Abstract
Background and aims
As of November 2020, the Coronavirus Disease 2019 (COVID 19) has infected more than 396,000 people in the Philippines. Although no study has been done on malnutrition among a general cohort of patients with COVID 19, it has long been associated with increased mortality and poor long-term outcomes. We aimed to determine the prevalence of malnutrition among patients with COVID 19 admitted in a tertiary government hospital.
Methods
Cross-sectional study on COVID 19-confirmed patients admitted to the COVID 19 wards from July 15 to September 15, 2020. Nutritional status was assessed using the Philippine Society for Parenteral and Enteral Nutrition (PhilSPEN) modified Subjective Global Assessment Grade (SGA) tool. Malnutrition was defined as those with SGA grades B and C. Chi-square test or Fisher exact test of association, as appropriate, was used to identify factors that have a significant association with malnutrition. Furthermore, logistic regression was done on factors with significant association.
Results
Among the 355 adult patients in the study, 71.83% (255/355) were malnourished [SGA B: 67.84% (173/255); SGA C: 32.16% (82/255)]. The following were shown to have significant association with malnutrition: community-acquired pneumonia (CAP) [p-value < 0.001], hospital-acquired pneumonia (HAP) [p-value 0.002], and chronic kidney disease (p-value 0.033). Multivariable logistic regression revealed that age [OR 1.02, CI 95% 1.00, 1.04, p-value 0.027] and CAP-Moderate Risk (MR) [OR 3.02, CI 95% 1.73, 5.27, p-value < 0.001] are significant predictors of malnutrition. All patients with CAP- High Risk and HAP were malnourished.
Conclusion
The prevalence of malnutrition was high (71.83%) in a general cohort of COVID 19 patients as measured by the modified SGA tool. The following are risk factors of malnutrition among patients with COVID 19: age, CAP, and HAP. Nutritional support and management of comorbidities are of paramount importance in the care of patients with COVID 19.
Keywords: Malnutrition, COVID 19, SGA, Age, CAP, HAP
1. Introduction
As of November 2020, the COVID-19 has affected more than 50.4 million people and resulted in more than 1.26 million deaths worldwide, with numbers continuously increasing daily [1]. In the Philippines, the disease has infected more than 396,000 people and resulted in almost seven thousand deaths [2]. This current pandemic has been declared by the World Health Organization as a global public health emergency [3].
Older adults and people of any age who have underlying medical conditions, especially if uncontrolled, are at a higher risk for acquiring severe illness from COVID-19 [4]. A cross-sectional study by Li et al. from Wuhan, China reported that 27.5% of patients aged 65 years and above were at risk for malnutrition and at least 52.7% were malnourished [5]. These figures were higher than the global incidence of malnutrition in the elderly signifying that there was a higher prevalence of malnutrition among COVID-19 patients [6]. The investigators attributed these findings to the following: first, protein consumption was increased from the acute inflammatory response from the coronavirus infection; second, the comorbid diseases of these patients, such as diabetes, may increase the risk for malnutrition; third, gastrointestinal symptoms such as diarrhea, vomiting, and poor appetite; and fourth, the patient's anxiety of having the disease may further aggravate poor appetite [5,[7], [8], [9]]. While there has been no study yet on malnutrition and mortality among patients with COVID-19, malnutrition has long been associated with increased mortality and poor long-term outcomes among patients with community acquired pneumonia. This may be due to the increased propensity of malnourished patients to develop impaired muscle and respiratory function [10].
Numerous tools have been employed to assess nutritional status and risks. One of the most widely used tool is the Subjective Global Assessment (SGA). It uses medical history which includes history of weight loss, food intake, gastrointestinal symptoms, functional capacity, disease and relation to nutritional requirements, combined with a brief physical examination suggestive of muscle wasting, alternations in fluid balance to assess nutritional status [11]. The tool is inexpensive, rapid to conduct and can be effectively used by nurses, dieticians and physicians [12,13]. In the Philippines, the modified SGA, developed by the Philippine Society of Enteral and Parenteral Nutrition (PhilSPEN), has been validated for use in the Filipino population. In addition to the standard SGA, the modified SGA tool also includes measurement of the Body Mass Index, serum albumin and total lymphocyte count [14]. This tool has been found to have a sensitivity of 94.7%, specificity of 96.2% and Positive Predictive Value of 95.7% in determining malnutrition in adults in both inpatient and outpatient settings [15].
