Abstract
We propose a theoretical model of insomnia symptoms and non‐suicidal self‐injury (NSSI) that posits bidirectional linkages. We hypothesised that heightened depressive symptoms and impulsivity that result from insomnia increase NSSI. We also posit that the shame associated with NSSI triggers repetitive negative thinking, in turn increasing insomnia. Using three longitudinal waves of questionnaire data collected annually from a sample of Swedish adolescents (n = 1,457; M age = 13.2, SD = 0.43; 52.7% boys), we assessed the mediating role of depressive symptoms, impulsivity, rumination, and worry on the link between insomnia and NSSI. After controlling for depressive symptoms, we found that insomnia was related to increases in NSSI from the second to the third time point (ß 23 = 0.09, p = .01). NSSI was consistently related to increased insomnia (ß 12 = 0.09, p = .01; ß 23 = 0.11, p < .001). In addition, depressive symptoms (ß ind = 0.01, p = .02), but not impulsivity (ß ind = 0.01, p = .09), mediated the path from insomnia to increased NSSI. Neither worry (ß ind = 0.00, p = .59) nor rumination (ß ind = 0.00, p = .96) mediated the link between NSSI and increased insomnia. We conclude that NSSI and insomnia maintain each other over time. Thus, screening adolescents for insomnia symptoms may help identify those at risk of NSSI. Although depression seems to explain why insomnia is a risk factor for NSSI, further studies should investigate why NSSI plays a role in the maintenance of insomnia. This understanding will lay the foundation for intervention.
Keywords: adolescence, bidirectional, insomnia, mechanisms, NSSI
1. INTRODUCTION
Sleep complaints, especially problems falling asleep, increase dramatically during adolescence (e.g. Ghekiere et al., 2019). Adolescents who sleep poorly also report more health‐risk behaviours (de Zambotti, Goldstone, Colrain, & Baker, 2018), including non‐suicidal self‐injury (NSSI; e.g. Lundh, Bjärehed, & Wångby‐Lundh, 2013; Wong, Brower, & Zucker, 2011). Although important, studies on the association between sleep and NSSI have three major limitations. First, many rely on poor quality measures. Second, they assume that sleep difficulties precede NSSI, but lack a guiding theoretical model that justifies this assumption. Third, they do not provide information about why adolescents who have sleep difficulties also engage in NSSI. In the present study, we aimed to overcome these limitations by developing and testing a theoretical model of inadequate sleep and NSSI. We examined some of the mechanisms that could explain the relations between adolescents’ sleep difficulties and NSSI.
1.1. Sleep difficulties
In line with the “Perfect Storm” model (Crowley, Wolfson, Tarokh, & Carskadon, 2018), sleep disturbances in adolescents have been attributed to biological changes (e.g. delay in sleep onset hormones), as well as psychosocial changes (e.g. school workload, worry) (Crowley et al., 2018). As a result, many adolescents experience symptoms of insomnia (Becker, Langberg, & Byars, 2015). Insomnia symptoms encompass difficulties falling asleep, staying asleep, and waking up too early, as well as non‐restorative sleep and daytime consequences (American Psychiatric Association, 2013). The rate of insomnia in adolescents is 18.5%, with somewhat higher levels among girls than boys (Hysing, Pallesen, Stormark, Lundervold, & Sivertsen, 2013). Given that insomnia has been proposed as a transdiagnostic factor in the development of a wide range of mental health problems (Harvey, Murray, Chandler, & Soehner, 2011); the rise in symptoms of insomnia (especially sleep onset difficulties) among adolescents is concerning (e.g. Ghekiere et al., 2019).
1.2. Non‐suicidal self‐injury
Non‐suicidal self‐injury (NSSI) includes direct and deliberate behaviour aimed at damaging one’s own body tissue without suicidal intent (Muehlenkamp, Claes, Havertape, & Plener, 2012). NSSI includes behaviours such as cutting or bruising one’s own skin. Sweden has some of the highest rates of NSSI in Europe, with up to 41% of adolescents engaging in NSSI at least once in their lifetimes (Muehlenkamp et al., 2012). NSSI mostly serves an emotional function, and helps adolescents to deal with emotions experienced as overwhelming or difficult to handle (e.g. Chapman, Gratz, & Brown, 2006). As this behaviour gives temporary relief from these negative emotions (e.g. Klonsky, 2009), some adolescents repeatedly engage in it each time they are negatively aroused. Although NSSI is associated with decreases in some negative emotions (e.g. depressive symptoms, loneliness, and frustration), some studies have shown an increase in others, specifically shame, guilt, and disgust, after engaging in NSSI (e.g. Jenkins & Schmitz, 2012). As adolescents who engage in NSSI are at risk of suicidal thoughts and behaviours (for a review see Andover, Morris, Wren, & Bruzzese, 2012), it is important to understand the temporal events and emotions involved in NSSI.
1.3. Sleep difficulties and NSSI
Cross‐sectional studies show that adolescents who self‐injured also reported sleep difficulties, including symptoms of insomnia (Hysing, Sivertsen, Stormark, & O'connor, 2015; Liu, Chen, Bo, Fan, & Jia, 2017; McGlinchey, Courtney‐Seidler, German, & Miller, 2017). A handful of longitudinal studies partially supported these findings, where sleep difficulties, and particularly insomnia, predicted later engagement in NSSI (Bandel & Brausch, 2020; Junker, Bjørngaard, Gunnell, & Bjerkeset, 2014; Lundh et al., 2013; Wong et al., 2011). However, this link disappeared when controlling for previous psychopathology (Bandel & Brausch, 2018; Junker et al., 2013). Although informative, these studies have limitations. First, most of them rely on dichotomised measures of NSSI (Hysing et al., 2015; Wong et al., 2011). Dichotomising removes information about individual differences and can attenuate statistical associations between variables (MacCallum, Zhang, Preacher, & Rucker, 2002). It is possible that, among other factors, these practices reduced the power to detect relationships between sleep difficulties and NSSI in previous studies. Also, some of the above mentioned studies used imprecise measures of sleep difficulties (e.g. single item or combining different sleep difficulties, such as insomnia symptoms and short sleep, into one measure) (Lundh et al., 2013; McGlinchey et al., 2017). Second, in the few studies using longitudinal data it was assumed that sleep difficulties precede NSSI, the alternative direction was not tested (Lundh et al., 2013; Wong et al., 2011). Third, none of the previous studies investigated potential mechanisms linking sleep difficulties and NSSI.
