Abstract
Some psychiatric hospitals have instituted mandatory COVID-19 testing for all patients referred for admission. Others have permitted patients to decline testing. Little is known about the rate of COVID-19 infection in acute psychiatric inpatients. Characterizing the proportion of infected patients who have an asymptomatic presentation will help inform policy regarding universal mandatory versus symptom-based or opt-out testing protocols. We determined the COVID-19 infection rate and frequency of asymptomatic presentation in 683 consecutively admitted patients during the surge in the New York City region between April 3rd, 2020 and June 8th, 2020. Among these psychiatric inpatients, there was a 9.8 % overall rate of COVID-19 infection. Of the COVID-19 infected patients, approximately 76.1 % (51/67) either had no COVID-19 symptoms or could not offer reliable history of symptoms at the time of admission. Had they not been identified by testing and triaged to a COVID-19 positive unit, they could have infected others, leading to institutional outbreak. These findings provide justification for psychiatric facilities to maintain universal mandatory testing policies, at least until community infection rates fall and remain at very low levels.
Keywords: COVID-19 testing, COVID-19 epidemiology, Psychiatric hospitals, COVID-19 ethics
1. Introduction
Patients with severe mental illness and substance-use disorders may have limited access to resources in the community, difficulty accessing or adhering to public health recommendations, and reside in population-dense dwellings such as shelters in higher rates than the general population. All of these factors potentiate the risk of contracting COVID-19 (Mosites et al., 2020; Shinn and Viron, 2020). Recent work with large population-level data confirms that populations with severe mental illness are at elevated risk of COVID-19 infection (Taquet et al., 2021; Wang et al., 2021a, 2021b). The confined environment of inpatient psychiatric facilities may further increase infection risk because patients share communal dining areas, bathrooms, and other common areas with limited space for social distancing. Significant institutional outbreaks have occurred in psychiatric facilities during the first wave of the COVID-19 pandemic, undermining the fundamental mission of psychiatric units or hospitals to provide a safe environment for patients to recover (Ji et al., 2020; Shao et al., 2020).
Given COVID-19 infection risk, some institutions have required nasopharyngeal swab testing for all psychiatric inpatients (Brody et al., 2020; Zhang et al., 2020). Mandatory universal testing provides the highest assurance that newly referred patients are unlikely to introduce COVID-19 and can be ethically grounded in a justice based argument that acute psychiatric inpatients, like those hospitalized for general medical problems, deserve access to hospital settings with the lowest possible risk of exposure to COVID-19 (Gillon, 1994). However, mandatory universal testing also comes at the cost of delays associated with testing and stresses available laboratory resources. The most substantial drawback of mandatory universal testing for COVID-19 may be the ethical tension that arises when patients refuse testing (Morris, 2020; Russ et al., 2020).
Because of these challenges, some psychiatric hospitals have adopted symptom-triggered or optional testing, which places a lower burden on COVID-19 testing resources and preserves the autonomy of patients who do not wish to be tested (Shahani et al., 2020). Information about the underlying rate of COVID-19 infection in acute psychiatric populations during COVID-19 community surges is limited. Characterizing the proportion of infected patients who have an asymptomatic presentation will help inform policy regarding universal mandatory versus symptom-based or opt-out testing protocols.
Here, we report the rate of COVID-19 infection and asymptomatic presentation in patients referred for admission to a large, free-standing New York psychiatric hospital during the first surge of the pandemic in the spring of 2020. In doing so, we highlight the challenges associated with having a large percentage of psychiatric patients who test positive for COVD-19 present without symptoms. We then contrast the rate of COVID-19 infection in our acute psychiatric population with the percent positive rate in the surrounding New York region in order to contextualize our findings with the timing and severity of the COVID-19 outbreak in the surrounding region.
2. Methods
On April 3, 2020 the Westchester Behavioral Health Center of New York Presbyterian Hospital adopted mandatory COVID-19 testing for all patients referred for inpatient psychiatric admission. Patients referred from Comprehensive Psychiatric Emergency Programs, Medical Emergency Departments, medical/surgical floors, or children's hospitals within the New York Presbyterian health system underwent nasopharyngeal swab SARS-CoV-2 Polymerase Chain Reaction testing (PCR) testing at those locations prior to transfer to our facility.