This study aimed to determine the prevalence of malnutrition among COVID-19 patients admitted in a tertiary government hospital and explore its association with various demographic and clinical factors.
2. Materials and methods
2.1. Study design
This was a cross sectional study on the prevalence of malnutrition among COVID 19 patients admitted to the Philippine General Hospital from July 15 to September 15, 2020. This study was approved by the University of the Philippines Manila Research Ethics Board (UPMREB 2020-356-01).
2.2. Study setting
The Philippine General Hospital, the largest tertiary hospital in the country, was designated by the Department of Health as one of three COVID-19 referral centers in the National Capital Region on March 23, 2020. It designated two of its wards (previously adult medical wards) as COVID-19 wards (each with a bed capacity of 33 beds). It also converted the Medical Intensive Care Unit (MICU) into a COVID-19 ICU (Bed capacity of 8). Patients who are admitted to these wards have at least one nasopharyngeal swab RT-PCR that tested positive for the SARS-CoV-2 virus. They may have one or more of the following: bacterial pneumonia, viral (COVID 19) pneumonia, chronic kidney disease requiring hemodialysis or not. These wards also receive transfers from other institutions and from the COVID-19 ICU. An average of five patients is admitted daily into these wards. A total of 2144 admissions have been recorded since February 3, 2020. There is no active nutrition support team in the hospital.
2.3. Study population
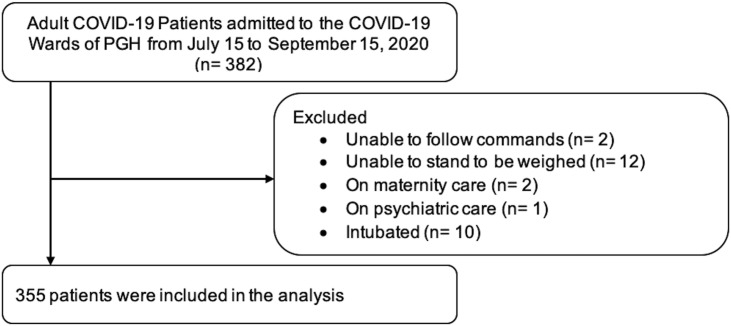
All adult patients aged 19 years and older with COVID-19 confirmed by a positive nasopharyngeal swab RT-PCR test and admitted to the COVID wards were recruited to the study. Patients who were unable to follow commands, answer when asked questions, stand to be weighed, needed maternity or psychiatric care, had missing data from their medical charts (e.g. no total lymphocyte count or serum albumin results), or did not consent were excluded (see Figure 1 ).
Fig. 1.
Study flow.
2.4. Study outcomes
Nutritional status and risk were assessed using the Philippine Society of Enteral and Parenteral Nutrition (PhilSPEN) developed Modified Subjective Global Assessment (SGA) Grade tool [14]. An SGA grade of A is normal/not malnourished, Grade B will show mild/moderate (if with +1/+2 subcutaneous fat or muscle loss) malnutrition and Grade C will show severe malnutrition. Nutritional risk score of 0–2 corresponds to low risk, a score of 3–5 corresponds to moderate risk while a score equal to 6 or greater corresponds to a high risk for malnutrition. The prevalence of malnutrition in this study was defined as participants with modified SGA scores B (mild/moderate) and C (severe).
2.5. Data collection procedure
The study was conducted from July 15 to September 15, 2020.
All ward admissions within the last 24 h were checked in the hospital's electronic database daily. Eligible patients were invited to participate in the study. Those who gave their written informed consent were enrolled and interviewed regarding weight loss, food intake, gastrointestinal symptoms, and functional capacity. The following information were obtained from their medical charts: birthdate, sex, nationality, educational attainment, employment status, city of residence, comorbidities, contact number, admission diagnoses, and latest available laboratory values of not more than 6 months for Serum Albumin and Total Lymphocyte count (TLC), physical examination on admission (i.e. edema/ascites). The height (rounded off to the nearest millimeter) and weight (rounded off to the nearest 100 g) on admission were also extracted from the medical charts. In the instances where the height and weight were not recorded on admission, the investigators measured them using the weighing scale with built-in height rod (Detecto 339) located in the wards. All data were recorded in electronic data collection forms using the Google Form application.
