Abstract
Background
Neglected fracture-dislocation thoracic spine without neurological deficit is an extremely rare injury. Current studies reveal that global sagittal balance is very important for quality of life (QOL). Complex deformity causes difficulty with dissection in the surgical planning and type of spinal osteotomy. Restoration of global balance parameters are related to a successful outcome, if the surgeon understands the morphology of complex bone deformity and the surgical tactics of spinal osteotomy.
Case presentation
A 23-year-old female presented with untreated thoracic kyphotic deformity without paraplegia (ASIA E), following a motor vehicle accident 2 months earlier. Radiographic imaging and computed tomography scan revealed a complex fracture-dislocation at the T8–T9 level with kyphosis deformity, abnormal C7 plump line, and 65 degrees of sagittal Cobb's angle (T7–T11). The multilevel Ponte osteotomy surgical technique was performed at the apex of the kyphosis. After the patient underwent corrective osteotomy and instrumentation, postoperative radiograph and CT scan revealed 24 degrees of sagittal Cobb's angle (T7–T11). The patient's balance was recovered when followed up at 1 year. The patient's quality of life was improved and thus she was extremely satisfied with this treatment.
Conclusion
Neglected fracture-dislocation thoracic spine without neurological deficit is rarely seen. It is a complex deformity injury. In this case, we performed multilevel Ponte osteotomy, instead of osteosynthesis, to restore the complex deformity that was affecting global balance. Successful outcomes are the result of good surgical preoperative planning and the surgical tactics of spinal osteotomy.
Keywords: Kyphosis deformity, Neglected fracture-dislocation, Spinal osteotomy
Introduction
Fracture-dislocation of the thoracic spine is usually caused by a high-velocity impact and can lead to spinal cord injury. The incidence of misdiagnosis varies in many studies, ranging from 19.5% to 36% [1]. Neglected fracture-dislocation thoracic spine without neurological deficit is an extremely rare injury. The neglected fracture is a fracture diagnosed more than 3 weeks after an injury due to the formation of fibrosis that occurs at the area of the injury and leads to a more difficult and complex operation [2]. The cause of missed or late detection may be undetected fractures on radiographic imaging and other factors, such as intoxication and alteration of consciousness in a polytraumatized patient. Delayed diagnosis can lead to serious complications, such as deterioration of neurological status, malunion or complex deformity, and it can affect global balance, which is important for quality of life (QOL) [3]. The complex spinal deformity form of neglected fracture-dislocation is difficult for dissection in the surgical planning and type of spinal osteotomy. The purpose of this study was to highlight the challenges in managing neglected fracture-dislocation thoracic spine without neurological deficit. The authors describe the surgical tactics of spinal osteotomy for the management of this injury.
Case report
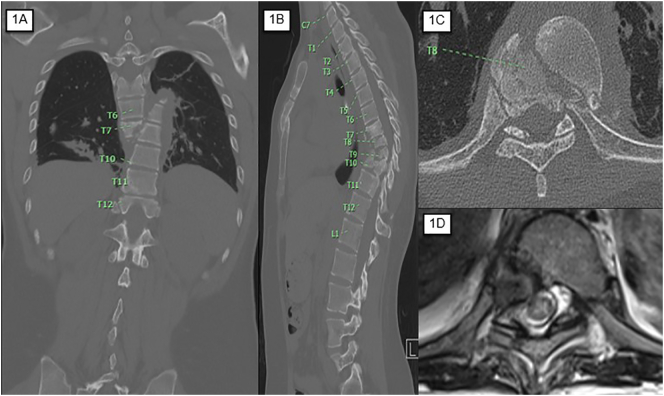
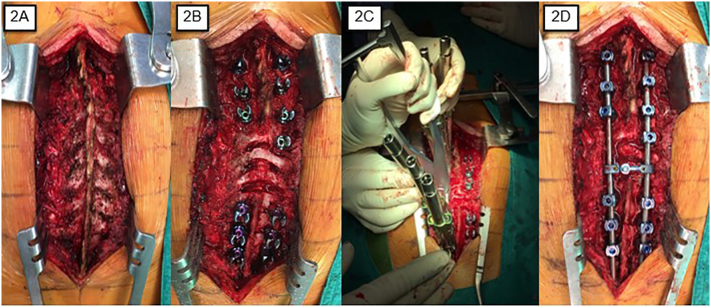