External hospitals referring patients for psychiatric admission were also required to provide results of a patient's PCR testing in the 72-hours prior to the planned admission. Patients referred directly from home or an ambulatory or inpatient setting where testing was not available were placed in a holding area and underwent PCR testing at the time of arrival to our site. COVID-19 positive patients with oxygen saturation below 94% on room air, shortness of breath or chest pain at rest, or other unstable medical illness were not accepted for psychiatric admission until they were medically stabilized (a full description of our medical review process prior to admission is available in Supplement 1). When patients refused testing at an outside facility or on admission, they were quarantined with contact and droplet isolation precautions and engaged therapeutically until they accepted PCR testing. All patients described in this report were eventually tested. A full description of our testing and triage protocol is available elsewhere (Brody et al., 2020).
All external results were reviewed by a medical nurse practitioner and recorded in a pre-admission note. Patients were then triaged to COVID-19 positive or COVID-19 negative units with different protocols for medical monitoring, personal protective equipment use, and isolation requirements. “Indeterminate” results were considered positive in accordance with laboratory guidance, and these patients were triaged to a COVID-19 positive unit
(Brody et al., 2020; Kanellopoulos et al., 2021).
For this report we reviewed the medical records of 683 consecutive patients who were accepted for psychiatric admission between April 3, 2020, when our health system adopted a mandatory testing policy, and June 8, 2020 when New York State entered Phase 1 reopening. These dates correspond to peak local COVID-19 transmission rates in our region (New York Forward, n.d.).
We collected the results of PCR testing for all patients in our sample. For all patients whose results were “positive" or " indeterminate," we then sub-classified patients as “symptomatic” or “asymptomatic” based on guidance of Centers for Disease Control and Prevention characterizing the symptoms of COVID-19 (Centers for Disease Control and Prevention, n.d.). Symptom assessment was based on patient-reported history of symptoms and physical exam conducted by a medical nurse practitioner at the time of admission. All physical exams included screening patients for the presence or absence of constitutional, ophthalmologic, otolaryngologic, cardiovascular, respiratory, gastrointestinal, endocrine, genitourinary, integumentary, hematologic/lymphatic, immunologic, musculoskeletal, neurologic, and allergic symptoms and signs. Patients with temperatures 100.0 degrees F or greater were defined as febrile and therefore symptomatic. Patients who were too psychiatrically impaired to cooperate with the admission history or physical exam were classified as "poor historians."
Patients who were COVID-19 positive at admission had a repeat nasopharyngeal-swab PCR test 14 days after their initial positive result if they were clinically improving, afebrile, and had not used antipyretic medication for 72 hours. If the second test was negative, it was repeated the following day for confirmation. On the basis of these results, we characterized the hospital courses of the COVID-19 positive patients as “infection resolved during hospitalization” (if two subsequent tests were negative); “patient discharged COVID-19 positive” (if they were discharged prior to the 14-day time frame or their last test was positive); or “required medical hospitalization” (if they became medically unstable and were transferred to an inpatient medical setting during the course of psychiatric admission). Four patients were discharged after their second COVID-19 test resulted negative but before a third confirmatory swab was obtained. For the purpose of this report, they were also characterized as “infection resolved during hospitalization.”
We used IBM SPSS version 26 to produce statistics that characterize our sample. Chi-squared tests were conducted to compare the COVID-19 positive and COVID-19 negative samples with respect to categorical demographic characteristics including gender, referral source, and insurance status. An independent samples Mann-Whitney U test was used to compare age between the COVID-19 positive and COVID-19 negative samples. Finally, we reported the weekly rate of COVID-19 infection in our sample referred for psychiatric admission and the percent positive rate in the greater New York region using data from the New York City Department of Health (New York Forward, n.d.).