The body mass index (BMI) was calculated by dividing the weight in kilograms with the height in meters squared. The WHO BMI cut-offs for the general population were used instead of the Asian-cut offs because it correlated better in predicting malnutrition among the Filipino population. BMI less than 18.5 kg/m2 is underweight, BMI between 18.5 and 24.9 kg/m2 is ideal, BMI between 25.0 and 29.9 kg/m2 is overweight and BMI more than 30 kg/m2 is considered obese.
Study participants were classified according to their risk for death using the A-DROP tool, which has been shown to be a reliable tool for risk stratification in hospitalized COVID-19 patients at point of admission, with a specificity and a sensitivity of 86% and 94%, respectively [16].
The PhilSPEN-formed modified SGA tool was used to assess and rate the nutritional status of the participants based on the information obtained from the chart and the interviews.
2.6. Statistical analysis
The data were organized in MS Excel software and analyzed in STATA 15.1 (Stata corp, College Station, TX, USA). Categorical variables were summarized using frequencies and percentages. The continuous variable in the study (i.e. age) was reported in mean and standard deviation.
The prevalence of malnutrition and nutrition risk were expressed in percent. Chi-square test or Fisher exact test of association, as appropriate (parametric or non-parametric data), were used to identify significant association between malnutrition and nutrition risk with the different clinical factors. Post-hoc univariable and multivariable logistic regression were performed to identify factors significantly associated with malnutrition. The confidence interval used is 95% (p-value cut-off of 0.05).
2.7. Ethical statement
The protocol of this study adheres to the ethical considerations and ethical principles set out in relevant guidelines, including the Declaration of Helsinki, WHO guidelines, International Conference on Harmonization-Good Clinical Practice, Data Privacy Act of 2012, and National Ethics Guidelines for Health Research 2017. Prior to commencement, the protocol was approved for Technical Review by the Department of Medicine followed by University of the Philippines Manila Research Ethics Board (UPMREB) Review Panel 4.
3. Results
-
1)
The Prevalence of Malnutrition and Nutrition Risk
The prevalence of malnutrition among the adult patients with COVID-19 admitted to the COVID-19 wards of PGH was 71.83% (255 of 355). This is made up of patients who scored SGA B 48.73% (173/355) and SGA C 23.10% (82/355). The prevalence of nutrition risks of the patients were also identified with those at low risk at 37.75% (134/355), moderate risk at 47.32% (168/355), and high risk at 14.93% (53/355).
-
2)
The Demographic and Clinical Profile of the Participants according to nutrition status
Table 1 shows the characteristics of the participants in the study. There were more males (56.06%) in the study than females (43.94%). As to educational attainment, there were more who completed secondary education (45.63%) than any other group. However, almost half of the participants were unemployed (49.86%) with some of them being retired (5.07%).
Table 1.
Demographic Data of Patients included in the study.
| Mean | SD | n | % | |
|---|---|---|---|---|
| Age | 54.68 | 15.27 | ||
| Below 65 years | 257 | 72.39% | ||
| 65 years & above | 98 | 27.61% | ||
| Sex | ||||
| Male | 199 | 56.06% | ||
| Female | 156 | 43.94% | ||
| Education | ||||
| None | 3 | 0.85% | ||
| Primary | 46 | 12.96% | ||
| Secondary | 162 | 45.63% | ||
| Tertiary | 144 | 40.56% | ||
| Employment | ||||
| Unemployed | 177 | 49.86% | ||
| Employed/Self-employed | 160 | 45.07% | ||
| Retired | 18 | 5.07% | ||
| Place | ||||
| Urban | 222 | 62.54% | ||
| Rural | 133 | 37.46% | ||
| Pneumonia | ||||
| COVID-19 Pneumonia | ||||
| Low | 48 | 13.52% | ||
| Moderate | 197 | 55.49% | ||
| Severe | 110 | 30.99% | ||
| Community-Acquired Pneumonia | ||||
| Low risk | 9 | 2.54% | ||
| Moderate risk | 120 | 33.80% | ||
| High risk | 34 | 9.58% | ||
| Hospital-Acquired Pneumonia | 22 | 6.20% | ||
| Co-morbidities | ||||
| Hypertension | 220 | 61.97% | ||
| Type 2 Diabetes Mellitus | 117 | 32.96% | ||
| Bronchial Asthma | 14 | 3.94% | ||
| Chronic Kidney Disease | 76 | 21.41% | ||
| Others | 196 | 55.21% | ||
| Body Mass Index | ||||
| Underweight (BMI<18.5 kg/m2) | 13 | 3.66% | ||
| Normal (BMI 18.5–24.9 kg/m2) | 164 | 46.20% | ||
| Overweight (BMI 25–29.9 kg/m2) | 159 | 44.79% | ||
| Obese (BMI >30 kg/m2) | 19 | 5.35% | ||
The proportion of participants with ideal BMIs (18.5–24.9 kg/m2) was 46.197% (164/355), overweight (25–29.9 kg/m2) at 44.789% (159/355), underweight (<18.5 kg/m2) at 3.661% (13/355), and obese (>or equal to 30 kg/m2) at 5.352% (19/355). Majority of the patients in the study (53.802%) did not have ideal BMIs.
