Abstract
Background:
Anterior cruciate ligament (ACL) tears are common in collegiate athletes. The rate of return to the preinjury level of sport activities after ACL reconstruction continues to evolve.
Purpose/Hypothesis:
The purpose was to determine the return-to-sport rate after ACL reconstruction in a cohort of National Collegiate Athletic Association Division I athletes in different sports. It was hypothesized that, with intensive supervision of rehabilitation, the return-to-sport rate would be optimal.
Study Design:
Case series; Level of evidence, 4.
Methods:
We retrospectively reviewed the records of 75 collegiate athletes from a single institution who had undergone unilateral or bilateral ACL reconstruction between 2001 and 2013 and participated in an extensive supervised rehabilitation program. Prospectively collected athlete data as well as data about preinjury exposure, associated lesions, surgical technique, time lost to injury, number of games missed, time to return to full sport activity or retire, and subsequent surgical procedures were extracted from the medical and athletic trainer records.
Results:
The 75 patients (40 male, 35 female; mean age, 20.1 years) underwent 81 reconstruction procedures (73 primary, 8 revision). The mean follow-up was 19.3 months. The overall return-to-sport rate was 92%. After reconstruction, 9 athletes (12%) retired from collegiate sports, but 3 of them returned to sport activities after graduation. Overall, 8 athletes (11%) experienced an ACL graft retear.
Conclusion:
The return-to-sport rate in our National Collegiate Athletic Association Division I athletes compared favorably with that reported in other studies in the literature. The strict follow-up by the surgeon, together with the high-profile, almost daily technical and psychological support given mainly by the athletic trainers during the recovery period, may have contributed to preparing the athletes for a competitive rate of return to sport at their preinjury level.
Keywords: activity level, anterior cruciate ligament reconstruction, collegiate athletes, return to sport
Anterior cruciate ligament (ACL) tears are a frequent sport-related knee injury that commonly requires surgical management. Every year in the United States more than 175,000 ACL reconstruction (ACLR) procedures are performed, with a prevalence of 1 in 3500 individuals that involves mostly young athletes.43 The main indication for this procedure is to restore knee stability to allow patients to return to the same preinjury daily and sport activity level with low risk of reinjury.10,24,43
Return to sport (RTS) at the preinjury level is a very important issue for professional, semiprofessional, and nonprofessional athletes. Many factors may play a role in the RTS decision: the extent of the injury, surgical technique, rehabilitation protocol, and patient’s psychological readiness and approach to the injury including the motivation to return.4,6,22,23,28,42 Shrier41 combined the various issues into 3 concepts that go into making the RTS decision: tissue health, tissue stresses, and risk tolerance modifiers. After an ACLR, not all the athletes with optimal functional and clinical outcomes will RTS at their preinjury level.7,8,18,23 RTS, career length, and reinjury rate after ACLR in professional athletes playing in the National Football League (NFL),12,14,39 the National Basketball Association (NBA),13,25 and professional soccer9,35,47,48 have been investigated. RTS varies considerably depending on the study, sport, sex, level of play, and definitions. While studies have focused on college-aged athletes, most of them have addressed American football,15,26,27,31,36 with little or no data on other collegiate sports or about women. Even less data are available on school-aged competitors.40
In general, approximately 800 athletes participate in 22 different sports each year at the University of Iowa. The increasing participation of collegiate athletes in competitive sports at a high level of competition is among the factors in the high number of ACL injuries in the collegiate sport population.1,6,27 The RTS rate after ACLR for collegiate athletes in general remains an underdeveloped concern. Our primary purpose was to determine the rate and length of time to RTS after ACLR across multiple sport disciplines in a cohort of collegiate athletes. Secondary questions of interest were sex differences for rate and time as well as reinjury rate after ACLR.
Methods
Approval from an institutional review board was obtained before study initiation. We reviewed the medical records of all collegiate athletes at the University of Iowa who underwent ACLR (primary and revision surgery, unilateral or bilateral) with or without concomitant procedures between 2001 and 2013. The surgeries were performed by 4 different sports medicine–experienced surgeons (C.M.H., M.J.B., B.R.W., A.A.). Patient characteristic data as well as data about preinjury exposure (days from start of the season to injury), associated lesions, type of surgical technique, time lost to injury (days from injury to RTS) and number of missed games, time from the surgery to return to full sport activity, and subsequent surgical procedures on the same knee were extracted from the medical and athletic trainer records archive (Sports Injury Monitoring System; FlanTech). Data in this database were entered each day by certified athletic trainers.