3. Results
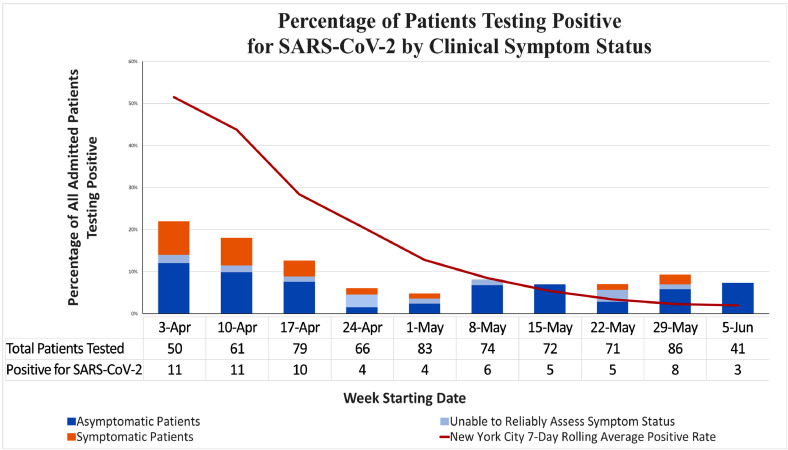
Among 683 patients in our sample, 9.8% (67/683) were identified as having a positive (or indeterminate) SARS-COV-2 nasopharyngeal swab PCR test result. Of the infected patients, 23.9% (16/67) had COVID-19 symptoms at the time of admission either by self-report or clinician evaluation. In contrast, 61.2% (41/67) were asymptomatic;14.9% (10/67) could not offer reliable history of COVID-19 related symptoms due to severe psychopathology. In total, symptoms of COVID-19 were absent or could not be assessed for 76.1% (51/67) of COVID-19 positive patients admitted during this two-month period of peak local COVID-19 transmission in the New York City region (Fig. 1 ).
Fig. 1.
Percentage of patients testing positive for SARS-CoV-2 by clinical symptom status.
During the study time period, our samples highest rate of COVID-19 infection (22%) occurred during the week after we initiated mandatory universal testing (April 3rd). This infection rate subsequently declined and leveled off at 7.5%-6.8% (May 8th-June 5th). The rate of decline in our sample was slower than the percent positive rate in the greater New York area. Complete infection rates for our sample and percent positive rates in the New York area are presented in Fig. 1.
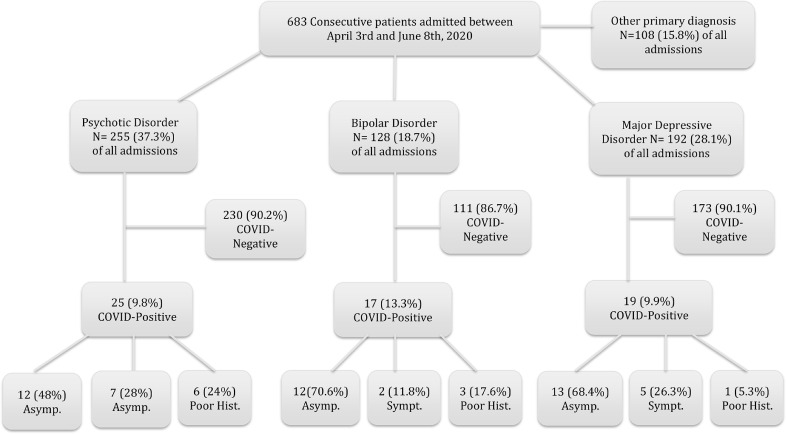
There were no significant differences between the COVID 19-positive and COVID 19-negative cohort in age, gender, or referral source (p > .05, Table 1 ). In a 4-way comparison between Medicaid, Medicare, commercial insurance, and uninsured, the COVID-19 positive cohort was more likely to have Medicaid as their insurance provider (p=0.001). Notably, 13.3% (17/128) of patients with Bipolar Disorder were COVID-19 positive, whereas 9.9% (19/192) of patients with Major Depressive Disorder and 9.8% (25/255) of patients with Psychosis were COVID-19 positive (Fig. 2 ). There was no statistically significant difference in the distribution of COVID-19 positive cases among the three psychiatric diagnostic categories. However, our sample was insufficient for detecting small differences in COVID-19 positive cases across diagnostic categories. Among COVID-19 positive cases, 28% (7/25) of those with a primary psychotic disorder had symptoms related to COVID-19 infection, whereas 11.8% (2/17) of patients with Bipolar Disorder and 26.3% (5/19) of patients with Major Depressive Disorder had COVID-19 symptoms (Fig. 2). These differences were not statistically significant but our sample was too small to detect differences in distribution of symptomatic COVID-19 cases across the major psychiatric diagnoses.
Table 1.