1.4. Proposed theoretical model
To the best of our knowledge, there is no clear theory that explains the association between sleep difficulties and NSSI. Several functional models of NSSI (e.g. Chapman et al., 2006) have proposed and identified triggers of this behaviour. Most evidence suggests that NSSI acts as an automatic negative reinforcer (e.g. Klonsky, 2007). That is, when stressful experiences evoke negative emotions perceived as overwhelming and difficult to handle, adolescents use NSSI as a coping strategy to decrease or eliminate such negative arousal. In addition to the substantial evidence that supports this model more generally, studies have identified two possible ways that negative emotions are linked to NSSI. First, strong evidence suggests that NSSI is a strategy to specifically deal with depressive symptoms (e.g. Nixon, Cloutier, & Jansson, 2008). Second, studies have shown that adolescents who engage in NSSI tend to report high levels of physiological reactivity in response to stress, as well as inability to act on the basis of choice rather than impulses (e.g. Lockwood, Daley, Townsend, & Sayal, 2017). Adolescents who experience sleep disturbances report subsequent depressive symptoms (Lovato & Gradisar, 2014). Also, insomnia and consequent sleep loss seem to hinder the ability to control impulses (e.g. Bauducco, Salihovic, & Boersma, 2019). Based on these theoretical and empirical premises, we postulate a theoretical model that suggests that insomnia symptoms act as a stressor (Palmer & Alfano, 2017), making adolescents more likely to experience depressive symptoms and impulsive behaviours, and use NSSI as a coping strategy.
The other direction of effects is also theoretically viable. Consistent with the hyperarousal model of insomnia (Riemann et al., 2010), individuals with insomnia experience elevated cognitive (e.g. rumination, worry, and intrusive thoughts) and physiological (e.g. cortical activity, blood pressure) arousal at bedtime, which prevents them from falling asleep and maintaining sleep (de Zambotti et al., 2018). Studies have shown that some adolescents who self‐injure often experience embarrassment and shame after the NSSI act (e.g. Jenkins & Schmitz, 2012). As people who experience shame are prone to rumination and worry (e.g. Orth, Berking, & Burkhardt, 2006) this may lead to insomnia symptoms as an indirect consequence of self‐injury. Thus, we hypothesise that engaging in NSSI makes adolescents more likely to experience rumination and worry, and thus develop symptoms of insomnia.
Integrating the functional model of NSSI (e.g. Chapman et al., 2006) and the hyperarousal model of insomnia (Riemann et al., 2010), we propose a single conceptual model of inadequate sleep and NSSI that posits bidirectional linkages. Specifically, we propose a theoretical model that sees depressive symptoms and impulsivity as mediating the relationship between insomnia symptoms and increased NSSI, as well as worry and rumination as mediating the relationship between NSSI and increased insomnia symptoms (Figure 1).
FIGURE 1.
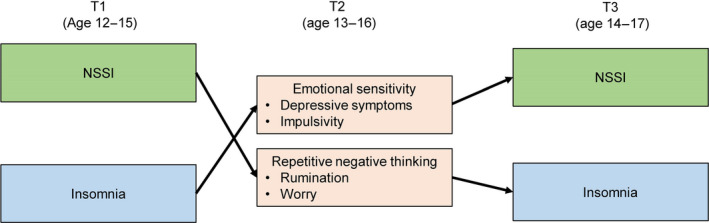
Proposed theoretical model
1.5. The present study
The present study had two aims. The first aim was to investigate the direction of effect between insomnia symptoms and NSSI, using validated measures of sleep difficulties and NSSI. The second aim was to investigate the mechanisms that explain the associations between symptoms of insomnia and NSSI. We expected that insomnia symptoms would predict increases in NSSI through depressive symptoms and impulsive behaviours. We also expected that adolescents who self‐injured would ruminate and worry, thus increasing their symptoms of insomnia.
2. METHODS
2.1. Participants
Data for the present study were drawn from the first three waves of a 5‐year longitudinal study (2014–2018), the “Three Cities Study”. The participants were 1,457 adolescents attending one of 18 public schools in three towns in central Sweden, who were followed annually from the seventh and eighth grades to high school. Retention rates were very good in the first few years (91.9% from T1 to T2; 81.3% from T1 to T3; 85.1% in all three waves, n = 1,339). Common reasons for discontinuation were that students were not present on the day of data collection or that they changed schools. We included all students who participated at T1.
At the beginning of the study, the adolescents ranged in age from 12 to 15 years (M age = 13.2, SD = 0.65). Most were boys (52.7%, n = 768) and were born in Sweden (89.2%). Most of the adolescents lived with both parents (69.9%), while the remaining alternated between parents every other week (14%), lived with only one parent (10.7% mother/2.5% father), or had other custodial arrangements (1.2%).
2.2. Procedure
Data collection took place annually during the spring. Before participation, we obtained passive consent from parents and active consent from students, who were informed of the purpose of the study, steps taken to protect their data, and their rights as participants. We used passive parental consent because its use increases participation rates and reduces sampling bias (e.g. Pokorny, Jason, Schoeny, Townsend, & Curie, 2001). All procedures were approved by the Uppsala Regional Ethics Board before the start of the study. The adolescents completed questionnaires in their classroom during school hours. During testing, trained research assistants were available for guidance, while teachers left the rooms. Each session was 90 min, with a half‐time snack break. After the session, each class received 300 Swedish crowns (~30 Euro) as a class‐wide honorarium. Adolescents who did not speak Swedish or reported other difficulties with understanding written language were excluded from the study.