All rehabilitation was performed in the sports medicine facilities under the close supervision of the athletic training staff. As with many other competitive teams, the rehabilitation process is intensive and extensive and must be completed before allowing return to practice and then to game competition. The rehabilitation protocol was not innovative or different from many published protocols, but rather it focused on very regular frequent communication preoperatively, postoperatively, and during the progression of activity after surgery. Communication and examination among the athlete, physical therapist, athletic trainer, conditioning coach, and surgeon were imperative for success. Particularly near the time for return, functional and psychological preparation was reviewed and discussed on a weekly basis. RTS was only determined when the athlete, the rehabilitation and athletic training staff, and the surgeon were completely satisfied with the athlete’s readiness to return. RTS was defined as return to full participation as part of the competitive sports team without restriction, consistent with the 2016 consensus statement from the First World Congress in Sports Physical Therapy.5 All the athletes were regularly followed throughout the duration of their collegiate career. All data were stratified according to sport and sex. Routine descriptive statistics were used to summarize the data.
Results
Table 1 summarizes some basic characteristics of our study sample. Between 2001 and 2013, a total of 75 athletes underwent 81 ACLR procedures (73 primary, 8 revision) with 6 bilateral subsequent procedures (not revisions to the same knee): 19 freshmen, 22 sophomores, 25 juniors, and 9 seniors (Table 1).
Table 1.
Summary of Patient Data by Sexa
| Male (n = 40) | Female (n = 35) | Overall (N = 75) | |
|---|---|---|---|
| Age, y, mean ± SD | 20.5 ± 1.57 | 19.4 ± 1.31 | 20.1 ± 1.58 |
| BMI, mean ± SD | 28.8 ± 4.1 | 23.4 ± 2.2 | 25.9 ± 4.3 |
| Collegiate class, n | |||
| Freshman | 10 | 9 | 19 |
| Sophomore | 12 | 10 | 22 |
| Junior | 13 | 12 | 25 |
| Senior | 5 | 4 | 9 |
| No. of surgeries (mean RTS, mo) | |||
| Athletics (track and field) | 1 (11.7) | 0 | 1 (11.7) |
| Basketball | 3 (7.8) | 4 (8.9) | 7 (8.7) |
| Cheerleading | 0 | 2 (4.2) | 2 (8.4) |
| Dance | 0 | 2 (7.1) | 2 (7.1) |
| Field hockey | 0 | 3 (7.3) | 3 (7.3) |
| American football | 27 (6.9) | 0 | 27 (6.9) |
| Gymnastics | 2 (8.6) | 6 (7.1) | 8 (7.5) |
| Soccer | 0 | 10 (11.5) | 10 (11.5) |
| Softball | 0 | 3 (8.6) | 3 (8.6) |
| Volleyball | 0 | 6 (6.7) | 6 (6.7) |
| Wrestling | 12 (6.7) | 0 | 12 (6.7) |
| Overall sport | 45 (7.0) | 36 (8.1) | 81 (8.2) |
aBMI, body mass index; RTS, return to sport.
The mean age was 20.1 years (range, 17-24 years); 40 of the 75 athletes (53%) were men, and 35 (47%) were women. For male athletes, 60% of all ACL tears occurred in football. For female athletes, 29% of injuries occurred in soccer. In men, 98% of the reconstructions used a bone–patellar tendon–bone (BPTB) autograft. In women, the BPTB autograft was used in 48%, and a hamstring autograft was used in 40% (Table 2).
Table 2.
Frequency of Graft Tissue Used by Tissue Type, Sport, and Sexa
| BPTB | Hamstring | BPTB Allo | Tib Ant Allo | Overall | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | F | All | M | F | All | M | F | All | M | F | All | M | F | |
| Athletics | 1 | — | 1 | — | — | — | — | — | — | — | — | — | 1 | — |
| Basketball | 3 | 2 | 5 | — | 2 | 2 | — | — | — | — | — | — | 3 | 4 |
| Cheerleading | — | — | — | — | 2 | 2 | — | — | — | — | — | — | — | 2 |
| Dance | — | — | — | — | 1 | 1 | — | — | — | — | 1 | 1 | — | 2 |
| Field hockey | — | 1 | 1 | — | 1 | 1 | — | — | — | — | 1 | 1 | — | 3 |
| American football | 26 | — | 26 | — | — | — | — | — | — | 1 | — | 1 | 27 | — |
| Gymnastics | 2 | 4 | 6 | — | 2 | 2 | — | — | — | — | — | — | 2 | 6 |
| Soccer | — | 6 | 6 | — | — | — | — | 1 | 1 | — | 3 | 3 | — | 10 |
| Softball | — | 2 | 2 | — | 1 | 1 | — | — | — | — | — | — | — | 3 |
| Volleyball | — | — | — | — | 6 | 6 | — | — | — | — | — | — | — | 6 |
| Wrestling | 11 | 11 | — | — | — | 1 | — | 1 | — | — | — | 12 | — | |
| Overall | 43 | 15 | 58 | — | 15 | 15 | 1 | 1 | 2 | 1 | 5 | 5 | 45 | 36 |
aDashes indicate no value for that field. Allo, allograft; BPTB, bone–patellar tendon–bone; F, female; M, male; Tib Ant, tibialis anterior.
