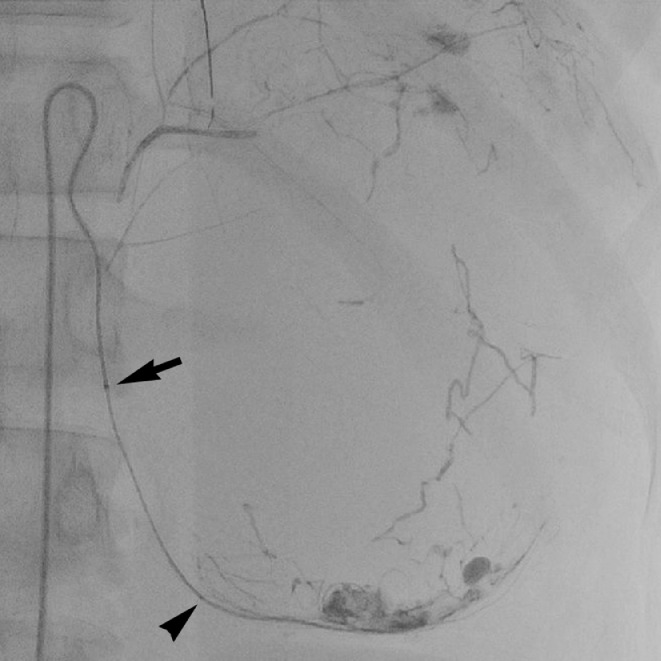
Fig. 4.
Fluoroscopy image during TAE of the left inferior adrenal artery using NBCA diluted with iodized oil shows the radiopaque casts of the embolisant in the left superior, middle, and inferior adrenal arteries and a 1.6-F inner microcatheter (arrowhead) coaxially advanced through a 2.6-F high-flow microcatheter (arrow).
Discussion
In adults, adrenal tumors are common and are even found incidentally on medical imaging examinations, as so-called “adrenal incidentaloma.” Approximately half of such adrenal tumors in adults are non-functioning adrenocortical adenomas, and adrenocortical carcinomas are diagnosed in only 1.4% of adrenal tumors in adults [5]. Weiss criteria are usually used for diagnosing adrenocortical carcinoma. In pediatric patients, however, the Weiss criteria show a discrepancy with clinical outcomes; thus, it is difficult to classify pediatric ACTs histopathologically into carcinomas and adenomas. Nevertheless, pediatric ACT should be treated as a malignant tumor, especially in patients aged 4 years or more [6]. Recently, Wieneke-index criteria have shown excellent consistency with the clinical outcome of ACT [6]. In comparison with the Weiss criteria, the Wieneke-index criteria focused more on macroscopic findings such as tumor weight and size. However, it was difficult to evaluate our case even with the Wieneke-index criteria because the tumor size and weight could be overestimated due to the massive intratumoral hemorrhage and the rupture and embolization could affect the histopathological evaluation, including necrosis, vascular, and capsular invasion.
There have been three previously reported pediatric cases of ruptured adrenocortical carcinomas treated with emergency adrenalectomy [2]. Of these, a 12-year-old female patient died 30 months after surgery; thus, we are closely following up our patient, and fortunately, no recurrent disease has been observed for 1.5 years. Interestingly, the previous three pediatric patients had non-functioning tumors, although virilization is the most common presentation of pediatric ACTs [1]. The lack of such clinical manifestations might delay the diagnosis of ACTs in these cases. Our patient had obvious symptoms of virilization, including lowered voice, beard growth, and hirsutism, which helped in the diagnosis. A previous report described other symptoms of virilization, including acne, increased muscle mass, and secretion and proliferation of sebaceous glands with characteristic adult odor [7]. According to the report, the elevation of urinary 17-keratosteroids and plasma DHEA-S in hormonal examination had high sensitivity in diagnosing pediatric ACTs. The latter was also observed in our case.
