Abstract
Background and Objectives
This study examined associations between exposure to the 2003 Severe Acute Respiratory Syndrome (SARS) epidemic and Chinese older adults’ depression and inflammation 8 years after the crisis. Further, this study investigated the buffering effects of perceived social support and social participation.
Research Design and Methods
Data were drawn from the 2011 China Health and Retirement Longitudinal Survey, including N = 4,341 Chinese adults aged 60 years and older. For the survey, local officials identified whether the 2003 SARS outbreak was one of the major disasters in the history of their communities. Depression was assessed by the Center for Epidemiological Studies-Depression scale and inflammation was measured by C-reactive protein (CRP) collected from participants via venous blood draws.
Results
Results from multilevel logistic regression models revealed that Chinese older adults living in communities exposed to SARS were more likely to have elevated CRP compared to those not living in such communities. Moreover, community SARS exposure was associated with greater risks of depression for Chinese older adults who had no perceived social support. Among Chinese older adults who had low levels of social participation, community SARS exposure was more strongly related to elevated CRP.
Discussion and Implications
Findings suggest community-level exposure to the SARS epidemic had enduring consequences for Chinese older adults’ health. However, active social participation and supportive social ties provided important resources that may buffer against negative effects of exposure to the SARS epidemic.
Keywords: Biomarkers, Epidemic, Health, Natural disaster, Social support
The current coronavirus disease 2019 (COVID-19) pandemic has revealed the vulnerability of many older adults to health problems associated not only with exposure to the disease itself, but also to the toxic stressors associated with living through this traumatic life event (Horesh & Brown, 2020). Because the pandemic is not under control, as there is no widely available vaccine or cure, it is impossible to understand the full nature of the consequences of this event for older adults throughout the world. In addition, there are few data sources available to researchers at this time to begin to study rigorously how this current disaster may affect the well-being of older adults—not only in the immediate term, but in the long term as well. Robust studies with high-quality national data will likely not be possible for years. Yet some insights may be drawn from similar recent events, such as the Severe Acute Respiratory Syndrome (SARS) outbreak of 2003.
Epidemic and pandemic events directly affect the health of individuals who are infected with the disease and suffer its effects. Such disasters also affect the health and well-being of those not directly infected, through the social isolation that results from being quarantined, losing a loved one, material deprivation, and experiencing survivor’s guilt (Bonanno et al., 2010; Norris & Wind, 2009). Further, the heightened possibility of infection through community exposure may act as a stressor, even for those who manage to avoid infection (Norris & Wind, 2009). Further, older adults’ social relationships—defined here by perceived social support and social participation—may act as buffers to trauma and stress associated with exposure to cataclysmic life events (Kaniasty, 2012). Social relationships may increase resiliency, which could help older adults cope with exposure to natural disasters.
We explore these possibilities by examining a unique data set from China that includes information about community exposure to an earlier coronavirus epidemic that caused great trauma and destruction, the SARS epidemic of 2003. SARS is genetically linked to COVID-19 and the two public health disasters have similarities, though the COVID-19 pandemic has been much more costly in terms of human of life and overall suffering. This study aims (a) to examine whether community exposure to the SARS epidemic is associated with depression and elevated inflammation levels among older Chinese adults 8 years following the disaster, and (b) to investigate whether negative health effects of exposure to the SARS epidemic vary according to the levels of social participation and/or perceived social support.
The 2003 SARS Epidemic
The COVID-19 virus continues to spread worldwide, but this is not the first global coronavirus outbreak. SARS, also caused by a coronavirus (SARS-Cov), is a highly contagious and potentially lethal disease. SARS made its first appearance in Guangdong Province, China, in 2002 and spread rapidly across 30 countries. By spring 2003, SARS had infected over 8,000 people and caused more than 800 deaths worldwide (World Health Organization, 2003a). The cumulative death toll was 349 out of 5,327 infection cases in mainland China and 300 out of 1,755 infection cases in Hong Kong (World Health Organization, 2003a).
The SARS epidemic was associated with high levels of psychological stress, including increased emotional distress (Liu et al., 2012), lower levels of subjective well-being (Lau et al., 2008), and higher rates of suicide (Chan et al., 2006). However, most research focused on the impact of SARS for survivors and health care workers in the epicenters of Guangdong Province and Hong Kong. Research is sparse regarding the long-term health consequence of SARS for older adults among the general population.
Trauma, Stress, and Health Consequences of Disaster Exposure
The stress process model (Pearlin & Bierman, 2013) serves as a framework for understanding how disasters affect people’s well-being. According to the stress process model, primary stressors, including stressful life events as well as chronic stressors, can undermine long-term health via psychological, social, and physiological mechanisms (Pearlin & Bierman, 2013). Public health disasters are traumatic life events with profound implications for people who are directly or indirectly exposed to the disaster. Although disasters often strike swiftly, the physical and psychological consequences may be long-lasting (Bonanno et al., 2010).
Extensive research has examined the health implications of disasters, including terrorist attacks, earthquakes, floods, famines, tornados, and disease epidemics (Norris & Wind, 2009). In addition to the direct fatalities and serious injuries resulting from disasters, disaster exposure takes a heavy toll on physical health. For instance, a prospective study found that people reported a decrease in self-reported health after experiencing a flood in South Korea (Heo et al., 2008). Another study found increased risks for cardiovascular disease and pneumonia among people who experienced the Great East Japan Earthquake (Aoki et al., 2012).
Moreover, serious psychological harm can result from disaster exposure. Studies indicate disasters increase risk for posttraumatic stress disorder, anxiety disorders, panic disorder, suicidality, and other psychiatric disorders (Norris & Elrod, 2006). Many people also express negative psychological responses, such as confusion and anger, from being quarantined during the current pandemic (Brooks et al., 2020). Disaster-related stress disorders are also linked to inflammation (Solomon et al., 2017) and depression (Bonanno et al., 2010), and these two health outcomes often co-occur (Valkanova et al., 2013).
Although limited, research is growing that investigates detrimental consequences of disaster exposure for mental and physical health among older adults. Some studies suggest advanced age is protective against disaster-related psychopathology because older adults have better coping skills based on earlier life experiences (Huang & Zhao, 2020). However, older adults are more vulnerable to disasters than younger persons because of their predisaster health conditions, decreased sensory awareness, physical impairments, and lower socioeconomic status (Lau et al., 2008). The current COVID-19 pandemic demonstrates that older adults are especially vulnerable to infection and hospitalization, as well as having a higher mortality risk (Le Couteur et al., 2020). In turn, this may lead to heightened stress responses among older adults who fear infection, even if such infection does not occur, or results in eventual recovery (Chan et al., 2006). Thus, it is crucial to understand the long-term consequences of disaster exposure among the older population.
