Abstract
The COVID-19 pandemic has resulted in substantial morbidity and mortality and challenged public health agencies and healthcare systems worldwide. In the U.S., physical distancing orders and other restrictions have had severe economic and societal consequences. Populations already vulnerable in the United States have experienced worse COVID-19 health outcomes. The World Health Organization has made recommendations to engage at risk populations and communicate accurate information about risk and prevention; to conduct contract tracing; and to support those affected by COVID-19. This Commentary highlights the ways in which an existing and cost-effective, but underutilized workforce, community health workers and non-clinical patient navigators, should be deployed to address the COVID-19 pandemic. Community health workers and non-clinical patient navigators have skills in community engagement and health communication and are able to gain the trust of vulnerable communities. Furthermore, many community health workers and non-clinical patient navigators have skills in assisting community members with meeting basic needs and with navigating public health and healthcare systems. Members of this workforce are more than prepared to conduct contact tracing. State, local, tribal, and territorial public health agencies and healthcare systems should be collaborating with national, state, and local organizations that represent and employ CHWs/non-clinical patient navigators to determine how to better mobilize this workforce to address the COVID-19 pandemic. Furthermore, Congress, the Centers for Medicare & Medicaid Services (CMS), and individual states need to adopt policies to sustainably fund their critically needed services in the long term.
Keywords: Contact tracing, Health education, Health communication, Health disparities, Coronavirus, Health policy
The novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes coronavirus disease 2019 (COVID-19) and has spread rapidly worldwide. In the U.S., the COVID-19 pandemic has resulted in serious societal and economic consequences, especially in communities of color, communities with low incomes, and non-U.S. born communities. Early statistics point to COVID-19 disparities in the US, with higher incidence, rates of hospitalization, and mortality among African Americans, Native Americans, and Latinx populations (Centers for Disease Control and Prevention, 2020; Thakur et al., 2020; Webb Hooper et al., 2020). Reasons for these disparities are complex, but may be related to discrimination, longstanding societal inequities, higher rates of comorbidities, and difficulties accessing healthcare, obtaining information, and physical distancing (Centers for Disease Control and Prevention, 2020; Thakur et al., 2020; Webb Hooper et al., 2020).
The World Health Organization (WHO) is facilitating a multi-level response to the pandemic. The WHO recommends authorities engage with all affected and at-risk individuals through participatory two-way communication. In the U.S., state, tribal, and local governments have been scaling up a workforce to find and test, isolate, and care for individuals diagnosed with COVID-19, as well as identify, trace, quarantine, and support contacts. Effective contact tracing is urgently needed because many people infected with COVID-19 are asymptomatic or pre-symptomatic and may infect others without realizing it. Furthermore, healthcare systems providing clinical care to those affected by COVID-19 need additional support to manage these patients while also managing patients with other conditions.
Community health workers (CHWs) and non-clinical patient navigators (NPNs) are critical to the COVID-19 pandemic response. Implemented in many settings globally (Wells and Gordon, 2020), CHWs are defined as “frontline public health workers who are trusted members of and/or have an unusually close understanding of the community served.” CHWs “serve as a liaison/link/intermediary between health/social services and the community to facilitate access to services” and “build individual and community capacity by increasing health knowledge and self-sufficiency”(American Public Health Association, 2014). CHWs use a variety of job titles, such as promotor(a), lay health advisor, and outreach worker. A related occupation, patient navigators provide barrier-focused interventions targeting a defined set of health services required to complete an episode of healthcare. Multiple patient navigation staffing models are being implemented in the U.S., including professional (i.e., nurse) and non-clinical models (i.e., layperson, CHW), with no known differences in their efficacy. In May 2019, an estimated 117,100 CHWs were employed in urban, rural, and tribal areas of the United States (Bureau of Labor Statistics U.S. Department of Labor, 2020a, Bureau of Labor Statistics U.S. Department of Labor, 2020b, Bureau of Labor Statistics U.S. Department of Labor, 2020c), but this may underestimate the CHW workforce given that one-third of CHWs are volunteers (U.S. Department of Health and Human Services Heath Resources and Services Administration Bureau of Health Professions, 2007).
