Abstract
Introduction
Quality in medical care must be measured in order to be improved. Trauma management is part of health care, and by definition, it must be checked constantly. The only way to measure quality and outcomes is to systematically accrue data and analyze them.
Material and methods
A systematic revision of the literature about quality indicators in trauma associated to an international consensus conference
Results
An internationally approved base core set of 82 trauma quality indicators was obtained: Indicators were divided into 6 fields: prevention, structure, process, outcome, post-traumatic management, and society integrational effects.
Conclusion
Present trauma quality indicator core set represents the result of an international effort aiming to provide a useful tool in quality evaluation and improvement. Further improvement may only be possible through international trauma registry development. This will allow for huge international data accrual permitting to evaluate results and compare outcomes.
Keywords: Performance, Product, Morbidity, Mortality, System, Analysis, Outcome, Data, Planning, World
Background
Quality in medical care must be measured in order to be improved. Trauma management is part of health care, and by definition, it must be checked constantly. The only way to measure quality and outcomes is to systematically accrue data and analyze them. However, one of the main issues encountered in this activity is the difficulty to obtain complete and affordable dataset. Health care systems as well as trauma systems are different. They are differently organized around the world; discrepancies exist between them. The profound differences in organizational models may reflect even in outcomes. The necessity to evaluate the quality of care in a local, national, and even international scale has been progressively considered more necessary in the last decades. Quality of care is characterized as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with the current professional knowledge” [1]. Measurement and feedback of performance are integral to the concept of a system of care [2, 3]. Since the early 1970s, the evidence of several deaths due to suboptimal trauma care in the USA has led to the development of structured trauma systems [4]. With the development of organizational models, the number of preventable deaths has progressively decreased [2]. Quality improvement evaluates the performance of both individual providers and the systems in which they work [1].
Evaluation of quality of the service offered by health systems may be measured with quality indicators (QI).
QI are performance measures designed to compare actual care against ideal criteria for the purposes of quality measurement, benchmarking, and identifying potential opportunities for improvement [5].
The US national system was the first in developing a structured trauma quality indicators (TQI) list and in providing several tools in order to continuously check and improve results. At present, many different TQI sets exist. However, concomitant existing significant variations in the utilization of indicators and limited evidence to support the use of specific indicators over others do not allow for an exchange in TQI within the different systems [5]. In fact, around the world, trauma systems are at different points in the organizational progression. TQI list generally adopted in a system cannot be entirely applied in a different one. Actually, no clearly defined and internationally approved TQI sets exist. However, a core set of universally applicable TQI that may be transversally adopted by all trauma systems is needed. Subcategories of indicators may then be elaborated and tailored according to dedicated system analysis.
The aim of this paper is to present a list of internationally approved core items for trauma management quality evaluation.
Material and methods
A systematic revision of the literature about QI for evaluating trauma care was conducted. Researches were done on MEDLINE, Embase, CINAHL, Cochrane Database of Systematic Reviews, Cochrane Database of Abstracts of Reviews of Effects, and Cochrane Central Register of Controlled Trials from the earliest available date through May 31, 2019. To increase the sensitivity of the search, the grey literature and select journals by hand were investigated, reference lists to identify additional studies were reviewed, and experts in the field were contacted. Moreover, websites of the major surgical and critical care societies worldwide were investigated for obtaining QI (American College of Surgeons, American Association for the Surgery of Trauma, Eastern Association for the Surgery of Trauma, Western Trauma Association, American Trauma Society, International Trauma Anesthesia, and Critical Care Society, British Trauma Society, Panamerican Trauma Society, Trauma Association of Canada, European Society for Trauma and Emergency Surgery, Australasian Trauma Society, Orthopedic Trauma Association, Trauma.org, the Society of Trauma Nurses). To further enlarge the research, also the main web search engines were utilized (i.e., Google, Yahoo, Bing, and Baidu) using the following search terms: trauma, quality, indicator, and injury.
All articles identifying and/or proposing 1 or more QI focusing on prehospital care, hospital care, posthospital care, or secondary injury prevention were considered.
Moreover, main world trauma centers’ TQI lists were analyzed. All the identified QI lists were then analyzed in order to summarize all retrieved indicators.
Once all the QI were summarized, an international expert panel web-based consensus survey was done to obtain a balanced QI list. Two hundred experts from all the 5 continents and from all the 6 WHO regions were asked to express their evaluation of importance (0–10 marks, where 0 was not relevant and 10 was very important) about all the proposed QI. Items with ≥ 70% of preferences to values 8 to 10 have been accepted as important and passed through the next steps. During the survey, expert panel components had the opportunity to suggest further quality indicators they consider important and not present in the proposed list.
Results of the survey were analyzed and discussed during an international event in Pisa, Italy, on September 27, 2019. Then, results of discussion were diffused for a further international round of evaluation and discussion between international panels of recognized experts in the field. Through subsequent rounds of evaluation, in a modified Delphi process, the manuscript reached the definitive version together with the definitive TQI core list.
Results
After systematic reviews of the existing literature about TQI and the trauma center/society protocol and TQI lists, a total of 1288 indicators were obtained. After analysis and elimination of duplicate QI or integration of the similar ones into a single comprehensive indicator, 89 were proposed for international evaluation. After international round, 82 were considered to be included into the definitive list (Tables 1, 2, 3, and 4).
Table 1.
Prevention and structure indicators
| Category | Subcategory | Indicators | Patients |
|---|---|---|---|
| Prevention | Activity to prevent and diffuse trauma risks and effect perception | All patients | |
| Measurement of injury risk perception and behavioral changes following sensibilization programs | All patients | ||
| Psychological consequences in observers | All patients | ||
| Copycat event prevention | All patients | ||
| Direct medical cost quantification | All patients | ||
| Indirect cost quantification | All patients | ||
| Structure | Center preparedness | Presence of data registry | All patients |
| Staff training requirements | All patients |
Table 2.