Table 2 shows the comparison between the malnourished and not malnourished groups. Malnutrition was found to be more common in patients with Community-Acquired Pneumonia (p-value <0.001), Hospital-Acquired Pneumonia (p-value 0.002), and Chronic Kidney Disease (p-value 0.033).
Table 2.
Comparison between patients with malnutrition or not.
| Malnourished n = 255 | Not Malnourished n = 100 | p-value | |
|---|---|---|---|
| Demographic characteristics | |||
| Sex | |||
| Male | 151 (75.88%) | 44 (24.12%) | 0.055 |
| Female | 104 (66.67%) | 52 (33.33%) | |
| Age | |||
| Below 65 years | 180 (70.04%) | 77 (29.96%) | 0.224 |
| 65 years & above | 75 (76.53%) | 23 (23.47%) | |
| Medical history | |||
| Co-morbidities | |||
| Hypertension | 165 (75.00%) | 55 (25.00%) | 0.090 |
| Type 2 Diabetes Mellitus | 89 (76.07%) | 28 (23.93%) | 0.213 |
| Bronchial Asthma | 10 (71.43%) | 4 (28.57%) | 1.000 |
| Chronic Kidney Disease | 62 (81.58%) | 14 (18.42 | 0.033 |
| COVID-19 Pneumonia | <0.001 | ||
| Low | 15 (31.25%) | 33 (67.75%) | |
| Moderate | 133 (67.51%) | 64 (32.49%) | |
| Severe | 107 (97.27%) | 3 (2.73%) | |
| Community-Acquired Pneumonia | <0.001 | ||
| Low risk | 4 (44.44%) | 5 (55.56%) | |
| Moderate risk | 97 (80.83%) | 23 (19.17%) | |
| High risk | 34 (100.00%) | – | |
| Hospital-Acquired Pneumonia | 22 (100.00%) | – | 0.002 |
There were more obese than underweight (13 vs 19). Furthermore, majority (77%) of the underweight were classified as malnourished, while only 15% of those who were obese were classified as malnourished (Table 6). The investigators did an analysis between underweight and obese with COVID-19 pneumonia severity. Our analysis showed that there is no sufficient evidence to conclude that either factors are associated with COVID-19 pneumonia severity (Table 5 ).
-
3)
The Demographic and Clinical Profile of Participants according to Nutrition Risk
Table 6.
PhilSPEN modified subjective global assessment.
| RISK LEVEL | LOW | MODERATE | HIGH | TOTAL |
|---|---|---|---|---|
| Risk score | (0–2) | (3–5) | (6–9) | |
| n (%) | 134 (37.75%) | 168 (47.32%) | 53 (14.93%) | 355 |
| Subjective Global Assessment | ||||
| A | 75 (75.00%) | 25 (25.00%) | – | 100 |
| B | 59 (34.10%) | 108 (62.43%) | 6 (3.47%) | 173 |
| C | – | 35 (42.68%) | 47 (57.32%) | 82 |
| Body Mass Index | ||||
| 18.5–24.9 kg/m2 | 78 (47.56%) | 78 (47.56%) | 8 (4.88%) | 164 |
| 25–29.9 kg/m2 | 48 (30.19%) | 73 (45.91%) | 38 (23.90%) | 159 |
| <18.5 kg/m2 | 1 (7.69%) | 7 (53.85%) | 5 (38.46%) | 13 |
| >30 kg/m2 | 9 (47.37%) | 7 (36.84%) | 3 (15.79%) | 19 |
| Albumin | ||||
| <2.5 g/dL | – | – | – | – |
| 2.5–3.4 g/dL | – | – | – | – |
| >3.4 g/dL | 134 (37.75%) | 168 (47.32%) | 53 (14.93%) | 355 |
| Total Lymphocyte Count | ||||
| >1500 cells/mm3 | 89 (78.76%) | 24 (21.24%) | – | 113 |
| 900–1500 cells/mm3 | 40 (32.79%) | 69 (56.56%) | 13 (10.66%) | 122 |
| <900 cells/mm3 | 5 (4.17%) | 75 (62.50%) | 40 (33.33%) | 120 |
Table 5.