Often deployed to reduce health disparities, CHWs/NPNs have a flexible scope of practice that includes providing culturally appropriate health education and information; cultural mediation among individuals, communities, and health and social service systems; care coordination, case management, and systems navigation; providing some direct clinical services (e.g., blood pressure measurements), implementing individual and community assessments; and conducting outreach. CHW interventions are effective in improving receipt of breast, cervical, and colorectal cancer screening (Community Preventive Services Task Force (CPSTF), 2020); retention in HIV care (Mwai et al., 2013); receipt of pediatric immunizations (Lewin et al., 2010); initiation of breastfeeding (Lewin et al., 2010); exclusive breastfeeding (Lewin et al., 2010); tuberculosis cure rates (Lewin et al., 2010); and control of blood pressure, blood glucose, and cholesterol (Community Preventive Services Task Force (CPSTF), 2020).
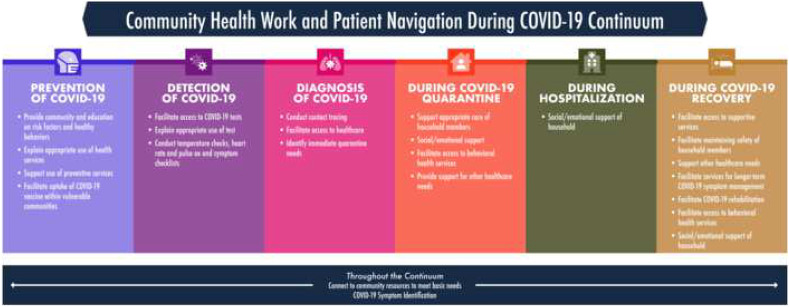
CHWs/NPNs have flexible and transferable skills critically needed across the COVID-19 disease continuum, from preventing SARS-CoV-2 virus spread to reducing the burden of those diagnosed with COVID-19 and living with its health, social, and economic impacts (Fig. 1 ). First, CHWs/NPNs can reach communities most at risk for COVID-19. CHWs/NPNs are well poised to work effectively with diverse communities due to their racial/ethnic and linguistic congruence. CHWs/NPNs understand vulnerable communities, networks within the communities, and local systems. This workforce acts as a cultural liaison between ethnic communities and the larger healthcare and public health systems. Therefore, CHWs/NPNs should be engaged by public health and health system decision makers to determine how to best adapt global recommendations and communications for local contexts.
Fig. 1.
Community health work and patient navigation during COVID-19 continuum.
Second, the nation's public health organizations already have experience with employing CHWs/NPNs. This will facilitate the hiring of new CHWs/NPNs or the shifting of COVID-19 tasks to established CHW/NPN employees or volunteers. Using their own COVID-19 data, each community or organization (i.e., towns, tribal communities, health clinics) that employs CHWs/NPNs can prioritize services for populations they deem most vulnerable for COVID-19. The services provided by CHWs/NPNs may change over time as the pandemic continues (i.e., contact tracing, promoting COVID-19 vaccination uptake and completion).
Third, CHWs/NPNs excel at providing culturally appropriate health education. People in the U.S. have reported obtaining COVID-19 information from various sources, such as social media, news media, messaging applications, websites, podcasts, the Trump administration, Wikipedia, late night comedy shows, friends, and family (Baum et al., 2020). Those who receive their news from social media, messaging applications, and Wikipedia are at higher risk of believing misinformation and disinformation statements (Baum et al., 2020; Jamieson and Albarracín, 2020). CHWs and NPNs have been trained in health communication approaches and are well poised to lead participatory community engagement interventions recommended by the WHO, which aim to provide accurate information on risks of COVID-19 and actions people can take to reduce their risk of it.
Fourth, public health officials should work closely with CHW/patient navigator associations to scale up the existing and previously trained patient navigation and CHW workforce to find and test, isolate, and care for individuals diagnosed with COVID-19. Across the country, public health agencies have been working to implement National Association of County and City Health Officials (NACCHO) and WHO recommendations to conduct contact tracing of individuals exposed to the virus. However, contact tracing has been difficult to implement effectively for multiple reasons, including a lack of COVID-19 testing, delays providing COVID-19 testing results, and surges in COVID-19 cases.