Process indicators (TTA Trauma Team Activation, GCS Glasgow Coma Scale, TBI traumatic brain injury, ED emergency department, AIS Abbreviated Injury Scale, ISS Injury Severity Score, CT computed tomography, TEG tromboelastography, ROTEM rotational thromboelastometry, ICU intensive care unit, EX-LAP explorative laparotomy, SBP systolic blood pressure, OR operating room, E-FAST extended focused assessment with sonography in trauma, REBOA resuscitative endovascular balloon occlusion of the aorta, CNS central nervous system)
| Category | Subcategory | Indicator | Patients |
|---|---|---|---|
| Process | Triage/prehospital | Time to first medical contact (on scene) | All patients |
| Prehospital time | ISS > 16 | ||
| Time to definitive trauma center | All patients | ||
| Acute pain management | Patients with documented pain assessment | ||
| Intubation of unconscious patients | Prehospital GCS < 9 | ||
| Pelvic binder in pelvic fracture | Mechanically and/or hemodynamically unstable pelvic fractures (AIS 3-5) | ||
| Field triage rate (undertriage) | All patients | ||
| Patient in shock with documented blood pressure who dies with no Emerg. Dept. thoracotomy or REBOA placement | Patients died in ER arrived with a documented blood pressure | ||
| Emergency dept. management | Trauma Team Activation (TTA) | Patients requiring TTA for whom TTA was activated | |
| Airway secured in ED for patients with GCS <9 | Patients with GCS < 9 | ||
| Tracheal intubation (GCS<9) | Patients with GCS < 9 | ||
| Adequate rewarming measures for hypothermia (temperature ≤ 35 °C) | Patients admitted to a trauma center | ||
| Operative management of patients with an abdominal gunshot wound | Patients with a penetrating abdominal injury by firearm | ||
| Tetanus prophylaxis | All patients with exposed soft tissues | ||
| Antibiotics for open fractures | Number of patients with an open fracture receiving an antimicrobial agent within 1 h of hospital arrival | ||
| Time to cranial CT for patients with GCS < 14 | GCS < 14 | ||
| Patient with GCS < 13 has a head CT within 4 h of arrival in ED | Adult TBI: GCS < 13; pediatric TBI: GCS < 12 | ||
| Time to CT scan from ED admission | ED patients with blunt force injuries AND trauma team activation (TTA) OR ED documented GCS < 9, receiving CT scan within 1 h of ED arrival | ||
| E-FAST in patient without CT | Patients without CT | ||
| Blood analysis performed/BE documented | All patients | ||
| Coagulation test (TEG/ROTEM) | All patients with active bleeding | ||
| ED stay > 1 h for patients with GCS < 9 or intubated (level I/II) | TBI patients with GCS ≥ 4 or ≤ 10 in a level I/II trauma center | ||
| ED stay > 1 h for patients admitted to ICU or OR | TBI patients with GCS ≥ 4 or ≤ 8 or intubated in a level I/II trauma center | ||
| Massive trasfusion protocol activation | Patients with active bleeding and signs of shock | ||
| Time to start of blood transfusion | Patients with at least one unit transfused | ||
| Orthopedic response time > 30 min in emergent case | Patients with orthopedic trauma | ||
| Unplanned ICU admission | Patients primarily admitted to ward then moved to ICU | ||
| Surgical management | Definitive bleeding control (in patients with PTM) | All patients age 18 years and older with an injury diagnosis AND prescribed a massive transfusion who receive attempted definitive bleeding control (laparotomy, thoracotomy, percutaneous therapy) within 30 min of the massive transfusion prescription | |
| Trauma | Time to first emergency surgery | Operated patients | |
| Delay to OR-EX-LAP (> 2 h): trauma | Operated patients | ||
| Time to laparotomy < 1 h for patients with a proven intra-abdominal bleeding causing hypotension | SBP < 90 or requires > 4 units of packed red blood cells in the first hour for hemorrhage due to injury | ||
| Time to surgery in patients with shock | SBP < 90 | ||
| Patients with bleeding pelvic fracture who die within 60 min from ED arrival without preperitoneal pelvic packing or REBOA placement | Patients with bleeding pelvic fracture | ||
| Neurosurgical | Time to surgical brain decompression | TBI with indication for decompression | |
| Patients with epidural or subdural hematoma receiving craniotomy > 4 h after arrival | Patients with epidural or subdural hematoma | ||
| Enteral or parenteral feeding for severe head injury patients < 7 days post-injury | TBI patients with GCS ≤ 10 | ||
| Failure monitoring of intracranial pressure in severe TBI with pathological CT finding | Severe TBI | ||
| Orthopedic | Open fracture grade 3 to OR > 8 h | Open fracture grade 3 | |
| Open long bone fracture surgery < 6 h | Open fracture of the tibia, fibula, humerus, radius, or ulna | ||
| Patient with pelvic fracture and hemodynamic instability on ED arrival with provisional stabilization of pelvic ring fracture within 12 h from arrival at the trauma center | Patients with SBP < 90 or requiring > 4 units of packed red blood cells in the first hour | ||
| Open fracture grade 1 or 2 to OR >16 h | Open fracture grade 1 or 2 | ||
| Open fractures—stabilized > 24 h | Long bones open fractures | ||
| Vascular | Ischemic limb revascularized < 6 h | Ischemic limb following vascular trauma | |
| Time to restore perfusion | Ischemic limb following vascular trauma | ||
| Deep vein thrombosis prophylaxis (within 24 h) in immobile patients | Patients immobilized ≥ 24 h (without CNS bleeds or spine/CNS surgery within 24 h) | ||
| Patients who experienced limb amputation without previous vascular shunt placement | Patients with limb amputation |
Table 3.
Outcome, post-traumatic management, and society integrational effect indicators (VAE ventilator-associated events, TBI traumatic brain injury, ED emergency department, ICU intensive care unit, OR operating room)
| Category | Subcategory | Indicator | Patients |
|---|---|---|---|
| Outcome | Admission data | ICU lenght of stay | Patients admitted to ICU |
| Lenght of stay | All patients | ||
| Ventilator-associated events (VAE) | All patients | ||
| Adverse events (according to Clavien-Dindo classification) | Complications during hospital stay | All patients | |
| Pulmonary embolus | All patients | ||
| Mortality | Mortality rate | Admitted patients | |
| Death < 48 h after arrival | All patients | ||
| Deaths >1 h after arrival occur on ward (not in ED) | Vital signs on arrival | ||
| Death > 48 h after arrival | All patients | ||
| Mortality in severe TBI | Severe TBI | ||
| Penetrating injury mortality | Patients with penetrating injury | ||
| Blunt multisystem injury mortality | Patients with multisystem injury | ||
| Blunt single-system mortality | Patients with single-system injury | ||
| TBI deaths > 3 h following arrival in level III/IV center | TBI with GCS >12 and max head AIS > max AIS in other anatomic regions | ||
| Failure to rescue (severe) | Patients died with unsolved severe complication | Patients who died among those with Clavien-Dindo grades 3–5 complications | |
| Functional outcome | Evaluation of patient functional status (at hospital) | All patients | |
| Outcomes review | Peer review of trauma deaths to evaluate quality of care and determine whether the death was potentially preventable | Dead patients | |
| Early post-op events | Tertiary survey | All patients | |
| Unexpected return to OR | All operated patients with no ongoing damage control surgery | ||
| Post-traumatic management | Long-term physical disability facilities/support | All patients | |
| Psychological disability facilities/support | All patients | ||
| Behavioral change and secondary health loss quantification | All patients | ||
| Tangible costs quantification | All patients | ||
| Intangible costs quantification | All patients | ||
| Society integrational effects | Observer consequences evaluation/support | All patients | |
| Carer consequences evaluation/support | All patients | ||
| Dependent consequence evaluation/support | All patients |
Table 4.