To our knowledge, only two adult patients treated with TAE for ruptured ACTs have been reported so far. A 47-year-old female patient with a ruptured non-functioning left adrenocortical carcinoma measuring 13.5 cm in diameter underwent embolization of the left middle adrenal artery followed by elective left adrenalectomy 2 months later. She underwent adjuvant chemotherapy and no recurrence was observed for 6 months [3]. In another case, a 71-year-old male patient with end-stage renal failure on dialysis underwent TAE for bleeding from a non-functioning right adrenocortical adenoma measuring 5.8 cm in diameter after a fall at home [4]. In both cases, there were no descriptions of embolic agents. In the present case, the initial TAE with gelatin sponge failed to stabilize the hemodynamic state of the patient; therefore, NBCA diluted with iodized oil was used in the second session because of its immediate and rigid embolic effect. Migration of the embolisant to proximal vessels and catheter adhesion to the vessel wall are considerable serious complications; however, these can be avoided by combining the use of the double coaxial microcatheter technique [8]. This technique is useful to catheterize thin arteries, especially in pediatric patients.
In conclusion, we experienced the first pediatric case of a ruptured ACT treated with TAE. Emergency TAE was an effective treatment to stabilize the hemodynamic state of the patient and enabled the subsequent elective surgery. NBCA with iodized oil showed better embolic effect than gelatine sponge and could be safely administered using the double coaxial microcatheter technique.
Patient Consent Statement
The parents of the patient gave written informed consent for publication of this case report.
Acknowledgments
The authors wish to acknowledge Dr. Masayuki Noguchi, Professor of Pathology, University of Tsukuba, for his work in histopathological diagnosis. The authors would like to thank Editage [http://www.editage.com] for editing and reviewing this manuscript for English language.
Footnotes
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributor Information
Miki Yoshida, Email: yosshi_1121@yahoo.co.jp.
Hiroaki Takahashi, Email: h.1982.takahashi@gmail.com.
Yuni Yamaki, Email: yamaki-kgs@umin.ac.jp.
Fumiko Chiba, Email: fumikoc@md.tsukuba.ac.jp.
Kensaku Mori, Email: moriken@md.tsukuba.ac.jp.
References
- 1.Ribeiro R.C., Pinto E.M., Zambetti G.P., Rodriguez-Galindo C. The International Pediatric Adrenocortical Tumor Registry initiative: contributions to clinical, biological, and treatment advances in pediatric adrenocortical tumors. Mol. Cell. Endocrinol. 2012;351:37–43. doi: 10.1016/j.mce.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 2.Polistina F.A., Farruggio A., Gasparin P., Pasquale S., Frego M. Spontaneously metachronous ruptures of adrenocortical carcinoma and its contralateral adrenal metastasis. Int. Cancer Conf. J. 2015;5:90–97. doi: 10.1007/s13691-015-0235-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kashiwagi S., Amano R., Onoda N., Noda S., Hirata K., Asano Y. Nonfunctional adrenocortical carcinoma initially presenting as retroperitoneal hemorrhage. BMC Surg. 2015;15:46. doi: 10.1186/s12893-015-0031-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee K.A., Jin H.Y. Non-surgically treated case of nonfunctioning ruptured adrenal adenoma in a patient on hemodialysis. Endocrine. 2019;65:213–216. doi: 10.1007/s12020-019-01948-3. [DOI] [PubMed] [Google Scholar]
- 5.Ichijo T., Ueshiba H., Nawata H., Yanase T. A nationwide survey of adrenal incidentalomas in Japan: the first report of clinical and epidemiological features. Endocr J. 2020;67:141–152. doi: 10.1507/endocrj.EJ18-0486. [DOI] [PubMed] [Google Scholar]
- 6.Gupta N., Rivera M., Novotny P., Rodriguez V., Bancos I., Lteif A. Adrenocortical carcinoma in children: a clinicopathological analysis of 41 patients at the Mayo Clinic from 1950 to 2017. Horm Res Paediatr. 2018;90:8–18. doi: 10.1159/000488855. [DOI] [PubMed] [Google Scholar]
- 7.Ribeiro R.C., Michalkiewicz E.L., Figueiredo B.C., DeLacerda L., Sandrini F., Pianovsky M.D. Adrenocortical tumors in children. Braz J Med Biol Res. 2000;33:1225–1234. doi: 10.1590/s0100-879x2000001000013. [DOI] [PubMed] [Google Scholar]
- 8.Uchikawa Y., Mori K., Shiigai M., Konishi T., Hoshiai S., Ishiguro T. Double coaxial microcatheter technique for glue embolization of renal arteriovenous malformations. Cardiovasc Intervent Radiol. 2015;38:1277–1283. doi: 10.1007/s00270-015-1188-y. [DOI] [PubMed] [Google Scholar]