Association between undernourishment/obesity with COVID-19 severity.
| BMI | COVID-19 Severity |
p-value | ||
|---|---|---|---|---|
| Mild |
Moderate |
Severe |
||
| n = 2 | n = 23 | n = 6 | ||
| Undernourished (BMI<18.5) | – | 11 (84.62%) | 2 (15.38%) | 0.564 |
| Obese (BMI ≥ 30) | 2 (11.11%) | 12 (66.67%) | 4 (22.22%) | |
The profiles of the patients included in the study grouped according to nutrition risk are shown in Table 3 . Malnutrition Risk was increased in patients with age above 65 years old (p-value 0.036), CAP (p-value <0.001), and Bronchial Asthma (p-value 0.003). There were no significant associations between malnutrition and other sociodemographic factors such as educational attainment, place of residence, or employment status.
-
4)
Regression analysis of Malnutrition/No Malnutrition and select variables
Table 3.
Comparison between patients with low, moderate, and high nutrition risk.
| Low Risk n = 134 | Moderate Risk n = 168 | High Risk n = 53 | p-value | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Sex | ||||
| Male | 68 (34.17%) | 94 (47.24%) | 37 (18.59%) | 0.061 |
| Female | 66 (42.31%) | 74 (47.44%) | 16 (10.26%) | |
| Age | ||||
| Below 65 years | 106 (41.25%) | 111 (43.19%) | 40 (15.56%) | 0.036 |
| 65 years & above | 28 (28.57%) | 57 (58.16%) | 13 (13.27%) | |
| Medical history | ||||
| Co-morbidities | ||||
| Hypertension | 77 (35.00%) | 114 (51.82%) | 29 (13.18%) | 0.090 |
| Type 2 Diabetes Mellitus | 38 (32.48%) | 59 (50.43%) | 20 (17.09%) | 0.335 |
| Bronchial Asthma | 10 (71.43%) | 1 (7.14%) | 3 (21.43%) | 0.003 |
| Chronic Kidney Disease | 20 (26.32%) | 41 (53.95%) | 15 (19.74%) | 0.057 |
| COVID-19 Pneumonia | ||||
| Low | 35 (72.92%) | 11 (22.92%) | 2 (4.16%) | |
| Moderate | 78 (39.59%) | 100 (50.76%) | 19 (9.65%) | <0.001 |
| Severe | 21 (19.09%) | 57 (51.82%) | 32 (29.09%) | |
| Community-Acquired Pneumonia | <0.001 | |||
| Low risk | 8 (88.89%) | 1 (11.11%) | – | |
| Moderate risk | 40 (33.33%) | 61 (50.83%) | 19 (15.93%) | |
| High risk | 2 (5.88%) | 18 (52.94%) | 14 (41.18%) | |
| Hospital-Acquired Pneumonia | 5 (22.73%) | 11 (50.00%) | 6 (27.27%) | 0.153 |
Individual (Univariable) logistic regression showed that age, CAP, and CKD are significant predictors of malnutrition among COVID-19 patients admitted in PGH (Table 4 ). Taking into account all the factors investigated (Multivariable logistic regression), age and CAP are significant predictors of malnutrition among COVID-19 patients admitted in PGH.
Table 4.
Factors predicting malnutrition among COVID-19 patients admitted in PGH.