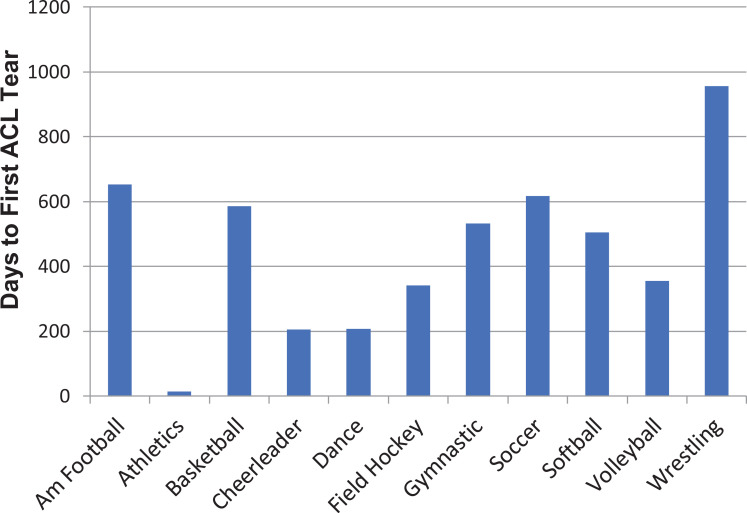
The mean number of days from the onset of collegiate training to the first ACL tear varied by sport (Figure 1).
Figure 1.
Mean number of days from the onset of collegiate training to first anterior cruciate ligament (ACL) tear by sport. Day 1 = first day of training as a freshman. Am, American.
All of the ACL tears in cheerleading and in dance occurred in the athlete’s first year of training. In wrestling, however, two-thirds of the injuries occurred in the athlete’s junior or senior season. A total of 49 associated lesions were found during either evaluation or surgery. There were an additional 40 procedures performed at the time of surgery (Table 3).
Table 3.
Associated Lesions and Other Procedures Performed During the Index Surgery by Sex
| Male | Female | Overall | |
|---|---|---|---|
| Associated lesions | |||
| Lateral meniscal tear | 13 | 7 | 20 |
| Medial meniscal tear | 6 | 4 | 10 |
| Medial collateral ligament tear | 6 | 3 | 9 |
| Medial and lateral meniscal tears | 2 | 1 | 3 |
| Lateral collateral ligament tear | 0 | 1 | 1 |
| Posterolateral corner avulsion | 0 | 1 | 1 |
| Other lesions | |||
| Tibial plateau fracture | 1 | 0 | 1 |
| Medial condyle chondral defect | 1 | 0 | 1 |
| Posterolateral corner injury | 1 | 0 | 1 |
| Patellofemoral ligament avulsion | 0 | 1 | 1 |
| Medial collateral ligament sprain | 0 | 1 | 1 |
| Concomitant procedures | |||
| Partial meniscectomy | 11 | 4 | 15 |
| Meniscal repair/reconstruction | 9 | 5 | 14 |
| Medial collateral ligament repair/reconstruction | 6 | 3 | 9 |
| Posterolateral corner repair/reconstruction | 0 | 1 | 1 |
| Lateral collateral ligament repair/reconstruction | 0 | 1 | 1 |
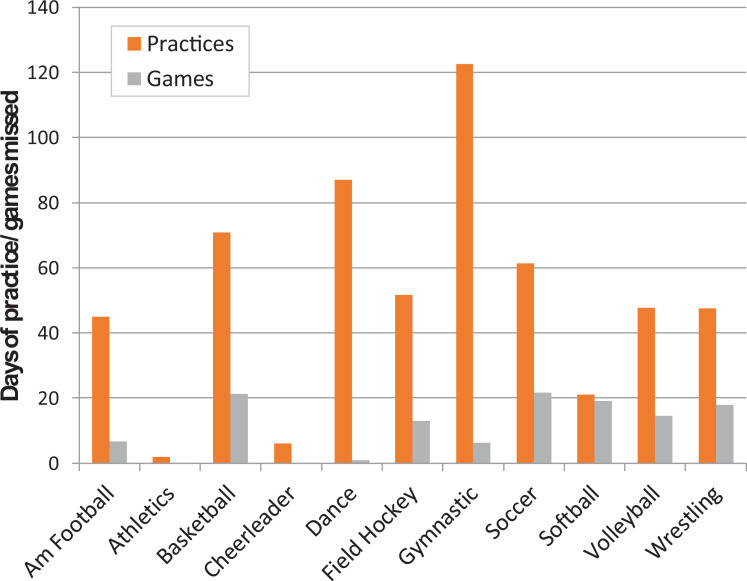
The overall rate of return to competitive sport activities was 92% (69 of 75 patients) at an average of 8.2 months (range, 3-16 months) from surgery. Table 1 presents the mean months to RTS by sex and sport. The numbers of practices and games missed are shown in Figure 2.