Secondary analysis of primary indicators
| 1. Error in management | |
| 2. Error in judgment, deviation for internal protocols | |
| 3. Error in diagnosis | |
| 4. Error in technique | |
| 5. Provider errors: | |
| • Treatment below the standard of care | |
| • Missed injuries | |
| • Error in prioritizing order of work up | |
| • Missing trauma scores: RTS, ISS, NISS, TRISS, etc. | |
| 6. Morbidity and mortality rates in frail patients (i.e., elderly or transplanted) |
Average agreement was of 97% within the different experts about the different QI.
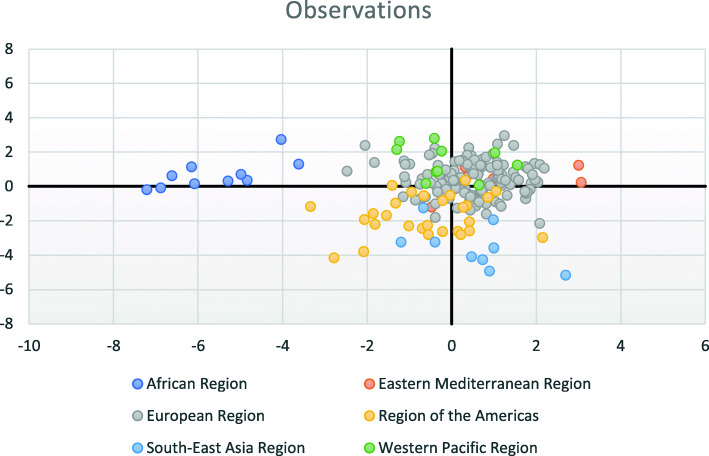
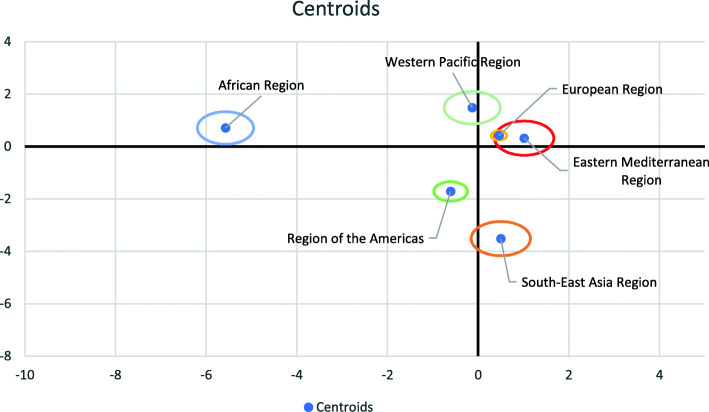
Participating centers and surgeon distribution across the different hospitals in the World Health Organization (WHO) regions are presented in Figs. 1 and 2. Answers were analyzed, and the distributions of the importance given to the different indicators have been reported in Figs. 3 and 4 showing some variation within the different the WHO regions.
Fig. 1.
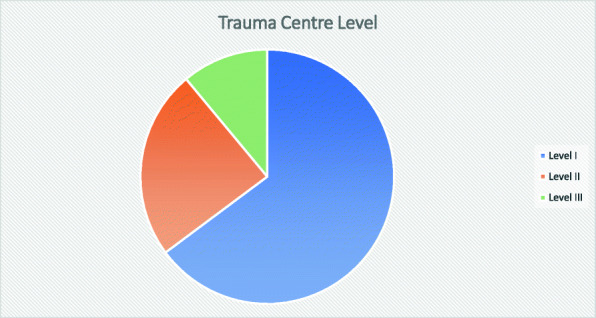
Trauma center level distribution of international experts
Fig. 2.
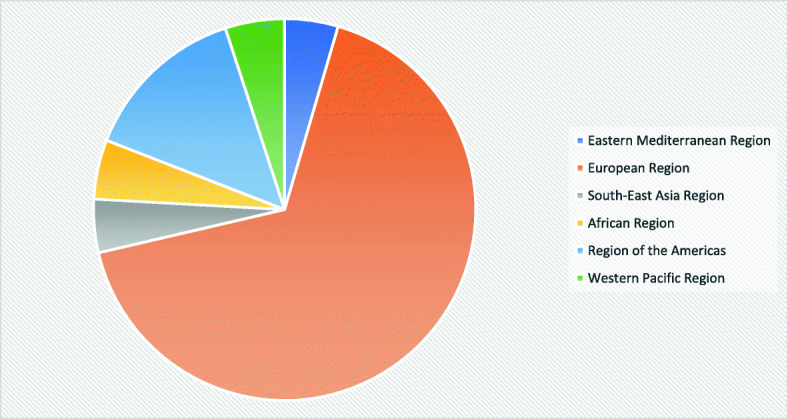
Expert distribution according to the World Health Organization (WHO) regions
Fig. 3.
Differences in perceiving the importance of the different items for the different answers according to the WHO region
Fig. 4.
Centroid distribution of the differences in perceiving the importance of the different items for the different answers according to the WHO region
The different regions showed homogeneous differences in perceiving the importance of the different items for the different answers (Fig. 3) and for the centroid of the average of the various answers (Fig. 4).
Categories into which TQI have been divided are as follows:
Prevention
Structure
Process
Outcome
Post-traumatic management
Society integrational effects
Discussion
According to the WHO definitions, quality comprises three elements: structure, process, and outcome [1].