| Factors | Univariable |
Multivariable |
||||
|---|---|---|---|---|---|---|
| Odds Ratio | 95% CI | p-value | Odds Ratio | 95% CI | p-value | |
| COVID-19 Severity | ||||||
| Low | Reference | Reference | ||||
| Moderate | 4.57 | [2.32, 9.02] | <0.001 | 3.36 | [1.65, 6.83] | 0.001 |
| Severe | 78.47 | [21.39, 287.79] | <0.001 | 35.56 | [9.21, 137.35] | <0.001 |
| Age≥65 | 1.39 | [0.81, 2.39] | 0.225 | |||
| Female | 0.64 | [0.40, 1.01] | 0.056 | |||
| Urban residence | 1.10 | [0.68, 1.76] | 0.708 | |||
| Educational Attainment | ||||||
| None | Reference | |||||
| Elementary | 6.36 | [0.53, 77.08] | 0.146 | |||
| High School | 4.00 | [0.35, 45.10] | 0.262 | |||
| College | 6.73 | [0.59, 76.54] | 0.124 | |||
| Community-Acquired Pneumonia | ||||||
| None | Reference | Reference | ||||
| Low Risk | 0.48 | [0.12, 1.85] | 0.285 | 0.93 | [0.23, 3.80] | 0.919 |
| Moderate Risk | 2.53 | [1.47, 4.34] | 0.001 | 1.69 | [0.92, 3.10] | 0.092 |
| High Risk | Omitteda | |||||
| Hospital-Acquired Pneumonia | Omitteda | |||||
| Chronic Kidney Disease | 1.97 | [1.05, 3.72] | 0.035 | 1.80 | [0.89, 3.66] | 0.105 |
| Hypertension | 1.55 | [0.97, 2.47] | 0.067 | |||
| Type 2 Diabetes Mellitus | 1.38 | [0.83, 2.29] | 0.214 | |||
| Bronchial Asthma | 0.98 | [0.30, 3.20] | 0.973 | |||
Predicts perfectly.
4. Discussion
Emerging studies on patients with COVID-19 indirectly shows the importance of nutrition in possibly determining the outcomes of patients with COVID-19 [17]. Our cross-sectional study found that 71.83% of adult patients admitted in the COVID-19 wards of PGH were malnourished. The risks for malnutrition of the participants were also determined: 37.75% were low risk (risk score of 0–2), 47.32% were moderate risk (risk score of 3–5), and 14.93% were high risk (risk score of 6 or more). Risk factors for malnutrition among patients diagnosed with COVID 19 found in this study are the following: older age, severity of pneumonia and presence of Chronic Kidney Disease.
Recent studies have shown that COVID-19 is associated with poorer outcomes in older patients with multiple comorbidities [18]. A recent Chinese publication found a high prevalence (52.7%) of malnutrition among 182 elderly patients (mean age of 68.5 years-old) diagnosed with COVID-19 using the Mini Nutritional Assessment (MNA) which is validated for use in the elderly population. The tool has a subjective (interview) part and takes into account anthropometric measures (BMI and calf circumference) [5]. In another study with French patients (mean age of 59.5 years-old), the prevalence of malnutrition was 37.5% using the Global Leadership Initiative on Malnutrition (GLIM) criteria. The GLIM criteria is similar with the MNA in that they have a subjective component and take into account the patient's BMI [19]. Despite the relatively younger cohort of the participants in our study compared to those mentioned above (Mean age 54.68 [SD 15.27] years-old), age was still shown to be a risk factor for malnutrition with every additional year conferring an additional 2–3% risk of being malnourished.
Our study has shown that those concurrently diagnosed with pneumonia had a higher risk of being malnourished. Furthermore, the more severe the pneumonia the higher the risk; those with CAP-Moderate Risk were 2.02 times (to as high as 2.53 times) likely to be malnourished, and those with CAP-High Risk and Hospital-Acquired Pneumonia were all malnourished. Malnutrition has long been associated with alterations in the lung's ability to resist invading pathogens that lead to increased incidence, more virulent and prolonged respiratory infection that ultimately lead to poor long-term outcome in these patients [10,20].
Our study has also shown that patients with COVID 19 and Chronic Kidney disease had approximately twice (OR 1.97) the risk of being malnourished. Malnutrition in CKD is caused by an interplay of several factors, such as decreased appetite and nutrient uptake, metabolic imbalances, hormonal derangements, inflammation, dialysis-related abnormalities, and increased catabolism [21].
Aside from nutritional status, the investigators also looked into nutrition risk. Age above 65 years old, CAP, and Bronchial Asthma were found to have a significant association with nutrition risk. The findings could be explained by the inflammatory nature of COVID-19 and the established cause of malnutrition which is multifactorial. These include the metabolic effects of underlying disease, reduced nutritional intake, age, educational level of the patients of living situation, and polypharmacy as seen in those having maintenance medications for chronic organ failure [22,23].
This study shows that majority of the participants included in the study currently have no jobs (unemployed and retired) and a considerable proportion have only finished secondary education. These socio-economic factors may contribute to the patients being malnourished on admission; those with no occupation and lesser educational attainment possibly have lesser access to and/or knowledge about adequate nutrition. COVID 19 has also exposed the vulnerability and weakness of the food systems. Wide scale lockdowns have interrupted food supply that have greatly affected the already impoverished and undernourished population who are at higher risk for acquiring COVID infection [24].