2.3. Missing data and attrition analyses
As most participants had complete data (89%), we used full imputation maximum likelihood (FIML) estimation in Mplus (Muthén & Muthén, 1998–2019) to handle missing data. To test for attrition effects, we conducted a logistic regression, regressing the attrition variable (dropout = 0, retention = 1) on all our study variables. The results showed that the adolescents who reported short sleep duration were more likely to dropout (odds ratio [OR] 1.4, 95% confidence interval [CI] 1.08–1.82; p = .01). None of the other study variables predicted dropout. Thus, we concluded that attrition only minimally affected our results.
2.4. Measures
2.4.1. Insomnia symptoms
Symptoms of insomnia were assessed using the Insomnia Severity Index (ISI) (Morin, 1993). The measure includes seven items assessing the symptoms of insomnia (i.e. falling asleep, waking up during the night, or too early in the morning), overall satisfaction with sleep, interference with daily activities, and worry about current sleep. Responses used a 4‐point Likert scale, with higher scores indicating more severe sleep problems. The time frame was changed from 2 weeks (in the original) to the last 6 months to match the rest of the survey. The Cronbach’s alphas were 0.85 at T1, 0.84 at T2, and 0.87 at T3.
2.4.2. Non‐suicidal self‐injury
Non‐suicidal self‐injury was measured using a shortened version of the original Deliberate Self‐Harm Inventory (Lundh, Karim, & Quilisch, 2007). A stem was added so that participants reported only non‐suicidal injuries (Tilton‐Weaver, Marshall, & Svensson, 2019). Adolescents responded to nine items about the extent to which they had inflicted non‐lethal injuries on themselves in the last 6 months and without suicidal intent. The responses format ranged from 0 times (0) to >5 times (6) to questions such as “In the last 6 months have you…purposely cut your wrists, arms, or some other part of your body? Purposely burnt yourself with a cigarette, lighter, or matches?”. The Cronbach’s alphas for this measure were 0.86 at T1, 0.84 at T2, and 0.90 at T3.
2.4.3. Depressive symptoms
Using the Center for Epidemiologic Studies‐Depression Child Scale (CES‐DC; Olsson & von Knorring, 1997), adolescents were asked how often they experienced 16 symptoms within the last week. Examples of situations were: “I was bothered by things that don’t usually bother me”; “I wasn’t able to feel happy, even when my family or friends tried to help me feel better”. Answers ranged from not at all (1) to often (4). In our study, the scale had Cronbach’s alphas of 0.94 at T1, 0.92 at T2, and 0.93 at T3.
2.4.4. Impulsivity (Urgency)
We used 11 items from the urgency subscale of the Urgency, Premeditation, Perseverance, Sensation seeking (UPPS) impulsive behaviour scale (Whiteside & Lynam, 2001) to assess strong impulses, especially when experiencing negative feelings (e.g. “When I am upset I often act without thinking”) (a 12th item was inadvertently omitted). Responses ranged from do not agree at all (1) to agree completely (4), with higher scores indicating more impulsivity. The UPPS impulsivity behaviour scale has good psychometric properties (Whiteside & Lynam, 2001). The Cronbach’s alphas in our study were 0.85 at T1, 0.86 at T2, and 0.87 at T3.
2.4.5. Worry
We used the Penn State Worry Questionnaire for Children (PSWQ‐C; Chorpita, Tracey, Brown, Collica, & Barlow, 1997) to ask adolescents about worries that they might have about school, their family, their health, or future events. Examples of the 14 statements are: “Many things make me worry” or “Once I start worrying, I can’t stop”. Responses ranged from not at all true (0) to always true (3). The Cronbach’s alphas were 0.89 at T1, 0.92 at T2, and 0.93 at T3.
2.4.6. Rumination
To assess ruminative thoughts, we used the rumination subscale of the Children’s Response Styles Scale (CRSS; Ziegert & Kistner, 2002). Adolescents read the following statement: “When I’m feeling sad…”, and rated a series of responses, such as “I think about the other times that I felt this way” or “I think about that I should have done things differently”. The answers could range from never (1) to often (5). The Cronbach’s alphas were 0.93 at T1, 0.93 at T2, and 0.94 at T3.
2.5. Analytic plan
To investigate the longitudinal association between sleep problems and NSSI, we tested cross‐lagged path models in MPlus (Muthén & Muthén, 1998–2019) for the links between insomnia and NSSI. During adolescence, girls report more internalising problems, including depressive symptoms (e.g. Lewinsohn, Gotlib, Lewinsohn, Seeley, & Allen, 1998) and rumination (e.g. Jose & Brown, 2008), as well as insomnia symptoms (e.g. Hysing et al., 2013) than boys. Also, there are controversies on whether girls are more likely to harm themselves than boys (for review see Plener, Schumacher, Munz, & Groschwitz, 2015). In addition, adolescents who report NSSI and/or sleep difficulties are likely to experience depressive symptoms (e.g. Lovato & Gradisar, 2014). For these reasons, we controlled for gender and depressive symptoms at T1 in our analyses in order to obtain more robust results.
To investigate the mechanisms that may explain the links between sleep problems and NSSI we used mediation analyses, with depressive symptoms, impulsivity, worry, and rumination as mediators. As expected, inspection of the distributions showed that the NSSI scale was positively skewed. Therefore, we used a logarithm transformation (ln x) that reduced the skewness from 5.94 to 3.98 at T1, 5.34 to 3.45 at T2, and 5.21 to 3.7 at T3. Before interpreting the results, we used the standard fit indices to assess the quality of the statistical models. Specifically, Comparative Fit Index (CFI) >0.95, Root Mean Square Error of Approximation (RMSEA) <0.06, and Standardised Root Mean Square Residual (SRMR) <0.08 indicate an acceptable model fit (Hu & Bentler, 1999).