Clinical and demographic characteristics of 683 consecutively admitted inpatients participating in universal COVID screening from April 3rd- June 8th, 2020
| Total (N=683) | COVID-19 positive (N=67) | COVID-19 negative (N=616) | |
|---|---|---|---|
| AGE in YEARS Mean (SD)/Range | 36.9 (16.6)/13-88 | 36.8 (14.8)/13-73 | 36.7 (16.8)/13-88 |
| GENDER | N (%) | N (%) | N (%) |
| Female | 325 (46.6) | 26 (38.8) | 299 (48.5) |
| Male | 353 (51.7) | 41 (61.2) | 312 (50.6) |
| Trans or non-binary | 5 (0.7) | 0 (0) | 5 (0.8) |
| PRIMARY ADMISSION DIAGNOSIS | N (%) | N (%) | N (%) |
| Psychosis | 255 (37.3) | 25 (37.3) | 230 (37.3) |
| Bipolar Disorder | 128 (18.7) | 17 (25.4) | 111 (18) |
| Major Depressive Disorder | 192 (28.1) | 19 (28.4) | 173 (28.1) |
| Other Mood Disorder | 57 (8.4) | 2 (3) | 55 (8.9) |
| Substance Use Disorders | 20 (2.9) | 2 (3) | 18 (2.9) |
| Eating Disorders | 29 (4.3) | 2 (3) | 27 (4.4) |
| Other | 2 (0.3) | 0 (0) | 2 (0.3) |
| PRIMARY INSURANCE | N (%) | N (%) | N (%) |
| Commercial | 249 (36.5) | 14 (20.9) | 235 (38.1) |
| Medicare | 100 (14.6) | 7 (10.4) | 93 (15.1) |
| Medicaid* | 250 (36.6) | 39 (58.2) | 211 (34.3) |
| Uninsured | 84 (12.3) | 7 (10.4) | 77 (12.5) |
| REFERRAL SOURCE | N (%) | N (%) | N (%) |
| CPEP | 368 (53.9) | 41 (61.2) | 327 (53.1) |
| Medical ER/Hospital | 204 (29.9) | 22 (32.8) | 182 (29.5) |
| Pediatric ER/Hospital | 45 (6.6) | 2 (3) | 43 (7) |
| Direct Community Admission | 57 (8.3) | 2 (3) | 55 (8.9) |
| Other Psychiatric Facility | 9 (1.3) | 0 (0) | 9 (1.5) |
| % = percent of total N within column |
* Indicates statistically significant difference (Chi Square=15.5, p<0.001); Medicaid insured patients were more likely than patients with other coverage or no insurance coverage to be COVID-19 positive.+
Fig. 2.
Psychiatric diagnosis, COVID-19 infection status, and presentation of COVID-19 symptoms.
Of the 67 patients who were COVID-19 positive at admission, 38 patients (56.7%) remained COVID-19 positive at the time of discharge. Twenty-eight patients (41.8%) had COVID-19 infection resolution during their hospitalization. One patient, who had a diagnosis of Dementia, became medically unstable with hypoxia and was transferred to an inpatient medical facility. He was stabilized, returned to our facility, and subsequently discharged home.
4. Discussion
The principal finding of this study is that 9.8% of patients admitted to the inpatient service of a psychiatric hospital in the New York metropolitan area during the first pandemic surge were COVID-19 positive. Of the infected patients, approximately 23.9% had COVID-19 symptoms at the time of admission, 14.9% were unable to offer a reliable history of COVID-19 symptoms, and 61.2% were asymptomatic. The infection rate of these patients did not recede as rapidly as the COVID-19 infection rate in the same community (Fig. 1). To our knowledge, this report is the largest to date to describe the rate of COVID-19 infection among patients referred for psychiatric admission during the first surge, a critical period in this pandemic.
We have been able to calculate the rate of COVID-19 infection because our hospital tested all psychiatric patients referred for admission, regardless of symptom status or known COVID-19 exposure. In the New York metropolitan area, COVID-19 testing was scarce in April of 2020 and was reserved only for individuals who exhibited COVID-19 symptoms (New York City Department of Health, n.d.). Testing availability increased dramatically over the time period described, which subsequently prompted changes in testing recommendations. The policy restrictions limiting testing to only the highest risk individuals at least partially account for very high percent rates in the community at the beginning of this time period.
In our sample, individuals with Bipolar Disorder represented the largest proportion (13.3%) of admitted COVID-19-positive patients. COVID-19 positive patients admitted due to Major Depression (9.9%) and Psychosis (9.8%) had similar proportions within their diagnostic category. This study was not powered to detect small differences in risk of COVID-19 infection; in future work we wish to examine whether individuals with specific psychiatric diagnoses present for admission with higher rates of COVID-19 infection.
