Abstract
OBJECTIVES
Asymmetric hearing loss is generally defined as a moderate-to-profound hearing loss in the poorer ear and a mild-to-moderate hearing loss in the better ear. Application of a bone conduction hearing aid is one of the possible treatments for the poorer ear in asymmetric hearing loss. However, the device essentially stimulates the contralateral better ear, precluding true binaural hearing. The aim of this paper is to evaluate the application and utility of bone-anchored hearing aids in the treatment of asymmetric hearing loss.
MATERIALS and METHODS
We retrospectively evaluated 215 implanted subjects in our clinic and extracted a series of 27 patients affected by asymmetric hearing loss and treated with bone-anchored hearing aids. All 27 subjects had a mixed hearing loss after middle ear surgery. The preoperative and postoperative audiological data of these patients were collected and analyzed.
RESULTS
The audiological tests showed an improvement in the performance of hearing perception of sound and speech in quiet and noise. Moreover, the subjects have positively answered the questionnaires administered to evaluate subjective benefits. All subscales of the abbreviated profile of hearing aid benefit and speech, spatial, and qualities of hearing scale showed a significant improvement with the device.
CONCLUSION
Bone-anchored hearing aids are a suitable treatment for asymmetric hearing loss. When other devices cannot be utilized or are not indicated, the bone conduction devices may allow good audiological results.
Keywords: Bone-anchored hearing aids, asymmetric, hearing loss
INTRODUCTION
Scientific literature reports several definitions of asymmetric hearing loss (AHL) [1]. An interaural asymmetry of 20 dB hearing loss (HL) at two contiguous frequencies or 15 dB HL at any two frequencies from 2–8 kHz seems to be the most robust definition of AHL with a level 3 of evidence [1, 2]. The definition was thought to be for sensorineural deafness, but it can be extended to mixed and conductive forms [3].
AHL causes a poorer quality of life in terms of an inability to benefit from binaural hearing. Binaural listening is essential for understanding speech in noise and complex listening environments [4–6]. Moreover, individuals with hearing asymmetry perform poorly on measures of sound localization [7].
Traditional treatments for patients with AHL include the use of bilateral hearing aids (HAs), use of contralateral routing of signal (CROS) HAs, use of bone-anchored HAs (BAHAs), and use of a cochlear implant (CI) [7]. All these therapeutic approaches can be distinguished in treatments that bypass or stimulate the impaired ear. The CROS HA system conducts the acoustic signals to the better ear; the poorer ear is not rehabilitated, and restoration of binaural hearing is not possible. The BAHA conducts the acoustic signals via bone to the two ears with a transcranial attenuation variable for frequencies. The attenuation is 3–5 dB up to 0.5 kHz, close to 0 dB at frequencies between 0.5 and 1.8 kHz, about 10 dB at 3–5 kHz, and slightly less at the highest frequencies (4 dB at 8 kHz) [8]. Therefore, a BAHA behaves like a CROS HA, stimulating the contralateral better ear and precluding true binaural hearing [7]. The cross-stimulation improves sound awareness for sounds transmitted through the poor ear, but speech understanding in noise and localization benefits are limited, because both require binaural cues [9]. On the contrary, bilateral HAs or bimodal stimulation with CI in the worse ear and HA in the contralateral better ear could provide binaural hearing, stimulating the impaired ear as well [7].
Among these devices, BAHAs seem to be less efficient for treating AHL. The indications for a bone conduction device in AHL are clearly not reported in available literature [5–7, 9, 10]. According to Food and Drug Administration (FDA) indications, BAHAs are utilized for conductive or mixed HL and for single side deafness (SSD) [11]. FDA reports only the characteristics of the ear to treat (type and threshold of HL), and it does not mention if the HL must be bilateral, symmetrical, or not [11]. In fact, BAHAs conduct the sound to the two ears and it should be utilized knowing the condition of both ears. Moreover, the best application for BAHA is bilateral symmetrical conductive HL [12]. Unilateral conductive or mixed HL or SSD do not receive comparable benefits [12]. The benefits are limited by the head shadow effect. Therefore, a question mark remains when we speak about the real use of BAHA for asymmetrical forms.