3. RESULTS
3.1. Descriptive and correlational analyses
Descriptive information and correlation analyses regarding the variables under study can be found in the Table S1. All variables were correlated to each other in the expected directions and at each time point (p < .001). As expected, both insomnia symptoms and NSSI were relatively rank‐order stable over time.
3.2. How are sleep problems and NSSI related over time?
We estimated the cross‐lagged association between NSSI and symptoms of insomnia. The model showed good fit: χ2(6) = 31.92, p < .001, CFI = 0.98, RMSEA = 0.05, SRMR = 0.02. After controlling for both depressive symptoms and gender, NSSI at T1 predicted increased insomnia symptoms at T2 (ß 12 = 0.09, 95% CI 0.03–0.15; p = .002), and NSSI at T2 predicted increased insomnia symptoms at T3 (ß 23 = 0.12, 95% CI 0.06–0.18; p < .001). Although insomnia symptoms at T1 did not significantly predict changes in NSSI at T2 (ß 12 = 0.02, 95% CI −0.06 to 0.09; p = .68), insomnia symptoms at T2 predicted an increase in NSSI at T3 (ß 23 = 0.09, 95% CI 0.02–0.16; p = .01); see Figure 2 for more information. These results support a bidirectional link between insomnia and NSSI, but more robust for NSSI predicting changes in symptoms of insomnia than the reverse.
FIGURE 2.
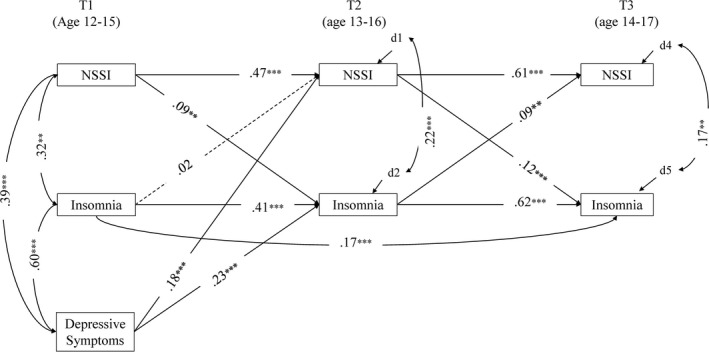
Cross‐lagged associations between NSSI and insomnia. **p < .01; ***p < .001. We controlled for gender, but for simplicity we did not include the β values in the model. The values are available on request to the first author
3.3. Which mechanisms link sleep difficulties and NSSI?
To test for mediation between sleep problems and NSSI we ran five different models. We ran the first model with all the mediators simultaneously. The first model did not have a good fit χ2(65) = 477.20, p = .00, CFI = 0.94, RMSEA = 0.07, SRMR = 0.08. So, we then ran each mediator separately. These models had much better fits. Based on the fit indices and that the models generated similar results, we decided to use these as our final models.
First, we included depressive symptoms and impulsivity as mediators between insomnia symptoms at T1 and NSSI at T3. After controlling for gender, results showed that depressive symptoms mediated the path from insomnia symptoms to increased NSSI (ß = 0.01, 95% CI 0.002–0.02, p = .02; χ2[14] = 68.78, p = .00, CFI = 0.98, RMSEA = 0.05, SRMR = 0.03). However, and after controlling for gender and depressive symptoms at T1, impulsivity did not significantly mediate the link between insomnia symptoms at T1 and NSSI at T3 (ß = 0.01, 95% CI 0.00–0.01, p = .07; χ2[16] = 72.65, p = .00, CFI = 0.98, RMSEA = 0.05, SRMR = 0.04); see Figure 3 for more information. Next, we included rumination and worry as mediators of the effect of NSSI at T1 on sleep difficulties at T3. After controlling for gender and depressive symptoms at T1, neither rumination (ß = 0.00, 95% CI −0.01 to 0.004, p = .59; χ2[16] = 99.72, p = .00, CFI = 0.97, RMSEA = 0.06, SRMR = 0.04) nor worry (ß = 0.002, 95% CI −0.01 to 0.01, p = .54; χ2[16] = 72.02, p = .00, CFI = 0.98, RMSEA = 0.05, SRMR = 0.04) were significant mediators; see Figure 3 for more detailed information.
FIGURE 3.