Social Participation and Perceived Support
The stress process model posits that people exposed to similar types and intensities of stressors may not exhibit similar outcomes, due to buffering factors (Pearlin & Bierman, 2013). Social participation and social support, which emanate from people’s social capital, play important roles in buffering stress (Pearlin & Bierman, 2013). Engaging in social activities promotes healthy aging by fulfilling older adults’ psychological and social needs, and active social participation contributes to a sense of self-efficacy and mastery for older adults. Social participation also benefits older people by providing opportunities to form social networks and exchange emotional intimacy, resulting in higher levels of perceived connectedness and lower levels of loneliness (Choi et al., 2020). However, social activity engagement does not guarantee the formation of high-quality social relationships, which are the source for perceived availability of support. Perceived support serves as a protective factor for older adults’ mental health by offering a sense of comfort and security. Both social participation and perceived availability of support are found to be associated with depression (Choi et al., 2020; Silverstein et al., 2020) and inflammation among older adults (Lee & Way, 2019).
Empirical evidence demonstrates that active social participation is associated with lower psychological distress (Matsuyama et al., 2016), and the lack of a robust social network was associated with moderate to serious mental health problems after the Great East Japan Earthquake (Yokoyama et al., 2014). The benefits of perceived social support for physical and mental health after a disaster are well-documented (Cherry et al., 2015; Norris & Elrod, 2006). Research shows that social support from network members aids those affected and contributes to a faster recovery from the negative consequences of exposure to disasters (Kaniasty, 2012). This is in part because survivors with high social capital have better access to resources in their community, such as financial, physical, and informational support (Aldrich, 2011). In China, adults with more social support showed lower risk of depression 6 months after the 2008 Wenchuan earthquake (Guo et al., 2015). However, research on the buffering effects of social participation and social support for SARS exposure and older adults’ health is lacking.
The Present Study
Using nationally representative data from the 2011 China Health and Retirement Longitudinal Survey (CHARLS), we examine 2003 SARS epidemic exposure at the community level and its implications for two health outcomes among Chinese older adults: depression and elevated inflammation. We also examine two potential buffers of the negative implications of SARS exposure for health: social participation and perceived social support. Specifically, we test the following hypotheses:
Hypothesis 1: Chinese older adults living in communities exposed to the SARS epidemic are more likely to (a) be depressed and (b) have elevated inflammation compared to those not living in communities exposed to SARS.
Hypothesis 2: The associations between community-level SARS exposure and both depression and elevated inflammation will be weaker among Chinese older adults who report having perceived support compared to those who report lacking perceived support.
Hypothesis 3: The associations between community-level SARS exposure and both depression and elevated inflammation will be weaker for Chinese older adults who report higher levels of social participation.
Method
Data and Sample
Data were taken from the 2011 wave of CHARLS, a nationally representative survey of Chinese adults aged 45 and older (Zhao et al., 2014). CHARLS adopted a stratified multistage (province–county/district–village/neighborhood) random probability sampling strategy, interviewing 17,708 residents from 450 communities across 28 provinces in China (response rate = 80.5%). For the 2011 wave, a venous blood sample was collected from participants by medically trained China Center for Disease Control and Prevention (CDC) staff. Among participants, 11,847 (67.0%) provided fasting blood samples from which biomarkers were identified (Zhao et al., 2014). CHARLS included a questionnaire regarding the social, economic, history, and policy environments of the community, based on professional interviewers’ observations and on interviews with knowledgeable community leaders. We obtained a measure of SARS exposure in the community from the CHARLS community survey (only available in the 2011 wave).
Our analysis included participants who were aged 60 years and older in 2011, and who provided fasting blood samples as part of the biomarker survey (n = 5,099). We excluded participants who moved to the survey community after the initial SARS disease appearance in 2002 (n = 758), resulting in a final study sample of 4,341 participants from 419 communities. We also used variables from the Harmonized CHARLS data files produced by the Center for Economic and Social Research at the University of Southern California.
Measures
Inflammation
We assessed inflammation using levels of C-reactive protein (CRP) from venous blood tests. CRP is a marker of systemic inflammation sensitive to chronic stress, and a predictor of cardiovascular disease, functional decline, and mortality (Kiecolt-Glaser et al., 2010). Other inflammatory biomarkers such as interleukin-6 (IL-6) and tumor necrosis factor alpha (TNF-α) were not available in the CHARLS data. We created a dichotomous indicator of elevated inflammation based on a threshold of CRP scores greater than or equal to 3.0 mg/l, which is widely used as a clinical cut point for inflammation in older Chinese samples (Yeh & Willerson, 2003; Zhang & Crimmins, 2019).
Depression
Participants were asked to respond to 10 items from the Center for Epidemiological Studies-Depression scale (CES-D; Radloff, 1977). Response options varied from 0 (rarely or none of the time) to 3 (most or all the time). Summary scores ranged from 0 to 30 (α = 0.80). A threshold of 12 for the 10-item CES-D scale was validated and recommended for identifying probable clinical depression among Chinese older adults (Cheng & Chan, 2005). This threshold was used to create a dichotomous indicator of depression.
SARS exposure
In the community survey, local officials, or two to three older persons who were familiar with the history of community, provided information about the three most severe natural disasters or epidemics that occurred in their community since 1945. The list included floods, droughts, fires, earthquakes, typhoons, snow, and epidemics of hepatitis A, SARS, measles, Hand, Foot, and Mouth Disease, mumps, influenza A, and AIDS. We considered the community to be exposed to the SARS epidemic (1 = yes) if SARS was mentioned as one of the three natural disasters or epidemics in the community.
Because the measure of SARS exposure was based on a retrospective account, we sought to assess the validity of the measure by examining whether communities identified as having been exposed to SARS in the CHARLS data cohered with those areas of China known to have had elevated incidence of SARS during the 2003 epidemic (e.g., World Health Organization, 2003b). In the CHARLS data, communities identified as being exposed to SARS included those areas that experienced local transmission of SARS during the 2003 SARS epidemic (e.g., Beijing, Guangdong Province, and Hebei Province). Further, those communities known not to have been exposed to infection during the 2003 SARS epidemic are also consistently identified in the CHARLS (e.g., Heilongjiang Province and Yunnan Province; see Fang et al., 2009; World Health Organization, 2003b). Thus, we believe the measure of community-level SARS exposure has adequate construct validity for this study.