Structure refers to stable, material characteristics (infrastructure, tools, technology) and the resources of the organizations that provide care and the financing of care (levels of funding, staffing, training, skills, payment schemes, incentives) [1].
Process is the interaction between caregivers and patients during which structural inputs from the health care system are transformed into health outcomes. The process is the actual provision of medical care to the patient [1].
Outcomes can be measured in terms of health status, deaths, or disability-adjusted life years—a measure that encompasses the morbidity and mortality of patients or groups of patients. Outcomes also include patient satisfaction or patient response to the health care system [1].
At present, however, trauma system evolution must take into consideration the necessity to relate the system to the context into which it operates. For this reason, quality evaluation must comprise some more aspects influenced by and influencing the trauma patient’s management.
Present manuscript aims to answer to the recognized necessity of an international agreement about a QI core set. Quality improvement is mainly a behavioral change, and it is impossible to change if no shared and agreed points exist. Shared and largely approved and agreed-on QI are needed to improve quality not in a competitive view but in a reciprocal improvement behavior. It is not possible to proceed with a transparent, explicit, systematic, data-driven performance measurement if there is no agreement upon indicators and measures. A very high number of existing proposed TQI have been searched, reported, and resumed. For sure, search may not have been exhaustive, despite the evaluation of multiple databases using comprehensive research strategies and imposing no language restrictions. As a counterpart, the very high number of redundant indicators clearly shows how it approximated the completeness. We can assume that very few eventual other QI may have been not considered.
Present paper demonstrated that a common set of clearly defined, evidence-based, broadly accepted trauma QIs does not exist. A large group of heterogeneous indicators are diffusely and non-homogeneously utilized. Moreover, the vision and perception of TQI across the world is widely different as clearly shown in Figs. 3 and 4. This different perception is the reflection of different cultural and organizational models, and at the same time, it results in slightly different priorities. However, present international effort aims also to balance the differences in a shared TQI in order to promote intersystem comparison and improvement.
One of the main factors emerging from the analysis is the imbalance existing between QIs evaluating prehospital, in-hospital, and posthospital management. In fact, current literature universally focused on in-hospital phase of trauma care. Very few QIs are dedicated to the analysis of the pre- and posthospital phases. This reflects the lack in organizational systems, indifferently from the WHO region and from the resources of the system. This may be due to a disconnect between the professional figures reflecting on the three phases of trauma management. The in-hospital phase is diffusely considered the most important. For this reason, organizational efforts are maximized in this part with very few resources dedicated to the others. However, it should be stressed as the pre- and posthospital phases may strongly impair the effectiveness of the in-hospital trauma management. Lastly, prevention phase is not considered nor evaluated at all.
Donabedian stratification of healthcare QIs into structure, process, and outcome evaluation is valid and diffusely accepted [6–8]. However, as trauma involves more than the hospital and may impact on multiple different levels of the sanitary and economical systems, its quality management evaluation should encompass more than the already defined three key-points. It must consider the system in which the “structure” is included in, and international trauma registries must consider obtaining data even regarding socio-economical setting together with the performance of the specific hospital/system.
This paper proposes a six level stratification of TQI: prevention, structure, process, outcome, post-traumatic management, and society integrational effects.
Quality measures other than mere hospital morbidity and mortality and management process are strongly needed to evaluate the real outcome dimensions referring to trauma prevention, health-related quality-of-life, psychosocial impact of the injury, etc. with the aim of providing a more refined specificity for all the different components of patient care.
All these phases reflect even direct and indirect costs that may be even very important in a national and international view. For these reasons, they should also be included into trauma system quality evaluation. Cost evaluation however should be done at a local or national level. International cost comparison may be impossible or at least useless due to vastly different organizational/legal/economical models.
Lastly, a need to improve the science behind the development, validation, and use of indicators is urgent.
Conclusion
Present trauma quality indicator core set represents the result of an international effort aiming to provide a useful tool in quality evaluation and improvement. Further improvement may only be possible through international trauma registry development. This will allow for huge international data accrual permitting to evaluate results and compare outcomes.
Acknowledgements
None
WSES Trauma Quality Indicators Expert Panel
