Abstract
Pediatric traumatic hip dislocations (PTHD) are rare and represent around 5% of all pediatric dislocations. Associated bony or soft tissue injury can occur as often as 17%–25% of the time. We report a case of an 8-year-old boy presenting a posterior hip dislocation after a low-energy trauma, which was initially managed with closed reduction and bed rest for 1 week. Two days after hospital discharge, he suffered a recurrent posterior hip dislocation. He was now managed with 4 weeks of bed rest and lower limb skin traction followed by 1 week of no weight-bearing on crutches. With 6 months of follow-up, he is asymptomatic, walking autonomously, with complete and painless range of motion of the affected hip and no major radiographic changes. Pediatric traumatic hip dislocation is a rare and challenging injury that should be managed promptly. Currently, there is no protocol concerning treatment in the literature and its largely dependent of patient and parents' cooperation.
Keywords: Child, Hip, Traumatic dislocation, Magnetic resonance imaging, Closed reduction
Introduction
Pediatric traumatic hip dislocations (PTHD) are rare and represent around 5% of all pediatric dislocations [[1], [2], [3]]. PTHD are usually posterior and are generally consequence of high-energy injuries [[1], [2], [3]]. It can also be associated with minor trauma, especially in children younger than 10 years-old, as a result of more flexible joint structures of the immature hip [[1], [2], [3], [4]]. Associated ipsilateral fractures (as acetabular and femoral head fractures) can occur as often as 17% and bony or soft tissue entrapment may occur up to 25% of the time [1,2].
Case presentation
We present an 8-year-old boy who suffered a ground-level fall on his knees. As previous medical history he had an elevated body mass index (27 Kg/m2). He presented to our emergency department with pain on his left hip and inability to bear weight. It was evident a limb length discrepancy, with his left lower limb in flexion, abduction and external rotation (Fig. 1). No other injury, including neurovascular, was detected. Anteroposterior radiograph (Fig. 2) showed a posterior hip dislocation, further confirmed with fluoroscopy later on (Fig. 3).
Fig. 1.
Clinical appearance at presentation.
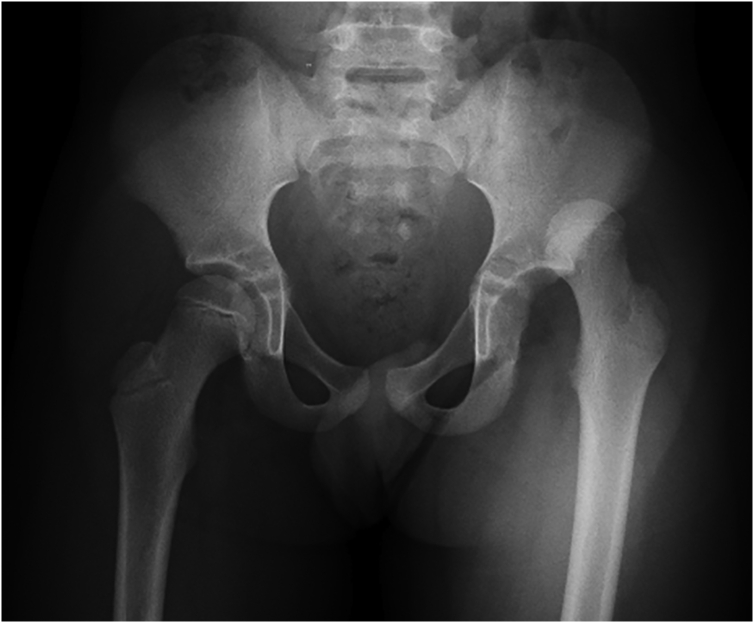
Fig. 2.
Anteroposterior radiograph at presentation.
Fig. 3.
Fluoroscopy before reduction of the dislocation.
Four hours since initial trauma, he was submitted to closed reduction under sedation and fluoroscopy, followed by testing of hip stability. Post-reduction radiographs showed a concentric reduction (Fig. 4A and B). After 48 h of bed rest, he tolerated walking with a hip orthosis and crutches without bearing weight. One week later he was discharged with indication for no weight-bearing on crutches while maintaining the hip orthosis.
Fig. 4.
Anteroposterior (A) and lateral (B) radiographs post-reduction.
He was brought to the hospital 2 days after discharge, for left hip pain while playing football. Once again, he was diagnosed with a posterior hip dislocation (Fig. 5) and was emergently submitted to closed reduction under sedation. Post reduction radiographs showed concentric reduction (Fig. 6). As it was an early recurrent dislocation, a magnetic resonance was done with evidence of an osteochondral avulsion of the posterior labrum and partial rupture of the posterior capsule, with no other evident acetabular or femoral head fractures (Fig. 7A, B, C and D). He was discharged after 4 weeks of bed rest and lower limb skin traction followed by 1 week of no weight-bearing on crutches.
Fig. 5.
Anteroposterior radiograph at the time of the second dislocation.
Fig. 6.
Anteroposterior radiograph post-reduction of the second dislocation.
Fig. 7.
Axial (A, B) and coronal (C, D) views of T2-STIR magnetic resonance imaging.
At 6 months of follow-up, he is asymptomatic, walking autonomously, with complete and painless range of motion of the left hip (Fig. 8A, B and C). Six months anteroposterior radiograph shows no apparent lesion (Fig. 9). A control magnetic resonance was done at 6 months after initial injury, showing mild articular effusion and an apparently healed posterior labrum and acetabular wall (Fig. 10A and B).