This study has several limitations. First, it is a single-center study done in a tertiary government hospital located in the National Capital Region that was designated as a COVID-19 referral center. This may have caused some selection bias-- the admitted patients were mostly from within the vicinity, or may have had more severe disease, hence may not be representative of COVID 19 patients in general. Second, other factors that may affect the nutrition status and/or severity of their diseases and comorbidities were not analyzed in the study, such as lifestyle habits, physical activity, and social support. Third, some of the collected data (e.g. weight loss prior to hospitalization, food intake) were subjective and may have been subject to recall bias. Fourth, the relatively small sample size may have limited the study's ability to demonstrate significant associations between malnutrition and other variables.
We recommend that larger multi-center studies be done in different COVID-19 referral centers or hospitals throughout the country to better reflect the burden of malnutrition among those with COVID-19. We also recommend that more objective measurements of malnutrition be taken (i.e. mid upper arm circumference and triceps skin fold).
5. Conclusion
The prevalence of malnutrition among hospitalized patients with COVID-19 was high (71.83%). Risk factors for malnutrition among these patients include older age, severity of pneumonia and chronic kidney disease. Routine nutrition screening and assessment for all patients admitted in the COVID wards and management of malnourished patients by a nutrition support team are recommended. Larger, multi-center studies that use more objective measures of malnutrition are also recommended.
6. Implications for clinical practice
Malnutrition is associated with poorer outcomes among admitted patients. Therefore, screening for malnutrition (by using a tool validated for Filipinos such as the modified SGA tool) and also addressing it is critical in treating and preventing further adverse health outcomes. This is important especially in the context of the current pandemic where different modes of therapy are still currently under investigation.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Statement contribution
RBL: Conceptualization, Methodology, Formal Analysis, Investigation, Resources, Data Curation, Writing – Original Draft, Visualization, Project Administration, and Funding Acquisition. BMP: Methodology, Writing – Original Draft, Visualization. EMM: Methodology, Writing – Original Draft, Visualization. HHC: Formal Analysis, Investigation, Resources, Data Curation, Writing – Original Draft. LPV: Conceptualization, Methodology, Writing – Original Draft, and Supervision.
Declaration of competing interest
The principal investigators and co-investigators have no relevant conflicts of interest.
Acknowledgements
The investigators would like to acknowledge the expert advice by Dr. Joyce B. Bernardino. We would also like to acknowledge the unwavering support of the administration of the Philippine General Hospital in the conduct of this study in the COVID 19 wards of the hospital.
References
- 1.COVID 19 Coronavirus Pandemic 2020. https://www.worldometers.info/coronavirus/ Accessed from.
- 2.COVID 19 Case tracker. 2020. https://www.doh.gov.ph/2019-nCoV Accessed from. [Google Scholar]
- 3.Coronavirus disease (COVID-19) Outbreak 2020. https://www.who.int/westernpacific/emergencies/covid-19 Accessed from.
- 4.Coronavirus disease 2019 (COVID-19) 2020. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html Accessed from. [Google Scholar]
- 5.Li T., Zhang Y., Gong C., Wang J., Liu B., Shi L., et al. Prevalence of malnutrition and analysis of related factors in elderly patients with COVID-19 in Wuhan, China. Eur J Clin Nutr. 2020;74(June 2020):871–875. doi: 10.1038/s41430-020-0642-3. Accessed from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaiser M.J., Bauer J.M., Rämsch C., Uter W., Guigoz Y., Cederholm T., et al. Frequency of malnutrition in older adults: a multinational perspective using the mini nutritional assessment. J Am Geriatr Soc. 2010;58:1734–1738. doi: 10.1111/j.1532-5415.2010.03016.x. [DOI] [PubMed] [Google Scholar]
- 7.Jia H. Pulmonary angiotensin-converting enzyme 2 (ACE2) and inflammatory lung disease. Shock. 2016;46:239–248. doi: 10.1097/SHK.0000000000000633. [DOI] [PubMed] [Google Scholar]