A substantial majority of the COVID-19-positive patients (61.2%) were asymptomatic by clinical assessment and 14.9% were unable to offer a reliable history of COVID-19 symptoms. We speculate that the high prevalence of asymptomatic infection in our sample reflects the wide spectrum of COVID-19 illness presentation. It is also a likely effect of our medical-review process, which excluded more severely-ill COVID-19 patients until they were medically stable. It is important to highlight that 14.9% of our COVID-19 positive patients were poor historians or could not be assessed for COVID-19 symptoms due to their psychiatric acuity. This finding reflects the severity of disorganization or lack of cooperation that is common in this patient population. In total, 76.1% of our patients were either asymptomatic or were not able to be assessed at the time of admission, underscoring the importance of mandatory universal testing.
Despite the expectation of wider vaccine distribution in the foreseeable future, almost one-third of Americans report they will delay vaccination, and 20% are reluctant to receive a COVID-19 vaccine (Rosenbaum, 2021). Further, patients with serious mental illness receive inconsistent preventative care (Druss et al., 2002). The requirement for a two-dose inoculation for both currently-approved vaccines and the unknown duration of efficacy of those vaccines are particularly problematic for patients with severe mental illness, who often face considerable barriers to care. These factors raise the possibility that patients with serious mental illness will remain potential reservoirs and vectors for COVID-19 in the foreseeable future. Taken together, we submit that our findings of slowly declining rates of COVID-19 infection in an acute psychiatric population and the high frequency of asymptomatic presentation present ample justification for psychiatric facilities to maintain universal mandatory testing policies, at least until community infection rates fall and remain at very low levels.
The observation that Medicaid-insured patients were over-represented in the COVID-19 positive cohort is consistent with well-documented reports that economic inequality is associated with increased risk of COVID-19 infection (Liao and de Maio, 2021). Only one of our COVID-19 positive patients medically decompensated during psychiatric admission, which supports with the practice of admitting patients with mild to moderate COVID-19 illness and severe psychiatric illness to psychiatric facilities for their care. The remainder of the COVID-19 positive patients were discharged according to treatment as usual for this population.
The primary strength of our report is the large sample size. The main limitation is that it is based on patients admitted early in the pandemic, when much was still unknown about COVID-19 symptomatology. The percent positive rate in the community should be interpreted in relation to the number of tests performed and the representativeness of the sample being tested. Although we speculate that clinicians will be better able to recognize subtle signs or symptoms of COVID-19 infection during subsequent waves or low-level community surges, our findings highlight the importance of universal testing in inpatient psychiatric facilities. A final limitation inherent to the retrospective nature of this report is that we do not have consistent information about the racial or ethnic background of our patient sample, many of whom decline to give this information or are too acutely impaired to participate with the patient registration process on admission.
In sum, approximately 10% of inpatient admissions to a psychiatric hospital of the New York metropolitan area tested COVID-19 positive during the first pandemic surge. Of these, 76.1% were either asymptomatic or were unable to offer a reliable history of COVID-19 symptoms due to severe psychopathology. These findings support the use of universal mandatory testing policies since asymptomatic patients or patients with an unclear symptomatic status may infect the remaining vulnerable psychiatric population. Further work is needed to better characterize the efficacy of universal testing protocols to prevent institutional outbreaks and to monitor the incidence of COVID-19 infection in populations with serious mental illness.
CRediT authorship contribution statement
Benjamin D. Brody: Conceptualization, Data curation, Investigation, Methodology, Project administration, Visualization, Writing - original draft, Writing - review & editing. Zhenzhen Shi: Investigation, Writing - review & editing. Charles Shaffer: Investigation, Visualization, Writing - review & editing. Daniel Eden: Investigation, Writing - review & editing. Katarzyna Wyka: Methodology, Formal analysis, Writing - review & editing. George S. Alexopoulos: Writing - review & editing. Sharon J. Parish: Conceptualization, Writing - review & editing. Dora Kanellopoulos: Conceptualization, Data curation, Formal analysis, Investigation, Project administration, Visualization, Writing - review & editing.
Declaration of Competing Interest
Dr. Alexopoulos served on Advisory Board of Eisai and of Janssen Pharmaceuticals and receives support from P50 MH113838. He also served on the Speakers Bureaus of Allergan, Otsuka, and Takeda-Lundbeck.None of the authors report any grant support, other external funding, or other conflicts of interest.
Footnotes
This research was approved by the Institutional Review Board of Weill Cornell Medical College.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2021.113833.