Social participation
Social participation was assessed by self-report of the frequency of engagement in eight activities in the month prior to the interview, including (a) interaction with friends, (b) playing Ma-jong/chess/cards or going to a community club, (c) providing help to family, friends, or neighbors, who did not live with the participant and who did not pay the participant for help, (d) going to a sport, social, or other kind of club, (e) taking part in a community-related organization, (f) doing voluntary or charity work, (g) caring for a sick or disabled adult who did not live with the participant and who did not pay the participant for help, and (h) attending an educational or training course. Each item was rated at 0 = not participating, 1 = not regularly, 2 = almost every week, and 3 = almost every day. A cumulative score was created to indicate level of social participation.
Perceived social support
Participants were asked “Suppose that in the future, you needed help with basic daily activities like eating or dressing. Do you have relatives or friends (besides your spouse/partner) who would be willing and able to help you over a long period of time?” Perceived social support was assessed as 1 = had perceived social support and 0 = no perceived social support.
Covariates
Individual characteristics included participants’ age (in years), gender (1 = female and 0 = male), education (1 = illiterate/no formal education [reference group], 2 = elementary school, 3 = middle school, 4 = high school or above), marital status (1 = married and 0 = divorced, never married, or widowed), urban–rural residence (1 = rural and 0 = urban), personal annual income (in yuan, transformed by the natural log), number of children, self-rated health (1 = fair or poor and 0 = good or excellent), activity of daily living limitations (a sum score of six items including dressing, eating, bathing, getting in and out of bed, using the toilet, and controlling urination), and instrumental activity of daily living limitations (a sum score of five items including managing money, taking medications, shopping for groceries, preparing meals, and house cleaning). Health behaviors included smoking (1 = never smoked, 2 = former smoker, and 3 = current smoker), alcohol consumption (1 = never drank, 2 = occasionally drink, and 3 = regularly drink), and vigorous physical activity (1 = no, 2 = yes, and 3 = no response due to survey design).
Community characteristics included neighborhood environment and infrastructure availability (Wang & Stokes, 2020). Neighborhood environment was measured by interviewers’ evaluation of community socioeconomic status (1 = poor to 7 = rich), tidiness of roads (1 = very dirty to 7 = very tidy), construction organization (1 = very disorganized to 7 = very organized), crowdedness (1 = very crowded to 7 = very sparse), handicapped access (1 = no handicapped access to 7 = very convenient), and Mandarin fluency (1 = cannot speak to 7 = fluent). A mean score was created with higher scores indicating a better environment (range = 1–7; α = .70). Infrastructure availability was measured by the availability of bus services, sewer systems, reconstructed toilet system, tap water, natural gas or liquefied gas, and waste management services (range = 0–6, α = .71).
Analytic Strategy
We first conducted bivariate analyses of individual and community characteristics by community-level SARS epidemic exposure. Next, we estimated multilevel logistic regression models for depression and elevated inflammation. Multilevel modeling was used to account for the nesting of individuals within communities (Snijders & Bosker, 2012). Interaction terms between SARS epidemic exposure and (a) social participation and (b) perceived social support were then included to examine potential moderation/buffering effects.
The vast majority (93%) of participants had complete information on all analytic variables. Missing data diagnostics revealed no clear pattern of missingness. Therefore, missing data were addressed using multiple imputation by chained equations (Royston, 2005). A total of 10 complete data sets generated and analyzed in Stata Version 16.
Results
Descriptive characteristics are presented in Table 1. Results from bivariate analyses showed that Chinese older adults living in communities exposed to the SARS epidemic were more likely to have elevated inflammation (26% vs 21%, p = .03) and perceived social support (74% vs 69%, p = .03) compared to their counterparts living in communities not exposed to SARS. However, they did not differ concerning depression (37% vs 33%, p = .09) or social participation (1.14 vs 1.19, p = .51).
Table 1.
Characteristics of Chinese Older Adults by Community SARS Epidemic Exposure From the CHARLS
| Variables | Full sample (N = 4,341) | Exposed to SARS (n = 492) | Not exposed to SARS (n = 3,849) | t or χ 2 | |||
|---|---|---|---|---|---|---|---|
| Mean/% | (SD) | Mean/% | (SD) | Mean/% | (SD) | ||
| Depression, % | 34 | 37 | 33 | ||||
| Inflammation, % | 22 | 26 | 21 | * | |||
| Social participationa | 1.19 | (1.70) | 1.14 | (1.77) | 1.19 | (1.70) | |
| Perceived social support, % | 70 | 74 | 69 | * | |||
| Individual characteristics | |||||||
| Age (in years) | 67.88 | (6.51) | 67.73 | (6.15) | 67.89 | (6.56) | |
| Female, % | 49 | 50 | 49 | ||||
| Education, % | |||||||
| Illiterate/no formal education | 61 | 56 | 61 | * | |||
| Elementary school | 24 | 23 | 25 | ||||
| Middle school | 11 | 15 | 10 | ** | |||
| High school or above | 4 | 6 | 3 | * | |||
| Married, % | 79 | 78 | 79 | ||||
| Number of children | 3.39 | (1.59) | 3.57 | (1.50) | 3.37 | (1.60) | ** |
| Income (in yuan) | 789.55 | (3,939) | 686.65 | (3,964) | 802.74 | (3,936) | |
| Rural residence, % | 69 | 66 | 69 | ||||
| ADL limitationsb | 0.57 | (1.24) | 0.65 | (1.30) | 0.56 | (1.24) | |
| IADL limitationsc | 0.70 | (1.29) | 0.74 | (1.33) | 0.69 | (1.29) | |
| Poor self-rated health, % | 35 | 36 | 35 | ||||
| Smoking, % | |||||||
| Never smoked | 57 | 60 | 57 | ||||
| Former smoker | 12 | 14 | 11 | ||||
| Current smoker | 31 | 26 | 32 | ** | |||
| Drinking alcohol, % | |||||||
| Never drank | 69 | 74 | 69 | * | |||
| Occasionally drink | 6 | 6 | 6 | ||||
| Regularly drink | 24 | 20 | 25 | * | |||
| Vigorous physical activity, % | |||||||
| No | 29 | 28 | 29 | ||||
| Yes | 12 | 11 | 12 | ||||
| No response | 59 | 60 | 59 | ||||
| Community characteristics | |||||||
| Neighborhood environmentd | 3.62 | (1.01) | 3.80 | (0.97) | 3.60 | (1.01) | |
| Infrastructure availibilitye | 2.71 | (1.90) | 3.23 | (1.89) | 2.64 | (1.89) | * |
Notes: ADL = activity of daily living; CHARLS = China Health and Retirement Longitudinal Survey; IADL = instrumental activity of daily living; SARS = Severe Acute Respiratory Syndrome; SD = standard deviation.
aSum score of eight items rated from 0 = did not participate to 3 = participated almost daily. bSum score of six ADL items coded as 1 = yes and 0 = no. cSum score of five IADL items coded as 1 = yes and 0 = no. dMean score of six items rated from 1 to 7. eSum score of six items coded as 1 = yes and 0 = no.