In this paper, we describe the benefits of BAHA in our patients affected by mixed AHL. Moreover, the main objective of this study is to evaluate the indications and utility of the bone conduction device in mixed AHL.
MATERIALS AND METHODS
This was a retrospective study conducted on a population of patients treated with a BAHA between January 2007 and January 2020 in our hospital. We analyzed all the documents of 215 implanted patients and selected 27 of them suffering from asymmetrical HL in accordance with Gimsing’s definition [2]. Patients who presented bilateral symmetrical HL and SSD were excluded from the study.
All selected patients had bilateral mixed asymmetric HL. The criterion interaural asymmetry of 20 dB hearing level at two contiguous frequencies or 15 dB hearing level at any two frequencies from 2–8 kHz was considered both for air and bone threshold. All patients in our series had previously undergone middle ear surgery (tympanoplasty or other) and were not able to fit HAs. Therefore, BAHA was the only choice to treat HL. All patients were fitted with one BAHA implanted behind the worse ear. Devices utilized were BP110 (3 patients), BAHA 4 (4 patients), BAHA 5 (7 patients), BAHA 5 Superpower (1 patient), PONTO 3 (1 patient), and PONTO 3 Power (11 patients). They were chosen based on the hearing threshold and among the available options in the market at the time of the surgery.
The patients underwent, before and after the implant, a battery of audiological tests including pure-tone audiometry, free field audiometry, and speech perception test (SPT). Speech perception was assessed using an SPT in Italian language both before (without BAHA) and after implantation (with BAHA) in free field and without lip-reading [13]. We evaluated the disyllabic words recognition score using lists of 20 Italian words and the phrases recognition score using lists of 10 Italian phrases at a level of 65 dB. Both words and phrases are phonetically balanced. Testing the open set speech recognition score with background noise, we considered a signal-to-noise ratio +10.
Moreover, the patients were submitted to subjective tests. They filled out the abbreviated profile of hearing aid benefit (APHAB) test and the speech, spatial, and qualities of hearing scale (SSQ) test to know the subjective evaluations of performances of the device.
Statistical Analysis
For the statistical analysis, descriptive statistics, means, and standard deviations (SDs) were performed. Analysis of variance (ANOVA) was evaluated using one-way ANOVA procedure, with p<0.05 chosen for the level of significance.
RESULTS
A total of 15 patients were female and 12 were male, with a mean age of 60.51 years (range, 25–83 years; SD, 15.41).
The mean and SD of air and bone threshold level are shown in Figure 1.
Figure 1.
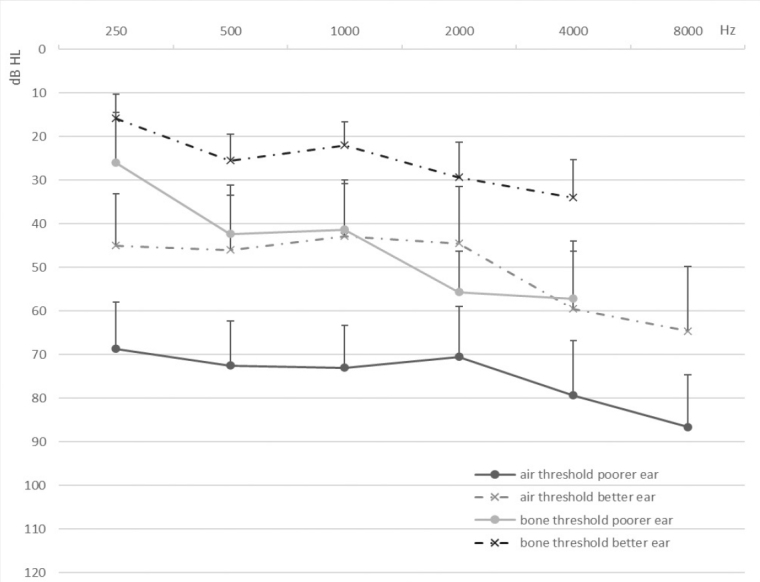
Pure-tone audiometry mean and SD of air and bone conduction threshold of the poorer and better ear.
SD: standard deviation.