- 8.Phielix E., Mensink M. Type 2 diabetes mellitus and skeletal muscle metabolic function. Physiol Behav. 2008;94:252–258. doi: 10.1016/j.physbeh.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 9.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., et al. Clinical characteristics of coronavirus disease 2019 in China. New england journal of medicine. 2019. https://www.nejm.org/doi/full/10.1056/NEJMoa2002032 Accessed from. [DOI] [PMC free article] [PubMed]
- 10.Yeo H.J., Byun K.S., Han J., Kim J.H., Lee S.E., Yoon S.H., et al. Prognostic significance of malnutrition for long-term mortality in community-acquired pneumonia: a propensity score matched analysis. Kor J Intern Med. 2019;34(4):841–849. doi: 10.3904/kjim.2018.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Steiber A.L., Kalantar-Zadeh K., Secker D., McCarthy M., Sehgal A., McCann L. Subjective Global Assessment in chronic kidney disease: a review. J Ren Nutr. 2004;14(4):191–200. doi: 10.1053/j.jrn.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Visser R., Dekker F.W., Boeschoten E.W., Stevens P., Krediet R.T. Reliability of the 7-point subjective global assessment scale in assessing nutritional status of dialysis patients. Adv Perit Dial Conf. 1999;15:222–225. [PubMed] [Google Scholar]
- 13.Jones C.H., Wolfenden R.C., Wells L.M. Is subjective global assessment a reliable measure of nutritional status in hemodialysis? J Ren Nutr. 2004;14:26–30. doi: 10.1053/j.jrn.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 14.Bernardino J., Li L. The prognostic capacity of the nutrition risk score and subjective global assessment (SGA) grade of the PhilSPEN modified SGA on mortality outcomes. PhilSPEN Online J Parenter Enteral Nutr. 2018;29(July 2016):134–136. http://www.philspenonlinejournal.com/POJ_0117.html Accessed from. [Google Scholar]
- 15.Lacuesta-Corro L., Paguia G., Lorenzo A., Navarette D., Llido L. The results of the validation process of a modified SGA (subjective global assessment) nutrition assessment and risk level tool designed by the clinical nutrition service of st. Luke’s medical center, a tertiary care hospital in the Philippines. PhilSPEN Online J Parenter Enteral Nutr. 2013;12(February 2012):1–7. http://www.philspenonlinejournal.com/POJ_0002.html Accessed from. [Google Scholar]
- 16.Fan G., Tu C., Zhou F., Liu Z., Wang Y., Song B., et al. Comparison of severity scores for COVID-19 patients with pneumonia: a retrospective study. Eur Respir J. 2020;56(3) doi: 10.1183/13993003.02113-2020. 2002113. Published 2020 Sep. 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rouget A., Vardon-Bounes F., Lorber P.,, Vavasseur A., Marion O., Marcheix B., et al. Prevalence of malnutrition in COVID-19 inpatients: the Nutricov study. 2020. https://assets.researchsquare.com/files/rs-41500/v1/5ba62f4a-860b-435f-8718-c5aacd5e61a3.pdf Accessed from. [DOI] [PMC free article] [PubMed]
- 18.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laviano A., Koverech A., Zanetti M. Nutrition support in the time of SARS-CoV-2 (COVID-19) Nutrition. 2020;74 doi: 10.1016/j.nut.2020.110834. 110834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Niederman M.S. In: Nutrition and ventilatory function. Current topics in rehabilitation. Ferranti R.D., Rampulla C., Fracchia C., Ambrosino N., editors. Springer; London: 1992. Malnutrition and lung host defenses: implications for the pathogenesis and prevention of pneumonia. [DOI] [Google Scholar]
- 21.Iorember F.M. Malnutrition in chronic kidney disease. Front Pediatr. 2018;6:161. doi: 10.3389/fped.2018.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Waitzberg D., Caiaffa W., Correia M. Hospital malnutrition: the Brazilian National Survey (IBRANUTRI): a study of 4000 patients. Nutrition. 2001;17:573–580. doi: 10.1016/s0899-9007(01)00573-1. [DOI] [PubMed] [Google Scholar]
- 23.Naber T., Schermer T., de Bree A., Nusteling K., Eggink L., Kruimel J., et al. Prevalence of malnutrition in nonsurgical hospitalized patients and its association with disease complications. Am J Clin Nutr. 1997;66:1232–1239. doi: 10.1093/ajcn/66.5.1232. [DOI] [PubMed] [Google Scholar]
- 24.The Global Nutrition Report’s Independent Expert Group . 2020. The 2020 global nutrition report in the context of COVID-19.https://globalnutritionreport.org/reports/2020-global-nutrition-report/2020-global-nutrition-report-context-covid-19/ Accessed at. [Google Scholar]