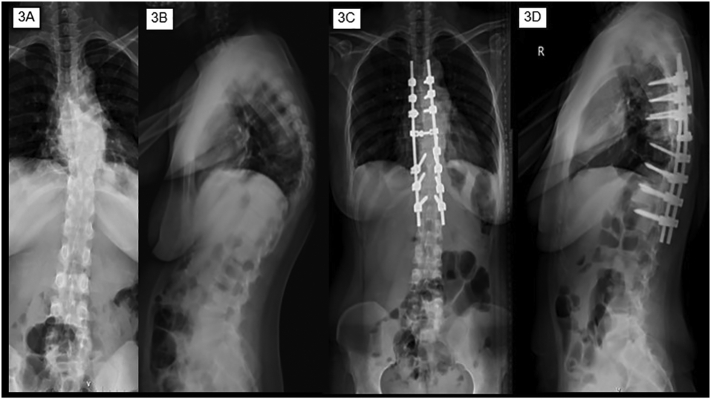
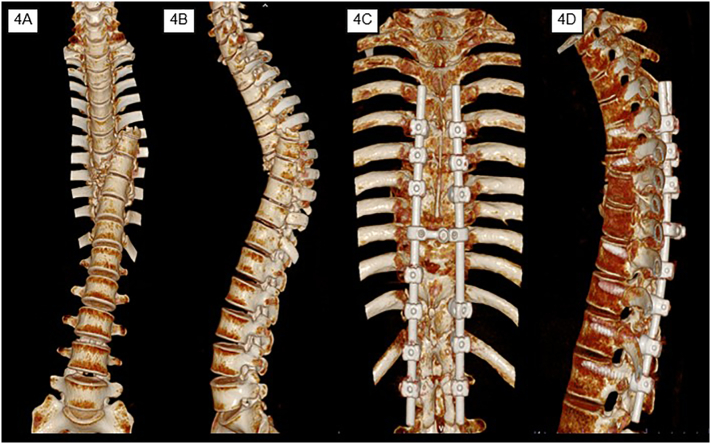
A 23-year-old female presented with untreated thoracic kyphotic deformity without paraplegia (ASIA E), following a motor vehicle accident 2 months earlier. She gradually developed progressive kyphosis deformity at the thoracic spine. She complained about painful thoracic kyphotic deformity. Her height was decreased about 8 cm and pain radiated to the anterior aspect of her left thigh when she changed position. Plain radiographs and computed tomography (CT) scan of the thoracolumbar spine showed a severely displaced coronal fracture-dislocation at the T8–9 level. The proximal part (T8 vertebra) displaced to the right side, and the distal part (T9 vertebra) migrated proximally and displaced to the left side (Fig. 1A). Sagittal imaging showed multilevel fractures and kyphotic deformity at the thoracic spine (Fig. 1B). Axial imaging of the T8 spinal level showed widening of the spinal canal without retropulsion fragment (Fig. 1C). The sagittal Cobb's angle between T7 and T11 was 65 degrees and the C7 plump line had a positive valve. The morphology configuration showed comminuted and failure at the anterior and middle column of the spine without posterior column failure; however, magnetic resonance imaging (MRI) scan showed no abnormal signal intensity of the spinal cord. The left-side neural foramen at T9–T10 was severely compromised (Fig. 1D), causing the patient pain. The patient underwent, under general anesthesia in the prone position for open reduction, decompression, corrective osteotomy, and instrumentation. The surgical tactic used was the multilevel Ponte osteotomy in order to restore the complex deformity. Intra-operative findings showed distorted alignment of the spine (Fig. 2A). The spinal navigator system assisted the pedicle screw insertion for T4 vertebra to L1 vertebra; then multilevel Ponte osteotomy was performed at the T8–10 level (Fig. 2B). The rod was rotated to correct the kyphotic curve of the thoracic spine (Fig. 2C), and then it connected the system with rods and crosslink (Fig. 2D). The comparison of preoperative and postoperative imaging (Fig. 3A–3D) and reconstructed three dimensional CT scan (Fig. 4A–4D) showed the rods and screws were in a good position and the sagittal Cobb angle was reduced from 65 to 24°. The patient's height was increased 8 cm. After the surgery, the patient used a Taylor brace for external support until the fusion site achieved union. The patient was asymptomatic and had good balance when followed up at 1 year. The patient was extremely satisfied with the treatment due to her improved back pain and quality of life. The patient returned to work.
Fig. 1.
CT scan of the patient (1A). The coronal plane shows the fracture-dislocation at the T8–9 level. The proximal part (T8 vertebra) displaced to the right side, and the distal part (T9 vertebra) migrated proximally and displaced to the left side (1B). The sagittal plane shows multilevel fractures and kyphotic deformity at the thoracic spine. Panel 1C shows widening of the spinal canal and no retropulsion fragment. Axial MRI at T9–T10 shows that the left-side neural foramen was compromised (1D).
Fig. 2.
It shows malalignment of the spine (2A), multilevel Ponte osteotomies at the T8–10 level (2B), rod rotation techniques (2C), and final construction (2D).
Fig. 3.
Plain radiographs pre-operative (3A, 3B) and post-operative (3C, 3D).
Fig. 4.
CT reconstruction pre-operative (4A, 4B) and post-operative (4C, 4D).
Discussion
In current reviews, the number of patients with spinal trauma following motor vehicle accidents has been increasing. Thoracic fractures can lead to spinal cord injury. Neglected or untreated injuries can lead to complications. Therefore, delay or misdiagnosis of a spinal fracture is a serious healthcare problem. Global sagittal malalignment is significantly correlated with QOL. The rigid deformity patterns that result from a neglected fracture-dislocation may require the use of spinal osteotomies for substantial increase [4]. Kyphotic deformity affects global spinal balance and causes pain due to instability. Preoperative planning for deformity correction should take into consideration the type of spinal osteotomy or spinal osteotomy classification. Schwab et al. [4] described the 6 anatomic grades of spinal resection for various osteotomies and classified deformity correction surgery.
Ponte et al. [5] reported in “The True Ponte Osteotomy: By the One Who Developed It” that it was originally developed for thoracic kyphosis operations in the years 1969–2015. This technique showed an effective correction of kyphosis angle from 80° (range 61°–102°) to 31° (range 15°–50°) by substantial posterior shortening [5]. In this case, it is similar to the power of correction of the Ponte osteotomy and it can be used to reduce the sagittal kyphosis angle from 65 to 24 degrees. However, neglected fracture-dislocation thoracic spine is an unstable injury. Alignment after osteotomy can be maintained by the pedicle screw and rod system. Due to the complex deformity of the injury, intra-operative CT scan (O-arm navigator system) is the most accurate instrument for neural injury prevention.
The keys to the success of the surgical tactics for deformity correction are the placement of the precontoured rigid rods and performing direct vertebral column derotation in combination with posterior column osteotomies. The pre-bending rod technique is determined from the kyphotic curvature in a normal thoracic spine. The rod derotation technique creates a kyphotic curve in the thoracic spine. In addition, the authors prefer posterolateral fusion at the osteotomy for lowering the rate of pseudarthrosis after osteotomy.
In conclusion, the authors report a rare case of neglected fracture-dislocation thoracic spine without neurological deficit. In this case, the patient underwent investigations using x-ray, CT, and MRI in order to help determine the grading of osteotomy and surgical planning. Multilevel Ponte osteotomies could restore the complex deformity that affected global sagittal balance. The successful outcome was a result of good surgical preoperative planning and the safe and effective surgical tactics of spinal osteotomy.
Ethical statement
The patient provided written informed consent to share the case details and any accompanying images published. Chiang Mai University Institutional Review Board, Faculty of Medicine and Chiang Mai University provided their approval to publish the case details. The patient's personal information remains confidential. There was no cost incurred or payment made or harm done to the patient as a result of this study.
Declaration of competing interest
No potential conflict of interest relevant to this article was reported.
Acknowledgments
Acknowledgement
The authors sincerely thank Trevor Todd Pearson for his assistance in English editing.
References
- 1.Aso-Escario J., Sebastián C., Aso-Vizán A., Martínez-Quiñones J.V., Consolini F., Arregui R. Delay in diagnosis of thoracolumbar fractures. Orthop Rev (Pavia). 2019 May 23;11(2):7774. doi: 10.4081/or.2019.7774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khatri K., Farooque K., Sharma V., Gupta B., Gamanagatti S. Neglected thoraco lumbar traumatic spine injuries. Asian Spine J. 2016 Aug;10(4):678–684. doi: 10.4184/asj.2016.10.4.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Savage J.W., Patel A.A. Fixed sagittal plane imbalance. Global Spine J. 2014 Dec;4(4):287–296. doi: 10.1055/s-0034-1394126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwab F, Blondel B, Chay E, Demakakos J, Lenke L, Tropiano P, et al. The comprehensive anatomical spinal osteotomy classification. Neurosurgery. 2015 Mar;76 Suppl 1:S33–41; discussion S41. [DOI] [PubMed]
- 5.Ponte A., Orlando G., Siccardi G.L. The true Ponte osteotomy: by the one who developed it. Spine Deform. 2018;6(1):2–11. doi: 10.1016/j.jspd.2017.06.006. [DOI] [PubMed] [Google Scholar]