Zygimantas Kuliesius1, Luigi Conti2, Agron Dogjani3, Jae Gil Lee4, Heitor Consani5, Domenico Russello6, Marina Bortul7, Teresa Gimenez Maurel8, Hossein Samadi Kafil9, Harissou Adamou10, Vasilescu Alin11, Umberto Robustelli12, Norio Sato13, Charalampos Seretis14, Martha Quiodettis15, Carlos Augusto Gomes16, Victor Kong17, Andee Dzulkarnaen Zakaria18, Ali Guner19, Mahir Gachabayov20, Sharfuddin Chowdhury21, Francesco Pata22, Alberto Garcia23, Miran Rems24, Koray Das25, J.G. Riedel26, Konstantinos Lasithiotakis27, Ruslan Sydorchuk28, Larysa Sydorchuk29, Eftychios Lostoridis30, Alexander Buia31, Michael McFarlane32, Renzo Ciani33, Virginia María Durán Muñoz-Cruzado34, Dario Tartaglia35, Orestis Ioannidis36, Måns Muhrbeck37, Martin Reicher26, Francesco Roscio38, Marco Ceresoli39, Dimitrios Tsiftsis40, Alfie Kavalakat41, Tadeja Pintar42, George Georgiou43, Gabriele Ricci44, Rajashekar Mohan45, Sten Saar46, Isidoro Di Carlo6, Arda Isik47, Ali Yasen Yasen Mohamed Ahmed48, Ricardo Alessandro Teixeira Gonsaga49, Fabrizio Sammartano50, Luis Tallon-Aguilar34, Tomohisa Shoko51, Jeremy Hsu52, Yoshiro Kobe53, Christian Galatioto35 Luigi Romeo54, Mauro Podda55, Andrea Mingoli56, Rafael Castro Delgado57, Gerald Ekwen58, Vanlander Aude59, Carles Olona60, Paolo Boati61, Stefano Magnone62, Massimo Capaldi44, Miklosh Bala63, Edoardo Picetti64, Ionut Negoi65, Kenneth Y. Y. Kok66, Asri Che Jusoh67, Bruno Amato68, Gabriela Elisa Nita69, Andrew de Beaux70, Zaza Demetrashvili71, R. Justin Davies72, Jae Il Kim73, André Pereira74, Luca Fattori39, Ciro Paolillo75, Wagih Ghannam76, Fernando Machado Rodriguez77, Luca Berardi78, Maria Gioffrè Florio79, Matthias Hecker80, Vincent Dubuisson81, Donal B. O’Connor82, Nicola De'Angelis83, Ivan Dobrić84, Damien Massalou85, Per Örtenwall86, Emmanouil Pikoulis87, Bakarne Ugarte-Sierra88, W.P. Zuidema89, Aristotelis Kechagias90, Sanjay Marwah91, Andrey Litvin92, Ioannis Nikolopoulos93, Antonio Pesce94, Selman Uranues95, Davide Luppi96, Sascha Flohe97, Aleix Martínez-Pérez98, Manuel Lorenzo99, Luigi Branca Vergano100, Mario Manca101, Paolo Malacarne102, Hayato Kurihara103, Sandy Widder104, Marsia Pucciarelli35, Fabio Monzani105, Pietro Brambillasca106, Davide Corbella106, Ferdinando Agresta107, Lynne Moore108, Luis Antonio Buonomo109, Amos O. Adeleye110, Dennis Kim111, Massimiliano Veroux94, Timothy Craig Hardcastle112, Salomone Di Saverio72, Alfonso Recordare113, Ines Rubio-Perez114, Sergey Shlyapnikov115, Razrim Rahim116, Gustavo Miguel Machain Vega117, Kessel Boris118, Robert Sawyer119, Oussama Baraket120, Kjetil Soreide121, Clemens Weber122, Chen-June Seak123, Simon Herman124, Emiliano Gamberini125, Silvia Costa126, Gualtiero Mazzocconi127, Edgard Lozada128, Dimitrios Manatakis129, Varut Lohsiriwat130, Adamu Ahmed131, Bahaa Elbery132, Guido Alberto Massimo Tiberio133, Massimo Santini134, Luca Mellace135, Cathrine Harstad Enoksen136, Piotr Major137, Dario Parini138, Mario Improta139, Paola Fugazzola139, Silvia Pini102, Gaetano Liberti140, Costanza Martino125, Lorenzo Cobianchi141, Gabriele Canzi142, Enrico Cicuttin141, Jakub Kenig143, Mauro Zago144, Sandro Giannessi145, Michelangelo Scaglione146, Eugenio Orsitto147, Roberto Cioni148, Lorenzo Ghiadoni105, Francesco Menichetti149, Vanni Agnoletti125, Gabriele Sganga150, Paolo Prosperi151, Franco Roviello152, Paolo De Paolis153, Giovanni Gordini154, Francesco Forfori155, Paolo Ruscelli156, Francesco Gabrielli39, Adolfo Puglisi35, Andrea Bertolucci35, Santino Marchi157, Massimo Bellini157, Sergio Casagli158, Belinda De Simone159, Fabio Carmassi146, Stefano Marchetti146, Marco Accorsini146, Camilla Cremonini35, Federica Morelli35.
1 Republican Vilnius University Hospital, Vilnius, Lithuania
2 Department of Surgery, G. Da Saliceto Hospital, Piacenza, Italy
3 Department of General Surgery and Trauma, University Hospital of Trauma, Tirana, Albania
4 Yonsei University College of Medicine, Seoul, Korea
5 Emergency section, Santa Casa, Piracicaba, Brazil
6 Department of Surgical Sciences and Advanced Technologies “G.F. Ingrassia”, Cannizzaro Hospital, University of Catania, Catania, Italy
7 Surgical Department, University of Trieste, Trieste, Italy
8 General and Digestive Surgery, Miguel Servet University Hospital, Zaragoza, Spain
9 Faculty of Medicine, Tabriz University of Medical Sciences, Tabriz, Iran
10 Faculty of Health Sciences, University of Zinder, Zinder National Hospital, Zinder, Niger
11 First Surgical Clinic, St. Spiridon Hospital, Grigore T. Popa University of Medicine and Pharmacy, Iasi, Romania
12 AORN Antonio Cardarelli, Napoli, Italy
13 Dept. of Emergency and Critical Care Medicine, Ehime University Hospital, Toon, Japan
14 George Eliot Hospital NHS Trust, Warwickshire, UK
15 General Surgery dept., Hospital Santo Tomas, Panama City, Panama
16 Hospital Universitário Terezinha de Jesus, Faculdade de Ciências Médicas e da Saúde de Juiz de Fora - Suprema, Juiz de Fora, Brazil
17 Department of Surgery, University of KwaZulu Natal, Durban, South Africa
18 Department of Surgery, School of Medical Sciences, University Sains Malaysia, Kelantan, Malaysia
19 Karadeniz Technical University, Dept. of General Surgery, Trabzon, Turkey
20 Vladimir City Emergency Hospital, Vladimir, Russia
21 Trauma Center, King Saud Medical City, Riyadh, Saudi Arabia
22 Department of Surgery, Nicola Giannettasio Hospital, Corigliano-Rossano, Italy
23 Division of Trauma and Acute Care Surgery, Fundación Valle del Lili, Cali, Colombia
24 Department of Abdominal and General Surgery, General Hospital Jesenice, Jesenice, Slovenia
25 Adana City Education and Research Hospital, Adana, Turkey
26 Dept. of General and Thoracic Surgery, University Hospital of Giessen, Giessen, Germany
27 Department of General Surgery, University Hospital of Heraklion, Crete, Greece
28 General Surgery Department, Bukovinian State Medical University, Chernivtsi, Ukraine
29 Family Medicine and Primary Care Department, Bukovinian State Medical University, Chernivtsi, Ukraine
30 1st Department of Surgery, Kavala General Hospital, Kavala, Greece