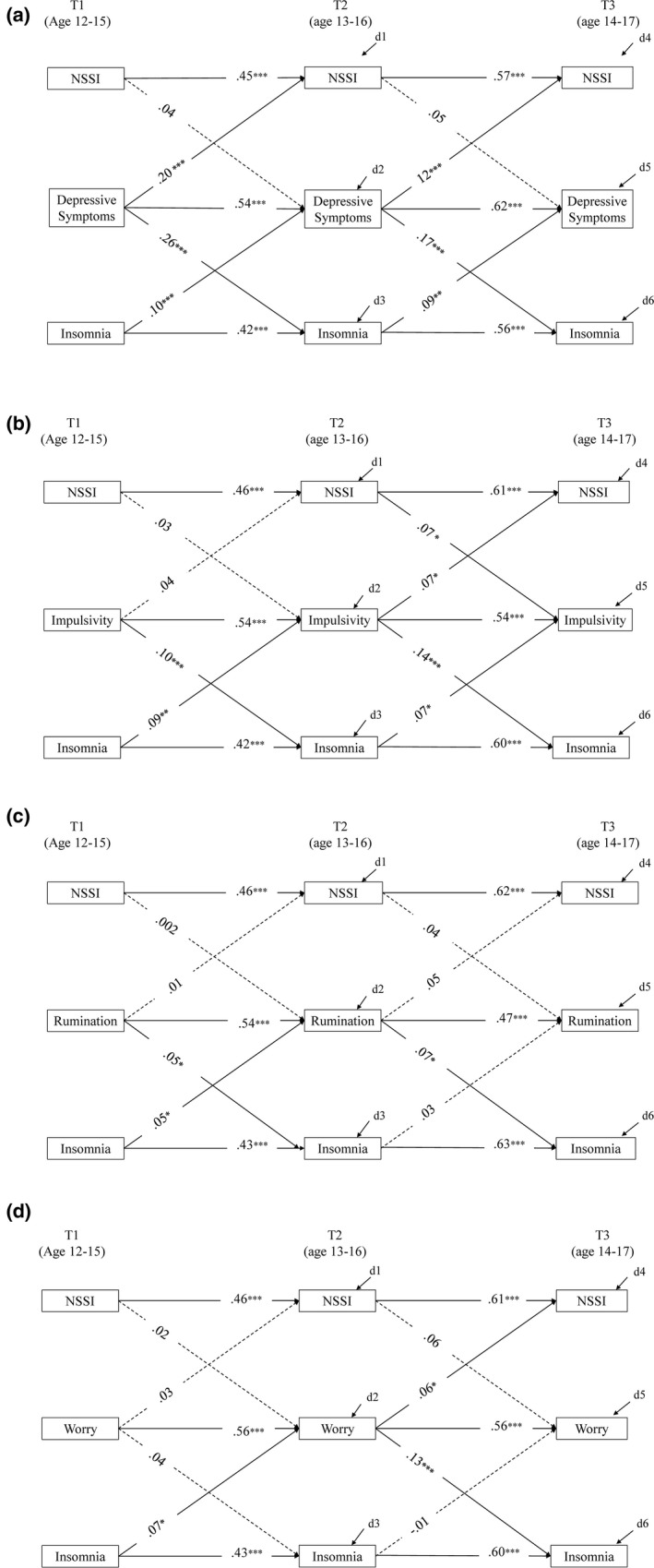
Mediators in the link between insomnia and NSSI. (a) Mediating role of depressive symptoms on the link between insomnia and NSSI. We allowed covariations between all the variables at T1, and correlations between the error terms of all variables at T2 and T3. The values are available on request to the first author. (b) Mediating role of impulsivity on the link between insomnia and NSSI. We allowed covariations between all the variables at T1, and correlations between the error terms of all variables at T2 and T3. The values are available on request to the first author. (c) Mediating role of rumination on the link between NSSI and insomnia. We allowed covariations between all the variables at T1, and correlations between the error terms of all variables at T2 and T3. The values are available on request to the first author. (d) Mediating role of worry on the link between NSSI and insomnia. We allowed covariations between all the variables at T1, and correlations between the error terms of all variables at T2 and T3. The values are available on request to the first author. *p < .05; **p < .01; ***p < .001
4. DISCUSSION
The present study examined the temporal links between insomnia symptoms and NSSI during adolescence, showing that these two problems are related over time, in a cyclical fashion. In addition, the present study provided a deeper understanding of the mechanisms that could explain these associations. Specifically, we showed that adolescents who reported insomnia symptoms were more likely to report depressive symptoms 1 year later. This, in turn, made them more likely to engage in NSSI.
With a few exceptions (e.g. Lundh et al., 2013), most studies examining the link between sleep difficulties and NSSI are cross‐sectional in nature (e.g. Hysing et al., 2015). In addition, these studies have used dichotomised measures to assess NSSI (e.g. Wong et al., 2011) or short and very broad measures of sleep difficulties (e.g. McGlinchey et al., 2017). Regardless of their design, these studies have assumed that sleep difficulties precede self‐injurious behaviours, without providing a theoretical foundation for such claims. Based on both the functional models of NSSI (e.g. Klonsky, 2007), as well as on the hyperarousal model of insomnia (Riemann et al., 2010), we proposed and tested a new theoretical model. By using three waves of data, and adopting validated measures of both insomnia symptoms and NSSI, we showed that insomnia symptoms and NSSI are reciprocally linked over time. These findings seem to challenge the unidirectional assumption that sleep problems in general, and insomnia in particular, drive NSSI.
Regarding the mechanisms behind the association between sleep disturbances and NSSI, our present results are consistent with the idea that insomnia symptoms trigger depressive symptoms and that adolescents use NSSI to cope with them. Researchers agree that NSSI is a maladaptive coping strategy for emotional distress (e.g. Klonsky, 2007, 2009) and that depressive symptoms and NSSI maintain and exacerbate each other over time (Marshall, Tilton‐Weaver, & Stattin, 2013). Insomnia, on the other hand, is a well‐established risk factor for both emotional distress and maladaptive emotion regulation (Palmer & Alfano, 2017), particularly but not limited to depression (de Zambotti et al., 2018). Thus, our present findings combined with others suggest that symptoms of insomnia may be both a transdiagnostic factor (contributing to both depressive symptoms and NSSI) and a comorbid problem.
Contrary to our expectations, impulsivity did not mediate the link between insomnia symptoms and NSSI. Also, rumination and worry did not act as mediators on the link between NSSI and insomnia symptoms. Our inability to find the proposed mediational links may be due to measurement issues. These issues include relying on one dimension of impulsivity, when other facets, such as sensation seeking, may be more important (Maxfield & Pepper, 2018); assessing rumination as a single dimension, rather than as a multidimensional construct or a general thinking style, which have different associations with psychological distress (e.g. Richmond, Hasking, & Meaney, 2017); and using a very general scale for worry. In addition, we used measures that were more trait‐like, when the impulsivity, rumination, and worry linking insomnia symptoms to NSSI may be more transitory. Future studies should further investigate the mediating roles of impulsivity, rumination, and worry using a variety of dimensions, and use designs that allows tapping into the fluctuation of these dimensions (e.g. using daily diaries).