Another reason that public health agencies may be experiencing difficulties with implementing contact testing is their reliance on personnel who have minimal experience with health care delivery, including volunteers, students, and reassigned government workers (Simmons-Duffin, 2020b). Research indicates CHWs have improved the outcomes of tuberculosis contact tracing (Ospina et al., 2012). In fact, NACCHO explicitly recommends that CHWs perform contact tracing and has suggested at least $3.7 billion in emergency supplement funding be provided to public health agencies to support a workforce of 100,000 contact tracers (National Association of County and City Health Officials (NACCHO), 2020). As of October 2020, 53,116 COVID-19 contact tracers were working nationwide, with 44 states having inadequate personnel (Simmons-Duffin, 2020a). Contact tracing requires building trust with a person who has tested positive for COVID-19 to obtain information on those potentially exposed to SARS-CoV-2 and assisting them in quarantining as required by public health agencies. However, a July 2020 survey found that less than half of U.S. adults surveyed were willing to follow all steps of contact tracing: speaking with public health officials, sharing data regarding where they had been and with whom they had close contact, and quarantining for 14 days (McClain and Rainie, 2020). For communities that historically experience health, social, and economic disparities, reducing distrust of public systems to improve health of communities is a key CHW/NPN function. CHW/NPNs have culturally competent assessment and intervention skills, often including motivational enhancement strategies, to assist individuals in accessing services and changing behaviors. Contact tracers should also identify and assist cases and contacts with basic needs, a common job responsibility of CHWs/NPNs. Meeting the basic needs of each affected individual and household is critical to support adherence to quarantine recommendations. To manage the impact of the disease, CHWs/NPNs can also provide needed support to those diagnosed with COVID-19.
Finally, a 2011 systematic review indicates that CHW interventions were promising in increasing childhood vaccination (Helzlsouer et al., 2016). As CHWs and NPNs are trusted community members, they may be instrumental in increasing uptake of the COVID-19 vaccines and addressing COVID-19 vaccination hesitancy.
While there are many reasons to increase and redirect the CHW and navigator workforce to meet the nation's needs with regard to the COVID-19 pandemic, there are challenges to doing so. The most critical challenge is the financing of this workforce. CHWs and non-clinical patient navigators are funded in a number of ways, including through healthcare system operational costs; private foundations; federal, state, and local grants; managed care models; and fee-for-service models. Continuing federal support for pandemic response could fund the expansion of CHW/NPN efforts. States can also fund this workforce through Medicaid using a number of different approaches (Albritton, 2016). For example, the Centers for Medicare and Medicaid Services (CMS) allow non-licensed practitioners, including CHWs, to deliver preventive care. States can also pass legislation and obtain an amendment to their state Medicaid plan. State Medicaid plan amendments enable the state to change their Medicaid policies or operational procedures and could be used for reimbursement of a broader range of services provided by CHWs. States are also allowed to improve their Medicaid program through Section 1115 of the Social Security Act. Thus, states could obtain a “Section 1115 waiver” to provide services not typically covered by Medicaid (including CHW services) as part of an experimental, demonstration, or pilot program. Finally, states could revise their contracts with managed care organizations (e.g., for Medicaid) to promote uptake of CHW services (Albritton, 2016). While research has found that CHW and NPN interventions are cost effective for improving certain health outcomes, such as preventing cardiovascular disease and type 2 diabetes, and managing type 2 diabetes (Jacob et al., 2019), there is no known research examining the cost or cost-effectiveness of CHW/NPN interventions for COVID care. Another challenge is that states, communities, and health care organizations that shift existing CHWs/NPNs to focus on pandemic response may have other patient needs which go unmet. Furthermore, shifting efforts of existing CHWs/NPNs to COVID-19 could increase stigmatization and reduce trust in these workers (Bhaumik et al., 2020). Finally, effectiveness of CHW and NPN responses to the COVID-19 pandemic may be limited if other pandemic efforts, such as a federal plan or robust, timely COVID-19 testing, are lacking.
Given the difficulty in controlling the spread of SARS-CoV-2 and the deleterious health, social, and economic effects of the pandemic, public health agencies and healthcare systems should be collaborating with organizations that represent and employ CHWs/NPNs to determine how to increase and shift the CHW and NPN workforce to address the COVID-19 pandemic. Funding for this workforce is needed from all levels of government, health care organizations, and from private foundations and individual philanthropists. Now is the time to implement and sustainably fund CHWs/NPNs for the COVID-19 response.
Funding
Dr. Kristen Wells' efforts were supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health, in the United States of America, under award number U54MD012397. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of Competing Interest
None.