31 Department of General, Visceral and Thoracic Surgery, Asklepios Klinik Langen, Langen, Germany
32 Department of Surgery, Radiology, Anaesthetics and Intensive Care, University of the West Indies, Mona, Jamaica
33 Aurelia Hospital, Roma, Italy
34 General and Digestive Surgery Department, Virgen del Rocío University Hospital, Seville, Spain
35 General Emergency and Trauma Surgery Department, Pisa University Hospital, Pisa, Italy,
36 4th Surgical Department, Medical School, Aristotle University of Thessaloniki, General Hospital “G. Papanikolaou”, Thessaloniki, Greece
37 Department of Surgery, and Department of Clinical and Experimental Medicine, Linköping University, Norrköping, Sweden
38 Division of General Surgery, ASST Valle Olona, Busto Arsizio, Italy
39 General Surgery Department, Milano-Bicocca University Hospital, Monza, Italy
40 Emergency Department, Nikaia General Hospital, Piraeus, Greece
41 Department of surgery, Jubilee Mission Medical College, Thrissur, India
42 Department of Surgery, UMC Ljubljana, Ljubljana, Slovenia
43 Surgical Department, Xanthi General Hospital, Xanthi, Greece
44 General and Emergency Surgery, San Camillo-Forlanini Hospital, Roma, Italy
45 Department of Surgery, K.S. Hegde Medical Academy, Mangalore, India
46 North Estonia Medical Centre, Tallinn, Estonia
47 General Surgery Department, Erzincan University, Erzincan, Turkey
48 General Surgery, Khartoum Teaching Hospital, Sudan
49 Surgery Trauma, Hospital Padre Albino, Catanduva, Brazil
50 Trauma Team and General Surgery, ASST Niguarda, Milano, Italy
51 Emergency and Critical Care Medicine, Tokyo Women's Medical University Medical Center East, Tokyo, Japan
52 Trauma, Westmead Hospital, Westmead, Australia
53 Dept. of Surgery, Chiba Emergency Medical Center, Chiba, Japan
54 Emergency Surgery Unit, Arcispedale Sant'Anna, Ferrara, Italy
55 Department of Emergency Surgery, Cagliari University Hospital, Cagliari, Italy
56 Surgery Dept., Policlinico Umberto I, Roma, Italy
57 SAMU-Asturias, Oviedo University, Oviedo, Spain
58 Surgery, JJ Dossen Memorial Hospital, Harper, Liberia
59 University Hospital Ghent, Ghent, Belgium
60 General and Digestive Surgery Dept., Joan XXIII University Hospital, Tarragona, Spain
61 ASST Santi Paolo e Carlo, Milano, Italy
62 General Surgery Unit, Papa Giovanni XXIII Hospital, Bergamo, Italy
63 Hadassah Hebrew University Medical Center, Jerusalem, Israel
64 Anesthesia and Intensive Care Dept., Parma University Hospital, Parma, Italy
65 General Surgery, Emergency Hospital of Bucharest, Bucharest, Romania
66 PAPRSB Institute of Health Sciences, University Brunei Darussalam, Bandar Seri Begawan, Brunei
67 General Surgery, Kuala Krai Hospital, Kuala Krai, Malaysia
68 Dpt. of Clinical Medicine and Surgery, AU Policlinico Federico II, Napoli, Italy
69 General Surgery, Sant'Anna Hospital, Castelnovo ne' Monti, Italy
70 Royal Infirmary of Edinburgh, Edinburgh, UK
71 Department of Surgery, Tbilisi State Medical University, Kipshidze Central University Hospital, Tbilisi, Georgia
72 Cambridge Colorectal Unit, Cambridge University Hospitals NHS Foundation Trust, Addenbrooke’s Hospital, Cambridge Biomedical Campus, Cambridge, UK
73 Dept. of Surgery, Inje University Ilsan Paik Hospital, Goyang, South Korea
74 Department of Surgery, Centro Hospitalar e Universitário do São João, Porto, Portugal
75 Emergency Department, ASST Spedali Civili di Brescia, Brescia, Italy
76 General Surgery Department, Mansoura University Hospital, Mansoura, Egypt
77 Departamento de Emergencia, Hospital de Clínicas, Montevideo, Uruguay
78 Trauma Center ed Emergenza Chirurgica, San Martino Polyclinic Hospital, Genova, Italy
79 DEA Emergenze, AOU Policlinico G. Martino, Messina, Italy
80 Department of Respiratory and Critical Care Medicine, University Hospital Giessen, Giessen, Germany
81 Bordeaux University Hospital, Bordeaux, France
82 Tallaght University Hospital, Dublin, Ireland
83 Department of Digestive, Hepato-Pancreato-Biliary Surgery and Liver Transplantation, Henri Mondor University Hospital, Paris, France
84 Clinical Hospital Centre Zagreb, Surgical Clinic, Zagreb, Croatia
85 Acute Care Surgery, Centre Hospitalier Universitaire de Nice, Nice, France
86 Dept. of Surgery, Sahlgrenska University Hospital, Gothenburg, Sweden
87 3rd Department of Surgery, Attiko Hospital, Athens, Greece
88 Department of General Surgery, Galdakao-Usansolo Hospital, Bizkaia, Spain
89 Trauma surgery, Amsterdam UMC, Amsterdam, The Netherlands
90 Department of Surgery, Kanta-Häme Central Hospital, Hämeenlinna, Finland
91 Department of Surgery, Pt. B.D., PGIMS, Rohtak, India
92 Department of Surgical Disciplines, Immanuel Kant Baltic Federal University, Regional Clinical Hospital, Kaliningrad, Russia
93 Lewisham and Greenwich NHS Trust, London, UK
94 Department of Medical and Surgical Sciences and Advanced Technologies “G.F. Ingrassia”, University Hospital of Catania, Catania, Italy
95 Department of Surgery, Medical University of Graz, Graz, Austria
96 General and Emergency Surgery, IRCCS Reggio Emilia, Reggio Emilia, Italy
97 Städt. Klinikum Solingen, Solingen, Germany
98 Department of General and Digestive Surgery, Hospital Universitario Doctor Peset, Valencia, Spain
99 Surgery Methodist Hospital, Dallas, Texas, USA
100 Orthopedic Department, Bufalini Hospital, Cesena, Italy
101 Versilia Hospital, Lido di Camaiore, Italy
102 Anesthesia and Intensive Care Unit PS, Pisa University Hospital, Pisa, Italy
103 Emergency Surgery and Trauma Unit, Humanitas Research Hospital, Rozzano, Italy
104 Department of Surgery, University of Alberta, Edmonton, Canada
105 Dept. Clinical and Experimental Medicine, Pisa University Hospital, Pisa, Italy
106 Department of Anesthesia, Hospital Papa Giovanni XXIII, Bergamo, Italy
107 General Surgery Dept., Civil Hospital, Adria, Italy
108 Universite Laval, Quebec, Canada
109 Hospital “Dr. Alberto Balestrini” La Matanza, Buenos Aires, Argentina