The mean and SD of free field audiometry of all the subjects without the device were 56.59±12.48, 57.17±11.26, 49.09±11.3, 50.91±14.61, and 63.80±16.8 at 0.25, 0.5, 1, 2, and 4 kHz, respectively, whereas the mean and SD of the free field audiometry for all the subjects with the device fitted were 41.73±12.96, 37.88±9.61, 29.43±7.91, 32.69±10.98, and 45±15.28 at 0.25, 0.5, 1, 2, and 4 kHz, respectively. The p-value of ANOVA for each frequency was 2.1×10−4, 5.2×10−8, 7.3×10−9, 1.1×10−5, and 2.3×10−4 for 0.25, 0.5, 1, 2, and 4 kHz, respectively (Figure 2). BAHA allows a better threshold at 0.5 and 1 kHz. The mean improvement of hearing threshold (difference between the pure-tone average [PTA] with and without the device) was 19 dB. In addition, the difference between the PTA with and without the device was statistically significant (p=1.6×10−9).
Figure 2.
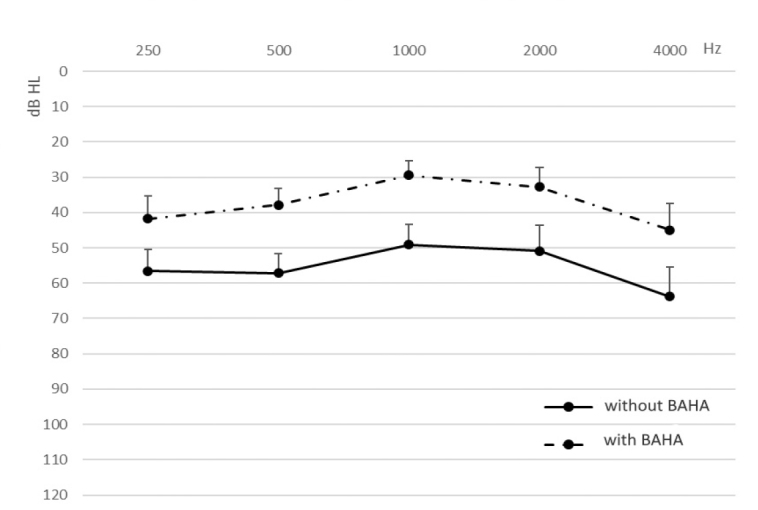
Mean and SD of free field audiometry of all the subjects without and with the device. The difference for each frequency was significant (p<0.05).
SD: standard deviation.
Table 1 shows the results of the SPT with and without the device. The mean and SD of the open set recognition in quiet of the disyllables and sentences without the device were 50.9%±40.43 and 73.75%±31.98, respectively, whereas with the device they were 89%±14 and 80.6%±25.71, respectively. The same data with noise for the disyllables and sentences without the device were 60%±32.5 and 50%±30.33, respectively, whereas with the device they were 84.1%±15.78 and 68.46%±24.09, respectively. The differences were significant for open set recognition of disyllables in quiet and in noise (p=0.002 in quiet and p=0.02 in noise). On the contrary, the differences in recognition of sentences in quiet and noise were not significant.
Table 1.
Mean (%) and SD of the identification in quiet and in noise of the disyllables and sentences without and with the device
| Quiet | Noise | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Without BAHA | With BAHA | Change (p) | Without BAHA | With BAHA | Change (p) | |
| Disyllables | 50.91±40.42 | 89±14 | 0.002 | 60±32.5 | 84.14±15.77 | 0.02 |
|
| ||||||
| Sentences | 73.75±31.98 | 80.6±25.71 | 0.66 | 50±30.33 | 68.46±24.09 | 0.17 |
BAHA: bone-anchored hearing aid; SD: standard deviation.
Differences were significant for recognition of disyllables in quiet and in noise.