References
- Albritton E. 2016. How states can fund community health workers through Medicaid to improve people’s health, decrease costs, and reduce disparities. (Families USA) [Google Scholar]
- American Public Health Association Support for community health worker leadership in determining workforce standards for training and credentialing. Policy number. 2014;201414 [Google Scholar]
- Baum M.A., Ognyanova K., Chwe H., Quintana A., Perlis R.H., Lazer D., Druckman J., Santillana M., Lin J., et al. 2020. The State of the Nation: A 50-State COVID-19 Survey Report #14: Misinformation and Vaccine Acceptance. [Google Scholar]
- Bhaumik S., Moola S., Tyagi J., Nambiar D., Kakoti M. Community health workers for pandemic response: a rapid evidence synthesis. BMJ Glob. Health. 2020;5 doi: 10.1136/bmjgh-2020-002769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Labor Statistics U.S. Department of Labor . Health Education Specialists; 2020. Occupational Employment and Wages, May 2019: 21–1091. [Google Scholar]
- Bureau of Labor Statistics U.S. Department of Labor . 2020. Occupational Employment and Wages, May 2019: 21–1094 Community Health Workers. [Google Scholar]
- Bureau of Labor Statistics U.S. Department of Labor . Health Educators and Community Health Workers; 2020. Occupational Outlook Handbook. [Google Scholar]
- Centers for Disease Control and Prevention . 2020. COVID-19 in Racial and Ethnic Minority Groups. [Google Scholar]
- Community Preventive Services Task Force (CPSTF) 2020. The community guide. [Google Scholar]
- Helzlsouer K.J., Appling S.E., Scarvalone S., Manocheh S., MacDonald R., Gallicchio L., Henninger D., Varanasi A.P. Development and evaluation of a technology-enhanced interdisciplinary navigation program for low-income breast cancer patients. J. Oncol. Navigation & Survivorship. 2016;7:10–18. [Google Scholar]
- Jacob V., Chattopadhyay S.K., Hopkins D.P., Reynolds J.A., Xiong K.Z., Jones C.D., Rodriguez B.J., Proia K.K., Pronk N.P., et al. Economics of community health workers for chronic disease: findings from community guide systematic reviews. Am. J. Prev. Med. 2019;56:e95–e106. doi: 10.1016/j.amepre.2018.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamieson K.H., Albarracín D. The Harvard Kennedy School (HKS) Misinformation Review. 2020. The relation between media consumption and misinformation at the outset of the SARS-CoV-2 pandemic in the US. [Google Scholar]
- Lewin, S., Munabi-Babigumira, S., Glenton, C., Daniels, K., Bosch-Capblanch, X., van Wyk, B.E., Odgaard-Jensen, J., Johansen, M., Aja, G.N., et al., 2010. Lay health workers in primary and community health care for maternal and child health and the management of infectious diseases. Cochrane Database Syst Rev 2010:Cd004015. [DOI] [PMC free article] [PubMed]
- McClain, C., Rainie, L., 2020. The challenges of contact tracing as U.S. battles COVID-19. Pew research center.
- Mwai G.W., Mburu G., Torpey K., Frost P., Ford N., Seeley J. Role and outcomes of community health workers in HIV care in sub-Saharan Africa: a systematic review. J. Int. AIDS Soc. 2013;16:18586. doi: 10.7448/IAS.16.1.18586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of County & City Health Officials (NACCHO) National Association of County & City Health Officials (NACCHO); 2020. NACCHO position statement: building COVID-19 contact tracing capacity in health departments to support reopening American society safely. [Google Scholar]
- Ospina J.E., Orcau À., Millet J.-P., Sánchez F., Casals M., Caylà J.A. Community health workers improve contact tracing among immigrants with tuberculosis in Barcelona. BMC Public Health. 2012;12:158. doi: 10.1186/1471-2458-12-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmons-Duffin S. NPR; 2020. COVID-19 Contact Tracing Workforce Barely ‘Inching Up’ As Cases Surge.https://www.npr.org/sections/health-shots/2020/06/18/879787448/as-states-reopen-do-they-have-the-workforce-they-need-to-stop-coronavirus-outbre [Google Scholar]
- Simmons-Duffin S. As states reopen, do they have the workforce they need to stop coronavirus outbreaks? NPR. 2020 [Google Scholar]
- Thakur N., Lovinsky-Desir S., Bime C., Wisnivesky J.P., Celedón J.C. The structural and social determinants of the racial/ethnic disparities in the U.S. COVID-19 pandemic. What’s our role? Am. J. Respir. Crit. Care Med. 2020;202:943–949. doi: 10.1164/rccm.202005-1523PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services Heath Resources and Services Administration Bureau of Health Professions . 2007. Community Health Worker National Workforce Study. [Google Scholar]
- Webb Hooper M., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. JAMA. 2020;323:2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells K.J., Gordon J.R. In: The Wiley Encyclopedia of Health Psychology. Gulliver S.B., Cohen L.M., editors. 2020. Patient navigation/community health workers; pp. 91–100. [Google Scholar]