Fig. 8.
Active range of motion (A, internal rotation; B, external rotation; C, abduction) at 6 months post-second dislocation.
Fig. 9.
Anteroposterior radiograph at 6 months post-second dislocation.
Fig. 10.
Coronal (A) and axial (B) views of T2-SPAIR magnetic resonance imaging.
Discussion
PTHD are considered orthopedic emergencies, due to the possible disruption of the vascular supply to the proximal epiphyseal plate of the femur [2]. Performing reduction of PTHD in the first 6 h is extremely important [2]. Delayed diagnosis and reduction can lead to a significant increase of avascular necrosis and degenerative arthritis [2,5]. Concentric reduction is usually achieved by closed means, in approximately 85% of the cases [5]. Open reduction may be necessary if the dislocation is irreducible by closed means, if reduction is nonconcentric or the hip is unstable, and if there is an associated lesion that needs surgical repair [2,5].
Following successful closed reduction, it is suggested the use of spica cast with hip abduction and bed rest [2,3]. In older children, above 10 years-old, it can be used a hip bracing and protected weight-bearing on crutches [2,3]. PTHD complications are infrequent in children, except for recurrent dislocation [2,3]. It is usually consequence of a labrum or capsule defect and it is more commonly seen in children treated with short period immobilization and allowed for early ambulation [2,3]. However, literature it is not unanimous regarding the period of non-weight bearing that should be recommended after reduction [3].
If it is not possible to obtain a stable and concentric closed reduction, magnetic resonance is the study of choice [[6], [7], [8]]. This imaging technique is more appropriated for evaluating characteristic structural injuries, specially lesions of the posterior labrum and fractures of the posterior unossified acetabular wall [8]. Some authors advocate that if this labral pathology is left untreated it could lead to further pain and degeneration of the hip [1,2]. However, there are reports of spontaneous healing of large posterior labral detachments in children with a good outcome [7]. A recent study also described successful outcomes with arthroscopically assisted reduction without repair of the avulsed osteochondral labrum defect in incongruent hip joints after PTHD in children [9]. Therefore, the need for surgical repair of this type of lesion alone or while performing an open reduction is debatable.
In conclusion, PTHD is a rare and challenging injury that should be managed promptly. Currently, there is no protocol concerning treatment in the literature and its largely dependent of patient and parents' cooperation.
References
- 1.Stenroos A., Laaksonen T., Nietosvaara Y. Traumatic hip dislocation in pediatric patients. Duodecim; laaketieteellinen aikakauskirja. 2017;133(8):749–752. [PubMed] [Google Scholar]
- 2.Yuksel S., Albay C. Early reduction of pediatric traumatic posterior hip dislocation is much more important than the treatment procedure. Pediatr. Emerg. Care. 2019;35(11):e206–e208. doi: 10.1097/PEC.0000000000001351. [DOI] [PubMed] [Google Scholar]
- 3.Furuya H., Shimamura Y., Kaneko K., Sakuramoto H., Hirata K., Arai Y. Traumatic dislocation of the hip in a child caused by trivial force for age. Case Rep Orthop. 2014;2014:467246. doi: 10.1155/2014/467246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hickerson L.E., Tuten H.R. Missed pediatric traumatic hip dislocation: a case report. JBJS Case Connector. 2013;3(1) doi: 10.2106/JBJS.CC.L.00037. [DOI] [PubMed] [Google Scholar]
- 5.Basaran S.H., Bilgili M.G., Ercin E., Bayrak A., Ones H.N., Avkan M.C. Treatment and results in pediatric traumatic hip dislocation: case series and review of the literature. Ulusal travma ve acil cerrahi dergisi. 2014;20(6):437–442. doi: 10.5505/tjtes.2014.52822. [DOI] [PubMed] [Google Scholar]
- 6.Blanchard C., Kushare I., Boyles A., Mundy A., Beebe A.C., Klingele K.E. Traumatic, posterior pediatric hip dislocations with associated posterior labrum osteochondral avulsion: recognizing the acetabular “fleck” sign. J. Pediatr. Orthop. 2016;36(6):602–607. doi: 10.1097/BPO.0000000000000507. [DOI] [PubMed] [Google Scholar]
- 7.Clement R.C., Carpenter D.P., Cuomo A.V. Spontaneous healing of a bucket-handle posterior labral detachment after hip dislocation in a five-year-old child: a case report. JBJS Case Connector. 2018;8(2) doi: 10.2106/JBJS.CC.17.00133. [DOI] [PubMed] [Google Scholar]
- 8.Thanacharoenpanich S., Bixby S., Breen M.A., Kim Y.J. MRI is better than CT scan for detection of structural pathologies after traumatic posterior hip dislocations in children and adolescents. Journal of Pediatric Orthopedics. 2018;40(2):86–92. doi: 10.1097/BPO.0000000000001127. [DOI] [PubMed] [Google Scholar]
- 9.Morris A.C., Yu J.C., Gilbert S.R. Arthroscopic treatment of traumatic hip dislocations in children and adolescents: a preliminary study. J. Pediatr. Orthop. 2017;37(7):435–439. doi: 10.1097/BPO.0000000000000670. [DOI] [PubMed] [Google Scholar]