Figure 2.
Mean numbers of practice and competition days missed by sport. Am, American.
Differences among sports reflected the unique training and competitive calendar of the various sports.
Of the 75 athletes, 69 (92%) returned to play in their original sport or changed sports (males, 98%; females, 89%). Nine athletes (12%) initially retired from collegiate sports—4 left for medical reasons, 1 graduated, and 4 left for personal reasons. Of these 9, 3 returned to sport activities after leaving the university (1 football player went to the NFL, another football player switched to professional wrestling, and 1 basketball player underwent an ACL revision surgery before returning to training and competition).
Among the 69 athletes who returned to sport, 65 continued to play their sport until the end of their collegiate career (mean, 19.3 remaining months of collegiate eligibility). The remaining 4 athletes were still eligible and engaged with their respective teams at the close of data. The average duration of participation after returning to full-time sport participation reflected their remaining eligibility (approximately 8 months for senior athletes, 14 months for juniors, 22 months for sophomores, and 27 months for freshmen).
After ACLR, 23 reoperations (31%) were performed (Table 4); the mean time between the primary ACLR and the first reoperation was 58.3 weeks (range, 4-148 weeks). Eight of the 75 athletes (11%) experienced an ACL graft retear an average time of 15.3 months (range, 8-24 months) after the index reconstruction.
Table 4.
Frequency of Repeat Surgeries by Sporta
| Meniscal Lesion | ACL Rerupture | Knee Derangement | Painful Hardware | Other | |
|---|---|---|---|---|---|
| American football | 1 | 1 | 2 | — | 1 |
| Basketball | 1 | 3 | 1 | 1 | — |
| Field hockey | — | — | — | — | — |
| Gymnastics | 1 | 1 | — | 1 | — |
| Soccer | — | 2 | — | 1 | 1 |
| Softball | — | — | 1 | 1 | — |
| Volleyball | — | 1 | 1 | — | — |
| Wrestling | — | — | 1 | — | — |
aDashes indicate no value for that field. ACL, anterior cruciate ligament.
Discussion
There has been considerable interest in the recent literature about the rate of RTS after ACL injury and reconstruction. In published reports, the rate of return to competitive sport has varied anywhere from 33% in competitive-level Australian team-sport athletes8 to 98% in NBA players.25 In our retrospective single-center study, we assessed RTS rates among Division I National Collegiate Athletic Association (NCAA) athletes who underwent ACLR.
Our overall RTS rate was 92% (95% male, 88.75% female), which compares favorably with published systematic reviews on return to competitive sport in collegiate and professional athletes.29,33,38 Consider American football. Erickson and coworkers21 reported that 92% of NFL quarterbacks successfully returned to professional football after a mean of 13 months. Kamath et al27 reported that 88.3% of Division I football players were able to RTS for a minimum of 1 season after reconstruction and 77% were able to complete their remaining collegiate eligibility. Shah and colleagues39 reported an overall rate of 63% (31/49) of NFL athletes getting back to their preinjury level at an average of 10.8 months after surgery. In a study from the Multicenter Orthopaedic Outcomes Network group, McCullough et al31 reported on 26 collegiate football players, of whom 69% returned to play after surgery.
In basketball, Busfield et al13 reported that of 27 NBA players undergoing ACLR, 21 (78%) returned to the professional level. Harris et al25 reported that 98% of NBA players returned to some level of professional play (NBA, D-League, international) the next season (11.6 months after surgery).
Data on soccer are largely from professional players. Collegiate RTS data are limited to a 1-year analysis of female soccer players from a single athletic conference26 where the RTS rate for 80 players was 85%. The rate was highest for players on a scholarship (91% vs 46%) and for younger players (those with the most remaining eligibility). Two papers have discussed outcomes in Major League Soccer (MLS) professionals. The first report20 was based on data between 1996 and 2012, and 52 injured players met the inclusion criteria (league matches both before and after surgery). Of the 52 players, 77% were able to return to competition, most of whom (98%) returned the following season (10 months). Of interest was that the players who had undergone ACLR performed better (number of games played, total shots, shots on goal, assists) than did matched controls. The second report summarized the 2014 to 2016 MLS seasons.9 This 2-year study showed that 74% of 54 players were able to return, but when compared with control players, the injured players had a shorter career duration in the MLS (1.3 vs 2.5 years), started fewer games, and played fewer minutes. A study on European-based professionals35 analyzed outcomes in the 2 highest levels of professional play for the 2010 to 2011 and 2011 to 2012 seasons from 5 major European leagues. The RTS rate for 125 injured players was 98% (mean, 209 days), of which 59% were able to return to the same level of competition. Five years post-ACLR, 70% were still playing, but only 25% were still playing at their preinjury level (vs 87% of controls).