110 Department of Surgery, College of Medicine, University of Ibadan, and Department of Neurological Surgery, University College Hospital, UCH, Ibadan, Nigeria
111 Department of Surgery, Harbor-UCLA Medical Center, Torrance, California, USA
112 Department of Trauma ICU, IALCH, University of KwaZulu-Natal, Durban, South Africa
113 General and Emergency Surgery Department, Angel Hospital, Venezia, Italy
114 General Surgery Department, Hospital Universitario La Paz, Madrid, Spain
115 Surgical Infections Department, Emergency Care Institute n.a. Djanelidze, Saint Petersburg, Russia
116 Department of Surgery, Port Dickson Hospital, Negeri Sembilan, Malaysia
117 Universidad Nacional de Asuncion, Facultad de Ciencias Medicas, Hospital de Clinicas, San Lorenzo, Paraguay
118 Surgical Division, Hillel Yaffe Medical Center, Hadera, Israel
119 Western Michigan University, Kalamazoo, Michigan, USA
120 General Surgery, Hospital Habib Bouguefa de Bizerte, Bizerte, Tunisia
121 Department of Gastrointestinal Surgery, Stavanger University Hospital, Stavanger, Norway
122 Department of Neurosurgery, Stavanger University Hospital, Stavanger, Norway
123 Department of Emergency Medicine, Lin-Kou Medical Center, Chang Gung Memorial Hospital, Taoyuan, Taiwan; College of Medicine, Chang Gung University, Taoyuan, Taiwan
124 Department of Traumatology, UMC Ljubljana, Ljubljana, Slovenia
125 Anesthesia and Intensive Care Unit, Bufalini Hospital, Cesena, Italy
126 Surgery, CHVNG/E, EPE, Vila Nova de Gaia, Portugal
127 Surgery, Sandro Pertini Hospital, Roma, Italy
128 Departament of Surgery, Hospital Regional de Alta Especialidad del Bajío, León, México
129 Department of Surgery, Athens Naval and Veterans Hospital, Athens, Greece;
130 Faculty of Medicine, Department of Surgery, Siriraj Hospital, Mahidol University, Bangkok, Thailand
131 Surgery, Ahmadu Bello University Teaching Hospital Zaria, Zaria, Nigeria
132 General Surgery, Al-Hussein University Hospital, Cario, Egypt
133 Surgical Clinic, Department of Clinical and Experimental Sciences, University of Brescia, ASST Spedali Civili di Brescia, Brescia, Italy
134 Emergency Medicine Department, Pisa University Hospital, Pisa, Italy
135 San Carlo Borromeo Hospital, Milano, Italy
136 Orthopaedic Department, Stavanger University Hospital, Stavanger, Norway
137 2nd Department of General Surgery, Jagiellonian University Medical College, Krakow, Poland
138 General Surgery, Santa Maria della Misericordia Hospital, Rovigo, Italy
139 General, Emergency and Trauma Surgery Department, Bufalini Hospital, Cesena, Italy
140 Neurosurgery, Pisa University Hospital, Pisa, Italy
141 University of Pavia, Department of General Surgery, IRCCS San Matteo, Pavia, Italy
142 Maxillofacial Surgery Unit, Emergency Department, ASST Niguarda, Milano, Italy
143 Department of General, Oncologic and Geriatric Surgery, Jagiellonian University Medical College, Kraków, Poland
144 Department of General Surgery, General Surgery Unit, Lecco Hospital, Lecco, Italy
145 General Surgery, San Jacopo Hospital, Pistoia, Italy
146 Orthopaedic Department, Pisa University Hospital, Pisa, Italy
147 Radiology Unit, Emergency Department, Pisa University Hospital, Pisa, Italy
148 Division of Interventional Radiology, Pisa University Hospital, Pisa, Italy
149 Infectious Diseases Clinic, Pisa University Hospital, Pisa, Italy
150 Department of Emergency Surgery, "A. Gemelli Hospital", Catholic University of Rome, Roma, Italy
151 Emergency Surgery Unit, Careggi University Hospital, Firenze, Italy
152 Unit of Surgical Oncology, Department of Medicine, Surgery and Neurosciences, University of Siena, Siena, Italy
153 General Surgery Dept., Gradenigo Hospital, Torino, Italy
154 Anesthesia and Critical Care, Ospedale Maggiore, Bologna, Italy
155 ICU Dept., Pisa University Hospital, Pisa, Italy
156 Emergency Surgery Unit, Torrette Hospital, Polytechnic University of Marche, Torrette, Italy
157 Gastrointestinal Unit, Department of Translational Sciences and New Technologies in Medicine and Surgery, Pisa University Hospital, Pisa, Italy
158 Neuro ICU dept. Pisa University Hospital, Pisa, Italy
159 Département de Chirurgie Viscérale, Centre Hospitalier Poissy/Saint Germain en Laye, Poissy, France
Abbreviations
- QI
Quality indicators
- TQI
Trauma quality indicators
- WHO
World Health Organization
- TTA
Trauma Team Activation
- GCS
Glasgow Coma Scale
- TBI
Traumatic brain injury
- ED
Emergency department
- AIS
Abbreviated Injury Scale
- ISS
Injury Severity Score
- CT
Computed tomography
- TEG
Tromboelastography
- ROTEM
Rotational thromboelastometry
- ICU
Intensive care unit
- EX-LAP
Explorative laparotomy
- SBP
Systolic blood pressure
- OR
Operating room
- E-FAST
Extended focused assessment with sonography in trauma
- REBOA
Resuscitative endovascular balloon occlusion of the aorta
- CNS
Central nervous system
- VAE
Ventilator-associated events
Authors’ contributions
FC, YK, EM, RM, RC, CO, RI, AWK, WB, MS, AH, LA, AL, VR, IC, FV, MC, ACM, BS, AP, OC, FAZ, MM, MMi, MC, VK, MS, GPF, YO, GLB, and FCa contributed to the manuscript conception and draft, critically revised the manuscript, and contributed important scientific knowledge giving the final approval.
Funding
None
Availability of data and materials
Not applicable
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Footnotes
The original online version of this article was revised: the author name Hossein Samadi Kafil was written incorrectly as Hossein Samadi Kaf mentioned in the WSES Trauma Quality Indicators Expert Panel and it has been updated.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
1/8/2025
The original online version of this article was revised: the author name Hossein Samadi Kafil was written incorrectly as Hossein Samadi Kaf mentioned in the WSES Trauma Quality Indicators Expert Panel and it has been updated.