*p < .05. **p < .01.
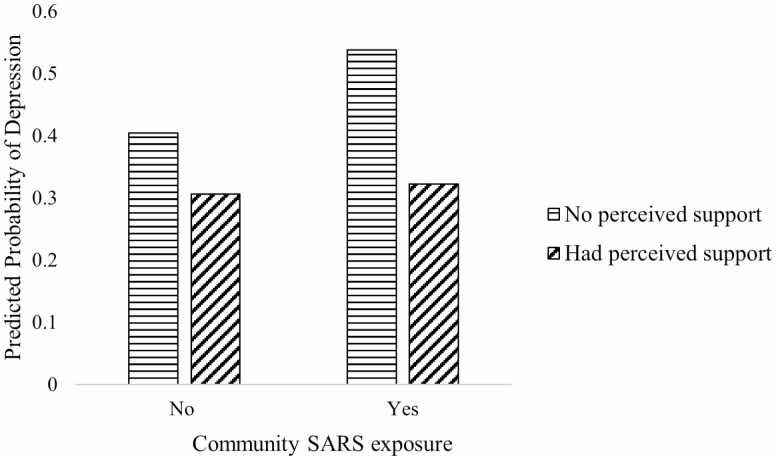
Table 2 presents results from multilevel logistic regression models concerning SARS epidemic exposure and depression. The results showed that living in communities exposed to SARS was not significantly associated with the risk of depression overall (Model 1). Older adults who perceived they had social support were at a lower risk of depression (Model 1: OR = 0.54, 95% CI = 0.45–0.65). We found a significant interaction between SARS exposure and perceived social support for older adults’ depression (Model 2: OR = 0.55, 95% CI = 0.32–0.94). In a stratified analysis (Supplementary Table 1), exposure to the SARS epidemic was significantly related to a higher risk of depression for Chinese older adults who reported no perceived social support (OR = 1.84, 95% CI = 1.15–2.93); however, the association between SARS exposure and depression was not significant for older adults who reported perceived social support (OR = 1.05, 95% CI = 0.73–1.52). Figure 1 illustrates how SARS exposure was related to the probability of depression depending on perceived social support (calculated from results in Model 2).
Table 2.
Results From Multilevel Logistic Models for Community SARS Epidemic Exposure and Depression Among Chinese Older Adults
| Variables | Model 1 | Model 2 | ||
|---|---|---|---|---|
| OR | [95% CI] | OR | [95% CI] | |
| Fixed effects | ||||
| SARS exposure | 1.30 | [0.97, 1.74] | 1.99** | [1.23, 3.21] |
| × Social participation | 1.03 | [0.89, 1.18] | ||
| × Perceived support | 0.55* | [0.32, 0.94] | ||
| Social participationa | 1.00 | [0.96, 1.05] | 1.00 | [0.95, 1.05] |
| Perceived social support | 0.54*** | [0.45, 0.65] | 0.58*** | [0.48, 0.70] |
| Individual characteristics | ||||
| Age | 0.98* | [0.97, 0.99] | 0.98* | [0.97, 0.99] |
| Female | 1.88*** | [1.51, 2.35] | 1.90*** | [1.52, 2.37] |
| Education (ref: no education) | ||||
| Elementary school | 1.04 | [0.86, 1.26] | 1.04 | [0.86, 1.26] |
| Middle school | 0.74* | [0.56, 0.99] | 0.74* | [0.56, 0.98] |
| High school and above | 0.68 | [0.42, 1.10] | 0.68 | [0.42, 1.10] |
| Married | 0.64*** | [0.53, 0.78] | 0.64*** | [0.53, 0.78] |
| Number of children | 1.06 | [0.99, 1.11] | 1.05 | [0.99, 1.11] |
| Income | 0.98 | [0.94, 1.02] | 0.98 | [0.94, 1.01] |
| Rural residence | 1.05 | [0.80, 1.37] | 1.04 | [0.80, 1.36] |
| ADL limitationsb | 1.26*** | [1.16, 1.37] | 1.26*** | [1.16, 1.37] |
| IADL limitationsc | 1.27*** | [1.18, 1.37] | 1.27*** | [1.18, 1.37] |
| Poor self-rated health | 2.55*** | [2.17, 3.00] | 2.54*** | [2.16, 2.99] |
| Smoking (ref: never smoked) | ||||
| Current smoker | 1.18 | [0.89, 1.57] | 1.19 | [0.90, 1.58] |
| Former smoker | 1.23 | [0.98, 1.53] | 1.23 | [0.99, 1.54] |
| Drink alcohol (ref: never drank) | ||||
| Occasionally drink | 0.98 | [0.69, 1.37] | 0.97 | [0.69, 1.36] |
| Regularly drink | 0.97 | [0.79, 1.19] | 0.96 | [0.79, 1.18] |
| Vigorous physical activity (ref: no) | ||||
| Yes | 1.23 | [0.95, 1.60] | 1.23 | [0.95, 1.60] |
| No response | 1.17 | [0.98, 1.38] | 1.17 | [0.98, 1.38] |
| Community characteristics | ||||
| Neighborhood environmentd | 0.97 | [0.86, 1.08] | 0.97 | [0.86, 1.08] |
| Infrastructure availibilitye | 0.88*** | [0.81, 0.96] | 0.88*** | [0.81, 0.95] |
| Random effects | B | (SE) | B | (SE) |
| Community variance | 0.31*** | (0.07) | 0.31*** | (0.07) |
Notes: N = 4,341. ADL = activity of daily living; CI = confidence interval; IADL = instrumental activity of daily living; OR = odds ratio; SARS = Severe Acute Respiratory Syndrome; SE = standard error.
aSum score of eight items rated from 0 = did not participate to 3 = participated almost daily. bSum score of six ADL items coded as 1 = yes and 0 = no. cSum score of five IADL items coded as 1 = yes and 0 = no. dMean score of six items rated from 1 to 7. eSum score of six items coded as 1 = yes and 0 = no.