Studies on high school athletes and other nonprofessional athletes have shown a wide range of RTS rates. Shelbourne et al40 surveyed 402 middle school– and high school–aged basketball and soccer players after ACLR. Survey results showed that 87% of female and male basketball players returned at a mean of 5.2 and 5.3 months, respectively, after surgery. Soccer players (n = 102) were able to return to low-level soccer activities (women, 5.3 weeks; men, 5.8 weeks), and 93% of girls and 80% of boys returned to soccer when they felt they were able to compete (both sexes, 5.1 months). Interestingly, 33% of the girls and 24% of the boys continued to play soccer in college when the NCAA data suggest that only about 5% to 6% of high school players go on to play soccer in college.34
McCullough et al31 reported that a total of 63% of a high school–aged cohort of football players had returned to play at the 2-year follow-up. Ardern and coworkers8 reported that only 33% of 503 athletes in competitive-level Australian rules football, basketball, netball, and soccer had attempted to return to competitive sport within 12 months.
It is entirely possible that returning an athlete to play too soon may lead to injury of the reconstructed ligament, requiring a revision surgery, or an injury to the contralateral knee. From the Swedish ACLR registry, 4.1% of 15,394 patients underwent a revision surgery, while 5% required surgery to their contralateral knee.2 A systematic review of 21 studies with 1641 patients reported reinjury rates ranging from 0% to 24%, with an overall rate of 7.2%. Contralateral injuries were fewer (2.25%).11 A single Division I university noted that athletes who arrived at the university with an ACLR (n = 35) had a 17% reinjury rate and a 20% rate of contralateral knee injury. Athletes who had an ACLR while in college (n = 54) had a 2% reinjury rate and an 11% rate of contralateral knee injury.26 A systematic review published in 2018 focused on RTS criteria and reinjury,30 reporting that 14% of athletes who met RTS criteria nevertheless experienced a second ACL injury (reinjury or contralateral injury). Time from surgery to RTS assessment or to second injury is not a variable that was routinely reported.
Sport-specific data, while more limited in terms of patient numbers, also have shown similar variability. For example, 8% of NFL quarterbacks (1/13) experienced a reinjury,21 while Dodson and coworkers17 reported that 12.3% of 219 injuries in players at all NFL positions were retears and 7.3% were contralateral injuries. For high school basketball, the retear rates were 7% and 13.8% for female and male athletes, respectively, roughly 2 years after the index surgery, while contralateral tear rates were 16.1% and 12.1% for female and male athletes, respectively, at 30 and 34 months after the index surgery.40 In the NBA, ACL tears are quite rare (0.7% of all game-related injuries16). Such injuries are more frequent in the Women’s NBA (1.9% of all game-related injuries16), especially in White versus non-White European American players (0.45 vs 0.07 per 1000 athlete-exposures).45 To date, discussions surrounding retear rates continue to evolve.
The data for soccer are also quite variable. Reinjury in high school players occurred in 24% and 13% of male and female athletes, respectively.40 This relationship of injury was reversed, with 8% and 19% of male and female athletes, respectively, sustaining an injury to the contralateral knee.40 In a wider range of ages, Allen et al3 found that 11% of female players sustained a reinjury within an average of 24 months and 17% experienced an ACL tear in the contralateral knee within 32 months. After ACLR, between 4%9 and 10%20 of MLS players sustained a reinjury. Of 21 Italian professionals with an ACLR, only 1 (5%) experienced a reinjury.48 Other European data have suggested that only 3% experienced a reinjury.47 While it is difficult to compare rates because of methodological differences (eg, medical records vs surveys), it is likely that the lower reinjury rates may be attributable to the quality and supervision of rehabilitation at the professional level. The higher rate of retear among school-aged athletes is in line with the currently available data, supporting the belief that the younger the age, the higher the risk of retear.2,19,32,37,46
Our finding of a high RTS among collegiate athletes of mixed sports (92%) compares favorably with the current literature. We believe that the synergistic cooperation among the surgeons, physical therapists, and athletic trainers in the postoperative period is essential for success. Weekly follow-up by the surgeon, together with daily technical and psychological support from the physical therapists and athletic trainers, can overcome some of the psychological factors that can affect RTS.6,23,28,44
An increasing number of studies have concluded that, in addition to a technically successful ACLR and an outstanding rehabilitation program, there are psychological factors that may prevent athletes from returning to sport at the same or higher level. For example, Tjong et al44 interviewed 31 patients aged 18 to 40 years after they underwent primary ACLR surgery and found 3 overarching themes: fear, lifestyle changes, and innate personality traits. These factors influenced the decision to RTS and to return at the preinjury level. Less relevant factors were the surgeon’s advice not to return, depressed mood, and persistent knee pain. Ardern and colleagues6 showed that psychological responses (readiness to return, fear of reinjury, sport locus of control, estimated number of months to return to play) observed before surgery and 4 months after surgery were predictive of athletes returning to their preinjury level of sport at 12 months. Although we did not investigate the reasons contributing to RTS, we maintain that a comprehensive approach with the surgeon and rehabilitation staff is essential to support the athlete through the rehabilitation process in order to determine when the athlete is ready. Most of this support is provided by the daily interaction with the athlete’s assigned physical therapist to help the athlete with sport-specific drills in a controlled environment during his or her early rehabilitation period. This gradual regimen in increasing sport-specific drills overcomes fear of reinjury and favors neuromuscular control recovery.