All in all, in the present study we used two specific models for NSSI and insomnia as a basis for developing our own theoretical model. Given the fact that our present study represents the first attempt at developing a theoretical model linking symptoms of insomnia to NSSI during adolescence, we believe it is too early to know whether the lack of expected associations is due to a statistical error (e.g. Type II error) or not. In our present study, we assessed adolescents at 1‐year intervals. It may be that our hypothesised mechanisms explain the link between insomnia symptoms and NSSI in a shorter period of time. Using a design that assesses these aspects more intensely (e.g. burst design such as daily diaries, ecological momentary assessment) might allow the determination of the associations hypothesised in our model, but that our present design did not manage to detect. In addition, and given the association between other sleep difficulties (e.g. nightmares, sleep deficit) and NSSI (e.g. Ennis et al., 2017), future studies should test this model using sleep problems other than insomnia symptoms.
The present study has several strengths. First, we used a large community‐based longitudinal sample, allowing us to investigate bidirectional links between sleep problems and NSSI over 2 years. Second, this is the first study to investigate the mechanisms explaining the association between sleep disturbances and NSSI using a longitudinal design with three measurement points. Third, we used standardised measures of both insomnia symptoms and NSSI. Last, our sample included mainly Swedish adolescents. A small number of reviews show that Swedish adolescents are more likely to engage in NSSI (e.g. Muehlenkamp et al., 2012) than their European counterparts. Thus, our present findings may help Swedish practitioners to better tackle NSSI among adolescents, hopefully decreasing its frequency. However, given cultural variations, further studies are needed to replicate our present findings in other settings. Despite these strengths, the present study also has limitations. Specifically, we focussed our attention on only four possible mediators. Other potential mechanisms should be tested. For example, we assumed, but did not specifically test, the idea that insomnia generates negative arousal states leading to the use of NSSI as a way of regulating negative emotions. Future studies could focus on emotion regulation issues, confirming that the negative feelings aroused by depression. Other potential mechanisms linking dysfunctional beliefs and attitudes about sleep (e.g. beliefs about the inability to cope with the negative consequences of insomnia), as well as impaired decision‐making and problem‐solving, have been proposed as mechanisms that explain the effect of insomnia on suicidal thoughts and behaviours (for review see McCall & Black, 2013). Studies in these directions are needed.
5. CONCLUSIONS
Our present study suggests a new approach to linking sleep and NSSI, merging the functional model of NSSI (e.g. Chapman et al., 2006) with the hyperarousal model of insomnia (Riemann et al., 2010). We propose that insomnia and NSSI are bidirectionally linked via emotional, cognitive, and physiological arousal. We specifically looked at depression, impulsivity, worry and rumination but future research should replicate and further develop this model by expanding knowledge of possible mediators.
Perhaps the most important message of the present study is that sleep difficulties and NSSI may be cyclically related, with depressive symptoms playing an important role in the escalation of NSSI. The bidirectionality between symptoms of insomnia and NSSI may suggest that these problems are either present at the same time (comorbidity) or there is an underlying condition that connects them. Because comorbidity is consistently associated with a greater demand for professional help as well as with greater interference with everyday life (e.g. Albert, Rosso, Maina, & Bogetto, 2008) future studies should use a more person‐oriented approach to assess these possibilities.
Our present findings also suggest that practitioners designing intervention efforts should target insomnia and the negative feelings it may generate for adolescents. Also, these findings have important implications for clinicians working with adolescents for at least three reasons. First, monitoring and assessing the adolescents’ sleep quality might allow the identification of a vulnerable group of adolescents, namely those who engage in NSSI. This early screening might prevent the engagement in more maladaptive behaviours, such as suicidal thoughts and conducts. Second, because better sleep might act as a protective factor against NSSI, treatments and interventions specifically designed to increase sleep quality, such as cognitive behavioural therapy for insomnia (de Zambotti et al., 2018), might also be able to indirectly target NSSI. Last, given the private nature of NSSI, as well as the stigma around it, adolescents might be more prone to seek/receive treatment for sleep difficulties than for NSSI. Therefore, knowledge of the association between sleep and NSSI is very important for practitioners working with adolescents.
AUTHOR CONTRIBUTIONS
DL and SB conceived the idea behind the study. All authors developed the theoretical framework. DL analysed the data. All authors contributed to the interpretation of the results. DL and SB wrote the manuscript with the input from LTW. All authors reviewed the final manuscript.
Supporting information
Table S1
ACKNOWLEDGEMENTS
This study was made possible by access to data from the Three Cities Study, a longitudinal research programme at the Department of Law, Psychology and Social work at Örebro University, Sweden and financed by the Swedish research agencies FORMAS, FORTE, VINNOVA, and Vetenskapsrådet [grant number 2012‐65]. We would like to thank Prof. Katja Boersma for the valuable feedback.
Latina D, Bauducco S, Tilton‐Weaver L. Insomnia symptoms and non‐suicidal self‐injury in adolescence: understanding temporal relations and mechanisms. J Sleep Res.2021;30:e13190 10.1111/jsr.13190
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Albert, U. , Rosso, G. , Maina, G. , & Bogetto, F. (2008). Impact of anxiety disorder comorbidity on quality of life in euthymic bipolar disorder patients: Differences between bipolar I and II subtypes. Journal of Affective Disorders, 105, 297–303. 10.1016/j.jad.2007.05.020 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (DSM‐5). American Psychiatric Association. [Google Scholar]
- Andover, M. S. , Morris, B. W. , Wren, A. , & Bruzzese, M. E. (2012). The co‐occurrence of non‐suicidal self‐injury and attempted suicide among adolescents: Distinguishing risk factors and psychosocial correlates. Child and Adolescent Psychiatry and Mental Health, 6, 11–17. 10.1186/1753-2000-6-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandel, S. L. , & Brausch, A. M. (2018). Poor sleep associates with recent nonsuicidal self‐injury engagement in adolescents. Behavioral Sleep Medicine, 18(1), 81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauducco, S. V. , Salihovic, S. , & Boersma, K. (2019). Bidirectional associations between adolescents’ sleep problems and impulsive behavior over time. Sleep Medicine: X, 1, 100009 10.1016/j.sleepx.2019.100009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker, S. P. , Langberg, J. M. , & Byars, K. C. (2015). Advancing a biopsychosocial and contextual model of sleep in adolescence: A review and introduction to the special issue. Journal of Youth and Adolescence, 44, 239–270. 10.1007/s10964-014-0248-y [DOI] [PubMed] [Google Scholar]
- Chapman, A. L. , Gratz, K. L. , & Brown, M. Z. (2006). Solving the puzzle of deliberate self‐harm: The experiential avoidance model. Behaviour Research and Therapy, 44, 371–394. 10.1016/j.brat.2005.03.005 [DOI] [PubMed] [Google Scholar]
- Chorpita, B. F. , Tracey, S. A. , Brown, T. A. , Collica, T. J. , & Barlow, D. H. (1997). Assessment of worry in children and adolescents: An adaptation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 35, 569–581. 10.1016/S0005-7967(96)00116-7 [DOI] [PubMed] [Google Scholar]
- Crowley, S. J. , Wolfson, A. R. , Tarokh, L. , & Carskadon, M. A. (2018). An update on adolescent sleep: New evidence informing the perfect storm model. Journal of Adolescence, 67, 55–65. 10.1016/j.adolescence.2018.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Zambotti, M. , Goldstone, A. , Colrain, I. M. , & Baker, F. C. (2018). Insomnia disorder in adolescence: Diagnosis, impact, and treatment. Sleep Medicine Reviews, 39, 12–24. 10.1016/j.smrv.2017.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ennis, C. R. , Short, N. A. , Moltisanti, A. J. , Smith, C. E. , Joiner, T. E. , & Taylor, J. (2017). Nightmares and nonsuicidal self‐injury: The mediating role of emotional dysregulation. Comprehensive Psychiatry, 76, 104–112. 10.1016/j.comppsych.2017.04.003 [DOI] [PubMed] [Google Scholar]
- Ghekiere, A. , Van Cauwenberg, J. , Vandendriessche, A. , Inchley, J. , Gaspar de Matos, M. , Borraccino, A. , … De Clercq, B. (2019). Trends in sleeping difficulties among European adolescents: Are these associated with physical inactivity and excessive screen time? International Journal of Public Health, 64, 487–498. 10.1007/s00038-018-1188-1 [DOI] [PubMed] [Google Scholar]
- Harvey, A. G. , Murray, G. , Chandler, R. A. , & Soehner, A. (2011). Sleep disturbance as transdiagnostic: Consideration of neurobiological mechanisms. Clinical Psychology Review, 31, 225–235. 10.1016/j.cpr.2010.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu, L. T. , & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hysing, M. , Pallesen, S. , Stormark, K. M. , Lundervold, A. J. , & Sivertsen, B. (2013). Sleep patterns and insomnia among adolescents: A population‐based study. Journal of Sleep Research, 22, 549–556. 10.1111/jsr.12055 [DOI] [PubMed] [Google Scholar]
- Hysing, M. , Sivertsen, B. , Stormark, K. M. , & O'Connor, Rory C. (2015). Sleep problems and self‐harm in adolescence. British Journal of Psychiatry, 207, 306–312. 10.1192/bjp.bp.114.146514 [DOI] [PubMed] [Google Scholar]
- Jenkins, A. L. , & Schmitz, M. F. (2012). The roles of affect dysregulation and positive affect in non‐suicidal self‐injury. Archives of Suicide Research, 16, 212–225. 10.1080/13811118.2012.695270 [DOI] [PubMed] [Google Scholar]
- Jose, P.E. , & Brown, I. (2008). When does the gender difference in rumination begin? Gender and age differences in the use of rumination by adolescents. Journal of Youth and Adolescence, 37, 180–192. https://doi.org/10.1007/s10964‐006‐9166‐y [Google Scholar]
- Junker, A. , Bjørngaard, J. H. , Gunnell, D. , & Bjerkeset, O. (2014). Sleep problems and hospitalization for self‐harm: A 15‐year follow‐up of 9,000 Norwegian adolescents. The Young‐HUNT Study. Sleep, 37, 579–585. 10.5665/sleep.3502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky, E. D. (2007). The functions of deliberate self‐injury: A review of the evidence. Clinical Psychology Review, 27, 226–239. 10.1016/j.cpr.2006.08.002 [DOI] [PubMed] [Google Scholar]
- Klonsky, E. D. (2009). The functions of self‐injury in young adults who cut themselves: Clarifying the evidence for affect‐regulation. Psychiatry Research, 166, 260–268. 10.1016/j.psychres.2008.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn, P. M. , Gotlib, I. H. , Lewinsohn, M. , Seeley, J. R. , & Allen, N. B. (1998). Gender differences in anxiety disorders and anxiety symptoms in adolescents. Journal of Abnormal Psychology, 107, 109–117. 10.1037/0021-843X.107.1.109 [DOI] [PubMed] [Google Scholar]
- Liu, X. , Chen, H. , Bo, Q. G. , Fan, F. , & Jia, C. X. (2017). Poor sleep quality and nightmares are associated with non‐suicidal self‐injury in adolescents. European Child & Adolescent Psychiatry, 26, 271–279. 10.1007/s00787-016-0885-7 [DOI] [PubMed] [Google Scholar]