The APHAB test is shown in Figure 3. The mean global score was 30.28% and 67.95%, with and without BAHA, respectively. The mean score for single subscales ease of communication (EC), background noise (BN), reverberation (RV), and aversiveness sound (AV) were 22.04, 32.7, 36.11, and 35.8 with the device, respectively, and 56.15, 71.98, 75.73, and 19.4 without the device, respectively. The APHAB questionnaire showed significant improvement in terms of the global score (mean global improvement, 37.7%, p<0.05 [p=3.73×10−7]). The differences for each subscale were 34.11%, 39.28%, 39.62%, and −16.39% for EC, RV, BN, and AV, respectively. Furthermore, statistically significant differences for all subscale scores were recorded (p=4.02×10−5 for EC, p=1.51×10−7 for BN, p=1.45×10−6 for RV, and p=0.02 for AV).
Figure 3.
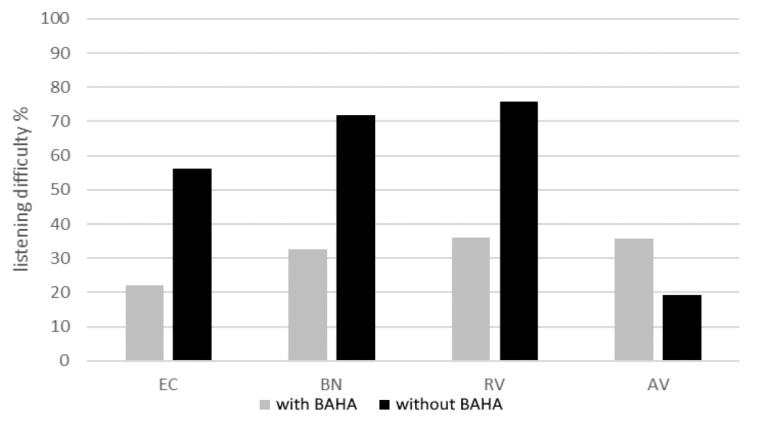
Subgroups of the APHAB test, EC, BN, RV, and AV are shown. Statistically significant differences for all subscale scores were recorded.
APHAB: abbreviated profile of hearing aid benefit; AV: aversiveness sound; BN: background noise; EC: ease of communication; RV: reverberation.
Results of the SSQ test are shown in Table 2. The mean score and SD for each subgroup, speech comprehension, spatial hearing, and sound quality, were 6.2±1.3, 5.7±0.8, and 7.78±1.1 with the device, respectively, and 4.9±1.5, 4.6±1.06, and 6.8±1.06 without the device, respectively. All the subgroups, speech comprehension, spatial hearing, and sound quality, were rated by patients with AHL as significantly better with the BAHA than without it (speech comprehension: p=0.02, spatial hearing: p=0.002, sound quality: p=0.049).
Table 2.
SSQ test
| Without BAHA | With BAHA | Change (p) | |
|---|---|---|---|
| Speech | 4.9 (SD 1.5; range, 3.1–8.1) | 6.2 (SD 1.4; range, 4.1–9.1) | 0.02 |
| Spatial | 4.6 (SD 1.1; range, 3.4–7.3) | 5.7 (SD 0.8; range, 4.7–7.8) | 0.002 |
| Qualities | 6.8 (SD 1.6; range, 3.2–8.7) | 7.8 (SD 1.1; range, 5.1–8.9) | 0.04 |
BAHA: bone-anchored hearing aid; SD: standard deviation; SSQ: speech, spatial, and qualities of hearing scale.
Mean score, SD, and range for each subgroup, speech, spatial, and qualities. The differences with and without the device were significant for each subgroup.
DISCUSSION
This study investigated the performance of BAHAs in a group of implanted patients with mixed AHL. In available literature, AHL has been extensively discussed and the bimodal stimulation with a HA in the better ear and CI in the worst ear seems to be the best choice of treatment, if the worse ear is suitable for CI [3,5,6,7,10,14]. Other options, such as BAHA, are evaluated as less effective and inappropriate for the restoration of binaural hearing [5–7]. But, in accordance with the definition, AHL is a big set that contains a lot of bilateral HL conditions [2]. AHL can be a form close to SSD or a nearly symmetric HL, and it can be a bilateral sensorineural, mixed, or conductive HL [1–3].
CI is indicated as a treatment for AHL in subjects with severe-to-profound HL in the poorer ear and better hearing in the other ear [3,5,6,7,10,14]. Arndt et al.[6] have selected patients affected by AHL, with HL in the better ear of ≤60 dB to 4 kHz and >30 dB in at least one frequency up to 4 kHz and a mean air conduction HL of more than 80 dB for the frequencies 0.5, 1, 2, and 4 kHz in the poorer ear. Analogously, for Thompson et al.,[10] the candidacy criteria for the patients with AHL included a PTA (500, 1,000, and 2,000 Hz) of ≥70 dB hearing level in the worst ear and a PTA between 35 and 55 dB hearing level in the contralateral. In these cases, CI is absolutely the best choice for restoring the quite deaf ear, and alternative treatment options, including conventional HAs, bilateral CROS (BiCROS) HAs, or BAHAs, showed limited benefits [10]. Moreover, CI treatment seems to be significantly superior to the alternative therapy options (CROS/BiCROS HA and BAHA) in speech comprehension in noise and in sound localization [6]. However, not all patients can be treated with a CI because not all patients meet the indications for the CI.
In subjects with an AHL similar to the previous reports, severe-to-profound HL in one and >30 dB to <60 dB up to 4 kHz in the other ear (close to SSD), Monini et al.[15] implanted a BAHA in the poorer ear. The authors underline that BAHAs minimally improve auditory and speech recognition in AHL, with an upgrading in subjective sound perception and a better overall quality of life. The authors concluded that the rehabilitation of some auditory features provided by BAHA in subjects with SSD can be positively extended also to AHL cases, leaving the task of restoring binaural hearing in unilateral deafness to cochlear implantation [15].
We would like to extensively qualify this concept and analyze all the AHL range, not only form close to SSD. In our series, the mean PTA (5.0, 1, and 2 kHz) was 68.7 dB in the worst ear, and only 12 (12/29, 41.2%) subjects had a PTA >70 dB hearing level. In the better ear, the mean PTA was 44.6 dB. On the basis of the audiometric threshold, we did not retain to propose CI for the treatment of the worst ear. Therefore, HAs or BAHAs are left as remaining useful treatments. Moreover, practically all subjects suffered with mixed HL, as an outcome of one or more otological surgical procedures. Many patients of our series previously underwent canal wall down tympanoplasty, and so the option of treatment of HL with a HA (or BiCROS HA) was complex and sometimes ineffective. Many patients tried to use HAs without success. In our series, the hearing threshold was too good for a CI and the conditions of the external and middle ear were unfitting for an HA. Therefore, BAHA was the only choice left and all patients were treated with a BAHA placed behind the worst ear. In our series, BAHA allowed a statistically significant mean improvement of hearing threshold of 19 dB revealed at the free field audiometry (p=1.6×10−9) and a statistically significant improvement of open set recognition in quiet and with BN of the disyllables of 38.1% (p=0.002) and 24.1% (p=0.02), respectively. In our series, the use of BAHA allowed satisfactory hearing and speech perception benefits.
Moreover, the subjective tests have shown good results in AHL series [15]. In our series, the APHAB test demonstrates more EC with the BAHA. Thanks to the device, the bother of RV is lesser, but AV and BN are a little more bothersome. The SSQ questionnaire showed improvement for all subjects affected by AHL. In particular, subjects were able to engage in conversation with a group of people with the device. All patients were able to localize the direction of a barking dog or a vehicle outdoors. Embarrassment for their handicap (HL) was reduced thanks to the BAHA. The SSQ test revealed statistically significant differences for each subscale thanks to the use of the device. These differences are substantial because SSQ included an analysis of the binaural system. Therefore, the SSQ results authorized us to write that the BAHA improves binaural listening in subjects affected by AHL.
The available literature and our results lead us to think that AHL can be treated according to the type and grade of HL of the worst ear (Figure 4) [3,5,6,7,10,14]. Severe-to-profound HL in the poorer ear can be resolved thanks to a CI, but moderate-to-severe HL must be treated with conventional HAs if possible. If the conditions of the external or middle ear are inappropriate for the HA, BAHA remains the only choice. Despite not being the first choice for the treatment of patients with AHL, BAHAs are able to improve the hearing threshold and audiological results in these patients.
Figure 4.
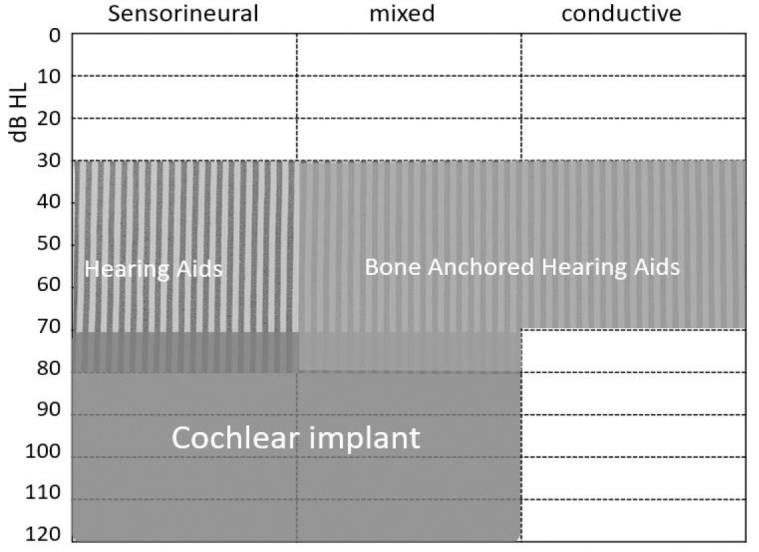
Indications for cochlear implant, hearing aids, and bone-anchored hearing aids based on type and degree of hearing loss of the worst ear. In abscissa is shown the type of hearing loss, in ordinate the hearing level in dB.
AHL can be treated thanks to different devices according to the grade and type of HL of the worst ear. BAHA is a suitable treatment for AHL, particularly when the poorer ear is affected by a mixed HL as an outcome of previous surgical treatments.
CONCLUSION
This study shows that BAHAs provide improvement in hearing performance and subjective benefit compared with the preoperative unaided condition in subjects affected by AHL.
AHL has to be treated with different devices on the basis of the hearing threshold of the poorer ear and the type of HL. For a PTA ≥70 dB hearing level in the poorer ear, the best choice is a bimodal stimulation with a CI in the worst ear and an HA in the better ear. For a PTA <70 dB hearing level in the poorer ear, the bilateral HAs are the best option and, if not suitable, BAHA for the poorer ear remains the only possible treatment.
BAHAs allow good audiological results and have to be considered as a possible treatment of this disease. Subjective questionnaires (APHAB and SSQ) showed an improvement of the performance in several conditions thanks to the BAHA and also described a possible restoration of binaural listening.
MAIN POINTS.
Asymmetric hearing loss is a big set that contains a lot of bilateral hearing loss conditions
Based on hearing thresholds, all the prostheses play a role in the treatment of the asymmetric hearing loss
For a PTA ≥70 dB hearing level in the poorer ear, the best choice is a bimodal stimulation
For a PTA <70 dB hearing level in the poorer ear, the bilateral HAs are the best option and, if not suitable, BAHA represents the second-best choice.
BAHA must be considered as a possible treatment of this disease
Footnotes
Ethics Committee Approval: All procedures performed were in accordance with the ethical standards of our institutional research committee, and in accordance with the tenets of the 1964 Helsinki Declaration and its later amendments, or with comparable ethical standards.
Informed Consent: Informed consent was obtained from all participants included in the study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – L.B.; Design - L.B.; Supervision - F.F.; Resource - L.B.; Materials - R.C.; Data Collection and/or Processing - G.F.; Analysis and/or Interpretation - C.C.; Literature Search - A.M., R.C.; Writing - L.B.; Critical Reviews - F.F., S.B.
Conflict of Interest: The authors have no conflict of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Duracovic N, Valente M, Goebel JA, Wick CC. What defines asymmetric sensorineural hearing loss. Laringoscope. 2019;129:1023–4. doi: 10.1002/lary.27504. [DOI] [PubMed] [Google Scholar]
- 2.Gimsing S. Vestibular schwannoma: when to look for it? J Laryngol Otol. 2010;124:258–64. doi: 10.1017/S0022215109991423. [DOI] [PubMed] [Google Scholar]
- 3.Sanhueza I, Manrique-Huarte R, Calavia D, Huarte A, Manrique M. Hearing impairment and quality of life in adults with asymmetric hearing loss: benefits af bimodal stimulation. J Int Adv Otol. 2019;15:62–9. doi: 10.5152/iao.2019.6224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sladen DP, Carlson ML, Dowling BP, Olund AP, DeJong MD, Breneman A, et al. Cochlear implantation in adults with asymmetric hearing loss: speech recognition in quiet and in noise, and health related quality of life. Otol Neurotol. 2018;39:576–81. doi: 10.1097/MAO.0000000000001763. [DOI] [PubMed] [Google Scholar]
- 5.Ketterer MC, Knopke S, Haussler SM, Hildenbrand T, Becker C, Grabel S, et al. Asymmetric hearing loss and the benefit of cochlear implantation regarding speech perception, tinnitus burden and psychological comorbidities: a prospective follow-up study. Eur Arch Otorhinolaryngol. 2018;275:2683–93. doi: 10.1007/s00405-018-5135-9. [DOI] [PubMed] [Google Scholar]
- 6.Arndt S, Laszig R, Aschendorff A, Hassepass F, Beck R, Wesarg T. Cochlear implant treatment of patients with single-sided deafness or asymmetric hearing loss. HNO. 2017;65:98–108. doi: 10.1007/s00106-016-0297-5. [DOI] [PubMed] [Google Scholar]
- 7.Firszt JB, reeder MR, Holden LK, Dwyer NY Asymmetric Hearing Study Team. Results in Adult Cochlear Implant Recipients with varied asymmetric hearing hearing: a prospective longitudinal study of speech recognition, localization and participant report. Ear Hear. 2018;39:854–62. doi: 10.1097/AUD.0000000000000548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stenfelt S. Transcranial attenuation of bone-conducted sound when stimulation is at the mastoid and at the bone conduction hearing aid position. Otol Neurotol. 2012;33:105–14. doi: 10.1097/MAO.0b013e31823e28ab. [DOI] [PubMed] [Google Scholar]
- 9.Lin LM, Bowditch S, Anderson MJ, May B, Cox KM, Niparko JK. Amplification in the rehabilitation of unilateral deafness: Speech in noise and directional hearing effects with bone-anchored hearing and contralateral routing of signal amplification. Otol Neurotol. 2006;27:172–82. doi: 10.1097/01.mao.0000196421.30275.73. [DOI] [PubMed] [Google Scholar]
- 10.Thompson NJ, Dillon MT, Buss E, Rooth MA, King ER, Bucker AL, et al. Subjective Benefits of Bimodal Listening in Cochlear Implant Recipients with Asymmetric Hearing Loss. Otolaryngol Head Neck Surg. 2020 Mar 17; doi: 10.1177/0194599820911716. 194599820911716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.U.S. Food and Drug Administration (FDA) BAHA BP100. Summary of Safety and Effectiveness. 510(k) No. K090720. Rockville, MD: FDA; Jun 17, 2009. [Accessed June 17, 2010.]. Available at: http://www.accessdata.fda.gov/cdrh_docs/pdf9/K090720.pdf. [Google Scholar]
- 12.Dumper J, Hodgetts B, Liu R, Brandner N. Indications for bone-anchored hearing AIDS: a functional outcomes study. J Otolaryngol Head Neck Surg. 2009;38:96–105. [PubMed] [Google Scholar]
- 13.Burdo S. Protocollo Comune per la Valutazione dei risultati in audiologia Riabilitativa. Florence, Italy: C.R.O; 1997. [Google Scholar]
- 14.van Loon MC, Smits C, Smit CF, Hensen EF, Merkus P. Cochlear Implantation in Adults with Asymmetric Hearing Loss: Benefits of Bimodal Stimulation. Otol Neurotol. 2017;38:e100–e106. doi: 10.1097/MAO.0000000000001418. [DOI] [PubMed] [Google Scholar]
- 15.Monini S, Battilocchi L, Salerno G, Filippi C, Barbara M. Bone conductive implantation in asymmetric hearing loss (AHL) Acta Otolaryngol. 2020;140:651–8. doi: 10.1080/00016489.2020.1752396. [DOI] [PubMed] [Google Scholar]