The strengths of the study are the cohort size made up of male and female athletes attending a single university, from multiple sports, and competing at the highest level of collegiate competition and the long follow-up period. Limitations of the study include its being a retrospective review (evidence level 4), as well as the lack of functional outcomes and data on the athletes’ performance ratings. Inclusion of functional outcomes, psychological tests, and sport-specific player efficiency rating measures will assess how physical and psychological status influence the RTS decision and subsequent performance. The inclusion of multiple surgeons and techniques can be viewed as a limitation. Including multiple surgeons adds technical variability, and the use of differing techniques only adds to the difficulty in arriving at specific conclusions. Having said that, we found no evidence of any systematic pattern of failure for any specific surgeon or surgical technique. On the other hand, this might also be a strength because the outcomes are representative of the process of reconstruction and not a testament to an individual surgeon’s skill or to outcomes specific to a single technique or choice of procedure. Technique selection was determined on a case-by-case basis based on both patient and surgeon factors. It could be argued that making no a priori effort to ensure similar characteristics between and among the procedures could be a study weakness or a strength. This could be a weakness in that we cannot make any suggestion of procedure choice according to selected patient characteristics. It could be a strength in that the results, as mentioned, are about outcomes of reconstruction and not about outcomes from a specific procedure. We are aware that the limited number of cases in the various subgroups of surgical procedures (eg, isolated ACLR, ACLR + meniscus, ACLR + cartilage, and ACLR + other ligament) adds variation to rehabilitation duration, RTS expectations, and outcomes that can limit the generalizability of the data to those subgroups. In spite of this limitation, our results are generally representative of ACLR outcomes. Data regarding outcomes for the reconstructions with additional procedures continue to evolve.
Conclusion
In this series, the overall RTS rate in Division I NCAA athletes from a single institution was 92% at an average of 8.2 months and compares favorably with the rates reported in comparable studies in the literature. The strict follow-up by the surgeon, together with the high-profile, frequent, almost daily technical and psychological support given by mainly the athletic trainers during the recovery period, seemed to contribute to preparing the athletes for a competitive rate of RTS to their preinjury level.
Acknowledgment
The authors greatly appreciate the professional editorial and publication assistance provided by Donald T. Kirkendall, ELS.
Footnotes
Final revision submitted June 5, 2020; accepted July 7, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: C.M.H. has received hospitality payments from Tornier. M.J.B. has received speaking fees from Arthrex. B.R.W. has received educational support from Wardlow Enterprises and consulting fees and speaking fees from Linvatec. A.A. has received consulting fees, speaking fees, and royalties from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Iowa (ID No. 201206718).