Appendix. Supplementary materials
References
- Brody B.D., Parish S.J., Kanellopoulos D., Russ M.J. A COVID-19 testing and triage algorithm for psychiatric units: one hospital's response to the New York region's pandemic. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, n.d. symptoms of coronavirus [WWW document]. URL https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html (accessed 12.4.20).
- Druss B.G., Rosenheck R.A., Desai M.M., Perlin J.B. Quality of preventive medical care for patients with mental disorders. Med. Care. 2002;40:129–136. doi: 10.1097/00005650-200202000-00007. [DOI] [PubMed] [Google Scholar]
- Gillon R. Medical ethics: four principles plus attention to scope. BMJ. 1994;309:184. doi: 10.1136/bmj.309.6948.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji, H., Liu, L., Huang, T., Zhu, Y., 2020. Nosocomial infections in psychiatric hospitals during the COVID-19 outbreak. The European journal of psychiatry 34, 177–179. https://doi.org/10.1016/j.ejpsy.2020.04.001. [DOI] [PMC free article] [PubMed]
- Kanellopoulos D., Bueno Castellano C., McGlynn L., Gerber S., Francois D., Rosenblum L., Runge M., Sanchez-Barranco P., Alexopoulos G.S. Implementation of telehealth services for inpatient psychiatric Covid-19 positive patients: a blueprint for adapting the milieu. Gener. Hosp. Psychiatry. 2021 doi: 10.1016/j.genhosppsych.2020.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao T.F., de Maio F. Association of social and economic inequality with coronavirus disease 2019 incidence and mortality across US counties. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.34578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris N.P. Refusing testing during a pandemic. Am. J. Public Health. 2020 doi: 10.2105/AJPH.2020.305810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosites E., Parker E.M., Clarke K.E.N., Gaeta J.M., Baggett T.P., Imbert E., Sankaran M., Scarborough A., Huster K., Hanson M., Gonzales E., Rauch J., Page L., McMichael T.M., Keating R., Marx G.E., Andrews T., Schmit K., Morris S.B., Dowling N.F., Peacock G., Buff A., Jamison C., Marcus R., Rao C.Y., Self J.L., Tobolowsky F., Williams S., Kay M., Bobba N., Cohen S., Fuchs J., Nguyen T., Stoltey J. Assessment of SARS-CoV-2 infection prevalence in homeless shelters — four U.S. cities, March 27–April 15, 2020. MMWR. Morbidity Mortality Weekly Rep. 2020;69:521–522. doi: 10.15585/mmwr.mm6917e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York City Department of Health, n.d. COVID-19 data [www document]. URL https://www1.nyc.gov/site/doh/covid/covid-19-data-trends.page (accessed 1.30.21).
- New York Forward, n.d. percentage positive results by region dashboard [www document]. URL https://forward.ny.gov/percentage-positive-results-region-dashboard (accessed 12.4.20).
- Rosenbaum L. Escaping catch 22 - overcoming vaccine hesitancy. N. Engl. J. Med. 2021 doi: 10.1056/NEJMms2101220. [DOI] [PubMed] [Google Scholar]
- Russ M.J., Sisti D., Wilner P.J. When patients refuse COVID-19 testing, quarantine, and social distancing in inpatient psychiatry: Clinical and ethical challenges. J. Med. Ethics. 2020;46:579–581. doi: 10.1136/medethics-2020-106613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahani L., Glazier S., Ostrosky L., Lane S., Soares J.C. Universal SARS-CoV-2 testing versus symptom based screening and testing in inpatient psychiatric setting. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao Ying, Shao Yang, Fei J.M. Psychiatry hospital management facing COVID-19: from medical staff to patients. Brain, Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinn A.K., Viron M. Perspectives on the COVID-19 pandemic and individuals with serious mental illness. J. Clin. Psychiatry. 2020 doi: 10.4088/JCP.20com13412. [DOI] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q.Q., Kaelber D.C., Xu R., Volkow N.D. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol. Psychiatry. 2021;26:30–39. doi: 10.1038/s41380-020-00880-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q.Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20:124–130. doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang E., LeQuesne E., Fichtel K., Ginsberg D., Frankle W.G. In-patient psychiatry management of COVID-19: rates of asymptomatic infection and on-unit transmission. BJPsych Open. 2020;6:e99. doi: 10.1192/bjo.2020.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.