Abstract
Background
Noise levels are monitored in call centres. A maximum of 52 to 55 dB(A) is recommended in order to prevent adverse events. We aimed at assessing the noise level and the impact of a visual noise indicator on the ambient noise level in a French Regional Emergency Medical Dispatch Centre (EMDC).
Methods
We conducted an observational study in the EMDC of the SAMU25 (University Hospital of Besancon). We measured the noise level using a SoundEarII® noise indicator (Dräger Medical SAS, France). The measurement took place in two phases on three consecutive days from 00:00 to 11:59 PM. At baseline, phase 1, the device recorded the average ambient noise for each minute without visual indication. Secondly, phase 2 included a sensor mounted with a light that would turn on green if noise was below 65 dB(A), orange if noise ever exceeded 65 and red if it exceeded 75 dB(A).
Results
In the presence of the visual noise indicator, the LAeq was significantly lower than in the absence of visual noise indicator (a mean difference of − 4.19 dB; P < 10–3). It was higher than 55 dB(A) in 84.9 and 43.9% of the time in phases 1 and 2, respectively.
Conclusions
The noise levels were frequently higher than the standards, and sometimes close to recommended limits, requiring preventive measures. The noise indicator had a positive effect on the ambient noise level. This work will allow the implementation of effective prevention solutions and, based on future assessments, could improve operators’ well-being and better care for patient.
Keywords: Medical call Centre, Noise exposure, Noise
Background
The activity of emergency medical dispatch centres (EMDC) in France is constantly increasing due to the ageing population, the decrease in the number of healthcare professionals, lack of resources, but also the environmental and industrial changes that lead to an increase in major disasters and health crises. Moreover, people constantly seek for more performant acute and emergency care. In response, the number of emergency medical dispatchers (EMD) was increased [1]. EMDs are working with emergency physicians in a limited space and in an increasingly noisier environment.
The noise effects have already been studied in call centres providing customer services. Noise is a primary hazard threatening human health [2]. It can affect physical and mental health [3–5]. Noise can cause hearing loss, stress, discomfort and musculoskeletal disorders [6–14]. A noisy environment is incompatible with undisturbed intellectual work [15]. Moreover, 16% of adult hearing loss worldwide is related to noise exposure [16]. Call centres operators may also be subject to accidental high-intensity noises associated with the use of headsets (i.e. acoustic shocks) [17], which could induce a startle effect and a temporary hearing loss [5, 18]. Standards and guidelines recommend a maximum noise level of 52 to 55 dB(A) for call centres to prevent adverse events [19–21]. However, the French National Research and Safety Institute (INRS) has shown that call centres operators may be exposed to noise levels that exceed these guidelines [5].
The impact of noise on the health of call centres operators has been widely studied and it is even considered as one of the harmful hazards, but little attention was given to noise assessment in EMDC especially since they are not really comparable to these call centres. Indeed, the French National Authority for Health (HAS) defines medical regulation as a medical act performed over the telephone [22]. EMD and emergency physicians deal with potentially life-threatening situations. In addition, the evaluation of the patient’s condition can only be done indirectly. It is therefore a very stressful and complex intellectual activity. Stress is moreover significant because of the degree of urgency and the impact of each decision on the evaluation and management of patients. Thus, we assessed the noise level in the EMDC of the SAMU 25, before and after implementing a visual noise indicator.
Methods
We conducted a single centre prospective observational study in the EMDC of Besancon University Hospital (France).
Noise level measurement in the EMDC of the SAMU25
The ambient A-weighted noise level was measured using a SoundEarII® noise indicator (Dräger Medical SAS, France) approved for indoor and outdoor noise level measurement (frequency: 20 Hz to 16 kHz, scope of measurement: 40 dB(A) to 115 dB(A), deviation: +/− 3 dB(A)). This device can generate light alerts, when the sound level exceeds predetermined thresholds. We fixed this device at a central point of the EMDC in order to be visible to the whole room. The average ambient noise level was continuously measured for each minute during a 6-day period, from 00:00 to 11:59 PM, with two phases of three consecutive days. At baseline, in phase 1, the device measured noise level without visual indication. In phase 2, the indicator was visible for each one in the room and the sensor warned the staff when the noise level exceeded the pre-set thresholds: the light turned green below 65 dB(A), orange when it exceeded the first predetermined threshold (65 dB(A)) and red when noise intensity exceeded the second threshold (75 dB(A)). We chose higher thresholds than those used in the French and international guidelines. The 65 dB(A) threshold is a recommended limit to ensure proper working conditions in call centres [15]. The 75 dB(A) is the value bellow which continuous and/or repetitive exposure is unlikely to have adverse effect on the health and safety of workers [23]. The acoustic data were analysed using the software SoundLog®.
The most common epidemiological indicators of noise exposure at the workplace are “equivalent continuous sound level” (LAeq.T) and percentile levels [24]. LAeq represents the averaged sound energy measured over a stated period of time T. For each phase, LAeq, T was calculated from 7:00 AM to 9:00 PM (LAeq, day) and from 9:00 PM to 07:00 AM (LAeq, night) according to French working time directives definitions and during the entire phase. Time spent above the INRS threshold (average background noise level at 52 dB(A)) and above the French and International organization for standardization (ISO) standards thresholds (55 dB(A)) were quantified.
Five additional conventional noise level indicators were calculated: minimum and maximum level achieved during the time of recording (Lmin or Lmax, respectively), background noise (L90, exceeded sound level 90% of the interval of time of the measurement), median noise (L50, exceeded sound level 50% of the interval of time of the measurement) and noise of crest (L10, exceeded sound level 10% of the interval of time of the measurement).
EMDC’s activity
The activity of our EMDC was estimated by the number of calls in progress during each recorded minute. We collected these data from Centaure 15®, a computerized software for file recording that is used in several EMDC in France. Based on the EMD schedules, we also considered the number of persons on duty for different periods of time (called time blocks). Each new time block began when the number of planned EMDC workers changed, and 46 different time blocks were defined for the 6 days (the time length ranged from 30 to 240 min).
Statistical analysis
A complex structure of the data was defined as follows: the noise level was measured and analysed at each minute. The number of calls was also defined at the minute level. The number of EMDC workers was defined at the time blocks level. The duration of exposure above thresholds was defined as the proportion of time spent above the 52 and 55 dB thresholds over the course of each of these time blocks.
To analyse the potential impact of the visual noise indicator on noise level (dependent variable LAeq), two-level mixed linear regression models were fitted: level 1 was defined by each minute of measurement and level 2 was defined by the time block. The analyses were adjusted on day and night periods, number of calls in progress, and number of planned EMDC workers. Interactions between number of calls and number of EMDC workers were tested.
The statistical analysis was conducted using SAS 9.4 (SAS Institute, Cary NC) and MlwiN 2.24 (Centre for Multilevel Modelling, University of Bristol).
Results
Ambient noise levels
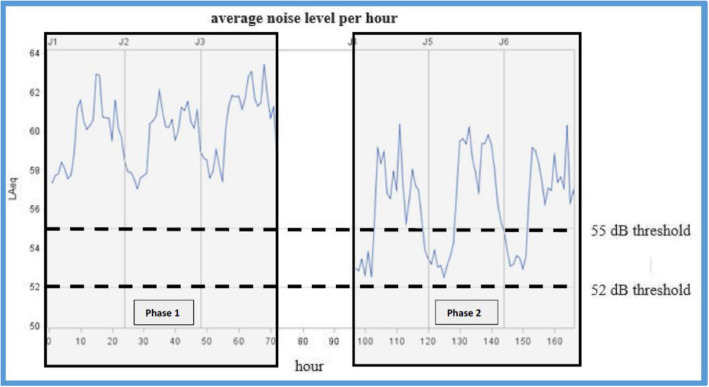
Overall noise levels during the two phases are presented in Table 1 and Fig. 1. During the 3 days of phase 1, the LAeq was higher than 52 dB(A) in 97.2% of the time, compared to 66.8% during the 3 days of phase 2., LAeq was higher than 55 dB(A) in 84.9% of the time during phase 1 compared to 43.9% during phase 2.
Table 1.
Noise levels indicators in phase 1 and phase 2 (dB(A))
| Noise level (dB(A)) | LAeq | Lmax | Lmin | L90 | L50 | L10 |
|---|---|---|---|---|---|---|
| Phase 1 | 60.3 | 76.5 | 48.5 | 54.2 | 58.9 | 62.8 |
| Phase 2 | 56.9 | 71.6 | 47.8 | 48.5 | 54.2 | 60.4 |
L10: exceeded noise level for 10% of the measurement period (crest noise)
L50: exceeded noise level for 50% of the measurement period (median noise)
L90: exceeded noise level for 90% of the measurement period (background noise)
The L10 and L90 are extensively used for impulsive sound levels and Background Noise respectively
LAeq = Equivalent Sound Level. It quantifies the noise environment to a single value of sound level for any desired duration. This descriptor correlates well with the effects of noise on people
Lmax = Maximum Sound Level: a maximum level during the measurement period
Lmin = Minimum Sound Level during the measurement period
Fig. 1.
Average sound level per hour (LAeq) time evolution
Association between noise level and activity
Table 2 presents the LAeq according to the phase 1 or 2 (absence/presence of visual indicator), the day/night period, the number of calls and the number of EMD workers.
Table 2.
Ambient noise level (LAeq) according to intervention, night and day period, and activity
| Na | Mean LAeq (dB) | SDb | |
|---|---|---|---|
| Intervention effect | |||
| Phase 1 | 4320 | 58,7 | 3,5 |
| Phase 2 | 4320 | 54,4 | 4,4 |
| Period | |||
| Day (07:00 AM – 09:00 PM) | 5040 | 57,6 | 4,5 |
| Night (09:00 PM – 07:00 AM) | 3600 | 55,1 | 4,2 |
| Number of calls per minute: | |||
| 0 | 2310 | 55,8 | 4,4 |
| 1–2 | 4307 | 56,4 | 4,5 |
| ≥ 3 | 2023 | 57,8 | 4,4 |
| Number of EMDC workers | |||
| 8–9 | 2850 | 54,8 | 4,0 |
| 10–17 | 4470 | 56,8 | 4,5 |
| 18–20 | 1320 | 59,8 | 3,6 |
aNumber of noise level measurements
bSD Standard deviation
The results of the two-level regression modelling are presented in Table 3. In the presence of the visual noise indicator (phase 2), the LAeq was significantly lower than in the absence of visual noise indicator (phase 1) (P < 10–3). The linear regression coefficient can be interpreted as a mean difference of – 4.28 dB (Model 1). In multivariable analysis, this difference remained similar (Models 2 and 3). The LAeq.T increased significantly with the number of EMDC workers regardless of the workload (Table 4). The number of calls differed significantly between the phase 1 and the phase 2 (Table 5, P < 10− 3). The average number of calls per minute declined from 2.5 by day to 1 during night time slots in phase 1 (p < 10− 3).
Table 3.
Multilevel models parameter estimates for ambient noise level LAeq
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| β | 95%CI | P | β | 95%CI | P | β | 95%CI | P | |
| Fixed Part | |||||||||
| Intercept | 58.93 | 56.83 | 56.8 | ||||||
| Intervention effect | |||||||||
| Phase 1 (without visual signal) | Ref | < 10−3 | Ref | < 10−3 | < 10−3 | ||||
| Phase 2 (with visual signal) | −4.28 | [−5.04; − 3.52] | −4.19 | [−4.63; − 3.74] | − 4.19 | [− 4.63; − 3.75] | |||
| Period | |||||||||
| Night (09:00 PM – 07:00 AM) | Ref | < 10− 3 | Ref | < 10− 3 | |||||
| Day (07:00 AM – 09:00 PM) | 1.51 | [1.17; 1.85] | 1.53 | [1.19; 1.87] | |||||
| Number of calls per minute | |||||||||
| 0 | Ref | 0.74 | 0.97 | ||||||
| 1–2 | −0.03 | [−0.22; 0.17] | 0.03 | [−0.25; 0.31] | |||||
| ≥ 3 | 0.06 | [−0.2; 0.31] | 0,00 | [−0.58; 0.58] | |||||
| Number EMDC workers | |||||||||
| 8–9 | Ref | < 10−3 | < 10− 3 | ||||||
| 10–17 | 1.41 | [0.88; 1.94] | 1.36 | [0.77; 1.95] | |||||
| 18–20 | 1.72 | [0.79; 2.64] | 2.76 | [1.6; 3.92] | |||||
| Tnteraction between the number of calls per minute and the number of EMDC workers | Ref | ||||||||
| 0 call per minute | 0.04 | ||||||||
| 1–2 calls per minute / 10–17 workers | −0.01 | [−0.41; 0.39] | |||||||
| ≥ 3 calls per minute / 10–17 workers | 0.24 | [−0.43; 0.90] | |||||||
| 1–2 calls per minute / 18–20 workers | −1.1 | [−1.97; −0.22] | |||||||
| ≥ 3 calls per minute / 18–20 workers | −1.16 | [−2.16; −0.16] | |||||||
| Random Part | |||||||||
| Level2: Time block | 1.58 | 0.39 | 0.38 | ||||||
| Level1: Minute | 13.93 | 13.88 | 13.87 | ||||||
| −2*loglikelihood: | 47,398.11 | 47,308.62 | 47,298.37 | ||||||
| Units: Time block | 46 | 46 | 46 | ||||||
| Units: Minute | 8640 | 8640 | 8640 | ||||||
CI Confidence Interval
Table 4.
Ambient noise levels LAeq according to both number of call and number of EMDC workers
| Number of people on duty | |||
|---|---|---|---|
| Number of calls | 8–9 | 10–17 | 18–20 |
| 0 | 56.3 | 59.3 | 63.4 |
| 1–2 | 56.5 | 59.0 | 61.5 |
| ≥3 | 57.7 | 59.2 | 61.1 |
The interaction between the number of calls and the numbers of EDMC workers was associated to a P-value lower then 10−3 in the two-level multivariable linear regression model
Table 5.
Number of calls total and per minute during phase 1 and 2
| Number of calls | Phase 1 | Phase 2 | Total |
|---|---|---|---|
| 0 | 1101 | 1209 | 2310 |
| 1–2 | 1979 | 2328 | 4307 |
| ≥3 | 1240 | 783 | 2023 |
| 4320 | 4320 | 8640 |
Chi-squared = 136.57–2 degrees of free (P < 10−3)
Discussion
Our study highlights several issues. First of all, the visual noise indicator proved itself very useful in reducing the noise level. During phase 1, the sound levels were very high. The overall equivalent sound level (LAeq) was 60.3 dB(A) during phase 1. The maximum average per minute reached up to 76.5 dB(A). In phase 1, the thresholds of 52 and 55 dB(A) respectively exceeded in 97.2 and 84.9% of the time whereas 66.8 and 43.9% of the time in phase 2. Second, the sound levels depended on the number of working people.
Impact assessment of the noise Indicator
The visual noise indicator allowed a significant reduction of nearly 3 dB(A) in ambient noise. The sound level (L50 = 58.9 dB(A)), exceeded by 50% during phase 1, was diminished by nearly 10% in phase 2 (L50 = 54.2 dB(A)) (Table 2). Further investigation is needed to see if this user-friendly device contributes in improving the working conditions and optimal call handling and better quality of work.
Noise level assessment
The recommended limit for background noise level is 52 dB(A) for undisturbed intellectual work [5]. The values found were greater [2, 4, 5] regardless of the considered time slot.
However, ambient noise is not the only sound perceived by the EMDs, additional noise comes from headsets too. A 20 dB(A) margin is necessary for intelligible and quality conversation. The sound level perceived directly by the EMDs could be much higher than the measured ambient noise level and may exceed the 80 dB(A) threshold requiring hearing loss preventive actions [25].
The ambient noise level within an EMDC seems comparable to that found in other call centres within the tertiary sector. It exceeded recommended limits almost all the time and sometimes even exceeded legal limits requiring preventive measures. This is worrisome. In EMDC, quick decisions, sometimes life-saving, have to be made. This requires utmost attention and focus. This is hardly compatible with a very high level of ambient noise and causes stress and exhaustion. Ambient noise can also make radio transmission less audible, leading to inaccurate assessment with possibly unfortunate repercussions.
Factors involved in variation of sound level
The difference in sound level between the day and night time slots seemed logical and mostly due to a decrease in activity. Accordingly, the increase in activity logically leads to an increase in the sound level. In the same way, the more the people, the louder the sound. This could have several reasons. First, the mere presence of a higher number of people will obviously entail a greater noise nuisance. Finally, within EMDC, there are additional parasite noises arising particularly from operators’ interactions. There are indeed numerous exchanges between staff members ranging from simple verbal instructions without using communication headsets, to discussions mostly unrelated to work.
This partly explains the rise of the additional noise disturbances with the increase in the number of people present in the closed space of the EMDC. When a large number of personnel were present in the centre, the noise level was lower when the workload was high rather than low. The reason is that an increased workload does not allow any slackness and forces the staff into focussing on work only.
A reduction of this parasite noises could be achieved by raising awareness and changing behaviours (such as forbidding off-microphone interactions) or by bringing in adjustments on work premises (less noisy material, installation or improvement of acoustic treatment solutions, enhanced office space layout …) or workstations (dual headsets, sound level controller, daily exposure time limitation).
Bias and limitations
This study has limitations. The use of a single sound level meter could inaccurately reflect the individual exposure to noise. Implementing different sound level meters could enhance accuracy in the measurements.
The sound level meter only gave equivalent continuous sound level for each minute. There are several fluctuating indoor and outdoor noise sources responsible for intense, punctual and significant short-term sound level increases in the EMDC: ambulances with sirens and helicopter landing and taking-off. They can exceed 120 dB(A) and be responsible of acoustics shocks. They are sources of stress but also of at least temporary hearing disorders. The most stressful and troublesome noises for the operators did not appear in our measures due to the time-averaged data processing.
Another limitation is the short duration of recording (3 days for each phase). In addition to a possible problem regarding the representativeness of the recorded period, a possible “novelty” effect could not be ruled out. The staff’s attention, considerable at the beginning of the device installation, could have diminished over time and led to a return to the previous sound level.
Conclusion
To our knowledge, this pilot study is the first to consider the noise level in an EMDC. Such noise levels are frequently higher than the standards and sometimes close to the recommended limits, requiring preventive measures. The noise indicator was associated to a substantial reduction in ambient noise. This might have had a positive effect on staff behaviour. Further multicentric studies are needed using a more efficient noise measurement system to take into consideration many other acoustic factors and confirm our findings. This might allow the implementation of effective prevention solutions to improve operators’ well-being.
Acknowledgements
The authors would like to express their appreciation for all the staff and physicians of the SAMU25 EMDC who made this study possible.
We are thankful for Dräger France for having graciously provided the Sound Ear System.
Abbreviations
- dB(A)
A-weighted decibels
- EMD
Emergency Medical Dispatchers in english
- EMDC
Emergency Medical Dispatch Centres
- HAS
Haute Autorité de Santé (French National Authority for Health)
- INRS
Institut National de Recherche et Sécurité (French National Research and Safety Institute)
- ISO
International Organization for Standardization
- L10
exceeded noise level for 10% of the measurement period (crest noise)
- L50
exceeded noise level for 50% of the measurement period (median noise)
- L90
exceeded noise level for 90% of the measurement period (background noise)
- LAeq
Equivalent Sound Level
- LAeq.T; LAeq, day
LAeq.T from 7:00 AM to 9:00 PM
- LAeq, night
LAeq.T from 9:00 PM to 07:00 AM
- Lmax
Maximum Sound Level
- Lmin
Minimum Sound Level
- SAMU25
Service d’Aide Médicale Urgente de Besançon
Authors’ contributions
JO and AK contributed to the design of the study and data collection. SP, AB and FM were responsible for the statistical analyses. JO, JBP and AK drafted the manuscript. JML and CL helped in collecting the data, TD reviewed the manuscript and all authors revised the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. The authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was not submitted to an ethics committee, because it doesn’t fit in the French Jardé’s law on research in humans. No patient was concerned, only the dispatchers working in the EDMC were concerned. The study was designed to protect the privacy of the participants (it was conducted anonymously and no individual data was collected). The study was presented to all the staff of the EMDC who gave a verbal consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Le Livre Blanc des Urgences. https://www.leslivresblancs.fr/livre/sante-medecine/systeme-hospitalier/organisation-de-la-medecine-durgence-en-france-un-defi-pour. Accessed 24 Jun 2020.
- 2.Beyan AC, Demiral Y, Cimrin AH, Ergor A. Call centers and noise-induced hearing loss. Noise Health. 2016;18:113–116. doi: 10.4103/1463-1741.178512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and non-auditory effects of noise on health. Lancet. 2014;383:1325–1332. doi: 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trompette N, Chatillon J. Evaluation des risques pour l’audition des opérateurs des centres d’appels téléphoniques et solutions de prévention. INRS, Note scientifique et technique 289. 2010. [Google Scholar]
- 5.Trompette N, Chatillon J. Survey of noise exposure and background noise in call centers using headphones. J Occup Environ Hyg. 2012;9(6):381–386. doi: 10.1080/15459624.2012.680852. [DOI] [PubMed] [Google Scholar]
- 6.D’Errico A, Caputo P, Falcone U, Fubini L, Gilardi L, Mamo C, et al. Risk factors for upper extremity musculoskeletal symptoms among call center employees. J Occup Health. 2010;52:115–124. doi: 10.1539/joh.L9117. [DOI] [PubMed] [Google Scholar]
- 7.Rechenberg L, Goulart B, Roithmann R. Impact of call center work in subjective voice symptoms and complaints--an analytic study. J Soc Bras Fonoaudiol. 2011;23:301–307. doi: 10.1590/S2179-64912011000400003. [DOI] [PubMed] [Google Scholar]
- 8.Norman K, Nilsson T, Hagberg M, Tornqvist EW, Toomingas A. Working conditions and health among female and male employees at a call center in Sweden. Am J Ind Med. 2004;46:55–62. doi: 10.1002/ajim.20039. [DOI] [PubMed] [Google Scholar]
- 9.Jones K, Sigmon J, Hock L, Nelson E, Sullivan M, Ogren F. Prevalence and risk factors for voice problems among telemarketers. Arch Otolaryngol Head Neck Surg. 2002;128:571–577. doi: 10.1001/archotol.128.5.571. [DOI] [PubMed] [Google Scholar]
- 10.Charbotel B, Croidieu S, Vohito M, Guerin A, Renaud L, Jaussaud J, et al. Working conditions in call-centers, the impact on employee health: a transversal study. Part II. Int Arch Occup Environ Health. 2009;82:747–756. doi: 10.1007/s00420-008-0351-z. [DOI] [PubMed] [Google Scholar]
- 11.D’Alcamo A, Omeri E, Urso P, Fossati S, Coggiola M, Levizzani G, et al. Assessment of comfort and health status of Call Center’s workers. G Ital Med Lav Ergon. 2011;33:348–350. [PubMed] [Google Scholar]
- 12.Chi CF, Lin YH. An ergonomic evaluation of a call center performed by disabled agents. Percept Mot Skills. 2008;107:55–64. doi: 10.2466/PMS.107.5.55-64. [DOI] [PubMed] [Google Scholar]
- 13.Conway PM, Campanini P, Punzi S, Fichera GP, Camerino D, Francioli L, et al. Work stress, common mental disorders and work ability index among call center workers of an Italian company. Epidemiol Prev. 2013;37:17–28. [PubMed] [Google Scholar]
- 14.Chevalier A, Dessery M, Boursier MF, Grizon MC, Jayet C, Reymond C, et al. Working conditions and psychosocial risk factors of employees in French electricity and gas company customer support departments. Int Arch Occup Environ Health. 2011;84:7–18. doi: 10.1007/s00420-010-0595-2. [DOI] [PubMed] [Google Scholar]
- 15.Smagowska B. Noise at workplaces in the call center. Arch Acoustics. 2010;35:253–264. doi: 10.2478/v10168-010-0024-2. [DOI] [Google Scholar]
- 16.Nelson DI, Nelson RY, Concha-Barrientos M, Fingerhut M. The global burden of occupational noise-induced hearing loss. Am J Ind Med. 2005;48:446–458. doi: 10.1002/ajim.20223. [DOI] [PubMed] [Google Scholar]
- 17.Westcott M. Acoustic shock injury (ASI) Acta Otolaryngol Suppl. 2006;556:54–58. doi: 10.1080/03655230600895531. [DOI] [PubMed] [Google Scholar]
- 18.Groothoff B. Acoustic shock in call centers. Aust Acoustical Soc. 2005;1:335–340. [Google Scholar]
- 19.Institut National de Recherche et de Sécurité . Les centres d’appels téléphoniques – Fiche pratique de sécurité. ED 108. 2009. [Google Scholar]
- 20.Planeau V, Robinet D. Évaluation de l’exposition sonore quotidienne des opérateurs de centres d’appels téléphoniques. INRS. Institut National de Recherche et de Sécurité. INRS Note Sci Tech. 2012;231:26. [Google Scholar]
- 21.International Organization for Standardization . Ergonomic requirements for office work with visual display terminals (VDTs) — Part 5: Workstation layout and postural requirements. EISO 9241–5. ISO. 1998. [Google Scholar]
- 22.Haute Autorité de Santé . Modalités de prise en charge d’un appel de demande de soins non programmés dans le cadre de la régulation médicale. 2011. [Google Scholar]
- 23.WHO . Environmental health criteria document No 12. Noise guidelines. Geneva: World Health Organisation; 1980. [Google Scholar]
- 24.Concha-Barrientos M, Steenland K, Prüss-Üstün A, Campbell-Lendrum DH, Corvalán CF, et al. Occupational noise: assessing the burden of disease from work-related hearing impairment at national and local levels. In: Marisol Concha-Barrientos, Diarmid Campbell-Lendrum, Kyle Steenland. World Health Organization; 2004.
- 25.Lazarus H. Prediction of verbal communication in noise—a development of generalized IL curves and the quality of communication (part 2) Appl Acoust. 1987;20(4):245–261. doi: 10.1016/0003-682X(87)90062-4. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available, but are available from the corresponding author on reasonable request.