References
- 1. Agel J, Rockwood T, Klossner D. Collegiate ACL injury rates across 15 sports: National Collegiate Athletic Association Injury Surveillance System data update (2004-2005 through 2012-2013). Clin J Sport Med. 2016;26(6):518–523. [DOI] [PubMed] [Google Scholar]
- 2. Ahldén M, Samuelsson K, Sernert N, et al. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012;40(10):2230–2235. [DOI] [PubMed] [Google Scholar]
- 3. Allen MM, Pareek A, Krych AJ, et al. Are female soccer players at an increased risk of second anterior cruciate ligament injury compared with their athletic peers? Am J Sports Med. 2016;44(10):2492–2498. [DOI] [PubMed] [Google Scholar]
- 4. Anderson AF, Snyder RB, Lipscomb AB., Jr Anterior cruciate ligament reconstruction: a prospective randomized study of three surgical methods. Am J Sports Med. 2001;29(3):272–279. [DOI] [PubMed] [Google Scholar]
- 5. Ardern CL, Glasgow P, Schneiders A, et al. 2016 consensus statement on return to sport from the First World Congress in Sports Physical Therapy, Bern. Br J Sports Med. 2016;50(14):853–864. [DOI] [PubMed] [Google Scholar]
- 6. Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41(7):1549–1558. [DOI] [PubMed] [Google Scholar]
- 7. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45(7):596–606. [DOI] [PubMed] [Google Scholar]
- 8. Ardern CL, Webster KE, Taylor NF, Feller JA. Return to the preinjury level of competitive sport after anterior cruciate ligament reconstruction surgery: two-thirds of patients have not returned by 12 months after surgery. Am J Sports Med. 2011;39(3):538–543. [DOI] [PubMed] [Google Scholar]
- 9. Arundale AJH, Silvers-Granelli HJ, Snyder-Mackler L. Career length and injury incidence after anterior cruciate ligament reconstruction in Major League Soccer players. Orthop J Sports Med. 2018;6(1):2325967117750825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Baer GS, Harner CD. Clinical outcomes of allograft versus autograft in anterior cruciate ligament reconstruction. Clin Sports Med. 2007;26(4):661–681. [DOI] [PubMed] [Google Scholar]
- 11. Barber-Westin SD, Noyes FR. Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: a systematic review. Phys Sportsmed. 2011;39(3):100–110. [DOI] [PubMed] [Google Scholar]
- 12. Brophy RH, Gill CS, Lyman S, et al. Effect of anterior cruciate ligament reconstruction and meniscectomy on length of career in National Football League athletes: a case control study. Am J Sports Med. 2009;37(11):2102–2107. [DOI] [PubMed] [Google Scholar]
- 13. Busfield BT, Kharrazi FD, Starkey C, Lombardo SJ, Seegmiller J. Performance outcomes of anterior cruciate ligament reconstruction in the National Basketball Association. Arthroscopy. 2009;25(8):825–830. [DOI] [PubMed] [Google Scholar]
- 14. Carey JL, Huffman GR, Parekh SG, Sennett BJ. Outcomes of anterior cruciate ligament injuries to running backs and wide receivers in the National Football League. Am J Sports Med. 2006;34(12):1911–1917. [DOI] [PubMed] [Google Scholar]
- 15. Daruwalla JH, Greis PE, Hancock R, Xerogeanes JW. Rates and determinants of return to play after anterior cruciate ligament reconstruction in NCAA Division 1 college football athletes: a study of the ACC, SEC, and PAC-12 conferences. Orthop J Sports Med. 2014;2(8):2325967114543901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Deitch JR, Starkey C, Walters SL, Moseley JB. Injury risk in professional basketball players: a comparison of Women’s National Basketball Association and National Basketball Association athletes. Am J Sports Med. 2006;34(7):1077–1083. [DOI] [PubMed] [Google Scholar]
- 17. Dodson CC, Secrist ES, Bhat SB, Woods DP, Deluca PF. Anterior cruciate ligament injuries in National Football League athletes from 2010 to 2013: a descriptive epidemiology study. Orthop J Sports Med. 2016;4(3):2325967116631949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dunn WR, Spindler KP; Consortium M. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(10):2040–2050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Edwards PH, Grana WA. Anterior cruciate ligament reconstruction in the immature athlete: long-term results of intra-articular reconstruction. Am J Knee Surg. 2001;14(4):232–237. [PubMed] [Google Scholar]
- 20. Erickson BJ, Harris JD, Cvetanovich GL, et al. Performance and return to sport after anterior cruciate ligament reconstruction in male Major League Soccer players. Orthop J Sports Med. 2013;1(2):2325967113497189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Erickson BJ, Harris JD, Heninger JR, et al. Performance and return-to-sport after ACL reconstruction in NFL quarterbacks. Orthopedics. 2014;37(8):e728–e734. [DOI] [PubMed] [Google Scholar]
- 22. Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31(4):564–573. [DOI] [PubMed] [Google Scholar]
- 23. Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):1021–1028. [DOI] [PubMed] [Google Scholar]
- 24. Gottlob CA, Baker CL, Jr, Pellissier JM, Colvin L. Cost effectiveness of anterior cruciate ligament reconstruction in young adults. Clin Orthop Relat Res. 1999;367:272–282. [PubMed] [Google Scholar]
- 25. Harris JD, Erickson BJ, Bach BR, Jr, et al. Return-to-sport and performance after anterior cruciate ligament reconstruction in National Basketball Association players. Sports Health. 2013;5(6):562–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Howard JS, Lembach ML, Metzler AV, Johnson DL. Rates and determinants of return to play after anterior cruciate ligament reconstruction in National Collegiate Athletic Association Division I soccer athletes: a study of the Southeastern Conference. Am J Sports Med. 2015;44(2):433–439. [DOI] [PubMed] [Google Scholar]
- 27. Kamath GV, Murphy T, Creighton RA, et al. Anterior cruciate ligament injury, return to play, and reinjury in the elite collegiate athlete: analysis of an NCAA Division I cohort. Am J Sports Med. 2014;42(7):1638–1643. [DOI] [PubMed] [Google Scholar]
- 28. Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):393–397. [DOI] [PubMed] [Google Scholar]
- 29. Lai CCH, Ardern CL, Feller JA, Webster KE. Eighty-three per cent of elite athletes return to preinjury sport after anterior cruciate ligament reconstruction: a systematic review with meta-analysis of return to sport rates, graft rupture rates and performance outcomes. Br J Sports Med. 2018;52(2):128–138. [DOI] [PubMed] [Google Scholar]
- 30. Losciale JM, Zdeb RM, Ledbetter L, Reiman MP, Sell TC. The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: a systematic review with meta-analysis. J Orthop Sports Phys Ther. 2018;49(2):43–54. [DOI] [PubMed] [Google Scholar]
- 31. McCullough KA, Phelps KD, Spindler KP, et al. Return to high school- and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40(11):2523–2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. McIntosh AL, Dahm DL, Stuart MJ. Anterior cruciate ligament reconstruction in the skeletally immature patient. Arthroscopy. 2006;22(12):1325–1330. [DOI] [PubMed] [Google Scholar]
- 33. Mohtadi NG, Chan DS. Return to sport-specific performance after primary anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2018;46(13):3307–3316. [DOI] [PubMed] [Google Scholar]
- 34. National Collegiate Athletic Association. Facts about NCAA sports. NCAA; 2009 Accessed Februrary 8, 2021 https://ncaaorg.s3.amazonaws.com/compliance/recruiting/NCAA_RecruitingFactSheet.pdf
- 35. Niederer D, Engeroff T, Wilke J, Vogt L, Banzer W. Return to play, performance and career duration after ACL rupture: a case-control study in the five biggest football nations in Europe. Scand J Med Sci Sports. 2018;28(10):2226–2233. [DOI] [PubMed] [Google Scholar]
- 36. Rugg CM, Wang D, Sulzicki P, Hame SL. Effects of prior knee surgery on subsequent injury, imaging, and surgery in NCAA collegiate athletes. Am J Sports Med. 2014;42(4):959–964. [DOI] [PubMed] [Google Scholar]
- 37. Sankar WN, Carrigan RB, Gregg JR, Ganley TJ. Anterior cruciate ligament reconstruction in adolescents: a survivorship analysis. Am J Orthop (Belle Mead NJ). 2008;37(1):47–49. [PubMed] [Google Scholar]
- 38. Sepulveda F, Sanchez L, Amy E, Micheo W. Anterior cruciate ligament injury: return to play, function and long-term considerations. Curr Sports Med Rep. 2017;16(3):172–178. [DOI] [PubMed] [Google Scholar]
- 39. Shah VM, Andrews JR, Fleisig GS, McMichael CS, Lemak LJ. Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med. 2010;38(11):2233–2239. [DOI] [PubMed] [Google Scholar]
- 40. Shelbourne KD, Sullivan AN, Bohard K, Gray T, Urch SE. Return to basketball and soccer after anterior cruciate ligament reconstruction in competitive school-aged athletes. Sports Health. 2009;1(3):236–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shrier I. Strategic Assessment of Risk and Risk Tolerance (StARRT) framework for return-to-play decision-making. Br J Sports Med. 2015;49(20):1311–1315. [DOI] [PubMed] [Google Scholar]
- 42. Smith FW, Rosenlund EA, Aune AK, MacLean JA, Hillis SW. Subjective functional assessments and the return to competitive sport after anterior cruciate ligament reconstruction. Br J Sports Med. 2004;38(3):279–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Spindler KP, Wright RW. Clinical practice: anterior cruciate ligament tear. N Engl J Med. 2008;359(20):2135–2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Tjong VK, Murnaghan ML, Nyhof-Young JM, Ogilvie-Harris DJ. A qualitative investigation of the decision to return to sport after anterior cruciate ligament reconstruction: to play or not to play. Am J Sports Med. 2014;42(2):336–342. [DOI] [PubMed] [Google Scholar]
- 45. Trojian TH, Collins S. The anterior cruciate ligament tear rate varies by race in professional women’s basketball. Am J Sports Med. 2006;34(6):895–898. [DOI] [PubMed] [Google Scholar]
- 46. van Eck CF, Schkrohowsky JG, Working ZM, Irrgang JJ, Fu FH. Prospective analysis of failure rate and predictors of failure after anatomic anterior cruciate ligament reconstruction with allograft. Am J Sports Med. 2012;40(4):800–807. [DOI] [PubMed] [Google Scholar]
- 47. Waldén M, Hagglund M, Magnusson H, Ekstrand J. ACL injuries in men’s professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL rupture. Br J Sports Med. 2016;50(12):744–750. [DOI] [PubMed] [Google Scholar]
- 48. Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, et al. Return to sport after anterior cruciate ligament reconstruction in professional soccer players. Knee. 2014;21(3):731–735. [DOI] [PubMed] [Google Scholar]