- Lockwood, J. , Daley, D. , Townsend, E. , & Sayal, K. (2017). Impulsivity and self‐harm in adolescence: A systematic review. European Child and Adolescent Psychiatry, 26, 1–16. 10.1007/s00787-016-0915-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovato, N. , & Gradisar, M. (2014). A meta‐analysis and model of the relationship between sleep and depression in adolescents: Recommendations for future research and clinical practice. Sleep Medicine Reviews, 18, 521–529. 10.1016/j.smrv.2014.03.006 [DOI] [PubMed] [Google Scholar]
- Lundh, L. G. , Bjärehed, J. , & Wångby‐Lundh, M. (2013). Poor sleep as a risk factor for nonsuicidal self‐injury in adolescent girls. Journal of Psychopathology and Behavioral Assessment, 35, 85–92. 10.1007/s10862-012-9307-4 [DOI] [Google Scholar]
- Lundh, L. G. , Karim, J. , & Quilisch, E. V. A. (2007). Deliberate self‐harm in 15‐year‐old adolescents: A pilot study with a modified version of the Deliberate Self‐Harm Inventory. Scandinavian Journal of Psychology, 48, 33–41. 10.1111/j.1467-9450.2007.00567.x [DOI] [PubMed] [Google Scholar]
- MacCallum, R. C. , Zhang, S. , Preacher, K. J. , & Rucker, D. D. (2002). On the practice of dichotomization of quantitative variables. Psychological Methods, 7, 19 10.1037/1082-989X.7.1.19 [DOI] [PubMed] [Google Scholar]
- Marshall, S. K. , Tilton‐Weaver, L. C. , & Stattin, H. (2013). Non‐suicidal self‐injury and depressive symptoms during middle adolescence: A longitudinal analysis. Journal of Youth and Adolescence, 42, 1234–1242. 10.1007/s10964-013-9919-3 [DOI] [PubMed] [Google Scholar]
- Maxfield, B. L. , & Pepper, C. M. (2018). Impulsivity and response latency in non‐suicidal self‐injury: The role of negative urgency in emotion regulation. Psychiatric Quarterly, 89, 417–426. 10.1007/s11126-017-9544-5 [DOI] [PubMed] [Google Scholar]
- McCall, W. V. , & Black, C. G. (2013). The link between suicide and insomnia: Theoretical mechanisms. Current Psychiatry Reports, 15, 389–397. 10.1007/s11920-013-0389-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlinchey, E. L. , Courtney‐Seidler, E. A. , German, M. , & Miller, A. L. (2017). The role of sleep disturbance in suicidal and nonsuicidal self‐injurious behavior among adolescents. Suicide and Life‐Threatening Behavior, 47, 103–111. 10.1111/sltb.12268 [DOI] [PubMed] [Google Scholar]
- Morin, C. M. (1993). Insomnia: Psychological assessment and management. New York, NY, USA: Guilford Press. [Google Scholar]
- Muehlenkamp, J. J. , Claes, L. , Havertape, L. , & Plener, P. L. (2012). International prevalence of adolescent non‐suicidal self‐injury and deliberate self‐harm. Child and Adolescent Psychiatry and Mental Health, 6, 1–9. 10.1186/1753-2000-6-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L. K. , & Muthén, B. O. (1998–2019). Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nixon, M. K. , Cloutier, P. , & Jansson, S. M. (2008). Nonsuicidal self‐harm in youth: A population‐based survey. Canadian Medical Association Journal, 178, 306–312. 10.1503/cmaj.061693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olsson, G. , & von Knotting, A. L. (1997). Depression among Swedish adolescents measured by the self‐rating scale Center for Epidemiology Studies‐Depression Child (CES‐DC). European Child & Adolescent Psychiatry, 6, 81–87. [DOI] [PubMed] [Google Scholar]
- Orth, U. , Berking, M. , & Burkhardt, S. (2006). Self‐conscious emotions and depression: Rumination explains why shame but not guilt is maladaptive. Personality and Social Psychology Bulletin, 32, 1608–1619. 10.1177/0146167206292958 [DOI] [PubMed] [Google Scholar]
- Palmer, C. A. , & Alfano, C. A. (2017). Sleep and emotion regulation: An organizing, integrative review. Sleep Medicine Reviews, 31, 6–16. 10.1016/j.smrv.2015.12.006 [DOI] [PubMed] [Google Scholar]
- Plener, P. L. , Schumacher, T. S. , Munz, L. M. , & Groschwitz, R. C. (2015). The longitudinal course of non‐suicidal self‐injury and deliberate self‐harm: A systematic review of the literature. Borderline Personality Disorder and Emotion Dysregulation, 2, 1–11. 10.1186/s40479-014-0024-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokorny, S. B. , Jason, L. A. , Schoeny, M. E. , Townsend, S. M. , & Curie, C. J. (2001). Do participation rates change when active consent procedures replace passive consent. Evaluation Review, 25, 567–580. 10.1177/0193841X0102500504 [DOI] [PubMed] [Google Scholar]
- Richmond, S. , Hasking, P. , & Meaney, R. (2017). Psychological distress and non‐suicidal self‐injury: The mediating roles of rumination, cognitive reappraisal, and expressive suppression. Archives of Suicide Research, 21, 62–72. 10.1080/13811118.2015.1008160 [DOI] [PubMed] [Google Scholar]
- Riemann, D. , Spiegelhalder, K. , Feige, B. , Voderholzer, U. , Berger, M. , Perlis, M. , & Nissen, C. (2010). The hyperarousal model of insomnia: A review of the concept and its evidence. Sleep Medicine Reviews, 14, 19–31. 10.1016/j.smrv.2009.04.002 [DOI] [PubMed] [Google Scholar]
- Tilton‐Weaver, L. C. , Marshall, S. K. , & Svensson, Y. (2019). Depressive symptoms and non‐suicidal self‐injury during adolescence: Latent patterns of short‐term stability and change. Journal of Adolescence, 75, 163–174. 10.1016/j.adolescence.2019.07.013 [DOI] [PubMed] [Google Scholar]
- Whiteside, S. P. , & Lynam, D. R. (2001). The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30, 669–689. 10.1016/S0191-8869(00)00064-7 [DOI] [Google Scholar]
- Wong, M. M. , Brower, K. J. , & Zucker, R. A. (2011). Sleep problems, suicidal ideation, and self‐harm behaviors in adolescence. Journal of Psychiatric Research, 45, 505–511. 10.1016/j.jpsychires.2010.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegert, D. I. , & Kistner, J. A. (2002). Response styles theory: Downward extension to children. Journal of Clinical Child and Adolescent Psychology, 31, 325–334. 10.1207/S15374424JCCP3103_04 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