Change history
4/7/2025
A Correction to this paper has been published: 10.1186/s13017-025-00577-8
Contributor Information
Federico Coccolini, Email: federico.coccolini@gmail.com.
the WSES Trauma Quality Indicators Expert Panel:
Zygimantas Kuliesius, Luigi Conti, Agron Dogjani, Jae Gil Lee, Heitor Consani, Domenico Russello, Marina Bortul, Teresa Gimenez Maurel, Hossein Samadi Kafil, Harissou Adamou, Vasilescu Alin, Umberto Robustelli, Norio Sato, Charalampos Seretis, Martha Quiodettis, Carlos Augusto Gomes, Victor Kong, Andee Dzulkarnaen Zakaria, Ali Guner, Mahir Gachabayov, Sharfuddin Chowdhury, Francesco Pata, Alberto Garcia, Miran Rems, Koray Das, J. G. Riedel, Konstantinos Lasithiotakis, Ruslan Sydorchuk, Larysa Sydorchuk, Eftychios Lostoridis, Alexander Buia, Michael McFarlane, Renzo Ciani, Virginia María Durán Muñoz-Cruzado, Dario Tartaglia, Orestis Ioannidis, Måns Muhrbeck, Martin Reicher, Francesco Roscio, Marco Ceresoli, Dimitrios Tsiftsis, Alfie Kavalakat, Tadeja Pintar, George Georgiou, Gabriele Ricci, Rajashekar Mohan, Sten Saar, Isidoro Di Carlo, Arda Isik, Ali Yasen Yasen Mohamed Ahmed, Ricardo Alessandro Teixeira Gonsaga, Fabrizio Sammartano, Luis Tallon-Aguilar, Tomohisa Shoko, Jeremy Hsu, Yoshiro Kobe, Christian Galatioto Luigi Romeo, Mauro Podda, Andrea Mingoli, Rafael Castro Delgado, Gerald Ekwen, Vanlander Aude, Carles Olona, Paolo Boati, Stefano Magnone, Massimo Capaldi, Miklosh Bala, Edoardo Picetti, Ionut Negoi, Kenneth Y. Y. Kok, Asri Che Jusoh, Bruno Amato, Gabriela Elisa Nita, Andrew de Beaux, Zaza Demetrashvili, R. Justin Davies, Jae Il Kim, André Pereira, Luca Fattori, Ciro Paolillo, Wagih Ghannam, Fernando Machado Rodriguez, Luca Berardi, Maria Gioffrè Florio, Matthias Hecker, Vincent Dubuisson, Donal B. O’Connor, Nicola De’Angelis, Ivan Dobrić, Damien Massalou, Per Örtenwall, Emmanouil Pikoulis, Bakarne Ugarte-Sierra, W. P. Zuidema, Aristotelis Kechagias, Sanjay Marwah, Andrey Litvin, Ioannis Nikolopoulos, Antonio Pesce, Selman Uranues, Davide Luppi, Sascha Flohe, Aleix Martínez-Pérez, Manuel Lorenzo, Luigi Branca Vergano, Mario Manca, Paolo Malacarne, Hayato Kurihara, Sandy Widder, Marsia Pucciarelli, Fabio Monzani, Pietro Brambillasca, Davide Corbella, Ferdinando Agresta, Lynne Moore, Luis Antonio Buonomo, Amos O. Adeleye, Dennis Kim, Massimiliano Veroux, Timothy Craig Hardcastle, Salomone Di Saverio, Alfonso Recordare, Ines Rubio-Perez, Sergey Shlyapnikov, Razrim Rahim, Gustavo Miguel Machain Vega, Kessel Boris, Robert Sawyer, Oussama Baraket, Kjetil Soreide, Clemens Weber, Chen-June Seak, Simon Herman, Emiliano Gamberini, Silvia Costa, Gualtiero Mazzocconi, Edgard Lozada, Dimitrios Manatakis, Varut Lohsiriwat, Adamu Ahmed, Bahaa Elbery, Guido Alberto Massimo Tiberio, Massimo Santini, Luca Mellace, Cathrine Harstad Enoksen, Piotr Major, Dario Parini, Mario Improta, Paola Fugazzola, Silvia Pini, Gaetano Liberti, Costanza Martino, Lorenzo Cobianchi, Gabriele Canzi, Enrico Cicuttin, Jakub Kenig, Mauro Zago, Sandro Giannessi, Michelangelo Scaglione, Eugenio Orsitto, Roberto Cioni, Lorenzo Ghiadoni, Francesco Menichetti, Vanni Agnoletti, Gabriele Sganga, Paolo Prosperi, Franco Roviello, Paolo De Paolis, Giovanni Gordini, Francesco Forfori, Paolo Ruscelli, Francesco Gabrielli, Adolfo Puglisi, Andrea Bertolucci, Santino Marchi, Massimo Bellini, Sergio Casagli, Belinda De Simone, Fabio Carmassi, Stefano Marchetti, Marco Accorsini, Camilla Cremonini, and Federica Morelli
References
- 1.World Health Organization (WHO). Guidelines for trauma quality improvement programmes. Geneva, Switzerland: WHO Press; 2009. ISBN 9789241597746 [Google Scholar]
- 2.Gruen RL, Gabbe BJ, Stelfox HT, Cameron PA. Indicators of the quality of trauma care and the performance of trauma systems. Br J Surg. 2012;99(Suppl 1):97–104. [DOI] [PubMed] [Google Scholar]
- 3.Gruen RL, Jurkovich GJ, McIntyre LK, Foy HM, Maier RV. Patterns of errors contributing to trauma mortality: lessons learned from 2594 deaths. Ann Surg. 2006;244:371–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.West JG, Trunkey DD, Lim RC. Systems of trauma care. A study of two counties. Arch Surg. 1979;114:455–60. [DOI] [PubMed] [Google Scholar]
- 5.Quality of Trauma for Adult Care Committee. Guide to quality indicators in adult trauma care. Calgary University. 2013 Jan. (https://site.cmg.io/scnresearch/00000000144.pdf. Access July 2020)
- 6.Donabedian A. An introduction to quality assurance in health care. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 7.Donabedian A. Evaluating the quality of medical care. Milbank Memorial Fund Q. 1966;44((3)(suppl)):166–206 Reprinted in Milbank Q. 2005;83(4):691-729. [PubMed] [Google Scholar]
- 8.Wyszewianski L, Wheeler J, Donabedian A. Market-oriented cost containment strategies and quality of care. Milbank Memorial Fund Q Health Soc. 1982;60(4):518–50. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable