Abstract
Background
Worldwide, rather few studies have examined the association between burnout and care quality using objectively measured quality indicators, with most of the studies have relied on perceived quality outcomes. This study aimed to examine the association between staff nurses’ burnout and selected objective quality metrics in long-term care wards in Japan.
Methods
This is a secondary analysis of a cross-sectional survey. Nurse managers and staff nurses working at randomly selected hospitals with long-term care wards—the equivalent of skilled nursing homes in Western countries— completed self-administered, anonymous questionnaires. The questionnaires collected data regarding care quality indicators, staff nurses’ burnout, and other confounders (e.g., ward size, participants’ years of experience, and patients’ conditions). All statistical analyses were conducted at the ward level. A multivariate regression analysis was used to examine associations between burnout and outcome indicators.
Results
Data from 196 wards in 196 hospitals (196 nurse managers and 2473 staff nurses) across Japan were analyzed. Multivariate regression analysis showed that higher emotional exhaustion was associated with higher rates of pneumonia and pressure ulcers (p-value = .036 and .032, respectively), and that reduced personal accomplishment was associated with higher rates of tube feeding (p-value = .018). A larger ward size was also associated with low rates of pneumonia (regression coefficient = −.001, p-value = .019).
Conclusions
Staff nurses’ burnout is a significant determinant of care quality in long-term care wards, implying that organizations that implement burnout reducing strategies may see greater benefits in patient outcomes. A large ward size was significantly associated with better care outcomes—specifically, low rates of pneumonia. Future research needs to determine feasible quality improvement measures in small-scale long-term care facilities, and to provide more comprehensive insights on ward-level variables that influence care quality in long-term care settings.
Keywords: Burnout, professional; Cross-sectional studies; Japan; Long-term care; Quality improvement; Quality of health care
Background
Burnout is a common, multifactorial phenomenon [1–4]. It is conceptualized as a prolonged response to chronic emotional and interpersonal stressors on the job, and is defined by the three dimensions of emotional exhaustion (EE), depersonalization (DP), and diminished sense of personal accomplishment (PA) [5]. The literature demonstrates that repercussions of burnout on care providers (e.g., attention deficits, anxiety, and insomnia) and organizations (e.g., high turnover, frequent employee absences, and frequent breaks) [6–8] can lead to poor-quality care (e.g., dissatisfaction with care, suboptimal patient care practices, and poor communication) and worsening patient safety (e.g., errors, adverse events, and safety perception) [9–13].
In long-term care (LTC) settings, nurses make up the largest proportion of the workforce [14], and they are exposed to a large number of stressors, including heavy workloads, time pressure, role conflict, role ambiguity, and physical tiredness [15, 16]. Besides, patients have complex needs, and a considerable number of them suffer from deterioration of cognitive and physical functions and impairment in the ability to communicate [3, 17]. Nurses in LTC settings, thus, are highly vulnerable to emotional strains, including burnout [18].
Worldwide, rather few studies have examined the association between burnout and care quality using objectively measured quality indicators [19], with most of the studies have relied on perceived quality outcomes, such as nurses’ perception of patient outcome [20, 21] and nurses’ rating of patient care [22]. The association between burnout and objective quality metrics is unclear, and therefore, we sought to investigate this association in LTC settings. Specifically, this study aimed to examine the association between staff nurses’ burnout and care quality in Japanese LTC wards using selected objective quality indicators, namely rates of pneumonia, rates of pressure ulcer, rates of using urinary catheters, and rates of using tube feeding. The principal research question was “Is objectively measured care quality in LTC wards related to staff nurses’ burnout?” Data reported in this manuscript are a part of a broader research project [23–25]. The current topic and results are distinct with no redundancy or duplication between the current study and any of the published studies from the same research project.
Methods
Design
This is a secondary analysis of a cross-sectional survey.
Setting, sampling and participants
This study was conducted in LTC wards across Japan. In Japan, LTC wards are comparable to skilled nursing homes in Western countries [26]. They provide LTC for older adults with severe physical and cognitive problems. Patients are generally admitted from acute/subacute hospital wards after acute treatments, or from home due to exacerbation of their morbidities [26], and the average length of the stay is about 152 days [27]. Nurses and nurse aides are the primary care providers in Japanese LTC wards. Nurses’ role is basically the same as that in general hospital wards and involves a wide range of tasks, including organization of medication, maintaining physical cleanliness, changing diapers, assistance with bathing, providing medical assistance, checking vital signs, and nutrition management, as well as providing palliative care, dementia care, respiratory care, rehabilitation, and recreation [23, 28]. Nurse aides provide, in principle, life assistance activities for the patients; such as assistance with meal, cleanliness, bathing, and movement; and work environment maintenance activities to support nurses’ work; such as organizing nursing supplies and equipment, sorting out documents and slips, and bed making. The patient-to-nurse ratio and the patient-to-nurse aid ratio are both around 20:1 [29]. Out of 3767 hospitals with LTC wards in Japan, 2000 were randomly selected. The researchers sent a letter to the nursing directors of those hospitals explaining the study aim and asking whether they were willing to participate in the study. All nurse managers and staff nurses in the LTC wards of the hospitals that agreed to participate in the study were eligible for participation.
Data collection
Nurse managers and staff nurses in the hospitals that agreed to participate in the study received self-administered, anonymous questionnaires. The nurse manager in each ward was responsible for distributing the questionnaires and then returning them to the researchers after completion via a pre-stamped envelope. Data were collected over three months (from September to November 2015).
Measurements
Care quality was assessed using four outcome indicators: the rate of patients with pneumonia, the rate of patients with pressure ulcers (degree two or worse as defined by the National Pressure Ulcer Advisory Panel [30]), the rate of patients with urinary catheter, and the rate of patients on tube feeding. These indicators were adapted from previous research on care quality in LTC settings [31–33] and were derived from multiple interviews with experienced LTC nurses and researchers in Japan. Nurse managers reported these outcomes reflecting all patients in the ward on the day of completing the questionnaires. Rates were calculated by dividing the number of patients with each outcome by the total number of patients in the ward. Since the four indicators represent negative outcomes, higher rates indicate poor-quality care.
Staff nurses’ burnout was assessed using the Japanese Burnout Scale [34], which is based on the Maslach Burnout Inventory [35]. The Japanese burnout scale consists of 17 items under three sub-scales: EE (i.e., feelings of being overextended and depleted of one’s emotional and physical resources [5 items]), DP (i.e., a negative, callous, or excessively detached response to various aspects of the job [6 items]), and PA (i.e., feelings of incompetence and a lack of achievement and productivity at work [6 items]). Each item was rated on a 5-point Likert scale ranging from 1 (never experienced) to 5 (always experience). Higher scores on EE and DP and lower scores on PA indicate higher burnout. Therefore, the PA scores were reversed so that higher scores indicate higher burnout across the three subscales. Maslach and Jackson [35] stated that the three subscales represent separate, but related, aspects of burnout and are recommended not to be used collectively. In the current study, therefore, the summed score for each subscale was computed and used separately. In the current study, the Cronbach’s alpha coefficient was .860 for the whole scale and .832, .852, and .731 for the EE, DP, and PA subscales, respectively.
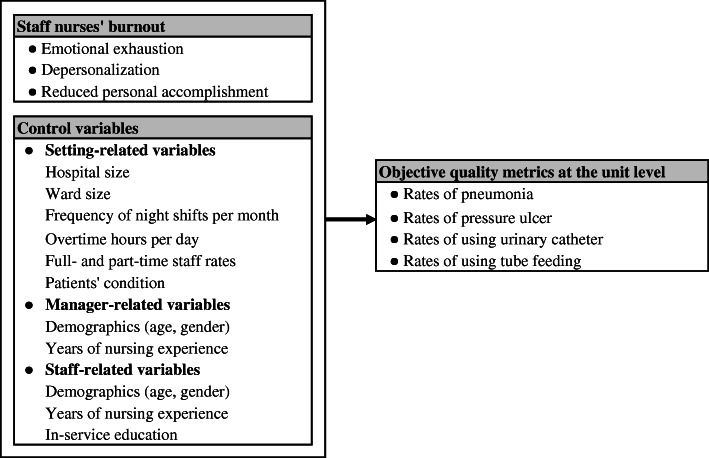
Both burnout and care quality might be influenced by healthcare system-related factors (e.g., resources and management styles), care provider-related factors (e.g., socio-demographic variables and competency) and patient-related factors (e.g., patient illness) [36–40]. Therefore, for a robust examination of the association between burnout and care quality, including such confounding variables is vital. Nevertheless, including all possible confounders in a single study may not be feasible given their broadness and heterogeneity. For this research, three types of confounders were included: setting-, manager-, and staff-related variables (Fig. 1). Setting- and manager-related variables were collected from nurse managers, whereas staff-related variables were collected from staff nurses. Setting-related variables included hospital size, ward size, frequency of night shifts in the ward, rates of full-time and part-time staff in the ward, and patients’ condition. The latter was assessed by computing the proportion of patients in three levels of dependency based on the activities of daily living (ADL), with level 1 indicating the lowest dependency and level 3 indicating the highest. This is based on the sum of a seven-level score (0: independent to 6: completely dependent) in four functions (bed mobility, transfer, eating, and toilet use). Level 1 corresponds to scores of 0–10, Level 2 to 11–22, and Level 3 to 23–24 points. These levels are used in the case mix-based payment system in Japan [41]. Manager-related variables included managers’ age, gender, and years of nursing experience. Staff-related variables included staff nurses’ age, gender, years of nursing experience, and in-service education. The latter was assessed by the number of seminars each respondent has attended in the last three months whether inside or outside the hospital.
Fig. 1.
Conceptual framework of the study
Data analysis
All statistical analyses were conducted at the ward level. Data collected from staff nurses were aggregated at the ward level using the group mean. Following the univariate analysis, bivariate analysis using the Mann-Whitney U-test or Spearman’s correlation was performed to determine which variables were associated with each of the outcome indicators. Besides, multivariate linear regression analysis using the forced entry method was performed to examine associations between burnout and outcome indicators, controlling for variables with p-value < .2 with any of the outcome indicators in the bivariate analysis. Before running the regression analysis, the four outcome indicators were log-transformed to meet the linear regression assumptions, and all explanatory variables were mean-centered. Multicollinearity between potentially explanatory variables was also examined, and when a high correlation (i.e., r > .7) was found, the most clinically significant variable was selected to be included in the model. Two variables in the current study (ward size and number of seminars inside the hospital) had outliers (one value for each variable: 96 beds and 10.14 seminars per month, respectively). Therefore, all analyses involving these variables were conducted with and without including the cases with outlier values, and the results were compared (i.e., sensitivity analysis). All analyses were conducted using SPSS Statistics software version 23 for Windows. All reported p-values are two-tailed, and the .05 level was used for statistical significance.
Ethical considerations
The Research Ethics Committee of the Graduate School of Medicine, The University of Tokyo, Japan, approved the current study (No. 10925). Along with the questionnaire, the researchers provided a letter stating the purpose and methods of the study, the voluntary nature of participation, and the confidentiality of responses. The researchers also stated that the completion and return of the questionnaires would be regarded as consent to participate. A permission to use the Japanese Burnout Scale [34] was obtained from the authors via e-mail.
Results
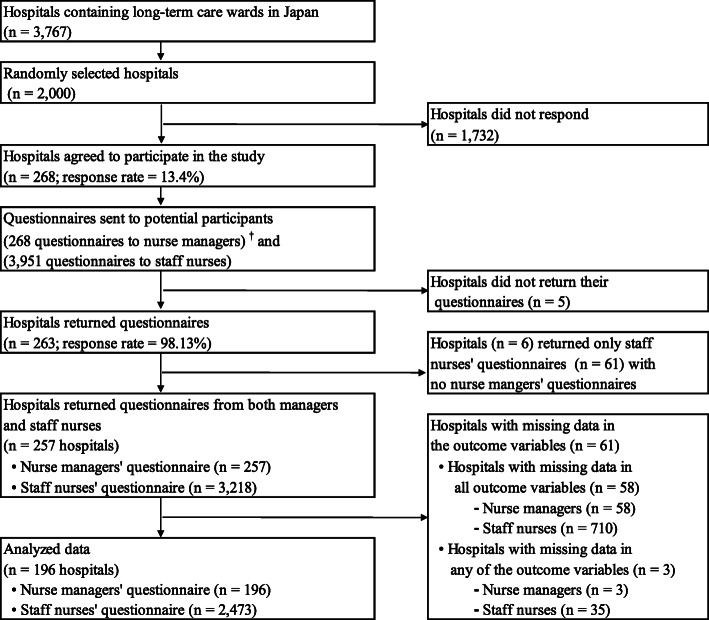
A total of 268 hospitals participated in this study (response rate = 13.4%). Of those, 257 (95.9%) have returned questionnaires from both nurse managers (n = 257) and staff nurses (n = 3218). Questionnaires from 61 hospitals were excluded due to missing data in the outcome variables. Thus, questionnaires from 196 nurse managers and 2473 staff nurses from 196 LTC wards in 196 hospitals were included in the analysis (Fig. 2). The sensitivity analysis showed that outliers were not influential, and therefore, they were included in all analyses.
Fig. 2.
Sampling flowchart. †One nurse manger per each ward and one ward per each hospital
Table 1 summarizes the distributional characteristics of the study variables. The median (and interquartile range) hospital and ward sizes were 150 (102.3–199) and 48 (40–53), respectively. The median rates of patients with pneumonia, pressure ulcer, urinary catheter, and tube feeding were .03 (.0–.06), .05 (.02–.10), .17 (.11–.27), and .36 (.22–.54), respectively. Nurse managers were predominantly female (96.9%), their mean (± standard deviation) age was 51.85 (± 7.17) years, and their median years of nursing experience was 30 (22–33). About 95% of staff nurses were female, their mean age was 44.14 (± 10.87) years, and their mean years of nursing experience was 18.03 (± 10.99). The mean number of seminars in the last three months was 2.59 (± 2.23) seminars inside the hospital and .77 (± 1.36) seminars outside the hospital. Regarding staff nurses’ burnout, the mean score was 15.67 (± 4.80) for EE, 12.36 (± 4.83) for DP, and 22.63 (± 3.93) for reduced PA.
Table 1.
Descriptive statistics of study variables
| Median [IQR], Mean ± SD, or n (%) |
|
|---|---|
| 1. Study settings-related data (n = 196) | |
| Hospital size (number of beds) | 150 [102.3–199] |
| Ward size (number of beds) | 48 [40–53] |
| Average frequency of night shifts per month | 5 [4–6] |
| Average overtime hours per day | .5 [.0–1.0] |
| Rate of full-time staff per bed | .49 ± .13 |
| Rate of part-time staff per bed | .07 [.02–.15] |
| Proportion of patients with ADL level 1 | .11 [.03–.23] |
| Proportion of patients with ADL level 2 | .23 [.14–.33] |
| Proportion of patients with ADL level 3 | .60 [.43–.79] |
| Care quality indicators | |
| Rates of patients with pneumonia | .03 [.0–.06] |
| Rates of patients with pressure ulcer | .05 [.02–.10] |
| Rates of patients with urinary catheter | .17 [.11–.27] |
| Rates of patients with tube feeding | .36 [.22–.54] |
| 2. Nurse managers-related data (n = 196) | |
| Managers’ gender | |
| Female | 190 (96.9%) |
| Male | 5 (2.6%) |
| Managers’ age (in years) | 51.85 ± 7.17 |
| Managers’ years of nursing experience | 30 [22–33] |
| 3. Staff nurses-related data (n = 2473) | |
| Staff nurses’ gender | |
| Female | 2335 (94.4%) |
| Male | 135 (5.5%) |
| Staff nurses’ age (in years) | 44.14 ± 10.87 |
| Staff nurses’ years of nursing experience | 18.03 ± 10.99 |
| In-service education in the last three months | |
| Number of seminars inside the hospital | 2.59 ± 2.23 |
| Number of seminars outside the hospital | .77 ± 1.36 |
| Burnout scores | |
| Emotional exhaustion | 15.67 ± 4.80 |
| Depersonalization | 12.36 ± 4.83 |
| Reduced personal accomplishment | 22.63 ± 3.93 |
IQR Inter-quartile range, SD Standard deviation, ADL Activity of daily living
Percentages may not add to 100% due to missing values
The bivariate analysis (Table 2) showed that higher EE was associated with higher rates of pneumonia (rho = .152, p-value = .033) and pressure ulcer (rho = .175, p-value = .014). Reduced PA was associated with higher rates of urinary catheter (rho = .164, p-value = .021) and tube feeding (rho = .148, p-value = .039). Table 2 also shows that high proportions of patients with ADL level 3 were significantly associated with high rates of urinary catheter (rho = .392, p-value ≤.001) and tube feeding (rho = .525, p-value ≤.001). Rates of pneumonia were negatively related to staff nurses’ age (rho = −.189, p-value = .008) and their years of nursing experience (rho = −.172, p-value = .016).
Table 2.
Bivariate analysis (n = 196) a
| Rates of negative events (care outcomes) in the ward b | ||||
|---|---|---|---|---|
| Pneumonia | Pressure ulcer | Urinary catheter | Tube feeding | |
| 1. Burnout c | ||||
| Emotional exhaustion | .152 ** | .175 ** | .079 | −.083 |
| Depersonalization | .140 * | .078 | .086 | −.060 |
| Reduced personal accomplishment | −.069 | −.059 | .164 ** | .148 ** |
| 2. Setting-related variables | ||||
| Hospital size | .038 | −.056 | −.016 | −.014 |
| Ward size | −.114* | .056 | .056 | .023 |
| Average frequency of night shifts per month | .055 | .029 | .076 | .081 |
| Average overtime hours per day | .037 | .048 | −.057 | −.117 * |
| Rate of full-time staff per bed | .102 * | −.009 | .010 | .024 |
| Rate of part-time staff per bed | .045 | −.036 | −.034 | .021 |
| Patients’ condition | ||||
| Proportion of patients with ADL level 1 | −.085 | −.047 | −.303 *** | −.400 *** |
| Proportion of patients with ADL level 2 | .043 | −.088 | −.279 *** | −.467 *** |
| Proportion of patients with ADL level 3 | .013 | .117 * | .392 *** | .525 *** |
| 3. Manager-related variables | ||||
| Managers’ gender | ||||
| Female | 98.13 | 98.27 | 97.95 | 97.83 |
| Male | 93.20 | 87.90 | 99.80 | 104.30 |
| Managers’ age | −.041 | −.013 | −.106 | −.012 |
| Managers’ years of nursing experience | −.023 | −.040 | −.101* | −.093* |
| 4. Staff-related variables c | ||||
| Percentage of female nurses in the ward | −.081 | .023 | .083 | .079 |
| Average of nurses’ age in the ward | −.189 ** | −.090 | −.104 * | −.048 |
| Average of nurses’ years of experience | −.172** | −.091 | −.079 | −.041 |
| In-service education c | ||||
| Seminars inside the hospital | .085 | −.058 | −.054 | .020 |
| Seminars outside the hospital | .023 | −.097 | −.030 | −.010 |
ADL Activity of daily living
a All analyses were conducted at the unit level
b Reported statistics are either correlation coefficients (Spearman’s rho) or mean ranks (for Mann-Whitney U-test)
c Data were collected from staff nurses and aggregated at the unit level using the group mean
* p-value ≤ .2; ** p-value < .05; *** p-value < .001
Four variables were excluded from the multivariate analysis because of the multicollinearity: the DP sub-scale due to a high correlation with the EE sub-scale (r = .785; p-value ≤ .001); the average of staff nurses’ age in the ward due to a high correlation with the average of their years of nursing experience (r = .883; p-value ≤ .001); and the proportions of patients with ADL levels 1 and 2 due to high correlation with the proportion of patients with ADL level 3 (r = −.741; p-value ≤ .001 and r = −.715; p-value ≤ .001, respectively). The multivariate regression analysis (Table 3) showed that high EE was associated with high rates of pneumonia (regression coefficient [B] = .002, p-value = .036) and pressure ulcer (B = .002, p-value = .032). Reduced PA was associated with higher rates tube feeding (B = .008, p-value = .018). The regression analysis also showed that a larger ward size was associated with low rates of pneumonia (B = −.001, p-value = .019). Higher proportions of patients with ADL level 3 were associated with higher rates of urinary catheter (B = .072, p-value ≤ .001) and tube feeding (B = .123, p-value ≤ .001).
Table 3.
Multivariate regression models (n = 196)
| Pneumonia rates | Pressure ulcer rates | Urinary catheter rates | Tube feeding rates | |
|---|---|---|---|---|
| B [95% CI]; p-value | B [95% CI]; p-value | B [95% CI]; p-value | B [95% CI]; p-value | |
| Constant | .016 [.013–.018]; ≤ .001 | .026 [.023–.030]; ≤ .001 | .076 [.070–.082]; ≤ .001 | .133 [.124–.141]; ≤ .001 |
| Emotional exhaustion | .002 [.000–.003]; .036 | .002 [.000–.004]; .032 | .001 [−.002–.005]; .528 | −.004 [−.009–.001]; .088 |
| Reduced personal accomplishment | −.002 [−.004–.000]; .072 | −.002 [−.004–.001]; .226 | .005 [.000–.010]; .054 | .008 [.001–.015]; .018 |
| Ward size | −.001 [−.001–.000]; .019 | .001 [.000–.001]; .597 | −.001 [−.001–.001]; .598 | .001 [−.001–.001]; .575 |
| Number of overtime hours per day | −.001 [−.002–.002]; .820 | −.001 [−.003–.002]; .601 | .002 [−.003–.007]; .536 | −.003 [−.010–.004]; .433 |
| Rate of full-time nurses in the ward | .008 [−.016–.032]; .519 | .006 [−.024–.036]; .691 | .009 [−.047–.066]; .744 | .029 [−.047–.105]; .455 |
| Proportion of patients with ADL level 3 | −.001 [−.011–.010]; .926 | .012 [−.002–.025]; .087 | .072 [.047–.098]; ≤ .001 | .123 [.089–.157]; ≤ .001 |
| Manager’s years of nursing experience | −.001 [−.001–.000]; .546 | .001 [.000–.001]; .886 | −.001 [−.001–.000]; .398 | −.001 [−.002–.000]; .078 |
| Average staff nurses’ experience in the ward | −.001 [−.001–.000]; .200 | .001 [−.001–.001]; .925 | −.001 [−.001–.001]; .916 | −.001 [−.003–.001]; .349 |
| F-test (p-value) | 2.291 (p = .023) | 1.131 (p = .345) | 5.014 (p ≤ .001) | 8.477 (p ≤ .001) |
| R2 (Adjusted R2) | .096 (.054) | .050 (.006) | .189 (.151) | .283 (.249) |
ADL Activity of daily living
All dependent variables (y) are log-transformed (Log10[y + 1]), and all independent variables (x) are mean centered (x-mean)
Discussion
The literature demonstrates the spiral down reciprocal association between burnout and care quality [42]. The current study is among the first to document the association between staff nurses’ burnout and objectively measured care quality in LTC settings. The findings suggest that interventions to manage staff burnout may positively impact not only staff but also patients [43], which highlight the significance of protecting and retaining the well-being and mental health of healthcare personnel [44]. The findings also revealed that different burnout sub-scales associate differently with different care outcomes, highlighting the distinct nature of the three burnout dimensions, and that using them collectively is not recommended [35]. Further, the current findings suggest that keeping a high proportion of experienced nurses in LTC settings may help to significantly improve patient outcomes.
In LTC settings, the high prevalence of burnout among nurses [3, 17, 45, 46] and its repercussions on care quality [46, 47] have been documented. For instance, higher burnout was associated with lower residential satisfaction [15], lower perceived quality-of-life [15], more depressive symptoms among residents [15], expressed emotions of criticism and hostility toward patients [48], and inadequate provision of comfort and support care [49]. Previous research also documented significant associations between hospital nurses’ burnout and negative patient outcomes, such as falls [20, 21] and nosocomial infection [19–21]. In other studies, however, there was no association between burnout and nosocomial infections [50] or pressure ulcer [11]. The current study confirmed that staff nurses’ burnout is a significant determinant of patient outcomes and that this association is not consistent in strength and significance across burnout sub-scales and the examined outcome indicators and may vary by the type of analysis. For instance, EE was associated with rates of pneumonia and pressure ulcers, but not with rates of urinary catheter or tube feedings in both bivariate and multivariate analyses. Conversely, reduced PA was associated only with rates of urinary catheter in the bivariate analysis and only with rates of tube feeding in the multivariate analysis. This is consistent with Salyers et al. [9], who reported that relationships between burnout and care quality differ by the type of burnout dimension, the unit of analysis, and source of quality rating.
Tawfik et al. [13] argued that objectively measuring care quality may not reliably identify certain events (e.g., near misses) and are difficult to connect to an individual provider (e.g., nurses) because of the team-based nature of caregiving. In contrast, subjective quality metrics might be more sensitive but more prone to bias (e.g., recall bias) [13]. Due to time and fund limitations, the current study relied on nurse managers’ reporting of patient outcomes instead of conducting direct observations. Nurse managers in Japanese LTC settings typically keep data regarding patient outcomes on the ward records, and therefore, the burden of reporting for the current study was minimal. By no means are the outcomes used in the current study exhaustive for evaluating care quality in LTC settings. Future research is required to establish the appropriate balance between the potential for bias with subjective quality measures and the insensitivity of objective measures [13].
The role of ward-level variables—such as infrastructure, staffing, high workload, high acuity of residents, presence of clinical education support, and high patient/carer ratio—in precipitating staff burnout and influencing care quality in LTC settings has been documented [13, 46, 51–53]. The bivariate analyses of the current study showed that the higher averages of staff nurses’ age and years of experience in the ward were associated with lower rates of pneumonia. This suggests that experienced nurses provide higher care quality than young, novice nurses, which may be explained by Benner’s [54] Novice to Expert Theory, implying that particular attention must be paid to young and novice nurses. The current study also showed that better care outcomes—precisely, low rates of patients with pneumonia—were related to a larger ward size. Previous research [55, 56] cited that strategies and innovation to enhance care quality may be challenging to implement and maintain in small-scale settings due to the lack of infrastructure, the lack of health information technology, limited resources, and the lack of adequate staff. These factors may, in part, explain the negative associations between the ward size and rates of pneumonia in the current study. Managers in small-scale settings, thus, need to pay more attention to care quality in their wards. This may include, but is not limited to, in-service training, reforming work patterns, and improvement of resources.
The outcome indicators examined in the current study are among the most reported in LTC settings worldwide. However, previous research on the association between burnout and these outcome indicators in LTC settings is scarce. The median rates of pneumonia (3%), pressure ulcers (5%), urinary catheters (17%), and tube feeding (36%) in the current study are comparable to those in the literature [57–62]. Although the current study is unable to determine whether burnout negatively affected care quality or whether negative outcomes caused burnout, findings may help to shed lights on potentially promising measures to improve care quality outcomes in LTC facilities. For instance, the current findings suggest that rates of pneumonia may be reduced by increasing the proportion of experienced nurses in the ward. Further, pneumonia prevention strategies [63, 64] need to be paid a particular attention by staff in small-size LTC facilities. Reducing nurses’ EE may be a promising strategy to help reduce rates of pneumonia and pressure ulcers in LTC facilities. Cimiotti et al. [19] argued that inadequate hand hygiene practices and lapses in other infection control procedures among nurses could be caused by cognitive detachment associated with high levels of burnout. Managers of LTC facilities with high rates of using urinary catheters and tube feeding need to pay a particular attention to nurses’ PA level. Interventions to minimize EE and enhance PA are cited in the literature and include individual-focused interventions (e.g., mindfulness, emotion regulation, stress management skills and communication skills training), organizational interventions (e.g., workload or schedule-rotation, stress management training program, debriefing sessions and a focus group) and combined interventions (e.g., stress management and resiliency training) [65, 66].
The current results are based on data derived from two distinct sources: nurse managers-reported data and staff nurses-reported data; and therefore, the possibility of personal bias is minimal. However, using a Likert scale to assess staff nurses’ burnout may be associated with a response bias. Besides, certain limitations of this study merit mention. First, this study provides only evidence of associations and is unable to determine a directionality or a causal relationship; future longitudinal studies are needed to clarify and confirm these relationships. Second, the low number of participating hospitals may raise questions regarding the generalizability of the findings; that is, only hospitals that were interested in providing high care quality might have agreed to participate in the study. The low number of participating hospitals also limited, to some extent, the inclusion of more predictors in the regression analysis. Third, the current results are based on a secondary analysis of a large-scale survey conducted primarily for other objectives. Therefore, of the numerous objective quality metrics in LTC settings [31–33, 67, 68], only four were examined in the current study. Some key care quality-related variables also were not included, such as the availability of audit systems, managerial style, professionals’ collaboration, and detailed patients’ characteristics. This limitation was evident in the low explanatory power of all regression models.
Conclusions
This cross-sectional survey found that care quality in LTC settings is related to staff nurses’ burnout, and therefore, organizations that take proactive actions to reduce burnout may see greater benefits in terms of patient outcomes. The association between burnout and care quality are not consistent in strength and significance across burnout sub-scales and the outcome indicators. Rates of pneumonia and pressure ulcers in LTC facilities may be reduced by reducing nurses’ EE. Rates of using urinary catheters and tube feeding also may be reduced by enhancing nurses’ PA levels. Future research needs to determine feasible quality improvement interventions in small-scale LTC facilities and to provide more comprehensive insights on ward-level variables that influence care quality in LTC settings.
Acknowledgements
Our sincere thanks go to the hospital administrators who agreed to participate in the current study. We also thank the managers and nurses who responded to the questionnaires.
Abbreviations
- ADL
Activity of daily living
- DP
Depersonalization
- EE
Emotional exhaustion
- LTC
Long-term care
- PA
Personal accomplishment
Authors’ contributions
NYM and AI conceptualized and designed the current study, and were major contributors in the data collection, funding acquisition, and reviewing of the manuscript. SE performed the data curation, formal analysis, data interpretation, and writing the original draft of the manuscript. AN was a major contributor in the writing and statistical analysis. All authors read and approved the final manuscript.
Funding
This research was supported by the JSPS KAKENHI Grant Number 25293462. The funder had no role in the design of this study; execution, analyses, interpretation of the data; or decision to submit results.
Availability of data and materials
The datasets of the current study are not publicly available due to containing information that could compromise the privacy of research settings and participants. Directors of participating hospitals and survey respondents were assured raw data would remain confidential and would not be shared.
Ethics approval and consent to participate
The Research Ethics Committee of the Graduate School of Nursing, The University of Tokyo, Japan, approved the current study (No. 10925). Along with the questionnaire, the researchers provided a letter stating the purpose and methods of the study, the voluntary nature of participation, and the confidentiality of responses. The researchers also stated that the completion and return of the questionnaires would be regarded as consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Sameh Eltaybani, Email: samehaltaybani@yahoo.com.
Noriko Yamamoto-Mitani, Email: noriko-tky@g.ecc.u-tokyo.ac.jp.
Ayako Ninomiya, Email: ayanino36@gmail.com.
Ayumi Igarashi, Email: igarashi-a@umin.ac.jp.
References
- 1.Bridgeman PJ, Bridgeman MB, Barone J. Burnout syndrome among healthcare professionals. Am J Health Syst Pharm. 2018;75(3):147–152. doi: 10.2146/ajhp170460. [DOI] [PubMed] [Google Scholar]
- 2.Chemali Z, et al. Burnout among healthcare providers in the complex environment of the Middle East: a systematic review. BMC Public Health. 2019;19(1):1337. doi: 10.1186/s12889-019-7713-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Costello H, et al. A systematic review and meta-analysis of the prevalence and associations of stress and burnout among staff in long-term care facilities for people with dementia. Int Psychogeriatr. 2019;31(8):1203–1216. doi: 10.1017/S1041610218001606. [DOI] [PubMed] [Google Scholar]
- 4.Dubale BW, et al. Systematic review of burnout among healthcare providers in sub-Saharan Africa. BMC Public Health. 2019;19(1):1247. doi: 10.1186/s12889-019-7566-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 6.Suñer-Soler R, et al. The consequences of burnout syndrome among healthcare professionals in Spain and Spanish speaking Latin American countries. Burn Res. 2014;1(2):82–89. doi: 10.1016/j.burn.2014.07.004. [DOI] [Google Scholar]
- 7.Salvagioni DAJ, et al. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS One. 2017;12(10):e0185781. doi: 10.1371/journal.pone.0185781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Linden DVD, et al. Work stress and attentional difficulties: an initial study on burnout and cognitive failures. Work Stress. 2005;19(1):23–36. doi: 10.1080/02678370500065275. [DOI] [Google Scholar]
- 9.Salyers MP, et al. The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med. 2017;32(4):475–482. doi: 10.1007/s11606-016-3886-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nayeri ND, et al. Burnout and productivity among Iranian nurses. Nurs Health Sci. 2009;11(3):263–270. doi: 10.1111/j.1442-2018.2009.00449.x. [DOI] [PubMed] [Google Scholar]
- 11.Thompson, D., The examination of practice environment, burnout, and missed care on pressure ulcer prevalence rates using a complexity science framework (Doctoral dissertation). Retrieved from: https://kuscholarworks.ku.edu/handle/1808/18427. Accessed 11 June 2020. 2014.
- 12.Garcia CL, et al. Influence of Burnout on Patient Safety: Systematic Review and Meta-Analysis. Medicina (Kaunas). 2019;55(9): 553. [DOI] [PMC free article] [PubMed]
- 13.Tawfik DS, et al. Evidence relating health care provider burnout and quality of care: a systematic review and meta-analysis. Ann Intern Med. 2019;171(8):555–567. doi: 10.7326/M19-1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dyer SM, et al., Review of International Systems for Long-Term Care of Older People. Adelaide: Flinders University. Retrieved from: https://agedcare.royalcommission.gov.au/sites/default/files/2020-01/research-paper-2-review-international-systems-long-term-care.pdf. 2019. Accessed 12 Feb 2021.
- 15.Chao SF. Does geriatric nursing staff burnout predict well-being of LTC residents? Geriatr Nurs. 2019;40(4):360–366. doi: 10.1016/j.gerinurse.2018.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Rai G. Burnout among long-term care staff. Adm Soc Work. 2010;34(3):225–240. doi: 10.1080/03643107.2010.480887. [DOI] [Google Scholar]
- 17.Ross MM, Carswell A, Dalziel WB. Staff burnout in long-term care facilities. Geriatrics Today. 2002;5:132–135. [Google Scholar]
- 18.Woodhead EL, Northrop L, Edelstein B. Stress, social support, and burnout among long-term care nursing staff. J Appl Gerontol. 2016;35(1):84–105. doi: 10.1177/0733464814542465. [DOI] [PubMed] [Google Scholar]
- 19.Cimiotti JP, et al. Nurse staffing, burnout, and health care-associated infection. Am J Infect Control. 2012;40(6):486–490. doi: 10.1016/j.ajic.2012.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Bogaert P, et al. Nursing unit teams matter: the relationship between nurse practice environment, nurse work characteristics, burnout and job outcome and quality of nursing care: a cross-sectional survey. Int J Nurs Stud. 2014;50(12):1667–1677. doi: 10.1016/j.ijnurstu.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 21.Nantsupawat A, et al. Nurse burnout, nurse-reported quality of care, and patient outcomes in Thai hospitals. J Nurs Scholarsh. 2015;48(1):83–90. doi: 10.1111/jnu.12187. [DOI] [PubMed] [Google Scholar]
- 22.Poghosyan L, et al. Nurse burnout and quality of care: cross-national investigation in six countries. Res Nurs Health. 2010;33(4):288–298. doi: 10.1002/nur.20383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eltaybani S, et al. Factors related to intention to stay in the current workplace among long-term care nurses: a nationwide survey. Int J Nurs Stud. 2018;80:118–127. doi: 10.1016/j.ijnurstu.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 24.Saito Y, et al. Work values and their association with burnout/work engagement among nurses in long-term care hospitals. J Nurs Manag. 2018;26(4):393–402. doi: 10.1111/jonm.12550. [DOI] [PubMed] [Google Scholar]
- 25.Yamamoto-Mitani N, et al. Staff nurses' evaluation of care process quality and patient outcomes in long-term care hospitals: a cross-sectional questionnaire survey. Int J Older People Nursing. 2020;15(4):e12334. [DOI] [PubMed]
- 26.Igarashi A, et al. Classification of long-term care wards and their functional characteristics: analysis of national hospital data in Japan. BMC Health Serv Res. 2018;18(1):655. doi: 10.1186/s12913-018-3468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ministry of Health, Labour and Welfare, Hospital Survey. Retrieved from: http://www.mhlw.go.jp/toukei/saikin/hw/iryosd/16/dl/gaikyo.pdf. Accessed 9 June 2020. (In Japanese). 2016.
- 28.Shoko F, et al. Current status of work load problem of nurse and care staffs in nursing homes and convalescent wards, and inter-professional collaboration. Nurs J Kagawa Univ. 2012;16(1):57–64. [Google Scholar]
- 29.Japan Ministry of Health, Labour and Welfare, Iryoryoyobyosyo (20:1 25:1) to kaigoryoyobyosyo tono hikaku [the comparison of Long-term care beds and sanatorium type medical care facilities for the elderly requiring care]. Retrieved from https://www.mhlw.go.jp/file/05-Shingikai-12401000-Hokenkyoku-Soumuka/0000096872.pdf. Accessed 12 Feb 2021. (In Japanese).
- 30.Edsberg LE, et al. Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System: revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43(6):585–597. doi: 10.1097/WON.0000000000000281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Medicare & Medicaid Services, Final Specifications for LTCH QRP Quality Measures and Standardized Patient Assessment Data Elements (SPADEs). Retrieved from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/LTCH-Quality-Reporting/Downloads/Final-Specifications-for-LTCH-QRP-Quality-Measures-and-SPADEs.pdf, 2017. Accessed 12 Feb 2021.
- 32.Gressel JW. Development of a quality ranking model for home health care providers. Health Mark Q. 2013;30(3):246–262. doi: 10.1080/07359683.2013.814503. [DOI] [PubMed] [Google Scholar]
- 33.National Quality Forum, National Voluntary Consensus Standards for Nursing Homes. Retrieved from: http://www.qualityforum.org/Publications/2011/07/National_Voluntary_Consensus_Standards_for_Nursing_Homes.aspx. 2011. Accessed 12 Feb 2021.
- 34.Kubo M, Tao M. Burnout among nurses. Japanese J Exp Soc Psychol. 1994;34(1):33–43. doi: 10.2130/jjesp.34.33. [DOI] [Google Scholar]
- 35.Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2(2):99–113. doi: 10.1002/job.4030020205. [DOI] [Google Scholar]
- 36.Hariharan TS, Griffin B. A review of the factors related to burnout at the early-career stage of medicine. Med Teach. 2019;41(12):1380–1391. doi: 10.1080/0142159X.2019.1641189. [DOI] [PubMed] [Google Scholar]
- 37.Manzano-Garcia G, Ayala JC. Insufficiently studied factors related to burnout in nursing: results from an e-Delphi study. PLoS One. 2017;12(4):e0175352. doi: 10.1371/journal.pone.0175352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mosadeghrad AM. Factors influencing healthcare service quality. Int J Health Policy Manag. 2014;3(2):77–89. doi: 10.15171/ijhpm.2014.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Naidu A. Factors affecting patient satisfaction and healthcare quality. Int J Health Care Qual Assur. 2009;22(4):366–381. doi: 10.1108/09526860910964834. [DOI] [PubMed] [Google Scholar]
- 40.Mosadeghrad AM. Factors affecting medical service quality. Iranian J Publ Health. 2014;43(2):210–220. [PMC free article] [PubMed] [Google Scholar]
- 41.Ikegami N. Games policy makers and providers play: introducing case-mix-based payment to hospital chronic care units in Japan. J Health Polit Policy Law. 2009;34(3):361–380. doi: 10.1215/03616878-2009-003. [DOI] [PubMed] [Google Scholar]
- 42.Williams ES, Savage GT, Linzer M. A proposed physician–patient cycle model. Stress Health. 2006;22(2):131–137. doi: 10.1002/smi.1088. [DOI] [Google Scholar]
- 43.Halbesleben JRB, et al. Nurse burnout and patient safety outcomes. West J Nurs Res. 2008;30(5):560–577. doi: 10.1177/0193945907311322. [DOI] [PubMed] [Google Scholar]
- 44.Hall, Louise H et al. Healthcare staff wellbeing, burnout, and patient safety: a systematic review. PloS one. 2016;11(7):e0159015. [DOI] [PMC free article] [PubMed]
- 45.De Rooij AH, et al. Professional caregivers' mental health problems and burnout in small-scale and traditional long term care settings for elderly people with dementia in the Netherlands and Belgium. J Am Med Dir Assoc. 2012;13(5):486. doi: 10.1016/j.jamda.2012.01.001. [DOI] [PubMed] [Google Scholar]
- 46.Sanchez S, et al. Burnout in the field of geriatric medicine: review of the literature. European Geriatric Medicine. 2015;6(2):175–183. doi: 10.1016/j.eurger.2014.04.014. [DOI] [Google Scholar]
- 47.Harrad R, Sulla F. Factors associated with and impact of burnout in nursing and residential home care workers for the elderly. Acta Biomed. 2018;89(7-S):60–69. doi: 10.23750/abm.v89i7-S.7830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tanaka K, et al. Burnout of long-term care facility employees: relationship with Employees' expressed emotion toward patients. Int J Gerontol. 2015;9(3):161–165. doi: 10.1016/j.ijge.2015.04.001. [DOI] [Google Scholar]
- 49.Hunter PV, et al. The influence of individual and organizational factors on person-centred dementia care. Aging Ment Health. 2016;20(7):700–708. doi: 10.1080/13607863.2015.1056771. [DOI] [PubMed] [Google Scholar]
- 50.Tawfik DS, et al. Burnout in the neonatal intensive care unit and its relation to healthcare-associated infections. J Perinatol. 2017;37(3):315–320. doi: 10.1038/jp.2016.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Estabrooks CA, et al. Who is looking after mom and dad? Unregulated workers in Canadian long-term care homes. Can J Aging. 2015;34(1):47–59. doi: 10.1017/S0714980814000506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Killett A, et al. How organizational factors interact to influence the quality of care of older people in the care home sector. J Health Serv Res Policy. 2013;18(1 Suppl):14–22. doi: 10.1177/1355819613476016. [DOI] [PubMed] [Google Scholar]
- 53.Yoon JY, et al. The impact of organizational factors on the urinary incontinence care quality in long-term care hospitals: a longitudinal correlational study. Int J Nurs Stud. 2012;49(12):1544–1551. doi: 10.1016/j.ijnurstu.2012.07.011. [DOI] [PubMed] [Google Scholar]
- 54.Benner P. From novice to expert. California: Addison-Wesley; 1984. [Google Scholar]
- 55.Landon BE, Normand S-LT. Performance measurement in the small office practice: challenges and potential solutions. Ann Intern Med. 2008;148(5):353–357. doi: 10.7326/0003-4819-148-5-200803040-00006. [DOI] [PubMed] [Google Scholar]
- 56.Wolfson D, et al. Quality improvement in small office settings: an examination of successful practices. BMC Fam Pract. 2009;10:14. doi: 10.1186/1471-2296-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bosco E, et al. Long-term care facility variation in the incidence of pneumonia and influenza. Open Forum Infect Dis. 2019;6(6):ofz230. [DOI] [PMC free article] [PubMed]
- 58.Anthony D, Alosoumi D, Safari R. Prevalence of pressure ulcers in long term care: a global review. J Wound Care. 2018;28(11):1–7. doi: 10.12968/jowc.2019.28.11.702. [DOI] [PubMed] [Google Scholar]
- 59.Smith PW, Nicolle LE. The chronic indwelling catheter and urinary infection in long-term–care facility residents. Infect Control Hosp Epidemiol. 2001;22(5):316–321. doi: 10.1086/501908. [DOI] [PubMed] [Google Scholar]
- 60.Gammack JK. Use and Management of Chronic Urinary Catheters in long-term care: much controversy, little consensus. J Am Med Dir Assoc. 2002;3(3):162–168. doi: 10.1016/S1525-8610(04)70459-4. [DOI] [PubMed] [Google Scholar]
- 61.Lan SH, et al. Tube feeding among elder in long-term care facilities: a systematic review and meta-analysis. J Nutr Health Aging. 2017;21(1):31–37. doi: 10.1007/s12603-016-0717-y. [DOI] [PubMed] [Google Scholar]
- 62.Burdsall D. Non-ventilator health care-associated pneumonia (NV-HAP): long-term care. Am J Infect Control. 2020;48(5S):A14–A16. doi: 10.1016/j.ajic.2020.03.007. [DOI] [PubMed] [Google Scholar]
- 63.Satheeshkumar PS, Papatheodorou S, Sonis S. Enhanced oral hygiene interventions as a risk mitigation strategy for the prevention of non-ventilator-associated pneumonia: a systematic review and meta-analysis. Br Dent J. 2020;228(8):615–622. doi: 10.1038/s41415-020-1452-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yoneyama T, et al. Oral care and pneumonia. Lancet. 1999;354(9177):P515. [DOI] [PubMed]
- 65.Zhang XJ, et al. Interventions to reduce burnout of physicians and nurses: an overview of systematic reviews and meta-analyses. Medicine (Baltimore) 2020;99(26):e20992. doi: 10.1097/MD.0000000000020992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pijpker R, et al. Combined interventions to reduce burnout complaints and promote return to work: a systematic review of effectiveness and mediators of change. Int J Environ Res Public Health. 2019;17(1):55. [DOI] [PMC free article] [PubMed]
- 67.Hutchinson AM, et al. The resident assessment instrument-minimum data Set 2.0 quality indicators: a systematic review. BMC Health Serv Res. 2010;10(166). [DOI] [PMC free article] [PubMed]
- 68.Castle NG, Ferguson JC. What is nursing home quality and how is it measured? Gerontologist. 2010;50(4):426–442. doi: 10.1093/geront/gnq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets of the current study are not publicly available due to containing information that could compromise the privacy of research settings and participants. Directors of participating hospitals and survey respondents were assured raw data would remain confidential and would not be shared.