*p < .05. **p < .01. ***p < .001.
Figure 1.
Community Severe Acute Respiratory Syndrome (SARS) epidemic exposure and perceived social support for depression among Chinese older adults. Notes: N = 4,341. Multilevel models were adjusted for individual- and community-level characteristics.
Table 3 shows results for multilevel logistic regression models concerning SARS epidemic exposure and elevated inflammation. Results indicated that living in communities exposed to the SARS epidemic was significantly associated with a higher risk of elevated CRP overall (Model 1: OR = 1.30, 95% CI = 1.01–1.69). Although social participation and perceived social support were not significantly associated with the risk of elevated CRP directly, we found a significant interaction between SARS exposure and social participation, indicating a buffering effect (Model 2: OR = 0.85, 95% CI = 0.74–0.99). In a stratified analysis separating older adults with high and low levels of social participation (Supplementary Table 2), community exposure to SARS was significantly associated with a higher risk of elevated CRP among those with low social participation (OR = 1.59, 95% CI = 1.15–2.20), but not among those with higher levels of social participation (OR = 0.80, 95% CI = 0.50–1.28). Figure 2 illustrates community exposure to the SARS epidemic and the probability of elevated CRP based on older adults’ social participation (calculated from results in Model 2).
Table 3.
Results From Multilevel Logistic Models for Community SARS Epidemic Exposure and Inflammation Among Chinese Older Adults
| Variables | Model 1 | Model 2 | ||
|---|---|---|---|---|
| OR | [95% CI] | OR | [95% CI] | |
| Fixed effects | ||||
| SARS exposure | 1.30* | [1.01, 1.69] | 0.97 | [0.59, 1.57] |
| × Social participation | 0.85* | [0.74, 0.99] | ||
| × Perceived social support | 1.47 | [0.85, 2.54] | ||
| Social participationa | 1.01 | [0.96, 1.06] | 1.03 | [0.98, 1.08] |
| Perceived social support | 0.90 | [0.76, 1.08] | 0.86 | [0.72, 1.04] |
| Individual characteristics | ||||
| Age | 1.02* | [1.00, 1.03] | 1.02* | [1.00, 1.03] |
| Female | 1.00 | [0.80, 1.24] | 1.00 | [0.80, 1.24] |
| Education (ref: no education) | ||||
| Elementary school | 0.99 | [0.82, 1.21] | 0.99 | [0.82, 1.21] |
| Middle school | 0.80 | [0.61, 1.06] | 0.81 | [0.61, 1.07] |
| High school and above | 1.05 | [0.70, 1.57] | 1.07 | [0.71, 1.60] |
| Married | 0.87 | [0.72, 1.06] | 0.87 | [0.72, 1.06] |
| Number of children | 1.06* | [1.00, 1.11] | 1.06* | [1.00, 1.11] |
| Income | 0.98 | [0.95, 1.02] | 0.98 | [0.95, 1.02] |
| Rural residence (ref: urban) | 0.89 | [0.70, 1.13] | 0.89 | [0.71, 1.14] |
| ADL limitationsb | 0.99 | [0.91, 1.07] | 0.99 [0.91, 1.07] | |
| IADL limitationsc | 1.08 | [0.99, 1.16] | 1.08 | [0.99, 1.16] |
| Poor self-rated health | 1.32** | 1.32** | 1.32** | [1.12, 1.57] |
| Smoking (ref: never smoked) | ||||
| Current smoker | 1.24 | [0.95, 1.64] | 1.23 | [0.94, 1.62] |
| Former smoker | 1.21 | [0.97, 1.51] | 1.21 | [0.97, 1.51] |
| Drinking alcohol (ref: never drank) | ||||
| Occasionally drink | 0.88 | [0.63, 1.24] | 0.89 | [0.64, 1.25] |
| Regularly drink | 1.02 | [0.84, 1.25] | 1.02 | [0.97, 1.25] |
| Vigorous physical activity (ref: no) | ||||
| Yes | 0.62** | [0.46, 0.83] | 0.62** | [0.46, 0.83] |
| No response | 0.90 | [0.76, 1.07] | 0.90 | [0.76, 1.07] |
| Community characteristics | ||||
| Neighborhood environmentd | 0.97 | [0.88, 1.08] | 0.97 | [0.87, 1.07] |
| Infrastructure availibilitye | 1.03 | [0.96, 1.10] | 1.03 | [0.96, 1.11] |
| Random effects | B | (SE) | B | (SE) |
| Community variance | 0.16** | (0.05) | 0.16** | (0.05) |
Notes: N = 4,341. ADL = activity of daily living; CI = confidence interval; IADL = instrumental activity of daily living; OR = odds ratio; SARS = Severe Acute Respiratory Syndrome; SE = standard error.
aSum score of eight items rated from 0 = did not participate to 3 = participated almost daily. bSum score of six ADL items coded as 1 = yes and 0 = no. cSum score of five IADL items coded as 1 = yes and 0 = no. dMean score of six items rated from 1 to 7. eSum score of six items coded as 1 = yes and 0 = no.
*p < .05. **p < .01.
Figure 2.
Community Severe Acute Respiratory Syndrome (SARS) epidemic exposure and social participation for inflammation among Chinese older adults. Notes: N = 4,341. Multilevel models were adjusted for individual- and community-level characteristics. Social participation was evaluated at low (1 SD below the mean) and high level (1 SD above the mean).
Discussion
Using a large national sample of Chinese older adults, this study examined the associations of community-level exposure to the 2003 SARS epidemic with risks of depression and elevated inflammation 8 years later. Findings demonstrated long-lasting harm for physiological health to Chinese older adults who lived in communities with exposure to SARS. Moreover, perceived social support and social participation emerged as salient protective factors for the health of Chinese older adults exposed to the SARS epidemic. Findings from this study offer important insights for future pandemic research among aging populations, especially for the rapidly developing COVID-19 pandemic.
Depression and Inflammation After the 2003 SARS Epidemic
Results from this study were mixed, yet highlight the potential long-term ramifications of community-level infectious disease exposure for older adults’ mental and physical health. Indeed, our findings suggest that even those who ultimately avoid infection are still at risk of experiencing negative health consequences years after the event has passed.
Unlike earlier studies that found increased depressive symptoms or higher depression risk after disaster exposure (Cherry et al., 2015), our results regarding depression risk following community exposure to SARS were fairly weak overall and offered little support for Hypothesis 1. Community-level SARS exposure was not related to the risk of depression overall, although the interaction term with perceived support was statistically significant. Results from a stratified model revealed a significant association between community-level SARS exposure and depression risk only among those who perceived a lack of social support. Overall, this may indicate emotional resilience following SARS exposure, at least among those with supportive networks, and those who survived to follow-up (Bonanno et al., 2008). People often have psychological trauma immediately after exposure to a disaster, yet they may cope with traumatic experiences and rebuild their psychological resilience as time passes (Pietrzak et al., 2012). Conversely, those who did not recover from trauma may be at higher risk of mortality, and unavailable to provide data years after an epidemic.
Results concerning elevated inflammation were stronger and more robust compared to depression. Our findings revealed that living in a community exposed to the SARS epidemic was related to a significantly higher risk of elevated CRP 8 years following the event. This is consistent with the stress process model (Pearlin & Bierman, 2013), and with empirical research on the health consequences of disasters (Norris & Elrod, 2006). These results also offer support for Hypothesis 1. Like other large-scale natural disasters, exposure to the SARS epidemic was a traumatic stressor, and older adults suffered from higher inflammation risk nearly a decade following the epidemic.
Elevated inflammation risk reflects some of the underlying physiological responses to a community-level traumatic stressor (Hänsel et al., 2010). Moreover, elevated CRP is a risk factor for cardiovascular disease, functional decline, and mortality (Zhang & Crimmins, 2019). Thus, our findings suggest health consequences of infectious disease epidemics, even for those individuals not directly affect or infected, may be quite long-lasting. Moreover, despite the apparent potential for psychological resilience, the physiological stress responses incited by SARS exposure may be more permanent, and thus, perhaps, more harmful in the long term.
Buffering Effects of Social Participation and Perceived Support
The impact of a disaster on health and well-being depends on a combination of risk and resilience factors (Bonanno et al., 2010). Our findings offered partial support for Hypotheses 2 and 3, which anticipated buffering effects of social support and social participation, as posited by the stress process model (Pearlin & Bierman, 2013). Results provided evidence for perceived support as a buffer for depression (Hypothesis 2) and social participation as a buffer for elevated inflammation (Hypothesis 3). Overall, findings were suggestive of the protective role that social capital and social relationships may play, even in the setting of an infectious disease epidemic. These findings are of particular interest, because many of the social partners and relationships these older adults engage with and rely on were likely also exposed to the SARS epidemic within the same community.
Although most disasters are unpredictable, prospective strengthening of social capital may lessen the long-term consequences for those exposed to the trauma associated with these events. Active social participation and supportive social ties are essential for healthy aging. Research has documented that social participation and support contribute to health and longevity for older adults (Sirven & Debrand, 2008). This study indicated that, even in circumstances that require social distancing and self-quarantine, efforts to bolster social capital and supportive relationships may be key, in both the immediate and the longer term. Results also suggested that social participation and support after the SARS epidemic event may be important in facilitating resilience and recovery (Bonanno et al., 2008). Thus, maintaining active social participation throughout life, and building social capital that yields effective social support in times of need, provides resilient coping strategies for older adults, even when disasters are not predictable.
Limitations
The research design was cross-sectional and based on observational data, limiting causal inference. Second, the measure of community-level exposure to the SARS epidemic was based on retrospective reports from local residents or community officials familiar with their community’s history. Because the CHARLS did not provide community identifiers, to protect confidentiality, this study was not able to use objective information from the China CDC to validate the incidence and severity of SARS exposure across all communities. Moreover, because the retrospective reports concerned the three most severe natural disasters or epidemics that occurred in the community since 1945, SARS exposure may not be reported by community representatives due to other more severe or more recent disasters in the community. Thus, this measure is subject to potential recall bias. Third, there was no information available in CHARLS concerning pre-SARS health conditions, or concerning participants’ actual or perceived individual exposure to SARS, and these factors may confound associations between community-level SARS exposure and older adults’ health. Future research concerning COVID-19 and other public health disasters may benefit from prospective longitudinal data analysis.
Potential confounders unavailable in the CHARLS data may also explain the implications of epidemic disaster exposure. Personality traits and coping styles may alter the effects of stressful events such as disaster and trauma on health, through appraisal and stress reduction (Riolli et al., 2002). During the epidemic, people may have experienced worries, fear of infection, discrimination of being potential SARS patients, and social isolation (Boyraz et al., 2020), and they may suffer from the loss of loved ones (Verdery et al., 2020). These psychological stressors may lead to acute mental disease and long-term health deterioration. In addition, there is a possibility of other unmeasured environmental factors, such as the perceived cohesion of neighborhoods and availability of relatives in the same neighborhood, that may partially explain the associations between epidemic exposure and older adults’ health.
Implications for Policy and Future Research
One of the central contributions of this study is that its findings set a baseline for future research on COVID-19 and its consequences for older adults. SARS and COVID-19 have similar epidemiological and clinical features (Xu et al., 2020), and their similarities include that both: (a) are novel and highly contiguous; (b) require testing and quarantine; (c) evidenced sudden onset and rapid spread; and (d) created large-scale public health emergencies. In addition, older adults were at higher risk of infection and mortality during the 2003 SARS and COVID-19 crises. Differences include that the 2003 SARS event was felt most heavily in urban China, whereas COVID-19 became a global pandemic with a much higher mortality count and economic impact. Yet even these differences served to underscore the importance of the present findings. Given the unprecedented scale of the COVID-19 pandemic, it is likely that its experience as a traumatic stressor is greater and more enduring than that of the 2003 SARS epidemic, even among those who avoid infection. The need to identify factors associated with resilience and recovery among the older population are of the utmost importance (Horesh & Brown, 2020).
Policymakers should provide resources to improve access to social support and participation in activities among older adults in the communities in which they reside, even and especially under circumstances of social distancing and quarantine. Such programs may help enhance resilience and buffer against the harmful effects of COVID-19 exposure and its related stress experiences among the older population. These activities may also help older adults build and maintain social capital for the future, as a source of social support in times of need, the most extreme of which may be largely unpredictable.
Conclusion
The present study makes several contributions to the growing literature concerning regional and global disasters and older adults’ health. Findings showed that health effects from exposure to disaster events, including the 2003 SARS epidemic, are long-lasting. This was particularly evident concerning elevated inflammation, indicating that stress from exposure to such disasters may “get under the skin.” Further, although evidence was somewhat mixed, both perceived social support and social participation emerged as stress buffers. As researchers and policymakers prepare for the long-term consequences of the COVID-19 pandemic, the present study offers both a baseline and a roadmap for examining such effects among the older population.
Supplementary Material
Funding
Dr. Wang acknowledges support from the National Institute on Aging (1R01AG060949); the Pennsylvania State University Population Research Institute, which is supported by an infrastructure grant by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2C-HD041025). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or other funding sources.
Conflict of Interest
None declared.
References
- Aldrich, D. P (2011). Ties that bond, ties that build: Social capital and governments in post disaster recovery. Studies in Emergent Order, 4, 58–68. [Google Scholar]
- Aoki, T., Fukumoto, Y., Yasuda, S., Sakata, Y., Ito, K., Takahashi, J., Miyata, S., Tsuji, I., & Shimokawa, H (2012). The Great East Japan Earthquake disaster and cardiovascular diseases. European Heart Journal, 33(22), 2796–2803. doi: 10.1093/eurheartj/ehs288 [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A., Brewin, C. R., Kaniasty, K., & Greca, A. M (2010). Weighing the costs of disaster: Consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest, 11(1), 1–49. doi: 10.1177/1529100610387086 [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A., Ho, S. M., Chan, J. C., Kwong, R. S., Cheung, C. K., Wong, C. P., & Wong, V. C (2008). Psychological resilience and dysfunction among hospitalized survivors of the SARS epidemic in Hong Kong: A latent class approach. Health Psychology, 27(5), 659–667. doi: 10.1037/0278-6133.27.5.659 [DOI] [PubMed] [Google Scholar]
- Boyraz, G., Legros, D. N., & Tigershtrom, A (2020). COVID-19 and traumatic stress: The role of perceived vulnerability, COVID-19-related worries, and social isolation. Journal of Anxiety Disorders, 76, 102307. doi: 10.1016/j.janxdis.2020.102307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., & Rubin, G. J (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 396(10227), 912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, S. M. S., Chiu, F. K. H., Lam, C. W. L., Leung, P. Y. V., & Conwell, Y (2006). Elderly suicide and the 2003 SARS epidemic in Hong Kong. International Journal of Geriatric Psychiatry, 21(2), 113–118. doi: 10.1002/gps.1432 [DOI] [PubMed] [Google Scholar]
- Cheng, S. T., & Chan, A. C (2005). The Center for Epidemiologic Studies Depression Scale in older Chinese: Thresholds for long and short forms. International Journal of Geriatric Psychiatry, 20(5), 465–470. doi: 10.1002/gps.1314 [DOI] [PubMed] [Google Scholar]
- Cherry, K. E., Sampson, L., Nezat, P. F., Cacamo, A., Marks, L. D., & Galea, S (2015). Long-term psychological outcomes in older adults after disaster: Relationships to religiosity and social support. Aging & Mental Health, 19(5), 430–443. doi: 10.1080/13607863.2014.941325 [DOI] [PubMed] [Google Scholar]
- Choi, E., Han, K. M., Chang, J., Lee, Y. J., Choi, K. W., Han, C., & Ham, B. J (2020). Social participation and depressive symptoms in community-dwelling older adults: Emotional social support as a mediator. Journal of Psychiatric Research. Advanced online publication. doi: 10.1016/j.jpsychires.2020.10.043 [DOI] [PubMed] [Google Scholar]
- Fang, L. Q., de Vlas, S. J., Feng, D., Liang, S., Xu, Y. F., Zhou, J. P., Richardus, J. H., & Cao, W. C (2009). Geographical spread of SARS in mainland China. Tropical Medicine & International Health, 14(Suppl. 1), 14–20. doi: 10.1111/j.1365-3156.2008.02189.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, S., Tian, D., Wang, X., Xiao, Y., He, H., Qu, Z., & Zhang, X (2015). Protective effects of social support content and support source on depression and its prevalence 6 months after Wenchuan earthquake. Stress & Health, 31(5), 382–392. doi: 10.1002/smi.2563 [DOI] [PubMed] [Google Scholar]
- Hänsel, A., Hong, S., Cámara, R. J., & von Känel, R (2010). Inflammation as a psychophysiological biomarker in chronic psychosocial stress. Neuroscience and Biobehavioral Reviews, 35(1), 115–121. doi: 10.1016/j.neubiorev.2009.12.012 [DOI] [PubMed] [Google Scholar]
- Heo, J. H., Kim, M. H., Koh, S. B., Noh, S., Park, J. H., Ahn, J. S., Park, K. C., Shin, J., & Min, S (2008). A prospective study on changes in health status following flood disaster. Psychiatry Investigation, 5(3), 186–192. doi: 10.4306/pi.2008.5.3.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh, D., & Brown, A. D (2020). Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice and Policy, 12(4), 331–335. doi: 10.1037/tra0000592 [DOI] [PubMed] [Google Scholar]
- Huang, Y., & Zhao, N (2020). Chinese mental health burden during the COVID-19 pandemic. Asian Journal of Psychiatry, 51, 102052. doi: 10.1016/j.ajp.2020.102052 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Kaniasty, K (2012). Predicting social psychological well-being following trauma: The role of postdisaster social support. Psychological Trauma: Theory, Research, Practice, and Policy, 4(1), 22–33. doi: 10.1037/a0021412 [DOI] [Google Scholar]
- Kiecolt-Glaser, J. K., Gouin, J. P., & Hantsoo, L (2010). Close relationships, inflammation, and health. Neuroscience and Biobehavioral Reviews, 35(1), 33–38. doi: 10.1016/j.neubiorev.2009.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau, A. L., Chi, I., Cummins, R. A., Lee, T. M., Chou, K. L., & Chung, L. W (2008). The SARS (Severe Acute Respiratory Syndrome) pandemic in Hong Kong: Effects on the subjective wellbeing of elderly and younger people. Aging & Mental Health, 12(6), 746–760. doi: 10.1080/13607860802380607 [DOI] [PubMed] [Google Scholar]
- Le Couteur, D. G., Anderson, R. M., & Newman, A. B (2020). COVID-19 through the lens of gerontology. The Journals of Gerontology, Series A: Biological Science and Medical Science, 75(9), e119–e120. doi: 10.1093/gerona/glaa077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, D. S., & Way, B. M (2019). Perceived social support and chronic inflammation: The moderating role of self-esteem. Health Psychology, 38(6), 563–566. doi: 10.1037/hea0000746 [DOI] [PubMed] [Google Scholar]
- Liu, X., Kakade, M., Fuller, C. J., Fan, B., Fang, Y., Kong, J., Guan, Z., & Wu, P (2012). Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Comprehensive Psychiatry, 53(1), 15–23. doi: 10.1016/j.comppsych.2011.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuyama, Y., Aida, J., Hase, A., Sato, Y., Koyama, S., Tsuboya, T., & Osaka, K (2016). Do community and individual-level social relationships contribute to the mental health of disaster survivors?: A multilevel prospective study after the Great East Japan Earthquake. Social Science & Medicine, 151, 187–195. doi: 10.1016/j.socscimed.2016.01.008 [DOI] [PubMed] [Google Scholar]
- Norris, F. H., & Elrod, C. L (2006). Psychosocial consequences of disaster: A review of past research. In Norris F. H., Galea S., Friedman M. J., & Watson P. J. (Eds.). Methods for disaster mental health research (pp. 20–42). The Guilford Press. [Google Scholar]
- Norris, F. H., & Wind, L. H (2009). The experience of disaster: Trauma, loss, adversities, and community effects. In Neria Y., Galea S., & Norris F. H. (Eds.), Mental health and disasters (pp. 29–44). Cambridge University Press. [Google Scholar]
- Pearlin, L. I., & Bierman, A (2013) Current issues and future directions in research into the stress process. In Aneshensel C. S., Phelan J. C., & Bierman A. (Eds.), Handbook of the sociology of mental health. Springer. [Google Scholar]
- Pietrzak, R. H., Tracy, M., Galea, S., Kilpatrick, D. G., Ruggiero, K. J., Hamblen, J. L., Southwick, S. M., & Norris, F. H (2012). Resilience in the face of disaster: Prevalence and longitudinal course of mental disorders following Hurricane Ike. PLoS One, 7(6), e38964. doi: 10.1371/journal.pone.0038964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff, L. S (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Riolli, L., Savicki, V., & Cepani, A (2002). Resilience in the face of catastrophe: Optimism, personality, and coping in the Kosovo crisis. Journal of Applied Social Psychology, 32(8), 1604–1627. doi: 10.1111/j.1559-1816.2002.tb02765.x [DOI] [Google Scholar]
- Royston, P (2005). Multiple imputation of missing values: Update of ice. The Stata Journal, 5, 527–536. doi: 10.1177/1536867X0500500404 [DOI] [Google Scholar]
- Silverstein, M., Gong, C. H., & Kendig, H (2020). Perceived availability of future care and depressive symptoms among older adults in China: Evidence from CHARLS. BMC Geriatrics, 20(1), 31. doi: 10.1186/s12877-020-1435-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirven, N., & Debrand, T (2008). Social participation and healthy ageing: An international comparison using SHARE data. Social Science & Medicine (1982), 67(12), 2017–2026. doi: 10.1016/j.socscimed.2008.09.056 [DOI] [PubMed] [Google Scholar]
- Snijders, T. A. B., and Bosker, R. J (2012). Multilevel analysis: An introduction to basic and advanced multilevel modeling (2nd ed.). Sage Publications. [Google Scholar]
- Solomon, Z., Levin, Y., Assayag, E. B., Furman, O., Shenhar-Tsarfaty, S., Berliner, S., & Ohry, A (2017). The implication of combat stress and PTSD trajectories in metabolic syndrome and elevated C-reactive protein levels: A longitudinal study. The Journal of Clinical Psychiatry, 78(9), e1180–e1186. doi: 10.4088/JCP.16m11344 [DOI] [PubMed] [Google Scholar]
- Valkanova, V., Ebmeier, K. P., & Allan, C. L (2013). CRP, IL-6 and depression: A systematic review and meta-analysis of longitudinal studies. Journal of Affective Disorders, 150(3), 736–744. doi: 10.1016/j.jad.2013.06.004 [DOI] [PubMed] [Google Scholar]
- Verdery, A. M., Smith-Greenaway, E., Margolis, R., & Daw, J (2020). Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proceedings of the National Academy of Sciences of the United States of America, 117(30), 17695–17701. doi: 10.1073/pnas.2007476117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, H., & Stokes, J. E (2020). Trajectories of rural-urban disparities in biological risks for cardiovascular disease among Chinese middle-aged and older adults. Health & Place, 64, 102354. doi: 10.1016/j.healthplace.2020.102354 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2003a). Summary table of SARS cases by country, 1 November 2002–7 August 2003 http://www.who.int/csr/sars/country/en/country2003_08_15.pdf
- World Health Organization (2003b). Summary table of areas that experienced local transmission of SARS during the outbreak period from 1 November 2002 to 31 July 2003 https://www.who.int/csr/sars/areas/areas2003_11_21/en/
- Xu, J., Zhao, S., Teng, T., Abdalla, A. E., Zhu, W., Xie, L., Wang, Y., & Guo, X (2020). Systematic comparison of two animal-to-human transmitted human coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses, 12(2), 244. doi: 10.3390/v12020244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh, E. T., & Willerson, J. T (2003). Coming of age of C-reactive protein: Using inflammation markers in cardiology. Circulation, 107(3), 370–371. doi: 10.1161/01.cir.0000053731.05365.5a [DOI] [PubMed] [Google Scholar]
- Yokoyama, Y., Otsuka, K., Kawakami, N., Kobayashi, S., Ogawa, A., Tannno, K., Onoda, T., Yaegashi, Y., & Sakata, K (2014). Mental health and related factors after the Great East Japan earthquake and tsunami. PLoS One, 9(7), e102497. doi: 10.1371/journal.pone.0102497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. S., & Crimmins, E. M (2019). Urban–rural differentials in age-related biological risk among middle-aged and older Chinese. International Journal of Public Health, 64(6), 831–839. doi: 10.1007/s00038-018-1189-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao, Y., Hu, Y., Smith, J. P., Strauss, J., & Yang, G (2014). Cohort profile: The China Health and Retirement Longitudinal Study (CHARLS). International Journal of Epidemiology, 43(1), 61–68. doi: 10.1093/ije/dys203 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.